Abstract
Background
For the past few years, only a few monovalent EV71 vaccines have been developed, while other enterovirus vaccines are in short supply. We conducted a quantitative meta-analysis to explore the epidemiological characteristics, routine laboratory diagnosis, clinical signs and risk factors for hand, foot and mouth disease (HFMD).
Methods
PubMed, Embase and the Web of Science were searched for eligible reports published before April 16, 2021, with no publication time or language restrictions. The primary outcome was the odds ratio of the epidemiological characteristics, routine laboratory diagnosis, and clinical signs associated with HFMD severity and death.
Results
After screening 10522 records, we included 32 articles comprising 781903 cases of hand, foot and mouth disease. Patients with severe illness developed some clinical signs (hypersomnia (OR = 21.97, 95% CI: 4.13 to 116.74), convulsion (OR = 16.18, 95% CI: 5.30 to 49.39), limb shaking (OR = 47.96, 95% CI: 15.17 to 151.67), and breathlessness (OR = 7.48, 95% CI: 1.90 to 29.40)) and had some changes in laboratory parameters (interleukin-6 levels standardized mean difference (SMD) = 1.57, 95%CI: 0.55 to 2.60), an increased neutrophils ratio (SMD = 0.55, 95%CI: 0.17 to 0.93), cluster of differentiation 4 (CD4+) (SMD = -1.38, 95%CI: -2.33 to -0.43) and a reduced lymphocytes ratio (SMD = -0.48, 95%CI: -0.93 to -0.33)) compared with patients with mild illness. The risk factors for death included cyanosis (OR = 5.82, 95% CI: 2.29 to 14.81), a fast heart rate (OR = 3.22, 95% CI: 1.65 to 6.30), vomiting (OR = 2.70, 95% CI: 1.33 to 5.49) and an increased WBC count (SMD = 0.60, 95% CI: 0.27 to 0.93).
Conclusions
China has the highest incidence of HFMD. Our meta-analyses revealed important risk factors that are associated with the severity and mortality of HFMD.
Introduction
Hand, foot and mouth disease (HFMD) is an infectious disease caused by enteroviruses, mainly enteroviruses 71 (EV71), coxsackievirus-A16 (CoxA16) and others, and usually affects children under five years old [1, 2]. The virus is generally spread via fecal–oral or personal contact with a sick person or their belongings. Oral pain, maculopapular rash, ulcers appearing on the oral mucosa, and emerging blisters on the hands, feet, and buttocks are typical symptoms of HFMD [3–5]. In recent years, HFMD outbreaks have been found in several parts of the world, especially in countries in the Asian-Pacific region such as China, Singapore and Japan [6–9]. The first case of HFMD was found in New Zealand, and it was officially named HFMD in 1956. In 2008, China listed HFMD as a class C infectious disease. Later, in 2010, coxsackievirus-A6 and coxsackievirus-A10 were identified as the common serotypes of HFMD and have remained so until now [10].
There were gender differences in the incidence of HFMD, with girls slightly lower than boys [11]. The prevalence of HFMD also varies with season, weather, countries and other factors [12]. The incidence of HFMD is relatively high in tropical and temperate zones [13]. The majority of HFMD outbreaks are reported in some Asian-Pacific region countries such as China, India, Malaysia [14]. Since 2014, China HFMD diseases accounted for 87%(9.8million/11.3million) of all HFMD cases reported to WHO [15]. By the end of 2015, China had reported more than 13 million cases of HFMD. The incidence of HFMD, foot and mouth disease (HFMD) had obvious seasonal, with a high incidence in May and June in China. Some severe cases of HFMD even show symptoms of pulmonary edema, pulmonary hemorrhage, nervous system diseases and other severe complications. HFMD remains a major challenge to the development of public health in China. In this study, we aimed to quantitatively analyze the epidemiology, routine laboratory diagnosis, clinical signs and risk factors for HFMD.
Methods
The Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement was used to design and report this review.
Literature search
A quantitative meta-analysis was conducted to explore the association between epidemiological characteristics, routine laboratory diagnosis, and clinical signs associated with HFMD severity and death. PubMed, Embase, and the Web of Science were comprehensively searched for eligible records (up to April 16, 2021), with no publication time or language restrictions. The search terms were “HFMD” OR “hand, foot and mouth disease”. Then, we performed a manual search of the reference lists from the eligible articles and identified reviews to complete our search.
Inclusion and exclusion criteria
Two researchers first filtered the retrieved records by accessing the titles and abstracts and then combined them with full-text screening to obtain eligible studies. The research area of this review was all over the world. The inclusion criteria of the literature were as follows: the studies were peer-reviewed for publication; the study time was specified in the study; the subjects were laboratory-confirmed HFMD patients; and the selected articles also met one or both of the following criteria: (1) the studies mentioned the association between the risk factors for and the death from HFMD; and (2) the studies included the clinical signs or routine laboratory diagnosis (including severe and mild disease patient groups) of HFMD.
The exclusion criteria of the studies were as follows: (1) abstract-only articles, letters, editorials, systematic reviews, duplicated publications, and so on; (2) data and information in the article were incomplete, suspicious, or inconsistent; (3) the full text could not be accessed; and (4) overlapping datasets (when facing studies with overlapping data, researchers selected the one with the largest sample size as a priority).
Data extraction and quality evaluation
Two reviewers completed data extraction and article screening, and disagreements were resolved by discussion and consensus. For all final included articles, we extracted the following data: the first author; year of publication; study region; study period; patient sex; median or mean age; clinical information about patients with HFMD (stiff neck, convulsions, hypersomnia, vomiting, limb shaking, hyperarousal, fever, breathlessness); routine laboratory parameters(white blood cell (WBC) count, C-reactive protein (CRP) levels, interleukin-6 (IL-6) levels, interleukin-10(IL-10) levels, lymphocyte ratio, neutrophil ratio, cluster of differentiation 4 (CD4+)); and risk factors. In addition, if the data were not reliable, we imported “NA”.
