Abstract
Background
Novel variants of concern (VOCs) have been associated with both increased infectivity and virulence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The virulence of SARS-CoV-2 is closely linked to age. Whether relative increases in virulence of novel VOCs are similar across the age spectrum or are limited to some age groups is unknown.
Methods
We created a retrospective cohort of people in Ontario, Canada, who tested positive for SARS-CoV-2 and were screened for VOCs (n = 259 984) between 7 February 2021 and 31 October 2021. Cases were classified as N501Y-positive VOC, probable Delta VOC, or VOC undetected. We constructed age-specific logistic regression models to evaluate associations between N501Y-postive or Delta VOC infections and infection severity using hospitalization, intensive care unit (ICU) admission, and death as outcome variables. Models were adjusted for sex, comorbidity, vaccination status, and temporal trends.
Results
Infection with either N501Y-positive or Delta VOCs was associated with significant elevations in risk of hospitalization, ICU admission, and death across age groups compared with infections where a VOC was not detected. The Delta VOC increased hospitalization risk in children aged <10 years by a factor of 2.5 (adjusted odds ratio; 95% confidence interval, 1.3 to 5.0) compared with non-VOCs. There was a significant inverse relationship between age and relative increase in risk of death with the Delta VOC, with younger age groups showing a greater relative increase in risk of death than older individuals.
Conclusions
SARS-CoV-2 VOCs appear to be associated with increased relative virulence of infection in all age groups, though low absolute numbers of outcomes in younger individuals make estimates in these groups imprecise.
Keywords: SARS coronavirus-2, virulence, health outcomes, epidemiology, age
Variants of concern for severe acute respiratory syndrome coronavirus 2 have been associated with overall increases in virulence. We found that variants with the N501Y mutation, as well as Delta variants, increase the severity of illness in both younger and older age groups.
Emerging severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants of concern (VOCs) have displayed increased infectivity as well as increased virulence relative to strains that circulated early in the pandemic [1–7]. In particular, the emergence of the highly infectious and virulent Delta variant has led to revised expectations of the pandemic’s severity and duration [8–11]. Notwithstanding the severe health and economic toll the SARS-CoV-2 pandemic has taken worldwide, one relatively assuasive aspect of its epidemiology had been decreased virulence of infection in children, with nearly 50% of infected children experiencing asymptomatic infection [12, 13]. However, in the summer of 2021, both the United Kingdom and the United States reported an extraordinary surge in pediatric hospitalizations related to SARS-CoV-2 infection [14–17]. The coincidence of this surge with Delta variant emergence in both countries has led some to suggest that this surge was driven by Delta variant emergence. However, surging admissions could simply reflect the increased infectivity of the Delta variant, resulting in larger numbers of infected children without any change in per-infection virulence. As such, it has been challenging to determine with certainty whether infection with the Delta VOC is more virulent in children than non-VOC SARS-CoV-2 or other VOCs, such as those with the N501Y mutation [18].
Indeed, heterogeneity in the effects of VOCs by age, more generally, would be of importance for understanding the likely impacts of future pandemic waves, as well as the epidemiology of SARS-CoV-2 in the post-pandemic era. In the Canadian province of Ontario, the VOC carrying the N501Y mutation (including the Alpha/B.1.1.7, Beta/B.1.351, and Gamma/P.1 VOC) replaced earlier SARS-CoV-2 lineages by April 2021 but were, in turn, replaced by the Delta (B.1.617.2) variant, which has been the dominant variant in the province since July 2021 [19, 20]. The availability of a single master dataset of all coronavirus disease 2019 (COVID-19) cases in the Canadian province of Ontario, which includes patient outcomes (hospitalization, intensive care unit [ICU] admission, and/or death), important covariates including underlying medical conditions, and virological typing data from February 2021 forward, provides an opportunity to evaluate age-specific risk associated with VOC infection and to determine whether there is heterogeneity in virulence across age groups. Our objectives were to estimate age-specific risks of severe illness in individuals infected with the Delta or N501Y-positive VOC relative to non-VOC SARS-CoV-2 infection, determine whether there is heterogeneity in differential risk by age group, and explore the possible sources of any such heterogeneity.
