Abstract
Cholangiocarcinoma (CCA) arises from the ductular epithelium of the biliary tree, either within the liver (intrahepatic CCA) or more commonly from the extrahepatic bile ducts (extrahepatic CCA). This disease has a poor prognosis and a growing worldwide prevalence. The poor outcomes of CCA are partially explained by the fact that a final diagnosis is challenging, especially the differential diagnosis between hepatocellular carcinoma and intrahepatic CCA, or distal CCA and pancreatic head adenocarcinoma. Most patients present with an advanced disease, unresectable disease, and there is a lack in non-surgical therapeutic modalities. Not least, there is an acute lack of prognostic biomarkers which further complicates disease management. Therefore, there is a dire need to find alternative diagnostic and follow-up pathways that can lead to an accurate result, either singlehandedly or combined with other methods. In the "-omics" era, this goal can be attained by various means, as it has been successfully demonstrated in other primary tumors. Numerous variants can reach a biomarker status ranging from circulating nucleic acids to proteins, metabolites, extracellular vesicles, and ultimately circulating tumor cells. However, given the relatively heterogeneous data, extracting clinical meaning from the inconsequential noise might become a tall task. The current review aims to navigate the nascent waters of the non-invasive approach to CCA and provide an evidence-based input to aid clinical decisions and provide grounds for future research.
Keywords: Cholangiocarcinoma, Biomarker, Proteomics, Metabolomics, Extracellular vesicles, Circulating nucleic acids
Core Tip: The current review paper aims to critically analyze the most recent developments in non-invasive cholangiocarcinoma diagnosis and prognosis. The article takes an in-depth look at the fields of circulating nucleic acids, proteomic and metabolomic-derived biomarkers, extracellular vesicles, and circulating tumor cells in an attempt to outline promising results for future research and clinical use.
INTRODUCTION
Cholangiocarcinoma (CCA) is a malignant tumor arising from the biliary epithelial cells. The latest World Health Organization Classification of Tumors-Digestive System Tumors acknowledges the heterogeneous nature of CCA, emphasizing the importance of tumor localization. In this matter, there are two main types of CCAs: Intrahepatic CCA (iCCA) and extrahepatic CCA (eCCA) [including both: Perihilar CCA (pCCA) and distal (dCCA)], featuring different aspects in etiology, molecular alterations, pathogenesis, behavior, potential diagnostic or prognostic biomarkers and hence a different clinical management[1].
iCCAs represent approximately 10%-15% of liver tumors and the second primary liver malignancy, after hepatocellular carcinoma (HCC)[2], while eCCAs account for 0.5-2 cases/10.000 person-years[3]. Although considered a relatively rare type of cancer, the incidence of CCA is rising in most geographic areas[4]. Both HCC and iCCA, although they are considered different diseases, do share some common risk factors including hepatitis B or C, non-biliary hepatic cirrhosis, alcoholic and non-alcoholic steatohepatitis, or metabolic syndrome. On the other hand, eCCA typically occurs in conditions associated with chronic biliary inflammation, such as primary sclerosing cholangitis, lithiasis, cysts, or liver fluke infections. In most cases, the exact etiology remains difficult to pinpoint[5].
To this point, CCA is notoriously difficult to diagnose. Diagnosing these tumors requires the correlation of clinical, imaging, and, when available, histopathologic data. In terms of treatment, surgical resection with curative intent remains the best option. However, most patients with CCA (approximately 70%) are diagnosed at late stages due to lack of specific symptoms[6]. Mortality rates are high, and thus the prognosis is poor[7], especially in the case of large tumors, satellite nodules, vascular or lymphatic invasion, positive resection margins, or advanced pathological tumor-node-metastasis stages (TNM)[8,9]. For surgically resectable tumors, the 5-year survival rate reaches 20%-30%, but the percentage drops to a bitter 0% for the rest of the cases[10]. After surgery, the recurrence rate is relatively high, reaching from 49% to 70%[11] and relapse occurs early, typically within 2 or 3 years after surgery[8].
These circumstances emphasize the necessity of novel, clinical-suited tools that would serve for early diagnosis, as prognostic indicators or in treatment guidance, such as biomarkers.
Biomarkers were defined by the Food and Drug Administration-National Institute of Health Biomarker Working Group back in 2016 as “a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention, including therapeutic interventions. Molecular, histologic, radiographic, or physiologic characteristics are types of biomarkers.”. While α-fetoprotein (AFP) is the most convenient and non-invasive serum biomarker for detecting HCC, elevated AFP was observed only in approximately 20% of a subgroup of CCA, namely iCCA patients[12].
The charbohydrate antigen 19-9 (CA19-9) is currently used worldwide in clinical practice as a non-specific serum marker for orientation in diagnosing CCA, but it bears a low sensitivity in European patients[13]. In terms of prognosis there are some validated tools that are useful in the clinical practice. These markers are not specific for CCA but rather apply to all human malignancies. Tumor size and differentiation, vascular involvement, lymph node status, margin status and presence of occult metastasis were all shown to be good predictors for overall survival (OS) for both iCCA and eCCA[14].
One option could be the study of tumor tissue in search of novel biomarkers. This strategy appeared to be fruitful, as several tumor tissue-based biomarkers were already identified. Mutations in TP53 and KRAS proto-oncogene are associated with an impaired outcome-lower OS and higher tumor recurrence than other mutations in resected CCA while several other genetic signatures with prognostic potential include epidermal growth factor receptor (EGFR), mucin 1 (MUC1), MUC4, and fascin (FSCN) expression[15]. Moreover, alteration in targetable pathways [e.g., fibroblast growth factor receptor 2 gene (FGFR2) involved in MAP kinase signaling, isocitrate dehydrogenase 1 and 2 (IDH1, IDH2)] were also depicted in CCA patients[16] and currently, several clinical trials are actively recruiting patients. Nevertheless, several microRNAs (miRs) expressions in tissue or deregulated immune responses [expression levels of cytotoxic T-lymphocyte antigen 4 (CTLA-4), forkhead box P3 (FOXP3), and programmed death-ligand 1 (PD-L1)] might have predictive capabilities in CCA patients[17,18]. Many other diagnostic and prognostic tissue-derived biomarkers have already been previously described[19].
Unfortunately, biopsy collection for tissue analysis is not an ideal biospecimen for biomarker assessment and translation to clinical practice. Although it offers absolute insights into tumor biology, the collection procedure presents several caveats and poses the risk of serious clinical complications[20]. As an alternative to tissue biopsy, a much more reliable biospecimen, already implemented in the clinical practice with several advantages over tissue, is the liquid biopsy (blood). Serum, plasma, or urine, collected non-invasively using well-established low-cost techniques are considered "ideal fluids" in biomarker research. Moreover, liquid biopsy encloses molecules from the whole body, and a single sample can offer a wide range of information and is enough for multiple measurements.
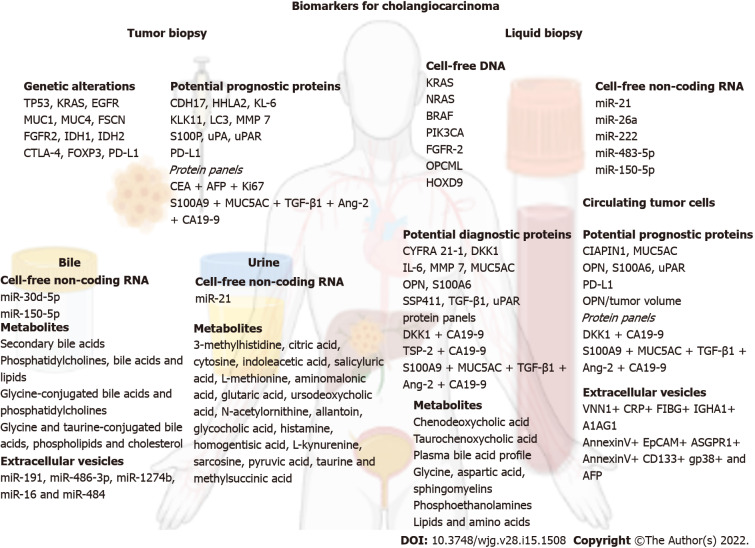
The current review aims to explore the nascent waters of the non-invasive biomarkers reported for CCA by taking an in-depth look at the fields of circulating nucleic acids, proteomic and metabolomic-derived biomarkers, extracellular vesicles, and circulating tumor cells (Figure 1) and provide an evidence-based input which could provide grounds for future research to pave the way for prospective validation and translation into the clinical practice of novel biomarkers. In this review the term CCA will make reference to all types of CCA, while the terms iCCA, hCCA, pCCA, and dCCA will stand for intrahepatic, hilar, perihilar and distal CCA, respectively.
Figure 1.
An overview on the biomarkers for cholangiocarcinoma. Created with biorender.com. A1AG1: Alpha-1 acid glycoprotein; AFP: Alpha fetoprotein; Ang-2: Angiopoietin-2; ASGPR1: Asialoglycoprotein receptor 1; CA19-9: Charbohydrate antigen 19-9; CDH17: Cadherin-17; CEA: Carcinoembryonic antigen; CIAPIN1: Cytokine-induced apoptosis inhibitor 1; CRP: C-reactive protein; CTLA-4: Cytotoxic T-lymphocyte antigen 4; CYFRA 21-1: Cytokeratin 19 fragment; DKK1: Dickkopf-1; EGFR: Epidermal growth factor receptor; EpCAM: Epithelial cell adhesion molecule; FGFR2: Fibroblast growth factor receptor 2; FIBG: Fibrinogen gamma chain; FOXP3: Forkhead box P3; FSCN: Fascin; HHLA2: Human endogenous retrovirus-H long terminal repeat-associating protein 2; IDH1: Isocitrate dehydrogenase 1; IDH2: Isocitrate dehydrogenase 2; IGHA1: Immunoglobulin heavy constant alpha 1; IL-6: Interleukin 6; Ki67: Proliferation marker protein Ki67; KL-6: Krebs von den Lungen 6; KLK11: Kallikrein related peptidase 11; LC3: Microtubule-associated protein 1A/1B-light chain 3; MMP-7: Metalloproteinase 7; MUC1: Mucin 1; MUC4: Mucin 4; MUC5AC: Mucin 5AC; OPN: Osteopontin; PD-L1: Programmed death-ligand 1; S100A6: S100 calcium-binding protein A6; S100A9: S100 calcium-binding protein A9; S100P: Tissue protein S100P; SSP411: Spermatogenesis-associated protein 20; TGF-β1: Transforming growth factor-β1; TSP-2: Thrombospondin-2; uPA: Urokinase-type plasminogen activator; uPAR: Urokinase-type plasminogen activator receptor; VNN1: Pantetheinase.
CIRCULATING NUCLEIC ACIDS
Circulating nucleic acids represent snippets of genetic material, either DNA (cell-free DNA–cfDNA) or RNA (usually miR), reaching various fluid compartments (serum, urine, bile) through active cellular export or following cell death. The road from bench to bedside for circulating nucleic acids has taken a relatively long time and has not quite reached the point of clinical applicability in cancer diagnosis. However, more than four decades have passed between the initial proof-of-concept[21] and present-day genome-wide cfDNA mutational integration[22]. The world of cfDNA and miRs seems to be emerging more promising than ever, as the highly effervescent field has started to deliver on the early expectations. Moreover, CCA might provide a unique setting for the method to flourish: A conventional diagnostic challenge, sometimes a hard to biopsy tumor, all while having a relatively underdeveloped therapeutic arsenal.
CfDNA–the mutational fingerprint
The analysis of circulating cfDNA can provide a quick, complete, and non-invasive mutational profile of any tumor, by amplifying each mutation encountered throughout the tumor burden. The method reflects the entirety of mutations, thus not being the subject of selection bias in the case of heterogeneous cancers. More specifically, tissue samples can provide the mutational palette only for the available specimen. Therefore, the genetic fingerprint of a tumor might be incomplete, as metastases or distant regions of a tumor might have additional alterations. Consequently, cfDNA provides (at least in principle) a better understanding of the disease, with a substantial impact in disease management, from diagnostics to guide therapeutic choices.
This concept has been recently validated for CCA, using plasma samples of patients with fully characterized mutation status[23]. According to the study design, 31 mutations in the KRAS, NRAS, BRAF, and PIK3CA genes were screened using multiplex polymerase chain reaction (PCR) and further quantified. The results were then compared with the mutational profile of the primary tumor, resulting in a perfect match. These results were partially reinforced by the work of a German team that performed the deep sequencing of 15 genes involved in CCA (n = 32), revealing a 74% overall blood-tissue sample concordance and 92% for intrahepatic tumors. Moreover, the patients were followed throughout chemotherapy, during which 63% of the patients had their mutational fingerprint altered[24]. This finding might have particular implications regarding treatment selection, especially in the case of loss of response. There is evidence of resistance to BGJ398, a pan-FGFR inhibitor, due to de novo point mutations in the FGFR-2 kinase domain, revealed by cfDNA analysis[25].
