Abstract
Background:
Naloxone is an opioid antagonist medication that can be administered by lay people or medical professionals to reverse opioid overdoses and reduce overdose mortality. Cost was identified as a potential barrier to providing expanded overdose education and naloxone distribution (OEND) in New York City (NYC) in 2017. We estimated the cost of delivering OEND for different types of opioid overdose prevention programs (OOPPs) in NYC.
Methods:
We interviewed naloxone coordinators at 11 syringe service programs (SSPs) and 10 purposively sampled non-SSPs in NYC from December 2017 to September 2019. The samples included diverse non-SSP program types, program sizes, and OEND funding sources. We calculated one-time start up costs and ongoing operating costs using micro-costing methods to estimate the cost of personnel time and materials for OEND activities from the program perspective, but excluding naloxone kit costs.
Results:
Implementing an OEND program required a one-time median start-up cost of $874 for SSPs and $2,548 for other programs excluding overhead, with 80% of those costs attributed to time and travel for training staff. SSPs spent a median of $90 per staff member trained and non-SSPs spent $150 per staff member. The median monthly cost of OEND program activities excluding overhead was $1,579 for SSPs and $2,529 for non-SSPs. The costs for non-SSPs varied by size, with larger, multi-site programs having higher median costs compared to single-site programs. The estimated median cost per kit dispensed excluding and including overhead was $19 versus $25 per kit for SSPs, and $36 versus $43 per kit for non-SSPs, respectively.
Conclusions:
OEND operating costs vary by program type and number of sites. Funders should consider that providing free naloxone to OEND programs does not cover full operation costs. Further exploration of cost-effectiveness and program efficiency should be considered across different types of OEND settings.
Keywords: Cost, naloxone, overdose education
INTRODUCTION
Distributing naloxone, an opioid antagonist medication for reversing opioid overdoses, is one of US Department of Health and Human Services’ Opioid Initiative’s three priority strategies for curtailing the opioid crisis.1 Naloxone may be administered by lay people or medical professionals to reverse overdoses,2 and can effectively reduce overdose mortality.3,4 Naloxone administration by lay people, especially people who currently or formerly use drugs, may play a key role in overdose reversal. Particularly when immediate access to emergency medical services is limited, such as in rural or underserved locations and in fentanyl-driven overdoses, it may require quicker response times and additional naloxone doses to avoid fatality.5 The receipt of naloxone is frequently paired with harm reduction education on overdose prevention and risk reduction.
In New York City (NYC), opioid overdose deaths reached a record high number in 2017 after seven consecutive years of overdose increases.6 While NYC has seen a modest decrease of 3% in overdose rates from 2017 to 2018, opioid overdose fatality rates still remain high due to fentanyl.6 In 2017, the NYC Mayor’s office released a strategy to address the opioid crisis called HealingNYC, with one of its goals to quadruple naloxone distribution to 100,000 naloxone kits.7 Over 100 registered opioid overdose prevention programs (OOPPs) provide overdose education and naloxone distribution (OEND) at no cost to participants in NYC. These programs are located in a variety of governmental agencies and non-governmental organizations including syringe service programs (SSPs), substance use disorder treatment programs, community health centers, hospital systems, programs for the unhoused, programs for justice impacted populations, and other types of community based organizations. The HealingNYC initiative ultimately resulted in an increased number and diversity of registered OOPPs for the distribution of naloxone, which required the expansion of training to accommodate new programs less familiar with engaging people who use drugs.
Recent studies have found that OEND is cost-effective, except in secondary school settings with low overdose rates.8–15 Most of these studies estimate the cost of delivering OEND by type of person trained (i.e. lay persons, law enforcement, emergency services), but not type of program delivering the training to lay persons. Costs have been identified as a barrier to providing effective OEND due to naloxone costs and staff time.16–19 For example, previous work has indicated that salary support for staff time, limited time availability of staff to provide OEND, and poor staff buy-in are barriers to OEND implementation.19 While programs may receive their naloxone kit supply at no cost from government agencies, as they do in NYC, other service delivery costs may still remain a barrier to providing OEND. To assess the resources needed by various types of OOPPs to provide OEND, we estimate start up and program operational costs for different types of OOPPs in NYC.
METHODS
Data Collection
At the end of 2017, approximately 176 OOPPs in NYC had registered with the New York State Department of Health to receive and subsequently dispense intranasal or intramuscular naloxone under a standing order.20 The vast majority of naloxone kits provided by DOHMH to OOPPs were the Narcan® nasal spray formulation, but intramuscular injection naloxone formulations were also available predominantly through SSPs as an option for people who preferred that to the nasal spray. In NYC, OEND is overseen by the NYC Department of Health and Mental Hygiene (DOHMH). OOPPs included all SSPs in NYC and several large hospital/health systems, substance use disorder treatment programs, government agencies, and community-based organizations. We interviewed 13 naloxone coordinators whom each represent an SSP with the exception of one coordinator who supports two programs, resulting in full representation of all 14 SSPs in NYC. We purposively sampled 16 non-SSPs to achieve a diversity of program types (i.e., programs for unhoused people, programs for justice impacted populations, large hospital/health systems, substance use disorder treatment programs, and other community-based organizations), program sizes (single site vs. multi-site), and funding sources (received funding from DOHMH to support OEND program costs vs. no funding from DOHMH to support program costs). We successfully recruited 10 of 16 non-SSP OOPPs (71% participation) that served individuals in the Bronx, Brooklyn, Manhattan, and Staten Island. This sample has at least one program from each of the major non-SSP program types that distributed the majority of naloxone kits among non-SSP OOPPs and includes an even number of single site and multi-site organizations. Three SSPs were not included in the analysis due to insufficient data, resulting in 11 SSPs and 10 non-SSPs included in the final analysis.