METHODS
Data Sources
We used Ontario’s Case and Contact Management (CCM) database to create a retrospective cohort of SARS-CoV-2 cases who underwent screening for VOCs and had test report dates between 7 February 2021 and 31 October 2021 (as routine screening for N501Y and E484K mutations began on 7 February 2021). Case information, including long-term care residence, demographics, underlying medical conditions, and outcomes including hospitalization, ICU admission, and death, is available in CCM [21]. Case vaccination status, including dates of first and second doses of SARS-CoV-2 vaccines, was obtained from COVaxON, Ontario’s centralized COVID-19 vaccine database. Individuals were considered partially vaccinated if 14 or more days had elapsed between the first vaccine dose and case episode date, considered fully vaccinated if the case episode date occurred 7 or more days after receipt of the second dose, and otherwise were considered unvaccinated [22, 23]. Note that there were 41 cases classified as fully vaccinated who had received 3 doses prior to their infection.
There has been an evolution in VOC screening and viral sequencing in Ontario over the course of the pandemic. VOC cases were initially identified in Ontario in December 2020, with subsequent targeted screening of isolates from individuals with a history suggestive of possible VOC infection (eg, travel). Systematic screening for VOCs with a low cycle threshold (<35) began in February 2021. Initial screening focused on the N501Y mutation, with screening for both N501Y and E484K initiated in March 2020. At that time, a 5% sampling of specimens was subjected to further sequencing regardless of screen results was initiated, with the fraction increased to 50% by late May 2021. As of June 2021, routine sequencing was discontinued on N501Y-positive/E484-negative specimens, which were presumed to be the Alpha lineage. The Alpha lineage (rather than Beta or Gamma) represented the overwhelming majority of Ontario’s N501Y-positive isolates [24]. More than 90% of infections were positive for the N501Y mutation as of April 2021, but that fraction decreased subsequently with emergence of the Delta variant, which represented more than 60% of all infections by July 2021 [19, 20, 24]. We excluded cases if VOC screening information was unavailable or screening had not been performed (N = 58 988).
Analysis
We constructed age group–specific logistic regression models for associations between N501Y-positive or Delta VOC infection and infection severity, defined as hospitalization, ICU admission, or death. Non-VOC infections were used as the referent. Models were adjusted for male sex, time (modeled as a week-on-week cubic trend), vaccination status (in age groups ≥10 years, since vaccination had not yet been approved for this age group [25]), documented major comorbidity (including asthma, chronic obstructive pulmonary disease, hematological disease, liver disease, cardiac disease, diabetes, renal disease, neurological disease, malignancy, or obesity), and being immune compromised. In relevant age groups, we also adjusted for documented pregnancy, long-term care residence, and healthcare worker status. Due to geographic variation in timing of the emergence of variants, we also adjusted for health unit region, with health units classified as “greater Toronto-Hamilton area,” “Ottawa,” and “other.” All of these covariates were expected a priori to confound the association between VOC exposure and disease severity. We considered odds ratios to approximate relative risks under the “rare disease assumption” [26].
As our major focus in this analysis was to identify and explore sources of heterogeneity across age groups, we made use of meta-analysis as an easily applicable, familiar, and interpretable set of statistical and graphical tools focused on heterogeneity [21, 27]. Alternate approaches (such as using multiplicative interaction terms for age groups and infecting variants) would also have been possible. Adjusted odds ratios and confidence intervals for relative severity of VOC from age group–specific models were incorporated into random effects meta-analyses to generate summary estimates of effect and to evaluate heterogeneity in effects by variant and age. Heterogeneity by age was assessed by constructing meta-regression models in which age group was treated as an ordinal variable in order to identify linear trends in effect across age groups.
We conducted regression analyses in R version 4.1.0; meta-analyses and meta-regression were performed using the meta package in R [28, 29]. The study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for observational research [30] and received ethics approval from the University of Toronto Research Ethics Board.
