Key Points
Question
Does the risk of suicide change for women when someone they live with in a previously handgun-free household lawfully acquires a handgun?
Findings
In this retrospective cohort study of 9.5 million women living in handgun-free homes, the suicide rate increased substantially after a cohabitant acquired a handgun compared with the rate among women whose cohabitants never acquired handguns. The increased rate of suicide was entirely from excess of firearm suicides.
Meaning
The findings suggest that the rate of suicide for women living in handgun-free homes increased significantly after an adult they lived with became a handgun owner.
This cohort study evaluates suicide rates among women who do not own guns with and without cohabitants who own guns.
Abstract
Importance
Little is known about the extent to which secondhand exposure to household firearms is associated with risk of suicide in adults who do not own guns, most of whom are women.
Objective
To evaluate changes in risk of suicide among women living in gun-free households after one of their cohabitants became a handgun owner.
Design, Setting, and Participants
This cohort study observed participants for up to 12 years and 2 months from October 18, 2004, to December 31, 2016. Data were analyzed from April to November 2021. The study population included 9.5 million adult women in California who did not own guns and who entered the study while living with 1 or more adults in a handgun-free home.
Exposures
Secondhand exposure to household handguns.
Main Outcomes and Measures
Suicide, firearm suicide, nonfirearm suicide.
Results
Of 9.5 million women living in handgun-free homes, 331 968 women (3.5% of the study population; mean [SD] age, 41.6 [18.0] years) became exposed to household handguns during the study period. In the entire study population, 294 959 women died: 2197 (1%) of these were by suicide, 337 (15%) of which were suicides by firearm. Rates of suicide by any method during follow-up were higher among cohort members residing with handgun owners compared with those residing in handgun-free homes (hazard ratio, 1.43; 95% CI, 1.11-1.84). The excess suicide rate was accounted for by higher rates of suicide by firearm (hazard ratio, 4.32; 95% CI, 2.89-6.46). Women in households with and without handguns had similar rates of suicide by nonfirearm methods (hazard ratio, 0.90; 95% CI, 0.63-1.27).
Conclusions and Relevance
In this study, the rate of suicide among women was significantly higher after a cohabitant of theirs became a handgun owner compared with the rate observed while they lived in handgun-free homes.
Introduction
In the US, more than one-third of adults live in households with firearms.1 More than 80% of the men in these homes personally own guns, but fewer than half of the women do.1 One outcome of this disparity is that women constitute approximately 85% of the adults who live in households with guns but do not own firearms themselves. Little is known about how secondhand exposure to firearms affects nonowners, especially with respect to suicide, which is the leading cause of violent death and of death by firearms in the US for both women and men.2
Epidemiologic studies have consistently shown a positive association between the presence of household firearms and suicide mortality, driven by higher rates of suicide by firearm.3,4,5,6,7,8 Collectively, these studies of overall exposure to household firearms, all of which are case-control studies, suggest that adults living in households with firearms are more than 3 times as likely to die by suicide compared with adults in gun-free homes.4 However, nearly all studies that have assessed household-level risk report only aggregate risk, which represents a weighted mean of the risks for firearm owners and nonowners residing in the same home. To our knowledge, only 1 study has evaluated how much risk is borne by nonowners who live with gun owners.9 In that case-control study, conducted among members of a health care system in Washington state from 1980 to 1992, 7% of suicide decedents and 5% of living control individuals had never purchased a handgun but lived with a family member who had (adjusted odds ratio, 1.5; 95% CI, 0.9-2.5). Sample size precluded examining suicide risk by method (ie, firearm vs nonfirearm), sex, or age (eg, adults vs children). Thus, for the 20 million US women and 4 million US men who currently live with a firearm owner but do not own guns themselves, the extent to which living in a household with firearms increases their risk of dying by suicide is not known.1,2
We observed a cohort of 9.5 million adult female residents of California for up to 12 years 2 months to estimate changes in rates of suicide among women who did not own guns after someone they lived with in a previously handgun-free household lawfully acquired a handgun.