We interviewed OOPP naloxone dispensing program leaders and staff between December 2017 and September 2019 to estimate the cost of OEND at each organization excluding the cost of the naloxone kits supplied by DOHMH. We conducted semi-structured interviews in person if possible (16 of 23) or by phone for approximately one to two hours on average. Oral consent was obtained prior to each interview. Interviews covered topics regarding OOPP staffing and staff titles of individuals providing OEND, and the time for staff to conduct typical OEND activities described in Figure 1 (see Appendix Table 1 for definitions). The cost of personnel time for staff providing OEND was estimated using NYC wage rates for similar positions from the US Bureau of Labor Statistics (Appendix Table 2).21 Fringe benefits for SSPs were derived from annual SSP budgets. We used the median fringe benefit rate for full time and part time employees. Fringe benefits for non-SSPs were estimated using the average national fringe rate across all industries from the US Bureau of Labor Statistics.21 Because costs were calculated from the program perspective, volunteer time was not included in the labor costs.
FIGURE 1.
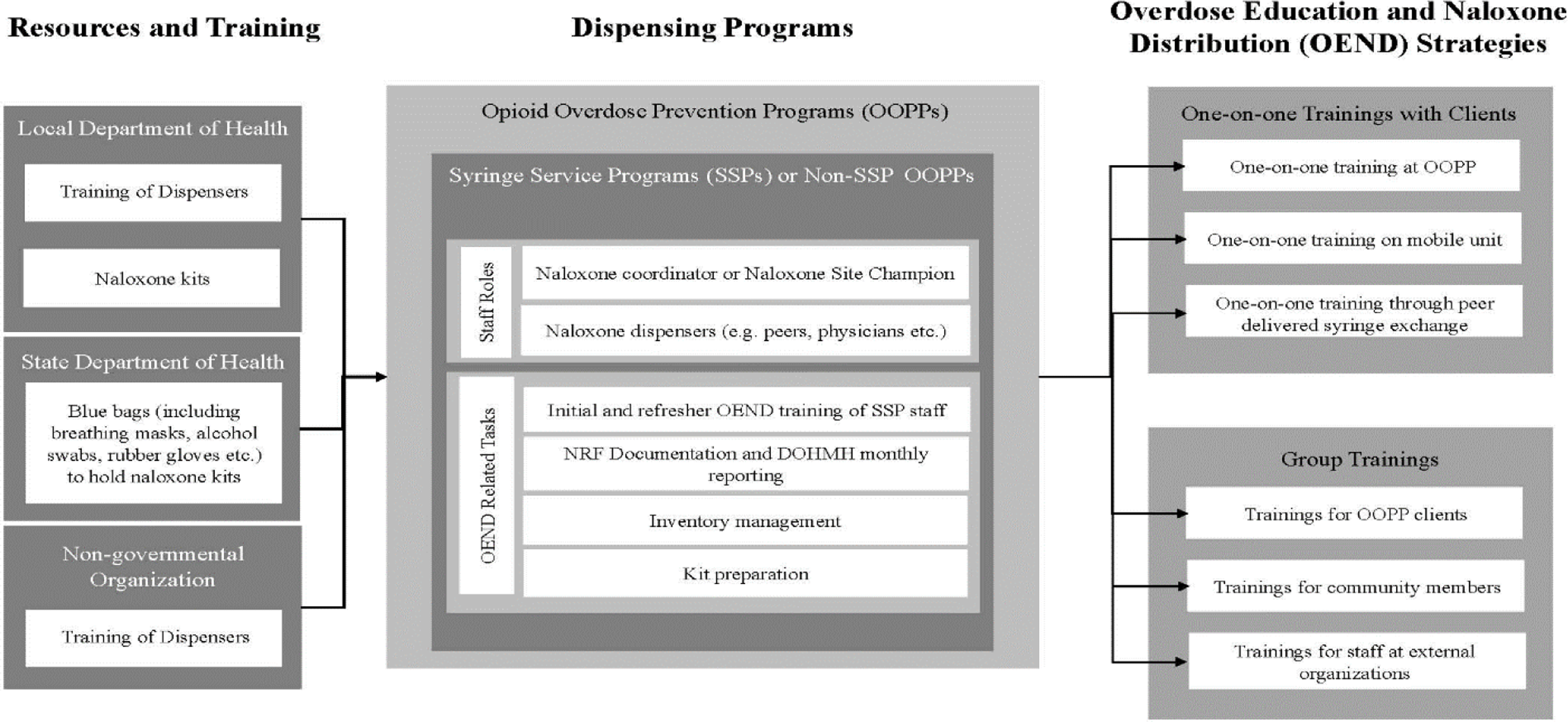
Overdose Education and Naloxone Distribution Resources and Activities
Note: Costs did not include: 1) the trainer time for delivering the training of dispensers by DOHMH or another external program 2) naloxone kits, and 3) blue bags. Staff time spent preparing kits, delivering training of dispensers, preparing blue bag OEND kits, managing inventory, providing trainings in one-on-one setting or in group settings and the subsequent documentation and reporting were included in the cost from the program perspective.
