Abstract
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus-2 has brought serious challenges for the medical field. Patients with COVID-19 usually have respiratory symptoms. However, liver dysfunction is not an uncommon presentation. Additionally, the degree of liver dysfunction is associated with the severity and prognosis of COVID-19. Prevention, diagnosis, and treatment of malnutrition should be routinely recommended in the management of patients with COVID-19, especially in those with liver dysfunction. Recently, a large number of studies have reported that nutrition therapy measures, including natural dietary supplements, vitamins, minerals and trace elements, and probiotics, might have potential hepatoprotective effects against COVID-19-related liver dysfunction via their antioxidant, antiviral, anti-inflammatory, and positive immunomodulatory effects. This review mainly focuses on the possible relationship between COVID-19 and liver dysfunction, nutritional and metabolic characteristics, nutritional status assessment, and nutrition therapy to provide a reference for the nutritionists while making evidence-based nutritional decisions during the COVID-19 pandemic.
Keywords: COVID-19, SARS-CoV-2, Liver dysfunction, Nutritional status assessment, Nutrition therapy
Core Tip: Patients with coronavirus disease 2019 (COVID-19) usually have respiratory symptoms, but liver dysfunction is not an uncommon presentation. The degree of liver dysfunction is associated with COVID-19 severity and prognosis. Nutrition has played a critical therapeutic and prognostic role in the management of patients with COVID-19-related liver dysfunction. This review mainly focuses on the possible relationship between COVID-19 and liver dysfunction, nutritional and metabolic characteristics, nutritional status assessment, and nutrition therapy in patients with COVID-19 to provide a reference for the nutritionists while making evidence-based nutritional decisions in the era of COVID-19.
INTRODUCTION
Since December 2019, novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has been a major global health-related issue and has caused an unprecedented pandemic[1,2]. As of January 2, 2022, a total of 288867634 confirmed cases of COVID-19 and 5437636 deaths have been reported worldwide[3]. The liver is one of the main organs involved in nutrient metabolism, including protein synthesis, glycogen storage, and detoxification[4]. Studies have shown that angiotensin-converting enzyme 2 (ACE2), a functional receptor that allows the entry of SARS-CoV-2 into host cells, is expressed in cholangiocytes (59.7% of cells) and hepatocytes (2.6% of cells), indicating that COVID-19-related liver dysfunction may occur through direct cytotoxicity due to continuous viral replication within liver cells[5-8]. Additionally, COVID-19-related liver dysfunction was observed in approximately 20%-30% of the infected patients, especially in critically ill patients, and it was associated with poor outcomes[9-12]. Therefore, COVID-19-related liver dysfunction should not be ignored.
Meanwhile, almost all patients with liver disease, especially those at an advanced stage, have signs of malnutrition, including mineral and vitamin deficiency[13]. Micronutrient deficiencies may lead to impaired immune responses, including improper cytokine secretion, secretory antibody alterations, and antibody affinity, which increase the susceptibility to SARS-CoV-2 infection[14]. The malnutritional status of the host can also be a virulence factor for SARS-CoV-2 infection[15]. In addition, the nutritional status of COVID-19 patients with liver dysfunction is significantly related to the disease severity. An evaluation of the patient’s nutritional status should not be ignored owing to the implications of nutritional status on the susceptibility, course, severity, and responsiveness to therapies[16,17]. Tailored nutritional therapy prescribed after evaluating the nutritional status has also been an integral part of the comprehensive treatment for patients with COVID-19. This paper mainly focuses on a possible relationship between COVID-19 and liver dysfunction, nutritional and metabolic characteristics, nutritional status assessment, and nutrition therapy in patients with COVID-19.
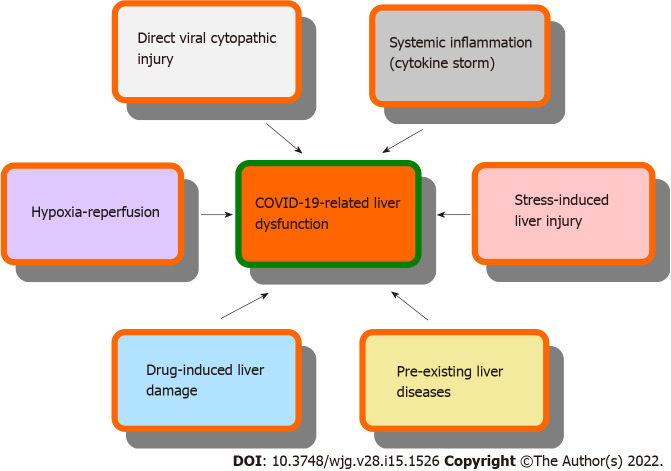
COVID-19 AND LIVER DYSFUNCTION
Liver dysfunction has been reported in a significant proportion of COVID-19 patients, especially in those with a severe illness[5]. Additionally, 2%-11% of patients with COVID-19 suffer from chronic liver disease. The prevalence of liver dysfunction in COVID-19 ranged from 3.75% to 59.04%; most studies reported a prevalence of 20%-30%[9-12]. A cross-sectional study reported that the prevalence of liver dysfunction in patients with COVID-19 was 59.04%; of the 62 patients, 44 (70.9%) were male and 18 (29.03%) were female. The average hospital stay of patients with liver dysfunction was 15 d (range, 10-16 d) compared with 10 d (range, 7-11 d) for patients with normal liver function[12]. In general, patients with COVID-19 who develop liver dysfunction are mostly male, elderly, and obese[5]. Another retrospective cohort study reported that of the 2273 COVID-19 patients at three hospitals in the NewYork-Presbyterian network, 45% suffered from mild liver injury, 21% from moderate liver injury, and 6.4% from severe liver injury. Patients with severe liver dysfunction had elevated levels of inflammatory markers, including ferritin and interleukin-6. They also suffered a worse clinical course, including higher rates of intensive care unit (ICU) admission (69%), intubation (65%), renal replacement therapy (33%), and mortality (42%)[10]. Several studies reported that the presence of liver dysfunction was closely related to higher admission, as well as higher ICU admission and/or death. The measurement of liver biochemical indexes might help the clinicians to evaluate the severity and prognosis of patients with COVID-19[18-23]. The mechanisms of COVID-19-related liver dysfunction may include direct viral cytopathic impairment, secondary liver injury resulting from a systemic inflammatory response or hypoxia-reperfusion, stress-induced liver injury, drug-induced liver damage, and, finally, exacerbation of the pre-existing liver diseases (Figure 1)[5,24-27]. Although COVID-19-related liver injuries are often transient and reversible, physicians, dietitians, and nutritionists need to take notice of the pre-existing liver damage, monitor liver function, improve supportive treatment, and prevent the occurrence of drug-induced liver injury[28].