Methods
The Stanford University institutional review board approved this study and provided a waiver of consent. Results are reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline (section X in the eAppendix in the Supplement).10
Study Design, Setting, and Population
This retrospective observational cohort study included 9.5 million adult female residents of California who did not own guns. Participants were observed for up to 12 years and 2 months from October 18, 2004, to December 31, 2016. Data were analyzed from April to November 2021. All study participants entered the study while living with 1 or more adults in a handgun-free household and all were registered voters in California.
Our study sample was drawn from a database assembled for the LongSHOT project,11,12 which is described in detail elsewhere. The LongSHOT database was formed by linking lawful handgun transactions from California’s Dealer Record of Sale (DROS) database to historical extractions of the California Statewide Voter Registration Database (SVRD) and to all-cause mortality data derived from the California Death Statistical Master Files. Within the LongSHOT cohort, we formed households by matching cohabitants—ie, LongSHOT members who, per the SVRD, resided at the same residential address during the same period. Section II in the eAppendix in the Supplement describes our household matching methodology.
To create the study sample, we applied several exclusion criteria to the parent cohort (section III in the eAppendix in the Supplement). First, members of single-adult households were excluded because they had no observable cohabitants, and members of households composed of 5 or more adult cohabitants were also dropped for reasons explained in section III in the eAppendix in the Supplement. Second, we excluded anyone who bought a handgun between January 1985, the first date transfers were recorded in DROS, and the study start date, October 18, 2004, as well as anyone who lived with them during the study period (to minimize exposure misclassification). Third, we used historical data on handgun acquisitions to identify people who were residing with handgun owners on the first day they came under observation and excluded them.13 Fourth, we used information in the DROS database on all lawful handgun acquisitions statewide—not only those observed in the parent cohort, which required being listed in an active voter file—and excluded adults residing at the most recent address of handgun owners who were not LongSHOT members (section III in the eAppendix in the Supplement). Fifth, a small number of women in our cohort (81 359) had missing data for census tracts or birth dates and were dropped. Thus, all members of the study cohort began contributing observation time as unexposed (ie, as women who did not own handguns and who lived in households with 1, 2, or 3 other adults, none of whom owned handguns).
Data Sources
DROS
Handgun transfers in California, including those between private parties, must be transacted through a licensed firearms dealer with few exceptions (eg, certain intrafamily transfers and purchases by dealers).14 Dealers are required to send details about the transfer and transferees to the California Department of Justice, where the information is electronically archived in the DROS database. This process has governed handgun transfers in California for decades. Details of long gun (ie, rifle and shotgun) transfers were not routinely archived until January 1, 2014. DROS data indicated which women in our study and which of their cohabitants had acquired handguns and the dates of acquisition. We obtained records of the 9.1 million handgun and long gun transfers recorded in the DROS database over a 32-year period from January 1, 1985, to December 31, 2016.
The SVRD
The SVRD enumerates all registered voters in the state. Because the SVRD must be kept up to date with new registrations, deregistrations (eg, deaths and out-of-state relocations), and changes of names and addresses, each extraction is a sample of adults known to be alive and residing in California on the extraction date. We obtained 13 historical extractions of the SVRD, spaced approximately 1 year apart and spanning our study period. These extractions included 74% of residents who were eligible to vote in California and 61% of all adult residents of the state (section I in the eAppendix in the Supplement).
California Death Statistical Master Files
The California Death Statistical Master Files are the state’s official mortality records. These files contain detailed information on deaths of state residents wherever the deaths occur. We obtained data on all deaths during the study period.
Key Measures
Exposure to Household-Level Handguns
To focus on our question of interest (does risk of suicide among women change when someone with whom they live in a handgun-free home lawfully acquires a handgun), we focused exclusively on the transition to secondhand exposure that occurs when a woman’s cohabitant in a handgun-free home lawfully acquires a handgun. Two other transitions to secondhand exposure are possible but do not pertain to our research question: when women who do not own handguns move in with a handgun owner or when a handgun owner moves in with them. We censored women involved in these other transitions on the day before the transition unless these other transitions occurred on or after the day of an eligible transition.
Primary Outcomes
Causes of death were coded according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). Suicide deaths are delineated according to method (codes -X60–X84), including suicide by firearm (codes X72–X74).