OOPP= Opioid Overdose Prevention Program; SSP= Syringe Service Program; NRF=Naloxone Recipient form; OEND= Overdose Education and Naloxone Distribution; DOHMH=Department of Health and Mental Hygiene.
At the time of the study, DOHMH required OOPPs to submit naloxone recipient forms on a monthly basis to document each naloxone kit dispensed. These forms included information regarding OEND location, and characteristics of the naloxone recipient. 22,23 Aggregated results allowed investigators to estimate the average number of naloxone kits dispensed per program per month. This study was approved by the Institutional Review Board of Weill Cornell Medical College.
Analysis
We calculated program costs using micro-costing methods to estimate the cost of personnel time and materials involved in OEND (Appendix Table 2). Start-up costs were collected from each program and included costs of conducting start-up OEND training sessions for staff members, developing training materials, and developing an inventory database. Staff members were initially trained either off site at one of two training sites or on site by other trained staff. If staff attended the training offsite, we included estimated travel time to attend the training. Ongoing OEND costs include variable costs, which are costs that are associated with each person receiving OEND and are calculated per OEND event, and time dependent costs, which are costs that occur on a regular weekly, monthly or quarterly basis.
Variable costs include costs of delivering one-on-one OEND onsite or on a mobile unit, group OEND trainings delivered at specific organizations, and group OEND trainings delivered at community events. Programs received group training requests from organizations across all boroughs, which were usually requests to train the staff at those organizations to respond to on-site overdoses. Occasionally, organizational trainings also included training for the organization’s clients. Community trainings were often held in high-need neighborhoods with the highest rates of overdoses, and were open to the public. We included the costs of OOPP staff travel time to and from the organizational or community trainings held off site in the variable costs for these group trainings.
Time dependent costs include tracking and managing naloxone inventory, blue bag assembly (i.e., inserting naloxone kits, educational materials, breathing mask, alcohol swab, etc into a blue bag for distribution), regularly scheduled overdose education client group trainings, naloxone recipient form database management, documentation and reporting to agencies that supply naloxone kits, and refresher OEND staff trainings. We used the monthly average number of kits distributed in the first half of 2018 for programs interviewed between December 2017–2018, and we used the monthly average for the first half of 2019 for programs interviewed in 2019 to estimate the annual cost per naloxone kit dispensed at each program.
We estimated overhead costs and applied site-specific overhead rates for SSPs and non-SSPs. Overhead costs for SSPs and non-SSPs were calculated using the ratio of costs for equipment, supplies, consultants, and program administration to costs of personnel, fringe benefits and travel as reported in 2017 IRS 990 Forms for each non-profit organization, except for the large hospital systems for which overhead was calculated based on previously published analyses.24
RESULTS
Characteristics of OEND Programs
Table 1 describes program characteristics of SSPs and non-SSPs, including OEND dispensing strategies. The 11 SSPs varied from one to six fixed sites with an average of two fixed sites per SSP. The five single-site non-SSPs were community-based organizations that served high-need populations at risk for witnessing or experiencing an overdose. Two of the multi-site non-SSPs were part of larger hospital systems that had 7–30 sites and three were large multi-site community-based organizations that had 15–52 sites.
Table 1:
Description of Opioid Overdose Prevention Programs (OOPPs)
| Program Type | ||||
|---|---|---|---|---|
| SSPs (N=11) | Single Site Non-SSPs (N=5)* | Multi-Site Non-SSPs (N=5) | ||
| Number of Fixed Sites (Range) | 1–6 | 1–2 | 7–52 | |
| Number of OOPPs that dispense through peer outreach | 11 | 2 | 0 | |
| Number of OOPPs that dispense through mobile units | 7 | 1 | 1 | |
| Median number of kits per month (Range) ** | 80 (27–187) | 52 (13–58) | 89 (37–196) | |
| Primary dispensing route | ||||
| One-on-one OEND | 7 | 4 | 4 | |
| Community OEND | 2 | 1 | 0 | |
| Organizational OEND | 2 | 0 | 1 | |
| Median number of trainings per month (Range) ** | ||||
| One-on-one OEND | 31 (9–90) | 46 (0–107) | 39 (8–68) | |
| On-site Group Client OEND | 1 (0–6) | 0 (0–8) | 3 (0–9) | |
| Group Community OEND | 0 (0–12) | 1 (0–1) | 0 (0–2) | |
| Group Organizational OEND | 4 (0–16) | 0 (0–2) | 1 (0–6) | |
Single-site non-SSPs is defined as having no more than two fixed sites
Rounded to nearest whole number
Seven SSPs had one or two mobile units to dispense syringes and naloxone kits, making an average of four stops per week and all eleven sites also dispensed naloxone through peers who deliver kits to other people who use drugs. Only one non-SSP delivered OEND on a mobile unit and no non-SSPs did peer delivery. All SSPs receive DOHMH funding to support a naloxone coordinator, peers and/or other staff involved with naloxone dispensing. Among non-SSPs, six out of ten received DOHMH funding to support OEND activities.
