Abstract
Post-traumatic hepatic biloma is a rare complication of closed trauma of the abdomen. Generally, biloma occurs spontaneously or secondary to traumatic or iatrogenic injury to the biliary system. It can lead to significant morbidity and mortality if not diagnosed promptly and properly managed. A 4-year-old child was admitted to the emergency room with abdominal pain following a traffic accident. Clinical examinations suspected closed abdominal trauma without biological signs of icteric cholestasis. Abdominal CT scan performed within 24 hours showed a focus of hepatic laceration, and follow-up imaging at 5 days showed post-traumatic intrahepatic cystic formations. This case report aims to emphasize the importance of imaging including ultrasound, CT, MRI, MRI cholangiopancreatography (MRCP), or hepatobiliary cholescintigraphy to establish the diagnosis and guide the therapeutic gestures.
Keywords: Biloma, Liver, Post-traumatic, MRI, CT, Ultrasound
Introduction
Post-traumatic biloma is a rare pathology, which can be defined as an abnormal, well-circumscribed, extra-biliary collection of bile [1]. Bilomas are usually secondary to an iatrogenic or traumatic rupture of the biliary tree resulting in a bile leak.
Morbidity and mortality are high in cases of superinfection, continuous bile leakage, or compression on surrounding structures [2]. Three to 5% of hepatic contusions in children following closed abdominal trauma are complicated by biloma, hemobilia, arteriovenous fistula, hepatic abscess, pseudoaneurysm, or secondary hemorrhage [3].
Revealed by unspecific signs and almost normal biological tests, the clinical diagnosis of bilomas is complicated and often delayed. Indeed, abdominal pain or distended abdomen, jaundice (choledocholithiasis), symptoms of peritoneal irritation, or peritonitis complicated with more severe sepsis, may be observed in patients [2]. However, radiological examinations can provide a diagnosis of certainty.
We report a case of intrahepatic biloma, collected in the radiology department, following a closed abdominal trauma after a car accident.
This case report aims to underline the importance of imaging including ultrasound, CT, MRI), MRI cholangiopancreatography (MRCP), or hepatobiliary cholescintigraphy to establish the diagnosis and guide the therapeutic gestures.
Case presentation
This was a 4-year-old male child who, following a traffic accident, presented with abdominal pain most evident in the right hypochondrium.
Admitted to the emergency room, the clinical examinations suspected a closed abdominal trauma with a stable hemodynamic state. Biological tests showed a slight elevation of C-Reactive Protein (CRP˂6 mg/L) with no sign of biological cholestasis. Sedimentation rate (SV) and Fibrinogen were normal.
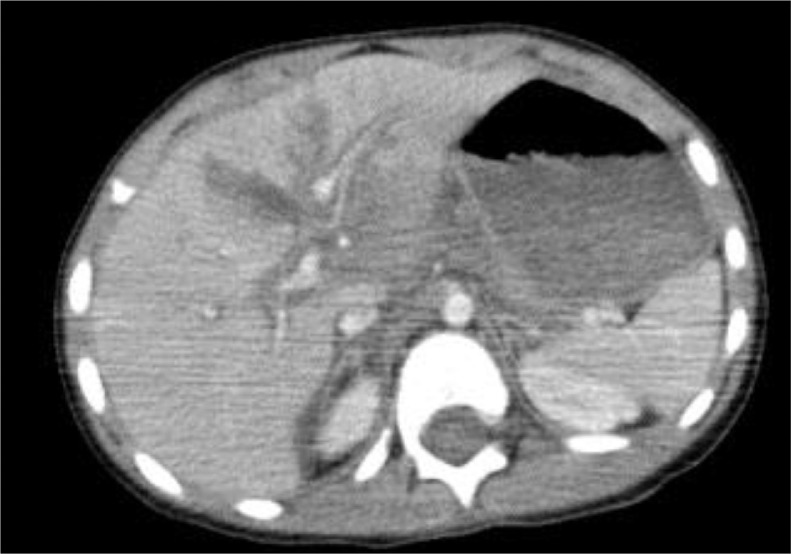
The initial abdominal CT scan with an injection of non-ionic iodinated contrast medium, performed within 24 hours after the accident, objectified a focus of hepatic laceration at the level of segment I, II, III, and IV, associated with a peritoneal effusion of medium abundance (Fig. 1). The child was hospitalized.
Fig. 1.
Abdominal CT scan with PDC injection in axial section at portal time: presence of a fairly well-limited hypodense area located at the level of segments I, II, III and IV in relation to a focus of hepatic laceration without lesion of the hepatic pedicle with moderate peritoneal effusion.
