Abstract
Purpose
Dietary diversity is a key proxy indicator of nutrient adequacy; however, limited studies have been done on it among pregnant women in Ethiopia. The study aimed to examine the prevalence of sub-optimal dietary diversity and its associated factors among pregnant women in Gurage zone, South Central Ethiopia.
Materials and Methods
A mixed-method approach, a longitudinal study complemented with an exploratory qualitative study, was conducted. In the longitudinal study, a consecutively included sample of 668 pregnant women was followed in three rounds of survey. Dietary diversity was assessed using the minimum dietary diversity score for women (MDD-W) tool. The average of three dietary diversity scores was used to define overall diversity. Consuming less than 5 of 10 standard food groups was considered as suboptimal dietary diversity. Multivariable logistic regression analysis was used to identify predictors of suboptimal dietary diversity. Qualitative data were analysed using the thematic analysis method.
Results
During the 16 to 20, 28 to 29 and 36 to 37 weeks of gestation surveys, 75.0, 78.7 and 76.5% of the women had sub-optimal dietary diversity. In aggregate, 84.4% (95% CI: 81.6, 87.3) of the women had sub-optimal dietary diversity. Rural residents (AOR: 1.91, 95% CI: 1.01, 3.62), women with no formal education (AOR: 5.51, 95% CI: 1.96, 15.53) and from food insecure households (AOR: 2.44, 95% CI: 1.07, 5.59) had higher odds of suboptimal dietary diversity. Women with higher nutritional knowledge (AOR: 0.92, 95% CI: 0.87, 0.98) were less likely to have suboptimal dietary diversity. Food taboos, poor nutritional literacy and pregnancy complications were also reported as factors affecting dietary diversity.
Conclusion
Majority of pregnant women in the area had sub-optimal dietary diversity. Improving the socio-economic status and promoting nutrition knowledge may improve women’s dietary diversity.
Keywords: dietary diversity, pregnant women, maternal nutrition, Ethiopia
Introduction
A healthy diet is essential at all times in life but particularly during pregnancy. Pregnant women are nutritionally vulnerable because of increased demand for most nutrients.1,2 Consuming a variety of food items during pregnancy plays a major role in ensuring optimal maternal and fetal nutrition. Taking a diverse diet during pregnancy helps to prevent nutritional deficiencies and their grave consequences, including increased risk of maternal mortality, malformation and low birth weight.1
Dietary diversity is eating of varieties of the food item and considered as the proxy measure of micronutrient adequacy.2,3 Among women of reproductive age, dietary diversity is commonly measured using the Minimum Dietary Diversity for Women (MDD-W) scale developed by the Food and Agriculture Organization of United Nations (FAO). Existing evidence suggests that dietary diversity is associated with nutrient adequacy among women4,5 and reduced risk of undesirable birth outcomes.6–8 Diversifying diet is one of the most sustainable approaches for tackling micronutrient deficiencies in any stage of life, including pregnancy. Dietary diversity ensures optimal intake of essential nutrients for maintaining good health both for the mother and fetus.2
Despite different international and national strategies to ensure a healthy diet for all, more than half of pregnant women in low- and middle-income countries (LMIC) are consuming an inadequately diverse diet.9 Diets in LMICs are poor in diversity and lack optimal nutrient density. Suboptimal consumption of micronutrient-dense foods, including animal-source foods, fruits and vegetables, puts pregnant women at risk of multiple micronutrient deficiencies.9 Micronutrient deficiency in pregnancy is common and remains a major public health problem in low- and middle-income countries.10,11
Previous studies done in different regions of Ethiopia have shown a high prevalence of inadequate dietary diversity among pregnant women. The reported prevalence of sub-optimal dietary diversity ranged from 39% in Tigray to 74.5% in Oromia region.12–16 The pooled national prevalence of inadequate dietary diversity was 53%.17 These findings suggest that more than half of all pregnant women in Ethiopia were getting an inadequately diversified diet.
Women in developing countries have a higher burden of nutrient inadequacy because of several underlying factors such as adolescent pregnancy, high fertility rate, short interval between pregnancies, and poor-quality diet.18 Other factors, such as formal education, occupation, family wealth status, antenatal clinic (ANC) visits, food taboos and nutritional knowledge were also significantly associated with dietary diversity among pregnant women.19
Nutritional status and dietary diversity of pregnant women are important predictors of pregnancy outcome. Suboptimal dietary diversity or inadequate intake of micronutrient is significantly associated with adverse maternal and fetal outcomes.20,21 Studies showed adverse pregnancy outcomes such as inadequate gestational weight gain, maternal anemia, low birth weight and preterm are associated with inadequate dietary diversity.7,22
Ethiopia is characterized by diverse agro-ecological and cultural variations leading to diverse dietary practices. In view of this, the study aimed to assess the prevalence and correlates of sub-optimal dietary diversity among pregnant women in Gurage zone, South Central Ethiopia. Unlike previous studies that measured dietary diversity at one point in time, we assessed dietary diversity in three follow-up surveys implemented during the second and third trimesters.
Materials and Methods
Study Setting
The Gurage Zone is one of the zones in the Southern Nations, Nationalities and Peoples Region of Ethiopia with its center at Wolkite town located 158 km west of Addis Ababa. In terms of population, it is a densely populated zone in Ethiopia with 441 people per square kilometer. It is composed of 14 districts and 5 town administrations.23 The zone has seven hospitals (two non-governmental and five governmental) and 72 health centers. The main source of food and economic activity is rain-fed agriculture. Common staple foods are enset (Ensete ventricosum), teff in the form of injera, green cabbage, maize and other cereals.23,24
Study Design and Population
Data were collected through an institution-based longitudinal study supplemented by an exploratory qualitative study. The study population was all pregnant women attending antenatal care (ANC) in selected districts of the Gurage zone. Women in their second trimester (16–20 weeks) with a singleton pregnancy, permanent residents (lived at least 1 year) and aged 15–49 years were included in the study. Pregnant women with known medical conditions like HIV/AIDS and diabetes mellitus were excluded.
The participants in the focus group discussion (FGD) were pregnant women, health extension workers and women’s development army. The health extension workers are trained professionals providing essential health services at health post. The women’s development armies are community health workers with no formal professional education but chosen as a leader to serve five households within the same neighborhood based on their clear understanding and practice of health extension packages.25 The key informants selected for in-depth interviews were heads of health centers and heads of district health departments.
Sample Size Determination
The sample size was calculated using single population proportion formula by considering the following assumption: 55.2% prevalence of inadequate dietary diversity,13 95% of confidence level and 5% marginal errors. To accommodate for the multistage nature of the study, we applied a design effect of 1.5. Furthermore, 20% was added for compensating possible non-response. Ultimately, a sample size of 684 was reached.
There were 6 FGDs, involving pregnant women, health extension workers and women’s development army. Eleven participants, including 3 heads of health centers, 3 heads of the district health office, 2 maternal and child nutrition coordinators and 3 community elders were contacted for in-depth interviews. The final sample of the qualitative study was 55.