Seven of the eleven SSPs and seven of the 10 non-SSPs distributed kits primarily through one-on-one trainings. The naloxone coordinator at SSPs led a median of eight external group trainings per month. For non-SSPs, single-site programs led a median of two external group trainings per month and multi-site programs led a median of three per month. Non-SSPs distribute more kits per month compared to SSPs with a median of 89 (range: 37–196) for multi-site non-SSPs, 52 (range:13–58) for single-site SSPs, and 80 (range: 27–187) for SSPs.
Start-up Costs
Median start-up costs (excluding overhead) were highest for multi-site non-SSPs ($6,842, range: $2,285-$51,446), followed by single-site non-SSPs ($2,039, range: $723- $2,930) and then SSPs ($874, range: $448-$4,504) (Table 2). Median incremental overhead costs were highest for multi-site non-SSPs ($793, range: $314-$25,412), followed by single-site non-SSPs ($363, range: $98- $870), and then SSPs ($168, range: $74- $977). Approximately 70% of start-up costs at non-SSPs were for initial staff training with 20% of these training costs from travel time to training sites. Approximately 90% of start-up costs at SSPs were for initial staff training, and approximately 30% of these training costs were for travel to training sites. The median cost to train staff at multi-site non-SSPs was $174 per person trained (range: $73 to $212), $145 per person trained (range: $99-$155) for single site non-SSPs, and $90 per person trained (range: $49-$132) for SSPs. The cost per person trained at non-SSPs was higher because staff at non-SSPs were more likely to be medical professionals who had higher salaries and because non-SSPs have more additional start-up costs than SSPs. It was also more costly for program staff to attend offsite training rather than onsite training due to additional costs of travel time. Seven out of 10 non-SSPs developed their own training materials for OEND trainings and three of the five multi-site non-SSPs developed inventory tracking databases to manage inventory over multiple sites, whereas SSPs generally used existing training materials and tracking databases.
Table 2.
New York City OEND Start-up Costs (2017 US Dollars)
| SSPs | Single Site non-SSPs | Multi-Site Non-SSPs | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n=11 | n=5 | N=5 | ||||||||
| Start-up Costs | Average ($) | Median ($) | Range ($) | Average ($) | Median ($) | Range ($) | Average ($) | Median ($) | Range ($) | |
| Staff Training | 1,156 | 789 | 448– 2,811 | 1,492 | 1,600 | 723–2,168 | 11,760 | 1,311 | 522–51,286 | |
| Training Material Development | 196 | 29 | 0– 1,182 | 327 | 0 | 0–1,330 | 524 | 300 | 92–1,093 | |
| Naloxone Tracking Database Development | 5 | 0 | 0– 57 | 59 | 0 | 0–296 | 2,024 | 219 | 0–7,769 | |
| Other Start up costs | 104 | 0 | 0– 1,145 | 0 | 0 | 0–0 | 185 | 0 | 0–923 | |
| Total start-up cost (without overhead) | 1,461 | 874 | 448– 4,504 | 1,878 | 2,039 | 723–2,930 | 14,493 | 6,842 | 2,285–51,446 | |
| Total start-up with overhead * | 1,745 | 1,024 | 522– 5,481 | 2,330 | 2,403 | 821–3,800 | 20,823 | 7,635 | 2,600–76,858 | |
Overhead for SSPs were calculated using actual budget contracts. Overhead for non-SSPs was calculated using 2017 IRS 990 Forms. SSP: Syringe Service Program
Ongoing Program Costs
The median monthly cost (excluding overhead) was highest for multi-site non-SSPs ($2,737, range: $924-$5,017), followed by single-site non-SSPs ($1,959, range $820-$31,502) and then SSPs ($1,579, range: $509- $2,788) (Table 3). Overhead added an additional median monthly cost of $628 for multi-site non-SSPs, $421 for single site non-SSPs, and $334 for SSPs. Four out of eleven SSPs and three out of ten non-SSPs had a higher proportion of their total costs for time-dependent activities (i.e., kit preparation, documentation, inventory management, and reporting) than for variable costs directly related to OEND service delivery. An additional SSP and two non-SSPs spent between 40–50% of their total costs on time-dependent activities.
Table 3.