Figure 1.
Mechanisms of coronavirus disease 2019-related liver dysfunction. COVID-19: Coronavirus disease 2019.
NUTRITIONAL AND METABOLIC CHARACTERISTICS OF PATIENTS WITH COVID-19
The main manifestation of patients with COVID-19 is high fever (range, 37.5-39.0 °C), which induces a catabolic state, including impaired glucose utilization, and increased energy utilization and protein breakdown. The metabolic effect of the temperature increase is said to be 10%-13% for every 1 °C increase, which should be considered in the nutritional recommendations[29]. Additionally, great influence on appetite and consciousness, and direct gastrointestinal damage may lead to nausea, vomiting, diarrhea, and feeding intolerance, which may adversely affect the nutrient intake and nutritional status[29]. Rouget et al[30] reported a high prevalence of malnutrition (37.5%) with 26% severe malnutrition according to the Global Leadership Initiative on Malnutrition (GLIM) criteria in a general cohort of patients with COVID-19. Bedock et al[31] reported that the overall incidence of malnutrition in COVID-19 patients was 42.1% (moderate: 23.7%; severe: 18.4%), while the incidence of malnutrition in patients admitted to the ICU reached 66.7% using the GLIM criteria. They found that lower albumin levels were related to a higher risk of admission to the ICU, and this association was independent of age and C-reactive protein levels. Li et al[32] found a high incidence (52.7%) of malnutrition according to the Mini Nutritional Assessment (MNA) in 182 elderly patients with COVID-19. Additionally, further regression analysis indicated that diabetes, low calf circumference, and low albumin level were independent risk factors for malnutrition. Malnutrition can impair the hepatic metabolic functions, and malnutrition alone can result in severe fatty liver[33].
NUTRITIONAL STATUS ASSESSMENT
According to the expert statements and practical guidance of the European Society for Clinical Nutrition and Metabolism for the nutritional management of individuals with SARS-CoV-2 infection, COVID-19 patients at risk of poor outcomes and high mortality, namely, the elderly and individuals with multiple comorbidities, should be assessed for malnutrition using the Malnutrition Universal Screening Tool (MUST) criteria; for hospitalized patients, the Nutrition Risk Screening 2002 (NRS-2002) criteria should be used[34]. Identification of the risk and presence of malnutrition should be conducted early in the overall assessment of all patients with COVID-19 using criteria such as MUST or NRS-2002. Ganatra et al[35] investigated and analyzed the nutritional risk and dietary intake of patients with COVID-19 and provided data supporting nutritional intervention using the NRS-2002 criteria. The Subjective Global Assessment criteria, the MNA criteria for geriatric patients, and the Nutrition Risk in Critically ill (NUTRIC) criteria for ICU patients have been used to further assess patients with COVID-19 and are accepted in clinical practice[36,37]. Zhang et al[38] reported that the modified NUTRIC score could be applied to nutritional risk evaluation and prognosis indication in critically ill patients with COVID-19[39]. Recently, the GLIM criteria for malnutrition diagnosis endorsed by clinical nutrition societies worldwide have been used to assess the nutritional status of patients with COVID-19[30,31].
NUTRITION THERAPY FOR COVID-19-RELATED LIVER DYSFUNCTION
Currently, the fight against the COVID-19 epidemic is entering a decisive stage[38]. Evidence-based and logical nutrition interventions can effectively improve the nutritional status and enhance the immunity, and they are essential for preventing and managing viral infections[40]. Patients with mild clinical manifestations or recovered patients who have returned home should rest in bed, carefully choose foods and recipes, maintain an adequate supply of energy and nutrients (including drinking water), improve their immune status, and speed up their recovery process. Severe, critically ill patients with COVID-19 often have loss of appetite and insufficient diet, which worsens their already weak immune system. For these patients, subsequent nutritional support should be adopted, and specific nutritional treatment plans should be formulated according to the general condition of the patient’s body, fluid intake, liver and kidney functions, and glucose and lipid metabolism[41]. Ten expert recommendations for medical nutritional therapy for patients with COVID-19 have been proposed by the Chinese Society for Parenteral and Enteral Nutrition to further promote patient recovery, improve their treatment effects, and reduce the mortality rate[42]. The main nutritional therapy recommendation is a five-step method, including diet and nutrition education, oral nutritional supplements, tube feeding, supplemental parenteral nutrition, and total parenteral nutrition[42].
