Abstract
Objective
To explore the current Chinese and English guidelines of urinary tract infection (UTI) in children and provide a summary of the recommendations of the guidelines.
Methods
An electronic search was conducted on databases, including Pubmed, SinoMed, Wangfang Data, CHKD, VIP, NICE, WHO, GIN and Medliveto retrieve data of the clinical practice guidelines on UTI from the establishment of the database to June 2020. Four assessors assessed the quality of guidelines using the Appraisal of Guidelines for Research & Evaluation II (AGREE II) and evaluated the specific recommendations in guidelines.
Results
(1) Nine guidelines including two from the USA (AAP and A guideline for the inpatient care of children with pyelonephritis) and the remaining from EAU/ESPU, SINEPE, KHA-CARI, CPS, ISPN, NICE and CMA-CSP were explored. (2) The AGREE II evaluation demonstrated higher scores of UTI guidelines in terms of ‘scope and purpose’ (72.99%±11.19%) and ‘clarity of presentation’ (75.62%±7.75%), whereas the average scores were lower in the aspect of ‘stakeholder involvement’ (35.49%±14.41%), ‘rigour of development’ (37.05%±10.05%), ‘applicability’ (37.75%±11.98%) and ‘editorial independence’ (43.06%±48.14%). The average scores of the guidelines were as follows: SINePe (72.57%), CMA-CSP (62.96%), EAU/ESPU (59.61%), AAP (56.86%), NICE (47.54%), CPS (40.93%), KHA-CARI (38.86%), ISPN (38.63%) and A guideline for the inpatient care of children with pyelonephritis (34.72%). (3) All the selected guidelines basically reached a consensus on urine sample retention methods in older children, the antibiotic treatment course and renal and bladder ultrasonography application but lacked a conclusion on the determination of urine culture results, the choice of voiding cystourethrography and Tc-99mdimercaptosuccinicacid, and antibiotic prophylaxis.
Conclusion
There remains a need to improve the quality of guidelinesfor UTI in clinical practice. Existing controversies on the current guidelines of UTI in some recommendations warrant further exploration to provide more evidence on formulating more unified and practical guidelines in the future.
Ethics and dissemination
No ethical approval is required for this research, as it did not include patients or patient data.
Keywords: Urinary tract infections, Protocols & guidelines, Clinical governance, Paediatric nephrology, EPIDEMIOLOGY, Paediatric urology
Strengths and limitations of this study.
To our knowledge, this is the first study that evaluates the quality of guideline of urinary tract infections (UTIs) in children by Appraisal of Guidelines for Research & Evaluation II (AGREE II).
Selection bias exists in this study because only guidelines published in English and Chinese were included.
AGREE Ⅱ tool does not account for the relative importance of the six domains.
AGREE II does not provide high-quality and minimum quality rating criteria.
Introduction
Urinary tract infections (UTIs) are a common clinical infectious disease, especially in infants, with approximately 7% incidence in infants with fever.1 The lack of specific clinical signs and symptoms largely contributes to missed and misdiagnosis of UTI in infants. Current evidence views UTI in childhood as an indicator of numerous renal diseases. UTI, for instance, has been revealed to be the first symptom in 30% of congenital anomalies of the kidney and urinary tract (CAKUT).2 3 Recurrent UTIs and CAKUT can certainly cause renal scars, long-term hypertension, some of which potentially progresses to chronic kidney diseases (CKD) and may have a detrimental effect on the quality of life of children. Therefore, it is imperative to practice early diagnosis, standardised treatment and prevention of relapses to reduce renal scar formation and prevent the occurrence of CKD.
The end of the 20th century has seen many countries issuing and/or updating the guidelines of UTIs in children both aimed to guide decision making among clinicians and reduce waste of resources. A consensus was made in 2007 on the diagnosis and management of UTI by the Chinese expert. However, after decades of development, the paediatric branch of the Chinese Medical Association in 2017 issued evidence-based guidelines of UTIs in children based on the latest research evidence.
In 2009, Appraisal of Guidelines for Research & Evaluation II (AGREE II) was published as a revised version of the original AGREE instrument, and the tool has presently been translated into multiple languages and is receiving wide application to assess the quality of guideline development.4
The present study explores the current UTI guidelines in children, evaluates the quality of guideline by AGREE II and compares and contrasts the selected recommendations of the guidelines aiming to provide a scientific basis for clinical diagnosis and treatment.
Methods
Inclusion and exclusion criteria
Inclusion criteria
The literature includes the diagnosis and treatment of UTI.
The type of literature is clinical guideline/consensus/norm.
The applicable object of the guidelines is limited to children.
The latest version of a set of guidelines that has been updated multiple times.
A complete guideline text, published in English or Chinese.