RESULTS
We included 259 984 cases in our analysis, with episode dates between 7 February 2021 and 31 October 2021. Among all reported cases, 64.6% were infections with the N501Y-positive VOC; 19.1% were classified as probable Delta infections. There were significant differences in hospitalization and ICU admission according to VOC status (Table 1). Individuals with a VOC were significantly younger and less likely to have comorbidities than individuals without a VOC. Significant differences were also seen in healthcare worker status, long-term care residence, and geographic location by VOC status. Cases infected with the Delta variant were more likely to be fully vaccinated, reflecting the fact that Delta became established in the population in the spring of 2020 once vaccination programs were underway.
Table 1.
Characteristics of Study Cohort With Test Date Between 7 February 2021 and 30 August 2021 by Variant of Concern Status
| Descriptor | All | VOC Not Detected | N501Y-Positive VOC | Probable Delta VOC | P Valuea |
|---|---|---|---|---|---|
| Total cases | 259 984 | 42 419 | 167 938 | 49 627 | |
| Hospitalized (%) | 13 517 (5.2) | 1814 (4.3) | 9112 (5.4) | 2591 (5.2) | <.001 |
| Admitted to intensive care unit | 2928 (1.1) | 298 (0.7) | 1980 (1.2) | 650 (1.3) | <.001 |
| Died | 2426 (0.9) | 401 (0.9) | 1572 (0.9) | 453 (0.9) | .86 |
| Male (%) | 131 910 (50.7) | 21 540 (50.8) | 85 432 (50.9) | 24 938 (50.3) | .052 |
| Age, years | <.001 | ||||
| <10 | 21 030 (8.1) | 2940 (6.9) | 12 176 (7.3) | 5914 (11.9) | |
| 10–19 | 31 586 (12.1) | 5107 (12) | 20 006 (11.9) | 6473 (13) | |
| 20–29 | 54 003 (20.8) | 8353 (19.7) | 34 831 (20.7) | 10 819 (21.8) | |
| 30–39 | 44 870 (17.3) | 7007 (16.5) | 28 800 (17.1) | 9063 (18.3) | |
| 40–49 | 37 956 (14.6) | 6011 (14.2) | 25 438 (15.1) | 6507 (13.1) | |
| 50–59 | 34 609 (13.3) | 6098 (14.4) | 23 412 (13.9) | 5099 (10.3) | |
| 60–69 | 21 136 (8.1) | 3869 (9.1) | 13 984 (8.3) | 3283(6.6) | |
| 70–79 | 9475 (3.6) | 1865 (4.4) | 6092 (3.6) | 1518 (3.1) | |
| ≥80 | 5319 (2) | 1169 (2.8) | 3199 (1.9) | 9,51 (1.9) | |
| Vaccination statusb | <.001 | ||||
| Unvaccinated | 226 142 (87) | 40 424 (95.3) | 152 195 (90.6) | 33 523 (67.5) | |
| Partially vaccinated | 22 536 (8.7) | 1812 (4.3) | 14 698 (8.8) | 6026 (12.1) | |
| Fully vaccinated | 11 306 (4.3) | 183 (0.4) | 1045 (0.6) | 10 078 (20.3) | |
| Comorbidityc | 13 071 (5.0) | 2803 (6.6) | 7602(4.5) | 2666 (5.4) | <.001 |
| Immune compromise | 2062 (0.8) | 388 (0.9) | 1241 (0.7) | 433 (0.9) | <.001 |
| Long-term care resident | 541 (0.2) | 111 (0.3) | 212 (0.1) | 218 (0.4) | <.001 |
| Healthcare worker | 4589 (1.8) | 981 (2.3) | 2604 (1.6) | 1004 (2) | <.001 |
| Pregnancy | 795 (0.3) | 125 (0.3) | 440 (0.3) | 230 (0.5) | <.001 |
| Geography | <.001 | ||||
| Greater Toronto area and Hamiltond | 180 532 (69.4) | 26 280 (62) | 126 374 (75.3) | 27 878 (56.2) | |
| Ottawa | 11 871 (4.6) | 1899 (4.5) | 7432 (4.4) | 2540 (5.1) | |
Abbreviation: VOC, variant of concern
P values are based on the χ2 test.