New York City OEND Ongoing Program Costs (2017 US Dollars)
| SSPs | Single Site Non-SSPs | Multi-Site Non-SSPs | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n=11 | n=5 | N=5 | ||||||||
| Variable Costs | Average ($) | Median ($) | Range ($) | Average ($) | Median ($) | Range ($) | Average ($) | Median ($) | Range ($) | |
| One-on-one training | 185 | 97 | 64–537 | 763 | 327 | 0–1,840 | 456 | 277 | 101–868 | |
| Client Group trainings | 28 | 14 | 0–113 | 93 | 23 | 0–374 | 486 | 240 | 0–1,906 | |
| Organizational trainings | 527 | 324 | 0–1,486 | 388 | 56 | 0–1,550 | 188 | 0 | 0–863 | |
| Community trainings | 207 | 41 | 0– 973 | 5,256 | 30 | 0–25,972 | 99 | 83 | 0–320 | |
| Monthly Variable Cost | 950 | 866 | 83– 2,083 | 6,500 | 1,434 | 393–27,527 | 1,229 | 654 | 101–2,775 | |
| Time Dependent Costs | Average ($) | Median ($) | Range ($) | Average ($) | Median ($) | Range ($) | Average ($) | Median ($) | Range ($) | |
| Refresher Staff Trainings | 73 | 56 | 12–280 | 89 | 14 | 0–393 | 597 | 533 | 15–1,440 | |
| Tracking and Inventory | 58 | 30 | 3–217 | 153 | 131 | 19–277 | 144 | 92 | 63–364 | |
| Documentation and Reporting | 453 | 401 | 10–1,189 | 201 | 190 | 53–337 | 808 | 646 | 311–1,894 | |
| Kit Preparation | 156 | 106 | 0–615 | 79 | 67 | 27–184 | 84 | 82 | 0–140 | |
| Other* | 3 | 0 | 0–38 | 813 | 255 | 0–3,192 | 0 | 0 | 0–0 | |
| Monthly Time Dependent Cost | 744 | 718 | 209–1,752 | 1,336 | 931 | 343–3,976 | 1,632 | 1,925 | 823–2,243 | |
| Total (without overhead) | 1,694 | 1,579 | 509–2,788 | 7,836 | 1,959 | 820–31,502 | 2,861 | 2,737 | 924–5,017 | |
| Total cost with overhead ** | 2,001 | 1,927 | 597– 3,393 | 8,433 | 2,465 | 1,006–33,059 | 3,643 | 3,524 | 1,051–5,645 | |
| Cost per kit (without overhead) | 21 | 19 | 10–59 | 165 | 62 | 36–543 | 27 | 27 | 17–35 | |
| Cost per kit with overhead ** | 29 | 25 | 14–79 | 181 | 76 | 45–570 | 34 | 34 | 25–41 | |
Other costs included yearly promotional video production, ongoing database management and recurring additional materials such as fentanyl testing strips.
Overhead for SSPs were calculated using actual budget contracts. We used the median overhead rate across all SSPs. Overhead for non-SSPs was calculated using 2017 IRS 990 Forms.
SSP: Syringe Service Program
The highest individual cost categories for both SSPs and non-SSPs were group OEND, one-on-one OEND, and documentation and reporting. SSPs had higher costs for delivering organizational or community group trainings because they often responded to training requests outside of their service area, resulting in higher travel costs. One-on-one trainings were more costly for non-SSPs because they were often delivered by higher salaried staff, such as a physician or nurse. Driven by a higher number of kits dispensed per month, SSPs reported spending considerable time (median 5 hours per month, range: 0–29 hours) on preparing the naloxone kits for distribution compared to non-SSPs (median 2 hours per month, range: 0–6 hours). This resulted in a median cost of $106 per month for SSPs (range: $0-$615) and a median cost of $70 per month for non-SSPs (range: $0-$184). Multi-site non SSPs had substantially higher refresher training costs (median $533) compared to SSPs and single site non-SSPs ($56 and $14, respectively) due to larger staff and more medical staff with higher wage rates.
The median ongoing program cost per kit distributed was lowest for SSPs ($19) and was almost double for single site non-SSPs compared with multi-site non-SSPs ($62 vs. $27), consistent with the lower number of kits distributed monthly by single-site versus multi-site non-SSPs. Overhead added an additional median cost of $6 per kit for SSPs, $14 per kit for single site non-SSPs, and $4 per kit for multi-site non-SSPs.
DISCUSSION
We estimated that starting an OEND program in NYC requires a one-time median start up cost of approximately $870 for SSPs and $2,500 for other programs, with 80% of those costs attributed to training staff to provide OEND. SSPs incur a median of $90 per staff member trained and non-SSPs incur a median of $150 per staff member. Training costs were higher for multi-site, large organizations with a larger staff to train. One strategy for reducing these costs for programs is to provide on-site staff training or virtual trainings rather than send staff to offsite trainings. Training is also more costly for organizations staffed primarily with medical professionals for OEND due to higher wage rates, although these professionals may obtain additional benefits from attending OEND trainings given the lack of other harm reduction training in medical education.25 Shifting these trainings to be required in medical school training or offered through continuing medical education in person or virtually may more effectively expand medical professional exposure and shift the cost burden to better resourced organizations. Several large health systems in the US have implemented comprehensive OEND programs that include encouraging medical professionals to provide naloxone prescriptions that can be filled at a pharmacy, implementing electronic health record alerts for OEND, and instituting in-house OEND training as part of medical education.26,27 Funders and health departments may improve overdose prevention efforts within large medical system settings by supporting these activities.
Monthly median costs before overhead for sustaining ongoing OEND activities were approximately $1,600 for SSPs and $2,500 for non-SSPs. The monthly costs for non-SSPs were also driven by the number of sites, with multi-site programs incurring higher costs ($2,700) compared to single-site programs ($2,000). In addition to having a larger staff to train and re-train, OEND programs that have multiple sites spend more time in managing inventory, documentation, and reporting across sites that increase cost. For single-site non-SSPs, inventory management can also be costly because they often do not have the existing inventory management tools and experience that SSPs have. Providing technical assistance to these programs, such as an inventory tracking sheet or guidance in incorporating tracking into electronic health record systems, could help lower their costs. Technical assistance may also improve efficiencies for all OOPPs, given that most programs incurred at least 50% of their total costs for activities other than those directly related to OEND service delivery. Since data collection for this study began, NYC DOHMH expanded their technical assistance and support for programs significantly, such as by pre-packaging blue bags that kits are distributed in, encouraging programs to refer requests for training from far away programs to DOHMH, and providing more support for documentation and reporting.