Moreover, the Study Quality Assessment Tools, which are provided by the National Institute of Health [16], were used to evaluate the quality of the original articles. The evaluation criteria were divided into three levels: poor, fair and good. Based on those criteria, the quality of the studies could be rated.
Statistical analyses
For the studies reporting the mean and standard deviation (SD) for extracted variables, the pooled estimates of the standard mean difference (SMD) and 95% confidence intervals (CIs) were calculated with a random effect model. When SD was not reported, we estimated the standard deviations based on possible CIs or other variance measures. For the studies reporting specific data on each group of cases, the pooled odds ratio (OR) and 95% CIs were calculated to evaluate the association between those factors and HFMD. The robustness of the results was evaluated by sensitivity analysis which omitted one study at a time. The heterogeneity of the included studies was reflected by the I-squared (I2) and chi-square tests. If p<0.05 and I2 >50%, the heterogeneity was confirmed to be significant. If the heterogeneity was significant, a random effect model was used. Otherwise, a fixed effect model was applied. In addition, Begg’s funnel plot Egger’s test and the trim-and-fill method were used to assess publication bias [17]. All of the statistical analyses were performed by R, version 4.04 meta package.
Results
Systematic review
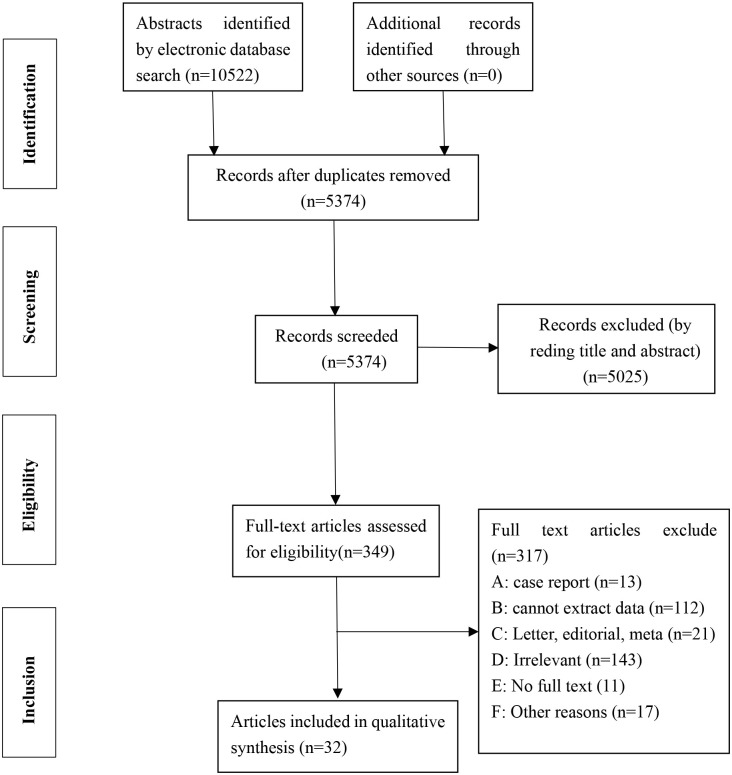
After a preliminary screening of the 10522 identified articles, 5152 articles were removed because they were duplicated. A total of 349 articles were selected to have the full- text reviewed, of which 317 studies were ruled out for the reasons formulated. Finally, we included 32 articles for further data extraction and meta-analysis (Fig 1 and Table 1). Almost all of the included articles reporting cases were from China, with only one article from Singapore. A total of 31 articles reporting cases from China were collected, which included East China (14 articles), Central China (9 articles), West China (5 articles), and Northeast China (1 article), and had steps over multiple regions (2 articles). Geographical or time trends were considered important reasons for publication bias when explaining the evidence for HFMD.
Fig 1. PRISMA flowchart used in the Study selection.
Table 1. The basic characteristics of studies in meta-analysis.