Another promising subfield of cfDNA in CCA is the study of cell-free epigenetics. A recently published report, which analyzed 40 samples of each patient group, hints towards distinct methylation profiles between benign biliary tract disease (BTD) and CCA. The methylation pattern of opioid-binding protein/cell adhesion molecule (OPCML) and homeobox D9 (HOXD9) had a promising discriminative potential, with an area under the receiver operating characteristic (AUROC) of 0.85 for diagnosing CCA[26].
However, we believe that, to this point, there is a dire need for more data to support these initial findings. Barriers regarding study design: Method synchronization, number of patients included, data heterogeneity, cost, and lack of validation prevent their use in clinical settings, while also preventing the funding of large-scale translational endeavors.
Cell-free non-coding RNA
Research in the past decade has revealed an increasing role of miRs as cancer biomarkers for multiple primary tumors, including CCA[27-31]. There are several qualities that, at least in theory, favor miRs as useful biomarkers: Relative specificity, long-term stability, presence in multiple fluids, as well as relative ease of detection and amplification through ever more accessible PCR techniques[19]. To this point, numerous studies[32-36] have investigated the role of miRs in CCA, some showing substantial promise[37-41]. These studies are briefly analyzed in Table 1. The viability of miRs as biomarkers in CCA was tested in two meta-analyses, each including approximately 500 patients and testing the diagnostic capabilities of the cell-free non-coding RNA method, without focusing on specific miRs. Overall, the results were promising, with an AUROC ranging between 0.88 and 0.90 for CCA detection[42,43].
Table 1.
The role of microRNAs as diagnostic and prognostic biomarkers in cholangiocarcinoma
|
Circulating microRNA
|
Biofluid
|
Comparison
|
Statistics
|
Discriminant specificity
|
Valuable considerations
|
Subjective rating
|
| miR-21 | Increased in serum[27,28]; plasma[34]; urine[35] | iCC (n = 74), HC (n = 74)[27]; CCA (n = 11), HC (n = 9)[28]. iCC (n = 25), HC (n = 7); CCA (n = 22), HC (n = 21) | AUROC vs HC: Serum: 0.91[27]; serum: 0.80[28]; plasma 0.94[34]. Combined miR-21 + miR 192. Urine: 0.85[35] | LOW. Also increased in HCC[36] and other malignancies[37,38] | Corelates well with tumor stage and survival[39]. Most data support | Useful |
| miR-150-5p | Decreased in serum and bile[40] | CCA (n = 28), PSC (n = 30), HC (n = 50) | Significantly decreased vs HC and PSC[40] association with | LOW. Upregulation suppresses tumor progression in colorectal cancer[41] | Appears to correlate with tumor staging. Added value of the CA19-9 combination. Contradictory findings: Report of being upregulated in iCCA (AUROC: 0.76)[27] | Debatable |
| miR-26a | Increased in serum[29] | CCA (n = 66), HC (n = 66) | AUROC vs HC: 0.90[29] | Moderate involved in HCC[30] | Correlates well with tumor stage, metastases, differentiation, and survival. Reliable decrease following curative surgery[29] | Promising |
| miR-30d-5p | Increased in bile[31] | CCA (n = 48), benign BTD (n = 58) | AUROC vs benign biliary obstruction 0.730[31] | Moderate downregulated in gastric cancer[32] | Increased sensitivity and specificity compared to CA19-9 | Debatable |
| miR-222; miR-483-5p | Increased in serum[33] | CCA (n = 70), PSC (n = 70), HC (n = 70) | AUROC vs PSC; miR-222: 0.71; miR-483-5p: 0.70 combined miR-222 and 483-5p: 0.74[33] | No evidence of overlap with other cancers | Might be useful for monitoring patients with PSC | Promising |
AUROC: Area under a receiver operating characteristic; CA19-9: Carcinoembrionic antigen 19-9; CCA: Cholangiocarcinoma; HC: Healthy controls; HCC: Hepatocellular carcinoma; iCCA: Intrahepatic cholangiocarcinoma; miRs: Micro RNAs; PSC: Primary sclerosing cholangitis.
However, there are some nuances in the study of miRs, which are worth addressing since the clinical future of the method might be at stake. Of critical relevance is the problem of specificity. Most biomarkers fare relatively well against healthy controls (HC), which is helpful for initial validation, yet far from desirable in a clinical scenario where the setting is less straightforward. This issue has been partially addressed in some study designs by comparisons with other benign BTD conditions, probably the most relevant being primary sclerosing cholangitis (PSC), which shares a common natural history pathway with CCA. However, in such conditions, the specificity and AUROCs tend to drop at least by 0.10-0.20 (as shown in Table 1). Consequently, their diagnostic biomarker value remains only slightly above the threshold for utility in the clinical scenario where the discriminative capabilities were most sought after. Moreover, there is the issue of overlapping with other cancers, which might further complicate the matter. In response, some designs have tried to implement a panel of up to eight miRs to generate distinct profiles depending on CCA subtypes (n = 14) and tumor progression[44].
The use of circulating nucleic acids in CCA diagnosis and prognosis is undoubtedly promising. Nevertheless, the field is still nascent, and most of the data come from studies with heterogeneous designs, most of which are proof-of-concept. Therefore, a potential research direction might be to stimulate reproducibility instead of novelty to provide the grounds for a quicker clinical application.
PROTEINS
Protein-based biomarkers in the clinical practice
Proteomics is a rapidly growing field of biomedical research in the postgenomic era, given the ever-expanding role of personalized medicine. Proteome-based biomarker studies target proteins that could serve as agents to fit a patient's molecular profile in the clinical practice for diagnostic, prognostic, and predictive molecules, their levels being measured from serum samples usually by ELISA.
There are three protein-based biomarkers currently used in the clinical practice towards assisting CCA diagnosis and prognosis: CA19-9 and CA125, and carcinoembryonic antigen (CEA)[45,46].
CA19-9 is a circulating high molecular weight glycoprotein produced by the biliary duct and pancreatic cells and secreted by the gastric and colonic epithelia. Up to 7% of the general population is not producing CA19-9 because of blood cell Lewis antigen deficiency. For CCA, CA19-9 is by far the most frequently used biomarker. Concerning CCA diagnosis, CA19-9 showed a somewhat limited diagnostic accuracy, with following performances: Sensitivity: 72% and specificity: 84%[13]. Hence its promise resides in assessing CCA prognosis. As recently reviewed by Lang et al[45] CA19-9 appears to be an independent prognostic biomarker associated with treatment outcome, as elevated CA19-9 serum levels pre- and postoperatively after systemic therapy show impaired OS. Nevertheless, several factors hamper CA19-9 use as a unique CCA prognostic biomarker[47], thus making its clinical use tumor-associated rather than tumor-specific.
Also known as MUC16, CA125 is the largest membrane-associated mucin, which is also, a glycoprotein. Being a well-known biomarker, CA125 is primary used for the ovarian cancer clinical management[48]. CA125 showed incipient potential diagnostic and prognostic value towards clinical management of CCA[45]. However, CA125 proves its predictive power only in combination with other biomarkers, such as CA19-9, CAE and AFP.
Being produced by the gastrointestinal tissue during fetal development, CEA is a cell surface glycoprotein and functions as an intracellular adhesion molecule. In clinical practice, CEA is extensively used in colorectal cancer monitoring[49]. CEA proved its potential value as a diagnostic biomarker, with rages of sensitivity reported between 40% and 79%, and specificity between 48% and 90%. CEA was also reported as a prognostic indicator for CCA, with expanded predictive capabilities in several biomarker combinations, such as with CA19-9[45].
The three glycoproteins are the most used biomarkers in the clinical management of CCA, and their role is to assist rather than provide a definite diagnostic or prognostic statement. Various other protein-based biomarker candidates reported as single molecules, combined with CA19-9 or as biomarker panels, have been spotlighted in several CCA studies. Towards identifying the potential biomarkers, several approaches have been used. With respect to the study design, CCA patient samples have been compared to (1) Only HC; (2) Only to benign BTD; (3) To benign BTD and HC; and (4) To other disease related conditions and HC. Other studies were interested only in searching biomarkers for iCCA and only one approach was headed towards subtypes of CCA, such as perihilar iCCA, hCCA, and eCCA. While the biospecimens are limited to serum and tissue, and the methods to ELISA or immunohistochemistry, the number of samples included appears to be very heterogenous, ranging from around 20 to up to over 200. The proteins associated with favorable diagnostic and with poor prognostic, potential protein-based biomarkers, are desciphered in Tables 2 and 3.
Table 2.
Proteins associated with favorable cholangiocarcinoma diagnostic potential
|
Protein
|
Comparison
|
SEN (%)
|
SPE (%)
|
AUC
|
Ref.
|
| Tissue | |||||
| CYFRA 21-1 | iCCA (n = 217) vs HC (n = 514) meta-analysis | 81.0 | 86.0 | 0.904 | [58] |
| DKK1 | iCCA (n = 37) vs HC (n = 50) | 75.7 | 100.0 | 0.872 | [52] |
| DKK1 + CA19-9 | iCCA(n = 79) vs HC (n = 160) | 74.7 | 56.3 | 0.793 | [60] |
| IL-6 | CCA (n = 26), HCC (n = 26) and HC (n = 23) | 73.0 | 92.0 | 0.875 | [53] |
| MMP-7 | CCA (n = 44) vs benign BTD (n = 36) | 76.3 | 46.8 | 0.730 | [56] |
| CCA (n = 59) vs benign BTD (n = 128) | 75.0 | 78.0 | 0.840 | [57] | |
| MUC5AC | CCA (n = 49), benign BTD (n = 23), HC (n = 16) | 71.0 | 94.7 | 0.909 | [55] |
| OPN | CCA (n = 107) vs HC (n = 55) | 87.5 | 100.0 | 0.964 | [50] |
| S100A6 | CCA (n = 112) vs HC (n = 42) | 86.2 | 90.9 | 0.909 | [51] |
| SSP411 | CCA (n = 30), benign BTD (n = 13) and HC (n = 23) | 90.0 | 83.3 | 0.913 | [54] |
| TGF-β1 | CCA (n = 45), other disease conditions related inflammation (n = 25) and HC (n = 45) | 71.1 | 68.9 | 0.668 | [78] |
| TSP-2 + CA19-9 | dCCA (n = 51), pancreatic ductal adenocarcinoma (n = 52), benign pancreatic diseases (n = 27) and HC (n = 52) | 79.0 | 96.0 | 0.920 | [61] |
| uPAR | CCA (n = 118), and HC (n = 76) | 95.3 | 89.7 | 0.969 | [59] |
| Biomarker panel: S100A9, MUC5AC, TGF-β1, Ang-2, and CA19-9 | CCA (n = 40), non-CCA (n = 40) and HC (n = 40) | 95.0 | 90.0 | 0.975 | [62] |
AUC: Area under the curve; BTD: Biliary tract disease; CCA: Cholangiocarcinoma; dCCA: Distal CCA; HC: Healthy controls; HCC: Hepatocellular carcinoma; iCCA: Intrahepatic cholangiocarcinoma; SEN: Sensitivity; SPE: Specificity; CYFRA 21-1: Cytokeratin 19 fragment; DKK1: Dickkopf 1; IL-6: Interleukin 6; MMP-7: Metalloproteinase 7; MUC5AC: Mucin 5AC; OPN: Osteopontin; S100A6: S100 calcium binding protein A6; SSP411: Spermatogenesis-associated protein 20; TGF-β1: Transforming growth factor-β1; TSP-2: Thrombospondin-2; uPAR: Urokinase-type plasminogen activator receptor; S100A9: S100 calcium binding protein A9; Ang-2: Angiopoietin-2.
Table 3.