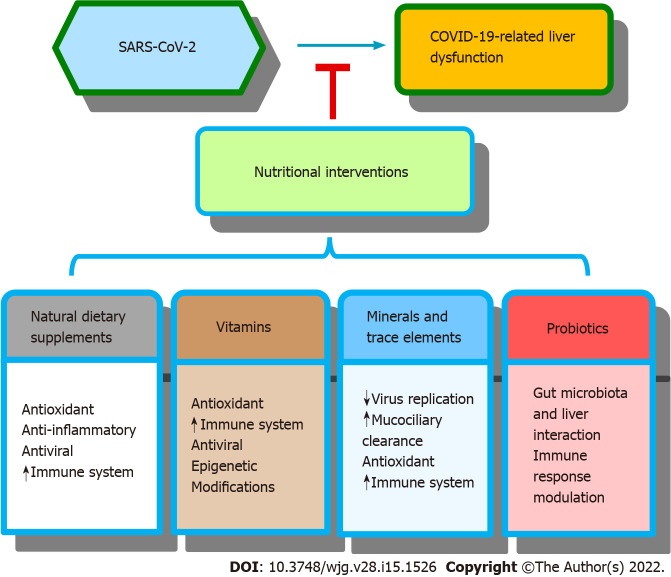
Numerous studies have found that nutrition therapy measures for patients with COVID-19 mainly include natural dietary supplements, vitamins, minerals, trace elements, and probiotics. A schematic summarizing the nutritional interventions for COVID-19-related liver dysfunction and their possible mechanisms is shown in Figure 2.
Figure 2.
Scheme showing the effects of nutritional interventions against coronavirus disease 2019-related liver dysfunction and their possible mechanisms. SARS-CoV-2: Severe acute respiratory syndrome coronavirus-2; COVID-19: Coronavirus disease 2019.
Natural dietary supplements
Rizzo et al[43] reviewed the properties of some vegetal products and their derivatives, including Lupin, salvia, garlic, and extra-virgin olive oil (EVOO), and they found that intake of these products or their extracts might prevent SARS-CoV-2 infection or improve the patients’ nutritional status. Lupin, salvia, garlic, and EVOO have anti-oxidant, anti-inflammatory, or antiviral properties and can recover the expression of ACE2 on the cell membrane, otherwise suppressed by SARS-CoV-2 binding and entry into the cytoplasm. Sikander et al[6] provided information and summarized the effects of natural bioactive antiviral, immunomodulatory, and hepatoprotective nutraceuticals (Silybum marianum, Solanum nigrum, Cichorium intybus, Allium sativum, Glycyrrhiza glabra, Phyllanthus amarus, Withania somnifera, Curcuma longa, and other hepatoprotective agents) that might be explored in managing COVID-19-induced liver dysfunction. Additionally, omega-3 long-chain polyunsaturated fatty acids (omega-3 LC-PUFAs) might also have effects on different stages of viral infection, including virus entry and replication, and help improve the inflammatory balance. An optimized omega-3 PUFA status, considering both the omega-3 precursor alpha-linolenic acid and long-chain derivatives, such as eicosapentaenoic acid and docosahexaenoic acid, might be helpful in preventing infectious diseases, including COVID-19[44].
Vitamins
Accumulating data have demonstrated that vitamin deficiency could be a risk factor for SARS-CoV-2 infection and it affects the COVID-19 susceptibility and prognosis[45]. For instance, vitamin A deficiency increases the severity of the disease, and appropriately timed intake during recovery reduces the death risk and speeds up the recovery. Studying interactions of vitamin A metabolism with SARS-CoV-2 infection may thus provide improved COVID-19 treatment[46]. Vitamin D deficiency may decrease the ability of the immune system to defend against COVID-19 and cause progression to severe disease[47]. Vitamin K deficiency may be a potentially modifiable risk factor for severe COVID-19; the mechanism is pneumonia-induced extrahepatic vitamin K consumption, resulting in accelerated elastic fiber damage and thrombosis[48]. Vitamins A, B, C, D, and E have been shown to be potentially beneficial in fighting against COVID-19 by exerting antioxidant and immunomodulatory effects, increasing natural barriers, and causing local paracrine signaling[49]. Additionally, vitamins can serve as epigenetic modifiers to enhance the immunity and reduce the inflammatory response in patients with COVID-19 and noncommunicable diseases. Combined vitamin therapy can improve the health in a more personalized manner or help in the prevention of infectious diseases in patients at risk for COVID-19[50]. Molecular simulations also suggest that vitamins, steroids, and retinoids may serve as ligands in the free fatty acid pocket of the SARS-CoV-2 spike protein and may thus provide a promising strategy for prophylaxis or therapeutics[51]. Supplements with vitamins A, B, C, D, E, and K may represent a cheap and safe approach and can be used as adjuvant therapy together with antiviral medicines in managing COVID-19[45,52]. However, caution must be exercised when recommending vitamin supplementation during the COVID-19 pandemic because the effects of hypervitaminosis can be serious, especially of fat-soluble vitamins A, D, and E[49]. More robust data from randomized controlled trials are needed in the near future.
Minerals and trace elements
Zinc (Zn) supplementation may inhibit SARS-CoV-2 virus replication, increase mucociliary clearance, and stimulate and activate the natural antiviral response of the immune system in patients with COVID-19[52]. Derwand et al[53] have also reported that the application of the combination therapy of Zn, low-dose hydroxychloroquine, and azithromycin to COVID-19 outpatients as early as possible after symptom onset resulted in significantly fewer hospitalizations and mortality rates.