Sampling Procedure
For the quantitative study, a multistage cluster sampling method was used to select pregnant women. Initially, the study area was divided into rural districts and urban town administrations. Six districts and two town administrations were taken to represent 14 districts and 5 town administrations within the Zone. Two representative healthy facilities were randomly selected from each district. Then, the sample size was allocated proportionally to 16 selected health facilities. The participants who fulfilled the eligibility criteria were consecutively included until the sample size was filled and those samples followed up to the end of pregnancy. For the qualitative study, a purposive sampling method was used to select participants whom we think could provide rich information on the existing maternal nutrition situation in the study area.
Quantitative Data Collection
An interviewer-administered structured questionnaire that was prepared partly by reviewing several published articles13–15,26,27 and partly by adopting standardized data collection tools2,28 was used for quantitative data collection. The questionnaire has different sections on socio-demographic variables, obstetric history, household food insecurity, maternal dietary diversity, maternal nutrition knowledge and practice.
The questionnaire was prepared in the English language and translated to the local Amharic language. The consistency was checked by translating it back to English and was edited by a person with good knowledge of both languages. Data were collected by trained and supervised enumerators. The questionnaire was pretested among pregnant women not participating in the actual study but living in a similar setting. The actual data collection was done among women at their 16 to 20 weeks of gestation and maternal dietary diversity score was repeated in two subsequent phases; 28 to 29 weeks and 36 to 37 weeks of gestation. The completeness of data was checked each day at the end of data collection. Incomplete data was traced back and edited accordingly.
Variables of the Study
The dependent variable of the study was maternal dietary diversity measured using the standard FAO’s minimum dietary diversity for women (MDD-W).2 This section of the questionnaire listed ten groups of food items: 1. Grains, white roots and tubers, 2. Pulses (beans, peas, and lentils), 3. Nuts and seeds, 4. Dairy products, 5. Meat, poultry, and fish, 6. Egg, 7. Dark green leafy vegetables, 8. Other vitamin A-rich fruits and vegetables, 9. Other vegetables, 10. Other fruits. Participants were asked whether they consumed items from each group in the preceding day from when they woke up in the morning, through the day and night for the subsequent 24 hours. Each food group consumed (scored 1) was summed up to a score ranging from 0 to 10. A score above 4 (women who consumed items from five or more groups) was categorized as optimal dietary diversity while those consuming food items from less than five groups were considered as having suboptimal dietary diversity.2,18 The average of sum of three dietary diversity scores was considered to determine overall dietary diversity across pregnancy.
The independent variables included a basic socio-demographic profile of the study subjects including place of residence (urban or rural), marital status, religion, educational level, occupation, husband’s occupation, husband’s education, family size and monthly income, and reproductive history that were assessed using standard demographic and health survey (DHS) questionnaire.29
The other independent variable was household food insecurity that was assessed using the household food insecurity access scale (HFIAS). The scale had nine questions intended to assess the experience of household food insecurity that occurred within the previous month.30 The households were categorized into 4 levels of food insecurity: food secure and mildly, moderately, and severely food insecure as per guidelines.28
Maternal nutritional knowledge and practice-related variables were also considered as independent variables of the study. Maternal nutritional knowledge was assessed using a non-standard scale containing ten items. Then, ten nutrition-related questions asked were recorded as complete answers (scored 2), incomplete answers (scored 1) and wrong answers (scored 0). Ultimately, maternal nutritional knowledge was scored out of twenty. Maternal dietary practices including meal frequency, meal skip, avoidances of food, craving and household access to food aid were also assessed. Women asked whether they were getting at least three meals per day or not and other dietary practice variables were assessed by yes or no questions.
Qualitative Data Collection
A guide was used for the in-depth interviews and focus group discussions to explore factors contributing to dietary diversity among pregnant women, available in Appendix 1. The interview guide explored dietary practice in terms of diversity, knowledge on the advantages of a diversified diet and factors that influence dietary diversity during pregnancy. During data collection, each question was probed for further exploration and the responses were recorded in a notebook and digital electronic recorder for later transcription.
Quantitative Data Processing and Analysis
The quantitative data were entered and cleaned using Epi-data statistical software and then exported to SPSS version 24. Frequency distribution, measure of central tendency and dispersion were used to describe the data. Numeric variables were checked for normality of the distribution by using probability plot and Shapiro Wilk test.
The association between dependent and independent variables was assessed using bi-variable and multivariable logistic regression. To test independent predictors of dietary diversity, all independent variables with a p-value of less than 0.25 in the bi-variable logistic regression model were considered as candidate variables for the multivariable analysis. Then the relationship was presented using adjusted odds ratio (AOR) with its corresponding 95% confidence interval.
Qualitative Data Management and Analysis
For the qualitative study, research assistants who were familiar with the local language and culture were involved. The professional’s word-by-word transcribing of the data from audio records was done in the local language each day at the end of data collection. Then, the transcribed information was translated from the local Amharic language to the English language in the word document. The data were analyzed by thematic analysis using NVIVO-version 11 software. After re-organizing data, an exploration such as the summary of word frequency and word cloud was done. The relevant information was coded and categorized into different themes. Final analysis was done by exploring different factors and creating a hierarchy chart of themes.
Results
Socio-Demographic Characteristics of Participants
Of the 684 women who have participated in the first phase of data collection, 668 (97.7%) were available in three consecutive contacts. The age range of the participants was 18 to 41 years [mean 25.6; SD 4.9]. Two hundred sixty-six (39.9%) participants were residents of rural areas and the rest (60.2%) were from urban areas. Nearly two-thirds (65.9%) of the respondents were of Gurage ethnicity and 45.2% were Muslims. The vast majority (98.5%) were married and 37.4% of women had secondary school education or higher. Among the participants, 237 (35.5%) were nulliparous, 196 (29.6%) were primiparous and the rest, 233 (34.8%) were multiparous (Table 1).
Table 1.
Socio-Demographic Characteristics of Pregnant Women Attending Antenatal Clinics in the Gurage Zone, Southern Ethiopia, 2021
| Variables | Frequency (n) | Percentage (%) |
|---|---|---|
| Age group (years) | ||
| 18−24 | 292 | 43.7 |
| 25–34 | 334 | 50.0 |
| 35 and above | 42 | 6.3 |
| Residence | ||
| Urban | 402 | 60.2 |
| Rural | 266 | 39.8 |
| Ethnicity | ||
| Gurage | 440 | 65.9 |
| Amhara | 109 | 16.5 |
| Oromo | 40 | 6.0 |
| Silte | 21 | 3.1 |
| Others | 58 | 8.5 |
| Educational attainment | ||
| No formal education | 188 | 28.1 |
| Primary education | 230 | 34.4 |
| Secondary education | 155 | 23.2 |
| Tertiary education | 95 | 14.2 |
| Religion | ||
| Muslim | 302 | 45.2 |
| Orthodox | 281 | 42.1 |
| Protestant | 63 | 9.4 |
| Others | 22 | 3.3 |
| Occupation | ||
| Housewife | 394 | 59.0 |
| Merchant | 81 | 12.1 |
| Government employed | 72 | 10.8 |
| Farmer | 75 | 11.2 |
| Others | 46 | 6.9 |
| Marital status | ||
| Married | 658 | 98.5 |
| Not every married | 10 | 1.5 |
| Husbands’ occupation (n=658) | ||
| Farmer | 192 | 28.7 |
| Merchant | 138 | 20.7 |
| Government employed | 121 | 18.3 |
| Daily laborers | 73 | 10.9 |
| Others | 133 | 20.2 |
| Husband’s education (n=658) | ||
| No formal education | 152 | 22.8 |
| Primary education | 216 | 32.3 |
| Secondary education | 150 | 22.5 |
| Tertiary education | 140 | 20.9 |
| Family size | ||
| 1–5 | 512 | 76.6 |
| >5 | 156 | 23.4 |
| Average monthly income (ETB) | ||
| 1st quartile (150–2000) | 207 | 31.0 |
| 2nd quartile (2001–4000) | 163 | 24.4 |
| 3rd quartile (4001–6000) | 158 | 23.7 |
| 4th quartile (6001–15,000) | 140 | 21.0 |
Abbreviation: ETB, Ethiopian Birr (1 USD was equivalent to 32 birr at time of study).