Proteins associated with poor outcome in cholangiocarcinoma patients
|
Protein
|
Comparison
|
Outcome
|
Ref.
|
| Tissue | |||
| CDH17 | CCA (n = 180) | High CDH17 was associated with a worse OS and recurrence-free survival | [64] |
| HHLA2 | iCCA (n = 218) meta-analysis | High HHLA2 expression was significantly associated with shorter OS | [74] |
| KL-6 | CCA (n = 21), cHCC-CCA (n = 12), HCC (n = 78) | A key molecule for tumor cell adhesion and invasion | [63] |
| KLK11 | CCA and adjacent normal tissues (n = 18) | OS of CCA patients with a high expression of KLK11 was significantly shorter than those with a low expression of KLK11 (414 d vs 809 d, respectively; P = 0.048) | [65] |
| LC3 | cHCC-CC (n = 40) | The 5-yr OS and disease-free survival rates were 61.2% and 74.6% in high LC3 expression patients and 0% and 0% in those with low LC3 expression | [70] |
| MMP-7 | Perihilar iCCA, hCCA, and eCCA (n = 66) | Patients with moderate to marked expression of MMP-7 had a significantly poorer prognosis, as compared to those with negative to focal expression | [72] |
| iCCA (n = 35) | The 5-yr survival rates of MMP-7(+) and MMP-7(−) patients were 72.7% and 18.3%, respectively | [73] | |
| PD-L1 | CCA (n = 2012) meta-analysis | Overexpression of PD-L1 was significantly associated with worse OS | [17] |
| S100P | CCA (n = 1925) meta-analysis | S100 calcium binding protein P overexpression was associated with poor OS | [69] |
| uPa | iCCA (n = 174) | High uPa expression was correlated with lymphatic invasion and metastasis of CCA patients | [71] |
| uPAR | CCA (n = 108) vs normal tissue (n = 108) | The median OS was 890 d for patients with uPAR positive vs 1.321 d for patients with uPAR negative | [59] |
| Biomarker panel: CEA, AFP, and Ki67 | iCCA (n = 92) | higher AFP, CEA, and Ki67, as well as more advanced TNM staging were associated with worse OS | [75] |
| Serum | |||
| CIAPIN1 | CCA (n = 159) vs HC (n = 93) | Higher CIAPIN1 level was significantly associated with shorter OS time | [66] |
| DKK1 + CA19-9 | iCCA (n = 79) vs HC (n = 160) | DKK-1 in combination with CA19-9 showed a better diagnostic performance than CA19-9 alone; low DKK-1 and CA19-9 were associated with longer OS | [60] |
| MUC5AC | CCA (n = 49), benign BTD (n = 23), HC (n = 16) | High MUC5AC level was related to a worse prognosis compared with patients with lower levels, with 3-yr survival rates of 21.5% and 59.3%, respectively | [55] |
| OPN | CCA (n = 107) vs HC (n = 55) | Poor postoperative survival | [50] |
| OPN/tumor volume | iCCA (n = 124) | Low circulating OPN per tumor volume was associated with shorter OS and disease-free survival | [77] |
| PD-L1 | CCA (n = 73) vs HC (n = 42) | Low PD-L1 levels displayed a strong trend towards an impaired prognosis | [76] |
| S100A6 | CCA (n = 112) vs HC (n = 42) | S100A6 potential was like those of the clinically established biomarkers CEA and CA19-9 | [67] |
| uPAR | CCA (n = 168) | Baseline level of uPAR was an independent predictor of survival; a high level of uPAR after 2 cycles of chemotherapy was associated with poor survival | [68] |
| CCA (n = 117), HC (n = 76) | Multivariate Cox-regression analysis revealed circulating uPAR levels as an independent prognostic marker following biliary tract cancer resection | [59] | |
| Biomarker panel: S100A9, MUC5AC, TGF-β1, Ang-2, and CA19-9 | CCA (n = 40), and non-CCA patients (n = 40) and HC (n = 40) | TGF-β1 and Ang-2 are predictors of higher TNM stages | [62] |
BTD: Biliary tract disease; CCA: Cholangiocarcinoma; cHCC-CC: Combined hepatocellular carcinoma and CCA; HC: Healthy controls; HCC: Hepatocellular carcinoma; iCCA: Intrahepatic cholangiocarcinoma; OS: Overall survival; CDH17: Cadherin-17; CYFRA 21-1: Cytokeratin 19 fragment; DKK1: Dickkopf 1; IL-6: Interleukin 6; MMP-7: Metalloproteinase 7; MUC5AC: Mucin 5AC; OPN: Osteopontin; S100A6: S100 calcium binding protein A6; SSP411: Spermatogenesis-associated protein 20; TGF-β1: Transforming growth factor-β1; TSP-2: Thrombospondin-2; uPAR: Urokinase-type plasminogen activator receptor; S100A9: S100 calcium binding protein A9; Ang-2: Angiopoietin-2; PD-L1: Programmed death-ligand 1; CIAPIN1: Serum cytokine-induced apoptosis inhibitor 1; AFP: Alpha-feto protein; LC3: Microtubule-associated protein 1A/1B-light chain 3; KLK11: Kallikrein related peptidase 11; KL-6: Mucin KL-6; HHLA2: Human endogenous retrovirus-H long terminal repeat-associating protein 2.
Proteins associated with favorable diagnostic potential in CCA patients
Multiple proteins appeared to have a role in CCA diagnosis, typically showing increased serum levels. These findings were reported in studies using serum as biospecimen and ELISA assays for their absolute quantification (Table 2). Such examples are osteopontin (OPN)[50] and S100 calcium-binding protein A6 (S100A6)[51] which efficiently discriminated between CCA and HC, and dickkopf-1 (DKK1) between iCCA and HC[52]. Studies reporting serum cytokine interleukin 6 (IL-6)[53], spermatogenesis-associated protein 20 (SSP411)[54] and MUC5AC[55] also included groups of metastatic liver cancer, HCC, and benign BTD disease. Metalloproteinase 7 (MMP-7) was assessed only in groups of CCA vs benign BTD[56,57].
After several reports, cytokeratin 19 fragment (CYFRA 21-1) was included in a comprehensive meta-analysis[58] and the pooled diagnostic indices showed a sensitivity of 81% and a specificity of 86% for iCCA diagnosis. More recently, the urokinase-type plasminogen activator receptor (uPAR)[59], reported as a single protein-based biomarker, proved to be a reliable tool for differentiating CCA from HC with sensitivity of 95% and specificity close to 90%, while transforming growth factor-β1 (TGF-β1) appears to help distinguishing CCA from other pro-inflammatory conditions and HC.
Moreover, the combination of MMP-7[57], DKK1[60], thrombospondin-2 (TSP-2)[61] and uPAR[59] assessed together with CA19-9 showed higher values of sensitivity and specificity than the markers measured individually to diagnose CCA patients. Not least, a biomarker panel consisting of five proteins investigated in a decision tree algorithms based study, namely S100A9, MUC5AC, TGF-β1, angiopoietin-2 (Ang-2), and CA19-9, showed to have the greatest diagnostic potential among all mentioned proteins towards CCA vs HC (sensitivity: 95%, specificity: 90%) and towards CCA vs non-CCA (sensitivity: 70%, specificity: 83%) differentiation[62].
Proteins associated with poor outcome in CCA patients
Concerning prognosis, several protein-based potential biomarkers have shown increased levels in CCA, most frequently by employing immunohistochemistry in tissue samples. The serum has also emerged as a biospecimen towards prognostic biomarkers exploration (Table 3). As such, high levels of tissue Krebs von den Lungen 6 (KL-6 mucin)[63], cadherin-17 (CDH17)[64], kallikrein-11[65], uPAR[59] and high levels of serum cytokine-induced apoptosis inhibitor 1 (CIAPIN1)[66], MUC5AC[55], OPN[50], S100A6[67] and uPAR[59,68] were found adverse prognostic factors for CCA patient’s survival. Subjected to meta-analysis, high levels of tissue PD-L1[17] and tissue protein S100P[69] were also proposed as potential prognostic markers of CCA. Out of a protein multimarker panel consisting of serum S100A9, MUC5AC, TGF-β1, Ang-2, and CA19-9, serum levels of TGF-β1 and Ang-2 provided predictive potential for both metastasis and TNM stage prognosis in CCA patients[62].
For patients with tumors of combined HCC and CCA (cHCC-CC), microtubule-associated protein 1A/1B-light chain 3 (LC3) increased tissue expression was found to predict postresection OS (5-year OS, 61.2%) and disease-free survival (74.6%)[70].
iCCA prognostic biomarkers were also of particular interest in some studies. High tissue levels of urokinase-type plasminogen activator (uPa)[71], MMP-7[72,73] and human endogenous retrovirus-H long terminal repeat-associating protein 2 (HHLA2), reported from a recent meta-analysis[74], were associated with adverse outcomes in iCCA patients. High serum DKK1 in combination with CA19-9 was independently associated with shorter survival[60]. Recently, Qiang et al[75] found that the biomarker panel consisting of CEA, AFP, and proliferation marker protein Ki67 are significant prognostic indicators in iCC patients.
Proteins that showed decreased levels in association with CCA were PD-L1 and OPN. The lack of serum PD-L1 level normalization after surgery seems to identify patients at high risk for recurrence and adverse outcomes[76]. By applying an innovative approach, decreased serum OPN per tumor volume was associated with invasive behavior and early recurrence of iCCA[77].
There is vast evidence of protein-based biomarkers reported in CCA diagnosis and prognosis, but only CA19-9 and CEA are currently employed in routine clinical practice. The data above reveals exciting results for new potential protein-based biomarkers used as single molecules (e.g., uPAR) or biomarker panels (e.g., S100A9, MUC5AC, TGF-β1, Ang-2, and CA19-9) for CCA.
Extrapolating from proteomic-derived biomarker studies in other diseases, it appears that using multiple-molecule panels instead of individual proteins provides better predictive results and shows more promise for a translation to clinical practice. However, future validation studies on large patient cohorts are needed towards establishing the real applicability and the subsequent translation of these biomarkers into the clinical practice.
METABOLITES
Metabolomics, another branch of omics-derived technologies, analyzes low molecular weight metabolites (< 1500 Da) in various biological fluids. One of the hallmarks of cancer is energy metabolism reprogramming. In order to promote cancer survival and subsequently cancer growth, there are several shifts in normal metabolic pathways (e.g., a higher glucose uptake rate and an increase in lactate production)[78,79]. A different or "wiser" use of metabolic pathways in cancer cells leads to the release of several metabolites in various body fluids, providing an opportunity for diagnosis and monitoring. Metabolic profiling is, therefore, a promising approach for the identification of potential biomarkers in several cancers, including CCA[80]. To date, several studies have investigated the potential of metabolomics in CCA diagnosis or prognosis in various body fluids.
We believe that investigating the molecular composition of the bile could provide more crucial information than other fluids due to at least two reasons. Firstly, it could unravel mechanistic information regarding the pathological alteration of the biliary epithelium. Secondly, it could identify biomarkers from nearby tumor cells, markers that might or might not be present in other body fluids. Several metabolite profiling studies of human bile have been performed over the past few years. One such study reported a reduction in the proportion of secondary bile acids in patients with CCA compared to those with biliary tract stones and healthy individuals[81]. Another study showed that changes in phosphatidylcholines, bile acids, and lipids could discriminate CCA from PSC and benign BTD (sensitivity: 88.9%; specificity: 78.1%)[82]. When comparing inoperable eCCA to non-malignant, non-cholestatic biliary diseases (including PSC), CCA was associated with increased levels of glycine-conjugated bile acids and phosphatidylcholines. Moreover, constructed models could discriminate CCA patients from those with non-malignant biliary diseases with an 80% sensitivity and 95% specificity: 95%[83].
Unfortunately, the impact of cholestasis on the metabolic profile was not investigated, and it is difficult to reach a solid conclusion. In contrast, the analysis of metabolites in patients with CCA, HCC, and non-malignant liver diseases showed a decrease in glycine and taurine-conjugated bile acids, phospholipids, and cholesterol in patients with CCA compared to control groups but only to a certain extent when compared to HCC[84].
In theory, if one biomarker is detected and validated in bile, it might provide sufficient grounds further to test it in more accessible and less invasive fluids (e.g., serum, urine, plasma). Nevertheless, metabolomics studies can also be performed directly on serum, plasma, or urine. Using serum, one study from the United Kingdom failed to show any differences between profiles from patients with benign biliary strictures and CCA[85]. In contrast, one study from China showed that two bile acids, chenodeoxycholic acid (CDCA) and taurochenoxycholic acid (TCDCA) (from plasma), had higher sensitivity and specificity than CA19-9 for CCA vs benign bile duct disease and CCA vs HC[86]. Furthermore, a study from Europe (Italy), using an artificial intelligence approach, found a plasma bile acid profile that could discriminate between CCA and benign BTD with an accuracy of 86.4%[87]. However, all the beforementioned studies could not offer more answers to some of the most critical clinical dilemmas when caring for patients with liver cancer.
In the liver cancer community, there are at least two primary clinical necessities. The first clinical dilemma is probably the most common scenario: One patient with advanced liver disease and focal liver lesions: Is it cancer? If the answer is yes, is it HCC or iCCA? In this setting, one study (on serum) has shown that the development of an algorithm combining glycine, aspartic acid, sphingomyelin (SM) (42:3), and SM (43:2) permitted accurate discrimination between HCC and iCCA with a sensitivity of 75% and specificity of 90%. In the same study, another algorithm discriminated PSC from iCCA with a sensitivity of 100% and specificity of 70%. Of note, these results were further validated in an independent cohort[88]. A similar finding was also reported in one study from China. A panel of four metabolites {PE (19:0/0:0), PE [18:2 (9Z, 12Z)/0:0], PC (14:0/0:0) and PC (18:0/0:0)} attained a diagnostic accuracy (HCC vs iCCA) of 99.7%[89].