Vaccination status defined as in the Methods section.
Comorbidities include 1 or more of the following: asthma, chronic obstructive pulmonary disease, hematological disease, liver disease, cardiac disease, diabetes, renal disease, neurological disease, malignancy, or obesity. Immune compromise was included as a separate covariate in models.
The greater Toronto area and Hamilton form a large conurbation in central Ontario consisting of 6 health units (Toronto, Peel, Durham, Halton, York, and Hamilton).
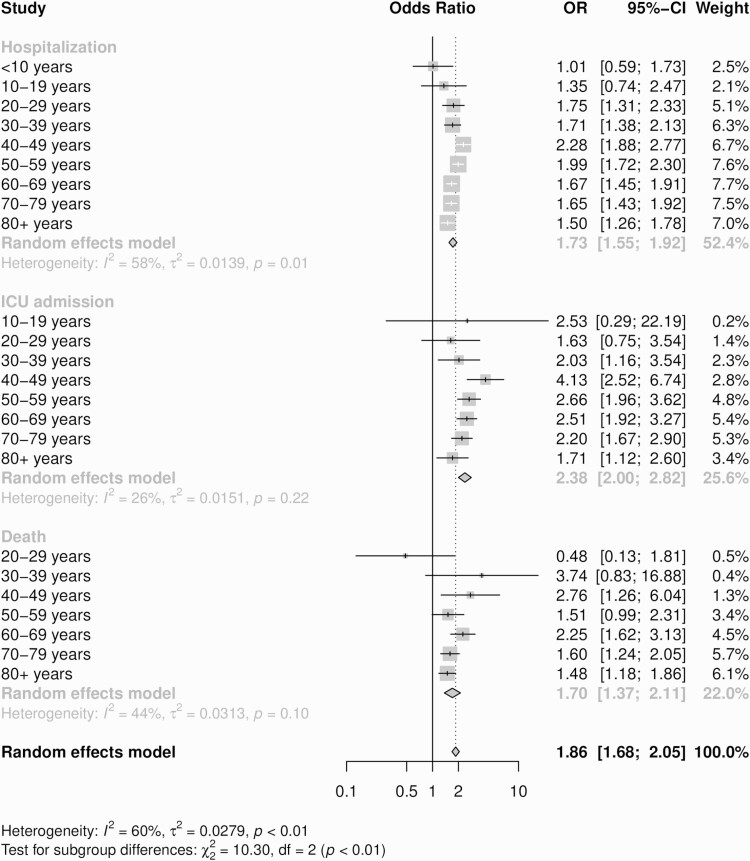
Adjusted odds ratios for hospitalization, ICU admission, and death by age category and VOC status are presented in Figures 1 and 2. N501Y-positive VOC infection was associated with a significant increase in hospitalization among people aged ≥20 years relative to infection with non-VOC SARS-CoV-2 strains. ICU admission risk was higher with N501Y-positive infection than with non-VOC infection in all groups aged ≥30 years. Risk of death was elevated in the 40- to 49-year age group and in people aged ≥60 years. For the N501Y-positive VOC, odds ratios could not be estimated for ICU admission in children aged <10 years or for death in those aged <20 years due to the rarity of these outcomes (Figure 1).
Figure 1.
Forest plot with adjusted ORs for hospitalization, ICU admission, and death by age group for N501Y-positive variant of concern (VOC) infection relative to non-VOC severe acute respiratory syndrome coronavirus 2 infection. Models were adjusted for sex, health unit region, age group, vaccination status, comorbidity, immune compromise, and (in relevant age groups) long-term care residence, healthcare worker status, and pregnancy. Abbreviations: CI, confidence interval; ICU, intensive care unit; OR, odds ratio.