Exclusion criteria
Guideline interpretations or translations and traditional Chinese Medicine guidelines were excluded, as well as any documents that were not guidelines (such as reviews and other guideline quality appraisal).
Literature search strategy
The following electronic databases will be searched: PubMed, SinoMed (The Chinese biomedical literature database), China Wanfang Digital Database, VIP database, China Hospital Knowledge Database (CHKD), NICE, WHO, GIN and Medlive, from database inception time to June 2020. The search terms included: urinary tract infection, guideline, practice guidelines as the topic, guidelines, guidance, recommendation, consensus, child, preschool, infant, adolescent, newborn, pediat, youth, toddle, teen, boy, girl and baby. Search strategy is in (online supplemental material 1).
bmjopen-2021-057736supp001.pdf (106.1KB, pdf)
Literature screening and data extraction
Two reviewers (BZ and FD) independently screened the articles according to inclusion and exclusion criteria by reading through the title and abstract. A third reviewer (LY) was consulted in the event of disagreement to reach a consensus. The reviewers used Microsoft office 2019 to extract the basic information from the selected guidelines, including title, guideline developers, country, target population, the tool of evidence quality and strength, and number of references.
Quality assessment
The research group comprised four clinicians experienced in paediatric nephrology and had been trained by an expert in evidence-based medicine, and they independently evaluated guidelines. The selected guidelines were independently using the AGREE II, which comprised 23 items in six domains: ‘Scope and purpose’, ‘Stakeholder involvement’, ‘Rigour of development’, ‘Clarity of presentation’, ‘Applicability’ and ‘Editorial independence’. Each item was rated on a seven-point scale from 1 (strongly disagree) to 7 (strongly agree). A scaled domain percentage score was calculated, according to the AGREE II methodology, as follows: . Only the scores in each domain were evaluated because the user manual for AGREE II does not provide high-quality and minimum quality rating criteria.
To resolve discrepancies between the four assessors, a method was used from a previous study: intraclass correlation coefficient (ICC) was calculated to assess inter-rater reliability, ICC values greater than 0.75 demonstrated acceptable stability.5 6
Comparison of recommendations
Recommendations on the diagnosis and treatment of UTIs in children reported in the selected guidelines were extracted and presented in comparative tables focusing on possible gaps and common messages.
Data analysis
Descriptive statistics were conducted in order to characterise the recommendation content. For quantitative data and the guidelines basic information, the statistical analysis was performed using Microsoft Office 2019, and ICCs were calculated by SPSS V.22.0.
Ethics and dissemination
No ethical approval is required for this research, as it did not include patients or patient data.
Results
Guideline selection
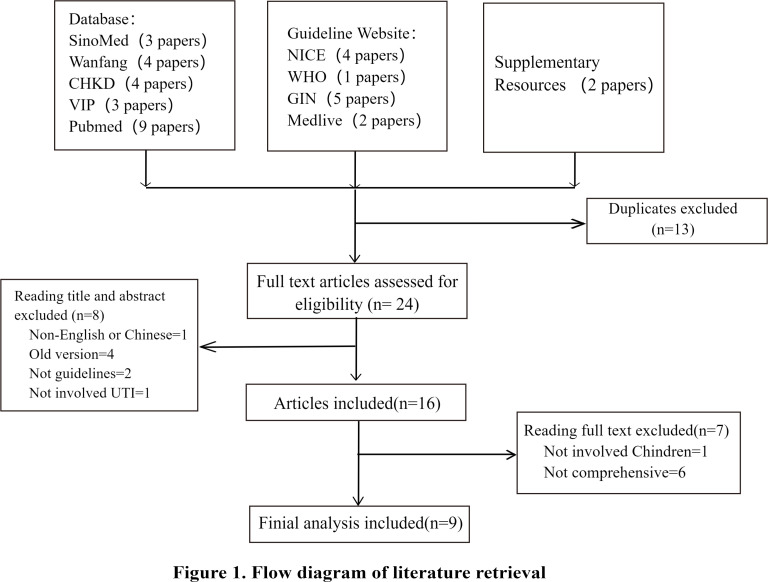
Of the 37 full texts retrieved and screened, nine articles were included in this study, including the USA7 8 (two articles), Europe9 (one article), Italy10 (one article), Australia11 (one article), Canada12 (one article), India13 (one article), UK14 (one article) and China15 (one article). The selected guidelines comprised nine medicine societies (AAP, EAU, ESPU, SINePe, KHA-CARI, CPS, ISPN, NICE, and CMA-CSP). Figure 1 (flow diagram of literature retrieval) shows the guideline screening process. Table 1 shows the basic information of the selected guidelines.
Figure 1.
Flow diagram of literature retrieval. CHKD, China Hospital Knowledge Database.
Table 1.