| First author | Publication year | Region | Year of admitted patients | Case number | Male number | Quality rating | ||
|---|---|---|---|---|---|---|---|---|
| Total | Mild | Severe | ||||||
| Chen et al. [18] | 2015 | East, China | 2013–2014 | 263 | 142 | 121 | 137 | Fair |
| Chen et al. [19] | 2013 | East, China | 2012 | 126 | 64 | 62 | 80 | Fair |
| Chong et al. [20] | 2003 | Singapore | 2000–2001 | 138 | NA | NA | 81 | Good |
| Deng et al. [21] | 2016 | West, China | 2014–2015 | 216 | 88 | 128 | 133 | Fair |
| Han et al. [22] | 2016 | East, China | 2013–2015 | 300 | 150 | 150 | 174 | Fair |
| Han et al. [23] | 2014 | China | 2008–2010 | 91 | 32 | 59 | 55 | Good |
| Han et al. [24] | 2011 | East, China | 2009 | 102 | 77 | 25 | 62 | Good |
| He et al. [25] | 2019 | East, China | 2012–2014 | 132 | 57 | 75 | 87 | Fair |
| Huang et al. [26] | 2012 | East, China | 2011 | 56 | 45 | 11 | 36 | Fair |
| Jiang et al. [27] | 2013 | Central, China | 2011 | 89 | 55 | 34 | NA | Fair |
| Jiang et al. [28] | 2012 | East, China | 2010 | 573 | 77 | 496 | 375 | Fair |
| Li et al. [29] | 2014 | Central, China | 2012 | 503 | 423 | 80 | 287 | Good |
| Li et al. [30] | 2014 | East, China | 2012 | 571 | 221 | 350 | 351 | Good |
| Li et al. [31] | 2013 | West, China | 2011 | 318 | 202 | 116 | 211 | Good |
| Liu et al. [32] | 2013 | East, China | 2009–2011 | 164 | NA | 123 | 130 | Good |
| Long et al. [33] | 2016 | Central, China | 2011–2014 | 553 | NA | NA | 335 | Fair |
| Pan et al. [34] | 2012 | Central, China | 2008–2009 | 369 | 140 | 229 | 241 | Good |
| Pan et al. [35] | 2019 | West, China | 2017–2018 | 55 | 17 | 38 | 38 | Fair |
| Qiu et al. [36] | 2019 | Central, China | 2013–2017 | 7203 | NA | NA | 4580 | Good |
| Ren et al. [37] | 2016 | East, China | 2015 | 86 | 19 | 67 | 52 | Good |
| Song et al. [38] | 2014 | Central, China | 2010–2012 | 167 | NA | NA | 107 | Good |
| Tang et al. [39] | 2011 | East, China | 2008–2009 | 186 | 62 | 124 | 120 | Good |
| Wang et al. [40] | 2014 | Central, China | 2009 | 120 | 60 | 60 | 72 | Fair |
| Wang et al. [41] | 2020 | West, China | 2013–2018 | 459 | NA | NA | 295 | Good |
| Xu et al. [42] | 2011 | Central, China | 2010 | 315 | NA | 210 | 210 | Good |
| Yang et al. [43] | 2020 | East, China | 2017 | 261 | 206 | 55 | 174 | Good |
| Zhang et al. [44] | 2017 | East, China | 2009–2014 | 530 | 345 | 185 | 379 | Good |
| Zhang et al. [45] | 2011 | China | 2008–2009 | 765220 | NA | 4067 | NA | Fair |
| Zhang et al. [46] | 2016 | Central, China | 2014–2015 | 100 | 58 | 42 | 64 | Good |
| Zheng et al. [47] | 2017 | West, China | 2009–2016 | 179 | NA | 52 | 112 | Good |
| Zheng et al. [48] | 2017 | East, China | 2014–2015 | 82 | 30 | 52 | 44 | Good |
| Zhou et al. [49] | 2012 | Northeast, China | 2008–2011 | 2379 | 1798 | 581 | 1385 | Good |
NA: not applicable
Clinical symptoms of HFMD
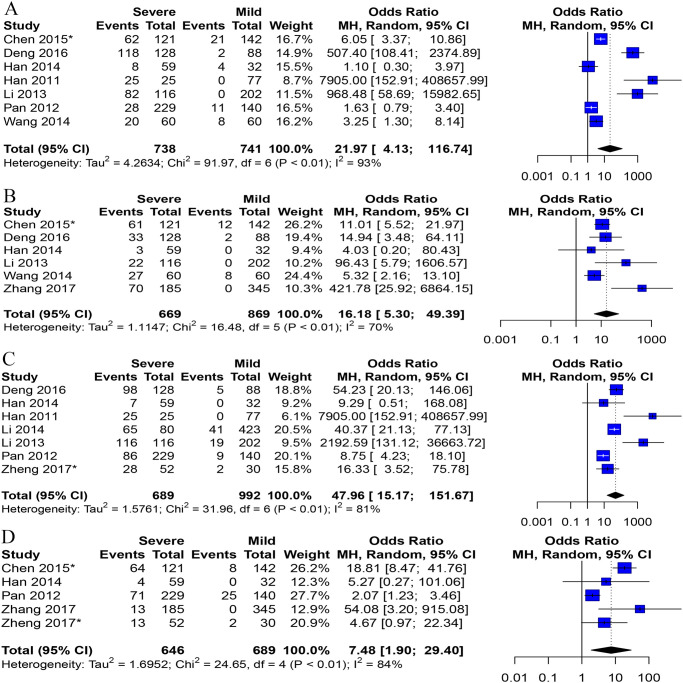
A total of 13 studies involving 3,173 patients assessed the relationship between HFMD and clinical symptoms. We analyzed the association between clinical symptoms and the severity of HFMD, and the results were as follows: hypersomnia (7 studies, 95% CI: 4.13 to 116.74), convulsion (6 studies, 95% CI: 5.30 to 49.39), vomiting (11 studies, 95% CI: 3.49 to 11.44), limb shaking (7 studies, 95% CI: 15.17 to 151.67), fever (8 studies, 95% CI: 2.87 to 12.06), breathlessness (5 studies, 95% CI: 1.90 to 29.40), hyperarousal (3 studies, 95% CI: 4.75 to 285.46), and stiff neck (3 studies, 95% CI: 1.76 to 110.28). For each symptom considered in three or more studies, the odds ratio (OR), 95% confidence interval (95% CI) and p value are shown in Fig 2 and S1 Table. There was significant heterogeneity (P < 0.1) among studies meta-analyzed of the 8 clinical symptoms, which used a random effect model with I-squared values >50%.
Fig 2. Forest plots of meta-analysis on a panel of clinical signs.
A Hypersomnia, B convulsion, C Limb shaking, D Breathlessness. *Data is converted from the original data.