Selenium (Se), one of the essential trace elements in the human body, has antioxidant and immunity-boosting effects that may induce a strong antiviral effect[54]. Recently, it was reported that the Se status was positively correlated with the survival rate of COVID-19 patients according to an exploratory study on the Se status in healthy individuals and patients with COVID-19 in the southern part of India[55]. Se has long been considered to help fight different viruses, such as herpes simplex virus type 1, influenza virus, Coxsackie virus, hepatitis C virus, and human immunodeficiency virus; the potential application of nano-Se may play an important role in combating COVID-19 in the future[54]. Nutrition inter-ventions that ensure an adequate status of Zn, Se, and vitamin D could protect against infection with the novel coronavirus SARS-CoV-2 and retard the course of COVID-19. Meanwhile, the initiation of adequate supplementation of Se in high-risk population immediately after the time of suspected SARS-CoV-2 infection is recommended[56].
Magnesium (Mg) is important for the activation of vitamin D and plays a protective role against oxidative stress. Mg deficiency increases the endothelial cell susceptibility to oxidative stress, induces endothelial dysfunction, decreases fibrinolysis, and increases coagulation. Mg-deficiency in animals and humans may lead to suppressed immune responses. However, upon supplementation with Mg, a partial or nearly full reversal of immunodeficiency occurs. Since Mg and vitamin D are important for immune function and cellular resilience, deficiency of either of the two micronutrients may contribute to cytokine storms in COVID-19 infection[57]. Furthermore, a low Mg status may induce the transition from mild to critical clinical manifestations of COVID-19[58]. Additionally, a recent review summarized the effect of Mg supplementation on various types of disorders and diseases, providing a reference supporting the possibility of Mg supplementation for supportive therapy of COVID-19 patients[59]. Additional epidemiological, basic, and clinical research on the potential role of Mg deficiency in COVID-19 is needed.
Copper (Cu) is an important micronutrient for both pathogens and hosts during viral infection. It has the capability of contact killing of several viruses, including SARS-CoV-2[60]. Enrichment of plasma Cu levels was hypothesized to boost both innate and adaptive immunity; Cu may have preventive and therapeutic effects against COVID-19[60]. A better understanding of Cu signaling, safety, assessment and interpretation methods, administration route, and dosage could open up new perspectives regarding the administration of therapeutic Cu to critically ill patients with COVID-19. Andreou et al[61] found that the combined use of Cu, colchicine, N-acetylcysteine, and nitric oxide (NO) with candidate antiviral agents, such as remdesivir or EIDD-2801, might be a potential treatment scheme for COVID-19. Physicians should consider Cu insufficiency in critically ill patients with COVID-19 and pay attention to Cu toxicity and estimate the adverse responses according to the Cu dose, and severity of Cu limitation, as well as the duration of Cu imbalance[62].
Probiotics
Beneficial live microbes in humans and animals are known as probiotics, and the chemical compounds that increase the probiotic growth rate are termed prebiotics[63]. SARS-CoV-2 infection is closely related to immune dysfunction and gut microbiota alterations. Delineating the mechanisms of probiotics, prebiotics, and a diet that promotes immunity and protects against SARS-CoV-2 presents possibilities of identifying microbial therapies to prevent and treat COVID-19[64]. Probiotics can exert beneficial effects by manipulating the gut microbiome, suppressing the gut opportunistic pathogens, decreasing the translocation of opportunistic organisms in the gut, activating the mucosal immunity, and modulating the innate and adaptive immune responses. Probiotics may be used as potential candidates to treat moderate and severe COVID-19 patients due to their benefits, including safety, ease of administration, high availability, and cost-effectiveness[65]. Emerging evidence has shown the role of gut microbiota in liver diseases through immune system cross-talk[66]. There is a lack of evidence that probiotics can directly inhibit SARS-CoV-2 infection, and probiotic therapy in COVID-19-related liver dysfunction is also not very effective. However, probiotics may be potentially helpful in the treatment of patients with severe COVID-19 and liver dysfunction[67].
CONCLUSION
Patients with COVID-19 usually have respiratory symptoms, but liver dysfunction is not an uncommon presentation and can lead to a delay in diagnosis and management[68]. Nutrition and immune statuses are two critical aspects of the successful fight against COVID-19[55]. Prevention, diagnosis, and treatment of malnutrition should be routinely recommended in the management of patients with COVID-19, especially in those with liver dysfunction[34,69]. Nutritional therapy is a basic treatment and one of the core contents of comprehensive treatment measures for patients with COVID-19. Evidence-based effective nutritional therapy should be based on reasonable and indexed nutritional evaluation[70].
Studies have shown that nutrition therapy measures, including natural dietary supplements, vitamins, minerals, trace elements, and probiotics, might have potential hepatoprotective effects against COVID-19-related liver dysfunction via their antioxidant, antiviral, anti-inflammatory, and positive immunomodulatory effects. Combination therapy strategies and personalized nutritional and behavioral approaches can be developed in the COVID-19 era[52,71]. Additionally, the risk of excessive intake of some nutrients due to the popularity of dietary supplements exists, and dietitians’ use of foods with protective effects against diseases has increased during the pandemic. Hence, consumers, patients, and nutritionists should be educated on the rational use of dietary supplements and health-protecting behaviors that can protect against COVID-19 for acute treatment, recovery, and prevention of chronic condition[72,73]. Moreover, additional tools and training are needed to optimize remote nutritional consultations, except for telemedicine, which have good prospects for dietary consultation[74]. Currently, many patients with COVID-19 have liver dysfunction, but nutritional studies related to this topic are not adequate. As nutritionists, it is our responsibility and obligation to facilitate further research in this area.
