Abstract
Since the outbreak of the coronavirus disease 2019 (COVID-19) pandemic, there have been a few variants of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), one of which is the Omicron variant (B.1.1.529). The Omicron variant is the most mutated SARS-CoV-2 variant, and its high transmissibility and immune evasion ability have raised global concerns. Owing to its enhanced transmissibility, Omicron has rapidly replaced Delta as the dominant variant in several regions. However, recent studies have shown that the Omicron variant exhibits reduced pathogenicity due to altered cell tropism. In addition, Omicron exhibits significant resistance to the neutralizing activity of vaccines, convalescent serum, and most antibody therapies. In the present review, recent advances in the molecular and clinical characteristics of the infectivity, pathogenicity, and immune evasion of Omicron variant was summarized, and potential therapeutic applications in response to Omicron infection were discussed. Furthermore, we highlighted potential response to future waves and strategies to end the pandemic.
Subject terms: Infectious diseases, Infectious diseases
Introduction
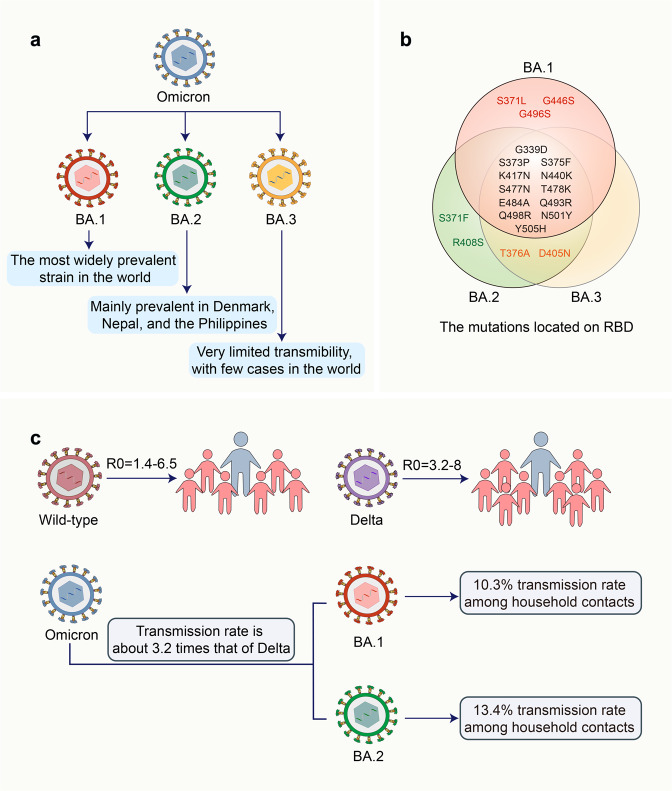
The Omicron variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first identified in South Africa and Botswana and was reported to the World Health Organization (WHO) on November 24, 2021, as a novel variant. This novel variant, also known as B.1.1.529, spreads rapidly and was classified as a variant of concern (VOC) by the WHO on November 26, 2021.1,2 Further examinations suggest that the Omicron variant did not develop from one of the earlier known variants, as evidenced by several differences between their genomes. Three possible explanations have been proposed for the development of the Omicron variant: silent evolution in a population with little sequencing, long-term evolution in one or a few persons with chronic infection, or evolution in other animals especially rodents.3 Notably, the Omicron variant is not a single strain, but evolved into three lineages: BA.1, BA.2, and BA.3. BA.1 was once the most widely prevalent strain in the world; however, BA.2 is gradually replacing BA.1 in several countries, such as Denmark, Nepal, and the Philippines. The transmissibility of BA.3 is very limited, with very few cases, at most a few hundred cases (Fig. 1a).
Fig. 1.
The sub-lineages of the SARS-CoV-2 Omicron variant. a The Omicron variant has evolved into three sub-lineages: BA.1, BA.2, and BA.3. b Venn diagram showing the mutations located on the S protein RBD of BA.1, BA.2, and BA.3. c Transmission speed of SARS-CoV-2 wild-type, Delta, and Omicron variants
The Omicron variant has caused global panic and concern owing to its contagious and vaccine-escape mutations. Presently, up to 60 mutations have been identified in the BA.1 lineage, with as many as 38 of these occurring in the spike (S) protein, one in the envelope (E) protein, two in the membrane (M) protein, and six in the nucleocapsid (N) protein (https://covid19dashboard.regeneron.com). BA.2 lineage possesses 57 mutations, with 31 in the S protein, of which the N-terminus is significantly different from that of BA.1. The receptor-binding domain (RBD) of the S protein is responsible for binding to the host receptor angiotensin-converting enzyme 2 (ACE2) and has the potential to increase infectivity and mediate escape from vaccine-induced neutralizing antibodies.4–6 Therefore, mutations located in the RBD of the S protein have attracted significant research attention. BA.1 and BA.2 share 12 mutations in the RBD, including G339D, S373P, S375F, K417N, N440K, S477N, T478K, E484A, Q493R, Q498R, N501Y, and Y505H. S371L, G446S, and G496S were only identified in BA.1, whereas R346K was found in a member of this group, namely BA.1.1. BA.2 possesses two unique mutations in RBD, including S371F and R408S, and shares T376A and D405N with BA.3 (Fig. 1b). Some of these mutations have also been found in previous variants and are known to lead to increased transmissibility, higher viral binding affinity, and antibody escape.7,8 For instance, mutations in the residues K417, E484, and N501, which have also been found in Beta (B.1.351) and Gamma (P.1) variants, have been suggested to mediate escape from vaccine-induced neutralization.5 The effects of most of the remaining Omicron mutations are unknown; thus, our understanding of the viral behavior and susceptibility of the Omicron variant to natural and vaccine-mediated immunity remains unclear. Moreover, individuals previously infected with other SARS-CoV-2 variants can be reinfected with this new variant.9 A recent study suggested that the Omicron variant is likely to infect individuals recovering from infections by previously prevalent variants.10,11 This evidence shows that mutations in Omicron evade immunity induced by the previous infection.
Given that the Omicron variant poses a serious threat to public health and could undermine global efforts to control the COVID-19 pandemic, there is an urgent need for in-depth studies and a comprehensive understanding of Omicron. Recently, several achievements have been made in understanding the Omicron variant. In this review, we summarized the recent progress in research on the characteristics of the Omicron variant, including its enhanced infectivity and transmissibility, reduced pathogenicity, and immune evasion ability. In addition, we discussed the effectiveness of existing vaccines, neutralizing antibodies, and antiviral drugs and highlighted possible response strategies to Omicron and future variants.
Infectivity and transmissibility
SARS-CoV-2 utilizes the S protein to bind to the main receptor ACE2 on the host-cell surface and enters the host cell through membrane fusion with the help of furin and type II transmembrane serine protease (TMPRSS2) or cathepsin L,12 which is a crucial process of infection. The Omicron variant shares a similar process of infection but is more contagious than previous variants. The findings of preliminary studies on the infectivity and transmissibility of Omicron are discussed below.
Binding to host receptor ACE2
ACE2 is a major receptor of SARS-CoV-2.13 The binding affinity of ACE2 for the S proteins of Omicron is one of the main factors determining viral infectivity. To date, the results on the binding affinity of the Omicron variant to ACE2 are slightly different, possibly owing to differences in experimental materials or methods. Moreover, the aggregation state of the protein has a significant impact on measurement results.14 Several studies have shown that the binding affinity of Omicron RBD to ACE2 is approximately 1.5–2.8 times that of the wild-type (WT).11,15–17 In contrast, some studies have suggested that the binding ability of Omicron RBD to ACE2 is comparable to that of WT.18,19 Compared with the previously prevalent Delta variant, Omicron RBD exhibits a similar or weaker binding ability to ACE2.11,17–19 In addition, the binding ability of Omicron RBD to ACE2 is much weaker than that of Alpha variant, with only one mutation, N501Y, in the RBD.16,19 Based on the above studies, it can be inferred that the binding ability of Omicron RBD to ACE2 is roughly between that of WT and Delta RBD. S477N, T478K, Q493R, Q496S, and Q498R have been reported to potentiate the interaction between Omicron and ACE2 by establishing new hydrogen bonds or salt bridges with the corresponding sites of ACE214,15,17,19 in addition to N501Y. However, K417N and E484A can cause a significant loss of polar interactions between Omicron and ACE2, offsetting some of the enhanced interactions forged by other mutations.14,15,17,19
Overall, mutations in the Omicron RBD did not affect its receptor recognition and binding to ACE2, and the Omicron RBD can efficiently bind to human ACE2 for host-cell entry. Notably, the Omicron S protein can bind to human ACE2 or ACE2 orthologs of different animal species to enter the target cells.20 These findings indicate the zoonotic potential of the Omicron variant, which could contribute to the development of highly infectious variants.