The second clinical dilemma is: One patient with distal bile duct obstruction: Is it cancer? dCCA or pancreatic ductal adenocarcinoma (PDAC)? A combination of serum levels of nine metabolites [acylcarnitine AC (16:0), ceramide Cer (d18:1/24:0), phosphatidylcholines PC (20:0/0:0) and PC (O-16:0/20:3), lysophosphatidylcholines PC (20:0/0:0) and PC (0:0/20:0), lysophosphatidylethanolamine PE (P-18:2/0:0), and sphingomyelins SM (d18:2/22:0) and SM (d18:2/23:0) and CA 19-9] could discriminate between dCCA and PDAC with a sensitivity of 55.9% and specificity of 89.5%[90]. Metabolic profiling of urine in patients with CCA was also applied, showing some metabolic differences in the urine of CCA compared to controls. As such, a urine metabolomic panel consisting of 3-methylhistidine, citric acid, cytosine, indoleacetic acid, salicyluric acid, L-methionine, aminomalonic acid, glutaric acid, ursodeoxycholic acid, N-acetylornithine, allantoin, glycocholic acid, histamine, homogentisic acid, L-kynurenine, sarcosine, pyruvic acid, taurine and methylsuccinic acid were identified as potential biomarkers for primary extrahepatic CCA[91]. Nevertheless, in terms of prognosis, only a few studies have shown the potential of metabolites to predict recurrence or OS[91,92].
The road ahead is still long for metabolomics in CCA. Metabolome studies in CCA have just begun, and some promising metabolites have already been identified. However, a shift from bench to bedside is not expected to appear in the next few years. First, identifying a specific metabolite with diagnostic or prognostic properties is a challenging goal due to the presence of many confounding factors (e.g., age, gender, diet, underlying liver disease, concomitant disease, drugs, and others). Secondly, the results from untargeted metabolomics might be different from targeted metabolomics, according to at least one recent metabolomics study, investigating plasma fetal bile acids towards assessing liver cirrhosis severity[93]. Not least, the reproducibility of many of these studies is a genuine concern (due to multiple analytical platforms, different sample preparation protocols), and standardized procedures are urgently needed.
EXTRACELLULAR VESICLES
In terms of minimally invasive biomarkers, EVs are the "new kids on the market". They hold great promise in the diagnosis and prognosis of cancer. EVs are encountered in all body fluids including blood[94], urine[95] and bile[96]. According to their size and biogenesis there are two classes: (1) Large EVs [also called microvesicles (MVs)] roughly ranging from 100 to 1000 nm in size, which directly bud from the plasma membrane of their parental cell; and (2) Small EVs (also called exosomes) are considerably smaller (below 100 nm) and originate from accumulated intraluminal vesicles within the endomembranous system, forming so-called multivesicular bodies[97].
The function of EVs depends on the type and content (e.g., lipids, proteins, nucleic acids) of their parent cells. They orchestrate many of the processes described by Hanahan et al[98] as "Hallmarks of Cancer"[98] either via paracrine signaling or horizontal transfer of bioactive agents[99]. In the initial steps of cancer genesis, EVs (released by cancer cells) appear to be responsible for the differentiation of mesenchymal stem cells into fibroblasts, contributing to stroma generation ant thus preparing their tumor niche[100]. Furthermore, EVs could transport miR species from human CCA cells to cancer-associated fibroblasts, a communication between cancer cells and the cancer microenvironment responsible for tumor growth and, later on, CCA cells-derived EVs can transfer oncogenes to normal cholangiocytes, increasing their migration and invasive potential [via increasing the expression of beta-catenin (CTNNB1) and decreasing the expression of E-cadherin (CDH1)], hence preparing the final processes of carcinogenesis: Tumor invasion and metastasis[101].
Some studies have already revealed the great potential of EVs content or surface markers in terms of diagnosis. Proteomic profiling of serum EVs has identified a panel of five proteins that could assist CCA diagnosis. The study design included CCA (n = 43), PSC (n = 30), HCC (n = 29) patients and HC (n = 32). As such, pantetheinase (VNN1), C-reactive protein, fibrinogen gamma chain (FIBG), immunoglobulin heavy constant alpha 1 (IGHA1) and alpha-1 acid glycoprotein (A1AG1) showed to have an increased concentration in serum EVs of CCA compared to all PSC, HCC and HC. Moreover, a panel of three EVs proteins, namely ficolin-2 (FCN2), inter-alpha-trypsin inhibitor heavy chain H4 (ITIH4), and FIBG showed to be able to discriminate between early-stage CCA and PSC patients with an AUC > 0.88[102].
A major challenge nowadays is the differential diagnosis between HCC and iCCA or between dCCA and PDAC. More often, the final diagnosis (HCC vs cCCA) in clinical practice is based on liver biopsy. In terms of EVs surface antigens, one study enrolling 172 patients with liver cancer (HCC or CCA), 54 with cirrhosis and no liver neoplasia, and 202 control subjects, found a combination of tumor-associated microparticles (AnnexinV+ epithelial cell adhesion molecule (EpCAM+) and asialoglycoprotein receptor 1 (ASGPR1+)) could diagnose CCA from healthy individuals and other cancer entities with up to 90% sensitivity. However, it was unable to differentiate between CCA and HCC[103]. Interestingly, later on, the same group in another study including a large set of patients, including 77 CCA, 67 HCC, identified a combination between EVs surface antigens (AnnexinV+ CD44v6, cut-off = 34 number per 103 AnnexinV+ EVs) together with AFP (cut-off = 30 ng/mL) that could discriminate between HCC and CCA (iCCA and eCCA) with both sensitivity and specificity of 100%[104]. Indeed, it is a novel potential diagnostic biomarker that could help clinicians diagnose CCA non-invasively and accurately. Further large multicenter studies are urgently necessary. In search of novel biomarkers for the differential diagnoses between dCCA and PDAC, one study including 50 patients (n = 20 pancreatic cancer, n = dCCA, n = 15 chronic pancreatitis, n = 10 common bile duct obstruction due to biliary stones patients) reported that the concentration of EVs per se in bile and serum could discriminate malignant from non-malignant pancreaticobiliary diseases with 100% sensitivity in bile and 47% in serum[105]. EVs cargo profile could also have diagnosis potential. In particular, a panel of 5 miRs (miR-191, miR-486-3p, miR-1274b, miR-16 and miR-484) isolated from bile EVs showed good diagnostic values for CCA diagnosis compared to non‐malignant biliary diseases (sensitivity: 67%; specificity: 96%)[106].
CIRCULATING TUMOR CELLS
Circulating tumor cells (CTCs) have been evaluated as a diagnostic marker in pancreatic, colorectal, breast or prostate cancer, and are associated with poor survival rates. However, only a handful of studies have assessed their potential in CCAs. CTCs are cancer-derived cells released from a primary solid tumor or local lymphoid reservoirs into the bloodstream, harboring tumor-initiation properties, and possibly enabling distant metastasis. Even after primary tumor resection, the permanence of viable CTCs in the portal venous blood seems to be a consequence of T-cell suppression by myeloid-derived suppressor cells and CTC-induced apoptosis[107]. Subsequently, CTCs proliferate and cluster, possibly under the influence of cell adhesion molecules such as plakoglobin, leading to tumor growth and immune resistance[107,108].
Identification of CTCs in peripheral blood relies on their overexpression of EpCAM. It has been performed using immunocytochemistry, reverse transcriptase-PCR, flow cytometry, or an enzyme-linked immunosorbent spot assay. The most used assay is CellSearch™, which uses ferrofluid nanoparticles with antibodies that target EpCAM, which is expressed in various of human epithelial tissues, carcinomas, and stem cells, and is involved in cell signaling, migration, proliferation, and differentiation[109-111]. In a study of 26 CCA patients, targeting CTCs using antibodies against EpCAM, DAPI, cytokeratin 8, 18, and/or 19, Al Ustwani et al[112] showed that 25% of patients with CCA had a significant amount of CTCs (≥ 2/7.5 mL of blood). Similar results were reported in another study, where out of 95 CCA patients, 24% had a count of two cells or higher per 7.5 mL blood, while 22% had a count of one cell, and the remainder of 54% no detectable cells[113]. Since CTCs seem to be relatively rare in peripheral blood, their potential as a diagnostic marker might be more evident in patients with metastatic disease and less in early tumors.
CTCs are also seemingly associated with more aggressive tumors, as patients with no CTCs in their blood sample had the best survival rate. In contrast, the presence of two or more CTCs was strongly associated with worse OS (median 18.1 mo vs 8.7 mo)[113]. However, their presence does not seem to predict treatment outcome, as evidenced in the ABC-03 trial[113,114].
The high degree of variability in detection rates might be explained by suboptimal EpCAM levels for detection, loss of epithelial surface antigens, or epithelial-mesenchymal transition[112,115,116]. To overcome these shortcomings, a novel glycosaminoglycan-SCH45-probe on a microfluidic platform has been employed to isolate CCA CTCs by combining multiple-capture approaches in a shorter period and using lower blood volumes compared to the traditional method. Using EpCAM as a conventional protein biomarker, the authors showed, by analyzing peripheral blood of 65 metastatic CCA patients, that CTCs could be detected in all advanced or metastatic CCA, suggesting that CTCs may maximize the predictive performance of liquid biopsies if the proper diagnostic tool is used[117]. Reduzzi et al[118] assessed an alternative to improving detection rates in a prospective study of 21 patients with advanced-stage biliary tract cancer. Using non-conventional CTCs lacking epithelial and leukocyte markers, but presenting aberrant genomes, the detection rate increased from 19% to 83%.
CONCLUSION
A non-invasive approach towards diagnosis and prognosis is the path forward in CCA, a type of cancer that sometimes appears to be hiding in plain sight. The previously discussed methods aim to provide the necessary leap forward towards a personalized approach and might allow for a refined characterization of the disease. However, most available reports are deeply heterogeneous, study protocols are not harmonized, and the number of included patients is inconsistent. These caveats appear to be the primary reasons for the gap between the wide range of cancer biomarkers that appear to be effective in individual studies and the relatively low number of biomarkers ready to be translated into the clinic. Consequently, the most challenging task in the short term might be not to find new molecules and pathways but rather to validate or infirm the role of current methods to shorten the bench to bedside gap.
Footnotes
Conflict-of-interest statement: All authors have no conflict of interest to declare.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: October 31, 2021
First decision: November 29, 2021
Article in press: March 6, 2022
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Romania
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gao W, China; Lang SA, Germany; Luo XZ, China; Mavroeidis VK, United Kingdom S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
Contributor Information
Lavinia-Patricia Mocan, Department of Histology, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania.
Maria Ilieș, Department of Proteomics and Metabolomics, MedFUTURE Research Center for Advanced Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400349, Romania. ilies.maria@umfcluj.ro.
Carmen Stanca Melincovici, Department of Histology, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania.
Mihaela Spârchez, 2nd Pediatrics Department, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania.
Rareș Crăciun, 3rd Medical Department, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania; Department of Gastroenterology, "Prof. dr. Octavian Fodor" Institute for Gastroenterology and Hepatology, Cluj-Napoca 400162, Romania.
Iuliana Nenu, 3rd Medical Department, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania; Department of Gastroenterology, "Prof. dr. Octavian Fodor" Institute for Gastroenterology and Hepatology, Cluj-Napoca 400162, Romania.
Adelina Horhat, 3rd Medical Department, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania; Department of Gastroenterology, "Prof. dr. Octavian Fodor" Institute for Gastroenterology and Hepatology, Cluj-Napoca 400162, Romania.
Cristian Tefas, 3rd Medical Department, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania; Department of Gastroenterology, "Prof. dr. Octavian Fodor" Institute for Gastroenterology and Hepatology, Cluj-Napoca 400162, Romania.
Zeno Spârchez, 3rd Medical Department, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania; Department of Gastroenterology, "Prof. dr. Octavian Fodor" Institute for Gastroenterology and Hepatology, Cluj-Napoca 400162, Romania.
Cristina Adela Iuga, Department of Proteomics and Metabolomics, MedFUTURE Research Center for Advanced Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400349, Romania; Department of Pharmaceutical Analysis, Faculty of Pharmacy, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania.
Tudor Mocan, 3rd Medical Department, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania; Department of Gastroenterology, "Prof. dr. Octavian Fodor" Institute for Gastroenterology and Hepatology, Cluj-Napoca 400162, Romania.
Carmen Mihaela Mihu, Department of Histology, Faculty of Medicine, "Iuliu Hațieganu" University of Medicine and Pharmacy, Cluj-Napoca 400012, Romania.
