Abstract
Objectives
To examine women’s perceptions of endometriosis-associated disease burden and its impact on life decisions and goal attainment.
Design
An anonymous online survey was distributed in October 2018 through the social media network MyEndometriosisTeam.com.
Participants
Women aged 19 years and older living in several English-speaking countries who self-identified as having endometriosis.
Outcome measures
Patients’ perspectives on how endometriosis has affected their work, education, relationships, overall life decisions and attainment of goals. Subanalyses were performed for women who identified as ‘less positive about the future’ (LPAF) or had ‘not reached their full potential’ (NRFP) due to endometriosis.
Results
743 women completed the survey. Women reported high levels of pain when pain was at its worst (mean score, 8.9 on severity scale of 0 (no pain) to 10 (worst imaginable pain)) and most (56%, n=415) experienced pain daily. Women reported other negative experiences attributed to endometriosis, including emergency department visits (66%, n=485), multiple surgeries (55%, n=406) and prescription treatments for symptoms of endometriosis (72%, n=529). Women indicated that they believed endometriosis had a negative impact on their educational and professional achievements, social lives/relationships and overall physical health. Most women ‘somewhat agreed’/‘strongly agreed’ that endometriosis caused them to lose time in life (81%, n=601), feel LPAF (80%, n=589) and feel they had NRFP (75%, n=556). Women who identified as LPAF or NRFP generally reported more negative experiences than those who were non-LPAF or non-NRFP.
Conclusions
Women who completed this survey reported pain and negative experiences related to endometriosis that were perceived to negatively impact major life-course decisions and attainment of goals. Greater practitioner awareness of the impact that endometriosis has on a woman’s life course and the importance of meaningful dialogue with patients may be important for improving long-term management of the disease and help identify women who are most vulnerable.
Keywords: gynaecology, community gynaecology, qualitative research
Strengths and limitations of this study.
A strength of our study is use of a quantitative survey with a meaningful sample size and sample population that spanned multiple countries.
This study is strengthened by targeted research questions developed based on existing conversations on a social network platform.
Another strength of this study is the use of a social network familiar to patients, facilitating honesty in responses to sensitive topics.
An important limitation of our study is possible self-selection bias due to voluntary participation in an online community and no targeted sampling; quantitative data may therefore not be generalisable to all women with endometriosis.
The study is limited by self-reported patient responses that were not confirmed by medical records or other complementary data.
Introduction
Endometriosis is an often chronic gynecologic disorder that impacts 10% of women of reproductive age.1 Endometrial-like tissue thriving outside the uterus leads to local and systemic inflammation that can result in a wide range of life-impacting effects, including pelvic pain, dysmenorrhea, dyspareunia and infertility.2–4 These debilitating effects have an immense impact on a patient’s quality of life and overall well-being.5 6 For example, symptoms of endometriosis may have a negative impact on women’s psychological health,7 8 strain social and intimate relationships5 9–11 and lead to losses in productivity, both at home and in the workplace.12 These issues have been further exacerbated by the COVID-19 pandemic, which has led to reduced access to medical care, delayed treatments, increased stress, loss of work productivity and mandated self-isolation.13 14
Outside the physical and emotional toll, the collective symptoms of endometriosis are also associated with direct and indirect costs that are burdensome to patients. Visits to physicians and emergency departments, pharmacy claims and other direct expenses are estimated to cost between $12 000 and $15 000 per patient per year in the USA, and the loss of work and productivity may amount to additional losses of thousands of dollars per patient.12 15–18
Most studies examining chronic diseases like endometriosis focus on one or two specific areas of the disease, such as its social, physical or psychological impact at a specific point in time.19 20 In contrast, few studies have examined the impact of endometriosis on a woman’s life course (ie, ‘life-course impairment’) based on how symptoms and experiences resulting from the disease influence major life events and decisions (such as whether to pursue educational opportunities, choose a career path, establish intimate relationships and plan for a family) and the overall ability of patients to attain their life goals.19 20 The few existing studies have small sample sizes or are qualitative, relying on informational interviews to ascertain the life-course impact of the disease, but highlight the substantial impacts that endometriosis can have on social activities, intimate relationships, education, work productivity and psychological well-being.11 21–23 Understanding life-course impairment, as opposed to focusing on the symptoms of the disease (such as pain or infertility, which are most often addressed individually not holistically), is vital because of the complicated inter-relationship among symptoms and their downstream effects. Individual symptoms can influence critical life decisions (eg, work, education or personal relationships) in ways that are interrelated and can impact other areas of a patient’s life. For example, chronic pain may influence the type and amount of work performed or whether a patient decides to work at all, which, in turn, can have financial implications on the patient’s lifestyle, family, relationships or sense of personal fulfilment.19 20 Symptoms may determine where a patient chooses to live because of financial considerations, healthcare access or proximity to support networks. Similarly, dyspareunia related to endometriosis may lead some women to avoid intimate relationships, which may have downstream implications for marriage, family planning and mental and emotional health.24 25 Cumulatively, persistent symptoms of endometriosis and their impact on daily activities and family and intimate relationships can negatively impact the trajectory of women’s lives and are profound and far-reaching.
The objective of this multinational survey was to gain a better understanding of patient perspectives on how endometriosis impacts their daily activities and identify how the disease may influence women’s major life decisions and attainment of their goals. In addition, we sought to understand the endometriosis-related life-course impacts specifically in women who reported low optimism or low goal attainment by investigating the specific reasons for life-course impairment among the subset of women who felt their lives were most negatively impacted by endometriosis. Insights into a patient’s complete experience with endometriosis are needed to develop and provide access to effective treatments to reduce the negative impacts of endometriosis on a woman’s life course. Greater awareness of the potential negative life-course impacts of endometriosis is important for helping physicians to identify and understand patients’ needs and improve the long-term management of endometriosis.
Methods
Ethics approval
The Advarra Institutional Review Board (Columbia, MD, USA) reviewed the cross-sectional survey for participants in the USA and determined that informed consent was not required (exempt determination #Pro00029982, 26 September 2018). However, participants did consent to participate in a survey and email invitations were provided to people who opted to receive communications.