Host-cell entry
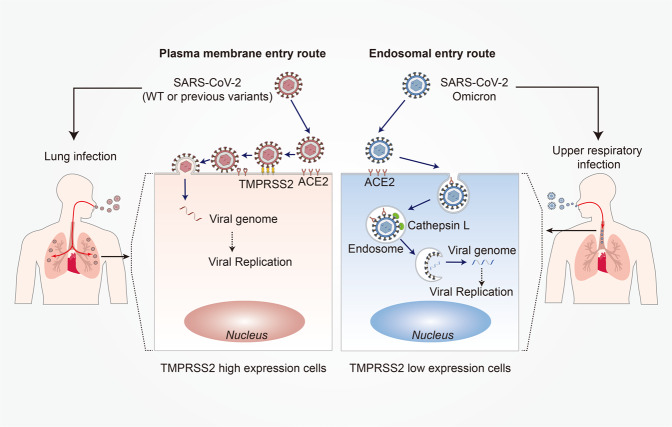
The entry of SARS-CoV-2 into the host cells after binding to host receptors is mediated by the S protein. The S protein is composed of S1 and S2 subunits.21 The S1 subunit contains the RBD, which binds to ACE2, whereas the S2 subunit contains the transmembrane portion of the S protein, which is responsible for anchoring the S protein to the membrane and mediating fusion of the viral membrane with cellular membranes.22,23 Cleavage of the S protein at the S1–S2 and S2 sites, mediated by furin24 and type II transmembrane serine protease (TMPRSS2)25or cathepsin L,26 is crucial for viral entry into host cells. Cleavage by TMPRSS2 and cathepsin L at the S2 site mediates two distinct SARS-CoV-2 entry pathways. As TMPRSS2 is present on the cell surface, TMPRSS2 mediates the plasma membrane route of entry, whereas cathepsin L in the endosome mediates the endosomal entry route.22
The Omicron variant harbors six unique mutations on S2 (N764K, D796Y, N856K, Q954H, N969K, and L981F) that have not been identified in previous VOC.27 Recent studies have reported that Omicron spike pseudotyped virus infection was reduced in TMPRSS2 expressing cells, but increased in cells that support endosomal entry, and that the Omicron variant prefers the endosomal entry route rather than the plasma membrane entry route.28–30 These findings suggest that mutations on the Omicron S protein non-RBD may alter the route of viral entry into host cells, which is associated with a shift in cellular tropism away from TMPRSS2 expressing cells, and explains the faster replication of Omicron in the upper airways than in the lungs, unlike that of other variants27,30–32 (Fig. 2). In addition, the Omicron variant contains three mutations in the furin cleavage site region (P681H, H655Y, and N679K). The basic mutation P681H in the polybasic cleavage site (PBCS), also present in Alpha and Gamma, has been demonstrated to promote furin-mediated cleavage of the S protein, potentially enhancing infectivity.33 However, the cleavage level of Omicron by furin is the weakest among the SARS-CoV-2 variants, indicating that other mutations near the furin cleavage site may severely interfere with its cleavage.34 Moreover, the fusion ability of the Omicron variant is the slowest among all SARS-CoV-2 variants,15,27,32 similar to SARS-CoV-1.34
Fig. 2.
The different entry routes and pathogenesis between SASR-CoV-2 WT or previous variants and Omicron variant. Left: SASR-CoV-2 WT or previous variants mainly infect lung epithelial cells, which are TMPRSS2 high expressed cells, and enter host cells by plasma membrane route. In the plasma membrane entry route, virus first binds to ACE2, then binds to TMPRSS2 and is cleaved at the S proteins. Next, the S protein anchors to the cell membrane and mediates fusion of the viral membrane with the cell membrane. Finally, a pore is formed in the membrane and the viral genome is released into the cell. Right: SASR-CoV-2 Omicron variant mainly infects the upper airway epithelial cells, which are TMPRSS2 low-expressed cells, and enter host cells by the endosomal route. In the endosomal entry route, a virus first binds to ACE2 and the virus–ACE2 complex is internalized via endocytosis into the endosomes, where S protein is cleaved by Cathepsin L. Then the viral and endosomal membranes are fused together to form a pore and release the viral genome
Transmissibility
The high transmissibility of the Omicron variant is a major cause of global concern. Since the advent of Omicron, it has rapidly replaced Delta as the dominant strain worldwide. In the US, Delta accounted for 99% of new cases on December 4, 2021; however, Omicron accounted for more than 95% by January 8, 2022.35 The basic reproduction number (R0) of the Delta variant was between 3.2 and 8.36 The transmissibility of the Omicron variant is ~3.2 times that of Delta, and the doubling time is approximately three days.37,38 Generally, BA.2 is ~1.4 times more transmissible than BA.1,39,40 with a transmission rate of ~13.4% among household contacts, whereas that of BA.1 was 10.3%41 (Fig. 1c).
The rapid spread of the Omicron variant is mainly due to its immune evasion ability, which is responsible for the infection of vaccinated and previously infected individuals.42 In addition, changes in cell entry and cellular tropism in the Omicron variant may also facilitate rapid transmission.27,28,31,43 Moreover, the Omicron variant has been shown to cause more asymptomatic infections than the other variants, which may contribute to the silent spread of the virus.44 Furthermore, the binding affinity of Omicron RBD to ACE2 contributes to transmission, but is not a major factor. However, whether Omicron infection can lead to higher viral loads remains controversial.45,46
Pathogenicity
The disease severity of the Omicron variant has sparked extensive discussion and has profoundly affected public policies. Growing evidence has shown that Omicron-infected patients exhibit milder symptoms than those infected by the earlier variants. Moreover, the Omicron variant is more likely to infect the upper respiratory tract and less able to cause lung infection. However, the observed reduction in pathogenicity is now amplified by enhanced immunity. Research from the UK shows that three doses of vaccination caused over 50% reduction in the odds of hospitalization with Omicron compared to those who were not immunized.47 Previous infection can also provide similar protection.48 The proportion of breakthrough infections caused by Omicron is much higher than that of previous variants, which would reduce the severity we observed. Therefore, the Omicron is still risky for unvaccinated individuals, especially the aged. The treatment of Omicron should be taken seriously.
Clinical symptoms
Analysis of the ZOE COVID study showed that the most common symptoms of Omicron infection were runny nose, headache, fatigue (mild or severe), sneezing, and sore throat.49,50 Generally, there are few differences between the symptom profiles of Omicron and Delta, with a lower occurrence of the classic symptoms of fever, cough, or loss of sense of smell or taste in Omicron-infected patients.49,50 There have been few cases of convulsions in children, but the cases were too few to conclude that they were the consequences of the infection.51 Furthermore, laboratory studies showed that the mutations in the Omicron variant altered the tropism of the virus. The Omicron variant exhibited a lower replication rate in lung and gut cell lines,27 but replicated faster in primary cultures of human nasal epithelial cells.28 Consistently, Omicron has been shown to replicate rapidly in human airway organoids and ex vivo explant cultures of human bronchus, but less efficiently in human alveoli organoids and ex vivo explant cultures of the human lung.31,43 These results revealed that Omicron tended to infect the upper respiratory tract, but not the lungs, which may contribute to enhanced transmissibility and better prognosis. Most studies attributed this to the inefficient TMPRSS2 usage of the Omicron variant.27,28,31,43 However, enhanced infection in the upper respiratory tract was not proven in rodent models, indicating that this point needed more evidence.32,52,53
Severity
A few real-world studies have indicated that the Omicron variant may be milder than earlier variants. A study of early cases in the Gauteng province of South Africa showed that the hospitalization rate during the fourth wave (Omicron-dominated) was ~4.9%, which was markedly below the rate in waves dominated by Beta or Delta variant, and the probability of severe illness was reduced by 73% in the Omicron-dominated wave.54 Outcomes in the Western Cape province of South Africa were similar, and the risk of severe hospitalization or death was reduced by ~25%.55,56 Moreover, patients infected by the Omicron variant and identified by the S gene target failure (SGTF) had significantly lower odds of hospitalization and severe disease than those by Delta.57 Several analyses of patients in the UK showed that the risk of hospitalization with Omicron was approximately one-third of that with Delta,58,59 with similar observations reported in France and Norway.60,61 In the United States, the percentage of hospitalization, intensive care unit (ICU) admission, receipt of invasive mechanical ventilation (IMV), and in-hospital death were lower during the Omicron pandemic than during the Delta pandemic, and the mean length of hospital stay was considerably shorter.62,63 Moreover, a high rate of asymptomatic carriage has been observed since the discovery of the Omicron variant,44 which may suggest milder symptoms of the variant.