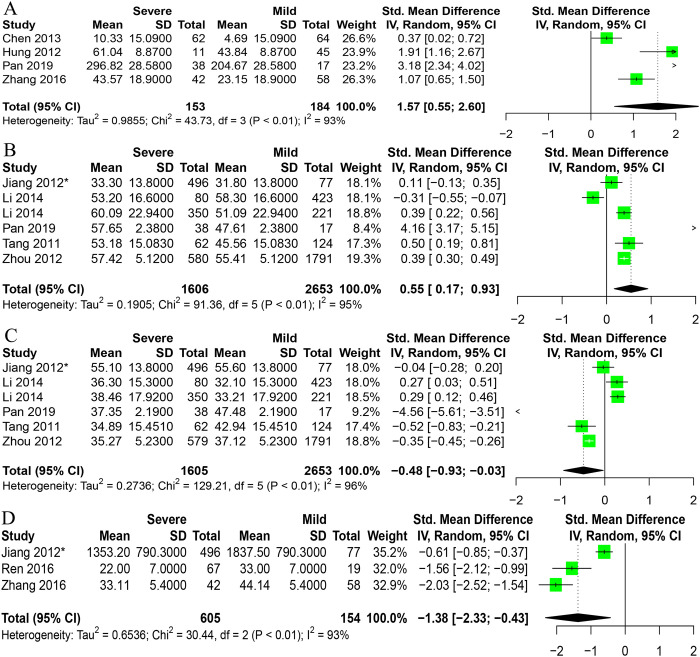
Routine laboratory diagnosis of HFMD
Sixteen studies, including 6048 cases, analyzed the connection between HFMD and routine laboratory diagnosis. We analyzed the routine laboratory diagnosis association between mild and severe HFMD. As shown in Fig 3 and S1 Table, the results of routine laboratory diagnoses for patients with severe HFMD showed IL-6 levels (SMD = 1.57, 95%CI: 0.55 to 2.60), and neutrophils ratio (SMD = 0.55, 95%CI: 0.17 to 0.93) compared with patients with mild HFMD, but the results displayed reduced CD4+ levels (SMD = -1.38, 95%CI: -2.33 to -0.43), lymphocytes ratio (SMD = -0.48, 95%CI: -0.93 to -0.33) and WBC count (SMD = -0.68, 95%CI: -1.33 to -0.04). However, there was no significant association with IL-10 and CRP (SMD = 0.33, 95%CI: -0.96, 1.62) levels in patients with severe cases of HFMD compared with patients with mild cases.
Fig 3. Forest plots of meta-analysis on a panel of routine laboratory parameters.
A IL-6, B Neutrophils, C Lymphocytes, D CD4+. *Data is converted from the original data.
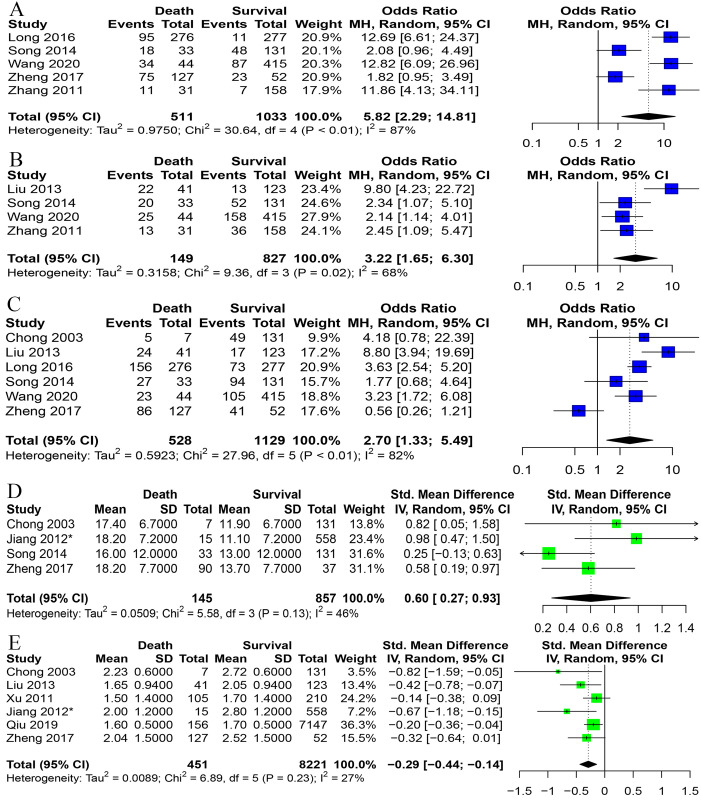
Risk factors for HFMD
For the risk of death from HFMD, we analyzed sex, age, cyanosis, fast heart rate, vomiting, duration of fever ≥3 days, and WBC count. Cyanosis (OR = 5.82, 95% CI: 2.29 to 14.81), fast heart rate (OR = 3.22, 95% CI: 1.65 to 6.30), and vomiting (OR = 2.70, 95% CI: 1.33 to 5.49) were risk factors for death in HFMD patients. A duration of fever ≥3 days and male sex had no significant risk of death from the disease. The WBC count (SMD = 0.60, 95% CI: 0.27 to 0.93) was elevated in patients who died compared with those who survived. Patient age was lower in patients who died compared with those who survived (SMD = -0.29, 95% CI: -0.44 to -0.14) (Fig 4 and S1 Table).
Fig 4. Forest plots on a panel of risk factors.
A Cyanosis, B Fast heart rate, C Vomiting, D WBC count, E Age. *Data is converted from the original data.
Sensitivity analysis and publication bias
Sensitivity analysis that omitted one study at a time shows that the results of our analysis are robust (S1–S3 Figs). The heterogeneity between the studies varied substantially. Publication bias, measured by Begg’s and Egger’s tests, was evident in only three analyses. However, these two tests may lack the statistical power to detect bias when the number of studies is small (i.e., fewer than 10), as we only included 3–8 studies.