Our estimated ongoing program cost per kit dispensed, excluding naloxone kit costs, (median $19 per kit for SSPs and $27-$62 per kit for non-SSPs) is higher than other estimates used in US cost-related studies of $10 or $13 per kit dispensed.10,13,15 Our cost estimates exceed previous estimates because it includes administrative and training costs beyond the cost of the time spent providing OEND. Costs previously cited in the literature were estimated based on the type of person who is dispensing naloxone (i.e. lay person, emergency medical services, law enforcement), but only one study focused on the setting (secondary schools) for estimating costs.9 Our setting-specific estimates may help inform future studies that examine the efficiency of distributing naloxone through different organizations and inform funders of the resources required to support various types of OEND programs. Future studies should not only take into account differences in costs among programs, however, but also differences in program effectiveness of reaching individuals who are most likely to observe an overdose.
While our cost estimates include a diversity of community-based OEND program types, this study was limited to one urban setting. These results may not be generalizable to all OOPPs in NYC due to the wide variety of programs, capacity, and experience across programs. Our study was also focused on community-based providers and excluded first responders. Data were collected when new, individual-level reporting requirements had just been initiated for OOPPs receiving free naloxone kits from NYC DOHMH, and therefore the levels of time-dependent costs for administrative activities may represent some inefficiencies associated with the launch of this initiative. The naloxone program in NYC expanded substantially during this time with the number of kits distributed to programs nearly tripling from 2017 to 2019, resulting in more kits dispensed by OOPPs, and coincided with DOHMH scaling up technical assistance to programs in staffing and resources; therefore, the cost per kit estimate range may be biased upwards.
Previous studies have demonstrated that OEND is a cost-effective strategy for preventing overdose fatalities,8,10–15 unless provided in settings where opioid overdoses are very rare.9 In this study, we found that OEND operating costs vary by program type and number of sites. Funders should consider that providing free naloxone to OEND programs without additional funding support does not cover the full cost of operating OEND programs. Given the robust literature on the performance of different types of community-based organizations providing OEND28–31 and the evidence of varying costs by program type in this study, further exploration of cost effectiveness and program efficiency should be considered across different community-based settings.
ACKNOWLEDGEMENTS
We would like to thank all of the opioid overdose prevention programs that participated in the study and provided their time and insightful input. We also thank Chelsea Amato, Gail Goldstein, Lara Maldjian, and Anistla Ruguma of the Bureau of Alcohol and Drug Use Prevention, Care and Treatment team at the NYC Department of Health and Mental Hygiene who provided assistance with collecting data from the programs and helpful feedback on the results.
FUNDING
This research was supported by the National Institute of Drug Abuse (U01DA047408, P30DA040500, T32DA031099). The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
APPENDIX
Appendix
Appendix Table 1.
Cost Category Definitions
| Cost Category | Description |
|---|---|
| Start-up Costs: One-time costs to a program in order to start the OEND program. | |
| Initial OEND Training for OOPP Staff | Initial OEND training of OOPP staff at a “Training of Dispensers” at the DOHMH or HRC and/or initial training onsite by program staff or invited trainer. |
| Training Material Development | Development or translation of overdose education and naloxone training materials from DOHMH or HRC to be more specific to population served or for organizational trainings. |
| Naloxone Tracking Database Development | Development of a database or excel sheet to track and document inventory and dispensing across multiple sites or multiple trainers. |
| Variable Costs: Costs that depend on the number of training encounters with clients. | |
| One-on-one Client Trainings (either onsite or through mobile unit) | Naloxone distribution through a one-on-one encounter with a client either onsite or on a mobile unit. One-on-one trainings can be delivered by peers, naloxone coordinator, physicians etc. |
| Organizational Trainings with Organization Staff | Training delivered to staff of an organization that is at high-risk of witnessing an overdose. |
| Community Trainings | Training delivered to members of a community in an open forum. |
| Time Dependent Costs: Costs that occur on a regularly scheduled basis and support OEND. | |
| Refresher OEND Training for OOPP Staff | Refresher OEND training for OOPP staff that can be delivered annually, or quarterly by site staff or HRC trainers. This can be done as part of a team meeting or one-on-one testing of trainers. |
| Client Group Trainings | Training of clients in a group setting on a regularly scheduled basis (ex. weekly, monthly). It can be part of an existing meeting such as a harm reduction group session. |
| Inventory Management | Time spent ordering kits and blue bags for the kits, preparing blue bags (including naloxone kits, educational materials, breathing masks, alcohol swabs, etc) and tracking inventory. |
| Naloxone Database Management | Time spent managing the naloxone tracking database. |
| Documentation and Reporting | Time spent documenting NRF forms (including scanning NRF forms) and reporting naloxone kit distribution to DOHMH for monthly reports. |
| Refresher OEND Training for OOPP Staff | Refresher OEND training for OOPP staff that can be delivered annually, or quarterly by site staff or HRC trainers. This can be done as part of a team meeting or one-on-one testing of trainers. |
Note: Naloxone=intranasal naloxone kits; OOPP= Opioid Overdose Prevention Programs; OEND= Overdose Education and Naloxone Distribution; DOHMH= Department of Health and Mental Hygiene; HRC= Harm Reduction Coalition; NRF= Naloxone Recipient Forms.