Additionally, preliminary laboratory data confirmed the lower pathogenicity of the Omicron variant compared with the earlier variants. The formation of multinuclear syncytia is a significant pathological step in COVID-19 infection, reflective of cell-cell fusion events during viral infection.64–66 In vitro assays have shown that the Omicron variant poorly induced multinuclear syncytia in multiple cell lines27,52 compared with previous variants.67 Moreover, higher cell viability was observed in Omicron variant-infected cells compared with those infected with previous variants,32 which was consistent with findings in vivo. Infection with the Omicron variant caused limited bodyweight loss, lower viral load in the upper and lower respiratory tracts, and limited lung pathological damage and mortality rates compared with earlier variants in both hamsters or human ACE2 (hACE2) transgenic mice.32,52,53 In addition, the Omicron variant was less effective in antagonizing cellular interferon signaling compared with the Delta variant. Moreover, the activation of the NF-κB pathway is less efficient in response to the Omicron variant,68 implying that Omicron may induce slighter inflammatory responses.34
The evidence above further confirms that the Omicron variant is less severe than previous variants. However, it is possible that the pathogenicity of the Omicron variant may be underestimated because of rising levels of herd immunity via previous infections and vaccinations.69–71 Notably, the proportion of young patients was higher among those infected with Omicron,57,72 which may result in reduced pathogenicity. In addition, the impact of Omicron is not attenuated by reduced pathogenicity, the healthcare system is still under enormous pressure because of the high transmissibility of the Omicron variant.54,73
Immune evasion
The most serious concern about the Omicron variant is its high immune evasion ability. The Omicron variant can escape the immune response established by vaccination or previous infection by other variants, which may result in high transmissibility.11,16,71,74–79 Data from the UK showed that BA.2 and BA.1 have similar immune evasion abilities.41,80,81 Moreover, a recent study showed that BA.2 can re-infect BA.1 convalescent patients, despite the small number of such cases identified.80
There are several mutations in the RBD region and N-terminal domain (NTD) of the Omicron variant, which are the main targets of neutralization.82–85 Unprecedented complexity in mutation patterns can alter antigenicity, invalidating the existing immunity.86 The cryo-electron microscopy (cryo-EM) structure helps to reveal the basis of immune evasion by Omicron. Omicron S-trimer exclusively formed one conformational state with one “up” RBD and two “down” RBDs, while a single-up conformation and all-down conformation were depicted in previous variants.15,87 Steric clashes, altered interactions at antibody-binding surfaces, and local changes in the spike structure were induced by mutations that interfered with antibody recognition.86,87
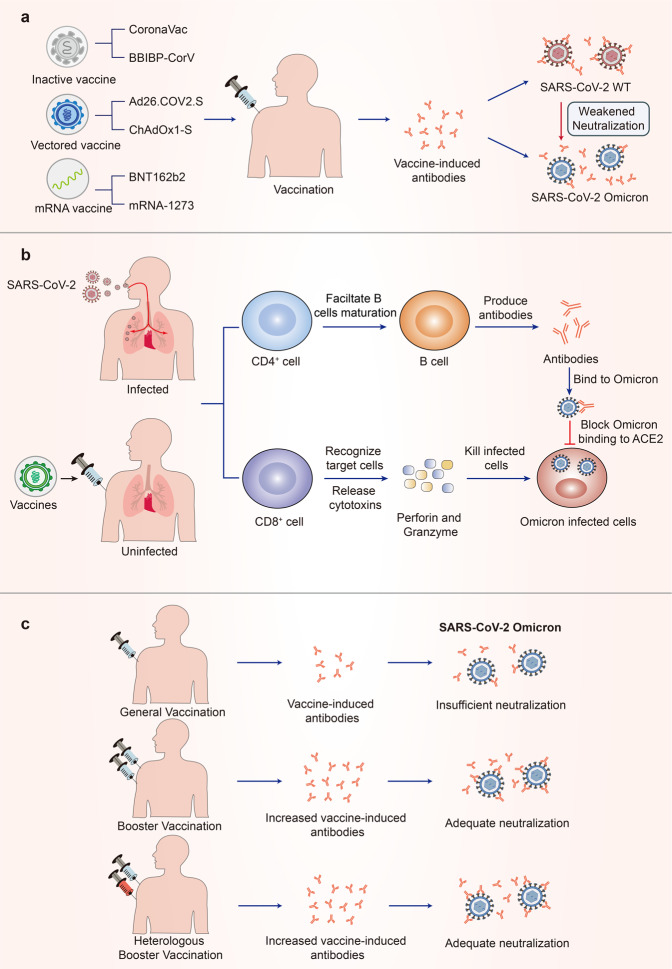
Vaccines
Since the outbreak of the COVID-19 pandemic, some vaccines have been developed to end the pandemic; however, these vaccines have been less effective against the Omicron variant. Available evidence shows that the major vaccines in use around the world are significantly less effective against Omicron. The neutralization activity against Omicron was below the lower limit of quantitation in over 80% of serum samples from individuals who received two doses of inactivated vaccines: CoronaVac and BBIBP-CorV.88–92 Moreover, Ad26.COV2.S, ChAdOx1-S, and Sputnik V, representative of vectored vaccines, failed to trigger effective neutralizing activity against the Omicron variant.16,93–95 RNA vaccines, such as BNT162b2 and mRNA-1273, which were proven to be the most effective against the WT strain, were completely ineffective against the Omicron variant in over 50% of individuals.92,93,95–102 In serum samples from individuals who had received two doses of BNT162b2 or mRNA-1273, there was a considerable decrease in the titers of neutralizing antibodies against the Omicron variant compared with the WT.93,94,96–98,103–106 Although each study differed due to differences in samples and testing methods, the findings showed that there was a considerable decrease in the neutralizing potency of two doses of RNA vaccines against Omicron. An observational study in the United States showed that the estimated effectiveness of two doses of RNA vaccines against Omicron was only ~30% 1 month after the second dose, with no effectiveness three months after the second dose for BNT162b2 and 6 months after the second dose for mRNA-1273.107 Data on other vaccines against Omicron variants have not been disclosed (Fig. 3a).
Fig. 3.
Vaccine-induced immunity against SARS-CoV-2 Omicron. a SARS-CoV-2 Omicron escapes vaccine immunity. The major vaccine candidates targeting SARS-CoV-2 induce antibodies after vaccination that can neutralize SARS-CoV-2 WT but are less effective against Omicron. b T-cell immune responses induced by SARS-CoV-2 infection or vaccination are effective against Omicron infection. c Booster vaccination or Heterologous booster vaccination can induce increased antibodies, which can provide adequate neutralization against Omicron
The cellular immune response is a major determinant of the clinical outcome of SARS-CoV-2.108 Multiple mutations in the spike protein of the Omicron variant contribute to escape from antibody neutralization, but components of the cellular immune response, such as T cells, can still target Omicron and provide protection from severe outcomes. Studies have shown that cellular immunity induced by vaccination or previous infection is highly conserved in the SARS-CoV-2 Omicron Spike.109–114 The median relative frequencies of SARS-CoV-2 spike-specific CD4+ T cells and CD8+ T cells that cross-recognize Omicron are ~70–90% in previously infected or vaccinated individuals,110–113 although there is still more than 50% reduction in 20% of individuals.114 In addition, booster vaccination enhances T-cell responses to Omicron spike.109,114 In vaccines, a median of 11 and 10 spike epitopes were recognized by CD4+ and CD8+ T cells in T-cell epitope repertoire analysis, respectively, with over 80% preservation for Omicron at the epitope level, which retained binding to HLA-I111,114 (Fig. 3b).
Although routine doses of vaccination are rarely effective in neutralizing the Omicron variant, substantial evidence has shown that booster vaccination can induce neutralizing immunity against Omicron more effectively.16,77,115 Post-booster vaccinations have shown a dozen-fold increase in neutralization titers for Omicron, indicating a significant reduction against the Omicron variant compared to the WT strain.88,93,96,99–101,116 Moreover, administering three doses of BNT162b2 and mRNA-1273 vaccines increased effectiveness against Omicron to ~65% and 72%, respectively, compared with unvaccinated mice.107 Interestingly, heterologous booster vaccination has the potential to induce adequate neutralizing efficacy,89,92,117,118 which is important for augmenting the protection provided by some vaccines with insufficient neutralizing antibodies. For instance, heterologous booster vaccination with aerosolized Ad5-nCoV, a representative of adenovirus-vectored vaccines, generated greater neutralizing antibody responses against the Omicron variant than that generated by homologous booster vaccination with CoronaVac,119 which provided an effective alternative in response to the Omicron. However, there is no evidence yet that heterologous vaccination is superior to homologous vaccination,120 and the protective efficacy obtained could be related to the type of vaccine. Therefore, further research on the mechanism and safety of heterologous vaccination is necessary, which could help solve the problem of vaccine shortage (Fig. 3c).
Overall, routine doses of vaccination can rarely provide adequate protection against the Omicron variant; therefore, homologous or heterologous booster vaccinations are necessary, which also highlights the significance of the supply and equitable distribution of vaccines. In addition, the plasma of convalescent individuals can hardly neutralize the Omicron variant, although cross-neutralization has been observed against earlier variants.77,91,95,115 However, infection plus vaccination can induce high-quality antibodies with superior neutralization capacity.91,94,95,99,103,116,121–123 Given a large number of infected individuals, this group of people may only require a routine vaccination dose to obtain effective protection against Omicron.