Dietary Practice and Household Food Security
Nearly a quarter (23.7%) of participants craved certain food items in the current pregnancy and 149 (22.3%) had avoided some food items. The reason for avoidance of foods was aversion or personal dislike (46.2%), food taboo (13.2%) and other medical reasons (28.3%). Regarding meals eaten, 188 (28.1%) of the women skipped at least one meal from the regular three meals each day while 480 (71.9%) had at least three meals per day. Out of those skipping meals, 117 (62.2%) women skip meal because of discomfort secondary to pregnancy and disease, 25 (13.3%) women skip due to religious fasting, 19 (10.1%) women skip due to food shortage and the rest, 27 (14.3%) women skip because of the other reasons.
According to the household food insecurity access scale score 398 (59.6%) of the households were food secure whereas 134 (20.1%) were mildly, 121 (18.1%) were moderately and 15 (2.2%) severely food insecure. Small proportions, 18 (2.7%), had received food aid from the safety net program during pregnancy.
Nutrition-Related Knowledge of Pregnant Women
On the assessment of nutrition-specific knowledge, 418 (62.6%) of women had nutritional information from at least one source including health professionals (48.1%), mass media (9.7%), friends (14%) and other sources (18%). The mean knowledge score was 9.14 (± 5.32), the range being 0 to 20. Regarding the specific question, 191 (28.6%) gave a complete answer, 307 (46.0%) gave an incomplete answer and 133 (19.9%) gave a wrong answer for appropriate nutritional practice during pregnancy. The frequency of participants who answered each question is depicted in Table 2.
Table 2.
Nutritional Knowledge Assessment on Pregnant Women Attending Antenatal Clinics in Gurage Zone, Southern Ethiopia, 2021
| Knowledge Variable | Frequency (n) | Percent (%) |
|---|---|---|
| Components of balanced diet | ||
| Wrong | 209 | 31.3 |
| Incomplete | 155 | 23.2 |
| Complete | 304 | 45.5 |
| Advantage of balanced diet | ||
| Wrong | 133 | 19.9 |
| Incomplete | 307 | 46.0 |
| Complete | 228 | 34.1 |
| Appropriate nutritional practice during pregnancy | ||
| Wrong | 145 | 21.7 |
| Incomplete | 332 | 49.7 |
| Complete | 191 | 28.6 |
| Source of protein | ||
| Wrong | 227 | 34.0 |
| Incomplete | 269 | 40.3 |
| Complete | 172 | 25.7 |
| Source of vitamins | ||
| Wrong | 261 | 39.1 |
| Incomplete | 271 | 40.6 |
| Complete | 136 | 20.4 |
| Source of calcium | ||
| Wrong | 385 | 57.6 |
| Incomplete | 205 | 30.7 |
| Complete | 78 | 11.7 |
| Source of iron | ||
| Wrong | 332 | 49.7 |
| Incomplete | 228 | 34.1 |
| Complete | 108 | 16.2 |
| Advantage of iron nutrient | ||
| Wrong | 222 | 33.2 |
| Incomplete | 271 | 40.6 |
| Complete | 175 | 26.2 |
| Effect of under nutrition on women | ||
| Wrong | 189 | 28.3 |
| Incomplete | 304 | 45.5 |
| Complete | 175 | 26.2 |
| Effect of maternal under nutrition on the fetus | ||
| Wrong | 235 | 35.2 |
| Incomplete | 299 | 44.8 |
| Complete | 134 | 20.1 |
Dietary Diversity Among Pregnant Women
Among the participants, 75.0% (95% CI: 71.6, 78.4) of women had suboptimal dietary diversity during 16 to 20 weeks of gestation. At the gestational age of 28 to 29 weeks, 78.7% (95% CI: 75.3, 81.7) of women had suboptimal dietary diversity and at 36 to 37 weeks of gestation, 76.5% (95% CI: 73.1, 79.6) of women had suboptimal dietary diversity. In the average score of aggregated dietary diversity, 84.4% (95% CI: 81.6, 87.3) of women had suboptimal dietary diversity. The average individual dietary diversity has no significant change across pregnancy; the mean dietary diversity score (±SD) was 3.39 ± 1.28 during 16 to 20 weeks, 3.45 ±1.25 during 28 to 29 weeks and 3.56 ±1.25 during 36 to 37 weeks of gestation. The aggregate mean dietary diversity score (±SD) was 3.46 (±0.9) with a range from 1 to 6.
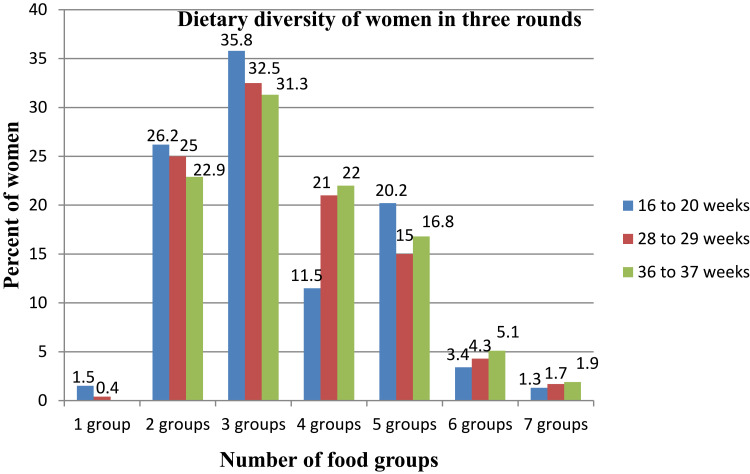
The majority of participants, 424 (63.5%) women consumed three or fewer groups of food items and only 32 (4.7%) women consumed greater than 6 food groups during the first round, 16 to 20 weeks. The details of food groups consumed in different rounds of data collection are depicted in Figure 1.
Figure 1.