Survey development
An online survey was created in a collaborative effort between AbbVie (North Chicago, IL, USA) and MyHealthTeams (San Francisco, CA, USA), a company that creates social networks for communities of individuals living with chronic conditions to foster discussion and provide support among people facing similar circumstances. The survey was programmed and administered through Qualtrics, an online survey tool that allows users to capture survey responses in an anonymised manner. The survey was provided in English and was available online on the social media network website MyEndometriosisTeam.com from 3 October to 25 October 2018. The 14 survey questions about women’s experiences with endometriosis were based on our knowledge about the disease state, existing publications and online conversations participants were having (see ‘Patient and public involvement’ for further detail). In addition, the survey contained four screening questions and six demographic questions (identified as online supplemental file). The primary goal of the survey was to capture patients’ perspectives on the negative impacts of endometriosis on different aspects of their life courses, including how endometriosis has affected their work, education, relationships, overall life decisions and attainment of goals. This portion of the survey was modelled after a validated instrument created to measure life-course impact of disease in patients with psoriasis.25 This tool was used as a starting point for model development as it has been validated for another chronic disease with excess psychological and psychosocial burden, has been used clinically and was published in the scientific literature. Survey questions were rotated to avoid any bias introduced by order of answer selections. Most survey questions were closed-ended and provided multiple-choice options to participants; two questions were open-ended and allowed participants to provide written responses detailing any life accomplishments they believed were impeded by endometriosis or to offer anything else they wanted to share about the impact of endometriosis on their lives. Responses were required for all closed-ended questions; therefore, no imputations for missing data were required. The survey used in this study is included in the supplementary material.
bmjopen-2021-052765supp001.pdf (1.7MB, pdf)
Patient and public involvement
Survey questions were developed based on conversations members were having on MyEndometriosisTeam.com to ensure both relevance of topics and patient-focused language. The social media network, MyEndometriosisTeam.com, was developed for women living with endometriosis and consists of more than 108 000 members across 13 countries. Based on institutional review board exemption requirements, people were asked at the beginning of the survey if they agreed to participate, and email invitations were sent only to those people who opted into receiving communications.
Participant eligibility and recruitment
Members of the social network MyEndometriosisTeam.com were recruited through 33 000 email invitations. Invitations posted on the public Facebook page for MyEndometriosisTeam recruited additional women to participate in the survey, which was live on the MyEndometriosisTeam.com website from 3 October to 25 October 2018. The English-language survey was conducted among an international population of women who were at least 19 years of age and who self-identified as having endometriosis. The survey was anonymous, and answers could not be linked to individual members.
Survey analysis
Descriptive statistics were used to tabulate survey responses in this cross-sectional study. After descriptive statistics were quantified for all respondents, a subanalysis was performed that restricted the survey responder population to women who ‘somewhat agreed’ or ‘strongly agreed’ that they were ‘less positive about the future’ (LPAF) or that they had ‘not reached their full potential’ (NRFP) because of endometriosis. These two questions were selected for this subanalysis to focus on the life-course impact attributed to endometriosis as identified by those who reported low optimism or low goal attainment. For this analysis, life-course impairment was defined as respondents who ‘somewhat agreed’ or ‘strongly agreed’ that endometriosis had negatively impacted their education, employment, relationships, social activities and physical and emotional well-being.
Results
Survey response and demographics
A total of 743 women completed the survey (table 1), which was live from 3 October to 25 October 2018.
Table 1.
Demographics and burden of endometriosis
| Characteristic | Overall respondents, n (%) (n=743) | LPAF respondents, n (%) (n=589) | NRFP respondents, n (%) (n=556) |
| Age at time of survey, years | |||
| 19–29 | 206 (28) | 179 (30) | 155 (28) |
| 30–39 | 339 (46) | 269 (46) | 259 (47) |
| 40–49 | 180 (24) | 128 (22) | 129 (23) |
| 50 or older | 18 (2) | 13 (2) | 13 (2) |
| Country | |||
| USA (excluding Puerto Rico*) | 474 (64) | 370 (63) | 364 (65) |
| UK | 128 (17) | 102 (17) | 92 (17) |
| Canada | 38 (5) | 32 (5) | 30 (5) |
| Australia | 37 (5) | 31 (5) | 27 (5) |
| South Africa | 20 (3) | 15 (3) | 9 (2) |
| Ireland | 17 (2) | 15 (3) | 12 (2) |
| Other | 15 (2) | 12 (2) | 13 (2) |
| New Zealand | 11 (1) | 9 (2) | 8 (1) |
| The Netherlands | 3 (0.4) | 3 (1) | 1 (<0.1) |
| Level of education | |||
| Some high school or less | 33 (4) | 21 (4) | 20 (4) |
| High school diploma | 111 (15) | 80 (14) | 76 (14) |
| Some college | 214 (29) | 164 (28) | 176 (32) |
| College degree | 254 (34) | 129 (22) | 113 (20) |
| Graduate school/degree | 111 (15) | 59 (10) | 50 (9) |
| Prefer not to answer | 20 (3) | 15 (3) | 10 (2) |
| Endometriosis stage | |||
| Stage 1 | 33 (4) | 24 (4) | 22 (4) |
| Stage 2 | 39 (5) | 28 (5) | 29 (5) |
| Stage 3 | 93 (13) | 70 (12) | 73 (13) |
| Stage 4 | 223 (30) | 191 (32) | 171 (31) |
| Not sure | 355 (48) | 276 (47) | 261 (47) |
| Method of diagnosis | |||
| Laparoscopic surgery | 650 (87) | 518 (88) | 494 (89) |
| Clinical only | 87 (12) | 66 (11) | 57 (10) |
| Not sure | 6 (0.8) | 5 (1) | 5 (1) |
*Patients from Puerto Rico were separated from the US population into the ‘other’ category due to institutional review board exemption qualifications that were different for residents of Puerto Rico vs residents of the 50 states of the USA.
LPAF, less positive about the future; NRFP, not reached their full potential.
Among respondents to the English-language survey, 474 (64%) were from the USA and 269 (36%) were from other countries, including one-fifth from the UK (17%, n=128), and one-fifth summed from Canada, Australia, South Africa, Ireland, New Zealand and The Netherlands (table 1). Most women (73%, n=542) were younger than 40 years of age. Almost half of the respondents (48%, n=355) were unaware of their stage of endometriosis (according to the revised American Society for Reproductive Medicine (rASRM) scoring system), which was obtained at their most recent surgery. Among the 52% of respondents who recalled their rASRM score, most (57%, n=223) reported having stage 4 endometriosis (table 1). Baseline demographics were generally comparable between the overall study population and women who identified as LFAP or NRFP (table 1).