References
- 1.WHO Classification of Tumours Editorial Board. Digestive System Tumours, WHO Classification of Tumours. 5th ed. World Health Organization: IARC Publications, 2019, ISBN 978-92-832-4499-8. [Google Scholar]
- 2.Tyson GL, Ilyas JA, Duan Z, Green LK, Younes M, El-Serag HB, Davila JA. Secular trends in the incidence of cholangiocarcinoma in the USA and the impact of misclassification. Dig Dis Sci. 2014;59:3103–3110. doi: 10.1007/s10620-014-3276-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bridgewater JA, Goodman KA, Kalyan A, Mulcahy MF. Biliary Tract Cancer: Epidemiology, Radiotherapy, and Molecular Profiling. Am Soc Clin Oncol Educ Book. 2016;35:e194–e203. doi: 10.1200/EDBK_160831. [DOI] [PubMed] [Google Scholar]
- 4.Saha SK, Zhu AX, Fuchs CS, Brooks GA. Forty-Year Trends in Cholangiocarcinoma Incidence in the U.S.: Intrahepatic Disease on the Rise. Oncologist. 2016;21:594–599. doi: 10.1634/theoncologist.2015-0446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banales JM, Cardinale V, Carpino G, Marzioni M, Andersen JB, Invernizzi P, Lind GE, Folseraas T, Forbes SJ, Fouassier L, Geier A, Calvisi DF, Mertens JC, Trauner M, Benedetti A, Maroni L, Vaquero J, Macias RI, Raggi C, Perugorria MJ, Gaudio E, Boberg KM, Marin JJ, Alvaro D. Expert consensus document: Cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA) Nat Rev Gastroenterol Hepatol. 2016;13:261–280. doi: 10.1038/nrgastro.2016.51. [DOI] [PubMed] [Google Scholar]
- 6.Forner A, Vidili G, Rengo M, Bujanda L, Ponz-Sarvisé M, Lamarca A. Clinical presentation, diagnosis and staging of cholangiocarcinoma. Liver Int. 2019;39 Suppl 1:98–107. doi: 10.1111/liv.14086. [DOI] [PubMed] [Google Scholar]
- 7.Aishima S, Oda Y. Pathogenesis and classification of intrahepatic cholangiocarcinoma: different characters of perihilar large duct type vs peripheral small duct type. J Hepatobiliary Pancreat Sci. 2015;22:94–100. doi: 10.1002/jhbp.154. [DOI] [PubMed] [Google Scholar]
- 8.Endo I, Gonen M, Yopp AC, Dalal KM, Zhou Q, Klimstra D, D'Angelica M, DeMatteo RP, Fong Y, Schwartz L, Kemeny N, O'Reilly E, Abou-Alfa GK, Shimada H, Blumgart LH, Jarnagin WR. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg. 2008;248:84–96. doi: 10.1097/SLA.0b013e318176c4d3. [DOI] [PubMed] [Google Scholar]
- 9.Jiang BG, Sun LL, Yu WL, Tang ZH, Zong M, Zhang YJ. Retrospective analysis of histopathologic prognostic factors after hepatectomy for intrahepatic cholangiocarcinoma. Cancer J. 2009;15:257–261. doi: 10.1097/PPO.0b013e31819e3312. [DOI] [PubMed] [Google Scholar]
- 10.DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, Choti MA, Yeo CJ, Schulick RD. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245:755–762. doi: 10.1097/01.sla.0000251366.62632.d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, Pawlik TM, Gores GJ. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60:1268–1289. doi: 10.1016/j.jhep.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 12.Liver Cancer Study Group of Japan. Primary liver cancer in Japan. Clinicopathologic features and results of surgical treatment. Ann Surg. 1990;211:277–287. [PMC free article] [PubMed] [Google Scholar]
- 13.Liang B, Zhong L, He Q, Wang S, Pan Z, Wang T, Zhao Y. Diagnostic Accuracy of Serum CA19-9 in Patients with Cholangiocarcinoma: A Systematic Review and Meta-Analysis. Med Sci Monit. 2015;21:3555–3563. doi: 10.12659/MSM.895040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mao ZY, Guo XC, Su D, Wang LJ, Zhang TT, Bai L. Prognostic Factors of Cholangiocarcinoma After Surgical Resection: A Retrospective Study of 293 Patients. Med Sci Monit. 2015;21:2375–2381. doi: 10.12659/MSM.893586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruys AT, Groot Koerkamp B, Wiggers JK, Klümpen HJ, ten Kate FJ, van Gulik TM. Prognostic biomarkers in patients with resected cholangiocarcinoma: a systematic review and meta-analysis. Ann Surg Oncol. 2014;21:487–500. doi: 10.1245/s10434-013-3286-x. [DOI] [PubMed] [Google Scholar]
- 16.Saha SK, Gordan JD, Kleinstiver BP, Vu P, Najem MS, Yeo JC, Shi L, Kato Y, Levin RS, Webber JT, Damon LJ, Egan RK, Greninger P, McDermott U, Garnett MJ, Jenkins RL, Rieger-Christ KM, Sullivan TB, Hezel AF, Liss AS, Mizukami Y, Goyal L, Ferrone CR, Zhu AX, Joung JK, Shokat KM, Benes CH, Bardeesy N. Isocitrate Dehydrogenase Mutations Confer Dasatinib Hypersensitivity and SRC Dependence in Intrahepatic Cholangiocarcinoma. Cancer Discov. 2016;6:727–739. doi: 10.1158/2159-8290.CD-15-1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xie Q, Wang L, Zheng S. Prognostic and Clinicopathological Significance of PD-L1 in Patients with Cholangiocarcinoma: A Meta-Analysis. Dis Markers. 2020;2020:1817931. doi: 10.1155/2020/1817931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling TH Rd, Meyer T, Kang YK, Yeo W, Chopra A, Anderson J, Dela Cruz C, Lang L, Neely J, Tang H, Dastani HB, Melero I. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Macias RIR, Kornek M, Rodrigues PM, Paiva NA, Castro RE, Urban S, Pereira SP, Cadamuro M, Rupp C, Loosen SH, Luedde T, Banales JM. Diagnostic and prognostic biomarkers in cholangiocarcinoma. Liver Int. 2019;39 Suppl 1:108–122. doi: 10.1111/liv.14090. [DOI] [PubMed] [Google Scholar]
- 20.Shyamala K, Girish HC, Murgod S. Risk of tumor cell seeding through biopsy and aspiration cytology. J Int Soc Prev Community Dent. 2014;4:5–11. doi: 10.4103/2231-0762.129446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leon SA, Shapiro B, Sklaroff DM, Yaros MJ. Free DNA in the serum of cancer patients and the effect of therapy. Cancer Res. 1977;37:646–650. [PubMed] [Google Scholar]
- 22.Zviran A, Schulman RC, Shah M, Hill STK, Deochand S, Khamnei CC, Maloney D, Patel K, Liao W, Widman AJ, Wong P, Callahan MK, Ha G, Reed S, Rotem D, Frederick D, Sharova T, Miao B, Kim T, Gydush G, Rhoades J, Huang KY, Omans ND, Bolan PO, Lipsky AH, Ang C, Malbari M, Spinelli CF, Kazancioglu S, Runnels AM, Fennessey S, Stolte C, Gaiti F, Inghirami GG, Adalsteinsson V, Houck-Loomis B, Ishii J, Wolchok JD, Boland G, Robine N, Altorki NK, Landau DA. Genome-wide cell-free DNA mutational integration enables ultra-sensitive cancer monitoring. Nat Med. 2020;26:1114–1124. doi: 10.1038/s41591-020-0915-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andersen RF, Jakobsen A. Screening for circulating RAS/RAF mutations by multiplex digital PCR. Clin Chim Acta. 2016;458:138–143. doi: 10.1016/j.cca.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 24.Ettrich TJ, Schwerdel D, Dolnik A, Beuter F, Blätte TJ, Schmidt SA, Stanescu-Siegmund N, Steinacker J, Marienfeld R, Kleger A, Bullinger L, Seufferlein T, Berger AW. Genotyping of circulating tumor DNA in cholangiocarcinoma reveals diagnostic and prognostic information. Sci Rep. 2019;9:13261. doi: 10.1038/s41598-019-49860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goyal L, Saha SK, Liu LY, Siravegna G, Leshchiner I, Ahronian LG, Lennerz JK, Vu P, Deshpande V, Kambadakone A, Mussolin B, Reyes S, Henderson L, Sun JE, Van Seventer EE, Gurski JM Jr, Baltschukat S, Schacher-Engstler B, Barys L, Stamm C, Furet P, Ryan DP, Stone JR, Iafrate AJ, Getz G, Porta DG, Tiedt R, Bardelli A, Juric D, Corcoran RB, Bardeesy N, Zhu AX. Polyclonal Secondary FGFR2 Mutations Drive Acquired Resistance to FGFR Inhibition in Patients with FGFR2 Fusion-Positive Cholangiocarcinoma. Cancer Discov. 2017;7:252–263. doi: 10.1158/2159-8290.CD-16-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wasenang W, Chaiyarit P, Proungvitaya S, Limpaiboon T. Serum cell-free DNA methylation of OPCML and HOXD9 as a biomarker that may aid in differential diagnosis between cholangiocarcinoma and other biliary diseases. Clin Epigenetics. 2019;11:39. doi: 10.1186/s13148-019-0634-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang LJ, He CC, Sui X, Cai MJ, Zhou CY, Ma JL, Wu L, Wang H, Han SX, Zhu Q. MiR-21 promotes intrahepatic cholangiocarcinoma proliferation and growth in vitro and in vivo by targeting PTPN14 and PTEN. Oncotarget. 2015;6:5932–5946. doi: 10.18632/oncotarget.3465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silakit R, Loilome W, Yongvanit P, Chusorn P, Techasen A, Boonmars T, Khuntikeo N, Chamadol N, Pairojkul C, Namwat N. Circulating miR-192 in liver fluke-associated cholangiocarcinoma patients: a prospective prognostic indicator. J Hepatobiliary Pancreat Sci. 2014;21:864–872. doi: 10.1002/jhbp.145. [DOI] [PubMed] [Google Scholar]
- 29.Wang LJ, Zhang KL, Zhang N, Ma XW, Yan SW, Cao DH, Shi SJ. Serum miR-26a as a diagnostic and prognostic biomarker in cholangiocarcinoma. Oncotarget. 2015;6:18631–18640. doi: 10.18632/oncotarget.4072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu JJ, Zhou C, Luo X, Luo SZ, Li ZH, Xu ZX, Xu MY. Linc-SCRG1 accelerates progression of hepatocellular carcinoma as a ceRNA of miR26a to derepress SKP2. J Exp Clin Cancer Res. 2021;40:26. doi: 10.1186/s13046-020-01825-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han HS, Kim MJ, Han JH, Yun J, Kim HK, Yang Y, Kim KB, Park SM. Bile-derived circulating extracellular miR-30d-5p and miR-92a-3p as potential biomarkers for cholangiocarcinoma. Hepatobiliary Pancreat Dis Int. 2020;19:41–50. doi: 10.1016/j.hbpd.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 32.Soliman SE, Elabd NS, El-Kousy SM, Awad MF. Down regulation of miR-30a-5p and miR-182-5p in gastric cancer: Clinical impact and survival analysis. Biochem Biophys Rep. 2021;27:101079. doi: 10.1016/j.bbrep.2021.101079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernuzzi F, Marabita F, Lleo A, Carbone M, Mirolo M, Marzioni M, Alpini G, Alvaro D, Boberg KM, Locati M, Torzilli G, Rimassa L, Piscaglia F, He XS, Bowlus CL, Yang GX, Gershwin ME, Invernizzi P. Serum microRNAs as novel biomarkers for primary sclerosing cholangitis and cholangiocarcinoma. Clin Exp Immunol. 2016;185:61–71. doi: 10.1111/cei.12776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Correa-Gallego C, Maddalo D, Doussot A, Kemeny N, Kingham TP, Allen PJ, D'Angelica MI, DeMatteo RP, Betel D, Klimstra D, Jarnagin WR, Ventura A. Circulating Plasma Levels of MicroRNA-21 and MicroRNA-221 Are Potential Diagnostic Markers for Primary Intrahepatic Cholangiocarcinoma. PLoS One. 2016;11:e0163699. doi: 10.1371/journal.pone.0163699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Silakit R, Loilome W, Yongvanit P, Thongchot S, Sithithaworn P, Boonmars T, Koonmee S, Titapun A, Khuntikeo N, Chamadol N, Techasen A, Namwat N. Urinary microRNA-192 and microRNA-21 as potential indicators for liver fluke-associated cholangiocarcinoma risk group. Parasitol Int. 2017;66:479–485. doi: 10.1016/j.parint.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 36.Xu J, Wu C, Che X, Wang L, Yu D, Zhang T, Huang L, Li H, Tan W, Wang C, Lin D. Circulating microRNAs, miR-21, miR-122, and miR-223, in patients with hepatocellular carcinoma or chronic hepatitis. Mol Carcinog. 2011;50:136–142. doi: 10.1002/mc.20712. [DOI] [PubMed] [Google Scholar]