Other Variables
Age, sex, and current residential address for eligible women in our study came from the SVRD. Because suicide rates and rates of firearm ownership vary by race and ethnicity, race and ethnicity data were imputed using validated methods as described in detail elsewhere11,15,16 and in section VI in the eAppendix in the Supplement. Race and ethnicity were defined as per the 2010 US Census Summary File 1.17 We geocoded the residential addresses and assigned them to census tracts—that is, geographically contiguous areas designed to approximate small neighborhoods.18 On average, these tracts contained fewer than 5000 people.
Using DROS data, we constructed 3 additional variables that (1) identified adults in the LongSHOT parent database who had acquired handguns prior to the beginning of our study period by linking data on handgun transfers in the 19.8 years preceding the study period (January 1, 1985, to October 17, 2004); (2) indicated the cumulative number of handguns owned based on acquisitions and transfers and used this time-varying variable to identify transfer of the last known handgun owned (ie, divestment); and (3) flagged participants in LongSHOT who acquired a long gun with an indicator variable that switched on at the date of first-known long gun acquisition. For additional details on all study variables, see sections IV, V, and VI in the eAppendix in the Supplement.
Observation and Exposure Time
The final analytic data set was at the person-period level. Eligible women entered the cohort on the date of the SVRD extract in which they first appeared. Their observation time ended the day before the date of the next extract in which they did not appear or when they met 1 of the exclusion criteria, the day before they acquired a handgun, death, or the end of the study period. When a handgun owner with whom a cohort member resided died, we censored the cohort member to account for uncertainty regarding the disposition of the decedent’s firearms, as California law allows certain intrafamilial transfers without requiring a record of the transfer.19 For balance, we also censored household members in unexposed homes when an adult in that household died.
Exposure time began on the day someone residing with a woman who did not own a gun acquired the household’s first documented handgun. Exposure time ended on the day before the date of the next extraction that showed study participants no longer residing with a handgun owner or when the observation period ended. Women censored for reasons other than the death of a gun owner they lived with could reenter the cohort and contribute person-time provided they were otherwise eligible at the time they reentered.
Statistical Analysis
We used extended Cox proportional hazard models to calculate hazard ratios (HRs) estimating the association between household exposure to a handgun and time to mortality (ie, all-cause, overall suicide, suicide by firearm, and suicide by other methods). The binary variable of interest distinguished exposed person-time (periods of cohabitation with 1 or more handgun owners) from unexposed person-time (periods of cohabitation with no handgun owners). Models allowed the baseline hazard to vary by census tract and adjusted for baseline age, race and ethnicity, number of adult cohabitants, and long gun ownership by study participants and their cohabitants. To estimate the cause-specific HR, we censored participants who died of causes other than the outcome of interest being modeled on the day before their death.20 We compared absolute risk differences between exposed and unexposed women by plotting adjusted cumulative incidence functions for competing risks data, using inverse probability weighting (section VIII in the eAppendix in the Supplement).21,22
Statistical analyses used R version 4.0.2 (R Foundation) and Stata version 14.1 (StataCorp). To account for multiple cohort members in the same household, we reported cluster-adjusted standard errors. For additional information regarding statistical analyses, see section VIII in the eAppendix in the Supplement.
Sensitivity Analyses
We explored the potential for meaningful bias due to unmeasured confounding in 2 ways. First, we conducted negative control outcome analyses.23 In these analyses, we used the same modeling approach and exposure time as in our main analyses, but the outcomes were lung cancer (ICD-10 code C34) and alcoholic liver disease (ICD-10 code K70), causes of death more common among people who smoke or drink heavily, respectively, both of which are established behavioral predictors of suicide not measured in our data.24,25,26,27,28 Second, we conducted bias analyses to calculate the minimum strength of association on the risk ratio scale that an unmeasured confounder would need to have with both our exposure and outcomes, conditional on the measured covariates, to fully explain away our main results.29,30
Results
Sample Characteristics
The study sample comprised 9 546 029 women (mean [SD] age, 41.6 [18.0] years) living with 1 to 3 other adults, none of whom owned handguns at study entry. Participants were observed for a mean (SD) of 5.5 (3.9) years, during which time 331 968 (3.5%) became exposed when any of their cohabitants acquired a handgun. A total of 1.09 million exposed person-years and 51.51 million unexposed person-years were analyzed. Compared with cohort members who remained unexposed throughout the study period, cohort members who became exposed were more likely to be White (246 201 [74.2%] exposed vs 5 523 900 [60.0%] unexposed), reside outside urban areas (50 427 [15.3%] exposed vs 836 078 [9.1%] unexposed), and live in a household with more than 2 adults (150 424 [45.3%] exposed vs 3 690 178 [40.1%] unexposed) (Table 1).