Diagnosis and symptoms
Diagnosis
Women began experiencing symptoms of endometriosis at a young age, with many experiencing symptoms by age 15. Most women (74%, n=549) reported having a diagnosis of endometriosis made more than 3 years after the appearance of symptoms (average delay of approximately 9 years). Nearly half of women (42%, n=313) said it took 10 years or longer after the initial onset of their symptoms to receive a surgical or clinical diagnosis of endometriosis. The younger the woman’s age at symptom onset, the longer the delay; it took, on average, 13 years to reach a surgical diagnosis for women who began experiencing symptoms by age 13. Most women (87%, n=650) reported their diagnosis had been confirmed by laparoscopy (table 1).
Endometriosis-associated pain
Most women (56%, n=415) reported experiencing pain daily and nearly an additional one-quarter of them reported feeling endometriosis-associated pain a few times per week. When asked to rate how severe their pain was in the last 12 months on a scale from 0 (no pain) to 10 (worst imaginable pain), more than half of the respondents (54%) rated their worst pain within the last 12 months as a 9 or 10. About two-thirds of women reported their endometriosis-associated pain had worsened over the years when asked if endometriosis-related pain had gotten better, worse or stayed the same.
Life-course impairment
Education and employment potential
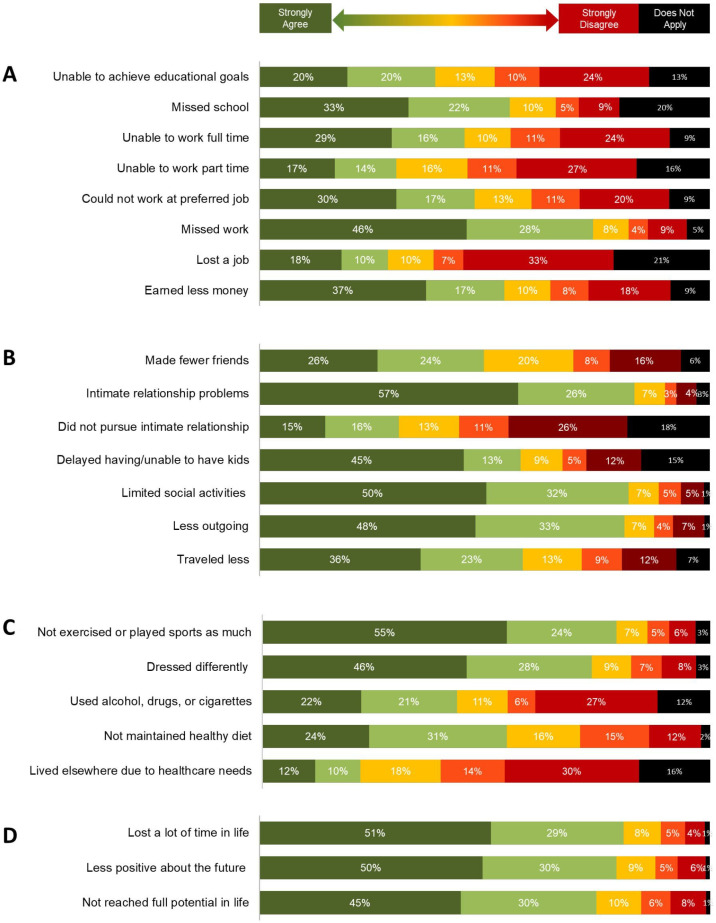
Many of the women surveyed said they ‘somewhat agreed’ or ‘strongly agreed’ that they had experienced difficulties achieving their educational goals (40%, n=290) or had missed school (55%, n=413) because of endometriosis-associated symptoms (figure 1A). Almost half of participants (45%, n=338) ‘somewhat agreed’ or ‘strongly agreed’ that they could not work full time, and a similar percentage (47%, n=355) reported not working at a job they would have preferred. Most reported that they had missed work (74%, n=550) or earned less money than they could have (54%, n=404) because of endometriosis-associated symptoms. These findings were consistent among patients in the USA compared with the rest of the world (online supplemental figure 1).
Figure 1.
Life-course impact of endometriosis. Women were asked to indicate how much they agreed with statements involving the impact of endometriosis on (A) educational and professional achievements, (B) social life and relationships, (C) physical well-being and (D) overall life course.
Relationships and social engagements
Most women ‘somewhat agreed’ or ‘strongly agreed’ that endometriosis-associated symptoms led to problems in their intimate relationships (83%, n=613) and/or created a barrier to starting a family (58%, n=431). Most women similarly believed that endometriosis-associated symptoms had led them to limit their social activities (82%, n=609), made them less outgoing (81%, n=602) and caused them to travel less (59%, n=434) (figure 1B).
Physical well-being
Most women ‘somewhat agreed’ or ‘strongly agreed’ endometriosis limited their ability to stay active (79%, n=588) and maintain a healthy diet (55%, n=406) (figure 1C). A high proportion of women (43%, n=323) perceived that endometriosis-associated symptoms resulted in use of alcohol, drugs or cigarettes.
Life-course impairment overall
Overall, most women (80%, n=601) ‘somewhat agreed’ or ‘strongly agreed’ endometriosis-associated symptoms had caused them to lose time from their daily lives (figure 1D). A similar number of women reported that they were less positive about the future because of their endometriosis-associated symptoms (80%, n=589), and 75% (n=556) ‘somewhat agreed’ or ‘strongly agreed’ that endometriosis-associated symptoms had kept them from reaching their full potential in life.