The percentage of pregnant women consuming food items from different food groups in the three different time periods of gestational age in the Gurage zone, Southern Ethiopia, 2021. The length of bar indicates percentage of pregnant women consumed from different number of food groups in proceeding 24 hours and the color of bars indicate different rounds. The majority of women consumed only 3 groups of food out of ten category in all rounds; gestational age of 16 to 20 weeks, 28 to 29 weeks and 36 to 37 weeks. No women consumed above 7 out of ten groups in any round.
Regarding the consumption pattern of specific food groups, grains and pulses are the most consumed food items followed by other vegetables such as tomato and fresh/green legumes in all rounds while the dark green leafy vegetables, such as cabbage, were the least consumed items at the first round, 16 to 20 weeks. The consumption of different food groups in different period of data collection are described in Table 3.
Table 3.
Consumption of Different Food Groups in Different Weeks of Gestation Among Pregnant Women Attending Antenatal Clinics in Gurage Zone, Southern Ethiopia, 2021
| Food Groups Consumed | Frequency of Women Consumed from Each Group | ||
|---|---|---|---|
| 16–20 Weeks n (%) |
28 to 29 Weeks n (%) |
36 to 37 Weeks n (%) |
|
| Grains, white roots and tubers | 665 (99.6%) | 668 (100.0%) | 668 (100.0%) |
| Pulses (beans, peas and lentils) | 522 (78.1%) | 552 (82.6) | 556 (83.2%) |
| Nuts and seeds | 174 (26.0%) | 207 (31.0%) | 214 (32.0%) |
| Meat, poultry and fish | 91 (13.6%) | 80 (12.0%) | 98 (14.7%) |
| Eggs | 101 (15.1%) | 75 (11.2%) | 75 (11.2%) |
| Dairy products | 110 (16.5%) | 104 (15.6%) | 143 (21.4%) |
| Dark green leafy vegetables | 39 (5.8%) | 103 (15.4%) | 118 (17.7%) |
| Vitamin-A rich vegetables | 90 (13.5%) | 146 (21.9%) | 141 (21.1%) |
| Other vegetables | 380 (56.9%) | 249 (37.3%) | 245 (36.7%) |
| Other fruits | 95 (14.2%) | 142 (21.3%) | 131 (19.6%) |
Factors Associated with Dietary Diversity
The bi-variable logistic regression analysis was done for age, residence, ethnicity, religion, level of education, occupation, husband’s level of education, husband’s occupation, marital status, family size, parity, craving for certain food item, avoidance of certain food items, skipping of meals, household food insecurity, average monthly income and nutritional knowledge. The variables eligible for the multivariable logistic regression model are described in Table 4.
Table 4.
Bi-Variable and Multi-Variable Logistic Regression of Factors Associated with Dietary Diversity Among Pregnant Women Attending Antenatal Clinics in the Gurage Zone, Southern Ethiopia, 2021
| Variables | Dietary Diversity | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Optimal | Sub-Optimal | |||
| Residence | ||||
| Urban | 81 | 321 | 1 | 1 |
| Rural | 23 | 243 | 2.66 (1.63, 4.36) | 1.91 (1.01, 3.62)a |
| Level of education | ||||
| No formal education | 11 | 177 | 7.43 (3.52, 15.67) | 5.51 (1.96, 15.53)a |
| Primary school | 27 | 203 | 3.47 (1.92, 6.26) | 2.48 (0.98, 6.22) |
| Secondary school | 36 | 119 | 1.53 (0.86, 2.70) | 1.51 (0.67, 3.38) |
| College and above | 30 | 65 | 1 | 1 |
| Occupation | ||||
| Housewife | 50 | 344 | 1 | 1 |
| Merchant | 17 | 64 | 1.91 (0.89, 4.09) | 0.56 (0.27, 1.17) |
| Government employed | 15 | 57 | 1.04 (0.43, 2.52) | 1.51 (0.82, 5.84) |
| Farmer | 12 | 63 | 1.05 (0.43, 2.60) | 1.13 (0.48, 2.64) |
| Others | 10 | 36 | 1.45 (0.57, 3.71) | 1.49 (0.56, 3.96) |
| Husbands occupation (n= 658) | ||||
| Farmer | 21 | 171 | 1 | 1 |
| Merchant | 27 | 111 | 0.50 (0.27, 0.93) | 1.50 (0.61, 3.66) |
| Government employed | 32 | 90 | 0.34 (0.18, 0.62) | 2.40 (0.76, 7.60) |
| Daily labourers | 10 | 63 | 0.76 (0.34, 1.70) | 0.69 (0.26, 1.88) |
| Others | 14 | 115 | 1.07 (0.53, 2.20) | 3.51 (1.32, 9.32) |
| Husbands education (n=658) | ||||
| No formal education | 12 | 140 | 4.23 (2.18, 8.17) | 4.31 (1.51, 12.33)a |
| Primary school | 22 | 182 | 3.52 (1.98, 6.24) | 4.78 (1.83, 12.51)a |
| Secondary school | 27 | 135 | 2.07 (1.19, 3.59) | 2.32 (1.03, 5.22)a |
| College and above | 41 | 99 | 1 | 1 |
| Craving for food | ||||
| Yes | 30 | 128 | 0.72 (0.45, 1.15) | 0.58 (0.33, 1.01) |
| No | 74 | 436 | 1 | 1 |
| Avoidance of certain food | ||||
| Yes | 13 | 136 | 2.22 (1.21, 4.10) | 3.05 (1.49, 6.25)a |
| No | 91 | 428 | 1 | 1 |
| Meal skip | ||||
| Yes | 9 | 179 | 4.91 (2.42, 9.94) | 5.18 (2.41, 11.13)a |
| No | 95 | 385 | 1 | 1 |
| Household food security | ||||
| Food secure | 75 | 323 | 1 | 1 |
| Mild food insecure | 20 | 111 | 1.29 (0.75, 2.21) | 1.22 (0.65, 2.30) |
| Moderate and severe food insecure | 9 | 130 | 3.35 (1.63, 6.89) | 2.44 (1.07, 5.59)a |
| Average Monthly income | ||||
| 1st quartile | 23 | 184 | 2.56 (1.44, 4.58) | 1.94 (1.40, 3.62)a |
| 2nd quartile | 23 | 140 | 1.95 (1.08, 3.51) | 1.45 (0.98, 2.01) |
| 3rd quartile | 24 | 134 | 1.79 (1.00, 3.20) | 1.22 (0.61, 2.44) |
| 4rth quartile | 34 | 106 | 1 | 1 |
| Nutritional education | ||||
| Yes | 71 | 321 | 0.51 (0.28, 0.82) | 0.61 (0.39, 0.95)a |
| No | 33 | 243 | 1 | 1 |
| Knowledge score | 0.89 (0.86, 0.94) | 0.92 (0.87, 0.98)a | ||
Note: Superscript “a” in the last column indicates significant association.
Abbreviations: COR, crude odds ratio; AOR, adjusted odds ratio.
Participants from the rural areas were 1.91 times more likely to have sub-optimal dietary diversity in comparison to those from urban areas (AOR: 1.91, 95% CI: 1.01, 3.62). Women who had no formal education were more likely to have sub-optimal dietary diversity compared to those who attended college or higher (AOR: 5.51, 95% CI: 1.96, 15.53). However, women who attended primary and secondary school had no statistically significant association with suboptimal dietary diversity.