Appendix Table 2.
Roles and Corresponding Wage Rates for New York City Area ($2017)
| Bureau of Labor Statistics (BLS) Job Title | BLS Wage Rate, $ (per hour) | Fringe Benefits* (%) | Total Cost, $ (Wage and Fringe) | |
|---|---|---|---|---|
| Role in SSP Program | ||||
| Program Director | Social and community service managers | 44.68 | 25.98 | 56.29 |
| Naloxone Coordinator | Community health worker | 22.72 | 25.98 | 28.62 |
| Peer | Social and human service assistants | 17.72 | 0.00 | 17.72 |
| Outreach Specialist | Community and social service specialists | 26.30 | 25.98 | 33.13 |
| Case Manager | Community health worker | 22.72 | 25.98 | 28.62 |
| Nurse | Registered nurse | 43.67 | 25.98 | 55.02 |
| Administrative Assistant | Social and human service assistants | 17.72 | 25.98 | 22.32 |
| Role in Non-SSPs | ||||
| Program Director | Social and community service managers | 44.68 | 46.43 | 65.43 |
| Assistant Director | Mental health and substance abuse social workers | 31.34 | 46.43 | 45.89 |
| Peer | Social and human service assistants | 17.72 | 0.00 | 17.72 |
| Driver | Minimum wage | 15.00 | 0.00 | 15.00 |
| Social Worker | Healthcare social workers | 31.53 | 46.43 | 46.17 |
| Database Administrator | Database administrator | 49.45 | 46.43 | 72.41 |
| Medical Director | Physicians and surgeons | 83.39 | 46.43 | 122.11 |
| Psychiatrist | Psychiatrist | 99.51 | 46.43 | 145.72 |
| Office Manager | Secretary and administrative assistant | 20.14 | 46.43 | 29.49 |
| Nurse | Registered nurse | 43.67 | 46.43 | 63.95 |
| Community Health Worker/ Case Manager | Community health worker | 22.72 | 46.43 | 33.27 |
| Residents | Medical resident | 27.50 | 46.43 | 40.27 |
| Pharmacy Coordinator | Pharmacy technician | 16.80 | 46.43 | 24.60 |
Fringe rate for SSPs was calculated using annual naloxone distribution budgets provided by the Department of Health and Mental Hygiene. We used the median fringe rate across all SSPs. Fringe rate for Non-SSPs was from the national civilian fringe rate from the Bureau of Labor Statistics. Part time employees at SSPs were paid through stipends and the majority did not receive fringe benefits. We did not assign fringe benefits to part time employees at Non-SSPs.
Footnotes
DISCLOSURE STATEMENT
The contents of this publication are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies or the U.S. government. The authors have no conflicts of interest to disclose.
REFERENCES
- 1.U.S. Department of Health and Human Services. ASPE Issue Brief: Opioid Abuse in the U.S. and HHS Actions to Address Opioid-Drug Related Overdoses and Deaths. March 26, 2015. [DOI] [PubMed]
- 2.U.S. Department of Health and Human Services (HHS). Facing Addiction in America: the Surgeon General’s Report on Alcohol, Drugs, and Health. . Washington DC: HHS;November 2016. [PubMed] [Google Scholar]
- 3.Rees DI SJ, Argys LM, Dave D, Latshaw J. With a Little Help from My Friends: The Effects of Good Samaritan and Naloxone Access Laws on Opioid-Related Deaths. The Journal of Law and Economics 2019;62(1):1–27. [Google Scholar]
- 4.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ (Clinical research ed). 2013;346:f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fairbairn N, Coffin PO, Walley AY. Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: Challenges and innovations responding to a dynamic epidemic. The International journal on drug policy. 2017;46:172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nolan ML MS, Tuzon E, Paone D. Unintentional Drug Poisoning (Overdose) Deaths in New York City in 2018. New York City Department of Health and Mental Hygiene. 2019;Epi Data Brief(116). [Google Scholar]
- 7.The City of New York Office of the Mayor. HealingNYC: Preventing Overdoses, Saving Lives. 2017; https://www1.nyc.gov/assets/home/downloads/pdf/reports/2017/HealingNYC-Report.pdf. Accessed September 20, 2019. [Google Scholar]
- 8.Bird SM, McAuley A, Perry S, Hunter C. Effectiveness of Scotland’s National Naloxone Programme for reducing opioid-related deaths: a before (2006–10) versus after (2011–13) comparison. Addiction (Abingdon, England). 2016;111(5):883–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cipriano LE, Zaric GS. Cost-effectiveness of naloxone kits in secondary schools. Drug and alcohol dependence. 2018;192:352–361. [DOI] [PubMed] [Google Scholar]
- 10.Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal. Annals of internal medicine. 2013;158(1):1–9. [DOI] [PubMed] [Google Scholar]
- 11.Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal in Russian cities. Journal of medical economics. 2013;16(8):1051–1060. [DOI] [PubMed] [Google Scholar]