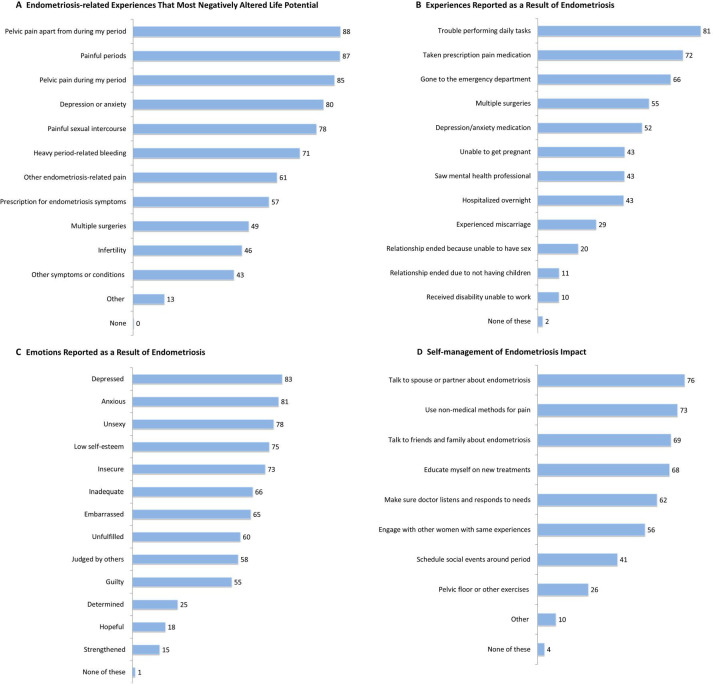
Experiences and emotions associated with endometriosis
Women reported that numerous experiences attributed to endometriosis had altered their life potential in a negative way (figure 2A) or negatively impacted their lives in other ways (figure 2B). The most frequent responses were common symptoms of endometriosis, including pelvic pain apart from menstruation, painful menstruation, pelvic pain during menstruation, and painful sexual intercourse.
Figure 2.
Experiences and emotions attributed to endometriosis. Respondents were asked to select which experiences related to endometriosis had the most negative impacts on their life potential. (A) Women were also asked to indicate which general negative experiences (B) and emotions (C) they had undergone because of endometriosis and what kinds of approaches they had taken to manage the impact of endometriosis (D).
Most women surveyed reported that endometriosis impacted their ability to perform daily tasks (81%, n=594); however, many of the negative experiences attributed to endometriosis were related to the use of healthcare services and treatments. For example, women reported taking prescription pain medications (72%, n=529), visiting emergency departments (66%, n=485), having multiple surgeries (55%, n=406), being hospitalised overnight (43%, n=313), taking prescription medication for depression or anxiety (52%, n=380) or seeing a mental health professional because of their endometriosis-associated symptoms (43%, n=316). Around half of the women surveyed reported that the experiences that most negatively impacted their lives were their need to take prescription medication (57%, n=427) and the multiple surgeries for endometriosis (49%, n=363). In addition, most women surveyed reported several negative emotions that they attributed to endometriosis, including feeling depressed (83%, n=607), anxious (81%, n=592), unsexy (78%, n=572) or having low self-esteem (75%, n=554; figure 2C).
Women managed the impact of their endometriosis in different ways (figure 2D). Most commonly, this included talking to a spouse or partner about their condition, using non-medical strategies (such as diet or exercise) to control their pain and seeking support from friends and family.
Additional analysis of women who believed their future and life potential were more impacted by endometriosis
Most of the sample included women who ‘somewhat agreed’ or ‘strongly agreed’ that they were LPAF (80%; n=589) or had NRFP in life (75%; n=556) because of endometriosis, and several questions limited to these women were further analysed (online supplemental table 1). Overall, the observational data in this study suggested women who believed they were LPAF or had NRFP generally reported more negative experiences than the fewer respondents who did not indicate they were LPAF (non-LPAF, 21%; n=154) or had NRFP (non-NRFP, 25%; n=187). Daily pain was reported by 62% of women who believed they were LPAF and 61% of women who had NRFP because of endometriosis (34% non-LPAF and 40% non-NRFP; online supplemental table S1A). Women who believed they were LPAF or had NRFP also reported negative experiences related to education and work they attributed to endometriosis, including having earned less money (61% LPAF, 29% non-LPAF, 66% NRFP and 21% non-NRFP), not working a preferred job (54% LPAF, 25% non-LPAF, 58% NRFP and 17% non-NRFP) or not achieving educational goals (44% LPAF, 21% non-LPAF, 47% NRFP and 16% non-NRFP) (online supplemental table S1B). Most women who believed their future and life potential were more impacted by their disease reported endometriosis-related experiences altered their life potential in a negative way (online supplemental table S1C). Similarly, many of these women reported negative experiences and emotions they attributed to endometriosis (online supplemental table S1D, E). All women used similar strategies to cope with and mitigate the impact of endometriosis on their lives (online supplemental table 1F).
Discussion
This survey found that women with endometriosis who self-reported pronounced symptoms reported experiences that negatively impacted their perspective of the future and overall life potential. For many women, endometriosis-associated symptoms negatively affect various areas of their lives, including education and employment, relationships and social engagements and physical well-being. Participants indicated that adverse experiences related to management of their disease and its impact on everyday life also believed that their future and life potential were negatively impacted by endometriosis.
Study implications
The severity of pain reported by women who completed the online survey indicates that respondents in our study may have had a greater symptom burden than did women participating in previous studies using similar pain scales.26–28 Women in our study also reported slightly lengthier delays in diagnosis after the onset of their first symptoms. Findings in previous studies have illustrated that delays are common in diagnosing endometriosis.15 29–37 Although some recent literature suggests that the delay in diagnosis may be slowly improving,35 the use of non-invasive and accurate diagnostic tools could improve diagnosis times and reduce women’s pain and distress.37 38 The delays in diagnosis reported by our study participants and others indicate many women experiencing troublesome symptoms of endometriosis may still wait extended periods before receiving a definitive diagnosis and initiating treatment.
