Abstract
A 53-year old female patient with history of hypocomplementaemic urticarial vasculitis syndrome (HUVS) and polyarteritis nodosa presented with progressive dyspnoea on exertion due to emphysema. Lung function revealed a severe obstructive ventilator disorder with a forced expiratory volume in 1 second of 22% of predicted, and a significant hyperinflation with a residual volume of 321% of predicted. Multi-detector computed tomography (MDCT) scan and quantitative CT analysis (StratX software) confirmed a lower lobe predominant emphysema. Considering the young age, the very severely impaired lung function, the relatively low nicotine abuse, the exclusion of alpha-1 antitrypsin deficiency, together with the known diagnosis of HUVS, the emphysema was more likely due to the vasculitis than to a typical chronic obstructive lung disease.
MDCT scan showed that particularly the segment 8 of the right lower lobe was severely emphysematous destroyed and hyperinflated. Invasive Chartis® measurement revealed no significant collateral ventilation of the isolated segment 8 of the right lower lobe, so that an endobronchial valve placement was performed. Three months following intervention, the MDCT scan revealed a complete collapse of the segment 8 on the right, which was associated with a significant clinical benefit and a mild reduction of the hyperinflation in the lung function test.
Keywords: Vasculitis, Emphysema, Hypocomplementaemic urticarial vasculitis syndrome, Valve implantation, Segmental valve implantation
1. Introduction
Chronic obstructive pulmonary disease (COPD) and emphysema are the major cause of chronic morbidity and comprise one of the top three causes of death worldwide [1]. The leading risk factor for COPD is cigarette smoking, but also environmental exposure or predisposing host factors may contribute to the development of COPD. Rare causes for a pulmonary emphysema are different forms of vasculitis [2,3]. Besides the specific treatment of the underlying vasculitis, the therapeutic approach for the vasculitis-induced emphysema is comparable to the treatment of smoking-induced COPD.
Endoscopic therapeutic modalities should be considered in case of significant hyperinflation. The reversible endoscopic valve treatment is beneficial in patients with severe hyperinflation and absent interlobar collateral ventilation (CV) [4].
In this manuscript, we report a case of a patient with emphysema most likely due to hypocomplementaemic urticarial vasculitis syndrome, who experienced a clinical and radiological benefit following segmental valve treatment.
2. Case presentation
2.1. Case summary
A 53-year old female patient presented with progressive dyspnoea on exertion. She complained about breathlessness after climbing 2–3 steps. The shortness of breath significantly impacted her day-to-day functioning and thus her quality-of-life. She only had cough occasionally, mainly non-productive. Her mMRC (Modified Medical Research Council) scale was 3 [5], her COPD Assessment Test (CAT) score 15 [6]. The patient had a known impaired lung function with forced expiratory volume in 1 second (FEV1) of 0.6L (22% of predicted), and a severe hyperinflation with a residual volume of 5.84L (321% of predicted). Moreover, the diffusion capacity was severely impaired with a transfer coefficient for carbon monoxide (TLCO) of 21% of predicted. She had a 15-pack-year smoking history and quit smoking 6 years previous to the presentation. An alpha-1-antitrypsin deficiency was excluded in several laboratory tests. Due to the obstructive ventilator disorder, the patient was treated with long-acting muscarinic antagonists, long-acting beta-agonists and inhaled corticosteroids. As the blood gas analysis revealed a pO2 of 64 mmHg, there was no need for long-term oxygen therapy.
Patient's anamnesis revealed a diagnose of hypocomplementaemic urticarial vasculitis syndrome (HUVS) established 18 years previous to the presentation. At the time of diagnosis, anti-C1-antibodies were positive, C3 and C4 were reduced with 42 mg/dl and <6,7 mg/dl (normal range: 82–160 mg/dL, and 16–46 mg/dl, respectively). Histology of skin biopsy was consistent with urticaria-vasculitis. At the time of the current presentation however, she received no specific treatment for HUVS, as the disease was non active (normal C3 and C4 levels) for several years. However, an ANCA-negative vasculitis of the abdominal vessels suspicious for polyarteritis nodosa, with a stenosis of the coeliac trunk and an aneurysm of the hepatic artery, was diagnosed 3 months previously and treated with immunosuppressive medication. In summary of the findings, it was assumed that the emphysema was mainly due to HUVS, which may be associated with pulmonary emphysema in 20% of patients [2].