- 37.Goto T, Fujiya M, Konishi H, Sasajima J, Fujibayashi S, Hayashi A, Utsumi T, Sato H, Iwama T, Ijiri M, Sakatani A, Tanaka K, Nomura Y, Ueno N, Kashima S, Moriichi K, Mizukami Y, Kohgo Y, Okumura T. An elevated expression of serum exosomal microRNA-191, - 21, -451a of pancreatic neoplasm is considered to be efficient diagnostic marker. BMC Cancer. 2018;18:116. doi: 10.1186/s12885-018-4006-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sierzega M, Kaczor M, Kolodziejczyk P, Kulig J, Sanak M, Richter P. Evaluation of serum microRNA biomarkers for gastric cancer based on blood and tissue pools profiling: the importance of miR-21 and miR-331. Br J Cancer. 2017;117:266–273. doi: 10.1038/bjc.2017.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu CH, Huang Q, Jin ZY, Xie F, Zhu CL, Liu Z, Wang C. Circulating microRNA-21 as a prognostic, biological marker in cholangiocarcinoma. J Cancer Res Ther. 2018;14:220–225. doi: 10.4103/0973-1482.193125. [DOI] [PubMed] [Google Scholar]
- 40.Wu X, Xia M, Chen D, Wu F, Lv Z, Zhan Q, Jiao Y, Wang W, Chen G, An F. Profiling of downregulated blood-circulating miR-150-5p as a novel tumor marker for cholangiocarcinoma. Tumour Biol. 2016;37:15019–15029. doi: 10.1007/s13277-016-5313-6. [DOI] [PubMed] [Google Scholar]
- 41.Chen X, Xu X, Pan B, Zeng K, Xu M, Liu X, He B, Pan Y, Sun H, Wang S. Correction for: miR-150-5p suppresses tumor progression by targeting VEGFA in colorectal cancer. Aging (Albany NY) 2021;13:13372–13373. doi: 10.18632/aging.203069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhou J, Liu Z, Yang S, Li X. Identification of microRNAs as biomarkers for cholangiocarcinoma detection: A diagnostic meta-analysis. Clin Res Hepatol Gastroenterol. 2017;41:156–162. doi: 10.1016/j.clinre.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 43.Liang Z, Liu X, Zhang Q, Wang C, Zhao Y. Diagnostic value of microRNAs as biomarkers for cholangiocarcinoma. Dig Liver Dis. 2016;48:1227–1232. doi: 10.1016/j.dld.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 44.Plieskatt J, Rinaldi G, Feng Y, Peng J, Easley S, Jia X, Potriquet J, Pairojkul C, Bhudhisawasdi V, Sripa B, Brindley PJ, Bethony J, Mulvenna J. A microRNA profile associated with Opisthorchis viverrini-induced cholangiocarcinoma in tissue and plasma. BMC Cancer. 2015;15:309. doi: 10.1186/s12885-015-1270-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lang SA, Bednarsch J, Joechle K, Amygdalos I, Czigany Z, Heij L, Ulmer TF, Neumann UP. Prognostic biomarkers for cholangiocarcinoma (CCA): state of the art. Expert Rev Gastroenterol Hepatol. 2021;15:497–510. doi: 10.1080/17474124.2021.1912591. [DOI] [PubMed] [Google Scholar]
- 46.Rompianesi G, Di Martino M, Gordon-Weeks A, Montalti R, Troisi R. Liquid biopsy in cholangiocarcinoma: Current status and future perspectives. World J Gastrointest Oncol. 2021;13:332–350. doi: 10.4251/wjgo.v13.i5.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tsen A, Barbara M, Rosenkranz L. Dilemma of elevated CA 19-9 in biliary pathology. Pancreatology. 2018;18:862–867. doi: 10.1016/j.pan.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 48.Zhang M, Cheng S, Jin Y, Zhao Y, Wang Y. Roles of CA125 in diagnosis, prediction, and oncogenesis of ovarian cancer. Biochim Biophys Acta Rev Cancer. 2021;1875:188503. doi: 10.1016/j.bbcan.2021.188503. [DOI] [PubMed] [Google Scholar]
- 49.You YN, Hardiman KM, Bafford A, Poylin V, Francone TD, Davis K, Paquette IM, Steele SR, Feingold DL On Behalf of the Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Rectal Cancer. Dis Colon Rectum. 2020;63:1191–1222. doi: 10.1097/DCR.0000000000001762. [DOI] [PubMed] [Google Scholar]
- 50.Loosen SH, Roderburg C, Kauertz KL, Pombeiro I, Leyh C, Benz F, Vucur M, Longerich T, Koch A, Braunschweig T, Ulmer TF, Heidenhain C, Tacke F, Binnebösel M, Schmeding M, Trautwein C, Neumann UP, Luedde T. Elevated levels of circulating osteopontin are associated with a poor survival after resection of cholangiocarcinoma. J Hepatol. 2017;67:749–757. doi: 10.1016/j.jhep.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 51.Onsurathum S, Haonon O, Pinlaor P, Pairojkul C, Khuntikeo N, Thanan R, Roytrakul S, Pinlaor S. Proteomics detection of S100A6 in tumor tissue interstitial fluid and evaluation of its potential as a biomarker of cholangiocarcinoma. Tumour Biol. 2018;40:1010428318767195. doi: 10.1177/1010428318767195. [DOI] [PubMed] [Google Scholar]
- 52.Shi RY, Yang XR, Shen QJ, Yang LX, Xu Y, Qiu SJ, Sun YF, Zhang X, Wang Z, Zhu K, Qin WX, Tang ZY, Fan J, Zhou J. High expression of Dickkopf-related protein 1 is related to lymphatic metastasis and indicates poor prognosis in intrahepatic cholangiocarcinoma patients after surgery. Cancer. 2013;119:993–1003. doi: 10.1002/cncr.27788. [DOI] [PubMed] [Google Scholar]
- 53.Cheon YK, Cho YD, Moon JH, Jang JY, Kim YS, Lee MS, Lee JS, Shim CS. Diagnostic utility of interleukin-6 (IL-6) for primary bile duct cancer and changes in serum IL-6 Levels following photodynamic therapy. Am J Gastroenterol. 2007;102:2164–2170. doi: 10.1111/j.1572-0241.2007.01403.x. [DOI] [PubMed] [Google Scholar]
- 54.Shen J, Wang W, Wu J, Feng B, Chen W, Wang M, Tang J, Wang F, Cheng F, Pu L, Tang Q, Wang X, Li X. Comparative proteomic profiling of human bile reveals SSP411 as a novel biomarker of cholangiocarcinoma. PLoS One. 2012;7:e47476. doi: 10.1371/journal.pone.0047476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ruzzenente A, Iacono C, Conci S, Bertuzzo F, Salvagno G, Ruzzenente O, Campagnaro T, Valdegamberi A, Pachera S, Bagante F, Guglielmi A. A novel serum marker for biliary tract cancer: diagnostic and prognostic values of quantitative evaluation of serum mucin 5AC (MUC5AC) Surgery. 2014;155:633–639. doi: 10.1016/j.surg.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 56.Leelawat K, Sakchinabut S, Narong S, Wannaprasert J. Detection of serum MMP-7 and MMP-9 in cholangiocarcinoma patients: evaluation of diagnostic accuracy. BMC Gastroenterol. 2009;9:30. doi: 10.1186/1471-230X-9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leelawat K, Narong S, Wannaprasert J, Ratanashu-ek T. Prospective study of MMP7 serum levels in the diagnosis of cholangiocarcinoma. World J Gastroenterol. 2010;16:4697–4703. doi: 10.3748/wjg.v16.i37.4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Guowei H, Yuan L, Ma L, Zhongyang L, Zhixing S, Lin L, Minqi L. The diagnostic efficacy of CYFRA21-1 on intrahepatic cholangiocarcinoma: A meta-analysis. Clin Res Hepatol Gastroenterol. 2019;43:266–272. doi: 10.1016/j.clinre.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 59.Loosen SH, Breuer A, Tacke F, Kather JN, Gorgulho J, Alizai PH, Bednarsch J, Roeth AA, Lurje G, Schmitz SM, Brozat JF, Paffenholz P, Vucur M, Ritz T, Koch A, Trautwein C, Ulmer TF, Roderburg C, Longerich T, Neumann UP, Luedde T. Circulating levels of soluble urokinase plasminogen activator receptor predict outcome after resection of biliary tract cancer. JHEP Rep. 2020;2:100080. doi: 10.1016/j.jhepr.2020.100080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim SY, Lee HS, Bang SM, Han DH, Hwang HK, Choi GH, Chung MJ, Kim SU. Serum Dickkopf-1 in Combined with CA 19-9 as a Biomarker of Intrahepatic Cholangiocarcinoma. Cancers (Basel) 2021;13 doi: 10.3390/cancers13081828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Byrling J, Hilmersson KS, Ansari D, Andersson R, Andersson B. Thrombospondin-2 as a diagnostic biomarker for distal cholangiocarcinoma and pancreatic ductal adenocarcinoma. Clin Transl Oncol. 2022;24:297–304. doi: 10.1007/s12094-021-02685-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kimawaha P, Jusakul A, Junsawang P, Thanan R, Titapun A, Khuntikeo N, Techasen A. Establishment of a Potential Serum Biomarker Panel for the Diagnosis and Prognosis of Cholangiocarcinoma Using Decision Tree Algorithms. Diagnostics (Basel) 2021;11 doi: 10.3390/diagnostics11040589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu HL, Inagaki Y, Seyama Y, Sugawara Y, Kokudo N, Nakata M, Wang FS, Tang W. Expression of KL-6 mucin, a human MUC1 mucin, in intrahepatic cholangiocarcinoma and its potential involvement in tumor cell adhesion and invasion. Life Sci. 2009;85:395–400. doi: 10.1016/j.lfs.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 64.Zheng BH, Shen S, Wong KF, Gong ZJ, Sun WT, Ni XJ, Wang JW, Hu MY, Liu H, Ni XL, Liu HB, Luk JM, Suo T. Clinical correlation of cadherin-17 marker with advanced tumor stages and poor prognosis of cholangiocarcinoma. J Surg Oncol. 2021;123:1253–1262. doi: 10.1002/jso.26399. [DOI] [PubMed] [Google Scholar]
- 65.Siriphak S, Chanakankun R, Proungvitaya T, Roytrakul S, Tummanatsakun D, Seubwai W, Wongwattanakul M, Proungvitaya S. Kallikrein-11, in Association with Coiled-Coil Domain Containing 25, as a Potential Prognostic Marker for Cholangiocarcinoma with Lymph Node Metastasis. Molecules. 2021;26 doi: 10.3390/molecules26113105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Truong SDA, Tummanatsakun D, Proungvitaya T, Limpaiboon T, Wongwattanakul M, Chua-On D, Roytrakul S, Proungvitaya S. Serum Levels of Cytokine-Induced Apoptosis Inhibitor 1 (CIAPIN1) as a Potential Prognostic Biomarker of Cholangiocarcinoma. Diagnostics (Basel) 2021;11 doi: 10.3390/diagnostics11061054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Loosen SH, Benz F, Niedeggen J, Schmeding M, Schüller F, Koch A, Vucur M, Tacke F, Trautwein C, Roderburg C, Neumann UP, Luedde T. Serum levels of S100A6 are unaltered in patients with resectable cholangiocarcinoma. Clin Transl Med. 2016;5:39. doi: 10.1186/s40169-016-0120-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grunnet M, Christensen IJ, Lassen U, Jensen LH, Lydolph M, Lund IK, Thurison T, Høyer-Hansen G, Mau-Sørensen M. Prognostic significance of circulating intact and cleaved forms of urokinase plasminogen activator receptor in inoperable chemotherapy treated cholangiocarcinoma patients. Clin Biochem. 2014;47:599–604. doi: 10.1016/j.clinbiochem.2014.01.030. [DOI] [PubMed] [Google Scholar]