The basic information of the selected guidelines
| Title | Source | Organisation/author | Country | Year of publication | Target population | The criteria for selecting the evidence | Number of references |
| Reaffirmation of AAP clinical practice guideline: the diagnosis and management of the initial urinary tract infection in febrile infants and young children 2–24 months | Pediatrics | AAP | USA | 2016 | Infants and young children 2–24 months | AAP policy | 17 |
| Urinary tract infections in children: EAU/ESPU Guidelines | European Urology | EAU/ESPU | Europe | 2014 | Children | EAU guidelines criteria—modified GRADE | 118 |
| Updated Italian recommendations for the diagnosis, treatment and follow-up of the first febrile urinary tract infection in young children | Acta Paediatrica | SINePe | Italy | 2019 | Infants and young children 2–36 months | SOTR | 107 |
| KHA-CARI guideline: diagnosis and treatment of urinary tract infection in children | Asian Pacific Society of Nephrology | KHA-CARI | Australia | 2014 | Children | GRADE | 18 |
| Urinary tract infections in infants and children: diagnosis and management | Paediatrics and child health | CPS | Canada | 2014 | Infants older than 2 months | Not described | 33 |
| Revised statement on management of urinary tract infections | Indian paediatrics | ISPN | India | 2011 | Children | Not described | 26 |
| Urinary tract infection in under 16s: diagnosis and management | NICE website | NICE | UK | 2018 | Children under 16s | Not described | / |
| A guideline for the inpatient care of children with pyelonephritis | Annals of Saudi Medicine | Aftab S Chishti | USA | 2010 | Hospitalised children | Not described | 63 |
| Evidence-based guideline on diagnosis and treatment of urinary tract infection (2016) | Chinese Journal of Pediatrics | CMA-CSP | China | 2017 | Children | ESC guidelines criteria | 18 |
AAP, American Academy of Pediatrics; CMA-CSP, Chinese Medical Association, Chinese Society of Pediatrics; CPS, Canadian Pediatric Society; EAU, European Association of Urology; ESC, European Society of Cardiology; ESPU, European Society for Pediatric Urology; GRADE, Grading of Recommendations, Assessment, Development, and Evaluation; ISPN, Indian Pediatric Nephrology Group; KHA-CARI, Kidney Health Australia, Caring for Australasians with Renal Impairment; NICE, National Institute for Health and Care Excellence; SINePe, Italian Society of Pediatric Nephrology; SORT, Strength of recommendation taxonomy.
Quality assessment
The four assessors independently evaluated the selected guidelines, and the scores are in (online supplemental material 2). Inter-rater reliability of the four assessors total scores was assessed using ICC (table 2). ICC values for all the nine guidelines were greater than 0.75 (0.787~0.925), providing evidence of high consistency in the assessment results between the four assessors. Table 3 illustrate the scores of the AGREE II quality assessment.
Table 2.
Intraclass correlation coefficient (ICC)
| Guideline | ICC | 95% CI | P value |
| AAP | 0.925 | 0.865 to 0.964 | <0.001 |
| EAU/ESPU | 0.908 | 0.836 to 0.955 | <0.001 |
| SINePe | 0.913 | 0.845 to 0.958 | <0.001 |
| KHA-CARI | 0.894 | 0.814 to 0.948 | <0.001 |
| CPS | 0.890 | 0.807 to 0.946 | <0.001 |
| ISPN | 0.799 | 0.666 to 0.898 | <0.001 |
| NICE | 0.850 | 0.742 to 0.925 | <0.001 |
| Pyelonephritis guideline | 0.905 | 0.831 to 0.954 | <0.001 |
| CMA-CSP | 0.895 | 0.814 to 0.948 | <0.001 |
Table 3.
Standardised scores of each domain by AGREE II of guidelines
| Scope and purpose (%) | Stakeholder involvement (%) | Rigour of development (%) | Clarity of presentation (%) | Applicability (%) | Editorial independence (%) | Average scores (%) | |
| AAP | 69.44 | 26.39 | 36.98 | 87.50 | 25.00 | 95.83 | 56.86 |
| EAU/ESPU | 75.00 | 31.94 | 45.83 | 73.61 | 33.33 | 97.92 | 59.61 |
| SINePe | 88.89 | 55.56 | 48.96 | 84.72 | 61.46 | 95.83 | 72.57 |
| KHA-CARI | 54.17 | 25.00 | 34.90 | 84.72 | 34.38 | 0.00 | 38.86 |
| CPS | 73.61 | 26.39 | 39.58 | 70.83 | 35.42 | 0.00 | 40.97 |
| ISPN | 62.50 | 40.28 | 25.52 | 63.89 | 39.58 | 0.00 | 38.63 |
| NICE | 91.67 | 41.67 | 26.56 | 72.22 | 53.13 | 0.00 | 47.54 |
| Pyelonephritis guideline | 66.67 | 12.50 | 25.00 | 75.00 | 29.17 | 0.00 | 34.72 |
| CMA-CSP | 75.00 | 59.72 | 54.17 | 68.06 | 22.92 | 97.92 | 62.96 |
| Means±SD (%) | 72.99±11.19 | 35.49±14.41 | 37.50±10.05 | 75.62±7.75 | 37.15±11.98 | 43.06±48.14 | / |
bmjopen-2021-057736supp002.pdf (50.2KB, pdf)
Scores of the six domains
Scope and purpose: this domain yielded an average score of 72.99%±11.19%. NICE demonstrated the highest score in this domain at 91.76%, while KHA-CARI showed the lowest score at 54.17%.