Therapeutic-neutralizing antibodies
In this section, we summarized the effect of neutralizing antibodies from vaccines and previous infections against the Omicron variant. The neutralizing ability of therapeutic-neutralizing antibodies against Omicron is weak. Most therapeutic-neutralizing antibodies with EUA approval or at advanced clinical development stages have failed to neutralize the Omicron variant (Table 1).16,75–77,106,115,124–126 Neutralizing antibodies can be divided into two groups. The first group contains the vast majority of neutralizing antibodies, including LY-CoV555 (marketed as bamlanivimab), LY-CoV016 (marketed as etesevimab), REGN10987 (marketed as imdevimab), REGN10933 (marketed as casirivimab), COV2-2196 (marketed as tixagevimab), COV2-2130 (marketed as cilgavimab) and CT-P59 (marketed as regdanvimab), which block binding of Spike protein to the receptor ACE2.16 Most of these antibodies lost their neutralizing ability against Omicron due to the destruction of the antigenic epitope.16,75,76,124,126 K417N, E484A, Q493R, and N501Y are the main sites responsible for the evasion.15 The combination of COV2-2196 and COV2-2130 exhibits neutralizing activity against Omicron; however, its neutralization ability against Omicron is 12–200-fold lower compared with that against the WT,16,115,124–127 due to the N440K and G446S mutations.76,115,127 However, this combination, especially COV2-2130, has been reported to retain activity against BA.2, perhaps due to the absence of G446S.128 The second group, represented by VIR-7831/S309 (marketed as sotrovimab), rarely competes with ACE2 but recognizes non-RBM epitopes that are conserved within sarbecoviruses, including SARS-CoV.129 S309 shows resistance to Omicron’s antibody escape, with only a two- to threefold decrease in neutralization efficiency for Omicron compared with the WT.16,76,115,124,126,127 G339D and N440K are presumed to interfere with the combination of S309 and spike protein due to the proximity of the antigenic site, but the impact is limited.76,127 BA.2 seems to have a greater negative impact on S309 because of the S371F mutation.128 Despite the presence of the S371L mutation in BA.1, S371F in BA.2 displayed distinct resistance to neutralizing antibodies compared to S371L.128 Brii-198 (marketed as romlusevimab) possesses neutralization efficiency against Omicron, but the neutralization ability is slightly weaker and can be inhibited by R346K.75 In addition, S2X259 possesses considerable neutralizing potency against the Omicron variant,16 but was less effective against the BA.2 strain.128 LY-CoV1404 (marketed as bebtelovimab), which has recently received EUA approval, possesses a high neutralization capacity against all identified variants.128,130 Structural analysis demonstrated that the epitope of LY-CoV1404 was highly conserved, except for N439 and N501. Fortunately, the N501Y mutation of Omicron does not interfere with its binding capacity.130
Table 1.
Neutralizing antibodies against SARS-CoV-2 Omicron variant
| Stages | Antibody name | Company | Neutralizing effect compared to SARS-CoV-2 WT | Mutations affecting neutralizing efficiency | Refs. |
|---|---|---|---|---|---|
| EUA (combined with etesevimab) | LY-CoV555 (bamlanivimab) | Lilly | Completely lost its activity | E484A, Q493R | 75 |
| EUA (combined with bamlanivimab) | LY-CoV016 (etesevimab) | Lilly | Completely lost its activity | S371L, K417N, Q493R; S371F, D405N | 75,128 |
| EUA | LY-CoV1404 (bebtelovimab) | Lilly | Almost identical | — | 128,130 |
| EUA (combined with casirivimab) | REGN10987 (imdevimab) | Regeneron Pharmaceuticals | Completely lost its activity | S371L, N440K, G446S; S371F | 75,115,128 |
| EUA (combined with imdevimab) | REGN10933 (casirivimab) | Regeneron Pharmaceuticals | Completely lost its activity | S371L, K417N, S477N, E484A, Q493R; S371F | 75,115,128 |
| EUA (combined with cilgavimab) | COV2-2196 (tixagevimab) | AstraZeneca | hundreds of times reduced | E484A, Q493R; S371F | 16,128 |
| EUA (combined with tixagevimab) | COV2-2130 (cilgavimab) | AstraZeneca | hundreds of times reduced in BA.1, but remained largely active in BA.2 | R346K; G446S | 16,128 |
| EUA | VIR-7831/S309 (sotrovimab) | GSK & Vir Biotechnology | 2–3-fold reduced in BA.1, but dozens of times reduced in BA.2 | G339D, S371L; S371F | 75,127,128 |
| Stage III | CT-P59 (regdanvimab) | Celltrion | Completely lost its activity | K417N, G446S, E484A, Q493R | 16,127 |
| Stage III | Brii-196 (amubarvimab) | Brii Biosciences | hundreds of times reduced | S371L, Q493R; S371F | 75,128 |
| Stage III | Brii-198 (romlusevimab) | Brii Biosciences | Maintains activity in BA.1, but is inhibited by R346K | R346K; S371F | 75,128 |
| Stage III | ADG20 (adintrevimab) | Adagio Therapeutics, Inc. | 20–200-folds reduced in BA.1, but almost lost activity in BA.2 | S371L; S371F | 75,77,115,128 |
| Stage I | DXP-604 | SINGLOMICS | About thirty times reduced | — | 76 |
| Preclinical | S2X259 | Humabs Biomed SA-Swiss Biotech | About ten times reduced in BA.1, and hundred times reduced in BA.2 | S371L; S371F | 75,128 |
| Preclinical | S2K146 | Vir Biotechnology | Basically retained activity | K417N, T478K, E484A, Q496S | 16 |
| Preclinical | S2H97 | Vir Biotechnology | Basically retained activity | — | 16 |
Overall, neutralizing antibodies targeting the conserved epitopes of SARS-CoV-2 variants and other sarbecoviruses may have broad prospects for the control of COVID-19 pandemic. Given that SARS-CoV-2 is prone to mutations, developing neutralizing antibodies targeting relatively conserved sites is an effective option to deal with emerging variants, such as Omicron. There are still some doubts about the efficacy of the antibodies mentioned above in treatment. A randomized controlled trial indicated that neither S309 nor Brii-198 showed efficacy in improving clinical outcomes despite the small sample size.68 Moreover, the efficacy of LY-CoV1404 is yet to be validated in clinical studies.
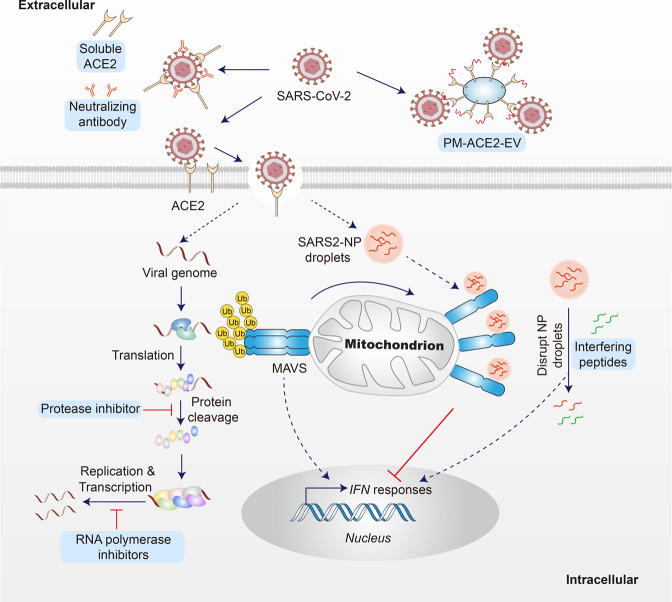
Antiviral drugs and potential treatments
In addition to vaccines and therapeutic-neutralizing antibodies, several antiviral drugs and potential treatments are being investigated for use against Omicron. Antibody therapies have been shown to be less effective against the Omicron variant; however, the situation seems different for antiviral drugs. In vitro assays have confirmed that Omicron is susceptible to most antiviral drugs under investigation, including remdesivir, molnupiravir, PF-07304814 (nirmatrelvir, a key component of paxlovid), EIDD-1931, ribavirin, favipravir, nafamostat, camostat, and aprotinin.68,126,131 These drugs have different mechanisms of action, indicating that the drug sensitivity profile of the Omicron variant does not change considerably in response to the drugs. There are only two missense mutations in the replicase–transcriptase complex (nsp7-10, nsp12, nsp14) of the Omicron variant, which may have little effect on RNA-dependent RNA polymerase-inhibitor drugs, such as remdesivir and molnupiravir.68 However, current research is still at the cellular level, and more clinical results are needed to support these conclusions. Moreover, the efficacy of several drugs is yet to be proven against Omicron. There is an urgent need to develop new broad-spectrum antiviral drugs in response to changing viruses and the current shortage of vaccines and drugs. Drugs that inhibit viral replication are likely to remain effective against the Omicron variant, which is also the mechanism of drugs that inhibit the binding of viruses to ACE2. The ACE2-targeting antibody has been shown to suppress the Omicron variant at the cellular level,132 which is a likely direction of exploration. Boosting the antibody responses using biochemical methods is also a method that could be explored. A recent study showed that an ultrapotent RBD-targeted biparatopic nanobody exhibited enhanced neutralizing activity against Omicron.133 In addition, it has been reported that engineered extracellular vesicles (EVs) enriched with palmitoylated ACE2 (PM‐ACE2) efficiently captured SARS‐CoV‐2 viruses and inhibited their interaction with cell surface ACE2, leading to reduced infection both in vitro and in vivo.134 Furthermore, it has been demonstrated that patients with COVID-19 exhibit impaired IFN responses, especially in patients with severe disease, which might contribute to the limited antiviral response.135–138 Therefore, targeting antiviral responses could be important in managing SARS-CoV-2. A recent study showed that the N protein of SARS-COV-2 inhibits the activity of MAVS, a key component of antiviral innate immunity, by undergoing liquid-liquid phase separation (LLPS) with RNA, thereby suppressing the antiviral immune response.139 Interestingly, the 246–365 domain of the N protein, which retains the phase-separation ability, is hardly mutated in the currently reported SARS-CoV-2 variants, including Omicron. Thus, targeting the SARS2-N protein LLPS could be a promising therapeutic approach against infection WT and variants of SARS-CoV-2. These potential treatments may help curb ongoing pandemics as well as any future outbreaks (Fig. 4).