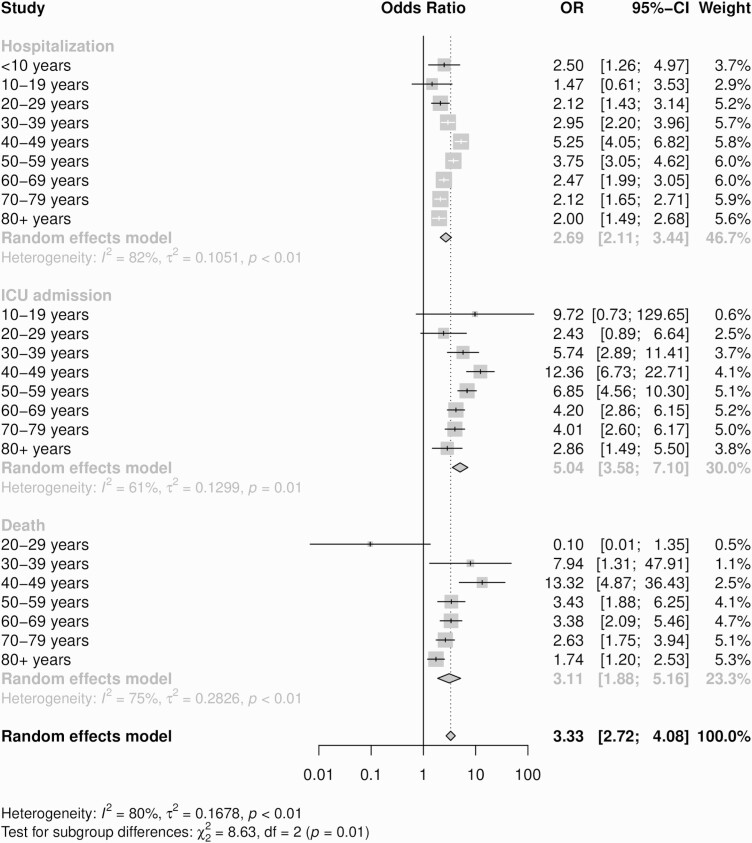
Figure 2.
Forest plot with adjusted ORs for hospitalization, ICU admission, and death by age group for the Delta variant of concern (VOC) infection relative to non-VOC severe acute respiratory syndrome coronavirus 2 infection. Models were adjusted for sex, health unit region, age group, vaccination status, comorbidity, immune compromise, and (in relevant age groups) long-term care residence, healthcare worker status, and pregnancy. Abbreviations: CI, confidence interval; ICU, intensive care unit; OR, odds ratio.
For Delta VOC infections, significantly elevated hospitalization risk was seen in all age groups except those aged 10 to 19 years. In children, the risk of hospitalization with the Delta VOC was 2.5-fold higher than that seen with non-VOC SARS-CoV-2. ICU admission risk could not be estimated for the Delta VOC in the <10 years age group, and elevations in risk among people aged <30 years were not different from risks seen with non-VOC infection. For people aged ≥30 years, marked increases in risk were observed. Odds ratios for death with the Delta variant could not be estimated for those aged <20 years; in adults aged >30 years, the risk of death was elevated with Delta VOC infection (Figure 2).
In random effects meta-analyses, we found no significant heterogeneity in odds ratios across age groups for death and ICU admission risk with the N501Y-positive VOC. By contrast, significant heterogeneity in risk estimates was seen for hospitalization risk across age groups with the N501Y-positive VOC and for hospitalization, ICU admission , and death risk with the Delta VOC (Figures 1 and 2). Across all outcomes, infection with the Delta VOC was associated with higher effect estimates relative to N501Y-positive infections. We evaluated the contribution of age to heterogeneity in estimates by constructing meta-regression models with age group treated as a 9-level ordinal variable. However, there was no significant linear association between age and relative risk of severe outcomes for either N501Y-positive variants or for the Delta variant (Table 2).
Table 2.