Stakeholder involvement: this domain yielded an average score of 35.49%±14.41%. SINePe demonstrated the highest score in this domain at 91.76%, while the USA guideline for the inpatient care of children with pyelonephritis showed the lowest score at 12.5%.
Rigour of development: this domain yielded an average score of 37.05%±10.05%. CMA-CSP demonstrated the highest score in this domain at 54.17%.
Clarity of presentation: this domain yielded an average score of 75.62%±7.75%. AAP demonstrated the highest score in this domain at 54.17%.
Applicability: this domain yielded an average score of 37.75%±11.98%. CMA-SINePe demonstrated the highest score in this domain at 54.17%.
Editorial independence: this domain yielded an average score of 43.06%±48.14%. Four guidelines AAP, EAU/ESPU, SINePe and CMA-CSP, scored more than 90%.
Scores of the nine guidelines
The average score for selected guidelines (from high to low) were as follows: SINePe (72.57%), CMA-CSP (62.96%), EAU/ESPU (59.61%), AAP (56.86%), NICE (47.54%), CPS (40.93%), KHA-CARI (38.86%), ISPN (38.63%) and the guideline for the inpatient care of children with pyelonephritis (34.72%).
Summary of recommendations
Similarities
A clean voided midstream urine sample is the preferred method for UTI diagnosis for toilet-trained children.
The choice of antibiotic should be based on resistance patterns of urinary pathogens, and the course of treatment of antibiotics is generally 3–4 days for lower urinary tract infection and 7–14 days for upper UTI.
Renal and bladder ultrasonography (RBUS) is recommended for all children with febrile UTI (except NICE), but voiding cystourethrography (VCUG) and Tc-99mdimercaptosuccinicacid (DMSA) are not regarded as routine examinations.
Antibiotic prophylaxis is not routinely recommended after the first febrile UTI, excepting high-grade VUR.
Differences
Urine collection method for non-toilet-trained children: AAP, EAU/ESPU, ISPN and the guideline for pyelonephritis in the USA are more inclined to bladder catheterisation (BC) and suprapubic aspiration (SPA); other guidelines (except CMA-CSP) recommend urinary bag or clean voided urine (CVU).
The guidelines (except NICE) recommend that the positive urinalysis be dependent on the urine collection method. Table 4 illustrates the specific results.
The recommendations for imaging evaluation slightly differ. Generally, the guidelines of AAP, EAU/ESPU, KHA-CARI, SINePe and CPS do not recommend for the sequence of VCUG and DMSA, while ISPN, NICE, CMA-CSP and the guideline for pyelonephritis in the USA tend to prioritise DMSA examination and give different opinions based on the age of the children. Table 4 illustrates the specific results.
There is no consistent regulation on the dose and course of antibiotic prophylaxis (EAU/ESPU, SINePe, KHA-CARI, CPS, ISPN and CMA-CSP), in particular, AAP and NICE failed to address this aspect. Table 4 illustrates the specific results.
Table 4.