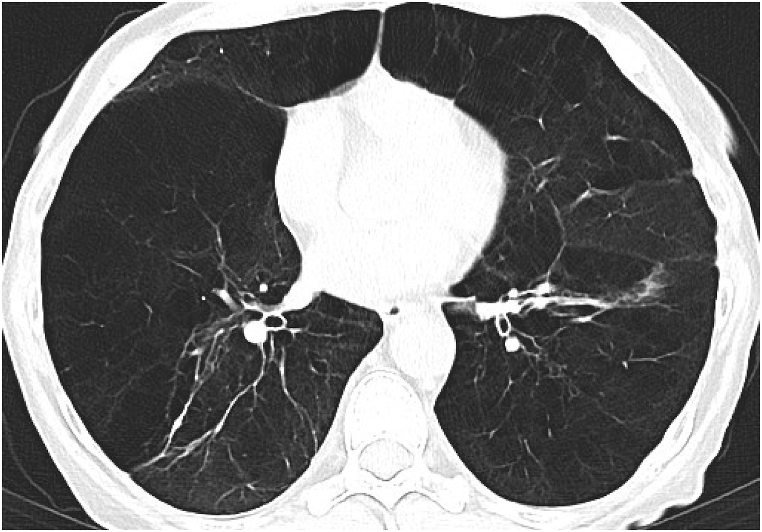
To evaluate further treatment approaches for emphysema, e.g. endobronchial valve treatment, a multi-detector computed tomography (MDCT) scan was performed that revealed a severe, mainly panlobular emphysema with a predominance of the lower lobes. Emphysema index assessed by quantitative CT (StratX) software (threshold of −950 HU) was found to be 58% in the right lower lobe and 53% in the left lower lobe. Moreover, quantitative CT analysis demonstrated an 80–95% fissure integrity of both major fissures.
Particularly, the segment 8 of the right lower lobe was severely emphysematous destructed and hyperinflated in the MDCT scan (Fig. 1). Therefore, an invasive assessment of collateral ventilation (CV) of this single lung segment and - in case of absent CV - an endobronchial one-way valve placement was planned. Hence, a bronchoscopy was performed under general anesthesia. CV was quantified using the Chartis® measurement system by placing the Chartis® catheter in the segment 8 of the right lower lobe. An absence of significant CV could be confirmed, so that one endobronchial valve was implanted. No complications occurred, so that the patient could be discharged 4 days following the bronchoscopic procedure.
Fig. 1.
Prior to valve treatment, the MDCT scan showed severe, mainly panlobular emphysema with a predominance of the lower lobes.
2.2. Outcome and follow-up
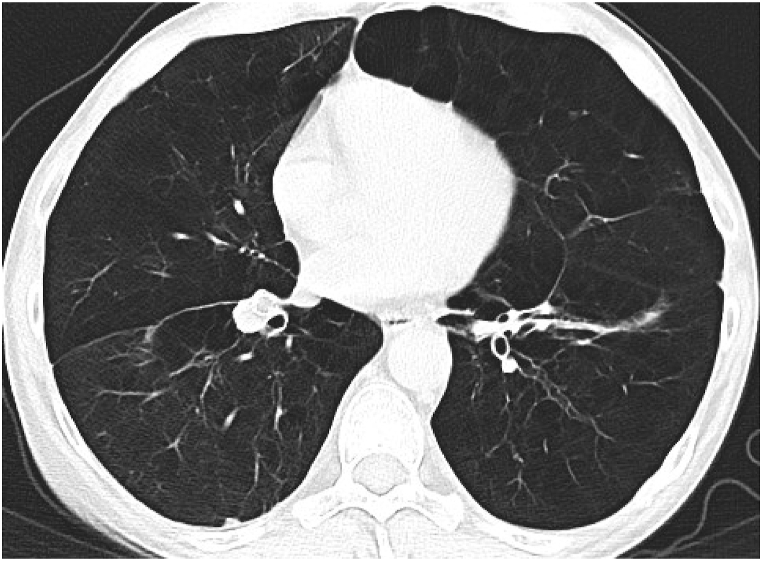
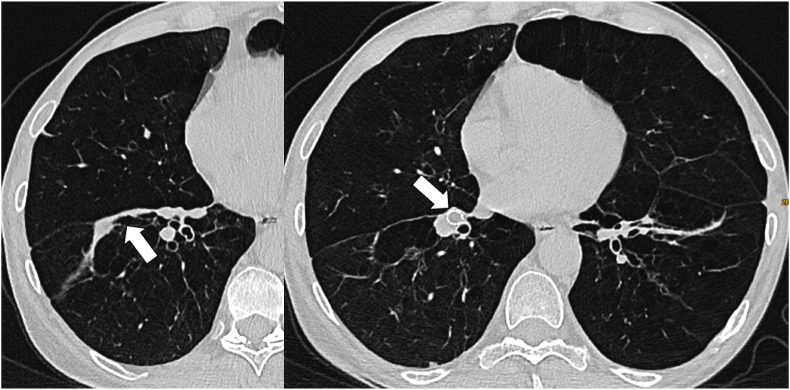
Three months following intervention, the patient reported a significant symptom relief with optimized exercise capacity and improved quality of life. The mMRC score was 2 [5], and the CAT score improved significantly from 15 to 6 [6]. Lung function however did not reveal a clinical relevant improvement. Only a mild RV reduction of 240 ml could be observed. Nevertheless, the CT scan taken 3 months after valve placement showed a complete collapse of the segment 8 of the right lower lobe (Fig. 2). Thus, the radiological assessment showed the optimal result following segmental treatment, which was associated with a subjective clinical relevant improvement (see Fig. 3).
Fig. 2.
Three months following valve treatment, the MDCT scan showed a complete collapse of the segment 8.
Fig. 3.
CT three months following valve treatment. Arrows point to the atelectatic segment 8.
3. Discussion