Table 1. Characteristics of Women Who Did Not Own Guns by Exposure to Handguns Through Cohabitants.
| Characteristic | No. (%) | |
|---|---|---|
| Women residing with handgun ownersa | Women residing with adults who did not own handguns | |
| Total female cohabitants | 331 968 | 9 214 061 |
| Age, yb | ||
| Mean | 40 | 42 |
| Median (range) | 41 (18-109) | 40 (18-109) |
| Race and ethnicityc | ||
| Asian | 15 724 (4.7) | 811 540 (8.8) |
| Black | 13 705 (4.1) | 636 130 (6.9) |
| Hispanic | 54 815 (16.5) | 2 171 630 (23.6) |
| White | 246 201 (74.2) | 5 523 900 (60.0) |
| Otherd | 378 (0.1) | 17 629 (0.2) |
| Missing/unknown | 1145 (0.3) | 53 232 (0.6) |
| No. of household adult residentse | ||
| 2 | 181 544 (54.7) | 5 523 883 (60.0) |
| 3 | 95 328 (28.7) | 2 428 704 (26.4) |
| 4 | 55 096 (16.6) | 1 261 474 (13.7) |
| Participant owned ≥1 registered long gunsf | 4 (0) | 274 (0) |
| ≥1 Cohabitants owned ≥1 registered long gunsf | 633 (0.2) | 3921 (0) |
| Residential locationg | ||
| Urban | 281 541 (84.8) | 8 377 983 (90.9) |
| Suburban | 35 399 (10.7) | 595 510 (6.5) |
| Large rural town | 8908 (2.7) | 144 942 (1.6) |
| Small rural town | 6120 (1.8) | 95 599 (1.0) |
| Missing/unknown | 0 | 27 (<0.1) |
Women were included in this group if they resided with handgun owners at any time while under observation.
Values refer to cohort members’ age on the first day they came under observation.
The California Statewide Voter Registration Database does not contain information on registrants’ race and ethnicity. Because suicide rates and rates of firearm ownership vary by race and ethnicity, race and ethnicity data for all LongSHOT cohort members were imputed using a package developed by Imai and Khanna15 for use in voter data. See section VI in the eAppendix in the Supplement.
Other includes American Indian and Alaska Native, Native Hawaiian and other Pacific Islander, some other race or ethnicity, and 2 or more races or ethnicities as defined in the 2010 US Census Summary File 1.17 Groups were consolidated because of low numbers.
Number of household adult residents is based on the number of adults in the LongSHOT12 data set who matched on address and date with the household of the cohort member when she came under observation.
California’s Dealer Record of Sale retained records of long gun transfers after 2014.
Categories for residential locations are based on rural-urban commuting area codes (section VI in the eAppendix in the Supplement). Values refer to cohort members’ residential location on the day they entered the cohort. Missing values arose from census tracts that could not be mapped to rural-urban commuting area codes from the 2010 US Census. Because our analyses were stratified by census tract, we did not adjust for urbanicity; these values are for descriptive purposes only.
Frequency and Rate of Death and Suicide
A total of 294 959 women died during the study period (Table 2); 2197 (1%) died by suicide, 337 (15%) of which were suicides by firearm. A firearm was used in 31 of the 64 suicides among women residing with handgun owners (48%) and in 306 of the 2133 suicides among those residing in households with no handgun owners (14%).
Table 2. Counts, Crude Rates, and Adjusted Hazard Ratios for All-Cause Mortality and Suicide Among Women by Handgun Ownership Among Cohabitants.
| Variable | Women residing with handgun ownersa | Women residing with adults who did not own handgunsb | Adjusted hazard ratio (95% CI)d | ||
|---|---|---|---|---|---|
| Deathsa | Crude rate | Deathsc | Crude rate | ||
| All cause | 4585 | 418.47 | 290 374 | 563.68 | 1.04 (1.01-1.07) |
| Suicide | 64 | 5.84 | 2133 | 4.14 | 1.43 (1.11-1.84) |
| Suicide by firearm | 31 | 2.83 | 306 | 0.59 | 4.32 (2.89-6.46) |
| Suicide by other method | 33 | 3.01 | 1827 | 3.55 | 0.90 (0.63-1.27) |
Rate denominators for study participants living with handgun owners consist of the exposure time women who did not own handguns contributed while in such a residential arrangement.