Summary of recommendations
| Criteria positive of urine culture | Antibiotic prophylaxis | Imaging | ||||
| Age | RBUS | VCUG | DMSA | |||
| AAP | BC/SPA: ≥5×104 CFU/mL | / | 2–24 months | All of febrile infants | Abnormal RBUS or other specific circumstances | / |
| EAU/ESPU | SPA: any; BC: ≥103–5×104 CFU/mL; CVU: ≥104 CFU/mL with symptoms or ≥105 CFU/mL without symptoms |
VUR III-V | / | All of febrile children | In febrile UTI children: <1 year, >1 year girl, >1 year boy with recurrent febrile UTI and toilet-trained children who were suspected of VUR | |
| SINePe | SPA: >104 CFU/mL BC: >104 CFU/mL CVU: >5×104 CFU/mL Urinary bag: >105 CFU/mL |
VUR Ⅳ–Ⅴ, recurrent febrile UTI; dose: one‐quarter to one‐third of the treatment dose; course: 12–24 months in girls and 6–12 months in boys. |
2–36 months | All of febrile children* | Abnormal RBUS or other high-risk factors† | VUR IV–V |
| KHA-CARI | SPA: any; BC: >105 CFU/mL; CVU: >105 CFU/mL |
A severe index UTI, recurrent UTI, VUR III–V; course: 6–24 months low dose |
/ | First UTI, not had antenatal ultrasound, had some special cases‡ | Abnormal RBUS; recurrent pyelonephritis | Renal functional decline |
| CPS | CVU: ≥5×105 CFU/mL BC: ≥5×104 CFU/mL SPA: any |
VUR Ⅳ-Ⅴ | <2 years | All of febrile infants | Abnormal RBUS; recurrent UTI in children <2 years | Only when the diagnosis of UTI is in doubt |
| >2 years | / | |||||
| ISPN§ | SPA: any; BC: >5×104 CFU/mL CVU: >105 CFU/mL |
All grades of VUR, recurrent UTI; Low dose; Course: VUR Ⅰ-Ⅱ until 1y old, VUR Ⅲ-Ⅴ up to 5y; |
<1 years | All UTI children | First UTI in children | First UTI in children |
| 1–5 years | Abnormal RBUS or DMSA | First UTI in children | ||||
| >5 years | Abnormal RBUS | Abnormal RBUS | ||||
| NICE | / | / | <6 months | All children¶ | Atypical/recurrent UTI | Atypical/recurrent UTI |
| 6 months–3 years | Atypical/recurrent UTI | Not recommend | Atypical/recurrent UTI | |||
| >3 years | Atypical/recurrent UTI | Not recommend | Recurrent UTI | |||
| Pyelonephritis guideline** | CVU: >104 CFU/mL in boys and >105 CFU/mL in girls; BC: >104 CFU/mL |
Not recommend | All | Boys | Abnormal DMSA | Boys |
| <3 years | Girls | Girls | ||||
| 3–7 years | Girls with fever >38.5℃ | Girls with fever >38.5℃ | ||||
| >7 years | Girls do not take any imaging examination | |||||
| CMA-CSP†† | SPA: any G-bacteria, G+bacteria >103 CFU/mL; BC: >105 CFU/mL; CVU: >104 CFU/mL in boys, and three times >105 CFU/mL in girls |
Dilated VUR, recurrent UTI; dose: one‐third of treatment dose |
≤2 years | First febrile UTI | Abnormal RBUS or DMSA; atypical UTI; recurrent UTI | First febrile UTI |
| >2 years | When RBUS is abnormal, performed as a programme of ≤2 years | |||||
*Not recommend RBUS during the febrile UTI, unless it is complicated, atypical or severe (presence of any of the following: septic state, fever persisting after 3 days of appropriate antibiotic treatment, elevated plasma creatinine, oliguria).
†First-degree relative with VUR, septicaemia, chronic kidney disease, age <6 months in a male infant, likely non-compliance of the family, abnormal bladder emptying, no clinical response to correct antibiotic treatment within 72 hours, bacteria other than Escherichia coli.
‡Special cases: bacteraemia,<3 months of age, atypical organisms (eg, Staphylococcus aureus or Pseudomonas), no clinical response to correct antibiotic treatment within 48 hours, renal impairment or significant electrolyte derangement, abdominal mass, poor urinary stream.
§Imaging evaluation of the first UTI.
¶For infants younger than 6 months with a first-time UTI that responds to treatment, ultrasound should be carried out within 6 weeks of the UTI.
**Imaging evaluation of the first pyelonephritis.
††Imaging evaluation of the first febrile UTI.
BC, bladder catheterisation; CVU, clean voided urine; RBUS, renal and bladder ultrasonography; SPA, suprapubic aspiration; UTI, urinary tract infection.
Discussion
Quality appraisal of the guidelines for UTIs in children with AGREE II
Nine guidelines have been analysed in this study. The quality appraisal with AGREE II demonstrated that four guidelines (SINePe, CMA-CSP, EAU/ESPU and AAP) exhibited scores greater than 50%. Among the six fields of the AGREE II tool, the scores of domain 1 ‘scope and purpose’ and domain 4 ‘clarity of presentation’ were >70%, while the scores of the other four fields were lower than 50%.
Of note, the rigour of development better reflected the quality of the guidelines. We reported low scores of guidelines in domain 3 (rigour of development), which is consistent with the previous findings by Chen et al.16 In the present study, the Chinese guideline exhibited the highest score in domain 3, particularly because it describes the evidence selection criteria and the search methods for the evidence. Moreover, EAU/ESPU, SINePe and KHA-CARI describe the evidence selection criteria and the methods for formulating the recommendations. There is a previous suggestion that guidelines be updated every 3–5 years.17 The publishing period in the present study is between 2010 and 2019, and five guidelines (ISPN, CPS, KHA-CARI, EAU/ESPU and the guideline for the inpatient care of children with pyelonephritis) had not been updated for more than 5 years.