A vasculitis-induced emphysema is a rare diagnosis, but can be found in 20%–50% of patients with HUVS, a small vessel vasculitis [7]. Moreover, there are some case reports about patients with emphysema due to granulomatosis with polyangiitis [3]. Histopathologically, patients with HUVS present a pulmonary capillaritis that may lead to obstructive airway disease and emphysema [8]. HUVS-related antibodies against the collagen-like region of C1q can form immune complexes in multiple tissues including the lungs [9], binding alveolar surfactant protein [7]. Treatment for HUVS includes antihistamines and corticosteroids. In cases with poor response to this first-line treatment, cyclosporine, colchicine, hydroxychloroquine, azathioprine, methotrexate, and dapsone, IL-1b inhibitors and Olamizumab present alternative treatment approaches [10]. The therapeutic approach for the vasculitis-induced emphysema is comparable to the treatment of smoking-induced COPD, including inhaled bronchodilators and inhaled corticosteroids depending on the symptoms and frequency of COPD exacerbations [1]. Smoking cessation, consequent physiotherapy and pulmonary rehabilitation are essential. Endoscopic valve therapy presents an invasive treatment modality for emphysema patients with severe hyperinflation. Thereby, the most emphysematous lung lobe is occluded by one-way-valves that allow air to be expelled during expiration, but not to enter during inspiration, and thus facilitate lobar atelectasis. A lobar occlusion is one important prerequisite for lobar volume reduction; a segmental treatment does not lead to a beneficial outcome in the majority of patients due to intralobar CV [11].
In this report, we describe a patient with an emphysema most likely due to HUVS that was diagnosed 18 years before. As the HUVS was not active for several years, the patients received no specific treatment. The obstructive airway disease and emphysema have already been diagnosed 10 years previously, at the age of 43. As COPD in patients younger than 50 years is rare, alternative causes than smoking have to be considered. In this patient, HUVS contributed most likely to the development of emphysema. The MDCT revealed a lower lobe predominant emphysema, whereby particularly the segment 8 of the right lower lobe was hyperinflated and emphysematous destroyed. In the majority of humans an interlobular CV can be observed, which preclude a beneficial effect after a segmental valve placement [12]. However, we confirmed an absent interlobular CV by Chartis® assessment of the segment 8 of the right lower lobe, so that a segmental valve treatment was assumed to be beneficial. Three months following the intervention, MDCT showed a complete collapse of the segment 8 that was associated with the patient's report of an improved exercise capacity and quality of life.