ACKNOWLEDGEMENTS
We thank Dr. Xu-Xia Li and other colleagues, the reviewers, and the editors for improving our paper.
Footnotes
Conflict-of-interest statement: There are no conflict of interest related to this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: March 12, 2021
First decision: April 17, 2021
Article in press: March 27, 2022
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Khan MKA, India S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
Contributor Information
Ming-Ke Wang, Department of Disease Control and Prevention, Naval Medical Center of PLA, Naval Medical University, Shanghai 200052, China.
Xue-Lu Yu, Department of Disease Control and Prevention, Naval Medical Center of PLA, Naval Medical University, Shanghai 200052, China.
Li-Yun Zhou, Department of Disease Control and Prevention, Naval Medical Center of PLA, Naval Medical University, Shanghai 200052, China.
Hong-Mei Si, Department of Disease Control and Prevention, Naval Medical Center of PLA, Naval Medical University, Shanghai 200052, China.
Ju-Fen Hui, Department of Disease Control and Prevention, Naval Medical Center of PLA, Naval Medical University, Shanghai 200052, China.
Deng-Yong Hou, Department of Disease Control and Prevention, Naval Medical Center of PLA, Naval Medical University, Shanghai 200052, China.
Wei-Peng Li, Department of Disease Control and Prevention, Naval Medical Center of PLA, Naval Medical University, Shanghai 200052, China.
Ji-Shun Yang, Medical Care Center, Naval Medical Center of PLA, Naval Medical University, Shanghai 200052, China. jasunyang@foxmail.com.
References
- 1.Abdulrab S, Al-Maweri S, Halboub E. Ursodeoxycholic acid as a candidate therapeutic to alleviate and/or prevent COVID-19-associated cytokine storm. Med Hypotheses. 2020;143:109897. doi: 10.1016/j.mehy.2020.109897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahase E. Covid-19: WHO declares pandemic because of "alarming levels" of spread, severity, and inaction. BMJ. 2020;368:m1036. doi: 10.1136/bmj.m1036. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Weekly epidemiological update on COVID-19 - 6 January 2022. [cited 6 January 2022]. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---6-january-2022 .
- 4.Yasutake K, Kohjima M, Nakashima M, Kotoh K, Nakamuta M, Enjoji M. Nutrition therapy for liver diseases based on the status of nutritional intake. Gastroenterol Res Pract. 2012;2012:859697. doi: 10.1155/2012/859697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cichoż-Lach H, Michalak A. Liver injury in the era of COVID-19. World J Gastroenterol. 2021;27:377–390. doi: 10.3748/wjg.v27.i5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sikander M, Malik S, Rodriguez A, Yallapu MM, Narula AS, Satapathy SK, Dhevan V, Chauhan SC, Jaggi M. Role of Nutraceuticals in COVID-19 Mediated Liver Dysfunction. Molecules. 2020;25 doi: 10.3390/molecules25245905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loganathan S, Kuppusamy M, Wankhar W, Gurugubelli KR, Mahadevappa VH, Lepcha L, Choudhary AK. Angiotensin-converting enzyme 2 (ACE2): COVID 19 gate way to multiple organ failure syndromes. Respir Physiol Neurobiol. 2021;283:103548. doi: 10.1016/j.resp.2020.103548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Merola E, Pravadelli C, de Pretis G. Prevalence of liver injury in patients with coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Acta Gastroenterol Belg. 2020;83:454–460. [PubMed] [Google Scholar]
- 10.Phipps MM, Barraza LH, LaSota ED, Sobieszczyk ME, Pereira MR, Zheng EX, Fox AN, Zucker J, Verna EC. Acute Liver Injury in COVID-19: Prevalence and Association with Clinical Outcomes in a Large U.S. Cohort. Hepatology. 2020;72:807–817. doi: 10.1002/hep.31404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jothimani D, Venugopal R, Abedin MF, Kaliamoorthy I, Rela M. COVID-19 and the liver. J Hepatol. 2020;73:1231–1240. doi: 10.1016/j.jhep.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaushik A, Wani SN, Baba MA, Agarwal AK. Prevalence of Abnormal Liver Function Tests in COVID-19 Patients at a Tertiary Care Centre. J Assoc Physicians India. 2020;68:73–75. [PubMed] [Google Scholar]
- 13.Hanje AJ, Fortune B, Song M, Hill D, McClain C. The use of selected nutrition supplements and complementary and alternative medicine in liver disease. Nutr Clin Pract. 2006;21:255–272. doi: 10.1177/0115426506021003255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muthuvattur Pallath M, Ahirwar AK, Chandra Tripathi S, Asia P, Sakarde A, Gopal N. COVID-19 and nutritional deficiency: a review of existing knowledge. Horm Mol Biol Clin Investig. 2021;42:77–85. doi: 10.1515/hmbci-2020-0074. [DOI] [PubMed] [Google Scholar]
- 15.Briguglio M, Pregliasco FE, Lombardi G, Perazzo P, Banfi G. The Malnutritional Status of the Host as a Virulence Factor for New Coronavirus SARS-CoV-2. Front Med (Lausanne) 2020;7:146. doi: 10.3389/fmed.2020.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cai CJ. Nutritional therapy in patients with liver dysfunction. Chin J Pract Surg. 2019;39:79–84. [Google Scholar]