SINePe demonstrated the highest applicability score because it considered the obstacles in the application of recommendations. For example, this guideline does not recommend a new imaging technique—contrast-enhanced voiding urosonography (ceVUS)—because it is time consuming, expensive and not available on a large scale, despite its high specificity, sensitivity and safety in VUR diagnosis. Other guidelines demonstrated low scores in domain 5 because they omit facilitators, barriers and potential resource implications of its application. These data strongly recommend the need to develop new guidelines, involving health economists, who can fully consider the cost-effectiveness of recommendations, to improve the applicability of the guidelines.
The development of many guidelines is funded by bodies, such as governments, professional associations and pharmaceutical companies. There should be an explicit statement that these bodies have not influenced the recommendations. In the present study, AAP, EAU/ESPU, SINePe and CMA-CSP guidelines provided statements regarding the source of funding and competing interests. Other guidelines did not provide such statements. In future, its importance for guideline developers to clarify their editorial independence to improve credibility of guidelines.
Comparison of recommendations in the selected guidelines
The selected guidelines reached a consensus in urine collection methods for toilet-trained children, RBUS application and treatment courses. However, there is no consensus on the standard of positive urine culture results, the choice of VUCG and DMSA and antibiotic prophylaxis.
Moreover, the criteria for determining the positive or negative results of urine culture varied across urine collection methods. Previously in 2016, a study reported 80% bacterial counts in children with UTI greater than 50 000 CFU/mL18; notably, AAP adopted this criterion. However, because low colony counts can be indicative of a UTI in some circumstances, EAU/ESPU outlines 1000–50000 CFU/mL as the criteria of BC. Swerkersson et al’s study reported similar results whereby 19% bacterial counts lower than 104 CFU/mL were found in the first diagnosis of UTI infants by SPA,19 which is in agreement with CPS.
Regarding the choice for imaging, no uniform opinions have been relayed on the order of VCUG and DMSA. Currently, two approaches, the ‘top-down’ method (DMSA scan and, if positive, VCUG) and the ‘down-top’ method (VCUG and, if positive, DMSA scan), have been described. Our analysis revealed that NICE, CMA-CSP, ISPN and the guideline for pyelonephritis in the USA tend to emulate the ‘top-down’ method, which can allow for early kidney damage assessment. Previous evidence indicates that UTI and renal scarring can occur in patients without VUR, and many renal scars are associated with the fetal period, therefore, may present renal dysplasia.20 In addition, DMSA demonstrates an upstanding predictive ability for high-grade VUR (99% sensitivity), which is why the ‘top-down’ method not only can decrease patient discomfort caused by invasive examinations but also save medical costs.21 Contrarily, the VUR-based ‘down-top’ method is strongly associated with renal scar formation and UTI recurrence. As such, early diagnosis and treatment of VUR are imperative in preventing further kidney damage. It is of particular note that the guideline of the American College of Radiology in 2017 recommends this method but does not recommend DMSA regardless of children’s age.22 Overall, in clinical practice, whether to apply the ‘top-down’ or ‘down-top’ approach should decide based on actual situation of patients.
SINePe guideline outlined a new imaging technique—ceVUS—that shows the ureter and bladder in real-time using ultrasound contrast agents. Compared with VCUG, it has the advantages of real-time imaging, radiation free and favourable safety profile. Mounting evidence shows that ceVUS is highly sensitive (80%–100%) and accurate (77%–86%) in the diagnosis of VUR, and the diagnosis agreement between VCUG and ceVUS is greater than 70%.23–27 EFSUMB (European Federation of Societies for Ultrasound in Medicine and Biology) guideline and Chinese expert consensus about VUR recommend the application of ceVUS in the following situations: (1) first examination for VUR in girls; (2) follow-up examinations for VUR in girls and boys after conservative or surgical therapy; and (3) screening high-risk patients for reflux.28 29 In this view, ceVUS holds promise as a preferred choice for VUR screening in the future.
For antibiotic prophylaxis, most selected guidelines (except NICE and AAP) recommend its application for high-grade VUR, but no consensus has been made on the regulation of the dose and course. SINePe suggests one-quarter to one-third of the treatment dose and duration of prophylaxis is 12‐24 months in girls and 6‐12 months in boys; however, ISPN has a different view that antibiotic prophylaxis can be until 1 year old for VUR Ⅰ–Ⅱ and 5 years old for VUR Ⅲ–Ⅳ. Meanwhile, we cannot ignore some dissents of benefit and risk assessment of antibiotic prophylaxis. Some researchers revealed that long-term antibiotic prophylaxis plays no or insignificant role in preventing UTI recurrence but increases the risk of resistant strains significantly.30 31 These data suggest the need to discuss and tailor the decision to use antibiotic prophylaxis in an individualised fashion.