Rate denominators for study participants living with only nonowners consist of the nonexposure time women who did not own guns contributed while in such a residential arrangement.
Death counts for study participants residing with handgun owners indicate deaths that occurred among women who did not own handguns during a period in which they were residing with 1 or more handgun owners. Death counts for study participants residing with only nonowners indicate deaths among women who did not own handguns during periods in which they resided with only nonowners.
Adjusted hazard ratios were estimated with the use of Cox proportional hazards models in which baseline hazards were stratified according to census tract. The models were controlled for age at the beginning of the study period, household size (based on adults on the California voter file), race and ethnicity, and binary indicators of individual and household ownership of rifles or shotguns.
Women living in households with handgun owners had lower rates of all-cause mortality than those living in households with no handgun owners in unadjusted analyses, but not in adjusted analyses (Table 2). Women living in households with handgun owners had substantially higher suicide rates in both unadjusted and adjusted analyses. Specifically, after adjustment, the relative rate of suicide was higher among exposed cohort members (HR, 1.43; 95% CI, 1.11-1.84). The excess rate was entirely accounted for by higher rates of suicide by firearm (HR, 4.32; 95% CI, 2.89-6.46), as exposed and unexposed women did not have substantively different rates of suicide by other methods (HR, 0.90; 95% CI, 0.63-1.27). Analyses restricted to households in which cohort members lived with only 1 other adult and those in which sex was not imputed produced HRs similar to those from the full cohort (section X in the eAppendix in the Supplement).
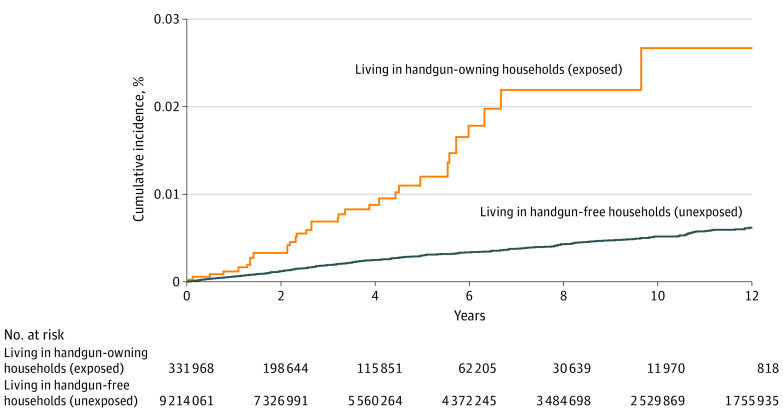
The excess rate of firearm suicide among cohabitants of handgun owners was apparent shortly after the first handgun was purchased and persisted as long as the household contained at least 1 handgun (Figure). The adjusted cumulative incidence of firearm suicide at 10 years was 0.027% (95% CI, 0.016-0.044) for women who were exposed to household firearms and 0.005% (95% CI, 0.005-0.006) for those who were not exposed. Thus, for every 100 000 women who did not own guns in our study who had a handgun enter their previously handgun-free home, we estimate that an extra 21 firearm suicides occurred over the ensuing 10 years compared with the number expected to have occurred had their cohabitants not acquired firearms.
Figure. Adjusted Cumulative Incidence Functions for Suicide by Firearm for Women Exposed and Unexposed to Handgun-Owning Cohabitants.
Sensitivity Analyses
Negative control outcome analyses found that rates of death from alcoholic liver disease (HR, 1.01; 95% CI, 0.75-1.37) and from lung cancer (HR, 0.90; 95% CI, 0.80-1.01) were not higher among women in our study who lived with cohabitants who owned handguns than among those who lived with cohabitants in handgun-free households (section IX in the eAppendix in the Supplement). Bias analyses showed that for a putative confounder to nullify our main results it would need to be strongly associated with our outcome and with living with a handgun owner (section IX in the eAppendix in the Supplement). For example, for a confounder to nullify the positive association detected between cohabitating with a handgun owner and suicide by firearm, it would need to both increase the risk of firearm suicide by a factor of 8 and be 8 times more common among women living with handgun owners than among women living only with nonowners (E-value, 8.1).