- 17.Fedele D, De Francesco A, Riso S, Collo A. Obesity, malnutrition, and trace element deficiency in the coronavirus disease (COVID-19) pandemic: An overview. Nutrition. 2021;81:111016. doi: 10.1016/j.nut.2020.111016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu Y, Li H, Guo X, Yoshida EM, Mendez-Sanchez N, Levi Sandri GB, Teschke R, Romeiro FG, Shukla A, Qi X. Incidence, risk factors, and prognosis of abnormal liver biochemical tests in COVID-19 patients: a systematic review and meta-analysis. Hepatol Int. 2020;14:621–637. doi: 10.1007/s12072-020-10074-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye L, Chen B, Wang Y, Yang Y, Zeng J, Deng G, Deng Y, Zeng F. Prognostic value of liver biochemical parameters for COVID-19 mortality. Ann Hepatol. 2021;21:100279. doi: 10.1016/j.aohep.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin L, Jiang X, Zhang Z, Huang S, Fang Z, Gu Z, Gao L, Shi H, Mai L, Liu Y, Lin X, Lai R, Yan Z, Li X, Shan H. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69:997–1001. doi: 10.1136/gutjnl-2020-321013. [DOI] [PubMed] [Google Scholar]
- 21.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hajifathalian K, Krisko T, Mehta A, Kumar S, Schwartz R, Fortune B, Sharaiha RZ WCM-GI research group∗. Gastrointestinal and Hepatic Manifestations of 2019 Novel Coronavirus Disease in a Large Cohort of Infected Patients From New York: Clinical Implications. Gastroenterology. 2020;159:1137–1140.e2. doi: 10.1053/j.gastro.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, Wang T, Guo W, Chen J, Ding C, Zhang X, Huang J, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang C, Li Q, Xu W, Chen L. Molecular and cellular mechanisms of liver dysfunction in COVID-19. Discov Med. 2020;30:107–112. [PubMed] [Google Scholar]
- 25.Lizardo-Thiebaud MJ, Cervantes-Alvarez E, Limon-de la Rosa N, Tejeda-Dominguez F, Palacios-Jimenez M, Méndez-Guerrero O, Delaye-Martinez M, Rodriguez-Alvarez F, Romero-Morales B, Liu WH, Huang CA, Kershenobich D, Navarro-Alvarez N. Direct or Collateral Liver Damage in SARS-CoV-2-Infected Patients. Semin Liver Dis. 2020;40:321–330. doi: 10.1055/s-0040-1715108. [DOI] [PubMed] [Google Scholar]
- 26.Li J, Fan JG. Characteristics and Mechanism of Liver Injury in 2019 Coronavirus Disease. J Clin Transl Hepatol. 2020;8:13–17. doi: 10.14218/JCTH.2020.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhong P, Xu J, Yang D, Shen Y, Wang L, Feng Y, Du C, Song Y, Wu C, Hu X, Sun Y. COVID-19-associated gastrointestinal and liver injury: clinical features and potential mechanisms. Signal Transduct Target Ther. 2020;5:256. doi: 10.1038/s41392-020-00373-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang RX, Zheng RD, Fan JG. Etiology and management of liver injury in patients with COVID-19. World J Gastroenterol. 2020;26:4753–4762. doi: 10.3748/wjg.v26.i32.4753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chapple LS, Fetterplace K, Asrani V, Burrell A, Cheng AC, Collins P, Doola R, Ferrie S, Marshall AP, Ridley EJ. Nutrition management for critically and acutely unwell hospitalised patients with coronavirus disease 2019 (COVID-19) in Australia and New Zealand. Aust Crit Care. 2020;33:399–406. doi: 10.1016/j.aucc.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rouget A, Vardon-Bounes F, Lorber P, Vavasseur A, Marion O, Marcheix B, Lairez O, Balardy L, Fourcade O, Conil JM, Minville V. Prevalence of malnutrition in coronavirus disease 19: the NUTRICOV study. Br J Nutr. 2021;126:1296–1303. doi: 10.1017/S0007114520005127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bedock D, Bel Lassen P, Mathian A, Moreau P, Couffignal J, Ciangura C, Poitou-Bernert C, Jeannin AC, Mosbah H, Fadlallah J, Amoura Z, Oppert JM, Faucher P. Prevalence and severity of malnutrition in hospitalized COVID-19 patients. Clin Nutr ESPEN. 2020;40:214–219. doi: 10.1016/j.clnesp.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li T, Zhang Y, Gong C, Wang J, Liu B, Shi L, Duan J. Prevalence of malnutrition and analysis of related factors in elderly patients with COVID-19 in Wuhan, China. Eur J Clin Nutr. 2020;74:871–875. doi: 10.1038/s41430-020-0642-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bischoff SC, Bernal W, Dasarathy S, Merli M, Plank LD, Schütz T, Plauth M. ESPEN practical guideline: Clinical nutrition in liver disease. Clin Nutr. 2020;39:3533–3562. doi: 10.1016/j.clnu.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 34.Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Krznaric Z, Nitzan D, Pirlich M, Singer P endorsed by the ESPEN Council. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr. 2020;39:1631–1638. doi: 10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ganatra S, Hammond SP, Nohria A. The Novel Coronavirus Disease (COVID-19) Threat for Patients With Cardiovascular Disease and Cancer. JACC CardioOncol. 2020;2:350–355. doi: 10.1016/j.jaccao.