Fig. 4.
Mechanisms of antiviral drugs and potential treatments against SARS-CoV-2 Omicron. Extracellularly, soluble ACE2, neutralizing antibodies, and palmitoylated ACE2-enriched EVs can capture SARS-CoV-2 viruses and inhibit SARS-CoV-2 interaction with cell-surface ACE2, resulting in reduced infection. Intracellularly, on the one hand, the released viral genome is translated to produce the polyproteins, which are cleaved by proteases to yield the RNA replicase–transcriptase complex. Then viral genome is duplicated and mRNA encoding structural proteins are transcribed. The protease inhibitors and RNA polymerase inhibitors can be used to inhibit the process of cleavage, transcription, and replication. On the other hand, the N protein of SARS-CoV-2 undergoes LLPS with RNA, which inhibits the aggregation and Lys-63-linked poly-ubiquitination of MAVS and thereby suppresses the innate antiviral immune response. The usage of interfering peptides disrupting N protein droplets can restore the impaired immune response
Conclusions and perspectives
The Omicron variant has attracted worldwide attention since its emergence owing to the high number of mutations, which increased its transmissibility and immune evasion capability. Although the binding ability of Omicron to ACE2 is still controversial, it has enhanced transmissibility, making it the dominant species in several regions within a short period of time. Omicron spikes inefficiently utilize TMPRSS2 to enter cells, but mainly rely on the endocytic pathway, which leads to a decrease in replication in the lung parenchyma and an enhanced ability to infect the upper respiratory tract,27,31,32 making the virus less pathogenic. Routine vaccination or a previous infection cannot provide effective protection against Omicron, and booster vaccination is required. Additionally, only a few neutralizing antibodies are active against Omicron, whereas most antiviral drugs in development are effective against it.
In the wake of the Omicron variant, it was believed that the effect would be minimal due to herd immunity established by vaccination and infection, and the development of specific drugs. Moreover, the discovery of the Omicron variant indicates that the attempt to end the COVID-19 pandemic might be hindered by the tendency of the virus to mutate. The major research focus should be the development of vaccines and drugs against possible variants of the virus.
Since the outbreak of the Omicron variant, several studies have been performed to improve our understanding of the mechanism and characteristics of the variant. Currently, vaccines, social distancing, and specific drugs are still effective means of resisting Omicron. Homologous or heterologous boosters and new vaccines against Omicron, and possibly new variants, have been proposed to improve protection in response to vaccine failure. However, early animal experiments have shown that Omicron-targeted vaccines were not more effective than booster jabs of already developed vaccines against the variant, although they all generated broad antibody responses to all variants, including Omicron.140–142 In naive mice immunized with Omicron-matched vaccines, high levels of potent antibodies against Omicron were produced, but their ability to inhibit previous variants was limited.142,143
Although it is believed that the omicron variant may likely not be the last mutant, it is expected that its effect will decrease with increasing immunity among the populace due to vaccines and infections. A previous study indicated that Omicron infection of vaccinated individuals, but not unvaccinated individuals, increases neutralizing activity against the Delta variant,144 indicating that the occurrence of previous variants is likely to reduce. Although no novel mutant has been discovered, the general trend is that the virus is becoming less severe, mainly because of enhanced immunity.
Furthermore, to effectively combat the Omicron variant and the pandemic in general, it is important to emphasize equal distribution of vaccines, especially in underdeveloped and developing regions. Presently, the three-injection vaccine can provide effective protection against Omicron, although there will be a percentage of breakthrough infections with milder symptoms. Some countries have approved the implementation of the fourth-injection vaccines. Recent researches show that the protection provided by the third dose of vaccines wanes over time, while the antibody levels can be restored by a fourth dose.145 Therefore, it is beneficial to administer a fourth dose of the vaccine to certain groups such as the elderly and immunocompromised individuals.146,147 Nevertheless, it is more crucial to complete the three doses of vaccination in a larger population than the fourth dose in healthy individuals, although we may need more boosters to maintain antibody levels in the long run. Furthermore, social distancing restrictions should not be lifted prematurely, as this can lead to unpredictable consequences.
Acknowledgements
We would like to apologize to those researchers whose related work we were not able to cite in this review. This work was supported by a special program from the Ministry of Science and Technology of China (2021YFA1101000), the Chinese National Natural Science Funds (31925013 and U20A20393 to L.Z.; 31871405, 32125016 and 82041009 to F.Z.), Zhejiang Provincial Natural Science Foundation of China under Grant (LBY21H060001 to L.Z.) and the Medical and the Medical and Health Research Project of Zhejiang Province (2020RC115 to L.Z.), Jiangsu National Science Foundation (BK20180043 and 19KJA550003 to F.Z.), the Zhejiang Natural Science Fund (LD19C070001to L.Z.), and the Key Project of University Natural Science Foundation of Jiangsu Province (19KJA550003), A project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions, and the Medical and Health Research Project of Zhejiang Province (2020RC155 to L.Z.).
Author contributions
Y.F. and X.L. conceived and drafted the manuscript. L.Z. discussed the concepts of the manuscript. S.W., L.Z., and F.Z. provided valuable discussion and revised the manuscript. All authors have read and approved the article.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Yao Fan, Xiang Li, Lei Zhang
Contributor Information
Shu Wan, Email: wanshu@zju.edu.cn.
Long Zhang, Email: zhanglong.2003@tsinghua.org.cn.
Fangfang Zhou, Email: zhoufangfang@suda.edu.cn.
References
- 1.Ledford H. How severe are Omicron infections? Nature. 2021;600:577–578. doi: 10.1038/d41586-021-03794-8. [DOI] [PubMed] [Google Scholar]
- 2.Burki TK. Omicron variant and booster COVID-19 vaccines. Lancet Respir. Med. 2022;10:e17. doi: 10.1016/S2213-2600(21)00559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kupferschmidt K. Where did ‘weird’ Omicron come from? Science. 2021;374:1179. doi: 10.1126/science.acx9738. [DOI] [PubMed] [Google Scholar]
- 4.Li Q, et al. SARS-CoV-2 501Y.V2 variants lack higher infectivity but do have immune escape. Cell. 2021;184:2362–2371. doi: 10.1016/j.cell.2021.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia-Beltran WF, et al. Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity. Cell. 2021;184:2372–2383. doi: 10.1016/j.cell.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cao Y, et al. Humoral immune response to circulating SARS-CoV-2 variants elicited by inactivated and RBD-subunit vaccines. Cell Res. 2021;31:732–741. doi: 10.1038/s41422-021-00514-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greaney AJ, et al. Complete mapping of mutations to the SARS-CoV-2 spike receptor-binding domain that escape antibody recognition. Cell Host Microbe. 2021;29:44–57. doi: 10.1016/j.chom.2020.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harvey WT, et al. SARS-CoV-2 variants, spike mutations and immune escape. Nat. Rev. Microbiol. 2021;19:409–424. doi: 10.1038/s41579-021-00573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pulliam, J. R. C. et al. Increased risk of SARS-CoV-2 reinfection associated with emergence of Omicron in South Africa. Science.10.1126/science.abn4947 (2022). [DOI] [PMC free article] [PubMed]
- 10.Abdullah, F. Tshwane district omicron variant patient profile - early features. https://www.samrc.ac.za/news/tshwane-district-omicron-variant-patient-profile-early-features (2022).