The higher pain burden and longer diagnostic delay reported in our sample, which may include higher numbers of women who sought social network support because they were more frustrated with their disease experience, could conceivably be due in part to their longer struggles with more challenging symptoms than would be observed in the general population of women with diagnosed endometriosis. Results from a recent study using the same social network to recruit participants found that the majority of respondents rated their worst pain higher than 7 on a 10-point scale, only a little lower than the pain rating given by the women in our study.39 Additionally, the previous study participants also experienced a diagnostic delay, supporting the theory that recruitment from this member-centred network may draw more women who have struggled longer with their disease.39 Interestingly, overall trends in diagnostic delays observed between age groups in our study are consistent with reports in previous research, that is, women whose symptom onset occurred at a younger age experienced longer times to diagnosis.15 31 35
Many respondents said they missed school and were generally unable to achieve their educational goals because of endometriosis. There is a dearth of research on the impact of endometriosis on women’s educational aspirations and their ability to achieve goals due to endometriosis-associated symptoms, compared with the impact endometriosis has on professional work or other areas of life.9 Findings from some existing studies suggest endometriosis-associated symptoms may impact grades, attendance or completion of educational programmes.21 22 40 Although informative, these studies were more qualitative in nature and involved small sample sizes.21 22 40 A quantitative study examining the lives of 78 women 15 years after receiving a verified diagnosis of endometriosis found only a fraction of women reported that their disease had a negative impact on their education.11 However, the women included in that study seemed to report less frequent pain and endometriosis-related effects, like depression, compared with the reports made by women in our study. Furthermore, the small sample was collected at a single Norwegian hospital and the findings may not be representative of women’s experiences with endometriosis on a wider scale.11 Regardless, any impact on education is concerning, and our study results emphasise the need for additional research into this overlooked area in women with endometriosis. Research on other medical conditions, like adolescent fibromyalgia, supports that chronic pain can negatively impact education, reinforcing the likelihood that endometriosis may have a similar impact.41 42
Respondents in the current study also reported endometriosis-associated symptoms caused them to miss work, earn less money, prevented them from a job they would have preferred or impeded their working full time or part time. Many health conditions that can occur with endometriosis can impact work productivity and potential, including depression, other chronic pain conditions or disorders and digestive disorders.43 Endometriosis was self-reported by respondents in this study, and it is possible that other chronic conditions (particularly, chronic overlapping pain conditions) may also contribute to women’s perceived interference with productivity and employment opportunities. Indeed, more than half of women with symptomatic endometriosis can be present with comorbid pain syndromes,44 and these may include conditions associated with pelvic pain, like dysmenorrhea, irritable bowel syndrome or painful bladder syndrome.45 46 Findings from previous studies have also illustrated that endometriosis-associated symptoms may lead to losses in productivity both at home and in the workplace, potentially impacting professional achievement.12 34 47 48 In our study, most women who indicated that they were LPAF or had NRFP because of endometriosis reported painful symptoms and negative experiences. Also, women who were LPAF or had NRFP often believed it was harder to perform daily tasks because of their disease.
Our results further support that endometriosis symptoms are disruptive and may lead to loss of productivity, ultimately influencing women’s major life decisions or consequences, including whether to work at reduced capacity or pursue preferred jobs. Results from a recent multicentre study of women with confirmed endometriosis and a matched comparison group found the disease forced some women to seek work outside desired professions, which, in turn, resulted in health-related limitations in career choices.48 These collective findings are concerning because satisfaction in a chosen profession—or, at a minimum, the options available to make life decisions regarding one’s profession—is an important component of an overall satisfying quality of life, and the decision to work less or pursue a less desirable job may have downstream implications for women’s finances, relationships, social lives, or travel decisions.19 48
Respondents to our survey reported endometriosis had a negative impact on their relationships, social engagements and ability to have children (when desired), which is consistent with findings from a host of previous studies that demonstrated the negative impacts of endometriosis on social well-being and health-related quality of life.9 12 34 47 Interestingly, 46% of women in our study reported experiencing infertility, which is slightly higher than the 14%–40% range reported in previous studies, again hinting at our population’s higher symptom burden.34 39 49 Other chronic pain conditions have also impacted these life-course components, including conditions related to musculoskeletal pain and chronic back pain.50 51
Similar to decisions involving education and professional achievement, life choices involving the pursuit of intimate relationships or starting a family may have downstream implications in other areas, like finance, psychological well-being or employment, which may have their own downstream impacts on additional aspects of a person’s life course.19 Likewise, women frequently reported not being physically active and having poorer diets because of their disease. Although few studies have examined this aspect of endometriosis, findings from two smaller studies have suggested that pain associated with the disease may also have a negative impact on exercise and nutrition.9 30 52
Of particular concern was the view of many women that their disease made them increase their use of alcohol, drugs or cigarettes. Research into whether pain and experiences related to endometriosis may be associated with higher rates of substance abuse is severely lacking. However, there are demonstrated associations between other chronic pain conditions and substance abuse that support our finding.53 54 The results from our study draw attention to this issue and highlight substance abuse as an important avenue for additional investigation.
The findings from our study indicate that women with endometriosis may experience many healthcare-related side effects. Of particular concern, patients noted that treatments meant to help reduce the burden of endometriosis may have their own negative impact. Many women perceived that use of prescription medications and multiple surgeries to control the symptoms of endometriosis had a negative impact on their life potential, and this response was also observed in women who indicated they were LPAF or believed they had NRFP due to their disease. Results from one recent study showed that medical treatment for a condition may increase a patient’s stress levels and potentially affect their psychological health.55 Patients who were taking prescription medications and who experienced more challenging adverse effects from their therapies had higher perceived stress levels, and women undergoing multiple surgeries were especially impacted. These reports underscore the potential value of supportive psychological care for patients with endometriosis as part of effective long-term disease management.
In general, women experienced a range of consequences that they attributed to living with and managing the limitations imposed by endometriosis. In addition to pain, women reported that the endometriosis-related experiences that most impacted their lives in a negative way included depression or anxiety (80%), heavy menstrual bleeding (71%), the need to take prescription treatments (57%) or undergo multiple surgeries (49%) or infertility (46%). In other studies, women have reported not feeling ‘normal’ or feminine, experiencing a range of negative emotions (eg, anger, depression, hopelessness, disappointment and exhaustion), having limited physical or sexual activity, struggling to find appropriate treatments, feeling guilt over disrupted relationships and suffering in silence due to endometriosis-related symptoms.22 23While each woman experienced the impact of endometriosis differently, the majority believed that they were living life less fully than they could have because of their endometriosis-associated symptoms. This belief was informed by the symptoms and healthcare requirements they faced, and, in turn, may have influenced major life decisions that could have their own deleterious effects on personal fulfilment and life potential. The interconnectedness of effects triggered by major life decisions highlights the importance of conducting further research into the cumulative burden of debilitating diseases like endometriosis within the context of an individual’s life course.
Strengths and limitations
Limitations of this study include the selection of participants from an online community with voluntary participation, no targeted sampling and no way to calculate a response rate. The participants were generally well educated, had access to healthcare and participated in an online patient social network. Data on race, ethnicity or socioeconomic status were not collected. Patients who experienced the most significant psychosocial impacts of endometriosis or lacked the resources to access the online community may not have been represented in the sample population, whereas the patients who were most affected by severe pelvic pain may have been more likely to participate in the study. These factors may have led to self-selection bias; therefore, the results of this study may not be generalisable to the overall population of patients with endometriosis. Any between-group comparisons are observational in nature and no definitive conclusions can be made in the absence of formal statistical analysis.