Participants with a history of having fewer than three meals daily had five times higher odds of sub-optimal dietary diversity (AOR: 5.18, 95% CI: 2.41, 11.13) compared to those taking three meals and more. Women with avoidance of certain food items during pregnancy had higher odds of suboptimal dietary diversity (AOR: 3.05, 95% CI: 1.49, 6.25). Women from households with moderate and severe food insecurity had higher odds of suboptimal dietary diversity compared to those from families with food security (AOR: 2.44, 95% CI: 1.07, 5.59). Similarly, women who had information related to nutrition during pregnancy were less likely to have suboptimal dietary diversity in comparison to those who did not. As the nutritional knowledge score increased, the odds of having suboptimal dietary diversity declined (Table 4).
Qualitative Findings on Factors Related to Dietary Diversity
Economic Constraints
The interview and focus group discussion explored the factors contributing to suboptimal dietary diversity. Economic constraint is one of the major factors affecting dietary practice which, in turn, had a great impact on dietary diversity during pregnancy. Women with low family income and from households of food insecurity face significant challenges in trying to diversify their food groups as recommended.
The dietary practices of pregnant women vary from one mother to another. The problem in one house is not a problem in the other home. For instance, the main problem for me is the economic constraints. I only eat what I get daily. Even sometimes I skip meal due to lack of money to buy food.
She was feeling bad, disappointed and expecting government to help her.
32-year-old, 8-month pregnant woman, rural residence with no formal education.
I know that eating different kinds of food during pregnancy is good to the mother and baby. However, in my family, we even worry not to lack food to eat. My husband is a daily laborer, so the food we eat depends on his daily income. I usually prepare the same kind of food which is less expensive in our village.
19-year-old, 9-month pregnant woman, urban residence with primary education.
Food Taboos
Regarding food taboos, different views were forwarded from key informants and participants in the focus group discussions. Health professionals, heads of health centers and woreda health offices reported that food taboos were becoming a thing of the past. Most pregnant women, particularly those from rural regions, still reported the practice of avoiding some food items during pregnancy due to taboos. Foods such as milk, yogurt and banana are believed to get plastered on the head of a baby resulting in meconium staining of amniotic fluid.
Dairy products such as milk, cheese and yogurt are prohibited during pregnancy. It is believed that these foods are plastered on the head of the fetus. It also makes the fetus dirty at delivery which would not be cleaned out easily. I heard in our village that this happened to a woman one year back; she frequently took yogurt in late pregnancy and during delivery, the fetus was dirty and very weak.
34-year-old woman, member of women development army force, rural residence, attended primary school.
Food taboos were becoming old history except in some remote rural areas. In past, food made from cabbage is not allowed to eat during pregnancy because it was believed to cross placenta and plastered in the body of fetus.
42-year-old man, maternal and child nutrition coordinator, urban resident, health professional.
There was also the belief that hot soup prepared from linseed and chicken meat (yedoro shorba) opened the cervix and led to abortions. Honey was also strictly avoided because it was thought to harden the skull of a baby and to make the membranes so strong that the amniotic fluid is trapped in its cavity leading to a difficult delivery.
There is a saying in our community that eating honey during pregnancy hardens the fetal skull and results in the fetus to be weak even die. It was also believed that honey prevents the rupture of fluid during pregnancy so it delays delivery. With this suspicion in my mind, I took honey, then immediately fetal movement was ceased. I was scared and went to the health center to consult a doctor. The doctor examined and told me that the fetus was fine. She gave me advice as it was not due to honey, then I become okay’. She was laughing and saying that these all are wrong thought but affects pregnant women.
26-year-old 8-month pregnant woman, urban residence, attended secondary school.
Gender Roles
The culture that loads women with many responsibilities in the family had a negative influence on the dietary practice of pregnant women. Women prepare and provide food for all family members. Since all members of the household ate from the common pot, a woman worries about how to adequately serve her family before thinking of herself. At times of shortage, they gave priority to their husbands and children. This culture puts men in the first place to food access by undermining the nutritional practice of women.
Our culture disfavors women; all family members are served by her. Even the husband did not care whether the wife was taking enough food or not. Rather, the reverse is true. Due to extreme respect for the husband, priority is given to the husband even with limited food. This affects women living in food-insecure families.
30-year-old men, head of the woreda health office, urban residence, health professional.
Cultural practices in most rural communities did not give care to women. Women are considered as caregivers to their husbands so that they make nutritious food for the husband that she may not eat. Husbands also expect that he should be served first. This practice might not change during pregnancy.
38-year-old, head of health center, urban residence, health professional.
Pregnancy Complications
Medical condition related to pregnancy reduce appetite. Nausea, vomiting and other conditions like gastritis were reported to be contributing factors to poor dietary practice. Women avoid certain kinds of food and skip a meal just because they did not feel fine after taking certain food.
Most of us, pregnant women experience severe nausea and vomiting at early pregnancy period that negatively influences dietary practice. During the first 5 months of this pregnancy, I passed through challenging times, ate nothing except taking fluids and some juice. I was admitted to hospital but now glory to God, it was getting better.
24-year-old 7 months pregnant woman, urban residence, completed secondary school.
Pregnancy is an important period in which we can appropriately intervene nutritional problems. However, most pregnant women face the challenge of morning sickness at an early pregnancy. This greatly affects their dietary practice. They avoid some foods they used to like during the pre-pregnancy time.
30-year-old woman, rural residence, health extension worker.
Lack of Nutritional Literacy
Knowledge and awareness of women on nutrition affects dietary diversity during pregnancy. It was reported that health education and counseling at the ANC were not enough to raise awareness among women about dietary diversity. It was known that most women in the study area were late to book for antenatal care and so they did not get the full services that ANC could provide. The health education given at conferences and home-to-home visits was reported as too weak to address the problem because it did not involve spouses or partners. Weak health services and a low level of knowledge and awareness among caregivers or partners thus had a major effect on the dietary practices of the women.
Pregnant women need someone who closely supports them; we [health extension workers] have seen this practically in the village. For the pregnant women living with partners having good awareness, there was good dietary practice. Therefore, all the family members should be aware of pregnant women’s dietary practices particularly partners or other caregivers. I understood that health education given only to women may not remove the problem from the deep root, so we should incorporate partners in the education. The health education given at health facilities and community needs modification of strategy.
24-year-old woman, health extension worker in the rural community.
I ate what we prepare at home for all family members. I have no awareness of the dietary practice of pregnant women. With God’s grace, I lack nothing to eat what I want but I do not know which food items are recommended during pregnancy.