- 11.Zhang X, et al. SARS-CoV-2 Omicron strain exhibits potent capabilities for immune evasion and viral entrance. Signal Transduct. Target Ther. 2021;6:430. doi: 10.1038/s41392-021-00852-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dong Y, et al. Coronavirus in continuous flux: from SARS-CoV to SARS-CoV-2. Adv. Sci. 2020;7:2001474. doi: 10.1002/advs.202001474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gheblawi M, et al. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2. Circ. Res. 2020;126:1456–1474. doi: 10.1161/CIRCRESAHA.120.317015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin W, et al. Structures of the Omicron Spike trimer with ACE2 and an anti-Omicron antibody. Science. 2022;375:1048–1053. doi: 10.1126/science.abn8863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cui Z, et al. Structural and functional characterizations of infectivity and immune evasion of SARS-CoV-2 Omicron. Cell. 2022;185:860–871. doi: 10.1016/j.cell.2022.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cameroni E, et al. Broadly neutralizing antibodies overcome SARS-CoV-2 Omicron antigenic shift. Nature. 2021;602:664–670. doi: 10.1038/s41586-021-04386-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mannar D, et al. SARS-CoV-2 Omicron variant: antibody evasion and cryo-EM structure of spike protein-ACE2 complex. Science. 2022;375:760–764. doi: 10.1126/science.abn7760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu L, et al. SARS-CoV-2 Omicron RBD shows weaker binding affinity than the currently dominant Delta variant to human ACE2. Signal Transduct. Target Ther. 2022;7:8. doi: 10.1038/s41392-021-00863-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han P, et al. Receptor binding and complex structures of human ACE2 to spike RBD from omicron and delta SARS-CoV-2. Cell. 2022;185:630–640. doi: 10.1016/j.cell.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffmann M, et al. The Omicron variant is highly resistant against antibody-mediated neutralization: Implications for control of the COVID-19 pandemic. Cell. 2022;185:447–456. doi: 10.1016/j.cell.2021.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wrapp D, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jackson CB, Farzan M, Chen B, Choe H. Mechanisms of SARS-CoV-2 entry into cells. Nat. Rev. Mol. Cell Biol. 2022;23:3–20. doi: 10.1038/s41580-021-00418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bayati A, Kumar R, Francis V, McPherson PS. SARS-CoV-2 infects cells after viral entry via clathrin-mediated endocytosis. J. Biol. Chem. 2021;296:100306. doi: 10.1016/j.jbc.2021.100306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang L, et al. Furin cleavage of the SARS-CoV-2 spike is modulated by O-glycosylation. Proc. Natl Acad. Sci. USA. 2021;118:e2109905118. doi: 10.1073/pnas.2109905118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoffmann M, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simmons G, et al. Inhibitors of cathepsin L prevent severe acute respiratory syndrome coronavirus entry. Proc. Natl Acad. Sci. USA. 2005;102:11876–11881. doi: 10.1073/pnas.0505577102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meng B, et al. Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts tropism and fusogenicity. Nature. 2022;603:706–714. doi: 10.1038/s41586-022-04474-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peacock, T. P. et al. The SARS-CoV-2 variant, Omicron, shows rapid replication in human primary nasal epithelial cultures and efficiently uses the endosomal route of entry. Preprint at bioRxiv.10.1101/2021.12.31.474653v1 (2022).
- 29.Willett, B. J. et al. The hyper-transmissible SARS-CoV-2 Omicron variant exhibits significant antigenic change, vaccine escape and a switch in cell entry mechanism. Preprint at medRxiv.10.1101/2022.01.03.21268111v2 (2022).
- 30.Zhao H, et al. SARS-CoV-2 Omicron variant shows less efficient replication and fusion activity when compared with Delta variant in TMPRSS2-expressed cells. Emerg. Microbes Infect. 2022;11:277–283. doi: 10.1080/22221751.2021.2023329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hui KPY, et al. SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo. Nature. 2022;603:715–720. doi: 10.1038/s41586-022-04479-6. [DOI] [PubMed] [Google Scholar]
- 32.Shuai H, et al. Attenuated replication and pathogenicity of SARS-CoV-2 B.1.1.529 Omicron. Nature. 2022;603:693–699. doi: 10.1038/s41586-022-04442-5. [DOI] [PubMed] [Google Scholar]
- 33.Peacock TP, et al. The furin cleavage site in the SARS-CoV-2 spike protein is required for transmission in ferrets. Nat. Microbiol. 2021;6:899–909. doi: 10.1038/s41564-021-00908-w. [DOI] [PubMed] [Google Scholar]
- 34.Du X, et al. Omicron adopts a different strategy from Delta and other variants to adapt to host. Signal Transduct. Target Ther. 2022;7:45. doi: 10.1038/s41392-022-00903-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. COVID data tracker: variant proportions.https://covid.cdc.gov/covid-data-tracker/#variant-proportions (2022).
- 36.Liu Y, Rocklov J. The reproductive number of the Delta variant of SARS-CoV-2 is far higher compared to the ancestral SARS-CoV-2 virus. J. Travel Med. 2021;28:taab124. doi: 10.1093/jtm/taab124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.UK Health Security Agency. SARS-CoV-2 variants of concern and variants under investigation in England-Thechnial briefing 33. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1043807/technical-briefing-33.pdf (2022).
- 38.Long B, et al. Clinical update on COVID-19 for the emergency clinician: presentation and evaluation. Am. J. Emerg. Med. 2022;54:46–57. doi: 10.1016/j.ajem.2022.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yamasoba, D. et al. Virological characteristics of SARS-CoV-2 BA.2 variant. Preprint at bioRxiv.10.1101/2022.02.14.480335v1 (2022).
- 40.Lyngse, F. P. et al. Transmission of SARS-CoV-2 Omicron VOC subvariants BA.1 and BA.2: evidence from Danish Households. Preprint at medRxiv.10.1101/2022.01.28.22270044v1 (2022).
- 41.Mahase E. Omicron sub-lineage BA.2 may have “substantial growth advantage,” UKHSA reports. BMJ. 2022;376:o263. doi: 10.1136/bmj.o263. [DOI] [PubMed] [Google Scholar]
- 42.Chaguza, C. et al. Rapid emergence of SARS-CoV-2 Omicron variant is associated with an infection advantage over Delta in vaccinated persons. Med (N Y). 10.1016/j.medj.2022.03.010 (2022). [DOI] [PMC free article] [PubMed]
- 43.Lamers, M. M. et al. SARS-CoV-2 Omicron efficiently infects human airway, but not alveolar epithelium. Preprint at bioRxiv10.1101/2022.01.19.476898v1 (2022).
- 44.Garrett, N. et al. High rate of asymptomatic carriage associated with variant strain Omicron. Preprint at medRxiv10.1101/2021.12.20.21268130v2 (2022).
- 45.Riediker M, et al. Higher viral load and infectivity increase risk of aerosol transmission for Delta and Omicron variants of SARS-CoV-2. Swiss Med. Wkly. 2022;152:w30133. doi: 10.4414/smw.2022.w30133. [DOI] [PubMed] [Google Scholar]
- 46.Migueres, M. et al. Influence of immune escape and nasopharyngeal virus load on the spread of SARS-CoV-2 Omicron variant. J. Infect. 10.1016/j.jinf.2022.01.036 (2022). [DOI] [PMC free article] [PubMed]
- 47.El-Shabasy RM, et al. Three waves changes, new variant strains, and vaccination effect against COVID-19 pandemic. Int. J. Biol. Macromol. 2022;204:161–168. doi: 10.1016/j.ijbiomac.2022.01.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pilz S, et al. SARS-CoV-2 reinfections: overview of efficacy and duration of natural and hybrid immunity. Environ. Res. 2022;209:112911. doi: 10.1016/j.envres.2022.112911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Iacobucci G. Covid-19: runny nose, headache, and fatigue are commonest symptoms of omicron, early data show. BMJ. 2021;375:n3103. doi: 10.1136/bmj.n3103. [DOI] [PubMed] [Google Scholar]
- 50.ZOE. What are the symptoms of Omicron? https://joinzoe.com/learn/omicron-symptoms (2022).
- 51.Ludvigsson, J. F. Convulsions in children with COVID-19 during the Omicron wave. Acta Paediatr. 10.1111/apa.16276 (2022). [DOI] [PMC free article] [PubMed]
- 52.Suzuki R, et al. Attenuated fusogenicity and pathogenicity of SARS-CoV-2 Omicron variant. Nature. 2022;603:700–705. doi: 10.1038/s41586-022-04462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Halfmann PJ, et al. SARS-CoV-2 Omicron virus causes attenuated disease in mice and hamsters. Nature. 2022;603:687–692. doi: 10.1038/s41586-022-04441-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jassat, W., Karim, S. & Mudara, C. Clinical severity of covid-19 patients admitted to hospitals in Gauteng, South Africa during the omicron-dominant fourth wave. Preprint at SSRN. https://ssrn.com/abstract=3996320 (2021).
- 55.Davies, M. A. et al. Outcomes of laboratory-confirmed SARS-CoV-2 infection in the Omicron-driven fourth wave compared with previous waves in the Western Cape Province, South Africa. Trop Med Int Health.10.1111/tmi.13752 (2022). [DOI] [PMC free article] [PubMed]
- 56.Abdullah F, et al. Decreased severity of disease during the first global omicron variant covid-19 outbreak in a large hospital in Tshwane, South Africa. Int. J. Infect. Dis. 2021;116:38–42. doi: 10.1016/j.ijid.2021.12.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wolter N, et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study. Lancet. 2022;399:437–446. doi: 10.1016/S0140-6736(22)00017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Agency, U. H. S. SARS-CoV-2 variants of concern and variants under investigation in England-Technical briefing: Update on hospitalisation and vaccine effectiveness for Omicron VOC-21NOV-01 (B.1.1.529). https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1045619/Technical-Briefing-31-Dec-2021-Omicron_severity_update.pdf (2022).