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martins PM, Gomes TLN, Franco EP, Vieira LL, Pimentel GD. High neutrophil-to-lymphocyte ratio at intensive care unit admission is associated with nutrition risk in patients with COVID-19. JPEN J Parenter Enteral Nutr. 2021 doi: 10.1002/jpen.2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ali AM, Kunugi H. Approaches to Nutritional Screening in Patients with Coronavirus Disease 2019 (COVID-19) Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18052772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang P, He Z, Yu G, Peng D, Feng Y, Ling J, Wang Y, Li S, Bian Y. The modified NUTRIC score can be used for nutritional risk assessment as well as prognosis prediction in critically ill COVID-19 patients. Clin Nutr. 2021;40:534–541. doi: 10.1016/j.clnu.2020.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nutrition Management in Critically Ill Project Team, Chinese Nutrition Society for Clinical Nutrition. Recommendations for nutrition therapy in critically ill COVID-19 patients. Chin J Clin Med. 2020;27:167–174. [Google Scholar]
- 40.Jayawardena R, Sooriyaarachchi P, Chourdakis M, Jeewandara C, Ranasinghe P. Enhancing immunity in viral infections, with special emphasis on COVID-19: A review. Diabetes Metab Syndr. 2020;14:367–382. doi: 10.1016/j.dsx.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Law S, Leung AW, Xu C. Severe acute respiratory syndrome (SARS) and coronavirus disease-2019 (COVID-19): From causes to preventions in Hong Kong. Int J Infect Dis. 2020;94:156–163. doi: 10.1016/j.ijid.2020.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chinese Society for Parenteral and Enteral Nutrition. Expert advice of medical nutritional treatment for novel coronavirus-caused pneumonia patients. Chin Arch Gen Surg. 2020;14:1. [Google Scholar]
- 43.Rizzo A, Sciorsci RL, Magrone T, Jirillo E. Exploitation of Some Natural Products for the Prevention and/or Nutritional Treatment of SARS-CoV2 Infection. Endocr Metab Immune Disord Drug Targets. 2021;21:1171–1182. doi: 10.2174/1871530320999200831231029. [DOI] [PubMed] [Google Scholar]
- 44.Weill P, Plissonneau C, Legrand P, Rioux V, Thibault R. May omega-3 fatty acid dietary supplementation help reduce severe complications in Covid-19 patients? Biochimie. 2020;179:275–280. doi: 10.1016/j.biochi.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allegra A, Tonacci A, Pioggia G, Musolino C, Gangemi S. Vitamin deficiency as risk factor for SARS-CoV-2 infection: correlation with susceptibility and prognosis. Eur Rev Med Pharmacol Sci. 2020;24:9721–9738. doi: 10.26355/eurrev_202009_23064. [DOI] [PubMed] [Google Scholar]
- 46.Stephensen CB, Lietz G. Vitamin A in resistance to and recovery from infection: relevance to SARS-CoV2. Br J Nutr. 2021;126:1663–1672. doi: 10.1017/S0007114521000246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Im JH, Je YS, Baek J, Chung MH, Kwon HY, Lee JS. Nutritional status of patients with COVID-19. Int J Infect Dis. 2020;100:390–393. doi: 10.1016/j.ijid.2020.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dofferhoff ASM, Piscaer I, Schurgers LJ, Visser MPJ, van den Ouweland JMW, de Jong PA, Gosens R, Hackeng TM, van Daal H, Lux P, Maassen C, Karssemeijer EGA, Vermeer C, Wouters EFM, Kistemaker LEM, Walk J, Janssen R. Reduced Vitamin K Status as a Potentially Modifiable Risk Factor of Severe Coronavirus Disease 2019. Clin Infect Dis. 2021;73:e4039–e4046. doi: 10.1093/cid/ciaa1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jovic TH, Ali SR, Ibrahim N, Jessop ZM, Tarassoli SP, Dobbs TD, Holford P, Thornton CA, Whitaker IS. Could Vitamins Help in the Fight Against COVID-19? Nutrients. 2020;12 doi: 10.3390/nu12092550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Singh V. Can Vitamins, as Epigenetic Modifiers, Enhance Immunity in COVID-19 Patients with Non-communicable Disease? Curr Nutr Rep. 2020;9:202–209. doi: 10.1007/s13668-020-00330-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shoemark DK, Colenso CK, Toelzer C, Gupta K, Sessions RB, Davidson AD, Berger I, Schaffitzel C, Spencer J, Mulholland AJ. Molecular Simulations suggest Vitamins, Retinoids and Steroids as Ligands of the Free Fatty Acid Pocket of the SARS-CoV-2 Spike Protein*. Angew Chem Int Ed Engl. 2021;60:7098–7110. doi: 10.1002/anie.202015639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Islam MT, Quispe C, Martorell M, Docea AO, Salehi B, Calina D, Reiner Ž, Sharifi-Rad J. Dietary supplements, vitamins and minerals as potential interventions against viruses: Perspectives for COVID-19. Int J Vitam Nutr Res. 2022;92:49–66. doi: 10.1024/0300-9831/a000694. [DOI] [PubMed] [Google Scholar]
- 53.Derwand R, Scholz M, Zelenko V. COVID-19 outpatients: early risk-stratified treatment with zinc plus low-dose hydroxychloroquine and azithromycin: a retrospective case series study. Int J Antimicrob Agents. 2020;56:106214. doi: 10.1016/j.ijantimicag.2020.106214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.He L, Zhao J, Wang L, Liu Q, Fan Y, Li B, Yu YL, Chen C, Li YF. Using nano-selenium to combat Coronavirus Disease 2019 (COVID-19)? Nano Today. 2021;36:101037. doi: 10.1016/j.nantod.2020.101037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Majeed M, Nagabhushanam K, Gowda S, Mundkur L. An exploratory study of selenium status in healthy individuals and in patients with COVID-19 in a south Indian population: The case for adequate selenium status. Nutrition. 2021;82:111053. doi: 10.1016/j.nut.2020.111053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alexander J, Tinkov A, Strand TA, Alehagen U, Skalny A, Aaseth J. Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19. Nutrients. 2020;12 doi: 10.3390/nu12082358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.DiNicolantonio JJ, O'Keefe JH. Magnesium and Vitamin D Deficiency as a Potential Cause of Immune Dysfunction, Cytokine Storm and Disseminated Intravascular Coagulation in covid-19 patients. Mo Med. 2021;118:68–73. [PMC free article] [PubMed] [Google Scholar]