Future implications
Examining the cumulative life-course impact of endometriosis may influence a physician’s ability to understand a woman’s complete experience with the disease, help identify patients who are most vulnerable to its impacts and inform options for management.9 20 22 56 A fuller understanding of the life-course impact of endometriosis may also elucidate patterns of patient needs and identify which forms of supportive multidisciplinary care are necessary, including the need for early referral to specialists and other professionals who provide complementary healthcare. These needs are likely to change over time, during the different phases of each patient’s life. For example, teams that include gynaecologists and pain specialists may help patients manage endometriosis-associated pain symptoms; reproductive endocrinologists may help manage infertility, if this occurs; sexual health counsellors may collaborate with patients who have dyspareunia and counsellors/psychologists may assist with chronic stress and mental health issues.57 Physicians who are responsive to patients’ individual needs and values can positively support overall quality of life in those patients who experience infertility58 59 and other negative symptoms of endometriosis, such as chronic abdominal pain, dysmenorrhea and dyspareunia.24 Endometriosis may also contribute to social inequalities; further research is needed to explore this topic and develop social policies to address these inequalities.
Conclusion
In our international survey of the impact of endometriosis on a woman’s life course, most respondents self-reported a high burden associated with the disease that affected overall life potential in many different ways. The findings of this survey add to our understanding of women’s experiences with endometriosis.
Supplementary Material
Acknowledgments
Financial assistance in developing the survey and collecting data was provided by AbbVie. In partnership with MyHealthTeams, AbbVie participated in the interpretation of data, review and approval of the manuscript, and was involved in the decision to submit the manuscript for publication. Medical writing support, funded by AbbVie, was provided by Michael M Schofield, PhD, Callie A S Corsa, PhD and Kersten Reich, MPH, CMPP, of JB Ashtin, who developed the first draft based on an author-approved outline and assisted in implementing author revisions.
Footnotes
Contributors: SAM, FT, OAF, AH, BS and SA-S contributed to the study concept and design. BS contributed to data acquisition and statistical analysis. SAM, FT, AMS, SCh, SCr, SE, OAF, AH, BS and SA-S contributed to data interpretation. SAM is responsible for the overall content as the guarantor.
Funding: Financial support for this study was provided by AbbVie Inc (award/grant number NA).
Competing interests: SAM is a consultant for AbbVie, Oratel Diagnostics and Celmatix and receives research support from the National Institutes of Health, Department of Defense and Marriott Family Foundations. FFT has received research support from NICHD-NIH and NIDDK-NIH, earns royalties from UpToDate, has served as a consultant for AbbVie, Myovant, and Uroshape, and conducts sponsored research for Eximis and Dot Laboratories. AMS, SCh, SCr, SE and OAF are employees of AbbVie and may own AbbVie stock/stock options. AH has received grant funding from the UK MRC, NIHR, CSO, Wellbeing of Women, Ferring, AstraZeneca, the Charles Wolfson Charitable Trust and Standard Life. His institution has received consultancy fees from Roche Diagnostics, Nordic Pharma, Ferring and AbbVie. He is Chair of the RCOG Academic Board, ESHRE National Representative for the UK, WES Board Member and Ambassador, SEUD Board Member, Trustee and Medical Advisor to Endometriosis UK and Medical Advisor to Pelvic Pain Support Network. BS is an employee of MyHealthTeams, which received compensation for the study and conducted the research on behalf of AbbVie. SA-S earns author royalties from UpToDate and has served as a consultant for AbbVie, Myovant and Eximis.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. AbbVie is committed to responsible data sharing regarding the clinical trials and studies we sponsor. This includes access to anonymised, individual and trial-level data (analysis data sets), as well as other information (eg, protocols and clinical study reports), as long as the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications. This study data can be requested by any qualified researchers who engage in rigorous, independent scientific research and will be provided following review and approval of a research proposal and statistical analysis plan and execution of a data sharing agreement. Data requests can be submitted at any time and the data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvie.com/our-science/clinical-trials/clinical-trials-data-and-information-sharing/data-and-information-sharing-with-qualified-researchers.html.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants. The Advarra Institutional Review Board (Columbia, MD, USA) reviewed the cross-sectional survey for participants in the USA (exempt determination #Pro00029982, 26 September 2018) and exempted this study. Informed consent was not obtained due to the exempt nature of this survey; however, participants did consent to participate in a survey and email invitations were provided to people who opted to receive communications.
References
- 1.Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med 2020;382:1244–56. 10.1056/NEJMra1810764 [DOI] [PubMed] [Google Scholar]
- 2.Kennedy S, Bergqvist A, Chapron C, et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod 2005;20:2698–704. 10.1093/humrep/dei135 [DOI] [PubMed] [Google Scholar]
- 3.Practice bulletin no. 114: management of endometriosis. Obstet Gynecol 2010;116:223–36. 10.1097/AOG.0b013e3181e8b073 [DOI] [PubMed] [Google Scholar]
- 4.Zondervan KT, Becker CM, Koga K, et al. Endometriosis. Nat Rev Dis Primers 2018;4:9. 10.1038/s41572-018-0008-5 [DOI] [PubMed] [Google Scholar]
- 5.De Graaff AA, D'Hooghe TM, Dunselman GAJ, et al. The significant effect of endometriosis on physical, mental and social wellbeing: results from an international cross-sectional survey. Hum Reprod 2013;28:2677–85. 10.1093/humrep/det284 [DOI] [PubMed] [Google Scholar]
- 6.Gallagher JS, DiVasta AD, Vitonis AF, et al. The impact of endometriosis on quality of life in adolescents. J Adolesc Health 2018;63:766–72. 10.1016/j.jadohealth.2018.06.027 [DOI] [PubMed] [Google Scholar]