- 59.Ulloa, A. C., Buchan, S. A., Daneman, N. & Brown, K. A. Estimates of SARS-CoV-2 Omicron variant severity in Ontario, Canada. J. Am. Med. Assoc. 10.1001/jama.2022.2274 (2022). [DOI] [PMC free article] [PubMed]
- 60.Houhamdi L, et al. Characteristics of the first 1119 SARS-CoV-2 Omicron variant cases, in Marseille, France, November-December 2021. J. Med. Virol. 2022;94:2290–2295. doi: 10.1002/jmv.27613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Veneti L, et al. Reduced risk of hospitalisation among reported COVID-19 cases infected with the SARS-CoV-2 Omicron BA.1 variant compared with the Delta variant, Norway, December 2021 to January 2022. Eur. Surveill. 2022;27:2200077. doi: 10.2807/1560-7917.ES.2022.27.4.2200077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Iuliano AD, et al. Trends in disease severity and health care utilization during the early Omicron variant period compared with previous SARS-CoV-2 high transmission periods—United States, December 2020-January 2022. MMWR Morb. Mortal. Wkly Rep. 2022;71:146–152. doi: 10.15585/mmwr.mm7104e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lewnard, J. A. et al. Clinical outcomes among patients infected with Omicron (B.1.1.529) SARS-CoV-2 variant in southern California. Preprint at medRxiv.10.1101/2022.01.11.22269045v2 (2022).
- 64.Bussani R, et al. Persistence of viral RNA, pneumocyte syncytia and thrombosis are hallmarks of advanced COVID-19 pathology. EBioMedicine. 2020;61:103104. doi: 10.1016/j.ebiom.2020.103104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Braga L, et al. Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia. Nature. 2021;594:88–93. doi: 10.1038/s41586-021-03491-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sanders DW, et al. SARS-CoV-2 requires cholesterol for viral entry and pathological syncytia formation. eLife. 2021;10:e65962. doi: 10.7554/eLife.65962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rajah MM, et al. SARS-CoV-2 Alpha, Beta, and Delta variants display enhanced spike-mediated syncytia formation. EMBO J. 2021;40:e108944. doi: 10.15252/embj.2021108944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bojkova D, et al. Reduced interferon antagonism but similar drug sensitivity in Omicron variant compared to Delta variant of SARS-CoV-2 isolates. Cell Res. 2022;32:319–321. doi: 10.1038/s41422-022-00619-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nealon J, Cowling BJ. Omicron severity: milder but not mild. Lancet. 2022;399:412–413. doi: 10.1016/S0140-6736(22)00056-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bhattacharyya RP, Hanage WP. Challenges in inferring intrinsic severity of the SARS-CoV-2 Omicron variant. N. Engl. J. Med. 2022;386:e14. doi: 10.1056/NEJMp2119682. [DOI] [PubMed] [Google Scholar]
- 71.Ferguson N, et al. Report 49: growth, population distribution and immune escape of Omicron in England. Imp. Coll. Lond. 2021;93038:1–10. [Google Scholar]
- 72.Maslo C, et al. Characteristics and outcomes of hospitalized patients in South Africa during the COVID-19 Omicron wave compared with previous waves. J. Am. Med. Assoc. 2022;327:583–584. doi: 10.1001/jama.2021.24868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mahase E. Covid-19: Hospital admission 50-70% less likely with omicron than delta, but transmission a major concern. BMJ. 2021;375:n3151. doi: 10.1136/bmj.n3151. [DOI] [PubMed] [Google Scholar]
- 74.Altarawneh HN, et al. Protection against the Omicron variant from previous SARS-CoV-2 infection. N. Engl. J. Med. 2022;386:1288–1290. doi: 10.1056/NEJMc2200133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liu L, et al. Striking antibody evasion manifested by the Omicron variant of SARS-CoV-2. Nature. 2021;602:676–681. doi: 10.1038/s41586-021-04388-0. [DOI] [PubMed] [Google Scholar]
- 76.Cao Y, et al. Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature. 2021;602:657–663. doi: 10.1038/s41586-021-04385-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Planas D, et al. Considerable escape of SARS-CoV-2 Omicron to antibody neutralization. Nature. 2021;602:671–675. doi: 10.1038/s41586-021-04389-z. [DOI] [PubMed] [Google Scholar]
- 78.Kuhlmann C, et al. Breakthrough infections with SARS-CoV-2 omicron despite mRNA vaccine booster dose. Lancet. 2022;399:625–626. doi: 10.1016/S0140-6736(22)00090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dejnirattisai W, et al. Reduced neutralisation of SARS-CoV-2 omicron B.1.1.529 variant by post-immunisation serum. Lancet. 2022;399:234–236. doi: 10.1016/S0140-6736(21)02844-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Callaway E. Why does the Omicron sub-variant spread faster than the original? Nature. 2022;602:556–557. doi: 10.1038/d41586-022-00471-2. [DOI] [PubMed] [Google Scholar]
- 81.Agency, U. H. S. COVID-19 vaccine surveillance report Week 4. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1050721/Vaccine-surveillance-report-week-4.pdf (2022).
- 82.Cerutti G, et al. Potent SARS-CoV-2 neutralizing antibodies directed against spike N-terminal domain target a single supersite. Cell Host Microbe. 2021;29:819–833. doi: 10.1016/j.chom.2021.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dejnirattisai W, et al. The antigenic anatomy of SARS-CoV-2 receptor binding domain. Cell. 2021;184:2183–2200. doi: 10.1016/j.cell.2021.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.McCallum M, et al. N-terminal domain antigenic mapping reveals a site of vulnerability for SARS-CoV-2. Cell. 2021;184:2332–2347. doi: 10.1016/j.cell.2021.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang L, et al. A proof of concept for neutralizing antibody-guided vaccine design against SARS-CoV-2. Natl Sci. Rev. 2021;8:nwab053. doi: 10.1093/nsr/nwab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sun C, et al. Parallel profiling of antigenicity alteration and immune escape of SARS-CoV-2 Omicron and other variants. Signal Transduct. Target Ther. 2022;7:42. doi: 10.1038/s41392-022-00910-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cerutti G, et al. Cryo-EM structure of the SARS-CoV-2 Omicron spike. Cell Rep. 2022;38:110428. doi: 10.1016/j.celrep.2022.110428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ai J, et al. Omicron variant showed lower neutralizing sensitivity than other SARS-CoV-2 variants to immune sera elicited by vaccines after boost. Emerg. Microbes Infect. 2022;11:337–343. doi: 10.1080/22221751.2021.2022440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang X, et al. Homologous or heterologous booster of inactivated vaccine reduces SARS-CoV-2 Omicron variant escape from neutralizing antibodies. Emerg. Microbes Infect. 2022;11:477–481. doi: 10.1080/22221751.2022.2030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lu L, et al. Neutralization of SARS-CoV-2 Omicron variant by sera from BNT162b2 or Coronavac vaccine recipients. Clin. Infect. Dis. 2021 doi: 10.1093/cid/ciab1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang Y, et al. Resistance of SARS-CoV-2 Omicron variant to convalescent and CoronaVac vaccine plasma. Emerg. Microbes Infect. 2022;11:424–427. doi: 10.1080/22221751.2022.2027219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cheng SMS, et al. Neutralizing antibodies against the SARS-CoV-2 Omicron variant following homologous and heterologous CoronaVac or BNT162b2 vaccination. Nat. Med. 2022;28:486–489. doi: 10.1038/s41591-022-01704-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Garcia-Beltran WF, et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell. 2022;185:457–466. doi: 10.1016/j.cell.2021.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schmidt F, et al. Plasma neutralization of the SARS-CoV-2 Omicron variant. N. Engl. J. Med. 2022;386:599–601. doi: 10.1056/NEJMc2119641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rossler A, et al. SARS-CoV-2 Omicron variant neutralization in serum from vaccinated and convalescent persons. N. Engl. J. Med. 2022;386:698–700. doi: 10.1056/NEJMc2119236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pajon R, et al. SARS-CoV-2 Omicron variant neutralization after mRNA-1273 booster vaccination. N. Engl. J. Med. 2022;386:1088–1091. doi: 10.1056/NEJMc2119912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Edara VV, et al. mRNA-1273 and BNT162b2 mRNA vaccines have reduced neutralizing activity against the SARS-CoV-2 omicron variant. Cell Rep. Med. 2022;3:100529. doi: 10.1016/j.xcrm.2022.100529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Doria-Rose, N. A. et al. Booster of mRNA-1273 Strengthens SARS-CoV-2 Omicron Neutralization. Preprint at medRxiv10.1101/2021.12.15.21267805v2 (2021).
- 99.Gruell H, et al. mRNA booster immunization elicits potent neutralizing serum activity against the SARS-CoV-2 Omicron variant. Nat. Med. 2022;28:477–480. doi: 10.1038/s41591-021-01676-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nemet I, et al. Third BNT162b2 vaccination neutralization of SARS-CoV-2 Omicron infection. N. Engl. J. Med. 2022;386:492–494. doi: 10.1056/NEJMc2119358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wu M, et al. Three-dose vaccination elicits neutralising antibodies against omicron. Lancet. 2022;399:715–717. doi: 10.1016/S0140-6736(22)00092-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Muik A, et al. Neutralization of SARS-CoV-2 Omicron by BNT162b2 mRNA vaccine-elicited human sera. Science. 2022;375:678–680. doi: 10.1126/science.abn7591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sievers BL, et al. Antibodies elicited by SARS-CoV-2 infection or mRNA vaccines have reduced neutralizing activity against Beta and Omicron pseudoviruses. Sci. Transl. Med. 2022;14:eabn7842. doi: 10.1126/scitranslmed.abn7842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kotaki, R. et al. SARS-CoV-2 Omicron-neutralizing memory B-cells are elicited by two doses of BNT162b2 mRNA vaccine. Sci. Immunol. 10.1126/sciimmunol.abn8590 (2022). [DOI] [PMC free article] [PubMed]
- 105.Cele S, et al. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature. 2021;602:654–656. doi: 10.1038/s41586-021-04387-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wilhelm, A. et al. Reduced neutralization of SARS-CoV-2 Omicron variant by vaccine sera and monoclonal antibodies. Preprint at https://www.medrxiv.org/content/10.1101/2021.12.07.21267432v2 (2021).