- 58.Iotti S, Wolf F, Mazur A, Maier JA. The COVID-19 pandemic: is there a role for magnesium? Magnes Res. 2020;33:21–27. doi: 10.1684/mrh.2020.0465. [DOI] [PubMed] [Google Scholar]
- 59.Tang CF, Ding H, Jiao RQ, Wu XX, Kong LD. Possibility of magnesium supplementation for supportive treatment in patients with COVID-19. Eur J Pharmacol. 2020;886:173546. doi: 10.1016/j.ejphar.2020.173546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Raha S, Mallick R, Basak S, Duttaroy AK. Is copper beneficial for COVID-19 patients? Med Hypotheses. 2020;142:109814. doi: 10.1016/j.mehy.2020.109814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Andreou A, Trantza S, Filippou D, Sipsas N, Tsiodras S. COVID-19: The Potential Role of Copper and N-acetylcysteine (NAC) in a Combination of Candidate Antiviral Treatments Against SARS-CoV-2. In Vivo. 2020;34:1567–1588. doi: 10.21873/invivo.11946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fooladi S, Matin S, Mahmoodpoor A. Copper as a potential adjunct therapy for critically ill COVID-19 patients. Clin Nutr ESPEN. 2020;40:90–91. doi: 10.1016/j.clnesp.2020.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khaled JMA. Probiotics, prebiotics, and COVID-19 infection: A review article. Saudi J Biol Sci. 2021;28:865–869. doi: 10.1016/j.sjbs.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hu J, Zhang L, Lin W, Tang W, Chan FKL, Ng SC. Review article: Probiotics, prebiotics and dietary approaches during COVID-19 pandemic. Trends Food Sci Technol. 2021;108:187–196. doi: 10.1016/j.tifs.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Angurana SK, Bansal A. Probiotics and Coronavirus disease 2019: think about the link. Br J Nutr. 2021;126:1564–1570. doi: 10.1017/S000711452000361X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Scarpellini E, Fagoonee S, Rinninella E, Rasetti C, Aquila I, Larussa T, Ricci P, Luzza F, Abenavoli L. Gut Microbiota and Liver Interaction through Immune System Cross-Talk: A Comprehensive Review at the Time of the SARS-CoV-2 Pandemic. J Clin Med. 2020;9 doi: 10.3390/jcm9082488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Aguila EJT, Lontok MADC, Aguila EJT. Letter: role of probiotics in the COVID-19 pandemic. Aliment Pharmacol Ther. 2020;52:931–932. doi: 10.1111/apt.15898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kamani L. What gastroenterologists should know during COVID-19 Pandemic! Pak J Med Sci. 2020;36:S124–S125. doi: 10.12669/pjms.36.COVID19-S4.2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cervantes-Pérez E, Cervantes-Guevara G, Martínez-Soto Holguín MC, Cervantes-Pérez LA, Cervantes-Pérez G, Cervantes-Cardona GA, González-Ojeda A, Fuentes-Orozco C, Ramírez-Ochoa S. Medical Nutrition Therapy in Hospitalized Patients With SARS-CoV-2 (COVID-19) Infection in a Non-critical Care Setting: Knowledge in Progress. Curr Nutr Rep. 2020;9:309–315. doi: 10.1007/s13668-020-00337-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yu KY, Shi HP. Explanation of expert recommendations on medical nutrition for patients with novel coronavirus pneumonia. Zhonghua Yi Xue Za Zhi. 2020;100:724–728. doi: 10.3760/cma.j.cn112137-20200205-00196. [DOI] [PubMed] [Google Scholar]
- 71.Formisano E, Di Maio P, Ivaldi C, Sferrazzo E, Arieta L, Bongiovanni S, Panizzi L, Valentino E, Pasta A, Giudice M, Demontis S. Nutritional therapy for patients with coronavirus disease 2019 (COVID-19): Practical protocol from a single center highly affected by an outbreak of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Nutrition. 2021;82:111048. doi: 10.1016/j.nut.2020.111048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hamulka J, Jeruszka-Bielak M, Górnicka M, Drywień ME, Zielinska-Pukos MA. Dietary Supplements during COVID-19 Outbreak. Results of Google Trends Analysis Supported by PLifeCOVID-19 Online Studies. Nutrients. 2020;13 doi: 10.3390/nu13010054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kamarli Altun H, Karacil Ermumcu MS, Seremet Kurklu N. Evaluation of dietary supplement, functional food and herbal medicine use by dietitians during the COVID-19 pandemic. Public Health Nutr. 2021;24:861–869. doi: 10.1017/S1368980020005297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kaufman-Shriqui V, Sherf-Dagan S, Boaz M, Birk R. Virtual nutrition consultation: what can we learn from the COVID-19 pandemic? Public Health Nutr. 2021;24:1166–1173. doi: 10.1017/S1368980021000148. [DOI] [PMC free article] [PubMed] [Google Scholar]