- 7.Laganà AS, La Rosa VL, Rapisarda AMC, et al. Anxiety and depression in patients with endometriosis: impact and management challenges. Int J Womens Health 2017;9:323–30. 10.2147/IJWH.S119729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vannuccini S, Lazzeri L, Orlandini C, et al. Mental health, pain symptoms and systemic comorbidities in women with endometriosis: a cross-sectional study. J Psychosom Obstet Gynaecol 2018;39:315–20. 10.1080/0167482X.2017.1386171 [DOI] [PubMed] [Google Scholar]
- 9.Culley L, Law C, Hudson N, et al. A qualitative study of the impact of endometriosis on male partners. Hum Reprod 2017;32:1667–73. 10.1093/humrep/dex221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Denny E, Mann CH. Endometriosis-associated dyspareunia: the impact on women’s lives. J Fam Plann Reprod Health Care 2007;33:189–93. 10.1783/147118907781004831 [DOI] [PubMed] [Google Scholar]
- 11.Fagervold B, Jenssen M, Hummelshoj L, et al. Life after a diagnosis with endometriosis - a 15 years follow-up study. Acta Obstet Gynecol Scand 2009;88:914–9. 10.1080/00016340903108308 [DOI] [PubMed] [Google Scholar]
- 12.Soliman AM, Coyne KS, Gries KS, et al. The effect of endometriosis symptoms on absenteeism and presenteeism in the workplace and at home. J Manag Care Spec Pharm 2017;23:745–54. 10.18553/jmcp.2017.23.7.745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leonardi M, Horne AW, Armour M, et al. Endometriosis and the coronavirus (covid-19) pandemic: clinical advice and future considerations. Front Reprod Health 2020;2. 10.3389/frph.2020.00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leonardi M, Horne AW, Vincent K. Self-management strategies to consider to combat endometriosis symptoms during the covid-19 pandemic. Hum Reprod Open 2020;2020:hoaa028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klein S, D’Hooghe T, Meuleman C, et al. What is the societal burden of endometriosis-associated symptoms? A prospective Belgian study. Reprod Biomed Online 2014;28:116–24. 10.1016/j.rbmo.2013.09.020 [DOI] [PubMed] [Google Scholar]
- 16.Simoens S, Dunselman G, Dirksen C, et al. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod 2012;27:1292–9. 10.1093/humrep/des073 [DOI] [PubMed] [Google Scholar]
- 17.Soliman AM, Taylor H, Bonafede M, et al. Incremental direct and indirect cost burden attributed to endometriosis surgeries in the United States. Fertil Steril 2017;107:1181–90. 10.1016/j.fertnstert.2017.03.020 [DOI] [PubMed] [Google Scholar]
- 18.Soliman AM, Yang H, Du EX, et al. The direct and indirect costs associated with endometriosis: a systematic literature review. Hum Reprod 2016;31:712–22. 10.1093/humrep/dev335 [DOI] [PubMed] [Google Scholar]
- 19.Bhatti ZU, Salek MS, Finlay AY. Chronic diseases influence major life changing decisions: a new domain in quality of life research. J R Soc Med 2011;104:241–50. 10.1258/jrsm.2011.110010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kimball AB, Gieler U, Linder D, et al. Psoriasis: is the impairment to a patient’s life cumulative? J Eur Acad Dermatol Venereol 2010;24:989–1004. 10.1111/j.1468-3083.2010.03705.x [DOI] [PubMed] [Google Scholar]
- 21.Huntington A, Gilmour JA. A life shaped by pain: women and endometriosis. J Clin Nurs 2005;14:1124–32. 10.1111/j.1365-2702.2005.01231.x [DOI] [PubMed] [Google Scholar]
- 22.Moradi M, Parker M, Sneddon A, et al. Impact of endometriosis on women’s lives: a qualitative study. BMC Womens Health 2014;14:123. 10.1186/1472-6874-14-123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cole JM, Grogan S, Turley E. “The most lonely condition I can imagine”: psychosocial impacts of endometriosis on women’s identity. Fem Psychol 2021;31:171–91. 10.1177/0959353520930602 [DOI] [Google Scholar]
- 24.Apers S, Dancet EAF, Aarts JWM, et al. The association between experiences with patient-centred care and health-related quality of life in women with endometriosis. Reprod Biomed Online 2018;36:197–205. 10.1016/j.rbmo.2017.10.106 [DOI] [PubMed] [Google Scholar]
- 25.Witzeman K, Antunez Flores O, Renzelli-Cain RI, et al. Patient-physician interactions regarding dyspareunia with endometriosis: online survey results. J Pain Res 2020;13:1579–89. 10.2147/JPR.S248887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bourdel N, Alves J, Pickering G, et al. Systematic review of endometriosis pain assessment: how to choose a scale? Hum Reprod Update 2015;21:136–52. 10.1093/humupd/dmu046 [DOI] [PubMed] [Google Scholar]
- 27.Chawla S. Treatment of endometriosis and chronic pelvic pain with letrozole and norethindrone acetate. Med J Armed Forces India 2010;66:213–5. 10.1016/S0377-1237(10)80039-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Facchin F, Barbara G, Saita E, et al. Impact of endometriosis on quality of life and mental health: pelvic pain makes the difference. J Psychosom Obstet Gynaecol 2015;36:135–41. 10.3109/0167482X.2015.1074173 [DOI] [PubMed] [Google Scholar]
- 29.Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertil Steril 2006;86:1296–301. 10.1016/j.fertnstert.2006.04.054 [DOI] [PubMed] [Google Scholar]
- 30.Bernuit D, Ebert AD, Halis G, et al. Female perspectives on endometriosis: Findings from the uterine bleeding and pain women’s research study. J Endomet 2011;3:73–85. 10.5301/JE.2011.8525 [DOI] [Google Scholar]
- 31.Greene R, Stratton P, Cleary SD, et al. Diagnostic experience among 4,334 women reporting surgically diagnosed endometriosis. Fertil Steril 2009;91:32–9. 10.1016/j.fertnstert.2007.11.020 [DOI] [PubMed] [Google Scholar]
- 32.Hadfield R, Mardon H, Barlow D, et al. Delay in the diagnosis of endometriosis: a survey of women from the USA and the UK. Hum Reprod 1996;11:878–80. 10.1093/oxfordjournals.humrep.a019270 [DOI] [PubMed] [Google Scholar]
- 33.Hudelist G, Fritzer N, Thomas A, et al. Diagnostic delay for endometriosis in Austria and Germany: causes and possible consequences. Hum Reprod 2012;27:3412–6. 10.1093/humrep/des316 [DOI] [PubMed] [Google Scholar]
- 34.Nnoaham KE, Hummelshoj L, Webster P, et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril 2011;96:366–73. 10.1016/j.fertnstert.2011.05.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Soliman AM, Fuldeore M, Snabes MC. Factors associated with time to endometriosis diagnosis in the United States. J Womens Health 2017;26:788–97. 10.1089/jwh.2016.6003 [DOI] [PubMed] [Google Scholar]