On the fifth day, an abdominal ultrasound check-up showed intrahepatic cystic formations, infra and supra centimetric, the largest of which was located between segments IV and V, measuring 39 × 38 mm, and came into contact with the intrahepatic bile duct.
The three ultrasound controls carried out at 1-week intervals noted a progressive and considerable increase in the volume of the cystic formations of segments IV and V measuring 64 × 56 mm, with disruption of the infra-centimetric cystic formations at 1-month post-trauma.
The follow-up CT scan noted 2 intrahepatic cystic formations in segments IV and II measuring 64 × 52 mm and 33 × 27 mm respectively.
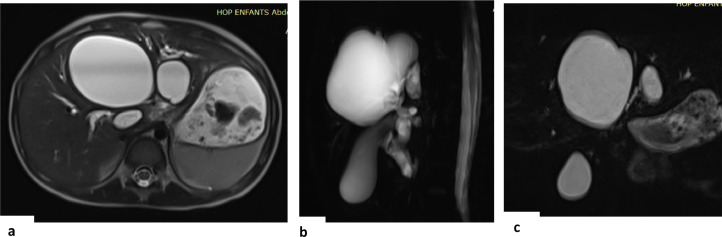
A Bili MRI performed at one and a half months noted 3 cystic formations communicating with the intrahepatic bile ducts (Fig. 2A, B, and C).
Fig. 2.
Abdominal MRI axial T2 sequence (A), 3D radial BILI sequence (B) and 3D BILI sequence (C) showing cystic formations communicating with the intrahepatic bile ducts.
Percutaneous drainage was performed, and the patient was put on antibiotic therapy.
The diagnosis of biloma was confirmed by the presence of bilirubin in the drainage fluid, and the follow-up imaging revealed the disappearance of intrahepatic cystic formations with complete resolution of symptoms.
Discussion
The biloma is a well-circumscribed collection of intra-abdominal bile, whether encapsulated or not, outside the biliary tree [2]. Clinically, bilomas present after iatrogenic or traumatic disruption of the biliary tree with abdominal pain in the right hypochondrium, nausea, vomiting, and sometimes fever in case of an infected biloma. The patient may be icteric in case of extrinsic compression of the bile duct. Our patient presented only abdominal pain in the right hypochondrium without evidence of jaundice.
Initial laboratory tests may be normal or reveal an inflammatory syndrome [4]. Indeed, our patient had only a slight increase in CRP.
Bilomas are most often secondary to rupture of the biliary tree by a traumatic cause and can rarely be spontaneous [5]. Usually, it is a blunt trauma of the right hypochondrium and the post-traumatic biloma may take 1 to 2 days to appear [6]. Our case showed this late appearance on the third day of the abdominal trauma with intrahepatic cystic formations following a car accident.
Bilomas can also be related to sickle cell disease by hepatic infarction [7] or be of iatrogenic origin (laparoscopic cholecystectomy, endoscopic retrograde cholangiopancreatography, radiofrequency ablation, arterial chemoembolization by catheter, liver transplantation, resection, and biopsy) [8,9]. These origins were not confirmed in our case.
Imaging remains the gold standard for establishing a diagnosis of biloma.
Abdominal ultrasound is a complementary imaging test to establish a diagnosis. Indeed, it allows to identification of cystic lesions and shows debris or blood clots in the biloma [2,10].
The CT scan, on the other hand, identifies a well-circumscribed collection of fluid with clear margins that may be either encapsulated or non-encapsulated [2,4,11]. It allows the differential diagnosis of biloma with postoperative seroma, hematoma, abscess, lymphocele, hepatic cyst, and pseudocyst [4].
MRI or hepatobiliary cholescintigraphy is often necessary to confirm the diagnosis [2]. Indeed, the biloma can be observed in hyposignal T1 and hypersignal T2. Sometimes, a peripheral enhancement of the biloma can be seen due to a reactive inflammation, after injection of gadolinium.
MRCP (magnetic resonance cholangiopancreatography) highlights the source of the biliary leak [12].
Hepatobiliary cholescintigraphy is effective in the diagnosis and treatment planning of bilomas. It is very sensitive when searching for a biliary leak. Ultrasound- or CT-guided biloma puncture is necessary to confirm the diagnosis when previous imaging and clinical findings are inconclusive [2].
The treatment of bilomas is based on three main options, namely percutaneous or endoscopic drainage, surgical drainage or close monitoring. The treatment strategy depends on the morphotype of the patient, the size and hepatic segmental location of the biloma, the continuous biliary leakage, as well as the superinfection [2]. In our patient percutaneous drainage was successfully performed.