Discussion
Children are most vulnerable to HFMD, even though most cases can be treated effectively. However, there are still some severe cases that progress rapidly and die in a short time from cardiopulmonary failure [8, 50]. With the issues related to an aging population, some countries have introduced corresponding policies to alleviate the problem of population aging, such as the introduction of the three-child policy, which makes the susceptible population to HFMD gradually increase. In our review, 32 articles and a total of 781903 HFMD cases in the region of China and Singapore were included.
All of the factors that we analyzed in the review significantly increased the risk of poor prognosis in patients with HFMD. The earlier the identification of the factors we analyzed occurred, the better the intensification of HFMD was avoided. Therefore, doctors need to know these factors to reduce severe cases of HFMD. Our review showed that all of the clinical symptoms had significant heterogeneity and related with HFMD, and a random effects model was used. China has published diagnosis and treatment guidelines for HFMD [51], which included earlier identification of severe patients. Some of our analyzed clinical signs were included in the guidelines, while others were not. A relevant meta-analysis involving 19 separate studies found that clinical characteristics such as convulsion, vomiting, limb shaking and fever were significantly increased risk of severe HFMD which is consistent with our results [12]. In addition, previous studies on hypersomnia have same conclusion: thought that hypersomnia have increased risk of severe HFMD [52]. For these reasons, we should increase the detection of some earlier diagnosis clinical signs that were not included in guidelines, such as stiff neck, hyperarousal and hypersomnia.
In terms of the routine laboratory parameters of HFMD, the Chinese diagnosis and treatment guidelines included WBC count, which we analyzed in this review. Although we extracted and analyzed the WBC count, the results of the analysis are different from the guidelines, and the lack of literature could have led to this result. Compared to those in patients with mild HFMD, the IL-6 and neutrophil ratio levels were increased in patients with severe HFMD, and the lymphocyte ratio and CD4+ count were reduced. In addition, CRP level was not associated with intensification of HFMD. Therefore, we think that the IL-6 levels, CD4+ levels, neutrophil ratio and lymphocyte ratio could be used as reference indices to identify patients with severe HFMD.
Currently, the risk factors for death from HFMD are not completely clear. Therefore, it is important to identify the risk factors associated with patients who died from HFMD. In this review, we evaluated the risk factors for HFMD in patients. Age is a significant factor that is associated with HFMD morbidity and death. Cyanosis and vomiting were reported in many studies, that suggested both were associated with HFMD mortality and were confirmed in the review [33, 38]. According to our results, a fast heart rate was a risk factor for death from HFMD. The WBC count is increased when patients have a poor prognosis. Wang et al. found that male patients more easily died from HFMD than female patients [53]. However, our study showed that male sex variable was not associated with death from HFMD. Similarly, a duration of fever ≥3 days was not associated with HFMD mortality.
Our study also had some limitations. First, our study did not analyze some variables because these indicators lacked data in the included articles. Second, our study had a certain amount of influence on the quality of the included articles. Third, we included 32 articles in this study, but relatively fewer literatures were included for every index and, at most, 11 articles were included. Fourth, almost all of the included articles were from China, and only one of the articles was from Singapore. When we excluded the article from Singapore, the results of the review were not altered.
Conclusions
In conclusion, China many regions had an occurrence of HFMD. China was the country with the highest incidence of HFMD. May to June was peak of the epidemic, and low age were a high-risk group of death. According to the results, cyanosis, a fast heart rate, vomiting and an increased WBC count appeared to increase HFMD mortality. We found that twelve factors are associated with the severe HFMD. Previous conclusion showed that convulsion, hypersomnia, vomiting, limb shaking and fever were significantly increased risk of severe HFMD which is consistent with our results. More attention should be paid when patients exhibit hypersomnia, convulsions, stiff neck, vomiting, limb shaking, hyperarousal, fever, breathlessness and certain laboratory parameters (IL-6 levels, CD4+ levels, neutrophil ratio and lymphocyte ratio) which could reduce the intensification of HFMD. In addition, relevant departments should combine epidemiological characteristics, risk factors and clinical signs to formulate policies to control and prevent HFMD.
Supporting information
A Breathlessness, B Convulsion, C Fever, D Hyperarousal, E Hypersomnia, F Limb shaking, G Stiff neck, H Vomiting.
(TIF)
A CD4+, B CRP, C IL-6, D IL-10, E Lymphocytes, F Neutrophils, G WBC count.
(TIF)
A Age, B Cyanosis, C Duration of fever ≥ 3 days, D Fast heart rate, E Male, F Vomiting, G WBC count.
(TIF)
(DOCX)
(DOCX)
(DOC)
(PDF)
(DOCX)
Acknowledgments
We wish to thank all the participants for volunteering their time to participate in this study and Bianli XU for supporting fund to this research.
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
The funder of Henan Young and Middle-aged Health Science and Technology Innovation talent Project (YXKC2020006) is Xueyong Huang, who is involved study design and decision to publish. The funders of Natural Science Foundation of China (81773500) and study on the epidemiology had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The project leader of Natural Science Foundation of China (81773500) has retired for three years, and the project is being run temporarily by Xueyong Huang, the second project leader.