Discussion
In this study of 9.5 million women who did not own guns, all of whom resided in homes without handguns at baseline, the rate of death by suicide increased significantly (HR, 1.43; 95% CI, 1.11-1.84) after an adult cohabitant lawfully acquired a handgun. This excess suicide rate, accounted for by a 4-fold increase in suicide by firearm, persisted throughout the 12-year follow-up period. To our knowledge, this study is the first to estimate the association between secondary exposure to household firearms and the rate of suicide among women who do not own handguns.
Limitations
This study has limitations. One threat to the validity of our estimates is unmeasured confounding, with perhaps the greatest concern being that we were unable to adjust for mental illness, a major risk factor for suicide. Residual confounding by mental health conditions is likely to be small and therefore not alter our conclusions for 4 reasons. First, prior research has shown that members of households with and without firearms appear to have similar rates of mental illness, suicidal ideation, and suicide attempts.31,32,33,34,35 Second, as exposure to firearms in our study was positively associated with the rate of suicide by firearms, but not suicide by other methods, it is difficult to imagine what risk factor other than access to a firearm would selectively affect firearm suicide. Third, our negative control outcome analyses did not detect evidence of meaningful residual confounding. Fourth, our computed E-values suggest that even if such an unidentified factor exists, for it to nullify our results it would have to be as strongly associated with firearm suicide as the strongest known suicide risk factors (eg, major depressive disorder and substance use disorder) and 8 times more common among women living with handgun owners than among women living only with nonowners.
Two other threats to validity suggest that the hazard ratios we report are likely to be lower bounds of the hazard associated with secondhand exposure to handguns. First, some cohort members or their cohabitants may have acquired handguns unlawfully (or acquired them before January 1985, the year our data on lawful acquisitions began), thereby biasing our results to the null because some households classified as unexposed may have contained handguns. Second, we only partially accounted for long gun ownership and thus some households unexposed to handguns may have contained unmeasured long guns. This latter omission is unlikely to have had a large effect on our estimates because fewer than 20% of firearm owners in California own only long guns, and only 10% of women who die by firearm suicide use long guns.36,37
Millions of people in the US have become new gun owners since the beginning of the COVID-19 pandemic.38,39,40 Prior work suggests a greater than 3-fold increase in the risk of dying by suicide for adults who become new gun owners.11 A less obvious outcome of the spike in firearm sales that began in March of 2020 is that millions of non–gun owners have also become exposed to household firearms for the first time, most of whom are women and children.40 Although our study data come from an earlier period and are restricted to registered voters, our cohort comprises a heterogeneous sociodemographic mix of adults from the most populous state in the US. Moreover, we have no reason to expect that the women in our study differ from similarly situated women with respect to characteristics that would meaningfully affect generalizability, such as access to the firearms in their home or preferences for particular suicide methods. As such, we conservatively estimate that women in these newly exposed households would be approximately 1.5 times as likely to die by suicide today compared with prior to the COVID-19 pandemic.
Conclusions
Our study tried to estimate changes in suicide rates among women when an adult cohabitant of theirs brought a handgun into their previously handgun-free home. Our estimate that the rate increased by a relative 50% is a statistic that may be of interest to the millions of women who currently do not own guns but reside with other adults who do, to the gun owners with whom they live, and to the tens of millions of other women who currently live in gun-free homes with other adults who may be thinking about buying a handgun.