- 36.Staal AHJ, van der Zanden M, Nap AW. Diagnostic delay of endometriosis in the Netherlands. Gynecol Obstet Invest 2016;81:321–4. 10.1159/000441911 [DOI] [PubMed] [Google Scholar]
- 37.Nnoaham KE, Hummelshoj L, Kennedy SH, et al. Developing symptom-based predictive models of endometriosis as a clinical screening tool: results from a multicenter study. Fertil Steril 2012;98:692–701. 10.1016/j.fertnstert.2012.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brosens I, Puttemans P, Campo R, et al. Non-invasive methods of diagnosis of endometriosis. Curr Opin Obstet Gynecol 2003;15:519–22. 10.1097/00001703-200312000-00011 [DOI] [PubMed] [Google Scholar]
- 39.Lamvu G, Antunez-Flores O, Orady M. Path to diagnosis and women’s perspectives on the impact of endometriosis pain. J Endomet Pelvic Pain Disord 2020;2284026520903214. [Google Scholar]
- 40.Gilmour JA, Huntington A, Wilson HV. The impact of endometriosis on work and social participation. Int J Nurs Pract 2008;14:443–8. 10.1111/j.1440-172X.2008.00718.x [DOI] [PubMed] [Google Scholar]
- 41.Murray CB, Groenewald CB, de la Vega R, et al. Long-term impact of adolescent chronic pain on young adult educational, vocational, and social outcomes. Pain 2020;161:439–45. 10.1097/j.pain.0000000000001732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kashikar-Zuck S, Lynch AM, Graham TB, et al. Social functioning and peer relationships of adolescents with juvenile fibromyalgia syndrome. Arthritis Rheum 2007;57:474–80. 10.1002/art.22615 [DOI] [PubMed] [Google Scholar]
- 43.de Graaf R, Tuithof M, van Dorsselaer S, et al. Comparing the effects on work performance of mental and physical disorders. Soc Psychiatry Psychiatr Epidemiol 2012;47:1873–83. 10.1007/s00127-012-0496-7 [DOI] [PubMed] [Google Scholar]
- 44.Smorgick N, Marsh CA, As-Sanie S, et al. Prevalence of pain syndromes, mood conditions, and asthma in adolescents and young women with endometriosis. J Pediatr Adolesc Gynecol 2013;26:171–5. 10.1016/j.jpag.2012.12.006 [DOI] [PubMed] [Google Scholar]
- 45.Yosef A, Allaire C, Williams C, et al. Multifactorial contributors to the severity of chronic pelvic pain in women. Am J Obstet Gynecol 2016;215:760.e1–4. 10.1016/j.ajog.2016.07.023 [DOI] [PubMed] [Google Scholar]
- 46.Evans SF, Brooks TA, Esterman AJ, et al. The comorbidities of dysmenorrhea: a clinical survey comparing symptom profile in women with and without endometriosis. J Pain Res 2018;11:3181–94. 10.2147/JPR.S179409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fourquet J, Báez L, Figueroa M, et al. Quantification of the impact of endometriosis symptoms on health-related quality of life and work productivity. Fertil Steril 2011;96:107–12. 10.1016/j.fertnstert.2011.04.095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sperschneider ML, Hengartner MP, Kohl-Schwartz A, et al. Does endometriosis affect professional life? A matched case-control study in Switzerland, Germany and Austria. BMJ Open 2019;9:e019570. 10.1136/bmjopen-2017-019570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Prescott J, Farland LV, Tobias DK, et al. A prospective cohort study of endometriosis and subsequent risk of infertility. Hum Reprod 2016;31:1475–82. 10.1093/humrep/dew085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Geisser ME, Cano A, Leonard MT. Factors associated with marital satisfaction and mood among spouses of persons with chronic back pain. J Pain 2005;6:518–25. 10.1016/j.jpain.2005.03.004 [DOI] [PubMed] [Google Scholar]
- 51.Leonard MT, Cano A. Pain affects spouses too: personal experience with pain and catastrophizing as correlates of spouse distress. Pain 2006;126:139–46. 10.1016/j.pain.2006.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fourquet J, Gao X, Zavala D, et al. Patients' report on how endometriosis affects health, work, and daily life. Fertil Steril 2010;93:2424–8. 10.1016/j.fertnstert.2009.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maleki N, Tahaney K, Thompson BL, et al. At the intersection of alcohol use disorder and chronic pain. Neuropsychology 2019;33:795–807. 10.1037/neu0000558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Groenewald CB, Law EF, Fisher E, et al. Associations between adolescent chronic pain and prescription opioid misuse in adulthood. J Pain 2019;20:28–37. 10.1016/j.jpain.2018.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lazzeri L, Orlandini C, Vannuccini S, et al. Endometriosis and perceived stress: impact of surgical and medical treatment. Gynecol Obstet Invest 2015;79:229–33. 10.1159/000368776 [DOI] [PubMed] [Google Scholar]
- 56.Oehmke F, Weyand J, Hackethal A, et al. Impact of endometriosis on quality of life: a pilot study. Gynecol Endocrinol 2009;25:722–5. 10.3109/09513590903159607 [DOI] [PubMed] [Google Scholar]
- 57.Ugwumadu L, Chakrabarti R, Williams-Brown E, et al. The role of the multidisciplinary team in the management of deep infiltrating endometriosis. Gynecol Surg 2017;14:15. 10.1186/s10397-017-1018-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aarts JWM, Huppelschoten AG, van Empel IWH, et al. How patient-centred care relates to patients' quality of life and distress: a study in 427 women experiencing infertility. Hum Reprod 2012;27:488–95. 10.1093/humrep/der386 [DOI] [PubMed] [Google Scholar]
- 59.Gameiro S, Canavarro MC, Boivin J. Patient centred care in infertility health care: direct and indirect associations with wellbeing during treatment. Patient Educ Couns 2013;93:646–54. 10.1016/j.pec.2013.08.015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-052765supp001.pdf (1.7MB, pdf)
Data Availability Statement
Data are available upon reasonable request. AbbVie is committed to responsible data sharing regarding the clinical trials and studies we sponsor. This includes access to anonymised, individual and trial-level data (analysis data sets), as well as other information (eg, protocols and clinical study reports), as long as the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications. This study data can be requested by any qualified researchers who engage in rigorous, independent scientific research and will be provided following review and approval of a research proposal and statistical analysis plan and execution of a data sharing agreement. Data requests can be submitted at any time and the data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvie.com/our-science/clinical-trials/clinical-trials-data-and-information-sharing/data-and-information-sharing-with-qualified-researchers.html.