4. Conclusion
This case suggests that patients with a vasculitis-induced emphysema should not be excluded from valve therapy. However, whether segmental valve treatment in comparison to a lobar treatment is more often successful in these patients remains to be assessed on individual basis.
References
- 1.Global Initiative of Chronic obstructive Lung disease . 2022. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. [Google Scholar]
- 2.Casal A., Díaz-Garel J., Pereiro T., Toubes M.E., Ricoy J., Valdés L. Pulmonary vasculitis. J. Thorac. Dis. 2018;10(9):5560–5575. doi: 10.21037/jtd.2018.08.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gadre S.K., Stoller J.K., Mehta A.C. Granulomatosis with polyangiitis and associated pulmonary emphysema: breathtaking vasculitis. Lung India. 2015;32(4):367–369. doi: 10.4103/0970-2113.159576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Criner G.J., Sue R., Wright S., Dransfield M., Rivas-Perez H., Wiese T., Sciurba F.C., Shah P.L., Wahidi M.M., de Oliveira H.G., Morrissey B., Cardoso P.F.G., Hays S., Majid A., Pastis N., Jr., Kopas L., Vollenweider M., McFadden P.M., Machuzak M., Hsia D.W., Sung A., Jarad N., Kornaszewska M., Hazelrigg S., Krishna G., Armstrong B., Shargill N.S., Slebos D.J., LIBERATE Study Group A multicenter randomized controlled trial of zephyr endobronchial valve treatment in heterogeneous emphysema (LIBERATE) Am. J. Respir. Crit. Care Med. 2018 Nov 1;198(9):1151–1164. doi: 10.1164/rccm.201803-0590OC. [DOI] [PubMed] [Google Scholar]
- 5.Mahler D.A., Wells C.K. Evaluation of clinical methods for rating dyspnea. Chest. 1988 Mar;93(3):580–586. doi: 10.1378/chest.93.3.580. [DOI] [PubMed] [Google Scholar]
- 6.Jones P.W., Harding G., Berry P., Wiklund I., Chen W.H., Kline Leidy N. Development and first validation of the COPD assessment test. Eur. Respir. J. 2009;34(3):648–654. doi: 10.1183/09031936.00102509. [DOI] [PubMed] [Google Scholar]
- 7.Breda L., Nozzi M., Harari S., Del Torto M., Lucantoni M., Scardapane A., Chiarelli F. Hypocomplementemic urticarial vasculitis (HUVS) with precocious emphysema responsive to azathioprine. J. Clin. Immunol. 2013 Jul;33(5):891–895. doi: 10.1007/s10875-013-9886-1. [DOI] [PubMed] [Google Scholar]
- 8.Hunt D.P., Weil R., Nicholson A.G., Burke M.M., Du Bois R.M., Wells A.U. Pulmonary capillaritis and its relationship to development of emphysema in hypocomplementaemic urticarial vasculitis syndrome. Sarcoidosis Vasc. Diffuse Lung Dis. 2006 Mar;23(1):70–72. [PubMed] [Google Scholar]
- 9.Siegert C.E., Kazatchkine M.D., Sjöholm A., Würzner R., Loos M., Daha M.R. Autoantibodies against C1q: view on clinical relevance and pathogenic role. Clin. Exp. Immunol. 1999 Apr;116(1):4–8. doi: 10.1046/j.1365-2249.1999.00867.x. PMID: 10209498; PMCID: PMC1905233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kolkhir P., Bonnekoh H., Kocatürk E., Hide M., Metz M., Sánchez-Borges M., Krause K., Maurer M. Management of urticarial vasculitis: a worldwide physician perspective. World Allergy Org. J. 2020 Mar 5;13(3) doi: 10.1016/j.waojou.2020.100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slebos D.J., Shah P.L., Herth F.J., Valipour A. Endobronchial valves for endoscopic lung volume reduction: best practice recommendations from expert panel on endoscopic lung volume reduction. Respiration. 2017;93(2):138–150. doi: 10.1159/000453588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gompelmann D., Eberhardt R., Herth F.J. Collateral ventilation. Respiration. 2013;85(6):515–520. doi: 10.1159/000348269. [DOI] [PubMed] [Google Scholar]