- 12.Langham S, Wright A, Kenworthy J, Grieve R, Dunlop WCN. Cost-Effectiveness of Take-Home Naloxone for the Prevention of Overdose Fatalities among Heroin Users in the United Kingdom. Value in health : the journal of the International Society for Pharmacoeconomics and Outcomes Research. 2018;21(4):407–415. [DOI] [PubMed] [Google Scholar]
- 13.Naumann RB, Durrance CP, Ranapurwala SI, et al. Impact of a community-based naloxone distribution program on opioid overdose death rates. Drug and alcohol dependence. 2019;204:107536–107536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Townsend T, Blostein F, Doan T, Madson-Olson S, Galecki P, Hutton DW. Cost-effectiveness analysis of alternative naloxone distribution strategies: First responder and lay distribution in the United States. The International journal on drug policy. 2019. [DOI] [PubMed] [Google Scholar]
- 15.Uyei J, Fiellin DA, Buchelli M, Rodriguez-Santana R, Braithwaite RS. Effects of naloxone distribution alone or in combination with addiction treatment with or without pre-exposure prophylaxis for HIV prevention in people who inject drugs: a cost-effectiveness modelling study. The Lancet Public health. 2017;2(3):e133–e140. [DOI] [PubMed] [Google Scholar]
- 16.Gupta R, Shah ND, Ross JS. The Rising Price of Naloxone - Risks to Efforts to Stem Overdose Deaths. The New England journal of medicine. 2016;375(23):2213–2215. [DOI] [PubMed] [Google Scholar]
- 17.Kerensky T, Walley AY. Opioid overdose prevention and naloxone rescue kits: what we know and what we don’t know. Addiction science & clinical practice. 2017;12(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wheeler E, Jones TS, Gilbert MK, Davidson PJ, Centers for Disease C, Prevention. Opioid Overdose Prevention Programs Providing Naloxone to Laypersons - United States, 2014. MMWR Morbidity and mortality weekly report. 2015;64(23):631–635. [PMC free article] [PubMed] [Google Scholar]
- 19.Winstanley EL, Clark A, Feinberg J, Wilder CM. Barriers to implementation of opioid overdose prevention programs in Ohio. Substance abuse. 2016;37(1):42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.SafeProject. State Naloxone Access Rules and Resources. https://www.safeproject.us/naloxone-awareness-project/state-rules/. Accessed February 14, 2020.
- 21.U.S. Bureau of Labor Statistics. Employer Costs for Employee Compensation Historical Listing. 2017; https://www.bls.gov/ncs/ect/sp/ececqrtn.pdf. Accessed April 1, 2017.
- 22.New York City Department of Health and Mental Hygiene. Naloxone Recipient Form (NRF). 2018; http://clinicalmonster.com/wp-content/uploads/2018/07/English_NRF-OOPP_052018-55054-Activated-VersiForm.pdf. Accessed March 21, 2019.
- 23.Dolatshahi J, Maldjian L, Welch A, Fulmer C, Winkelstein E. Tracking Community Naloxone Dispensing: Part of a Strategy to Reduce Overdose Deaths. Online J Public Health Inform. 2019;11(1):e445. [Google Scholar]
- 24.Teixeira PA, Bresnahan MP, Laraque F, et al. Telementoring of primary care providers delivering hepatitis C treatment in New York City: Results from Project INSPIRE. Learn Health Syst. 2018;2(3):e10056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oldfield BJ, Tetrault JM, Wilkins KM, Edelman EJ, Capurso NA. Opioid overdose prevention education for medical students: Adopting harm reduction into mandatory clerkship curricula. Substance abuse. 2020;41(1):29–34. [DOI] [PubMed] [Google Scholar]
- 26.Devries J, Rafie S, Polston G. Implementing an overdose education and naloxone distribution program in a health system. Journal of the American Pharmacists Association : JAPhA. 2017;57(2S):S154–S160. [DOI] [PubMed] [Google Scholar]
- 27.Oliva EM, Christopher MLD, Wells D, et al. Opioid overdose education and naloxone distribution: Development of the Veterans Health Administration’s national program. Journal of the American Pharmacists Association : JAPhA. 2017;57(2S):S168–S179.e164. [DOI] [PubMed] [Google Scholar]
- 28.Clark AK, Wilder CM, Winstanley EL. A systematic review of community opioid overdose prevention and naloxone distribution programs. Journal of addiction medicine. 2014;8(3):153–163. [DOI] [PubMed] [Google Scholar]
- 29.Mueller SR, Walley AY, Calcaterra SL, Glanz JM, Binswanger IA. A Review of Opioid Overdose Prevention and Naloxone Prescribing: Implications for Translating Community Programming Into Clinical Practice. Substance abuse. 2015;36(2):240–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spelman JF, Peglow S, Schwartz AR, Burgo-Black L, McNamara K, Becker WC. Group Visits for Overdose Education and Naloxone Distribution in Primary Care: A Pilot Quality Improvement Initiative. Pain Med. 2017;18(12):2325–2330. [DOI] [PubMed] [Google Scholar]
- 31.Wenger LD, Showalter D, Lambdin B, et al. Overdose Education and Naloxone Distribution in the San Francisco County Jail. J Correct Health Care. 2019;25(4):394–404. [DOI] [PubMed] [Google Scholar]