Meta-Regression–derived Age-related Relative Change in Odds Ratio Associated With N501Y-Positive and Probable Delta Variants of Concern
| Variant | Outcome | Relative Odds Ratio | 95% Confidence Interval | τ2a | R2b(%) |
|---|---|---|---|---|---|
| Probable Delta | |||||
| Hospitalization | 0.99 | .89–1.09 | 0.102 | 2.94 | |
| ICU admission | 0.90 | .76–1.07 | 0.0966 | 25.67 | |
| Death | 0.85 | .64–1.13 | 0.2064 | 26.98 | |
| N501Y-positive | |||||
| Hospitalization | 1.00 | .95–1.05 | 0.0154 | 0 | |
| ICU admission | 0.95 | .86–1.06 | 0.0147 | 2.12 | |
| Death | 0.98 | .84–1.14 | 0.0414 | 0 | |
Age category treated as a 9-level ordinal variable for the purpose of estimating linear trends. Coefficients can be interpreted as change in risk per 10-year change in age category.
Abbreviation: ICU, intensive care unit.
Estimated amount of residual heterogeneity due to between-age group variation.
Fraction of heterogeneity accounted for by including age in meta-regression models.
DISCUSSION
The landscape of SARS-CoV-2 infection continues to change rapidly, with novel VOCs impacting both transmissibility and virulence of infection. In this analysis, we evaluated the relative impact of earlier N501Y-positive VOC and subsequent Delta VOC infections on severity of infection by age group. We found that, as reported previously, Delta VOC infection is more virulent than infection with both N501Y-positive VOC and non-VOC SARS-CoV-2 strains [7, 10, 31]. We found no statistical evidence that the increase in virulence of the Delta VOC in the population as a whole is diminished in younger people. The absence of significant elevations of risk in younger age groups for some outcomes is likely to reflect lower absolute risk (and number of events) in these groups, with consequent lack of precision in estimates. Notably, the risk of hospitalization with the Delta VOC appears significantly increased in children.
Due to the relative rarity of ICU admission and death in younger age groups, we were unable to generate relative risk estimates for these outcomes with the Delta variant in children. However, an increase in virulence as well as transmissibility with the Delta VOC in children would be consistent with recent observed surges in pediatric hospitalizations reported in the United States and United Kingdom [14–17, 32]. In the United States, Delahoy and colleagues recently linked marked increases in pediatric hospitalizations associated with the emergence of the Delta VOC [32]. The authors evaluated risk of severe illness conditional on hospitalization (using indicators such as ICU admission, highest level of respiratory support, and length of stay) and did not find these risks to be increased after emergence of the Delta variant relative to the period prior to Delta emergence. However, such an approach fails to identify pediatric hospitalization as a manifestation of enhanced virulence, overlooks possible changes in hospitalized case mix associated with Delta VOC emergence, and may be subject to limitations in statistical power given the (fortunately) lower risk of severe outcomes among pediatric cases, as in our study.
Our analysis is subject to important limitations. First, the relative rarity of severe outcomes in younger age groups means that our estimates for these groups are imprecise. Furthermore, when evaluating associations in children and teens, our failure to identify heterogeneity in severity by age may simply be related to the imprecision of estimates in these age groups, rather than true lack of heterogeneity. A second limitation is the degree to which frequency of testing, particularly in younger age groups, has been dynamic in Ontario during the COVID-19 pandemic [21]. Increasing frequency of testing in undertested younger age groups over time, as VOCs emerged in the population, could increase the fraction of mild cases identified and may complicate estimation of relative severity over time.
In summary, we found no evidence to suggest that the apparent increase in virulence of SARS-CoV-2 VOCs is limited to a particular age group. The relative rarity of severe outcomes in children and teens means that more study is needed to assess the robustness and generalizability of these findings. As the Delta variant has now been replaced by the Omicron variant in Ontario [24], future work needs to also incorporate estimates of age-related severity of infection with the latter variant.
Notes
Acknowledgments. We thank the staff at Public Health Ontario, Ontario’s public health units, and Ontario Health for collecting, sequencing, analyzing, and providing access to the data used for this analysis
Disclaimer. The work does not represent the views of the Public Health Agency of Canada.
Financial support. The research was supported by a grant to D. N. F. from the Canadian Institutes for Health Research (2019 coronavirus disease 2019 [COVID-19] rapid researching funding OV4-170360).