eAppendix. Supplementary data
References
- 1.Davern M, Bautista R, Freese J, Morgan SL, Smith TW. General Social Survey, 1972-2021. NORC. Accessed March 3, 2022. https://gssdataexplorer.norc.org/
- 2.Centers for Disease Control and Prevention . Web-based Injury Statistics Query and Reporting System (WISQARS). Accessed January 9, 2022. https://www.cdc.gov/injury/wisqars/index.html
- 3.Kellermann AL, Rivara FP, Somes G, et al. Suicide in the home in relation to gun ownership. N Engl J Med. 1992;327(7):467-472. doi: 10.1056/NEJM199208133270705 [DOI] [PubMed] [Google Scholar]
- 4.Anglemyer A, Horvath T, Rutherford G. The accessibility of firearms and risk for suicide and homicide victimization among household members: a systematic review and meta-analysis. Ann Intern Med. 2014;160(2):101-110. doi: 10.7326/M13-1301 [DOI] [PubMed] [Google Scholar]
- 5.Wiebe DJ. Homicide and suicide risks associated with firearms in the home: a national case-control study. Ann Emerg Med. 2003;41(6):771-782. doi: 10.1067/mem.2003.187 [DOI] [PubMed] [Google Scholar]
- 6.Miller M, Barber C, White RA, Azrael D. Firearms and suicide in the United States: is risk independent of underlying suicidal behavior? Am J Epidemiol. 2013;178(6):946-955. doi: 10.1093/aje/kwt197 [DOI] [PubMed] [Google Scholar]
- 7.Dahlberg LL, Ikeda RM, Kresnow MJ. Guns in the home and risk of a violent death in the home: findings from a national study. Am J Epidemiol. 2004;160(10):929-936. doi: 10.1093/aje/kwh309 [DOI] [PubMed] [Google Scholar]
- 8.Brent DA, Perper JA, Moritz G, Baugher M, Schweers J, Roth C. Firearms and adolescent suicide. a community case-control study. AJDC. 1993;147(10):1066-1071. doi: 10.1001/archpedi.1993.02160340052013 [DOI] [PubMed] [Google Scholar]
- 9.Cummings P, Koepsell TD, Grossman DC, Savarino J, Thompson RS. The association between the purchase of a handgun and homicide or suicide. Am J Public Health. 1997;87(6):974-978. doi: 10.2105/AJPH.87.6.974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-1457. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 11.Studdert DM, Zhang Y, Swanson SA, et al. Handgun ownership and suicide in California. N Engl J Med. 2020;382(23):2220-2229. doi: 10.1056/NEJMsa1916744 [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y, Holsinger EE, Prince L, et al. Assembly of the LongSHOT cohort: public record linkage on a grand scale. Inj Prev. 2020;26(2):153-158. doi: 10.1136/injuryprev-2019-043385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915-920. doi: 10.1093/aje/kwg231 [DOI] [PubMed] [Google Scholar]
- 14.California Penal Code §§11106, 26905.
- 15.Imai K, Khanna K. Improving ecological inference by predicting individual ethnicity from voter registration records. Polit Anal. 2016;24:263-272. doi: 10.1093/pan/mpw001 [DOI] [Google Scholar]
- 16.Mullen L, Blevins C, Schmidt B. Package ‘gender’: predict gender from names using historical data. Accessed November 29, 2021. https://cran.r-project.org/web/packages/gender/gender.pdf
- 17.US Census Bureau . 2010 Census summary file 1. Accessed March 29, 2022. https://www2.census.gov/programs-surveys/decennial/2010/technical-documentation/complete-tech-docs/summary-file/sf1.pdf
- 18.United States Census Bureau . Geographic areas reference manual. November 29, 2021. https://www.census.gov/programs-surveys/geography/guidance/geographic-areas-referencemanual.html
- 19.California Penal Code §§16720, 27875.