30-year-old 7-month pregnant woman, rural residence, no formal education
Discussion
This study sought to assess the prevalence of dietary diversity and its associated factors during second and third trimester among pregnant women attending ANC clinic in Gurage zone, southern Ethiopia. It revealed that nearly one in four pregnant women in Gurage Zone attained the minimum optimal dietary diversity in each of three rounds. The average sub-optimal dietary diversity across the pregnancy was 84.4%. The main factors associated with sub-optimal dietary diversity among the women were dwelling in rural areas, lack of formal education, husband’s lower educational attainment, household food insecurity, avoidance of certain food items due to food taboos and pregnancy complications, poor nutritional knowledge, societal expectation of gender role, lack of awareness of a pregnant woman’s nutritional needs among their spouses and others who should be concerned with their welfare. Some of these factors were closely related to household income and the strategies employed by health workers to convey health and nutritional information to the population.
The high prevalence of sub-optimal dietary diversity among pregnant women in Gurage was in remarkable agreement with another study conducted in Shashemane town where only 25.4% of pregnant women achieved minimum dietary diversity.12 However, reports from other parts of Ethiopia had found lower levels of sub-optimal dietary diversity, notably the 53% from East Gojjam Zone,14 55.2% from Bale Zone13 and 57% from Dire Dawa.31 The observed gap in prevalence could be due to differences in socio-demographic characteristics, geographic differences or the season in which the study was conducted. The difference in the dietary diversity scoring tools used could also have contributed to the observed differences.
Women from the rural areas were nearly two times more likely to have suboptimal dietary diversity during pregnancy compared to urban dwellers. This is consistent with earlier reports from Bale Zone, Ethiopia and from Ghana,13,32 but studies from other parts of Ethiopia did not show such an association between place of abode and dietary diversity.14,15 The differences seen between urban and rural women in this study may be related to household income and educational attainment rather than the geographical location of the residence. Women in the urban areas had higher income, were more educated and had easier access to the markets where farm products are brought for sale, which enhances the opportunity for them to get items from the different food groups needed to achieve optimal dietary diversity.
Women with no formal education in the study population were less likely to achieve minimum optimal dietary diversity compared to their formally educated counterparts, a finding that is in accordance with what had been reported from different regions of Ethiopia,15,33–35 Kenya,36 Tanzania37 and Ghana.32 The possible explanation for this, apart from the higher incomes associated with better education, could be that formal education makes women more knowledgeable about food groups and nutrient-preserving methods of food preparation. Women with higher education may also be more likely to understand the nutrition-related health education provided in health facilities and put such knowledge to use. The study also revealed that women with husbands who attended tertiary education were more likely to achieve optimal dietary diversity compared to those with less educated husbands. This could be due to increased awareness and support of educated husbands in ensuring the dietary diversity of pregnant women. The studies from Bangladesh,38 Ghana18 and Tigray Region in Ethiopia15 had supported this finding.
The nutritional information given to pregnant women at ANC visits, conferences and using different media was also found to be associated with dietary diversity. Women having nutrition-related education were less likely to have sub-optimal dietary diversity in comparison to those who did not get information. Similar findings had been reported from Malawi,39 Ghana,40 and from the Southwest and Northwest regions of Ethiopia.41,42 Improvement in nutritional knowledge improves dietary practice, which favors dietary diversity. One cautionary note that emerged from the focus group discussions and in-depth interviews is the necessity for improving the effectiveness of these nutrition educational activities by involving the spouses and partners of the pregnant women in the health education targeted at the women.
The dietary practice of women during pregnancy greatly influences dietary diversity. Findings from this study showed that women who had avoidance to certain food items due to food taboos were twice as likely to have suboptimal dietary diversity than women with no such avoidance, a situation that had also been reported from other parts of Africa.18 Further exploration revealed that aversion to these food items, particularly eggs and dairy products were rooted in strongly held beliefs that had a long history in the community. Such beliefs include maternal ingestion of honey making the baby big, with attendant difficulties in labor and delivery; consuming milk, cheese, yogurt, porridge and banana leading to a heavy coating of the baby’s skin with dirt, and eating hot soup from chicken and linseed resulting in abortion. The reports from other studies support this result.43–46
Women skipping meals or not being able to eat a minimum of three meals per day contributed to sub-optimal dietary diversity and this was largely related to pregnancy complications such as nausea and vomiting. In-depth interviews and focus group exploration showed pregnant women skip meal because of nausea and vomiting that had decreased their appetite and caused discomfort after eating. This is a situation that had also been reported from Illu Aba Bor Zone, Ethiopia,41 East Gojjam Zone, Ethiopia14 and Indonesia.47 As the frequency of meals increases, the chance of increasing dietary diversity also seems to rise.
Household income is a major determinant of what can be expended on food and, consequently, of household food security. The women from households with greater monthly incomes had lower odds of having sub-optimal dietary diversity in comparison to women with lesser monthly income, a finding that corroborates what had been previously reported.19,48,49 Household food insecurity had a strong association with women’s dietary diversity in this study. The participants were categorized into food secure, mild, moderate and severe food-insecure households but the last two categories were merged for the analysis due to few numbers of subjects under them. It was shown that women from moderate and severe food-insecure families had higher odds of having sub-optimal dietary diversity in comparison to those from food-secure families. A previous study conducted in Illu Aba Bor Zone revealed similar findings.41 Other studies50,51 also reported findings consistent with this. Economic deprivation certainly limits the options available for dietary diversity and the views expressed at the FGDs buttressed this.
Participants were included in this study in their early second trimester, specifically 16 to 20 weeks of gestational age and followed up to the end of pregnancy. The dietary diversity scoring was done in three different contacts to overcome the limitation of single dietary diversity scoring. On the other hand, adopting a mixed-method approach allowed a deeper exploration of some of the factors that contributed to the characteristics found to be associated with poor dietary diversity in the populations, making this study more robust. One limitation of the study was measuring dietary diversity using FOA guideline (MDD-W) that assessed only the preceding 24-hour consumption, which may not be the usual consumption. Limitations of recall and social desirability bias may also have affected the findings.
Conclusions
Nearly three in four pregnant women in the Gurage Zone of Ethiopia had sub-optimal dietary diversity, especially residents of rural areas, those with no formal education and those from lower monthly income and food insecure households. Providing nutritional education and a higher nutritional knowledge score were associated with a lower prevalence of sub-optimal dietary diversity. The dietary practice of women during pregnancy such as skipping meals and engaging in avoidance of certain food items due to food taboos were associated with sub-optimal dietary diversity. Policies, strategies and interventions aimed at promoting maternal and fetal nutrition should focus on promoting women’s education and tackling the problem of household food insecurity. In addition, efforts should be made to strengthen nutritional health education in health facilities, with the inclusion of the women’s spouses or partners in such activities.
Acknowledgments
The authors would like to thank Pan African University, life and earth science institute (including Health and Agriculture) for sponsoring this research project. Our heartfelt gratitude goes to all participants of the study, data collectors and heads of Gurage zone and district health office for cooperation during data collection.