References
- 1.Li ZQ, Qin ZQ, Tan HF, Zhang CH, Xu JX, Chen J, et al. Analysis of the coverage of inactivated enterovirus 71 (EV71) vaccine and adverse events following immunization with the EV71 vaccine among children from 2016 to 2019 in Guangzhou. Expert Rev Vaccines. 2021:1–12. Epub 2021/05/27. doi: 10.1080/14760584.2021.1933451 . [DOI] [PubMed] [Google Scholar]
- 2.Cai K, Wang Y, Guo Z, Yu H, Li H, Zhang L, et al. Clinical characteristics and managements of severe hand, foot and mouth disease caused by enterovirus A71 and coxsackievirus A16 in Shanghai, China. BMC Infect Dis. 2019;19(1):285. Epub 2019/03/29. doi: 10.1186/s12879-019-3878-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kou Z, Jia J, Liu X, Luo T, Xin X, Gong J, et al. Epidemiological characteristics and spatial-temporal clusters of hand, foot, and mouth disease in Qingdao City, China, 2013–2018. PLoS One. 2020;15(6):e0233914. doi: 10.1371/journal.pone.0233914 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Li Y, Yang Y, Peng C, Fu X, Gu X, et al. Virological investigation of genetic variation of enterovirus type 71 in hand, foot and mouth disease. Exp Ther Med. 2020;20(1):543–9. Epub 2020/06/17. doi: 10.3892/etm.2020.8728 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.He X, Dong S, Li L, Liu X, Wu Y, Zhang Z, et al. Using a Bayesian spatiotemporal model to identify the influencing factors and high-risk areas of hand, foot and mouth disease (HFMD) in Shenzhen. PLoS Negl Trop Dis. 2020;14(3):e0008085. Epub 2020/03/21. doi: 10.1371/journal.pntd.0008085 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xing W, Liao Q, Viboud C, Zhang J, Sun J, Wu JT, et al. Hand, foot, and mouth disease in China, 2008–12: an epidemiological study. The Lancet Infectious Diseases. 2014;14(4):308–18. doi: 10.1016/S1473-3099(13)70342-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Phung D, Nguyen HX, Nguyen HLT, Do CM, Tran QD, Chu C. Spatiotemporal variation of hand-foot-mouth disease in relation to socioecological factors: A multiple-province analysis in Vietnam. Sci Total Environ. 2018;610–611:983–91. Epub 2017/08/26. doi: 10.1016/j.scitotenv.2017.08.158 . [DOI] [PubMed] [Google Scholar]
- 8.Koh WM, Bogich T, Siegel K, Jin J, Chong EY, Tan CY, et al. The Epidemiology of Hand, Foot and Mouth Disease in Asia: A Systematic Review and Analysis. Pediatr Infect Dis J. 2016;35(10):e285–300. Epub 2016/06/09. doi: 10.1097/INF.0000000000001242 Communicable Disease Public Health Research (CDPHRG12NOV021), the Centre for Infectious Disease Epidemiology and Research, the Ministry of Education Tier 1 grant and the President’s Graduate Fellowship to W.M.K. The funders had no role in the decision to publish. T.B. is employed by commercial company, Standard Analytics. The remaining authors have no financial relationships relevant to this article to disclose. The authors have no conflicts of interest to disclose. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Upala P, Apidechkul T, Suttana W, Kullawong N, Tamornpark R, Inta C. Molecular epidemiology and clinical features of hand, foot and mouth disease in northern Thailand in 2016: a prospective cohort study. BMC Infect Dis. 2018;18(1):630. Epub 2018/12/14. doi: 10.1186/s12879-018-3560-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J, Zhou J, Xie G, Zheng S, Lou B, Chen Y, et al. The Epidemiological and Clinical Characteristics of Hand, Foot, and Mouth Disease in Hangzhou, China, 2016 to 2018. Clin Pediatr (Phila). 2020;59(7):656–62. Epub 2020/03/10. doi: 10.1177/0009922820910822 . [DOI] [PubMed] [Google Scholar]
- 11.Esposito S, Principi N. Hand, foot and mouth disease: current knowledge on clinical manifestations, epidemiology, aetiology and prevention. Eur J Clin Microbiol Infect Dis. 2018;37(3):391–8. doi: 10.1007/s10096-018-3206-x . [DOI] [PubMed] [Google Scholar]
- 12.Sun BJ, Chen HJ, Chen Y, An XD, Zhou BS. The Risk Factors of Acquiring Severe Hand, Foot, and Mouth Disease: A Meta-Analysis. Can J Infect Dis Med Microbiol. 2018;2018:2751457. doi: 10.1155/2018/2751457 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen B, Yang Y, Xu X, Zhao H, Li Y, Yin S, et al. Epidemiological characteristics of hand, foot, and mouth disease in China: A meta-analysis. Medicine (Baltimore). 2021;100(20):e25930. doi: 10.1097/MD.0000000000025930 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li P, Huang Y, Zhu D, Yang S, Hu D. Risk Factors for Severe Hand-Foot-Mouth Disease in China: A Systematic Review and Meta-Analysis. Front Pediatr. 2021;9:716039. doi: 10.3389/fped.2021.716039 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiang Y, Xu J, Lai H, Lin H. Association between Meteorological Parameters and Hand, Foot and Mouth Disease in Mainland China: A Systematic Review and Meta-Analysis. Iranian journal of public health. 2021;50(9):1757–65. doi: 10.18502/ijph.v50i9.7046 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giang HTN, Banno K, Minh LHN, Trinh LT, Loc LT, Eltobgy A, et al. Dengue hemophagocytic syndrome: A systematic review and meta-analysis on epidemiology, clinical signs, outcomes, and risk factors. Rev Med Virol. 2018;28(6):e2005. Epub 2018/08/16. doi: 10.1002/rmv.2005 . [DOI] [PubMed] [Google Scholar]