Small asymptomatic fluid collections are usually reabsorbed and do not require intervention. Ultrasound-guided aspiration is preferred to CT scan in most cases. The prognosis is good in cases of bilomas treated by percutaneous drainage, without continuous bile leaks. Surgical management of biloma is indicated in cases of failed percutaneous drainage or persistent bile leaks [2].
Complications of biloma include infection, septic shock, abscess formation, and biliary tree impact cholestasis [4]. Risks of percutaneous biloma drainage include bleeding, infection, damage to surrounding structures, and failure to drain the biloma [4]. No complications were observed in our patient and the evolution was satisfactory.
Conclusion
Posttraumatic liver biloma is a rare and late complication of liver injury secondary to abdominal trauma, which increases morbidity and length of hospitalization. The onset of clinical symptoms is often insidious with a delay in diagnosis. Imaging remains the gold standard in the diagnosis and therapeutic management of post-traumatic bilomas.
Patient consent
We confirm that all the methods and techniques used in this study were carried out in accordance with international standards of research ethics and data protection.
Participation in the study was voluntary and anonymous.
An administrative authorization to conduct the study was requested and obtained from the management of the CHU ibn Rochd of Casablanca, and the written consent of the patient’s parents was requested and obtained.
Footnotes
Competing Interests: The authors have declare that we have no known conflicts of interest associated with this publication and that there was no significant financial support for this work that could have influenced its outcome.
References
- 1.Gould L, Patel A. Ultrasound detection of extrahepatic encapsulated bile: ‘biloma’. AJR Am J Roentgenol. 1979;132(6):1014–1015. doi: 10.2214/ajr.132.6.1014. [DOI] [PubMed] [Google Scholar]
- 2.Copelan A, Bahoura L, Tardy F, Kirsch M, Sokhandon F, Kapoor B. Etiology, diagnosis, and management of bilomas: a current update. Tech Vasc Interv Radiol. 2015;18(4):236–243. doi: 10.1053/j.tvir.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Giss SR, Dobrilovic N, Brown RL, Garcia VF. Complications of nonoperative management of pediatric blunt hepatic injury: diagnosis, management, and outcomes. J Trauma Acute Care Surg. 2006;61(2):334–339. doi: 10.1097/01.ta.0000197605.27190.2c. [DOI] [PubMed] [Google Scholar]
- 4.Vazquez JL, Thorsen MK, Dodds WJ, Quiroz FA, Martinez ML, Lawson TL, et al. Evaluation and treatment of intraabdominal bilomas. AJR Am J Roentgenol. 1985;144(5):933–938. doi: 10.2214/ajr.144.5.933. [DOI] [PubMed] [Google Scholar]
- 5.Della Valle V, Eshja E, Bassi EM. Spontaneous biloma: a case report. J Ultrasound. 2015;18(3):293–296. doi: 10.1007/s40477-013-0053-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ragavan M, Duraiprabhu A, Madan R, Murali K, Francis G, Subramanian M. Posttraumatic Intrahepatic Bilioma. Indian J Surg. 2015;77(Suppl 3):1399–1400. doi: 10.1007/s12262-014-1071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lebensburger J, Esbenshade A, Blakely M, Hankins J, Wang W. Biloma and pneumobilia in sickle cell disease. Pediatr Blood Cancer. 2008;51(2):288–290. doi: 10.1002/pbc.21575. [DOI] [PubMed] [Google Scholar]
- 8.Liu J, Wu Y, Xu E, Huang Q, Ye H, Tan L, et al. Risk factors of intrahepatic biloma and secondary infection after thermal ablation for malignant hepatic tumors. Int J Hyperthermia. 2019;36(1):980–985. doi: 10.1080/02656736.2019.1660422. [DOI] [PubMed] [Google Scholar]
- 9.Sakamoto I, Iwanaga S, Nagaoki K, Matsuoka Y, Ashizawa K, Uetani M, et al. Intrahepatic biloma formation (bile duct necrosis) after transcatheter arterial chemoembolization. AJR Am J Roentgenol. 2003;181(1):79–87. doi: 10.2214/ajr.181.1.1810079. [DOI] [PubMed] [Google Scholar]
- 10.Thomas S, Jahangir K. Noninvasive imaging of the biliary system relevant to percutaneous interventions. Semin Interv Radiol. 2016;33(4):277–282. doi: 10.1055/s-0036-1592328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akin K, Ozturk A, Guvenc Z, Isiklar I, Haberal M. Localized fluid collections after liver transplantation. Transplant Proc. 2006;38(2):627–630. doi: 10.1016/j.transproceed.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290(16):2168–2173. doi: 10.1001/jama.290.16.2168. [DOI] [PubMed] [Google Scholar]