Funding Statement
This study is part of PhD thesis funded by Pan African University (PAU), life and earth science institute (Including Health and Agriculture), a continental initiative of the African Union Commission (AU), Addis Ababa, Ethiopia. The funding university had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Considerations
Ethical approval was obtained from the institutional review board of Wolkite University, Ethiopia (RCSUILC/059/2013) and the joint Ethics Review Committee of the University of Ibadan and the University College Hospital, Ibadan, Nigeria (UI/EC/20/0463). A brief explanation of all research activities, aim, benefit, and risk has been given to the participants. The respondents were informed about voluntary participation and their full legitimate rights to withdraw at any time. Confidentiality of data was kept during each stage of data handling. The written informed consent that includes publication of anonymised response for qualitative part of study was taken from the study participants. The study conforms to the provision of the declaration of Helsinki.52
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
- 1.Tuncalp Ӧ, Pena-Rosas JP, Lawrie T, et al. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG. 2017;124(6):860–862. doi: 10.1111/1471-0528.14599 [DOI] [PubMed] [Google Scholar]
- 2.FAO. Minimum Dietary Diversity for Women: A Guide for Measurement. Rome: FAO; 2016:82. [Google Scholar]
- 3.Ruel MT. Operationalizing dietary diversity: a review of measurement issues and research priorities. J Nutr. 2003;133(11):3911S–26S. doi: 10.1093/jn/133.11.3911S [DOI] [PubMed] [Google Scholar]
- 4.Nguyen PH, Huybregts L, Sanghvi TG, et al. Dietary diversity predicts the adequacy of micronutrient intake in pregnant adolescent girls and women in Bangladesh, but use of the 5-group cutoff poorly identifies individuals with inadequate intake. J Nutr. 2018;148(5):790–797. doi: 10.1093/jn/nxy045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gómez G, Nogueira Previdelli Á, Fisberg RM, et al. Dietary diversity and micronutrients adequacy in women of childbearing age: results from elans study. Nutrients. 2020;12(7):1994. doi: 10.3390/nu12071994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rammohan A, Srinivas G, Deepti S, Dibyasree G, Uma S. Maternal dietary diversity and odds of low birth weight: empirical findings from India. Women Health. 2019;59(4):375–390. doi: 10.1080/03630242.2018.1487903 [DOI] [PubMed] [Google Scholar]
- 7.Cano-Ibáñez N, Martínez-Galiano JM, Amezcua-Prieto C, Olmedo-Requena R, Bueno-Cavanillas A, Delgado-Rodríguez M. Maternal dietary diversity and risk of small for gestational age newborn: findings from a case–control study. Clin Nutr. 2020;39(6):1943–1950. doi: 10.1016/j.clnu.2019.08.019 [DOI] [PubMed] [Google Scholar]
- 8.Samuel S, Darebo T, Desta DT. Socio-economic and dietary diversity characteristics are associated with anemia among pregnant women attending antenatal care services in public health centers of Kembata Tembaro zone. Southern Ethiopia. 2020;8(4):1978–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee S, Talegawkar SA, Merialdi M, Caulfield LE. Dietary intakes of women during pregnancy in low-and middle-income countries. Public Health Nutr. 2013;16(8):1340–1353. doi: 10.1017/S1368980012004417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christian P. Micronutrients, birth weight, and survival. Annu Rev Nutr. 2010;30:83–104. doi: 10.1146/annurev.nutr.012809.104813 [DOI] [PubMed] [Google Scholar]
- 11.Gernand AD, Schulze KJ, Stewart CP, West KP, Christian P. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat Rev Endocrinol. 2016;12(5):274–289. doi: 10.1038/nrendo.2016.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desta M, Akibu M, Tadese M, Tesfaye M. Dietary diversity and associated factors among pregnant women attending antenatal clinic in Shashemane, Oromia, Central Ethiopia: a cross-sectional study. J Nutr Metab. 2019;2019:1–7. doi: 10.1155/2019/3916864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hailu S, Woldemichael B. Dietary diversity and associated factors among pregnant women attending antenatal care at public health facilities in Bale Zone, Southeast Ethiopia. Nutr Diet Suppl. 2019;11:1–8. doi: 10.2147/NDS.S179265 [DOI] [Google Scholar]
- 14.Yeneabat T, Adugna H, Asmamaw T, et al. Maternal dietary diversity and micronutrient adequacy during pregnancy and related factors in East Gojjam zone, Northwest Ethiopia, 2016. BMC Pregnancy Childbirth. 2019;19(1):1–9. doi: 10.1186/s12884-019-2299-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jemal K, Awol M. Minimum dietary diversity score and associated factors among pregnant women at alamata general hospital, Raya Azebo Zone, Tigray Region, Ethiopia. Public Health Nutr. 2019;2019:8314359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aliwo S, Fentie M, Awoke T, Gizaw Z. Dietary diversity practice and associated factors among pregnant women in North East Ethiopia. BMC Res Notes. 2019;12(1):123. doi: 10.1186/s13104-019-4159-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hidru HD, Berwo Mengesha M, Hailesilassie Y, Tekulu Welay F. Burden and determinant of inadequate dietary diversity among pregnant women in Ethiopia: a systematic review and meta-analysis. J Nutr Metab. 2020;2020:1–10. doi: 10.1155/2020/1272393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gyimah LA, Annan RA, Apprey C, et al. Dietary diversity and its correlates among pregnant adolescent girls in Ghana. PLoS One. 2021;16(3):e0247979. doi: 10.1371/journal.pone.0247979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shrestha V, Paudel R, Sunuwar DR, Lyman ALT, Manohar S, Amatya A. Factors associated with dietary diversity among pregnant women in the western hill region of Nepal: a community based cross-sectional study. PLoS One. 2021;16(4):e0247085. doi: 10.1371/journal.pone.0247085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zerfu T, Umeta M, Baye K. Dietary diversity during pregnancy is associated with reduced risk of maternal anemia, preterm delivery, and low birth weight in a prospective cohort study in rural Ethiopia. Am J Clin Nutr. 2016;103(6):1482–1488. doi: 10.3945/ajcn.115.116798 [DOI] [PubMed] [Google Scholar]
- 21.Kibret KT, Chojenta C, Gresham E, Tegegne TK, Loxton D. Maternal dietary patterns and risk of adverse pregnancy (hypertensive disorders of pregnancy and gestational diabetes mellitus) and birth (preterm birth and low birth weight) outcomes: a systematic review and meta-analysis. Public Health Nutr. 2019;22(3):506–520. doi: 10.1017/S1368980018002616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Augustin H, Winkvist A, Bärebring L. Poor dietary quality is associated with low adherence to gestational weight gain recommendations among women in Sweden. Nutrients. 2020;12(2):317. doi: 10.3390/nu12020317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sinaga M, Mohammed A, Teklu N, Stelljes K, Belachew T. Effectiveness of the population health and environment approach in improving family planning outcomes in the Gurage, zone South Ethiopia. BMC Public Health. 2015;15(1):1123. doi: 10.1186/s12889-015-2484-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dendir Z, Simane B. Livelihood vulnerability to climate variability and change in different agroecological zones of Gurage Administrative zone, Ethiopia. Prog Disaster Sci. 2019;3:100035. doi: 10.1016/j.pdisas.2019.100035 [DOI] [Google Scholar]
- 25.Yitbarek K, Abraham G, Morankar S. Contribution of women’s development army to maternal and child health in Ethiopia: a systematic review of evidence. BMJ open. 2019;9(5):e025937. doi: 10.1136/bmjopen-2018-025937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jessica A, Reginald A, Herman L, Anthony E, Su PL. Prevalence of anaemia and low intake of dietary nutrients in pregnant women living in rural and urban areas in the Ashanti region of Ghana. PLoS One. 2020;15(1):e0226026. doi: 10.1371/journal.pone.0226026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Loha E, Workicho A. Burden and determinants of undernutrition among young pregnant women in Ethiopia. PLoS One. 2019;15(3):e12751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide: version 3. 2007.