- 17.Mena LJ, Felix VG, Melgarejo JD, Maestre GE. 24-Hour Blood Pressure Variability Assessed by Average Real Variability: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2017;6(10). Epub 2017/10/21. doi: 10.1161/JAHA.117.006895 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen M. The risk factors of enterovirus 71 infected hand-foot-mouth disease and its clinical care. Chinese Journal of Microecology. 2015;27(10):1190–4, 8. [Google Scholar]
- 19.Chen x, Ge h, Xie q. Significance of detection of serum procalcitonin,C reactive protein,interleukin-6 and interleukin-10 in children with hand-foot-and-mouth disease. Chinese Journal of Microecology. 2013;25(1):54–7. [Google Scholar]
- 20.C C-Y, C K-P, Wym N, G L, T Te-S, L S-H, et al. Hand, foot and mouth disease in Singapore: a comparison of fatal and non-fatal cases. Acta Paediatrica. 2003;92(10):1163–9. doi: 10.1111/j.1651-2227.2003.tb02478.x [DOI] [PubMed] [Google Scholar]
- 21.Deng HL, Zhang YF, Li YP, Zhang Y, Xie Y, Wang J, et al. N-terminal pro-brain natriuretic peptide levels associated with severe hand, foot and mouth disease. BMC Infect Dis. 2016;16(1):585. Epub 2016/10/21. doi: 10.1186/s12879-016-1929-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han FX, Gao JH, Gai JH. Clinical significance of combined liver function and high-sensitivity C-reactive protein measurement in children with hand-foot-mouth disease. Genet Mol Res. 2016;15(3). Epub 2016/10/06. doi: 10.4238/gmr.15038744 . [DOI] [PubMed] [Google Scholar]
- 23.Han J, Wang Y, Gan X, Song J, Sun P, Dong XP. Serum cytokine profiles of children with human enterovirus 71-associated hand, foot, and mouth disease. J Med Virol. 2014;86(8):1377–85. Epub 2014/03/13. doi: 10.1002/jmv.23929 . [DOI] [PubMed] [Google Scholar]
- 24.Han L, Sun B, Zheng C. The Early Condition Analysis and Prognostic Evaluation of Hand-foot-mouth Disease Children. Chinese General Practice. 2011;14(2B):466–8. [Google Scholar]
- 25.He Y, Feng Z, Wang W, Chen Y, Cheng J, Meng J, et al. Global cytokine/chemokine profile identifies potential progression prediction indicators in hand-foot-and-mouth disease patients with Enterovirus A71 infections. Cytokine. 2019;123:154765. Epub 2019/07/01. doi: 10.1016/j.cyto.2019.154765 . [DOI] [PubMed] [Google Scholar]
- 26.Huang X, Fan L, Chen G. The change and clinical significance of serum IL-6, IL-10 and IL-17 level in children with hand,foot and mouth disease. Chongqing Medicine. 2012;41(30):3157–9. [Google Scholar]
- 27.Jiang T, Li SJ, Ouyang WX, Tan YF, Liu FR, Xiao GJ, et al. [Changes in Th17 and CD4+CD25+ Treg cells and their significance among children with hand, foot and mouth disease]. Zhongguo Dang Dai Er Ke Za Zhi. 2013;15(12):1113–5. Epub 2013/12/18. . [PubMed] [Google Scholar]
- 28.Jiang T, Zhang H, Zhang T, Liang L, Wu H et al. Clinical analysis of 573 cases of hand,foot,and mouth disease. Journal of Pathogen Biology. 2012;7(3):216–9. [Google Scholar]
- 29.Li F, Li W. Clinical characteristics of sever hand,foot,and mouth disease. Chinese Journal of Nosocomiology. 2014;24(22):5688–90. [Google Scholar]
- 30.Li W, Teng G, Tong H, Jiao Y, Zhang T, Chen H, et al. Study on risk factors for severe hand, foot and mouth disease in China. PLoS One. 2014;9(1):e87603. Epub 2014/02/04. doi: 10.1371/journal.pone.0087603 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li Y, Dang S, Deng H, Wang W, Jia X, Gao N, et al. Breastfeeding, previous Epstein-Barr virus infection, Enterovirus 71 infection, and rural residence are associated with the severity of hand, foot, and mouth disease. Eur J Pediatr. 2013;172(5):661–6. doi: 10.1007/s00431-013-1939-1 . [DOI] [PubMed] [Google Scholar]
- 32.Liu T, Jiang B, Niu W, Ding S, Wang L, Sun D, et al. [Analysis of clinical features and early warning indicators of death from hand, foot and mouth disease in Shandong province]. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine]. 2013;47(4):333–6. . [PubMed] [Google Scholar]
- 33.Long L, Gao LD, Hu SX, Luo KW, Chen ZH, Ronsmans C, et al. Risk factors for death in children with severe hand, foot, and mouth disease in Hunan, China. Infect Dis (Lond). 2016;48(10):744–8. doi: 10.1080/23744235.2016.1185801 . [DOI] [PubMed] [Google Scholar]
- 34.Pan J, Chen M, Zhang X, Chen Y, Liu H, Shen W. High risk factors for severe hand, foot and mouth disease: a multicenter retrospective survey in Anhui Province China, 2008–2009. Indian journal of dermatology. 2012;57(4):316–21. doi: 10.4103/0019-5154.97683 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pan Z, Shen Y, Liang C, Xue W, Peng M, Hu P, et al. Peripheral blood natural killing T cell number decrease,inhibitory receptor upregulation and dysfunction may participate in the severity of hand,foot and mouth disease. Immunological Journal. 2019;35(9):790–8. [Google Scholar]