Potential conflicts of interest. D. N. F. has served on advisory boards related to influenza and severe acute respiratory syndrome coronavirus 2 vaccines for Seqirus, Pfizer, AstraZeneca, and Sanofi-Pasteur Vaccines; has been a paid consultant on COVID-19 for JP Morgan Chase Bank, Farallon, and the WE Foundation; has given paid lectures to the Canadian Association for Alternative Strategies and Assets and the Canadian Society of Account Executives; and has served as a legal expert on issues related to COVID-19 epidemiology for the Elementary Teachers Federation of Ontario and the Registered Nurses Association of Ontario. A. R. T. was employed by the Public Health Agency of Canada when the research was conducted. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Contributor Information
David N Fisman, Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canadaand.
Ashleigh R Tuite, Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canadaand; Centre for Immunization Readiness, Public Health Agency of Canada, Ottawa, Ontario, Canada.
References
- 1. Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science 2021; 372:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brown KA, Joh E, Buchan SA, et al. Inflection in prevalence of SARS-CoV-2 infections missing the N501Y mutation as a marker of rapid Delta (B.1.617.2) lineage expansion in Ontario, Canada. medRxiv 2021; 2021.06.22.21259349. preprint: not peer reviewed. [Google Scholar]
- 3. Brown KA, Gubbay J, Hopkins J, et al. Rapid rise of S-gene target failure and the UK variant B.1.1.7 among COVID-19 isolates in the greater Toronto area, Canada. medRxiv 2021; 2021.02.09.21251225. preprint: not peer reviewed. [Google Scholar]
- 4. Nyberg T, Twohig KA, Harris RJ, et al. Risk of hospital admission for patients with SARS-CoV-2 variant B.1.1.7: cohort analysis. BMJ 2021; 373:n1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bager P, Wohlfahrt J, Fonager J, et al. Risk of hospitalisation associated with infection with SARS-CoV-2 lineage B.1.1.7 in Denmark: an observational cohort study. Lancet Infect Dis 2021; 21:1507–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Funk T, Pharris A, Spiteri G, et al. Characteristics of SARS-CoV-2 variants of concern B.1.1.7, B.1.351 or P.1: data from seven EU/EEA countries, weeks 38/2020 to 10/2021. Euro Surveill 2021; 26:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sheikh A, McMenamin J, Taylor B, Robertson C; Public Health Scotland and the EAVE II Collaborators. . SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021; 397:2461–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nunes-Vaz R, Macintyre CR . Observations on the current outbreak of the SARS-CoV-2 Delta variant in Sydney. Glob Biosecurity 2021; 3. Available at: https://jglobalbiosecurity.com/articles/10.31646/gbio.121/. Accessed 1 September 2021. [Google Scholar]
- 9. Scudellari M. How the coronavirus infects cells—and why Delta is so dangerous. Nature 2021; 595:640–4. [DOI] [PubMed] [Google Scholar]
- 10. Ong SWX, Chiew CJ, Ang LW, et al. Clinical and virological features of SARS-CoV-2 variants of concern: a retrospective cohort study comparing B.1.1.7 (Alpha), B.1.315 (Beta), and B.1.617.2 (Delta). Clin Infect Dis 2021; ciab721:1–9. Available at: 10.1093/cid/ciab721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fisman DN, Tuite AR.. Progressive increase in virulence of novel SARS-CoV-2 variants in Ontario, Canada. medRxiv 2021; 2021.07.05.21260050. preprint: not peer reviewed. [Google Scholar]
- 12. Sah P, Fitzpatrick MC, Zimmer CF, et al. Asymptomatic SARS-CoV-2 infection: a systematic review and meta-analysis. Proc Natl Acad Sci U S A 2021; 118. Available at: https://www.pnas.org/doi/epdf/10.1073/pnas.2109229118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Herrera-Esposito D, de los Campos G.. Age-specific rate of severe and critical SARS-CoV-2 infections estimated with multi-country seroprevalence studies. medRxiv 2021; 2021.07.29.21261282. preprint: not peer reviewed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Borter G. Children hospitalized with COVID-19 in U.S. hits record number 4 minute read. Reuters; Last accessed 3 September 2021. Available at: https://www.reuters.com/world/us/children-hospitalized-with-covid-19-us-hits-record-number-2021-08-14/ . [Google Scholar]
- 15. American Academy of Pediatrics. Children and COVID-19: state-level data report. Available at: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/. Accessed 3 September 2021.