- 69.Liu BX, Tang CT, Dai XJ, Zeng L, Cheng F, Chen Y, Zeng C. Prognostic Value of S100P Expression in Patients With Digestive System Cancers: A Meta-Analysis. Front Oncol. 2021;11:593728. doi: 10.3389/fonc.2021.593728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Perng DS, Hung CM, Lin HY, Morgan P, Hsu YC, Wu TC, Hsieh PM, Yeh JH, Hsiao P, Lee CY, Li YC, Wang YC, Chen YS, Lin CW. Role of autophagy-related protein in the prognosis of combined hepatocellular carcinoma and cholangiocarcinoma after surgical resection. BMC Cancer. 2021;21:828. doi: 10.1186/s12885-021-08553-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thummarati P, Wijitburaphat S, Prasopthum A, Menakongka A, Sripa B, Tohtong R, Suthiphongchai T. High level of urokinase plasminogen activator contributes to cholangiocarcinoma invasion and metastasis. World J Gastroenterol. 2012;18:244–250. doi: 10.3748/wjg.v18.i3.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Itatsu K, Zen Y, Yamaguchi J, Ohira S, Ishikawa A, Ikeda H, Sato Y, Harada K, Sasaki M, Sakamoto H, Nagino M, Nimura Y, Ohta T, Nakanuma Y. Expression of matrix metalloproteinase 7 is an unfavorable postoperative prognostic factor in cholangiocarcinoma of the perihilar, hilar, and extrahepatic bile ducts. Hum Pathol. 2008;39:710–719. doi: 10.1016/j.humpath.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 73.Hirashita T, Iwashita Y, Ohta M, Komori Y, Eguchi H, Yada K, Kitano S. Expression of matrix metalloproteinase-7 is an unfavorable prognostic factor in intrahepatic cholangiocarcinoma. J Gastrointest Surg. 2012;16:842–848. doi: 10.1007/s11605-011-1813-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang C, Xu J, Ye J, Zhang X. Prognostic value of HHLA2 expression in solid tumors: A meta-analysis based on the Chinese population. Medicine (Baltimore) 2021;100:e26789. doi: 10.1097/MD.0000000000026789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Qiang Z, Zhang W, Jin S, Dai K, He Y, Tao L, Yu H. Carcinoembryonic antigen, α-fetoprotein, and Ki67 as biomarkers and prognostic factors in intrahepatic cholangiocarcinoma: A retrospective cohort study. Ann Hepatol. 2021;20:100242. doi: 10.1016/j.aohep.2020.07.010. [DOI] [PubMed] [Google Scholar]
- 76.Roderburg C, Loosen SH, Bednarsch J, Alizai PH, Roeth AA, Schmitz SM, Vucur M, Luedde M, Paffenholz P, Tacke F, Trautwein C, Ulmer TF, Neumann UP, Luedde T. Levels of Circulating PD-L1 Are Decreased in Patients with Resectable Cholangiocarcinoma. Int J Mol Sci. 2021;22 doi: 10.3390/ijms22126569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhou KQ, Liu WF, Yang LX, Sun YF, Hu J, Chen FY, Zhou C, Zhang XY, Peng YF, Yu L, Zhou J, Fan J, Wang Z. Circulating osteopontin per tumor volume as a prognostic biomarker for resectable intrahepatic cholangiocarcinoma. Hepatobiliary Surg Nutr. 2019;8:582–596. doi: 10.21037/hbsn.2019.03.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kimawaha P, Jusakul A, Junsawang P, Loilome W, Khuntikeo N, Techasen A. Circulating TGF-β1 as the potential epithelial mesenchymal transition-biomarker for diagnosis of cholangiocarcinoma. J Gastrointest Oncol. 2020;11:304–318. doi: 10.21037/jgo.2019.01.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Boroughs LK, DeBerardinis RJ. Metabolic pathways promoting cancer cell survival and growth. Nat Cell Biol. 2015;17:351–359. doi: 10.1038/ncb3124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Macias RIR, Banales JM, Sangro B, Muntané J, Avila MA, Lozano E, Perugorria MJ, Padillo FJ, Bujanda L, Marin JJG. The search for novel diagnostic and prognostic biomarkers in cholangiocarcinoma. Biochim Biophys Acta Mol Basis Dis. 2018;1864:1468–1477. doi: 10.1016/j.bbadis.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 81.Park JY, Park BK, Ko JS, Bang S, Song SY, Chung JB. Bile acid analysis in biliary tract cancer. Yonsei Med J. 2006;47:817–825. doi: 10.3349/ymj.2006.47.6.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Albiin N, Smith IC, Arnelo U, Lindberg B, Bergquist A, Dolenko B, Bryksina N, Bezabeh T. Detection of cholangiocarcinoma with magnetic resonance spectroscopy of bile in patients with and without primary sclerosing cholangitis. Acta Radiol. 2008;49:855–862. doi: 10.1080/02841850802220092. [DOI] [PubMed] [Google Scholar]
- 83.Sharif AW, Williams HR, Lampejo T, Khan SA, Bansi DS, Westaby D, Thillainayagam AV, Thomas HC, Cox IJ, Taylor-Robinson SD. Metabolic profiling of bile in cholangiocarcinoma using in vitro magnetic resonance spectroscopy. HPB (Oxford) 2010;12:396–402. doi: 10.1111/j.1477-2574.2010.00185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nagana Gowda GA, Shanaiah N, Cooper A, Maluccio M, Raftery D. Visualization of bile homeostasis using (1)H-NMR spectroscopy as a route for assessing liver cancer. Lipids. 2009;44:27–35. doi: 10.1007/s11745-008-3254-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Alsaleh M, Leftley Z, Barbera TA, Koomson LK, Zabron A, Crossey MME, Reeves HL, Cramp M, Ryder S, Greer S, Prince M, Sithithaworn P, Shariff M, Khuntikeo N, Loilome W, Yongvanit P, Shen YL, Cox IJ, Williams R, Wadsworth CA, Holmes E, Nash K, Taylor-Robinson SD. Characterisation of the Serum Metabolic Signature of Cholangiocarcinoma in a United Kingdom Cohort. J Clin Exp Hepatol. 2020;10:17–29. doi: 10.1016/j.jceh.2019.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang X, Yang Z, Shi Z, Zhu Z, Li C, Du Z, Zhang Y, Wang Z, Jiao Z, Tian X, Zhang J, Zhai W, Kan Q. Analysis of bile acid profile in plasma to differentiate cholangiocarcinoma from benign biliary diseases and healthy controls. J Steroid Biochem Mol Biol. 2021;205:105775. doi: 10.1016/j.jsbmb.2020.105775. [DOI] [PubMed] [Google Scholar]
- 87.Negrini D, Zecchin P, Ruzzenente A, Bagante F, De Nitto S, Gelati M, Salvagno GL, Danese E, Lippi G. Machine Learning Model Comparison in the Screening of Cholangiocarcinoma Using Plasma Bile Acids Profiles. Diagnostics (Basel) 2020;10 doi: 10.3390/diagnostics10080551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Banales JM, Iñarrairaegui M, Arbelaiz A, Milkiewicz P, Muntané J, Muñoz-Bellvis L, La Casta A, Gonzalez LM, Arretxe E, Alonso C, Martínez-Arranz I, Lapitz A, Santos-Laso A, Avila MA, Martínez-Chantar ML, Bujanda L, Marin JJG, Sangro B, Macias RIR. Serum Metabolites as Diagnostic Biomarkers for Cholangiocarcinoma, Hepatocellular Carcinoma, and Primary Sclerosing Cholangitis. Hepatology. 2019;70:547–562. doi: 10.1002/hep.30319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liang Q, Wang C, Li B, Zhang AH. Lipidomics analysis based on liquid chromatography mass spectrometry for hepatocellular carcinoma and intrahepatic cholangiocarcinoma. RSC Adv. 2015;5:63711–63718. [Google Scholar]
- 90.Macias RIR, Muñoz-Bellvís L, Sánchez-Martín A, Arretxe E, Martínez-Arranz I, Lapitz A, Gutiérrez ML, La Casta A, Alonso C, González LM, Avila MA, Martinez-Chantar ML, Castro RE, Bujanda L, Banales JM, Marin JJG. A Novel Serum Metabolomic Profile for the Differential Diagnosis of Distal Cholangiocarcinoma and Pancreatic Ductal Adenocarcinoma. Cancers (Basel) 2020;12 doi: 10.3390/cancers12061433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang X, Li J, Zhang AH. Urine metabolic phenotypes analysis of extrahepatic cholangiocarcinoma disease using ultra-high performance liquid chromatography-mass spectrometry. RSC Adv. 2016;6:63049–63057. [Google Scholar]
- 92.Alsaleh M, Barbera TA, Reeves HL, Cramp ME, Ryder S, Gabra H, Nash K, Shen YL, Holmes E, Williams R, Taylor-Robinson SD. Characterization of the urinary metabolic profile of cholangiocarcinoma in a United Kingdom population. Hepat Med. 2019;11:47–67. doi: 10.2147/HMER.S193996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mocan T, Kang DW, Molloy BJ, Jeon H, Spârchez ZA, Beyoğlu D, Idle JR. Plasma fetal bile acids 7α-hydroxy-3-oxochol-4-en-24-oic acid and 3-oxachola-4,6-dien-24-oic acid indicate severity of liver cirrhosis. Sci Rep. 2021;11:8298. doi: 10.1038/s41598-021-87921-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Caby MP, Lankar D, Vincendeau-Scherrer C, Raposo G, Bonnerot C. Exosomal-like vesicles are present in human blood plasma. Int Immunol. 2005;17:879–887. doi: 10.1093/intimm/dxh267. [DOI] [PubMed] [Google Scholar]
- 95.Pisitkun T, Shen RF, Knepper MA. Identification and proteomic profiling of exosomes in human urine. Proc Natl Acad Sci U S A. 2004;101:13368–13373. doi: 10.1073/pnas.0403453101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Masyuk AI, Huang BQ, Ward CJ, Gradilone SA, Banales JM, Masyuk TV, Radtke B, Splinter PL, LaRusso NF. Biliary exosomes influence cholangiocyte regulatory mechanisms and proliferation through interaction with primary cilia. Am J Physiol Gastrointest Liver Physiol. 2010;299:G990–G999. doi: 10.1152/ajpgi.00093.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Théry C, Witwer KW, Aikawa E, Alcaraz MJ, Anderson JD, Andriantsitohaina R, Antoniou A, Arab T, Archer F, Atkin-Smith GK, Ayre DC, Bach JM, Bachurski D, Baharvand H, Balaj L, Baldacchino S, Bauer NN, Baxter AA, Bebawy M, Beckham C, Bedina Zavec A, Benmoussa A, Berardi AC, Bergese P, Bielska E, Blenkiron C, Bobis-Wozowicz S, Boilard E, Boireau W, Bongiovanni A, Borràs FE, Bosch S, Boulanger CM, Breakefield X, Breglio AM, Brennan MÁ, Brigstock DR, Brisson A, Broekman ML, Bromberg JF, Bryl-Górecka P, Buch S, Buck AH, Burger D, Busatto S, Buschmann D, Bussolati B, Buzás EI, Byrd JB, Camussi G, Carter DR, Caruso S, Chamley LW, Chang YT, Chen C, Chen S, Cheng L, Chin AR, Clayton A, Clerici SP, Cocks A, Cocucci E, Coffey RJ, Cordeiro-da-Silva A, Couch Y, Coumans FA, Coyle B, Crescitelli R, Criado MF, D'Souza-Schorey C, Das S, Datta Chaudhuri A, de Candia P, De Santana EF, De Wever O, Del Portillo HA, Demaret T, Deville S, Devitt A, Dhondt B, Di Vizio D, Dieterich LC, Dolo V, Dominguez Rubio AP, Dominici M, Dourado MR, Driedonks TA, Duarte FV, Duncan HM, Eichenberger RM, Ekström K, El Andaloussi S, Elie-Caille C, Erdbrügger U, Falcón-Pérez JM, Fatima F, Fish JE, Flores-Bellver M, Försönits A, Frelet-Barrand A, Fricke F, Fuhrmann G, Gabrielsson S, Gámez-Valero A, Gardiner C, Gärtner K, Gaudin R, Gho YS, Giebel B, Gilbert C, Gimona M, Giusti I, Goberdhan DC, Görgens A, Gorski SM, Greening DW, Gross JC, Gualerzi A, Gupta GN, Gustafson D, Handberg A, Haraszti RA, Harrison P, Hegyesi H, Hendrix A, Hill AF, Hochberg FH, Hoffmann KF, Holder B, Holthofer H, Hosseinkhani B, Hu G, Huang Y, Huber V, Hunt S, Ibrahim AG, Ikezu T, Inal JM, Isin