Study limitations
First, selection bias exists in this study because only guidelines published in English and Chinese were included. Second, we may have missed some guidelines because of the limitation of the search strategy. Third, AGREE Ⅱ tool has some limitations, for example, it does not account for the relative importance of the six domains, domain 3 (rigour of development) is considered of equal importance to other domains. There is a need to carefully consider the recommendations if the scores for domain 3 are low.
In conclusion, although the current guidelines of UTI in children can be adopted in clinical practice, their qualities are uneven. As such, there is a whole lot of room for improvement, especially in the areas of the rigour of development, applicability, editorial independence and stakeholder involvement. Additionally, the existing controversial opinions warrants continued exploration to provide powerful evidence.
Supplementary Material
Footnotes
Contributors: HW is the guarantor for the article. BZ, YL and HW conceptualised and designed the study, carried out the initial analysis and drafted the initial manuscript. BZ, FD, LM and YL used Appraisal of Guidelines for Research & Evaluation II (AGREE II) instrument to evaluate the retrieved guidelines. YL trained four reviews on the use of AGREE II instrument. All authors approved the fnal manuscript as submitted and agree to be accountable for all aspects of the work.
Funding: Funding this study is supported by Beijing Municipal Science & Technology Commission (No. Z191100006619062) and Special Foundation for National Science and Technology Basic Research Program of China (2019FY101200).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Shaikh N, Morone NE, Bost JE, et al. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J 2008;27:302–8. 10.1097/INF.0b013e31815e4122 [DOI] [PubMed] [Google Scholar]
- 2.Arshad M, Seed PC. Urinary tract infections in the infant. Clin Perinatol 2015;42:17–28. 10.1016/j.clp.2014.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sastre JBL, Aparicio AR, Cotallo GDC, et al. Urinary tract infection in the newborn: clinical and radio imaging studies. Pediatr Nephrol 2007;22:1735–41. 10.1007/s00467-007-0556-5 [DOI] [PubMed] [Google Scholar]
- 4.AGREE Collaboration . Development and validation of an international appraisal instrument for assessing the quality of clinical practice guidelines: the agree project. Qual Saf Health Care 2003;12:18–23. 10.1136/qhc.12.1.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiaofan C, Li Youping CZ, et al. Quality assessment of global guidelines on diet intervention for hypertension. Chin J Evid-based Med 2015;15:36–46. [Google Scholar]
- 6.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979;86:420–8. 10.1037/0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- 7.SUBCOMMITTEE ON URINARY TRACT INFECTION . Reaffirmation of AAP clinical practice guideline: the diagnosis and management of the initial urinary tract infection in febrile infants and young children 2-24 months of age. Pediatrics 2016;138:e20163026. 10.1542/peds.2016-3026 [DOI] [PubMed] [Google Scholar]
- 8.Chishti AS, Maul EC, Nazario RJ, et al. A guideline for the inpatient care of children with pyelonephritis. Ann Saudi Med 2010;30:341–9. 10.4103/0256-4947.68549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein R, Dogan HS, Hoebeke P, et al. Urinary tract infections in children: EAU/ESPU guidelines. Eur Urol 2015;67:546–58. 10.1016/j.eururo.2014.11.007 [DOI] [PubMed] [Google Scholar]
- 10.Ammenti A, Alberici I, Brugnara M, et al. Updated Italian recommendations for the diagnosis, treatment and follow-up of the first febrile urinary tract infection in young children. Acta Paediatr 2020;109:236–47. 10.1111/apa.14988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McTaggart S, Danchin M, Ditchfield M, et al. KHA-CARI guideline: diagnosis and treatment of urinary tract infection in children. Nephrology 2015;20:55–60. 10.1111/nep.12349 [DOI] [PubMed] [Google Scholar]
- 12.Robinson JL, Finlay JC, Lang ME, et al. Urinary tract infections in infants and children: diagnosis and management. Paediatr Child Health 2014;19:315–9. 10.1093/pch/19.6.315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Indian Society of Pediatric Nephrology, Vijayakumar M, Kanitkar M, et al. Revised statement on management of urinary tract infections. Indian Pediatr 2011;48:709–17. [PubMed] [Google Scholar]