- 29.ICF CSACEa. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF. 2016. [Google Scholar]
- 30.Adubra L, Savy M, Fortin S, et al. The Minimum Dietary Diversity for Women of Reproductive Age (MDD-W) indicator is related to household food insecurity and farm production diversity: evidence from Rural Mali. Curr Develop Nutr. 2019;3(3). doi: 10.1093/cdn/nzz002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shenka A, Damena M, Abdo M, Roba KT. Dietary diversity and nutritional status of pregnant women attending public hospitals in Dire Dawa City Administration, Eastern Ethiopia. East African J Health Biomedl Sci. 2018;2(1):10–17. [Google Scholar]
- 32.Amugsi DA, Lartey A, Kimani-Murage E, Mberu BU. Women’s participation in household decision-making and higher dietary diversity: findings from nationally representative data from Ghana. J Health Popul Nutr. 2016;35(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kiboi W, Kimiywe J, Chege P. Dietary diversity, nutrient intake and nutritional status among pregnant women in Laikipia County, Kenya. Int j Health Sci. 2016;2016:378–379. [Google Scholar]
- 34.Aliwo S, Fentie M, Awoke T, Gizaw Z. Dietary diversity practice and associated factors among pregnant women in North East Ethiopia. BMC Res Notes. 2019;12(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Delil R, Zinab B, Mosa H, Ahmed R, Hassen H. Determinants of dietary diversity practice among pregnant women attending antenatal clinic at Wachemo University Nigist Eleni Mohammed memorial referral hospital, Southern Ethiopia. PLoS One. 2021;16(4):e0250037. doi: 10.1371/journal.pone.0250037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kiboi W, Kimiywe J, Chege P. Determinants of dietary diversity among pregnant women in Laikipia County, Kenya: a cross-sectional study. BMC Nutr. 2017;3(1):1–8. doi: 10.1186/s40795-017-0126-6 [DOI] [Google Scholar]
- 37.Ochieng J, Afari-Sefa V, Lukumay PJ, Dubois T. Data: dietary diversity and the potential role of men in improving household nutrition in Tanzania. 2016. [DOI] [PMC free article] [PubMed]
- 38.Kundu S, Jharna DE, Banna MHA, Khan MSI. Factors associated with dietary diversity and physical activity of pregnant women in Bangladesh: a cross‐sectional study at an antenatal care setting. Lifestyle Med. 2021;2:e41. [Google Scholar]
- 39.Katenga-Kaunda LZ, Kamudoni PR, Holmboe-Ottesen G, et al. Enhancing nutrition knowledge and dietary diversity among rural pregnant women in Malawi: a randomized controlled trial. BMC Pregnancy Childbirth. 2021;21(1):1–11. doi: 10.1186/s12884-021-04117-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Agyei EA, Afrifa SK, Munkaila A, Gaa PK, Kuugbee ED, Mogre V. Income level but not nutrition knowledge is associated with dietary diversity of rural pregnant women from Northern Ghana. J Nutr Metab. 2021;2021:1–7. doi: 10.1155/2021/5581445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tsegaye D, Tamiru D, Belachew T. Factors associated with dietary practice and nutritional status of pregnant women in rural communities of Illu Aba Bor zone, Southwest Ethiopia. Nutr Diet Suppl. 2020;12:103–112. doi: 10.2147/NDS.S257610 [DOI] [Google Scholar]
- 42.Alemayehu MS, Tesema EM. Dietary practice and associated factors among pregnant women in Gondar town north west, Ethiopia, 2014. Int J Nutr Food Sci. 2015;4(6):707–712. doi: 10.11648/j.ijnfs.20150406.27 [DOI] [Google Scholar]
- 43.Ekwochi U, Osuorah CDI, Ndu IK, Ifediora C, Asinobi IN, Eke CB. Food taboos and myths in South Eastern Nigeria: the belief and practice of mothers in the region. J Ethnobiol Ethnomed. 2016;12:7. doi: 10.1186/s13002-016-0079-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walters C, Bendulo P, Stoecker B. Assessment of dietary diversity, antenatal care, food taboos, meal frequency, and nutritional status of pregnant adolescents in rural Malawi: a cross-sectional study. African J Food Agric Nutr Dev. 2019;19(3):14555–14570. doi: 10.18697/ajfand.86.17530 [DOI] [Google Scholar]
- 45.Tela FG, Gebremariam LW, Beyene SA. Food taboos and related misperceptions during pregnancy in Mekelle city, Tigray, Northern Ethiopia. PLoS One. 2020;15(10):e0239451. doi: 10.1371/journal.pone.0239451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zepro NB. Food taboos and misconceptions among pregnant women of Shashemene District, Ethiopia, 2012. Sci J Public Health. 2015;3(3):410–416. doi: 10.11648/j.sjph.20150303.27 [DOI] [Google Scholar]
- 47.Diana R, Christianti DF, Anwar F, Kusuma R, Rachmayantis RD, Khomsan A. Food suggestions, meal frequency and dietary diversity among pregnant women: a quantitative study. Future Food. 2020;8(3).doi: 10.17170/kobra-202007201470 [DOI] [Google Scholar]
- 48.Kobiro DH, Delil R, Tamiru D, Zinab B. Determinants of dietary diversity among pregnant women attending public health facilities in Hossana town, South Ethiopia. 2019. [DOI] [PMC free article] [PubMed]
- 49.Olatona FA, Olowu OJ, Goodman OO, Amu EO. Dietary habits, diversity, and predictors among pregnant women attending primary health care centers for antenatal care in Lagos, Nigeria. Fam Med Prim Care Rev. 2021;10(8):3076. doi: 10.4103/jfmpc.jfmpc_397_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lama N, Lamichhne R, Bhandari R, et al. Factors influencing dietary diversity of pregnant women attending antenatal care in western regional hospital, Nepal: a cross-sectional study. J Karnali Acad Health Sci. 2019;2(3):189–196. doi: 10.3126/jkahs.v2i3.26653 [DOI] [Google Scholar]
- 51.Na M, Mehra S, Christian P, et al. Maternal dietary diversity decreases with household food insecurity in rural Bangladesh: a longitudinal analysis. J Nutr. 2016;146(10):2109–2116. doi: 10.3945/jn.116.234229 [DOI] [PubMed] [Google Scholar]
- 52.World Medical Association. Ethical principles for medical research involving human subjects. Jahrbuch Für Wissenschaft Und Ethik. 2009;14(1):233–238. doi: 10.1515/9783110208856.233 [DOI] [Google Scholar]