M, Ivanova A, Jackson HK, Jacobsen S, Jay SM, Jayachandran M, Jenster G, Jiang L, Johnson SM, Jones JC, Jong A, Jovanovic-Talisman T, Jung S, Kalluri R, Kano SI, Kaur S, Kawamura Y, Keller ET, Khamari D, Khomyakova E, Khvorova A, Kierulf P, Kim KP, Kislinger T, Klingeborn M, Klinke DJ 2nd, Kornek M, Kosanović MM, Kovács ÁF, Krämer-Albers EM, Krasemann S, Krause M, Kurochkin IV, Kusuma GD, Kuypers S, Laitinen S, Langevin SM, Languino LR, Lannigan J, Lässer C, Laurent LC, Lavieu G, Lázaro-Ibáñez E, Le Lay S, Lee MS, Lee YXF, Lemos DS, Lenassi M, Leszczynska A, Li IT, Liao K, Libregts SF, Ligeti E, Lim R, Lim SK, Linē A, Linnemannstöns K, Llorente A, Lombard CA, Lorenowicz MJ, Lörincz ÁM, Lötvall J, Lovett J, Lowry MC, Loyer X, Lu Q, Lukomska B, Lunavat TR, Maas SL, Malhi H, Marcilla A, Mariani J, Mariscal J, Martens-Uzunova ES, Martin-Jaular L, Martinez MC, Martins VR, Mathieu M, Mathivanan S, Maugeri M, McGinnis LK, McVey MJ, Meckes DG Jr, Meehan KL, Mertens I, Minciacchi VR, Möller A, Møller Jørgensen M, Morales-Kastresana A, Morhayim J, Mullier F, Muraca M, Musante L, Mussack V, Muth DC, Myburgh KH, Najrana T, Nawaz M, Nazarenko I, Nejsum P, Neri C, Neri T, Nieuwland R, Nimrichter L, Nolan JP, Nolte-'t Hoen EN, Noren Hooten N, O'Driscoll L, O'Grady T, O'Loghlen A, Ochiya T, Olivier M, Ortiz A, Ortiz LA, Osteikoetxea X, Østergaard O, Ostrowski M, Park J, Pegtel DM, Peinado H, Perut F, Pfaffl MW, Phinney DG, Pieters BC, Pink RC, Pisetsky DS, Pogge von Strandmann E, Polakovicova I, Poon IK, Powell BH, Prada I, Pulliam L, Quesenberry P, Radeghieri A, Raffai RL, Raimondo S, Rak J, Ramirez MI, Raposo G, Rayyan MS, Regev-Rudzki N, Ricklefs FL, Robbins PD, Roberts DD, Rodrigues SC, Rohde E, Rome S, Rouschop KM, Rughetti A, Russell AE, Saá P, Sahoo S, Salas-Huenuleo E, Sánchez C, Saugstad JA, Saul MJ, Schiffelers RM, Schneider R, Schøyen TH, Scott A, Shahaj E, Sharma S, Shatnyeva O, Shekari F, Shelke GV, Shetty AK, Shiba K, Siljander PR, Silva AM, Skowronek A, Snyder OL 2nd, Soares RP, Sódar BW, Soekmadji C, Sotillo J, Stahl PD, Stoorvogel W, Stott SL, Strasser EF, Swift S, Tahara H, Tewari M, Timms K, Tiwari S, Tixeira R, Tkach M, Toh WS, Tomasini R, Torrecilhas AC, Tosar JP, Toxavidis V, Urbanelli L, Vader P, van Balkom BW, van der Grein SG, Van Deun J, van Herwijnen MJ, Van Keuren-Jensen K, van Niel G, van Royen ME, van Wijnen AJ, Vasconcelos MH, Vechetti IJ Jr, Veit TD, Vella LJ, Velot É, Verweij FJ, Vestad B, Viñas JL, Visnovitz T, Vukman KV, Wahlgren J, Watson DC, Wauben MH, Weaver A, Webber JP, Weber V, Wehman AM, Weiss DJ, Welsh JA, Wendt S, Wheelock AM, Wiener Z, Witte L, Wolfram J, Xagorari A, Xander P, Xu J, Yan X, Yáñez-Mó M, Yin H, Yuana Y, Zappulli V, Zarubova J, Žėkas V, Zhang JY, Zhao Z, Zheng L, Zheutlin AR, Zickler AM, Zimmermann P, Zivkovic AM, Zocco D, Zuba-Surma EK. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7:1535750. doi: 10.1080/20013078.2018.1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 99.Słomka A, Mocan T, Wang B, Nenu I, Urban SK, Gonzales-Carmona M, Schmidt-Wolf IGH, Lukacs-Kornek V, Strassburg CP, Spârchez Z, Kornek M. EVs as Potential New Therapeutic Tool/Target in Gastrointestinal Cancer and HCC. Cancers (Basel) 2020;12 doi: 10.3390/cancers12103019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dutta S, Reamtong O, Panvongsa W, Kitdumrongthum S, Janpipatkul K, Sangvanich P, Piyachaturawat P, Chairoungdua A. Proteomics profiling of cholangiocarcinoma exosomes: A potential role of oncogenic protein transferring in cancer progression. Biochim Biophys Acta. 2015;1852:1989–1999. doi: 10.1016/j.bbadis.2015.06.024. [DOI] [PubMed] [Google Scholar]
- 101.Haga H, Yan IK, Takahashi K, Wood J, Zubair A, Patel T. Tumour cell-derived extracellular vesicles interact with mesenchymal stem cells to modulate the microenvironment and enhance cholangiocarcinoma growth. J Extracell Vesicles. 2015;4:24900. doi: 10.3402/jev.v4.24900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Arbelaiz A, Azkargorta M, Krawczyk M, Santos-Laso A, Lapitz A, Perugorria MJ, Erice O, Gonzalez E, Jimenez-Agüero R, Lacasta A, Ibarra C, Sanchez-Campos A, Jimeno JP, Lammert F, Milkiewicz P, Marzioni M, Macias RIR, Marin JJG, Patel T, Gores GJ, Martinez I, Elortza F, Falcon-Perez JM, Bujanda L, Banales JM. Serum extracellular vesicles contain protein biomarkers for primary sclerosing cholangitis and cholangiocarcinoma. Hepatology. 2017;66:1125–1143. doi: 10.1002/hep.29291. [DOI] [PubMed] [Google Scholar]
- 103.Julich-Haertel H, Urban SK, Krawczyk M, Willms A, Jankowski K, Patkowski W, Kruk B, Krasnodębski M, Ligocka J, Schwab R, Richardsen I, Schaaf S, Klein A, Gehlert S, Sänger H, Casper M, Banales JM, Schuppan D, Milkiewicz P, Lammert F, Lukacs-Kornek V, Kornek M. Cancer-associated circulating large extracellular vesicles in cholangiocarcinoma and hepatocellular carcinoma. J Hepatol. 2017;67:282–292. doi: 10.1016/j.jhep.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 104.Urban SK, Sänger H, Krawczyk M, Julich-Haertel H, Willms A, Ligocka J, Azkargorta M, Mocan T, Kahlert C, Kruk B, Jankowski K, Patkowski W, Zieniewicz K, Hołówko W, Krupa Ł, Rzucidło M, Gutkowski K, Wystrychowski W, Król R, Raszeja-Wyszomirska J, Słomka A, Schwab R, Wöhler A, Gonzalez-Carmona MA, Gehlert S, Sparchez Z, Banales JM, Strassburg CP, Lammert F, Milkiewicz P, Kornek M. Synergistic effects of extracellular vesicle phenotyping and AFP in hepatobiliary cancer differentiation. Liver Int. 2020;40:3103–3116. doi: 10.1111/liv.14585. [DOI] [PubMed] [Google Scholar]
- 105.Severino V, Dumonceau JM, Delhaye M, Moll S, Annessi-Ramseyer I, Robin X, Frossard JL, Farina A. Extracellular Vesicles in Bile as Markers of Malignant Biliary Stenoses. Gastroenterology. 2017;153:495–504.e8. doi: 10.1053/j.gastro.2017.04.043. [DOI] [PubMed] [Google Scholar]
- 106.Li L, Masica D, Ishida M, Tomuleasa C, Umegaki S, Kalloo AN, Georgiades C, Singh VK, Khashab M, Amateau S, Li Z, Okolo P, Lennon AM, Saxena P, Geschwind JF, Schlachter T, Hong K, Pawlik TM, Canto M, Law J, Sharaiha R, Weiss CR, Thuluvath P, Goggins M, Shin EJ, Peng H, Kumbhari V, Hutfless S, Zhou L, Mezey E, Meltzer SJ, Karchin R, Selaru FM. Human bile contains microRNA-laden extracellular vesicles that can be used for cholangiocarcinoma diagnosis. Hepatology. 2014;60:896–907. doi: 10.1002/hep.27050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Arnoletti JP, Fanaian N, Reza J, Sause R, Almodovar AJ, Srivastava M, Patel S, Veldhuis PP, Griffith E, Shao YP, Zhu X, Litherland SA. Pancreatic and bile duct cancer circulating tumor cells (CTC) form immune-resistant multi-cell type clusters in the portal venous circulation. Cancer Biol Ther. 2018;19:887–897. doi: 10.1080/15384047.2018.1480292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Goto W, Kashiwagi S, Asano Y, Takada K, Takahashi K, Hatano T, Takashima T, Tomita S, Motomura H, Ohsawa M, Hirakawa K, Ohira M. Circulating tumor cell clusters-associated gene plakoglobin is a significant prognostic predictor in patients with breast cancer. Biomark Res. 2017;5:19. doi: 10.1186/s40364-017-0099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Osta WA, Chen Y, Mikhitarian K, Mitas M, Salem M, Hannun YA, Cole DJ, Gillanders WE. EpCAM is overexpressed in breast cancer and is a potential target for breast cancer gene therapy. Cancer Res. 2004;64:5818–5824. doi: 10.1158/0008-5472.CAN-04-0754. [DOI] [PubMed] [Google Scholar]
- 110.Maetzel D, Denzel S, Mack B, Canis M, Went P, Benk M, Kieu C, Papior P, Baeuerle PA, Munz M, Gires O. Nuclear signalling by tumour-associated antigen EpCAM. Nat Cell Biol. 2009;11:162–171. doi: 10.1038/ncb1824. [DOI] [PubMed] [Google Scholar]
- 111.Litvinov SV, van Driel W, van Rhijn CM, Bakker HA, van Krieken H, Fleuren GJ, Warnaar SO. Expression of Ep-CAM in cervical squamous epithelia correlates with an increased proliferation and the disappearance of markers for terminal differentiation. Am J Pathol. 1996;148:865–875. [PMC free article] [PubMed] [Google Scholar]
- 112.Al Ustwani O, Iancu D, Yacoub R, Iyer R. Detection of circulating tumor cells in cancers of biliary origin. J Gastrointest Oncol. 2012;3:97–104. doi: 10.3978/j.issn.2078-6891.2011.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Valle JW, Wasan H, Lopes A, Backen AC, Palmer DH, Morris K, Duggan M, Cunningham D, Anthoney DA, Corrie P, Madhusudan S, Maraveyas A, Ross PJ, Waters JS, Steward WP, Rees C, Beare S, Dive C, Bridgewater JA. Cediranib or placebo in combination with cisplatin and gemcitabine chemotherapy for patients with advanced biliary tract cancer (ABC-03): a randomised phase 2 trial. Lancet Oncol. 2015;16:967–978. doi: 10.1016/S1470-2045(15)00139-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Backen AC, Lopes A, Wasan H, Palmer DH, Duggan M, Cunningham D, Anthoney A, Corrie PG, Madhusudan S, Maraveyas A, Ross PJ, Waters JS, Steward WP, Rees C, McNamara MG, Beare S, Bridgewater JA, Dive C, Valle JW. Circulating biomarkers during treatment in patients with advanced biliary tract cancer receiving cediranib in the UK ABC-03 trial. Br J Cancer. 2018;119:27–35. doi: 10.1038/s41416-018-0132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sieuwerts AM, Kraan J, Bolt J, van der Spoel P, Elstrodt F, Schutte M, Martens JW, Gratama JW, Sleijfer S, Foekens JA. Anti-epithelial cell adhesion molecule antibodies and the detection of circulating normal-like breast tumor cells. J Natl Cancer Inst. 2009;101:61–66. doi: 10.1093/jnci/djn419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Budd GT, Cristofanilli M, Ellis MJ, Stopeck A, Borden E, Miller MC, Matera J, Repollet M, Doyle GV, Terstappen LW, Hayes DF. Circulating tumor cells vs imaging--predicting overall survival in metastatic breast cancer. Clin Cancer Res. 2006;12:6403–6409. doi: 10.1158/1078-0432.CCR-05-1769. [DOI] [PubMed] [Google Scholar]
- 117.Gopinathan P, Chiang NJ, Bandaru A, Sinha A, Huang WY, Hung SC, Shan YS, Lee GB. Exploring Circulating Tumor Cells in Cholangiocarcinoma Using a Novel Glycosaminoglycan Probe on a Microfluidic Platform. Adv Healthc Mater. 2020;9:e1901875. doi: 10.1002/adhm.201901875. [DOI] [PubMed] [Google Scholar]
- 118.Reduzzi C, Vismara M, Silvestri M, Celio L, Niger M, Peverelli G, De Braud F, Daidone MG, Cappelletti V. A novel circulating tumor cell subpopulation for treatment monitoring and molecular characterization in biliary tract cancer. Int J Cancer. 2020;146:3495–3503. doi: 10.1002/ijc.32822. [DOI] [PMC free article] [PubMed] [Google Scholar]