- 16. Anthes E. The Delta variant is sending more children to the hospital. Are they sicker, too? New York Times 2021. Available at: https://www.nytimes.com/2021/08/09/health/coronavirus-children-delta.html. Accessed 2 September 2021. [Google Scholar]
- 17. Roucaute D, Santi P, Hecketsweiler C.. Le variant Delta provoque des craintes pour la rentrée scolaire. Le Monde. 2021. Available at: https://www.lemonde.fr/planete/article/2021/08/26/variant-delta-inquietudes-autour-d-une-rentree-scolaire-a-risque_6092366_3244.html. Accessed 2 September 2021. [Google Scholar]
- 18. Tuite AR, Fisman DN, Odutayo A, et al. COVID-19 hospitalizations, ICU admissions and deaths associated with the new variants of concern. 2021. Available at: https://covid19-sciencetable.ca/sciencebrief/covid-19-hospitalizations-icu-admissions-and-deaths-associated-with-the-new-variants-of-concern/. Accessed 5 July 2021.
- 19. Public Health Ontario. Epidemiologic summary: SARS-CoV-2 whole genome sequencing in Ontario, June 30, 2021. 2021. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-sars-cov2-whole-genome-sequencing-epi-summary.pdf?sc_lang=en. Accessed 5 July 2021.
- 20. Public Health Ontario. Epidemiologic summary: estimating the prevalence and growth of SARS-CoV-2 variants in Ontario using mutation profiles. 2021. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-prevalence-growth-voc-mutation-epi-summary.pdf?sc_lang=en. Accessed 5 July 2021.
- 21. Fisman DN, Greer AL, Brankston G, et al. COVID-19 case age distribution: correction for differential testing by age. Ann Intern Med 2021; 174:1430–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chung H, He S, Nasreen S, et al. Effectiveness of BNT162b2 and mRNA-1273 COVID-19 vaccines against symptomatic SARS-CoV-2 infection and severe COVID-19 outcomes in Ontario, Canada. medRxiv 2021. September 30, 2021. Available at: 10.1101/2021.06.28.21259420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nasreen S, He S, Chung H, et al. Effectiveness of COVID-19 vaccines against variants of concern, Canada. medRxiv 2021. 10.1101/2021.06.28.21259420. [DOI] [Google Scholar]
- 24. Ontario COVID-19 Science Advisory Table. Ontario dashboard. Tracking omicron. 2022. Available at: https://covid19-sciencetable.ca/ontario-dashboard/#percentcausedbyvariants. Accessed 15 February 2022.
- 25. Fisman DN, Lee N, Tuite AR.. Timing of breakthrough infection risk after vaccination against SARS-CoV-2. medRxiv 2022; 2022.01.04.22268773. preprint: not peer reviewed. [Google Scholar]
- 26. Greenland S, Thomas DC.. On the need for the rare disease assumption in case-control studies. Am J Epidemiol 1982; 116:547–53. [DOI] [PubMed] [Google Scholar]
- 27. Fisman D, Patrozou E, Carmeli Y, et al. Geographical variability in the likelihood of bloodstream infections due to gram-negative bacteria: correlation with proximity to the equator and health care expenditure. PLoS One 2014; 9:e114548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2017. Available at: https://www.R-project.org/. Accessed 24 September 2021. [Google Scholar]
- 29. Balduzzi S, Rücker G, Schwarzer G.. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 2019; 22:153–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ 2007; 85:867–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Twohig KA, Nyberg T, Zaidi A, et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: a cohort study. Lancet Infect Dis 2021; 22:35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Delahoy MJ, Ujamaa D, Whitaker M, et al. Hospitalizations associated with COVID-19 among children and adolescents—COVID-NET, 14 states, March 1, 2020-August 14, 2021. MMWR Morb Mortal Wkly Rep 2021; 70:1255–60. [DOI] [PMC free article] [PubMed] [Google Scholar]