- 107.Accorsi EK, et al. Association between 3 doses of mRNA COVID-19 Vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta variants. J. Am. Med. Assoc. 2022;327:639–651. doi: 10.1001/jama.2022.0470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Moss P. The T cell immune response against SARS-CoV-2. Nat. Immunol. 2022;23:186–193. doi: 10.1038/s41590-021-01122-w. [DOI] [PubMed] [Google Scholar]
- 109.GeurtsvanKessel CH, et al. Divergent SARS CoV-2 Omicron-reactive T- and B cell responses in COVID-19 vaccine recipients. Sci. Immunol. 2022;7:eabo2202. doi: 10.1126/sciimmunol.abo2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liu J, et al. Vaccines elicit highly conserved cellular immunity to SARS-CoV-2 Omicron. Nature. 2022;603:493–496. doi: 10.1038/s41586-022-04465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tarke A, et al. SARS-CoV-2 vaccination induces immunological T cell memory able to cross-recognize variants from Alpha to Omicron. Cell. 2022;185:847–859. doi: 10.1016/j.cell.2022.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gao Y, et al. Ancestral SARS-CoV-2-specific T cells cross-recognize the Omicron variant. Nat. Med. 2022;28:472–476. doi: 10.1038/s41591-022-01700-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Keeton R, et al. T cell responses to SARS-CoV-2 spike cross-recognize Omicron. Nature. 2022;603:488–492. doi: 10.1038/s41586-022-04460-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Naranbhai V, et al. T cell reactivity to the SARS-CoV-2 Omicron variant is preserved in most but not all individuals. Cell. 2022;185:1041–1051. doi: 10.1016/j.cell.2022.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Dejnirattisai W, et al. SARS-CoV-2 Omicron-B.1.1.529 leads to widespread escape from neutralizing antibody responses. Cell. 2022;185:467–484. doi: 10.1016/j.cell.2021.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wratil PR, et al. Three exposures to the spike protein of SARS-CoV-2 by either infection or vaccination elicit superior neutralizing immunity to all variants of concern. Nat. Med. 2022;28:496–503. doi: 10.1038/s41591-022-01715-4. [DOI] [PubMed] [Google Scholar]
- 117.Kaku CI, et al. Broad anti-SARS-CoV-2 antibody immunity induced by heterologous ChAdOx1/mRNA-1273 vaccination. Science. 2022;375:1041–1047. doi: 10.1126/science.abn2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Costa Clemens SA, et al. Heterologous versus homologous COVID-19 booster vaccination in previous recipients of two doses of CoronaVac COVID-19 vaccine in Brazil (RHH-001): a phase 4, non-inferiority, single blind, randomised study. Lancet. 2022;399:521–529. doi: 10.1016/S0140-6736(22)00094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhang, Z. et al. Aerosolized Ad5-nCoV booster vaccination elicited potent immune response against the SARS-CoV-2 Omicron variant after inactivated COVID-19 vaccine priming. Preprint at medRxiv.10.1101/2022.03.08.22271816v1 (2022).
- 120.Liu X, et al. Safety and immunogenicity of heterologous versus homologous prime-boost schedules with an adenoviral vectored and mRNA COVID-19 vaccine (Com-COV): a single-blind, randomised, non-inferiority trial. Lancet. 2021;398:856–869. doi: 10.1016/S0140-6736(21)01694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhao X, et al. Effects of a prolonged booster interval on neutralization of Omicron variant. N. Engl. J. Med. 2022;386:894–896. doi: 10.1056/NEJMc2119426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Moncunill G, et al. Determinants of early antibody responses to COVID-19 mRNA vaccines in a cohort of exposed and naive healthcare workers. EBioMedicine. 2022;75:103805. doi: 10.1016/j.ebiom.2021.103805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chatterjee D, et al. SARS-CoV-2 Omicron Spike recognition by plasma from individuals receiving BNT162b2 mRNA vaccination with a 16-weeks interval between doses. Cell Rep. 2022;38:110429. doi: 10.1016/j.celrep.2022.110429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.VanBlargan LA, et al. An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nat. Med. 2022;28:490–495. doi: 10.1038/s41591-021-01678-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zost SJ, et al. Potently neutralizing and protective human antibodies against SARS-CoV-2. Nature. 2020;584:443–449. doi: 10.1038/s41586-020-2548-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Takashita E, et al. Efficacy of antibodies and antiviral drugs against Covid-19 Omicron variant. N. Engl. J. Med. 2022;386:995–998. doi: 10.1056/NEJMc2119407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.McCallum M, et al. Structural basis of SARS-CoV-2 Omicron immune evasion and receptor engagement. Science. 2022;375:864–868. doi: 10.1126/science.abn8652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Iketani S, et al. Antibody evasion properties of SARS-CoV-2 Omicron sublineages. Nature. 2022 doi: 10.1038/s41586-022-04594-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Pinto D, et al. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature. 2020;583:290–295. doi: 10.1038/s41586-020-2349-y. [DOI] [PubMed] [Google Scholar]
- 130.Westendorf, K. et al. LY-CoV1404 (bebtelovimab) potently neutralizes SARS-CoV-2 variants. Preprint at bioRxiv10.1101/2021.04.30.442182v6 (2022). [DOI] [PMC free article] [PubMed]
- 131.Li P, et al. SARS-CoV-2 Omicron variant is highly sensitive to molnupiravir, nirmatrelvir, and the combination. Cell Res. 2022;32:322–324. doi: 10.1038/s41422-022-00618-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ou J, et al. ACE2-targeting antibody suppresses SARS-CoV-2 Omicron and Delta variants. Signal Transduct. Target Ther. 2022;7:43. doi: 10.1038/s41392-022-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chi X, et al. An ultrapotent RBD-targeted biparatopic nanobody neutralizes broad SARS-CoV-2 variants. Signal Transduct. Target Ther. 2022;7:44. doi: 10.1038/s41392-022-00912-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Xie F, et al. Engineering extracellular vesicles enriched with palmitoylated ACE2 as COVID-19 therapy. Adv. Mater. 2021;33:e2103471. doi: 10.1002/adma.202103471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hadjadj J, et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369:718–724. doi: 10.1126/science.abc6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Blanco-Melo D, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181:1036–1045. doi: 10.1016/j.cell.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Arunachalam PS, et al. Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans. Science. 2020;369:1210–1220. doi: 10.1126/science.abc6261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Trouillet-Assant S, et al. Type I IFN immunoprofiling in COVID-19 patients. J. Allergy Clin. Immunol. 2020;146:206–208. doi: 10.1016/j.jaci.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wang S, et al. Targeting liquid-liquid phase separation of SARS-CoV-2 nucleocapsid protein promotes innate antiviral immunity by elevating MAVS activity. Nat. Cell Biol. 2021;23:718–732. doi: 10.1038/s41556-021-00710-0. [DOI] [PubMed] [Google Scholar]
- 140.Waltz, E. Omicron-targeted vaccines do no better than original jabs in early tests. Nature.10.1038/d41586-022-00003-y (2022). [DOI] [PubMed]
- 141.Gagne, M. et al. mRNA-1273 or mRNA-Omicron boost in vaccinated macaques elicits similar B cell expansion, neutralizing antibodies and protection against Omicron. Cell.10.1016/j.cell.2022.03.038 (2022). [DOI] [PMC free article] [PubMed]
- 142.Ying, B. et al. Boosting with Omicron-matched or historical mRNA vaccines increases neutralizing antibody responses and protection against B.1.1.529 infection in mice. Preprint at bioRxiv.10.1101/2022.02.07.479419v1 (2022).
- 143.Lee, I.-J. et al. Omicron-specific mRNA vaccine induced potent neutralizing antibody against Omicron but not other SARS-CoV-2 variants. Preprint at bioRxiv.10.1101/2022.01.31.478406v1 (2022).
- 144.Khan, K. et al. Omicron infection of vaccinated individuals enhances neutralizing immunity against the Delta variant. Preprint at medRxiv. 10.1101/2021.12.27.21268439v2 (2022).
- 145.Regev-Yochay, G. et al. Efficacy of a fourth dose of Covid-19 mRNA vaccine against Omicron. N. Engl. J. Med. 10.1056/NEJMc2202542 (2022). [DOI] [PMC free article] [PubMed]
- 146.Caillard S, et al. Antibody response to a fourth messenger RNA COVID-19 vaccine dose in kidney transplant recipients: a case series. Ann. Intern. Med. 2022;175:455–456. doi: 10.7326/L21-0598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Teles M, et al. Attenuated response to fourth dose SARS-CoV-2 vaccination in patients with autoimmune disease: a case series. Ann. Rheum. Dis. 2022 doi: 10.1136/annrheumdis-2021-221641,. [DOI] [PMC free article] [PubMed] [Google Scholar]