- 36.Qiu J, Yan H, Cheng N, Lu X, Hu X, Liang L, et al. The Clinical and Epidemiological Study of Children with Hand, Foot, and Mouth Disease in Hunan, China from 2013 to 2017. Sci Rep. 2019;9(1):11662. doi: 10.1038/s41598-019-48259-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ren JS, Sun HM, Zhang L, Lin JD, Wen C, Fang DH. [Expression of vasoactive intestinal peptide in peripheral blood of children with hand, foot and mouth disease]. Zhongguo Dang Dai Er Ke Za Zhi. 2016;18(11):1106–10. doi: 10.7499/j.issn.1008-8830.2016.11.010 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Song CL, Cheng YB, Chen D, Gu X, Li HB, Yan XQ. [Risk factors for death in children with severe hand, foot and mouth disease]. Zhongguo Dang Dai Er Ke Za Zhi. 2014;16(10):1033–6. . [PubMed] [Google Scholar]
- 39.Tang F, Ji H, Li L, Zu R, Xu K, Huo X, et al. Case-control study on effect factors of serve Hand-foot-mouth disease among children. Acta Universitatis Medicinalis Nanjing. 2011;31(1):123–6, 8. [Google Scholar]
- 40.Wang Q, Zhang W, Zhang Y, Yan L, Wang S, Zhang J, et al. Clinical features of severe cases of hand, foot and mouth disease with EV71 virus infection in China. Arch Med Sci. 2014;10(3):510–6. doi: 10.5114/aoms.2014.43745 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Y, Zhao H, Ou R, Zhu H, Gan L, Zeng Z, et al. Epidemiological and clinical characteristics of severe hand-foot-and-mouth disease (HFMD) among children: a 6-year population-based study. BMC Public Health. 2020;20(1):801. doi: 10.1186/s12889-020-08961-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu Q-h, Gao L-d, Huang W, Hu S-x, Zhang F, Deng Z-h, et al. Risk factors of death cases of hand-foot-and-mouth disease in Hunan province. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine]. 2011;45(10):904–8. . [PubMed] [Google Scholar]
- 43.Yang X, Li Y, Zhang C, Zhan W, Xie J, Hu S, et al. Clinical features and phylogenetic analysis of severe hand-foot-and-mouth disease caused by Coxsackievirus A6. Infect Genet Evol. 2020;77:104054. doi: 10.1016/j.meegid.2019.104054 . [DOI] [PubMed] [Google Scholar]
- 44.Zhang B, Wan X, Ouyang FS, Dong YH, Luo DH, Liu J, et al. Machine Learning Algorithms for Risk Prediction of Severe Hand-Foot-Mouth Disease in Children. Sci Rep. 2017;7(1):5368. doi: 10.1038/s41598-017-05505-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang J, Sun J, Chang Z, Zhang W, Wang Z, Feng Z. Characterization of hand, foot, and mouth disease in China between 2008 and 2009. Biomed Environ Sci. 2011;24(3):214–21. doi: 10.3967/0895-3988.2011.03.002 . [DOI] [PubMed] [Google Scholar]
- 46.Zhang Y, Wu Y, Shi H, Wang L, Zhao Z. Changes of T lymphocyte subsets,NK cells,serum interleukin and TNF alpha in children with hand,foot and mouth disease. Chinese Journal of Nosocomiology. 2016;26(11):2604–6. [Google Scholar]
- 47.Zheng G, Cao J, Yu J, Zhang Z, Liu Q, Chen J. Risk factors for death in children with critical and severe hand-foot-and-mouth disease in Chongqing, China: An observational study. Medicine (Baltimore). 2017;96(49):e8934. doi: 10.1097/MD.0000000000008934 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng W, Shi H, Chen Y, Xu Z, Chen J, Jin L. Alteration of serum high-mobility group protein 1 (HMGB1) levels in children with enterovirus 71-induced hand, foot, and mouth disease. Medicine (Baltimore). 2017;96(17):e6764. doi: 10.1097/MD.0000000000006764 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhou H, Guo S-z, Zhou H, Zhu Y-f, Zhang L-j, Zhang W. Clinical characteristics of hand, foot and mouth disease in Harbin and the prediction of severe cases. Chinese Medical Journal. 2012;125(7):1261–5. doi: 10.3760/cma.j.issn.0366-6999.2012.07.013 [DOI] [PubMed] [Google Scholar]
- 50.Clarkson E, Mashkoor F, Abdulateef S. Oral Viral Infections: Diagnosis and Management. Dent Clin North Am. 2017;61(2):351–63. doi: 10.1016/j.cden.2016.12.005 . [DOI] [PubMed] [Google Scholar]
- 51.Li XW, Ni X, Qian SY, Wang Q, Jiang RM, Xu WB, et al. Chinese guidelines for the diagnosis and treatment of hand, foot and mouth disease (2018 edition). World J Pediatr. 2018;14(5):437–47. doi: 10.1007/s12519-018-0189-8 . [DOI] [PubMed] [Google Scholar]
- 52.Fang Y, Wang S, Zhang L, Guo Z, Huang Z, Tu C, et al. Risk factors of severe hand, foot and mouth disease: a meta-analysis. Scand J Infect Dis. 2014;46(7):515–22. doi: 10.3109/00365548.2014.907929 . [DOI] [PubMed] [Google Scholar]
- 53.Wang Y, Feng Z, Yang Y, Self S, Gao Y, Longini IM, et al. Hand, Foot, and Mouth Disease in China Patterns of Spread and Transmissibility. Epidemiology. 2011;22(6):781–92. doi: 10.1097/EDE.0b013e318231d67a [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A Breathlessness, B Convulsion, C Fever, D Hyperarousal, E Hypersomnia, F Limb shaking, G Stiff neck, H Vomiting.
(TIF)
A CD4+, B CRP, C IL-6, D IL-10, E Lymphocytes, F Neutrophils, G WBC count.
(TIF)
A Age, B Cyanosis, C Duration of fever ≥ 3 days, D Fast heart rate, E Male, F Vomiting, G WBC count.
(TIF)
(DOCX)
(DOCX)
(DOC)
(PDF)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting information files.