- 14.National Institute for Health and Care Excellence (UK) . Urinary tract infection in under 16S: diagnosis and management. London, 2018. [PubMed] [Google Scholar]
- 15.Subspecialty Group of Renal Diseases, the Society of Pediatrics, Chinese Medical Association . [Evidence-based guideline on diagnosis and treatment of urinary tract infection 2016]. Zhonghua Er Ke Za Zhi 2017;55:898–901. 10.3760/cma.j.issn.0578-1310.2017.12.005 [DOI] [PubMed] [Google Scholar]
- 16.Chen H, YH H, ZY L. Analysis of current situation of the quality of clinical practice guidelines for children with urinary tract infections based on agree II. Lin Chuang Er Ke Za Zhi 2016;34:50–4. [Google Scholar]
- 17.Shekelle PG, Ortiz E, Rhodes S, et al. Validity of the agency for healthcare research and quality clinical practice guidelines: how quickly do guidelines become outdated? JAMA 2001;286:1461–7. 10.1001/jama.286.12.1461 [DOI] [PubMed] [Google Scholar]
- 18.Tullus K. Low urinary bacterial counts: do they count? Pediatr Nephrol 2016;31:171–4. 10.1007/s00467-015-3227-y [DOI] [PubMed] [Google Scholar]
- 19.Swerkersson S, Jodal U, Åhrén C, et al. Urinary tract infection in infants: the significance of low bacterial count. Pediatr Nephrol 2016;31:239–45. 10.1007/s00467-015-3199-y [DOI] [PubMed] [Google Scholar]
- 20.Wennerström M, Hansson S, Jodal U, et al. Primary and acquired renal scarring in boys and girls with urinary tract infection. J Pediatr 2000;136:30–4. 10.1016/S0022-3476(00)90045-3 [DOI] [PubMed] [Google Scholar]
- 21.Zhang X, Xu H, Zhao R-fang. [Efficacy of acute (99m)Tc-dimercaptosuccinic acid scan in predicting vesicoureteral reflux among young children with febrile urinary tract infection]. Zhonghua Er Ke Za Zhi 2010;48:334–7. [PubMed] [Google Scholar]
- 22.Expert Panel on Pediatric Imaging:, Karmazyn BK, Alazraki AL, et al. ACR Appropriateness Criteria® Urinary Tract Infection-Child. J Am Coll Radiol 2017;14:S362–71. 10.1016/j.jacr.2017.02.028 [DOI] [PubMed] [Google Scholar]
- 23.Wong LS, Tse KS, Fan TW, et al. Voiding urosonography with second-generation ultrasound contrast versus micturating cystourethrography in the diagnosis of vesicoureteric reflux. Eur J Pediatr 2014;173:1095–101. 10.1007/s00431-014-2297-3 [DOI] [PubMed] [Google Scholar]
- 24.Ključevšek D, Battelino N, Tomažič M, et al. A comparison of echo-enhanced voiding urosonography with X-ray voiding cystourethrography in the first year of life. Acta Paediatr 2012;101:e235–9. 10.1111/j.1651-2227.2011.02588.x [DOI] [PubMed] [Google Scholar]
- 25.Kis E, Nyitrai A, Várkonyi I, et al. Voiding urosonography with second-generation contrast agent versus voiding cystourethrography. Pediatr Nephrol 2010;25:2289–93. 10.1007/s00467-010-1618-7 [DOI] [PubMed] [Google Scholar]
- 26.Papadopoulou F, Anthopoulou A, Siomou E, et al. Harmonic voiding urosonography with a second-generation contrast agent for the diagnosis of vesicoureteral reflux. Pediatr Radiol 2009;39:239–44. 10.1007/s00247-008-1080-x [DOI] [PubMed] [Google Scholar]
- 27.Riccabona M, Avni FE, Damasio MB, et al. ESPR Uroradiology Task Force and ESUR Paediatric Working Group--Imaging recommendations in paediatric uroradiology, part V: childhood cystic kidney disease, childhood renal transplantation and contrast-enhanced ultrasonography in children. Pediatr Radiol 2012;42:1275–83. 10.1007/s00247-012-2436-9 [DOI] [PubMed] [Google Scholar]
- 28.Sidhu PS, Cantisani V, Deganello A, et al. Role of contrast-enhanced ultrasound (CEUS) in paediatric practice: an EFSUMB position statement. Ultraschall Med 2017;38:33–43. 10.1055/s-0042-110394 [DOI] [PubMed] [Google Scholar]
- 29.Pediatric Urology Group, Branch of Pediatric Surgery, Chinese Medical Association . Expert consensus on management of primary vesicoureteral reflux in children. J Clin Ped Sur 2019;18:811–6. [Google Scholar]
- 30.Wang H-HS, Gbadegesin RA, Foreman JW, et al. Efficacy of antibiotic prophylaxis in children with vesicoureteral reflux: systematic review and meta-analysis. J Urol 2015;193:963–9. 10.1016/j.juro.2014.08.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Selekman RE, Shapiro DJ, Boscardin J, et al. Uropathogen resistance and antibiotic prophylaxis: a meta-analysis. Pediatrics 2018;142. 10.1542/peds.2018-0119 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-057736supp001.pdf (106.1KB, pdf)
bmjopen-2021-057736supp002.pdf (50.2KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.