- 20.Austin PC, Latouche A, Fine JP. A review of the use of time-varying covariates in the Fine-Gray subdistribution hazard competing risk regression model. Stat Med. 2020;39(2):103-113. doi: 10.1002/sim.8399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cole SR, Hernán MA. Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed. 2004;75(1):45-49. doi: 10.1016/j.cmpb.2003.10.004 [DOI] [PubMed] [Google Scholar]
- 22.Neumann A, Billionnet C. Covariate adjustment of cumulative incidence functions for competing risks data using inverse probability of treatment weighting. Comput Methods Programs Biomed. 2016;129:63-70. doi: 10.1016/j.cmpb.2016.03.008 [DOI] [PubMed] [Google Scholar]
- 23.Lipsitch M, Tchetgen Tchetgen E, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology. 2010;21(3):383-388. doi: 10.1097/EDE.0b013e3181d61eeb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Darvishi N, Farhadi M, Haghtalab T, Poorolajal J. Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PLoS One. 2015;10(5):e0126870. doi: 10.1371/journal.pone.0126870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller M, Hemenway D, Rimm E. Cigarettes and suicide: a prospective study of 50,000 men. Am J Public Health. 2000;90(5):768-773. doi: 10.2105/AJPH.90.5.768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Norström T, Rossow I. Alcohol consumption as a risk factor for suicidal behavior: a systematic review of associations at the individual and at the population level. Arch Suicide Res. 2016;20(4):489-506. doi: 10.1080/13811118.2016.1158678 [DOI] [PubMed] [Google Scholar]
- 27.Poorolajal J, Darvishi N. Smoking and suicide: a meta-analysis. PLoS One. 2016;11(7):e0156348. doi: 10.1371/journal.pone.0156348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76(suppl):S11-S19. doi: 10.1016/j.drugalcdep.2004.08.003 [DOI] [PubMed] [Google Scholar]
- 29.Mathur MB, VanderWeele TJ. Sensitivity analysis for unmeasured confounding in meta-analyses. J Am Stat Assoc. 2020;115(529):163-172. doi: 10.1080/01621459.2018.1529598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the e-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 31.Ilgen MA, Zivin K, McCammon RJ, Valenstein M. Mental illness, previous suicidality, and access to guns in the United States. Psychiatr Serv. 2008;59(2):198-200. doi: 10.1176/ps.2008.59.2.198 [DOI] [PubMed] [Google Scholar]
- 32.Miller M, Barber C, Azrael D, Hemenway D, Molnar BE. Recent psychopathology, suicidal thoughts and suicide attempts in households with and without firearms: findings from the National Comorbidity Study Replication. Inj Prev. 2009;15(3):183-187. doi: 10.1136/ip.2008.021352 [DOI] [PubMed] [Google Scholar]
- 33.Sorenson SB, Vittes KA. Mental health and firearms in community-based surveys: implications for suicide prevention. Eval Rev. 2008;32(3):239-256. doi: 10.1177/0193841X08315871 [DOI] [PubMed] [Google Scholar]
- 34.Miller M, Swanson SA, Azrael D. Are we missing something pertinent? a bias analysis of unmeasured confounding in the firearm-suicide literature. Epidemiol Rev. 2016;38(1):62-69. doi: 10.1093/epirev/mxv011 [DOI] [PubMed] [Google Scholar]
- 35.Swanson SA, Eyllon M, Sheu YH, Miller M. Firearm access and adolescent suicide risk: toward a clearer understanding of effect size. Inj Prev. 2020;injuryprev-2019-043605. doi: 10.1136/injuryprev-2019-043605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hanlon TJ, Barber C, Azrael D, Miller M. Type of firearm used in suicides: findings from 13 states in the National Violent Death Reporting System, 2005-2015. J Adolesc Health. 2019;65(3):366-370. doi: 10.1016/j.jadohealth.2019.03.015 [DOI] [PubMed] [Google Scholar]
- 37.Kravitz-Wirtz N, Pallin R, Miller M, Azrael D, Wintemute GJ. Firearm ownership and acquisition in California: findings from the 2018 California Safety and Well-being Survey. Inj Prev. 2020;26(6):516-523. doi: 10.1136/injuryprev-2019-043372 [DOI] [PubMed] [Google Scholar]
- 38.Crifasi CK, Ward JA, McGinty EE, Webster DW, Barry CL. Gun purchasing behaviours during the initial phase of the COVID-19 pandemic, March to mid-July 2020. Int Rev Psychiatry. 2021;33(7):593-597. doi: 10.1080/09540261.2021.1901669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lyons VH, Haviland MJ, Azrael D, et al. Firearm purchasing and storage during the COVID-19 pandemic. Inj Prev. 2021;27(1):87-92. doi: 10.1136/injuryprev-2020-043872 [DOI] [PubMed] [Google Scholar]
- 40.Miller M, Zhang W, Azrael D.. Firearm purchasing during the COVID-19 pandemic: results from the 2021 National Firearms Survey Annals of Internal Medicine. 2022;175:219-225. doi: 10.7326/M21-3423 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplementary data