Abstract
Background
Ataxia-telangiectasia is an autosomal recessive, multi-system, and life-shortening disease caused by mutations in the ataxia-telangiectasia mutated gene. Although widely reported, there are no studies that give a comprehensive picture of this intriguing condition.
Objectives
Understand the natural history of ataxia-telangiectasia (A-T), as reported in scientific literature.
Search methods
107 search terms were identified and divided into 17 searches. Each search was performed in PubMed, Ovid SP (MEDLINE) 1946-present, OVID EMBASE 1980 –present, Web of Science core collection, Elsevier Scopus, and Cochrane Library.
Selection criteria
All human studies that report any aspect of A-T.
Data collection and analysis
Search results were de-duplicated, data extracted (including author, publication year, country of origin, study design, population, participant characteristics, and clinical features). Quality of case-control and cohort studies was assessed by the Newcastle-Ottawa tool. Findings are reported descriptively and where possible data collated to report median (interquartile range, range) of outcomes of interest.
Main results
1314 cases reported 2134 presenting symptoms. The most common presenting symptom was abnormal gait (1160 cases; 188 studies) followed by recurrent infections in classical ataxia-telangiectasia and movement disorders in variant ataxia-telangiectasia. 687 cases reported 752 causes of death among which malignancy was the most frequently reported cause. Median (IQR, range) age of death (n = 294) was 14 years 0 months (10 years 0 months to 23 years 3 months, 1 year 3 months to 76 years 0 months).
Conclusions
This review demonstrates the multi-system involvement in A-T, confirms that neurological symptoms are the most frequent presenting features in classical A-T but variants have diverse manifestations. We found that most individuals with A-T have life limited to teenage or early adulthood. Predominance of case reports, and case series demonstrate the lack of robust evidence to determine the natural history of A-T. We recommend population-based studies to fill this evidence gap.
Introduction
Ataxia-telangiectasia (A-T) is an autosomal recessive, multi-system, progressive and life-shortening disease due to mutations in the ataxia-telangiectasia mutated (ATM) gene on chromosome 11q.26. The severest form, classical A-T, most often caused by a truncating mutation, results in either the absence of ATM protein or its ATM kinase activity. Variant form with reduced kinase activity presents with a milder phenotype and a slower disease progression [1].
A-T generally presents at 12–18 months with an unsteadiness of gait due to cerebellar ataxia. The ataxia gradually worsens and by the age of 10 years children are unable to walk. Other features such as dysarthria, oculomotor apraxia, dysphagia, choreoathetosis, dystonia, tremor, myoclonus, and peripheral neuropathy gradually develop and often worsen. The majority do not have severe cognitive impairment in childhood, although progressive cognitive impairment has been reported over time [2, 3]. Telangiectasia, the other eponymous feature, develops at 3–4 years of age, mostly in the bulbar conjunctiva but can sometimes be found in other organs such as the bladder. Immunological deficits make individuals with A-T more prone to recurrent infections, particularly sinopulmonary infections with progressive deterioration of lung function. Increased risk of malignancies such as leukaemia, lymphoma, and solid tumours further impact longevity with life expectancy generally limited to 20–30 years of age in people with classical A-T.
This wide spectrum of manifestations and multi-disciplinary interest in A-T means that numerous academic papers have been published on this condition. Whilst textbook and narrative reviews exist [4], no attempt has ever been made to collate the available information to give a complete, multi-faceted picture of this intriguing condition. The aim of this study is to perform a systematic review of all scientific literature reporting the natural history of A-T.
Aims and objectives
To describe the natural history of ataxia-telangiectasia (A-T) from birth to death as presented in existing scientific literature.
P–People of all ages, gender and ethnicity
I (E)–Diagnosis of ataxia-telangiectasia
C–People without ataxia-telangiectasia (where comparison group included)
O—Age of onset of cerebellar gait ataxia
Age of wheelchair use
Length of survival and cause of death
Presenting features of A-T
Understanding levels of AFP throughout life course of A-T
Methods
Protocol and registration
The review protocol can be accessed at Open Science Framework [5].
Eligibility criteria
All study types were included. There were no restrictions on length of follow-up, or type of publication.
Information sources
Six databases (PubMed; Ovid SP (MEDLINE) 1946- present; OVID EMBASE 1980 –present; Web of Science core collection; Elsevier Scopus (Categories; medicine, biochemistry, genetics and molecular biology, immunology and microbiology, neuroscience, pharmacology, toxicology and pharmaceutics, health professions); and the Cochrane Library) were searched from the date of the database creation to 19th August 2021.
Search
Initially A-T was identified by combining “Ataxia-telangiectasia”; “Ataxia-telangectasia”; “Ataxia telangiectasia” “Ataxia telangectasia”; “Louis-Bar”; and “Louis Bar” with the ‘OR’ function. A further 103 search terms were grouped into 17 searches and then combined with the above search using the ‘AND’ function. The full search strategy is given in S1 Protocol. In order to ensure that no relevant search terms were missed both UK and US English spellings were included, truncating was used where appropriate and common misspellings, for example ‘telangectasia’ were included.
Study selection
Included studies were selected as described in Table 1.
Table 1. Criteria for study selection for review of natural history of ataxia-telangiectasia.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Participants | All ages and gender with a diagnosis of A-T | Animals, plants, or no cases with a diagnosis of A-T |
| Type of article | Original research articles/data | Review articles, not original articles |
| Clinical relevance | Described clinical data | Laboratory or animal data only |
| Location | All countries | N/A |
A-T, ataxia-telangiectasia; N/A, not applicable
The review includes reports of cases of A-T at all ages (children and adults). Cases of classical and variant A-T were included. Cases were identified as variant A-T if reported as such or reported to have some ATM protein kinase activity. Other participants were presumed to have classical A-T.
Data collection process
All titles and articles were downloaded to a citation software (Endnote X9; Clarivate Analytics, Philadelphia) and duplicates removed automatically. The search was uploaded into a review software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org) which identified and removed some more duplicates. The remaining articles were sorted by title, year, journal, and authors, and remaining duplicates were manually removed.
One author (EP) screened all titles and abstracts and selected the full text articles. Full text articles were reviewed by EP who extracted data using a bespoke data extraction form (Microsoft Excel, 2016 Microsoft Corporation, United States). Any data extraction difficulties were discussed and resolved with two authors (SO and WW).
The extracted data included author, year of publication, country of origin, study design, study population, number of cases of A-T in study’ participant characteristics such as age, gender, clinical features related to the review’s primary and secondary outcomes.
No assumptions were made during data collection. Only statements about the presence or lack of presence of an outcome were included in the analysis.
Where reported, age of onset/diagnosis for each outcome was extracted. Where symptoms were reported as having occurred ‘by’ an age and the age of onset was not determinable, it was not included.
Outcomes
Primary outcomes
Age of onset of cerebellar gait ataxia
Age of wheelchair use
Length of survival and cause of death
Presenting features of A-T
Understanding levels of AFP throughout life course of A-T
Secondary outcomes
Missed and incomplete diagnoses
Reasons for diagnostic delays
Age of onset of other neurological signs and symptoms, for example movement disorders, dysarthria, developmental delay, imaging findings
- Other diagnosis, types, age of onset and treatments (where available)
- Common recurrent infections
- Respiratory conditions including bronchiectasis, interstitial lung disease
- Malignancies
- Diabetes
- Granulomatous disease
- Skin conditions
- Use of gastrostomy (reasons and age of insertion)
- Laboratory findings including vitamin D, dyslipidaemia
Any other findings
Assessment of risk of bias
Quality assessment of cohort and case-control studies was completed by EP and AY using the Newcastle-Ottawa tool [6], as recommended by the Cochrane Collaboration [7]. The ratings for cohort studies were converted to ARHQ standards [8].
Identification of multiple reports of same cases
In addition to removing duplicates, we identified and combined multiple reports of the same cases, where identifiable and possible. Initial full text review revealed that some cases were included in several reports. We identified such duplications by pattern recognition and matching them on characteristics such as age and gender of the case, presence of unusual diagnoses or other common features, authors, and site of study. The information from such reports were then combined such that in the analyses they represented one patient. However, we acknowledge that not all multiple reports of the same individual can be identified in this manner. Where we were unable to reasonably ascertain that the reports were of the same case, we included them as individual cases.
Statistical analyses
The extracted data were analysed using calculations of total number of a sign/symptom/diagnosis, age range, and median age of onset or diagnosis (dependent on variable). Findings are reported descriptively and where possible data are collated to report median (range, interquartile range) of each presentation or feature of the condition. Statistical analysis was performed in Microsoft Excel 2016 (Microsoft, Redmond).
Dealing with missing data
This review is limited to the data that were available in the included studies. Due to the large number of studies and large volume of missing data, it was not feasible to contact the authors to attempt full data collection on each included case.
Subgroup analysis
A sub-group analysis was performed with the same method as above of cases with presumed or confirmed variant A-T and those with presumed or confirmed classical A-T.
The PRISMA check list was used in compiling this report, S1 Checklist.
Results
Results of the search
The search yielded 209086 titles and abstracts (Fig 1). After removal of 193404 duplicates and exclusion of 14399 articles by review of title and abstract, 1283 full text articles were reviewed.
Fig 1. PRISMA diagram.
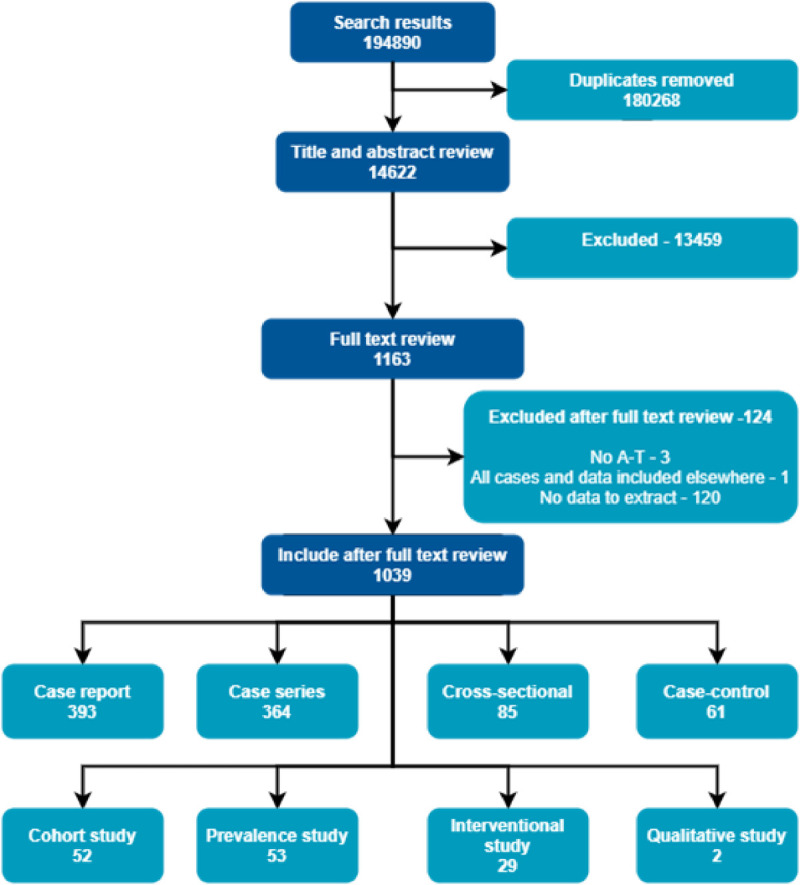
Included studies
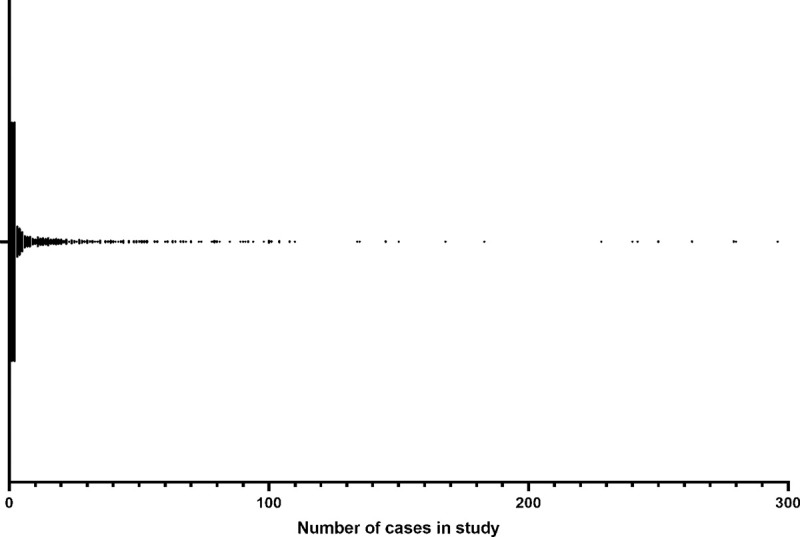
We included 1131 studies of eight different types: 434 case reports, 378 case series, 100 cross-sectional, 70 case-control, 57 cohort, 60 prevalence, 29 interventional, and 3 qualitative studies. Most studies included fewer than 10 cases although there were 33 studies with more than 100 cases each (Fig 2). The median (IQR, range) number of participants per study was 2 (1 to 12, 1 to 585). Six studies [9–14] did not report the number of participants.
Fig 2. Number of cases per study.
A total of 18247 participants were included in these studies. Median age at inclusion was (IQR) (n = 1648) 144.0 months (84.0–240.0). The youngest case was of a 6 day old infant diagnosed by newborn screening programme and the oldest was 78 years of age. Sex was reported in 7840 cases of which 3719 (47.4%) were female. There were 457 (2.5%) confirmed/presumed variant cases included in 60 reports [1, 15–73].
Studies were widely reported across North America, Europe, and parts of Asia. There were fewer reports from Africa, parts of South America and the Middle East.
Family history
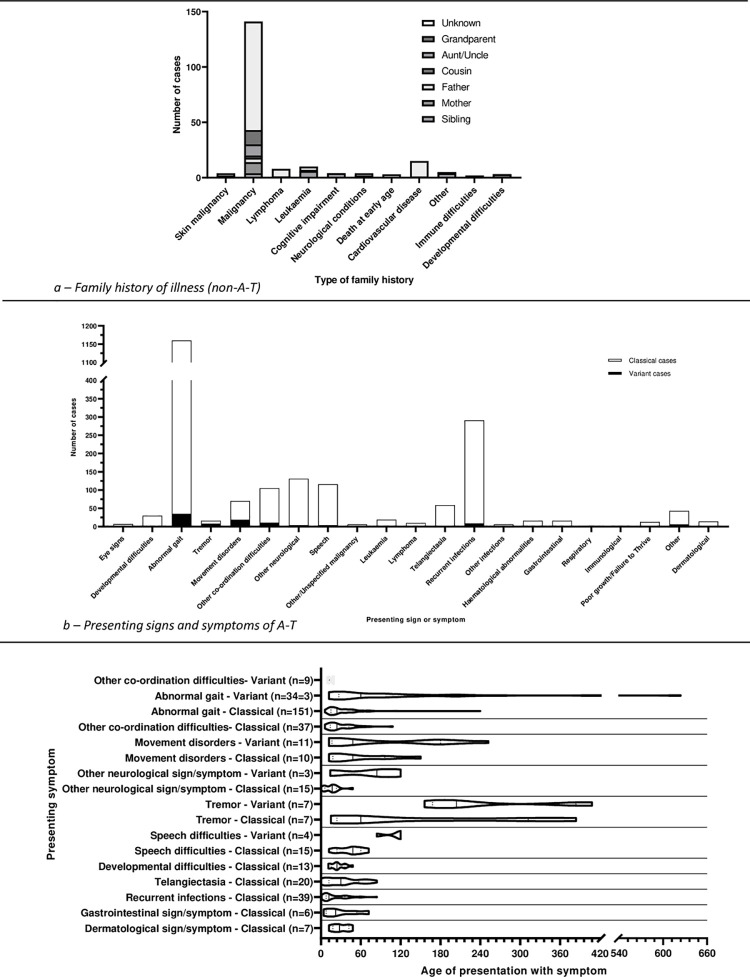
Of the 18246 cases, family history of A-T was reported in 1274 cases (Table 2) and 142 cases (53 studies) had 199 illnesses or symptoms other than A-T in a relative (Fig 3A). 1279 cases (109 studies [15, 53, 65, 71, 72, 78, 87, 88, 95, 99–101, 109, 110, 115, 118–221]) were the children of consanguineous relationships, and 186 cases (86 studies [23, 33, 41, 50, 54, 62, 63, 65, 71, 74, 84, 88, 95, 111, 116, 142, 146, 151–153, 188, 208–210, 212, 214, 216, 218, 219, 221–277]) were reported as being born of non-consanguineous relationships.
Table 2. Family history of ataxia-telangiectasia (A-T) in reported case of A-T.
| Relation with A-T | Number of cases (number of studies) references |
|---|---|
| First degree relative | 710 (151) |
| [17, 24, 27, 28, 33, 37, 41, 49, 58, 66, 72, 76, 90–92, 108, 109, 118–120, 129, 132, 133, 137–140, 145, 152, 161, 168, 170, 172, 175, 176, 180, 183, 185, 195, 196, 200, 204, 211, 221, 225–227, 235, 240, 245, 247–250, 256, 257, 261, 262, 265, 275, 278–369] | |
| Second degree relative | 18 (5) |
| [66, 109, 111, 161, 175, 227] | |
| Third degree relative | 24 (6) |
| [66, 124, 159, 206, 315, 370] | |
| Unspecified relation | 522 (25) |
| [44, 87, 108, 142–144, 154, 156, 162, 175, 177, 182, 195, 199, 211, 213, 352, 371–378] |
Fig 3. Family history of other illness, and presenting symptoms and signs.
Birth and early childhood
Gestational age at birth was reported in 320 cases (68 studies); 289 cases at term gestation, 31 cases <37 weeks gestation. The lowest gestation was reported as “< 30 weeks”. Birth weight was reported in 41 cases (34 studies [43, 59, 63, 84, 108, 110, 111, 139, 178, 206, 212, 231, 242, 252, 254, 263, 268, 272, 276, 298, 305, 325, 372, 380, 384, 391, 399–406]) with median (range) of 2.9.5 (1.32 to 4.08) kg.
Antenatal problems were reported in 20 cases (12 studies [84, 106, 108, 129, 143, 231, 236, 263, 372, 384, 404, 407]) while 25 postnatal concerns were reported in 22 cases (12 studies [84, 214]).
Details are provided in S3-S5 Tables in S1 File.
Diagnosis
329 cases reported an age of diagnosis as shown in Table 3.
Table 3. Age of diagnosis of ataxia-telangiectasia as reported in literature.
| Number of studies (references) | Number of cases | Median (IQR, range) (in months) | |
|---|---|---|---|
| All cases | [221] | 329 | 72.0 (36.0–120.0, 0.7–720.0) |
| [16, 18, 27, 30, 42, 47, 50, 54, 59, 62, 70, 74, 76, 80–83, 89, 99, 101, 103, 105, 106, 110, 111, 113, 116, 119, 121, 122, 124–126, 128, 134, 135, 140, 148, 150, 153, 154, 160, 164–166, 169, 174, 176, 177, 181, 184, 187, 188, 193, 196, 203, 205–208, 211, 214, 219, 221–223, 225, 226, 228–230, 236–238, 240, 241, 245–247, 252, 255, 257, 259, 261–264, 271, 272, 276, 281, 290, 302, 304, 310, 340, 354, 355, 359, 362, 365, 373, 375, 378, 382, 385, 386, 388, 390–392, 394, 396, 404, 405, 408–506] | |||
| Variant cases only | [14] | 14 | 354.0 (231.0–456.0, 24.0–720.0) |
| [16, 18, 27, 30, 42, 47, 50, 54, 59, 62, 65, 70, 71, 363] | |||
| Classical cases only | [209] | 315 | 72.0 (36.0–108.0, 0.7–528.0) |
| [27, 30, 42, 47, 50, 59, 62, 65, 70, 74, 76, 80–83, 89, 99, 101, 103, 105, 106, 110, 111, 113, 116, 119, 121, 122, 124–126, 128, 134, 135, 140, 148, 150, 153, 154, 160, 164–166, 169, 174, 176, 177, 181, 184, 187, 188, 193, 196, 203, 205–208, 211, 214, 215, 217, 219, 221–223, 225, 226, 228–230, 236–238, 240, 241, 245–247, 252, 255, 257, 259, 261–264, 271, 272, 276, 281, 290, 302, 304, 310, 340, 354, 355, 359, 362, 365, 373, 375, 378, 382, 385, 386, 388, 390–392, 394, 396, 404, 405, 408–508] |
17 cases (10 studies [106, 119, 124, 133, 204, 247, 261, 310, 359, 404]) reported a delay in diagnosis. Case reports were excluded from this analysis. Most cases were reported as being diagnosed at the first presentation. Most reported cases were diagnosed without any delay, however a minority were diagnosed late: the median delay in diagnosis (n = 17) was 0.0 i.e., diagnosed at first presentation but there was wide variation with a range of 0.0–312.0 (IQR, 0.0–43.0) months.
Missed, or incorrect diagnoses reported are shown in S1 Fig. Cerebral palsy was the most common incorrect diagnosis. 7 of the 14 cases reported with a specific type of cerebral palsy, had the ataxic form.
Clinical features
The presenting sign(s)/symptom(s) were reported in 1314 cases. These included 2134 signs/symptoms (Fig 3B and 3C).
Neurological
Ataxia and mobility
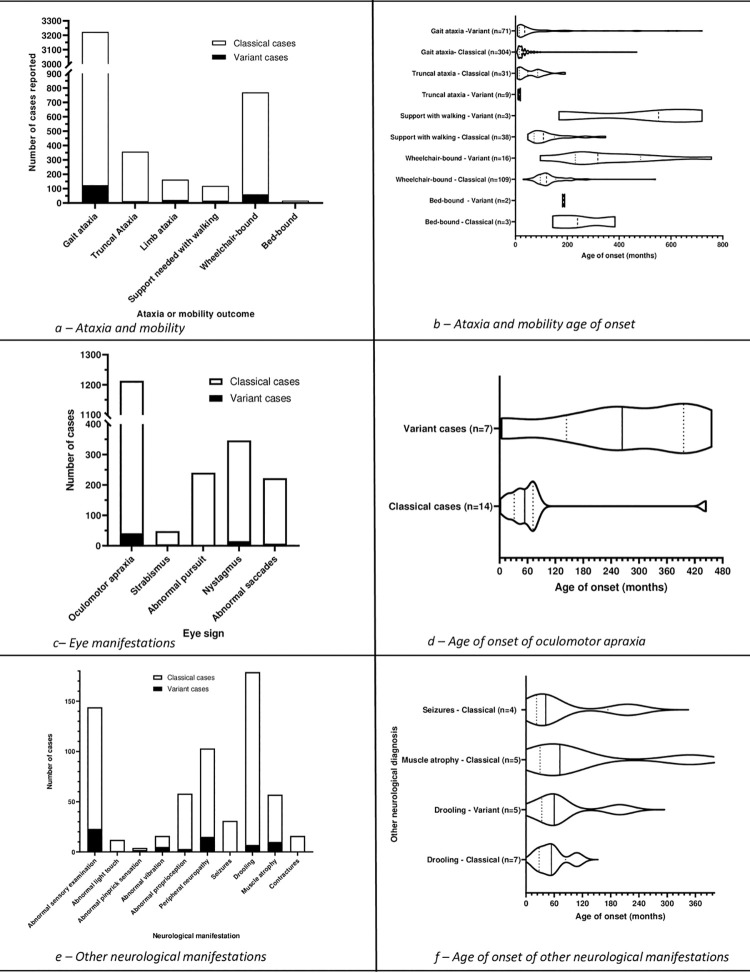
Cerebellar gait ataxia was reported in 3223 cases, truncal ataxia in 357 cases and limb ataxia in 163 cases (Fig 4A).
Fig 4. Ataxia, mobility, eye movements, oculomotor apraxia, and other neurological manifestations.
3 cases (1 study [36]) reported ataxia at 12 months that no longer had ataxia at 48 months, 72 months, and 72 months respectively.
Fig 4B shows all reported age data for cerebellar gait ataxia, truncal ataxia, limb ataxia and mobility.
Eye signs
Data was reported within the included studies on oculomotor apraxia, strabismus, pursuit, nystagmus, and saccades (Fig 4C and 4D).
17 further cases (1 study [537]) may also have had strabismus (reported as lateral gaze deviation or squint).
Other neurological features
Within the included articles, data were reported on sensory examination, peripheral neuropathy, seizures, drooling, muscle atrophy, and contractures (Fig 4E and 4F).
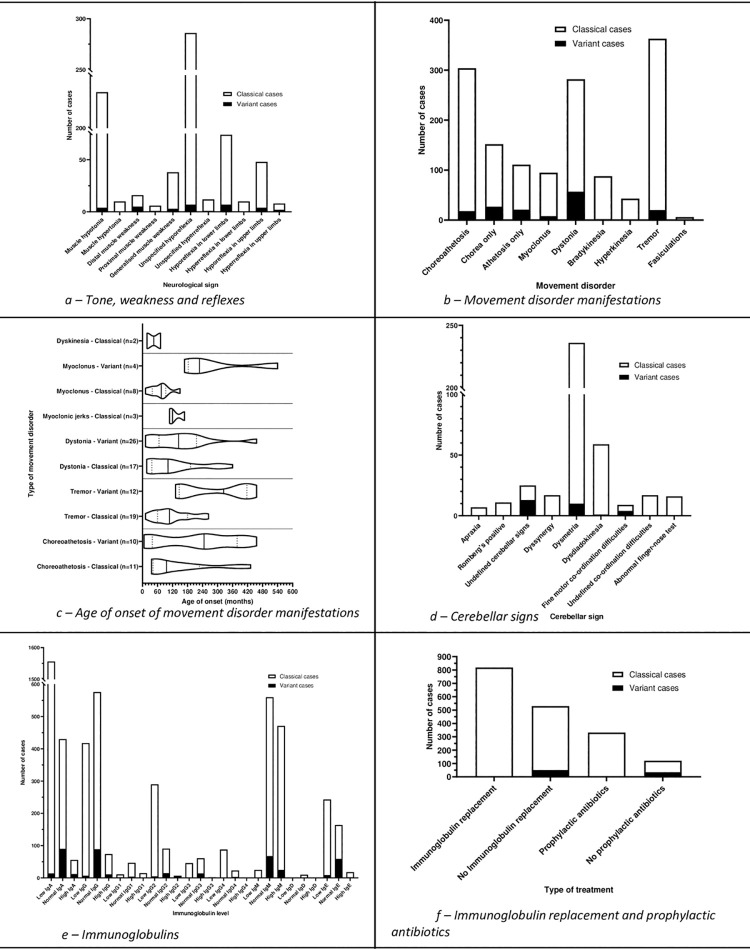
Tone, weakness and reflexes
Included studies reported data on reflexes, muscle tone, and muscle weakness (Fig 5A).
Fig 5. Tone and weakness, movement disorders, cerebellar signs, immunoglobulin levels, immunoglobulin replacement, and prophylactic antibiotics.
Several cases had progression of the reflexes from normal to hyporeflexia over time.
Dysarthria
1219 cases (177 studies [18, 28, 31, 33, 36, 38, 41, 42, 47–49, 52, 57, 59, 62, 63, 65, 66, 72, 73, 75, 76, 80, 84, 87, 95, 99, 100, 103, 106, 108, 109, 111, 116, 118–120, 122, 123, 126, 129, 131, 138–141, 143, 147, 159, 165, 166, 174–176, 179, 181, 190, 191, 202, 206, 208, 211, 213, 216, 217, 219–226, 228–231, 233, 234, 236–238, 240, 242, 245, 247, 248, 251, 254, 255, 260, 265, 268, 271, 276, 278, 285, 287, 288, 290, 298, 303, 305, 310, 319, 323, 325, 326, 331, 335, 339, 342, 345, 347, 348, 363, 366, 368, 369, 372, 379, 380, 384, 388–390, 392, 394–396, 399, 401, 404, 405, 407, 409–411, 414, 415, 431, 435, 439, 440, 448, 449, 469, 472, 476, 479, 490, 494, 495, 501, 518, 519, 524, 528, 529, 534, 537, 538, 540, 541, 544, 555, 563, 574, 585, 586, 590, 604, 607, 609, 620, 625, 629, 633, 651]) reported dysarthria, 39 presumed/confirmed variant cases and 1180 in presumed/confirmed classical cases. Overall, the median age of onset (n = 58) was 60 months (range 12.0–528.0 months, IQR 36.0–96.0 months).
Movement disorders
Included studies reported a wide range of movement disorders (Fig 5B and 5C).
Data were reported on sites of dystonia; 6 cases, upper limb; 7 cases, cervical; 2 cases retrocollis; 2 cases laryngeal; 2 cases truncal; 5 cases, cervical, trunk and limb dystonia; 1 case, leg; 1 case, head; 1 case, oromandibular; and 1 case, finger dystonia.
Cerebellar signs
107 included studies reported cerebellar signs (Fig 5D).
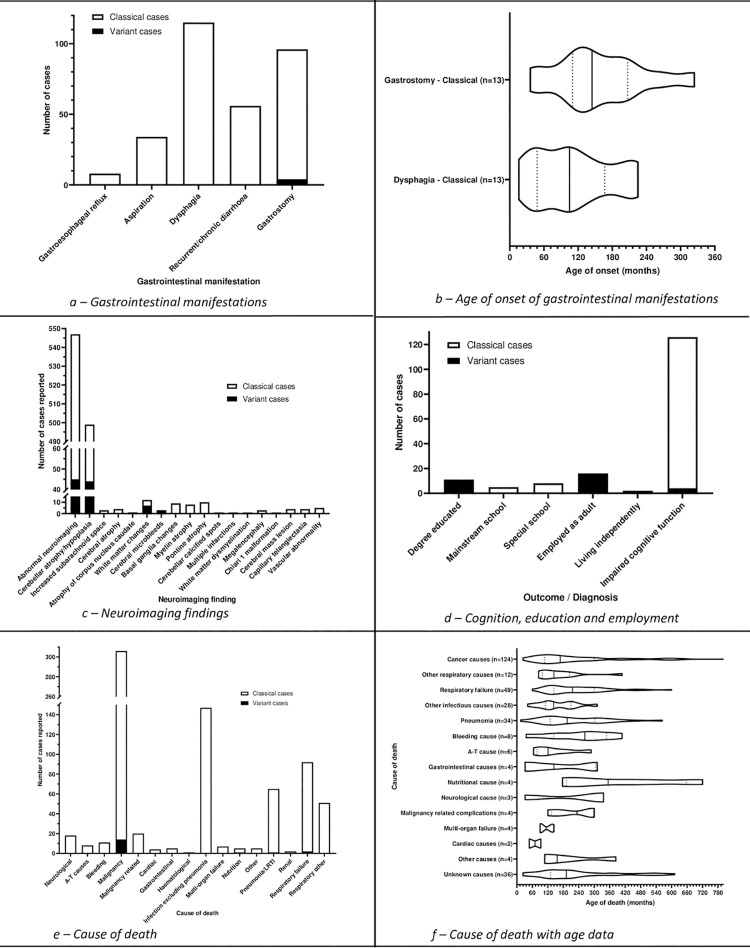
Neuroimaging findings
546 cases (156 studies) reported abnormal neuroimaging (MRI or CT). Cerebellar atrophy/hypoplasia was the most common neuroimaging finding (Fig 8C).
Fig 8. Gastrointestinal, neuroimaging, cognitive and educational manifestations, and cause of death.
All cerebellar atrophy was reported on MRI, except for 46 cases; 21 cases (8 studies [119, 123, 139, 145, 159, 180, 299, 392]) reported it after CT scan, 12 cases (7 studies [108, 231, 276, 345, 347, 358, 464]) reported it at post-mortem, 11 cases (5 studies [191, 225, 355, 378, 467]) reported cerebellar atrophy but did not report the imaging modality, and 2 cases [237, 298] reported it on pneumoencephalogram.
Electromyography (EMG)
62 cases (27 studies [33, 38, 41, 49, 53, 55, 72, 118, 120, 123, 139, 143, 186, 208, 212, 213, 338, 358, 366, 368, 372, 388, 392, 519, 528, 683, 684]) reported an abnormal EMG. The youngest age at which an abnormal EMG was reported was 4 years 0 months. The oldest age a normal EMG reported was 18 years 0 months. 16 cases were reported to have both abnormal motor and sensory nerve conduction. 1 case was reported to have only abnormal motor nerve conduction, and 10 cases were reported to only have abnormal sensory nerve conduction.
Immunology
Immunoglobulin levels and replacement
Reported immunoglobulin levels are shown in (Fig 5E).
819 cases (147 studies) reported the use of immunoglobulin replacement therapy (Figs 5F and 6A). 3 cases (1 study [24]) were received immunoglobulin replacement temporarily. 2 variant cases were reported to receive immunoglobulin replacement [66].
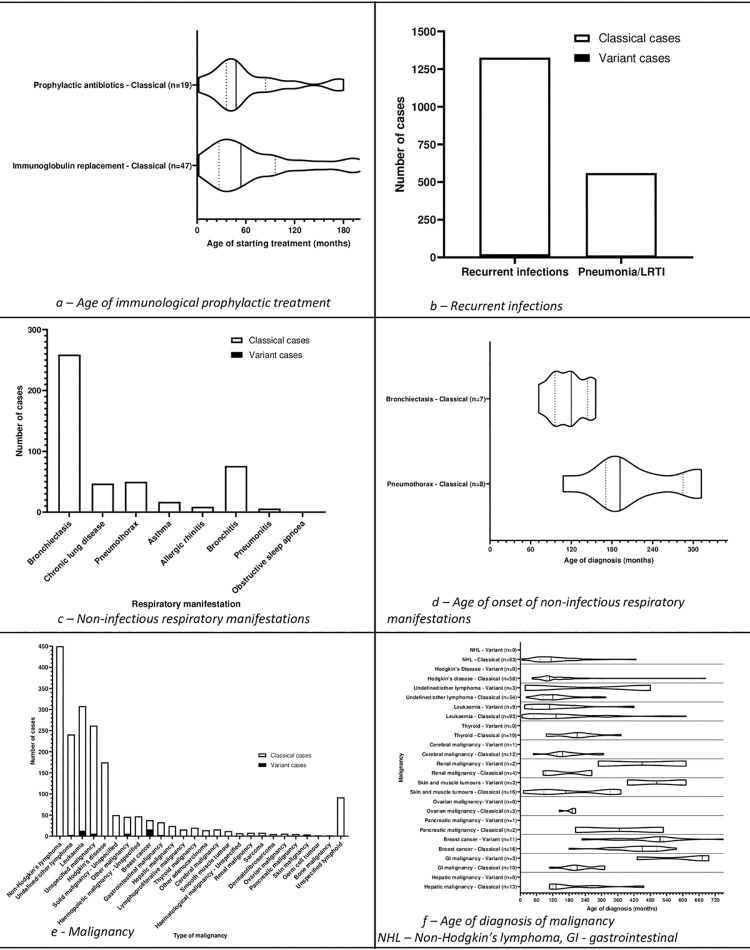
Fig 6. Age at start of prophylactic antibiotic and immunoglobulin replacement, non-infectious respiratory manifestations, and malignancy.
Prophylactic antibiotics
332 cases (56 studies) reported the start of use of prophylactic antibiotics (Figs 7F and 8A) including one [243] who had prophylactic antibiotics post-splenectomy.
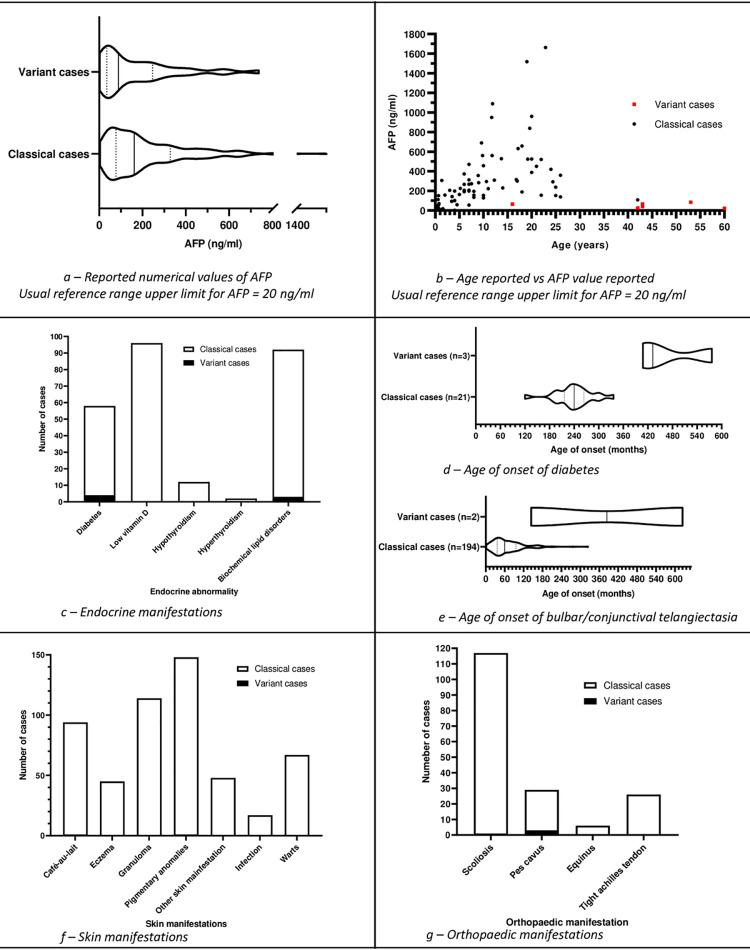
Fig 7. Alpha fetoprotein (AFP), endocrine, bulbar telangiectasia, skin, and orthopaedic manifestations.
Recurrent infections
1326 cases reported recurrent infections (Fig 6B).
Further breakdown of recurrent infections is available in S2 Fig.
Non-infectious respiratory manifestations
Studies included in the review reported non-infectious manifestations including bronchiectasis, chronic lung disease, pneumothorax, asthma, allergic rhinitis, bronchitis, pneumonitis, and obstructive sleep apnoea (Fig 6C and 6D).
259 cases reported bronchiectasis. The youngest age at which bronchiectasis was diagnosed was < 3 years [228]. The oldest child reported with no bronchiectasis was 108.0 months (n = 3) [43] and was in the presumed/confirmed variant group.
50 cases (13 studies) reported pneumothorax. 2 cases (2 studies [91, 240]) reported bilateral pneumothoraces. A further 5 cases (1 study [175]) reported that they had 2 pneumothoraces, but it could not be discerned if it was bilateral or two separate events. 2 cases (1 study [712]) were after gastrostomy tube insertion.
Malignancy
1889 malignancies were reported in 1706 cases (365 studies). Only malignant tumours were included (Fig 6E and 6F).
The median age of diagnosis of NHL (n = 85) reported was 116.4 months (range 6–427.2 months, IQR 72.0–168.0 months). The median age of diagnosis of Hodgkin’s disease (n = 61) reported was 108.0 months (range 44.0–684.0 months, IQR 96.0–166.0 months). The median age of diagnosis of leukaemia (n = 99) reported was 132.0 months (range 1.0–612.0 months, IQR 54.0–204.0 months).
Further breakdown of the results is available in the supplementary files, including the presenting symptoms of Hodgkin’s lymphoma, non-Hodgkin’s lymphoma and leukaemia (S3–S5 Figs).
Alpha-feto protein (AFP) levels
1685 cases (292 studies [21, 22, 24, 27, 28, 30, 33, 35–38, 41, 42, 47–50, 52, 54, 74, 78, 83, 88, 89, 91, 99–101, 103, 105–107, 109, 115, 119–124, 126, 128, 129, 131–135, 138, 140, 143, 147, 148, 150, 160, 161, 165, 166, 168, 169, 172, 174, 177, 180, 183, 184, 191–193, 195–197, 199, 214, 223, 225, 227–229, 233, 236, 238, 239, 241, 244–248, 250–252, 256–259, 261, 263–270, 272, 273, 287, 294, 299, 300, 303, 304, 307, 312, 316, 318, 326, 338, 346, 354, 355, 359, 378, 381–383, 385, 388, 390, 391, 395, 404, 405, 414–419, 422, 423, 428, 429, 431, 433–435, 438–440, 443–445, 448, 450, 451, 455, 458, 460, 461, 464, 468–470, 476, 478, 479, 481–483, 486, 492, 493, 495, 497, 500, 509, 510, 515, 516, 520, 522, 525, 528, 530, 531, 533, 534, 536, 539–541, 545, 550, 556, 558, 564, 567, 570, 575, 576, 580, 582, 583, 589, 591, 597, 599, 601, 604, 609–611, 619, 620, 625, 649, 661, 675, 678, 689, 692, 693, 699, 715, 804, 806, 819, 899–907] [43, 53, 59, 61–63, 65–67, 72, 76, 77, 84, 92, 94–96, 102, 194, 203, 204, 207, 208, 211, 213, 214, 216–219, 221, 233, 362, 363, 368, 369, 375, 396, 398, 409, 411, 424, 481, 501, 504, 521, 532, 616, 628, 631, 641, 642, 768, 893]) reported raised levels of AFP. Reported individual AFP values and relationship between age and AFP level is reported in Fig 7A and 7B.
Endocrine
Reported endocrine manifestations of A-T including diabetes, hypothyroidism and biochemical lipid disorders are described in Fig 7C and 7D.
In addition, 5 cases (1 study [75]) of rickets were reported.
Dermatology
Bulbar telangiectasia
2642 cases (346 studies [17–19, 23, 24, 29, 35–38, 42, 47, 49, 75, 80, 87, 91, 99–101, 103, 104, 106–113, 115, 116, 118–126, 128, 129, 131, 132, 134, 138, 139, 141, 143, 145, 147, 149, 150, 152, 155, 158,166, 168, 172, 174–176, 180, 181, 222–234, 236–240, 242, 244, 247, 248, 250, 251, 254–256, 258–263, 265–267, 278, 281–285, 287–290, 294, 298–300, 302, 304, 305, 307, 309, 310, 316, 317, 319, 323–326, 331, 332, 335, 338–340, 369, 372, 374–376, 382–385, 388–392, 401, 403–405, 407, 410–412, 414–418, 423–429, 431–433, 435, 439, 440, 444, 445, 447, 448, 450, 451, 455–457, 467–470, 472, 473, 476, 477, 513, 518, 520, 523–525, 527, 528, 530, 534–536, 543, 546, 547, 555, 556, 562, 563, 566, 569, 571–576, 580, 582, 583, 588, 589, 591–595, 598–604, 608–610, 651, 770, 841, 918–920] [47, 52, 53, 57, 58, 63, 66–68, 72, 76, 77, 79, 83, 84, 96, 183, 186, 189–194, 196, 197, 199, 202, 204–206, 211–213, 215, 217–221, 231, 269–276, 345–347, 349, 350, 353–355, 358, 361, 365, 366, 368, 378, 393–397, 406, 483, 485, 488, 489, 492–495, 497–499, 501–504, 521, 538, 540, 554, 611, 616, 618, 621, 626, 628, 630, 631, 633, 640, 646, 658, 718, 921–925]; reported bulbar of conjunctival telangiectasia. The age of presentation of bulbar or conjunctival telangiectasia is shown on Fig 7E.
294 cases (80 studies [18, 23, 24, 42, 52–54, 61, 66, 75, 76, 80, 84, 88, 91, 101, 104, 108, 111, 166, 175, 179, 190, 194, 212, 217, 221, 224, 225, 228, 230, 231, 236, 239, 242, 244, 248, 254, 259, 270, 271, 274, 289, 290, 315, 331, 347, 366, 372, 384, 394, 401, 403, 406, 414, 426, 428, 435, 448, 449, 457, 468, 483, 489, 492, 493, 498, 502, 518, 535, 547, 556, 573, 574, 592, 640, 651, 718, 841, 895]) reported other telangiectasia. A breakdown of these results is shown in S6 Fig. Other reported skin manifestations are shown in Fig 7F.
Orthopaedics
Scoliosis, pes cavus abnormalities, equinus foot abnormalities and tight Achilles tendon(s) were reported as shown in Fig 7G.
Four cases reported age of diagnosis of scoliosis (median 131.4 months, range 102.0 months– 172.8 months). An additional 62 cases reported a mean age of diagnosis resulting in overall mean age of diagnosis (n = 66) of 153.0 months. One study [372] reported surgery for left thoracolumbar scoliosis at 14 years.
Gastrointestinal
A variety of gastrointestinal manifestations and interventions were reported (Fig 8A and 8B).
The reported gastrostomy insertion indications are described in S7 Fig.
66 cases (14 studies [35, 226, 233, 345, 431, 448, 449, 463, 659, 743, 768, 818, 909, 916]) reported a diagnosis of fatty liver or hepatic steatosis and age of diagnosis was reported in 2 cases (252.0 months and 336.0 months). Seven cases were in the presumed/confirmed variant group and 59 cases were in the presumed/confirmed classical group.
Other medical problems
The word cloud in S8 Fig shows other medical conditions that were reported in the literature that have not been reported elsewhere in this review.
Reproductive health
7 studies [35, 52, 106, 119, 356, 396, 644] reported 12 cases of pregnancy (8 healthy infants in 4 cases and 8 further cases who were pregnant at least once). 6 presumed/confirmed classical cases and 6 presumed/confirmed variant cases. One study [644] reported one male who had 2 children. There were 2 case reports of primary [251, 636] and 2 cases of secondary [432, 636] amenorrhoea. 2 studies [111, 287] reported 7 cases of delayed menarche. 1 study [52] reported delayed sexual characteristics in 4 of 14 cases. One study [636] reported one case of no puberty by 19 years.
Social outcomes
Included studies reported limited data on cognitive function, employment and education. The data that were reported are shown in Fig 8D.
As expected, there were several reports of delayed neurological development in early life (S9 Fig).
Death
1705 deaths were reported. 294 cases reported age of death (Table 4). 752 causes of death were reported in 687 cases. 1021 cases did not report a cause of death, or it was unknown (Fig 8E and 8F with further details in S6 Table in S1 File).
Table 4. Age of death in ataxia-telangiectasia.
Quality assessment of included studies
72 case control studies were quality assessed. The total number of stars (*) available was 10 with 10 stars representing the best quality. There were one, 10*; 6, 9*; 14, 8*; 17, 7*; 14, 6*; 11, 5*; 7, 4*; and one, 3* studies (see details in S7 Table in S1 File).
58 cohort studies were assessed. Using full criteria 56 studies were rated poor and 2 rated as fair when converted to AHRQ standards. Large numbers of downgrading were due to the lack of a control group. When this criterion was removed, of the 52 studies without a comparable group, 7 studies were rated poor, 29 fair, and 16 good. Details are given in S8 Table in S1 File. The 6 studies that had a comparable cohort were rated as 1 poor (abstract only), 1 fair (full text), and 4 good (all full text).
Discussion
This review puts together a cohesive narrative of evidence based-information about A-T that will allow healthcare professionals and researchers to provide better information to families, and design and deliver research to improve care.
Summary of evidence
We found a large volume of literature on A-T with over 1000 studies included in the analysis. Despite excluding duplicate cases, we found reports of 18247 cases. Most were classical A-T but 2.5% were reported as variants. The worldwide prevalence of variant A-T is not determined as yet.
This review contains cases of A-T from across the world with a large variety of phenotypic features in addition to the expected features including cerebellar gait ataxia and conjunctival/bulbar telangiectasia. There was a wide range in the age of cases reported.
Although cases were reported from 74 countries, nearly a quarter of the cases were from the USA and another quarter from just four other countries (the UK, Italy, Germany, and Turkey). The data presented may therefore be skewed towards presentations as seen in certain parts of the world. There are limited or no cases reported from several regions including Sub-Saharan Africa, parts of South America, and the Middle East. It is unlikely that A-T does not occur in these regions. This distribution may represent the global inequity in the care of children with A-T and a reporting/publication bias.
Main findings
Although, as expected, most cases reported cerebellar ataxia, we found reports of cases with no cerebellar ataxia including 47 reports of classical A-T. These may be incomplete reports, inaccurate diagnoses, or could have been rarer presentations where other features such as leukaemia present before the ataxia manifests. Such reports, especially with a genetic diagnosis, are also more likely with screening pre-symptomatic young children such as when there is a family history.
In keeping with the existing view, we found that the median reported age of wheelchair requirement is 10 years. This requirement comes considerably later, by 26–27 years, in those with variant A-T. As expected, cerebellar gait ataxia was the most reported first presenting symptom however over a quarter did not have ataxia as their first clinical presentation. Dysarthria was reported as the first presentation in 9% of cases. Fewer reports of cases with typical presentations may be less likely to be published due to a bias towards reporting and publication of unusual presentations.
Although we found only a few cases, diagnosis in the newborn period due to screening of those with immunological abnormalities or family history is likely to become more common particularly following the introduction of routine screening for severe combined immunodeficiency disease in several countries including the UK. Such an early diagnosis may confer some benefit such as earlier provision of support for neurological signs and symptoms, treatment for related conditions such as bronchiectasis, and early diagnosis and management of malignancies.
As expected, median age of death was lower in classical cases (14 years 0 months) compared to variant cases (48 years 0 months), likely due to no ATM protein kinase activity resulting in a more severe phenotype in classical cases.
Raised AFP is often used as part of the diagnostic process. Although AFP results were reported in 158 studies, longitudinal results of AFP were very rarely presented. It was difficult to extract AFP data in relation to the time of diagnosis of the various clinical manifestations of A-T. Lower AFP at an older age was seen in those with variant A-T. A longitudinal study of AFP would help to show the pattern of AFP levels throughout the course of the disease and possibly lead to earlier diagnosis of malignancy, or clinical manifestations of A-T, enabling earlier treatments or supportive care.
Secondary outcomes
As A-T is a rare disease, it is not unusual for the condition to be misdiagnosed. We found that, most often, A-T was mis-labelled as cerebral palsy (CP). Since delay in developmental milestones manifest first, the infant is labelled with CP before the recognition of ataxia. In addition, due to its rarity, and perhaps due to limited knowledge of the condition among physicians, A-T may not be considered initially. We found that classical cases were diagnosed at a median age of 6 years and variant cases at 29 years and 6 months. Variant A-T is often diagnosed much later in life when typical symptoms manifest, or a diagnosis is initially missed, or not considered, due to the milder phenotype.
Dystonia was a common feature in both variant and classical cases. Although data were limited to 43 cases, dystonia appears to present earlier in variant compared to classical cases. Dysarthria however was reported at a much older age in the variant group, compared to the classical group similar to oculomotor apraxia.
In comparison to the classical group, very few cases of recurrent infections were reported in variant cases, suggesting immunological impairment is not a common part of the variant phenotype. Despite interstitial lung disease being a recognised complication of A-T, only three cases reported the use of home oxygen. Bronchiectasis was reported more commonly than interstitial lung disease.
Lymphoma and leukaemia were the most common malignancies reported. Very few cases of lymphoma were reported in the variant group where we found reports of a wide variety of solid tumours. We are not aware of a routine screening protocol for malignancy in people with A-T in the UK, despite almost 10% of cases in this review reporting a history of at least 1 malignancy and there are likely to be many more that were not reported. However, some countries do have screening programmes for all people with A-T, which we think would be very helpful, by facilitating early diagnosis of malignancies.
Similarly, although difficulties with nutrition and swallowing are well known in A-T, we found very few cases, mostly of classical A-T, that reported gastrostomy insertion. Data were not sufficient to determine if gastrostomy insertion improved outcomes.
We found some cases of diabetes, youngest at the age of 10 years. Data were limited and we were unable to determine the presence of risk factor and types of treatment needed. There is growing evidence [961] for the development of hepatic steatosis/fatty liver and its association with A-T and we found 66 cases that reported hepatic steatosis and several that reported dyslipidaemia.
As expected, cerebellar atrophy was the most common neuropathological finding reported. Several studies reported mild, moderate or severe cerebellar atrophy, but none presented a standardised classification thus making it difficult to combine the reports. Limited data on EMG/nerve conduction studies were reported in the literature. Some reported peripheral neuropathy. Not much information was available about axonal neuropathy, particularly in children, however EMG is an uncomfortable procedure that is often not tolerated. Exploring this gap in our understanding may enable clinicians to diagnose unsafe swallowing or scoliosis earlier. A longitudinal EMG/nerve conduction study is needed.
Vitamin D deficiency is a concern in A-T exacerbated by advice to avoid sun exposure to reduce the risk of skin cancers. We found 152 cases that reported vitamin D levels and over a third were normal. This demonstrates that it is possible to maintain adequate vitamin D levels with supplementation and appropriate life-style advice.
We found reports of granulomatous disease only among classical cases suggesting that granulomas are linked to a lack of protein kinase. Similarly, scoliosis was only reported in classical cases suggesting that this is a feature of the more severe clinical phenotype.
Few studies reported IQ or cognitive function using a standardised and validated tool. We were unable to determine if A-T is associated with global impairment or if only specific domains are affected. Some cognitive tests are dependent on speech, motor movements and eye movements, and therefore it is difficult to test IQ in people with A-T demonstrating yet another gap in our knowledge of A-T.
Strengths and limitations
Despite our comprehensive literature search and review, we did not find population-based studies and were unable to determine the prevalence of A-T. We have included a wide variety of studies to ensure a complete representation of the available literature. However, this made data extraction and synthesis a challenge. There is no standardised reporting format for A-T. Most case reports concentrate on positive findings and very few report the absence of signs or symptoms. Clinical features were, often, arbitrarily classified such as mild/moderate/severe and in the absence of a standardised classification, such reports could not be compared with each other.
We expect that, similar to other rare diseases, reports of A-T are subject to a reporting and publication bias. It is likely that rarer or unusual presentations are more likely to be published and the typical presentation may be under-represented in literature and, therefore, in this review. We also found several publications from same authors or the same centres. It is possible that some such reports will include the same cases. Duplicate reporting is also more likely in a condition such as A-T due to the multi-system involvement. The same case may be reported several times with publications focusing on a different aspect of the case each time. Where possible, we excluded identifiable duplicates, but it is likely that some may remain unnoticed. Due to the large volume of literature, it was unfeasible to contact authors and request further information on this or other matters. We were unable to access a few full text articles and were limited to English language reports.
We followed a standardised search strategy, data extraction, assessed quality of publications where possible, and combined the available data. Data were only extracted pre-intervention in interventional studies as the intervention could change the natural history of the disease. Where reports only presented non-specific information, data was excluded to ensure reliability. With attention to methodological rigour, we ensured that despite the limitations, this review is a concise yet exhaustive overview of A-T literature.
Conclusion
A-T is a widely reported condition. We found that classical and variant cases are reported in many forms but there is a lack of standardised reporting and population-based studies. Well designed population-based longitudinal cohort studies are required to find the true prevalence and natural history of the condition. Development of core outcomes sets will further enable comparison between populations and cohorts if similar outcomes are reported in a standardised manner in all studies. Such epidemiological research will provide the high-quality evidence needed to improve care of those with A-T and their families and work towards trying to find a cure for this life-shortening disease.
Supporting information
(PDF)
(PDF)
Table S1 Outcome definitions and, Table S2 Study type definitions and, Table S3 Reported antenatal problems and, Table S4 Reported birth weight and gestation and, Table S5 Reported postnatal problems and, Table S6 Detailed cause of death and, Table S7 Quality assessment Case-control studies and, Table S8 Quality assessment Cohort studies.
(PDF)
(PDF)
(XLSX)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
WW is in receipt of an award funding the work from Action for A-T (https://actionforat.org/), A-T Society (https://www.atsociety.org.uk/) and BrAshA-T (https://brashat.org.au/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Jackson T.J., Chow G., Suri M., Byrd P., Taylor M. R., Whitehouse W. P., Longitudinal analysis of the neurological features of ataxia-telangiectasia. Developmental Medicine & Child Neurology, 2016. 58(7): p. 690–7. doi: 10.1111/dmcn.13052 [DOI] [PubMed] [Google Scholar]
- 2.Vinck A., Verhagen M. M., Gerven Mv, de Groot I. J., Weemaes C. M., Maassen B. A, et al., Cognitive and speech-language performance in children with ataxia telangiectasia. Developmental neurorehabilitation, 2011. 14(5): p. 315–22. doi: 10.3109/17518423.2011.603368 [DOI] [PubMed] [Google Scholar]
- 3.Hoche F., et al., The Cerebellar Cognitive Affective Syndrome in Ataxia-Telangiectasia. Cerebellum, 2019. 18(2): p. 225–244. doi: 10.1007/s12311-018-0983-9 [DOI] [PubMed] [Google Scholar]
- 4.Rothblum-Oviatt C., et al., Ataxia telangiectasia: a review. Orphanet Journal Of Rare Diseases, 2016. 11(1): p. 159. doi: 10.1186/s13023-016-0543-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petley E. Scoping Review of the Natural History of Ataxia-Telangiectasia [Internet]. 2021. [Google Scholar]
- 6.Wells GA, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [cited 2021 29 October]. [Google Scholar]
- 7.Higgins JPT and Green S, Cochrane Handbook for Systematic Reviews of Interventions. 2011. [Google Scholar]
- 8.M, V., et al., Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. Agency for Healthcare Research and Quality Methods Guide for Comparative Effectiveness Reviews. 2012. [PubMed] [Google Scholar]
- 9.Kobayashi N., Yata J., Primary Immunodeficiency Diseases And Malignancy In Japan Hiroshi Hayakawa. The Japanese Journal of Pharmacology, 1989. 49(1): p. 135–138. doi: 10.1254/jjp.49.135 [DOI] [PubMed] [Google Scholar]
- 10.Andrade I.G.A., Costa-Carvalho B. T., Sarni R. O. S., Da Silva R., Hix S., Dyslipidemia and reduced antioxidant vitamins in ataxia telangiectasia patients. Journal of Clinical Immunology, 2014. Conference: p. 2014 Clinical Immunology Society, CIS Annual Meeting: Primary Immune Deficiency Diseases North American Conference. Baltimore, MD United States. Conference Publication: (var.pagings). 34 (3) (pp 371). [Google Scholar]
- 11.Iourov I., et al., Mosaic expression of chromosome instability in the ataxia telangiectasia brain. Chromosome Research, 2009. 17: p. 177–178. [Google Scholar]
- 12.Erichsen A.K., Koht J., Stray-Pedersen A., Abdelnoor M., Tallaksen C. M., Prevalence of hereditary ataxia and spastic paraplegia in southeast Norway: a population-based study. Brain, 2009. 132(Pt 6): p. 1577–88. doi: 10.1093/brain/awp056 [DOI] [PubMed] [Google Scholar]
- 13.Bhatt J.M., Bush A., Microbiological surveillance in lung disease in ataxia telangiectasia. European Respiratory Journal, 2014. 43(6): p. 1797–801. doi: 10.1183/09031936.00141413 [DOI] [PubMed] [Google Scholar]
- 14.Lopez-Rodriguez E., Fernandez-Alvarez H., Ordaz-Favila J. C., Ophthalmologic features of the phakomatoses in children. Revista Mexicana de Oftalmologia, 1998. 72(6): p. 302–306. [Google Scholar]
- 15.Bielorai B., Fisher T., Waldman D., Lerenthal Y., Nissenkorn A., Tohami T., et al., Acute lymphoblastic leukemia in early childhood as the presenting sign of ataxia-telangiectasia variant. Pediatric Hematology & Oncology, 2013. 30(6): p. 574–82. doi: 10.3109/08880018.2013.777949 [DOI] [PubMed] [Google Scholar]
- 16.Pajor H.A., Naji Z. A., Lawler M. H. , Adult onset ataxia-telangiectasia with left lower leg malignant sarcoma requiring left knee disarticulation amputation: A case report. PM and R, 2015. Conference: p. 2015 Annual Assembly of the American Academy of Physical Medicine and Rehabilitation. Boston, MA United States. Conference Publication: (var.pagings). 7 (9 SUPPL. 1) (pp S162). [Google Scholar]
- 17.Sutton I.J., Last J. I., Ritchie S. J., Harrington H. J., Byrd P. J., Taylor A. M., Adult-onset ataxia telangiectasia due to ATM 5762ins137 mutation homozygosity. Annals of Neurology, 2004. 55(6): p. 891–5. doi: 10.1002/ana.20139 [DOI] [PubMed] [Google Scholar]
- 18.Krenn M., et al., Adult-onset variant ataxia-telangiectasia diagnosed by exome and cDNA sequencing. Neurol Genet, 2019. 5(4): p. e346. doi: 10.1212/NXG.0000000000000346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Driessen G.J., Ijspeert H., Weemaes C. M., Haraldsson A., Trip M., Warris A., et al., Antibody deficiency in patients with ataxia telangiectasia is caused by disturbed B- and T-cell homeostasis and reduced immune repertoire diversity. Journal of Allergy & Clinical Immunology, 2013. 131(5): p. 1367–75.e9. doi: 10.1155/2015/213928 [DOI] [PubMed] [Google Scholar]
- 20.Sanal O., Ersoy F., Tezcan I., Metin A., Yel L., Berkel A. I., et al., Antibody production against pneumococcal polysaccharide in patients with ataxia-telangiectasia. Molecular Immunology, 1998. 35(11–12): p. 756–756. [DOI] [PubMed] [Google Scholar]
- 21.Liebrich W., Esser M., Emmanuel S, Ataxia telangiectasia. Current Allergy and Clinical Immunology, 2018. 31(4). [Google Scholar]
- 22.Chaila E., Taylor M., Murphy R., Enright H., Ataxia telangiectasia presenting with a normal level of ATM protein, multiple myeloma and prolonged survival. Journal of Neurology, 2005. 252: p. 102–103. [Google Scholar]
- 23.Stankler L., Bennett F. M., Ataxia telangiectasia. Case report of a benign variant with telangiectasia recurrent infection and low IgA. British Journal of Dermatology, 1973. 88(2): p. 187–9. [PubMed] [Google Scholar]
- 24.van Os N.J.H., Jansen A. F. M., van Deuren M., Haraldsson A., van Driel N. T. M., Etzioni A., et al., Ataxia-telangiectasia: Immunodeficiency and survival. Clinical Immunology, 2017. 178: p. 45–55. doi: 10.1016/j.clim.2017.01.009 [DOI] [PubMed] [Google Scholar]
- 25.Tavani F., Zimmerman R. A., Berry G. T., Sullivan K., Gatti R., Bingham P., Ataxia-telangiectasia: the pattern of cerebellar atrophy on MRI. Neuroradiology, 2003. 45(5): p. 315–9. doi: 10.1007/s00234-003-0945-9 [DOI] [PubMed] [Google Scholar]
- 26.Saunders-Pullman R.J., Gatti R., Ataxia-telangiectasia: without ataxia or telangiectasia? Neurology, 2009. 73(6): p. 414–5. doi: 10.1212/WNL.0b013e3181b39140 [DOI] [PubMed] [Google Scholar]
- 27.Simonin C., et al., Attenuated presentation of ataxia-telangiectasia with familial cancer history. Journal of Neurology, 2008. 255(8): p. 1261–3. doi: 10.1007/s00415-008-0857-z [DOI] [PubMed] [Google Scholar]
- 28.Meissner W., Stoppa-Lyonnet D., Couturier J., Hall J., Henry P., Tison F., An atypical variant of ataxia telangiectasia presenting as idiopathic torsion dystonia. Movement Disorders, 2008. 23(1): p. S157–S157. [Google Scholar]
- 29.Paine R.S., Efron M. L., Atypical variants of the ’ataxia telangiectasia’ syndrome. Report of two cases, including one with apparent dominant inheritance. Developmental Medicine & Child Neurology, 1963. 5: p. 14–23. [PubMed] [Google Scholar]
- 30.Georgiev D., Mehta D., Zacharia A., Vinke R. S., Milabo C., Candelario J., et al., Bilateral Deep Brain Stimulation of the Globus Pallidus Pars Interna in a Patient with Variant Ataxia-Telangiectasia. Movement Disorders Clinical Practice, 2016. 3(4): p. 405–408. doi: 10.1002/mdc3.12287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schrader C., Capelle H. H., Kinfe T. M., Dengler R., Dressler D., Krauss J. K., Chronic thalamic deep brain stimulation in ataxia telangiectasia (A-T; Louis-Bar-Syndrome). Movement Disorders, 2009. 24: p. S491–S491. [Google Scholar]
- 32.Verhagen M.M., Abdo W. F., Willemsen M. A., Hogervorst F. B., Smeets D. F., Hiel J. A., et al., Clinical spectrum of ataxia-telangiectasia in adulthood. Neurology, 2009. 73(6): p. 430–7. doi: 10.1212/WNL.0b013e3181af33bd [DOI] [PubMed] [Google Scholar]
- 33.de Graaf A.S., de Jong G., Kleijer W. J., An early-onset recessive cerebellar disorder with distal amyotrophy and, in two patients, gross myoclonia: a probable ataxia telangiectasia variant. Clinical Neurology & Neurosurgery, 1995. 97(1): p. 1–7. [DOI] [PubMed] [Google Scholar]
- 34.Shenhod E., et al., Functional parameter measurements in children with ataxia telangiectasia. Dev Med Child Neurol, 2020. 62(2): p. 207–213. doi: 10.1111/dmcn.14334 [DOI] [PubMed] [Google Scholar]
- 35.Schon K., et al., Genotype, extrapyramidal features, and severity of variant ataxia-telangiectasia. Ann Neurol, 2019. 85(2): p. 170–180. doi: 10.1002/ana.25394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Os N.J.H., et al., Genotype-phenotype correlations in ataxia telangiectasia patients with ATM c.3576G>A and c.8147T>C mutations. J Med Genet, 2019. 56(5): p. 308–316. doi: 10.1136/jmedgenet-2018-105635 [DOI] [PubMed] [Google Scholar]
- 37.Gilad S., et al., Genotype-phenotype relationships in ataxia-telangiectasia and variants. Am J Hum Genet, 1998. 62(3): p. 551–61. doi: 10.1086/301755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Silvestri G., et al., Homozygosity for c 6325T>G transition in the ATM gene causes an atypical, late-onset variant form of ataxia-telangiectasia. Journal of Neurology, 2010. 257(10): p. 1738–40. doi: 10.1007/s00415-010-5583-7 [DOI] [PubMed] [Google Scholar]
- 39.Chopra C., Davies G., Taylor M., Anderson M., Bainbridge S., Tighe P., et al., Immune deficiency in Ataxia-Telangiectasia: a longitudinal study of 44 patients. Clinical & Experimental Immunology, 2014. 176(2): p. 275–82. doi: 10.1111/cei.12262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Staples E.R., McDermott E. M., Reiman A., Byrd P. J., Ritchie S., Taylor A. M., et al., Immunodeficiency in ataxia telangiectasia is correlated strongly with the presence of two null mutations in the ataxia telangiectasia mutated gene. Clinical & Experimental Immunology, 2008. 153(2): p. 214–20. doi: 10.1111/j.1365-2249.2008.03684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saviozzi S., Saluto A., Taylor A. M., Last J. I., Trebini F., Paradiso M. C., et al., A late onset variant of ataxia-telangiectasia with a compound heterozygous genotype, A8030G/7481insA. Journal of Medical Genetics, 2002. 39(1): p. 57–61. doi: 10.1136/jmg.39.1.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Newrick L., Sharrack N., Hadjivassiliou M., Late-onset ataxia telangiectasia. Neurology: Clinical Practice, 2014. 4(4): p. 365–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chrzanowska K., Stumm M., Bialecka M., Saar K., Bernatowska-Matuszkiewicz E., Michalkiewicz J., et al., Linkage studies exclude the AT-V gene(s) from the translocation breakpoints in an AT-V patient. Clinical Genetics, 1997. 51(5): p. 309–13. doi: 10.1111/j.1399-0004.1997.tb02479.x [DOI] [PubMed] [Google Scholar]
- 44.Reiman A., Srinivasan V., Barone G., Last J. I., Wootton L. L., Davies E. G., et al., Lymphoid tumours and breast cancer in ataxia telangiectasia; substantial protective effect of residual ATM kinase activity against childhood tumours. British Journal of Cancer, 2011. 105(4): p. 586–91. doi: 10.1038/bjc.2011.266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carranza D., Vega A. K., Torres-Rusillo S., Montero E., Martinez L. J., Santamaria M., et al., Molecular and Functional Characterization of a Cohort of Spanish Patients with Ataxia-Telangiectasia. NeuroMolecular Medicine, 2017. 19(1): p. 161–174. doi: 10.1007/s12017-016-8440-8 [DOI] [PubMed] [Google Scholar]
- 46.McConville C.M., Stankovic T., Byrd P. J., McGuire G. M., Yao Q. Y., Lennox G. G., et al., Mutations associated with variant phenotypes in ataxia-telangiectasia. American Journal of Human Genetics, 1996. 59(2): p. 320–30. [PMC free article] [PubMed] [Google Scholar]
- 47.Cummins G., et al., Myoclonic head jerks and extensor axial dystonia in the variant form of ataxia telangiectasia. Parkinsonism & Related Disorders, 2013. 19(12): p. 1173–4. doi: 10.1016/j.parkreldis.2013.08.013 [DOI] [PubMed] [Google Scholar]
- 48.Schrader C., Cordes A., Hahn M., Dengler R., Dork T., Natural history, phenotype, and genotype of a case of late-onset ataxia telangiectasia. Movement Disorders, 2006. 21: p. S335–S336. [Google Scholar]
- 49.Verhagen M.M., Martin J. J., van Deuren M., Ceuterick-de Groote C., Weemaes C. M., Kremer B. H., et al., Neuropathology in classical and variant ataxia-telangiectasia. Neuropathology, 2012. 32(3): p. 234–44. doi: 10.1111/j.1440-1789.2011.01263.x [DOI] [PubMed] [Google Scholar]
- 50.Farnsworth E, W.K., Wright D, Mohammad S.S, Bennetts B, Ho G , A novel ATM deletion in a 2-year-old female with variant Ataxia-telangiectasia. Twin Research and Human Genetics, 2019. 22(5): p. 382. [Google Scholar]
- 51.Exley A.R., et al., Premature ageing of the immune system underlies immunodeficiency in ataxia telangiectasia. Clinical Immunology, 2011. 140(1): p. 26–36. doi: 10.1016/j.clim.2011.03.007 [DOI] [PubMed] [Google Scholar]
- 52.Verhagen M.M., Last J. I., Hogervorst F. B., Smeets D. F., Roeleveld N., Verheijen F., et al., Presence of ATM protein and residual kinase activity correlates with the phenotype in ataxia-telangiectasia: a genotype-phenotype study. Human Mutation, 2012. 33(3): p. 561–71. doi: 10.1002/humu.22016 [DOI] [PubMed] [Google Scholar]
- 53.Terenty T.R., Robson P., Walton J. N., Presumed ataxia-telangiectasia in a man. British Medical Journal, 1978. 2(6140): p. 802. doi: 10.1136/bmj.2.6140.802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carrillo F., et al., Prominent oromandibular dystonia and pharyngeal telangiectasia in atypical ataxia telangiectasia. Cerebellum, 2009. 8(1): p. 22–7. doi: 10.1007/s12311-008-0055-7 [DOI] [PubMed] [Google Scholar]
- 55.Byrd P.J., Srinivasan V., Last J. I., Smith A., Biggs P., Carney E. F., Exley A., et al., Severe reaction to radiotherapy for breast cancer as the presenting feature of ataxia telangiectasia. British Journal of Cancer, 2012. 106(2): p. 262–8. doi: 10.1038/bjc.2011.534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Driessen G.J., Jspeert H I., Weemaes C., Harraldsson A., Trip M., Warris A., et al., Severity of antibody deficiency in ataxia telangiectasia is associated with intrinsic defects in B-and T-cell development. Journal of Clinical Immunology, 2012. Conference: p. 15th Biennial Meeting of the European Society for Immunodeficiency, ESID 2012. Florence Italy. Conference Publication: (var.pagings). 32 (SUPPL. 1) (pp S256–S257). [Google Scholar]
- 57.Dork T., Bendix-Waltes R., Wegner R. D., Stumm M., Slow progression of ataxia-telangiectasia with double missense and in frame splice mutations. American Journal of Medical Genetics. Part A, 2004. 126A(3): p. 272–7. doi: 10.1002/ajmg.a.20601 [DOI] [PubMed] [Google Scholar]
- 58.Albertyn C., Cawley N., Taylor A. T. M., Srinivasan V., Last J. I., Murphy R. P., VARIANT ATAXIA TELANGIECTASIA IN SIBLINGS WITH NORMAL alpha-FETOPROTEIN LEVELS. Journal of Neurology Neurosurgery and Psychiatry, 2010. 81(11): p. E48–E48. [Google Scholar]
- 59.Claes K., Depuydt J., Taylor A. M., Last J. I., Baert A., Schietecatte P., et al., Variant ataxia telangiectasia: clinical and molecular findings and evaluation of radiosensitive phenotypes in a patient and relatives. NeuroMolecular Medicine, 2013. 15(3): p. 447–57. doi: 10.1007/s12017-013-8231-4 [DOI] [PubMed] [Google Scholar]
- 60.Mendieta S.G.E., Variant ataxia-telangiectasia in Mennonites and neuromuscular presentations. Movement Disorders, 2013. 28: p. S234–S234. [Google Scholar]
- 61.Saunders-Pullman R., Raymond D., Stoessl A. J., Hobson D., Nakamura K., Pullman S., et al., Variant ataxia-telangiectasia presenting as primary-appearing dystonia in Canadian Mennonites.[Erratum appears in Neurology. 2012 Mar 27;78(13):1029 Note: Nakamura, T [corrected to Nakamura, K]]. Neurology, 2012. 78(9): p. 649–57. doi: 10.1212/01.wnl.0000413427.91173.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paucar M., et al., Variant ataxia-telangiectasia with prominent camptocormia. Parkinsonism Relat Disord, 2019. 62: p. 253–255. doi: 10.1016/j.parkreldis.2018.12.017 [DOI] [PubMed] [Google Scholar]
- 63.Taylor A.M., Flude E., Laher B., Stacey M., McKay E., Watt J., et al., Variant forms of ataxia telangiectasia. Journal of Medical Genetics, 1987. 24(11): p. 669–77. doi: 10.1136/jmg.24.11.669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fiorilli M., Antonelli A., Russo G., Crescenzi M., Carbonari M., Petrinelli P., Variant of ataxia-telangiectasia with low-level radiosensitivity. Human Genetics, 1985. 70(3): p. 274–7. doi: 10.1007/BF00273456 [DOI] [PubMed] [Google Scholar]
- 65.Arıcan P., et al., Variant ataxia-telangiectasia in a child presenting with laryngeal dystonia. Turk J Pediatr, 2020. 62(3): p. 491–494. doi: 10.24953/turkjped.2020.03.019 [DOI] [PubMed] [Google Scholar]
- 66.Bistritzer J., et al., Phenotypic variability in patients with unique double homozygous mutations causing variant ataxia telangiectasia. Eur J Paediatr Neurol, 2021. 32: p. 36–39. doi: 10.1016/j.ejpn.2021.03.008 [DOI] [PubMed] [Google Scholar]
- 67.Chamova T., et al., Clinical variability of variant of ataxia-telangiectasia among Bulgarian patients with mutations in ATM. European Journal of Neurology, 2020. 27(Supplement 1): p. 367–368. [Google Scholar]
- 68.McGrath-Morrow S.A., et al., DNA methylation and gene expression signatures are associated with ataxia-telangiectasia phenotype. Sci Rep, 2020. 10(1): p. 7479. doi: 10.1038/s41598-020-64514-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nambot S., 58P An atypical late-onset case of homozygous ATM variant supported by a complex molecular mechanism of mosaic uniparental isodisomy. Annals of Oncology, 2020. 31(Supplement 5): p. S1235. [Google Scholar]
- 70.Schoenaker M.H.D., et al., Early diagnosis of ataxia telangiectasia in the neonatal phase: a parents’ perspective. European Journal of Pediatrics, 2020. 179(2): p. 251–256. doi: 10.1007/s00431-019-03479-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schröder S., et al., Evidence of pathogenicity for the leaky splice variant c.1066-6T>G in ATM. Am J Med Genet A, 2020. 182(12): p. 2971–2975. doi: 10.1002/ajmg.a.61870 [DOI] [PubMed] [Google Scholar]
- 72.Shimazaki H., et al., Late-onset autosomal recessive cerebellar ataxia and neuropathy with a novel splicing mutation in the ATM gene. J Integr Neurosci, 2020. 19(1): p. 125–129. doi: 10.31083/j.jin.2020.01.1239 [DOI] [PubMed] [Google Scholar]
- 73.Veenhuis S.J.G., et al., Dysarthria in children and adults with ataxia telangiectasia. Dev Med Child Neurol, 2021. 63(4): p. 450–456. doi: 10.1111/dmcn.14811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thompson S., Iyer A., Byrd P., Taylor M., Spinty S., Dopa-Responsive Dystonia and Chorea as a Presenting Feature in Ataxia-Telangiectasia. Movement Disorders Clinical Practice, 2014. 1(3): p. 249–251. doi: 10.1002/mdc3.12048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moin M., Aghamohammadi A., Kouhi A., Tavassoli S., Rezaei N., Ghaffari S. R., et al., Ataxia-telangiectasia in Iran: clinical and laboratory features of 104 patients. Pediatric Neurology, 2007. 37(1): p. 21–8. doi: 10.1016/j.pediatrneurol.2007.03.002 [DOI] [PubMed] [Google Scholar]
- 76.Boyarchuk O., et al., Clinical and immunological presentation of ataxia-telangiectasia. Archives of the Balkan Medical Union, 2020. 55(4): p. 573–581. [Google Scholar]
- 77.Oska S., et al., Melanoma arising in a patient with ataxia-telangiectasia: A call for full skin examinations in this patient population. Pediatr Dermatol, 2020. 37(4): p. 767–768. [DOI] [PubMed] [Google Scholar]
- 78.Azarsiz E., Karaca N. E., Gunaydin N. C., Gulez N., Ozturk C., Aksu G., et al., Do elevated serum IgM levels have to be included in probable diagnosis criteria of patients with ataxia-telangiectasia? International Journal of Immunopathology & Pharmacology, 2014. 27(3): p. 421–7. doi: 10.1177/039463201402700312 [DOI] [PubMed] [Google Scholar]
- 79.Li G.L., Waite E., and Wolfson J., T-cell prolymphocytic leukemia in an adolescent with ataxia-telangiectasia: novel approach with a JAK3 inhibitor (tofacitinib). Blood Advances, 2017. 1(27): p. 2724–2728. doi: 10.1182/bloodadvances.2017010470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mock C., Coleman G., Ree J. H., Abuelo D. N., Crowley J. P., Ataxia telangiectasia and acinic cell carcinoma of the parotid gland. Journal of Surgical Oncology, 1988. 39(2): p. 133–8. doi: 10.1002/jso.2930390214 [DOI] [PubMed] [Google Scholar]
- 81.Stenlake K., Marion M. H., An unusual presentation of ataxia-telangiectasia. Journal of Neurology, 2004. 251: p. 66–67. doi: 10.1007/s00415-004-0273-y [DOI] [PubMed] [Google Scholar]
- 82.Sze S.K., et al., Retrospective Diagnosis of Ataxia-Telangiectasia in an Adolescent Patient With a Remote History of T-Cell Leukemia. J Pediatr Hematol Oncol, 2019. [DOI] [PubMed] [Google Scholar]
- 83.Trimis G.G., Athanassaki C. K., Kanariou M. M., Giannoulia-Karantana A. A., Unusual absence of neurologic symptoms in a six-year old girl with ataxia-telangiectasia. Journal of Postgraduate Medicine, 2004. 50(4): p. 270–1. [PubMed] [Google Scholar]
- 84.Bernard G., Shevell M., The wobbly child: an approach to inherited ataxias. Seminars in Pediatric Neurology, 2008. 15(4): p. 194–208. doi: 10.1016/j.spen.2008.10.011 [DOI] [PubMed] [Google Scholar]
- 85.Osundwa V.M., Dawod S. T., The occurrence of ataxia-telangiectasia and common variable immunodeficiency in siblings: case report. Annals of Tropical Paediatrics, 1994. 14(1): p. 71–3. doi: 10.1080/02724936.1994.11747695 [DOI] [PubMed] [Google Scholar]
- 86.Drolet B.A., Drolet B., Zvulunov A., Jacobsen R., Troy J., Esterly N. B., Cutaneous granulomas as a presenting sign in ataxia-telangiectasia. Dermatology, 1997. 194(3): p. 273–5. doi: 10.1159/000246117 [DOI] [PubMed] [Google Scholar]
- 87.Akturk H., Sutcu M., Somer A., Piskin S., Acar M., Ozmen M., et al., Ataxia telangiectasia in Turkey: multisystem involvement of 91 patients. World Journal of Pediatrics, 2017. 13(5): p. 465–471. doi: 10.1007/s12519-017-0011-z [DOI] [PubMed] [Google Scholar]
- 88.Isaian A., et al., Erratum: BAK, BAX, and NBK/BIK proapoptotic gene alterations in Iranian patients with ataxia telangiectasia (Journal of Clinical Immunology doi: 10.1007/s10875-009-9340-6). Journal of Clinical Immunology, 2010. 30(4): p. 620. [DOI] [PubMed] [Google Scholar]
- 89.Iyer A., Taylor M., Spinty S., Dopa-responsive dystonia in ataxia telangiectasia. Developmental Medicine and Child Neurology, 2014. Conference: p. 2014 Annual Meeting of the British Paediatric Neurology Association. Winchester United Kingdom. Conference Publication: (var.pagings). 56 (SUPPL. 1) (pp 58). doi: 10.1002/mdc3.12048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sanal O., Ozbas-Gerceker F., Yel L., Ersoy F., Tezcan I., Berkel A. I., et al., Defective anti-polysaccharide antibody response in patients with ataxia-telangiectasia. Turkish Journal of Pediatrics, 2004. 46(3): p. 208–13. [PubMed] [Google Scholar]
- 91.Frais M.A., Gastric adenocarcinoma due to ataxia-telangiectasia (Louis-Bar syndrome). Journal of Medical Genetics, 1979. 16(2): p. 160–1. doi: 10.1136/jmg.16.2.160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen K.T.K., Overberg‐Schmidt U. S., Henze G., Low grade non‐hodgkin’s lymphoma after high grade non‐hodgkin’s lymphoma in a child with ataxia teleangiectasia. Cancer, 1994. 74(5): p. 1649–1650. [DOI] [PubMed] [Google Scholar]
- 93.Jacobs M.F., et al., Hepatosplenic αβ T-Cell Lymphoma as Second Malignancy in Young Adult Patient With Previously Undiagnosed Ataxia-Telangiectasia. J Pediatr Hematol Oncol, 2020. 42(6): p. e463–e465. doi: 10.1097/MPH.0000000000001537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kim M., et al., Clinical characteristics of ataxia-telangiectasia presenting dystonia as a main manifestation. Clin Neurol Neurosurg, 2020. 199: p. 106267. doi: 10.1016/j.clineuro.2020.106267 [DOI] [PubMed] [Google Scholar]
- 95.Mandola A.B., et al., Ataxia Telangiectasia Diagnosed on Newborn Screening-Case Cohort of 5 Years’ Experience. Front Immunol, 2019. 10: p. 2940. doi: 10.3389/fimmu.2019.02940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rodriguez R.S., et al., Novel Compound Heterozygous Mutation c.3955_3958dup and c.5825C>T in the ATM Gene: Clinical Evidence of Ataxia-Telangiectasia and Cancer in a Peruvian Family. Mol Syndromol, 2021. 12(5): p. 289–293. doi: 10.1159/000515696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sze S.K., et al., Retrospective Diagnosis of Ataxia-Telangiectasia in an Adolescent Patient With a Remote History of T-Cell Leukemia. J Pediatr Hematol Oncol, 2021. 43(1): p. e138–e140. doi: 10.1097/MPH.0000000000001672 [DOI] [PubMed] [Google Scholar]
- 98.Veiga-Fernandez A., et al., Ataxia-teleangiectasia followed up in a hereditary gynaecological cancer unit of a tertiary hospital. International Journal of Gynecological Cancer, 2020. 30(SUPPL 4): p. A91–A92. [Google Scholar]
- 99.Masri A.T., Bakri F. G., Al-Hadidy A. M., Musharbash A. F., Al-Hussaini M., Ataxia-telangiectasia complicated by craniopharyngioma—a new observation. Pediatric Neurology, 2006. 35(4): p. 287–8. doi: 10.1016/j.pediatrneurol.2006.05.011 [DOI] [PubMed] [Google Scholar]
- 100.Tabatabaiefar M.A., Alipour P., Pourahmadiyan A., Fattahi N., Shariati L., Golchin N., et al., A novel pathogenic variant in an Iranian Ataxia telangiectasia family revealed by next-generation sequencing followed by in silico analysis. Journal of the Neurological Sciences, 2017. 379: p. 212–216. doi: 10.1016/j.jns.2017.06.012 [DOI] [PubMed] [Google Scholar]
- 101.Ben Abdallah Chabchoub R., et al., [Ataxie telangiectasia et telangiectasies vesicales]. Tunisie Medicale, 2014. 92(11): p. 695. [PubMed] [Google Scholar]
- 102.Ahmed O., Felimban Y., and Almehdar A., T cell ALL in a child with Ataxia telangiectasia; diagnosis and management challenges. Hematology, 2021. 26(1): p. 348–354. doi: 10.1080/16078454.2021.1908725 [DOI] [PubMed] [Google Scholar]
- 103.Jawad T., Stallings R. L., Lynch T., Late presentation of ataxia telangiectasia (AT). Movement Disorders, 2004. 19: p. S21–S22. [Google Scholar]
- 104.Lerner B., Ataxia-Telangiectasia. Archives of Dermatology, 1971. 104(3): p. 332–&. [Google Scholar]
- 105.Tomioka H., Kaneoya A., Mochizuki Y., Harada H., Primary diffuse large b-cell lymphoma arising in the tongue accompanied by ataxia-telangiectasia: A case report. Journal of Clinical and Diagnostic Research, 2015. 9(6). doi: 10.7860/JCDR/2015/12121.6107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dawson A.J., Marles S., Tomiuk M., Riordan D., Gatti R. A., Ataxia-telangiectasia with female fertility. American Journal of Medical Genetics. Part A, 2015. 167A(8): p. 1937–9. doi: 10.1002/ajmg.a.37084 [DOI] [PubMed] [Google Scholar]
- 107.Macias M.A., Delamorena M., Bahna S. L., Day N. K., Good R. A., Ataxia Telangiectasia with Agammaglobulinemia-G and Masquerading as Chiari Malformation. Journal of Allergy and Clinical Immunology, 1993. 91(1): p. 145–145. [Google Scholar]
- 108.Harley R.D., Baird H. W., Craven E. M., Ataxia-telangiectasia. Report of seven cases. Archives of Ophthalmology, 1967. 77(5): p. 582–92. doi: 10.1001/archopht.1967.00980020584004 [DOI] [PubMed] [Google Scholar]
- 109.Seshachalam A., Cyriac S., Reddy N., Gnana S., Ataxia telangiectasia: Family management. Indian Journal of Human Genetics, 2010. 16(1): p. 39–42. doi: 10.4103/0971-6866.64940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Alonazi N.A., Hundallah K. J., Al Hashem A. M., Mohamed S., A novel variant in ATM gene causes ataxia telangiectasia revealed by whole-exome sequencing. Neurosciences, 2018. 23(2): p. 162–164. doi: 10.17712/nsj.2018.2.20170463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Utian H.L. and Plit M., Ataxia Telangiectasia. J Neurol Neurosurg Psychiatry, 1964. 27: p. 38–40. doi: 10.1136/jnnp.27.1.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Barsky S., Gigli I., Ataxia Telangiectasia. Archives of Dermatology, 1960. 82(4): p. 657–658. [Google Scholar]
- 113.Harris V.J., Seeler R. A., Ataxia-telangiectasia and Hodgkin’s disease. Cancer, 1973. 32(6): p. 1415–20. doi: [DOI] [PubMed] [Google Scholar]
- 114.Matsuoka M., Matsuoka H., Okada J., Urisu A., Sato C., Torii S., et al., Follow-up studies of immunological disorders in patients with ataxia-telangiectasia II. Study of a boy with T cell malignancy. Japanese Journal of Clinical Immunology, 1983. 6(4): p. 249–258. [Google Scholar]
- 115.Ohta S., Katsura T., Shimada M., Shima A., Chishiro H., Matsubara H., Ataxia-telangiectasia with papillary carcinoma of the thyroid. American Journal of Pediatric Hematology/Oncology, 1986. 8(3): p. 255–7. [PubMed] [Google Scholar]
- 116.Gabhale Y., Vaideeswar P., Bavdekar S. B., Fatal hemoptysis in a child with ataxia-telangiectasia: zeroing down on the rare cause. Journal of Postgraduate Medicine, 2010. 56(4): p. 293–6. doi: 10.4103/0022-3859.70946 [DOI] [PubMed] [Google Scholar]
- 117.Andrade I.G.A., et al., Selenium levels and glutathione peroxidase activity in patients with ataxia-telangiectasia: association with oxidative stress and lipid status biomarkers. Orphanet J Rare Dis, 2021. 16(1): p. 83. doi: 10.1186/s13023-021-01732-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cruz Martinez A., Barrio M., Gutierrez A. M., Lopez E., Abnormalities in sensory and mixed evoked potentials in ataxia telangiectasia. Journal of Neurology Neurosurgery and Psychiatry, 1977. 40(1): p. 44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.de Jonge J., Tijssen C. C., Ataxia telangiectasia in a brother and sister at older age. Clinical Neurology & Neurosurgery, 1988. 90(3): p. 279–81. [DOI] [PubMed] [Google Scholar]
- 120.Saeed M., Ataxia telangiectasia in two brothers and one sister. Pakistan Paediatric Journal, 2014. 38(4): p. 252–256. [Google Scholar]
- 121.Kamiya M., et al., Ataxia telangiectasia with vascular abnormalities in the brain parenchyma: report of an autopsy case and literature review. Pathol Int, 2001. 51(4): p. 271–6. doi: 10.1046/j.1440-1827.2001.01199.x [DOI] [PubMed] [Google Scholar]
- 122.Ingale S.Y., Yadav P., Mishra L., Sukumaran A., Ataxia Telangiectasia: A Rare Case Report. Journal of Evolution of Medical and Dental Sciences-Jemds, 2016. 5(74): p. 5515–5516. [Google Scholar]
- 123.Stell R., Bronstein A. M., Plant G. T., Harding A. E., Ataxia telangiectasia: a reappraisal of the ocular motor features and their value in the diagnosis of atypical cases. Movement Disorders, 1989. 4(4): p. 320–9. doi: 10.1002/mds.870040405 [DOI] [PubMed] [Google Scholar]
- 124.Sharma A., Buxi G., Yadav R., Kohli A., Ataxia telangiectasia: A report of two cousins and review of literature. Indian Journal of Medical and Paediatric Oncology, 2011. 32(4): p. 217–222. doi: 10.4103/0971-5851.95145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bagis H S.H., Aydin H, Ozturk O, Ataxia telangiectasia: Case report. Gazi Medical Journal 2019. doi: 10.2478/folmed-2018-0045 [DOI] [PubMed] [Google Scholar]
- 126.Kanaganayagam A., Ataxia telangiectasia—a case report. Medical Journal of Malaysia, 1980. 35(2): p. 139–43. [PubMed] [Google Scholar]
- 127.Sasihuseyinoglu A.S., Yllmaz M., Bisgin A., Dogruel D., Altintas D. U., Duyuler G., et al., Ataxia-Telangiectasia Clinical and Laboratory Features: Single Center Results. Pediatric, Allergy, Immunology, and Pulmonology, 2018. 31(1): p. 9–14. [Google Scholar]
- 128.Aghamohammadi A., Imai K., Moazzami K., Abolhassani H., Tabatabaeiyan M., Parvaneh N., et al., Ataxia-telangiectasia in a patient presenting with hyper-immunoglobulin M syndrome. Journal of Investigational Allergology & Clinical Immunology, 2010. 20(5): p. 442–5. [PubMed] [Google Scholar]
- 129.Maqbool S., Ayub Z., Hussain W., Ataxia-telangiectasia in children. JPMA—Journal of the Pakistan Medical Association, 1992. 42(4): p. 101–2. [PubMed] [Google Scholar]
- 130.Porras O., Telatar M., Arguedas O., Abdelnour A., Leiva I., Gatti R. A., Ataxia-Telangiectasia in Costa Rica: Clinical, laboratory and genetic characteristics. Molecular Immunology, 1998. 35(11–12): p. 796–796. [Google Scholar]
- 131.Sales V.S.F., Dias S. M. M., Novaes A. E. M., Rego K. D., Santos E. S. C., Junior G. C., et al., Ataxia-telangiectasia in rio grande do norte: Immunological and clinical features of 5 patients. Journal of Clinical Immunology, 2017. Conference: p. 7th Meeting of the Latin American Society for Immunodeficiencies, LASID 2017. Brazil. 37 (1 Supplement 1) (pp S42–S43). [Google Scholar]
- 132.Sfaihi L., Stoppa Lyonnet D., Ben Ameur S., Dubois D’enghien C., Kamoun T., Barbouch M. R., et al., Ataxia-telangiectasia in the south of Tunisia: A study of 11 cases. Tunisie Medicale, 2015. 93(8–9): p. 511–5. [PubMed] [Google Scholar]
- 133.Etzioni A., Ben-Barak A., Peron S., Durandy A., Ataxia-telangiectasia in twins presenting as autosomal recessive hyper-immunoglobulin M syndrome. Israel Medical Association Journal: Imaj, 2007. 9(5): p. 406–7. [PubMed] [Google Scholar]
- 134.Kalmarzi R.N., Aghamohammadi A., Movahedi M., Tavakol M., Darabi B., Rezaei N., et al., Ataxia-telangiectasia presenting as hyper-immunoglobulin M syndrome. Allergy, 2012. 67: p. 274–275. [Google Scholar]
- 135.Perreault S., Bernard G., Lortie A., Le Deist F., Decaluwe H., Ataxia-telangiectasia presenting with a novel immunodeficiency. Pediatric Neurology, 2012. 46(5): p. 322–4. doi: 10.1016/j.pediatrneurol.2012.02.027 [DOI] [PubMed] [Google Scholar]
- 136.Schwartzman J.S., Sole D., Naspitz C. K., Ataxia-telangiectasia: a clinical and laboratory review study of 14 cases. Allergologia et Immunopathologia, 1990. 18(2): p. 105–11. [PubMed] [Google Scholar]
- 137.Chaouki S., Benjelloun Dakhama B. S., Alaoui K., Arqam L., Atmani S., Bouharrou A., et al., Ataxia-telangiectasia: Case reports and literature review. Journal de Pediatrie et de Puericulture, 2008. 21(2): p. 98–101. [Google Scholar]
- 138.Alterman N., Fattal-Valevski A., Moyal L., Crawford T. O., Lederman H. M., Ziv Y., et al., Ataxia-telangiectasia: mild neurological presentation despite null ATM mutation and severe cellular phenotype. American Journal of Medical Genetics. Part A, 2007. 143A(16): p. 1827–34. doi: 10.1002/ajmg.a.31853 [DOI] [PubMed] [Google Scholar]
- 139.Larnaout A., Belal S., Ben Hamida C., Ben Hamida M., Hentati F., Atypical ataxia telangiectasia with early childhood lower motor neuron degeneration: a clinicopathological observation in three siblings. Journal of Neurology, 1998. 245(4): p. 231–5. doi: 10.1007/s004150050210 [DOI] [PubMed] [Google Scholar]
- 140.Afifi P.O., Elsanadiky H. H., Audiological findings in children with ataxia-telangiectasia (A-T) syndrome. International Journal of Pediatric Otorhinolaryngology, 2017. 92: p. 94–98. doi: 10.1016/j.ijporl.2016.11.012 [DOI] [PubMed] [Google Scholar]
- 141.Al-Baradie R., Chronic childhood ataxia: ataxia-telangiectasia. Neurosciences, 2010. 15(4): p. 296–7. [PubMed] [Google Scholar]
- 142.Matos J., Ornellas L., Carvalho B., Clinical features of patients with ataxia-telangiectasia at reference center in Sao Paulo, Brazil. World Allergy Organization Journal, 2012. Conference: p. 22nd World Allergy Congress. Cancun Mexico. Conference Publication: (var.pagings). 5 (SUPPL. 2) (pp S189–S190). [Google Scholar]
- 143.Mahadevappa M., Santhosh D. V., Netravathi M., Ravi Y., Pal P. K., Clinical profile of hundred patients with ataxia telangiectasia from India. Parkinsonism and Related Disorders, 2016. Conference: p. 21st World Congress on Parkinson’s Disease and Related Disorders. Milan Italy. Conference Publication: (var.pagings). 22 (SUPPL. 2) (pp e153–e154). [Google Scholar]
- 144.Ehlayel M.S., Elsaid M. F., Shami R., Salem K., Abdulbari Bener A., Clinico-radiological correlation in children with ataxia telangiectasia in Qatar. Allergy: European Journal of Allergy and Clinical Immunology, 2015. Conference: p. 34th Congress of the European Academy of Allergy and Clinical Immunology. Barcelona Spain. Conference Publication: (var.pagings). 70 (SUPPL. 101) (pp 215). [Google Scholar]
- 145.Assencioferreira V.J., Bancovsky I., Diament A. J., Gherpelli J. L. D., Moreira F. A., Computed-Tomography in Ataxia-Telangiectasia. Journal of Computer Assisted Tomography, 1981. 5(5): p. 660–661. doi: 10.1097/00004728-198110000-00010 [DOI] [PubMed] [Google Scholar]
- 146.Rezaei N., Pourpak Z., Aghamohammadi A., Farhoudi A., Movahedi M., Gharagozlou M., et al., Consanguinity in primary immunodeficiency disorders; the report from Iranian Primary Immunodeficiency Registry. American Journal of Reproductive Immunology, 2006. 56(2): p. 145–51. doi: 10.1111/j.1600-0897.2006.00409.x [DOI] [PubMed] [Google Scholar]
- 147.Coskun M., Aydingoz U., Tacal T., Ariyurek M., Demirkazik F., Oguzkurt L., CT and MR imaging of splenic leiomyoma in a child with ataxia telangiectasia. Pediatric Radiology, 1995. 25(1): p. 45–7. doi: 10.1007/BF02020844 [DOI] [PubMed] [Google Scholar]
- 148.Joshi R.K., Al Asiri R. H., Halekm A., Abanmi A., Patel C. K., Cutaneous granuloma with ataxia telangiectasia—a case report and review of literature. Clinical and Experimental Dermatology, 1993. 18(5): p. 458–561. doi: 10.1111/j.1365-2230.1993.tb02251.x [DOI] [PubMed] [Google Scholar]
- 149.Erman B., Demirtas D., Bildik H. N., Cagdas-Ayvaz D., Sanal O., Tezcan I., Defective pneumococcal antibody response in patients with recurrent respiratory tract infections. Turkish Journal of Pediatrics, 2017. 59(5): p. 555–560. doi: 10.24953/turkjped.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 150.Shafiei A.E., MA, Delay diagnosis of ataxia-telangiectasia in a 13-year-old girl presenting as Cerebral Palsy and Hodgkin lymphoma. Allergy: European Journal of Allergy and Clinical Immunology, 2019. 73(Supplement 105): p. 461. [Google Scholar]
- 151.Das S.D., S; Thomas M; Yoganathan S; Srivastava V; Cleave AS; Barney A, A descriptive study with molecular and cytogenetic analysis in patients of ataxia telangiectasia(AT) from the Indian subcontinent. International Parkinson and Movement Disorder Society, 2019. [Google Scholar]
- 152.Katafuchi Y., Matsuishi T., Ishihara O., Terasawa K., Okudera T., Ejima Y., Diagnosis of Ataxia-Telangiectasia—Computed-Tomography and X-Ray-Sensitivity. Brain & Development, 1985. 7(2): p. 161–161. [Google Scholar]
- 153.Shabestari M.S., Maljaei S. H., Baradaran R., Barzegar M., Hashemi F., Mesri A., Rezaei N., Distribution of primary immunodeficiency diseases in the Turk ethnic group, living in the northwestern Iran. Journal of Clinical Immunology, 2007. 27(5): p. 510–6. doi: 10.1007/s10875-007-9101-3 [DOI] [PubMed] [Google Scholar]
- 154.Kraus M., Lev A., Simon A. J., Levran I., Nissenkorn A., Levi Y. B., et al., Disturbed B and T cell homeostasis and neogenesis in patients with ataxia telangiectasia. Journal of Clinical Immunology, 2014. 34(5): p. 561–72. doi: 10.1007/s10875-014-0044-1 [DOI] [PubMed] [Google Scholar]
- 155.Saemundsen A.K., Berkel A. I., Henle W., Henle G., Anvret M., Sanal O., et al., Epstein-Barr-virus-carrying lymphoma in a patient with ataxia-telangiectasia. British Medical Journal Clinical Research Ed., 1981. 282(6262): p. 425–7. doi: 10.1136/bmj.282.6262.425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Gathmann B., et al., The European internet-based patient and research database for primary immunodeficiencies: Update 2011. Clinical and Experimental Immunology, 2012. 167(3): p. 479–491. doi: 10.1111/j.1365-2249.2011.04542.x [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 157.Bazregari S., Azizi G., Tavakol M., Asgardoon M. H., Kiaee F., Tavakolinia N., et al., Evaluation of infectious and non-infectious complications in patients with primary immunodeficiency. Central European Journal of Immunology, 2017. 42(4): p. 336–341. doi: 10.5114/ceji.2017.72825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Nasrullayeva G., Mammadova V., Family case of ataxiatelangiectasiya. Journal of Clinical Immunology, 2012. Conference: p. 15th Biennial Meeting of the European Society for Immunodeficiency, ESID 2012. Florence Italy. Conference Publication: (var.pagings). 32 (SUPPL. 1) (pp S398–S399). [DOI] [PubMed] [Google Scholar]
- 159.Hernandez D., McConville C. M., Stacey M., Woods C. G., Brown M. M., Shutt P., et al., A family showing no evidence of linkage between the ataxia telangiectasia gene and chromosome 11q22-23. Journal of Medical Genetics, 1993. 30(2): p. 135–40. doi: 10.1136/jmg.30.2.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ghosh S., Schuster F. R., Binder V., Niehues T., Baldus S. E., Seiffert P., et al., Fatal outcome despite full lympho-hematopoietic reconstitution after allogeneic stem cell transplantation in atypical ataxia telangiectasia. Journal of Clinical Immunology, 2012. 32(3): p. 438–40. doi: 10.1007/s10875-012-9654-7 [DOI] [PubMed] [Google Scholar]
- 161.Vilozni D., Berkun Y., Levi Y., Weiss B., Jacobson J. M., Efrati O. , The feasibility and validity of forced spirometry in ataxia telangiectasia. Pediatric Pulmonology, 2010. 45(10): p. 1030–6. doi: 10.1002/ppul.21291 [DOI] [PubMed] [Google Scholar]
- 162.Bousfiha A.A., et al., First report on the Moroccan registry of primary immunodeficiencies: 15 years of experience (1998–2012). Journal of Clinical Immunology, 2014. 34(4): p. 459–68. doi: 10.1007/s10875-014-0005-8 [DOI] [PubMed] [Google Scholar]
- 163.Anonymous, The French national registry of primary immunodeficiency diseases. Clinical Immunology, 2010. 135(2): p. 264–272. doi: 10.1016/j.clim.2010.02.021 [DOI] [PubMed] [Google Scholar]
- 164.Rezaei N., Aghamohammadi A., Moin M., Pourpak Z., Movahedi M., Gharagozlou M., et al., Frequency and clinical manifestations of patients with primary immunodeficiency disorders in Iran: update from the Iranian Primary Immunodeficiency Registry. Journal of Clinical Immunology, 2006. 26(6): p. 519–32. doi: 10.1007/s10875-006-9047-x [DOI] [PubMed] [Google Scholar]
- 165.Senturk N., Hindioglu U., Sahin S., Gokoz A., Granulomatous skin lesions in a patient with ataxia telangiectasia. British Journal of Dermatology, 1998. 139(3): p. 543–4. [DOI] [PubMed] [Google Scholar]
- 166.Alsalamah M., Roifman C. M., Hemophagocytic lymphohistiocytosis associated with ataxia telangiectasia. LymphoSign Journal, 2017. 4(3): p. 113–116. [Google Scholar]
- 167.Chessa L., Antonozzi I., Fiorilli M., Arslanian A., Prudente S., Piombo G., et al., Histopathologic Findings in a Fetus with Prenatally Diagnosed Ataxia-Telangiectasia. American Journal of Human Genetics, 1993. 53(3): p. 1539–1539. [Google Scholar]
- 168.Nam N.J., Herzog R., Humoral and cell-mediated immunity in two brothers with ataxia-telangiectasia. Annals of Allergy Asthma & Immunology, 2008. 100(1): p. A50–A50. [Google Scholar]
- 169.de Laet C., Casimir G., Duchateau J., Vamos E., Devalck C., Sariban E., et al., [Leukemia lymphoma T-cell as first manifestation of ataxia-telangiectasia]. Archives de Pediatrie, 1996. 3(7): p. 681–4. doi: 10.1016/0929-693x(96)87089-8 [DOI] [PubMed] [Google Scholar]
- 170.Marshall C., Life through the eyes of a disabled person. Archives of Disease in Childhood, 2004. 89(9): p. 887. doi: 10.1136/adc.2003.046433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Seemanova E., Misovicova N., Schindler D. , Louis-Bar syndrome of ataxia telangiectasia in consanguinous family. Cesko Slovenska Pediatrie, 2006. 61(11): p. 666–668. [Google Scholar]
- 172.Nguyen K., Missirian C., Zattara H., Stoppa-Lyonnet D., Azulay J., A mild form of ataxia-telangiectasia without telangiectasia caused by a novel mutation in the ATM gene. Movement Disorders, 2006. 21: p. S408–S408. [Google Scholar]
- 173.Balta G., Patiroglu T., Gumruk F., Sanal O., Gurgey A., Altay C., Molecular characterization of a prototype family harboring two genomic instability disorders: Ataxia telangiectasia and fanconi anemia. Blood, 2007. 110(11): p. 501A–501A.17395779 [Google Scholar]
- 174.Jeddane L., Ailal F., Dubois-d’Enghien C., Abidi O., Benhsaien I., Kili A., et al., Molecular defects in Moroccan patients with ataxia-telangiectasia. NeuroMolecular Medicine, 2013. 15(2): p. 288–94. doi: 10.1007/s12017-013-8218-1 [DOI] [PubMed] [Google Scholar]
- 175.Micol R., Ben Slama L., Suarez F., Le Mignot L., Beaute J., Mahlaoui N., et al., Morbidity and mortality from ataxia-telangiectasia are associated with ATM genotype. Journal of Allergy & Clinical Immunology, 2011. 128(2): p. 382–9.e1. doi: 10.1155/2015/213928 [DOI] [PubMed] [Google Scholar]
- 176.Kupeli S., Neurofibromatosis type-1 in a patient with ataxia-telangiectasia. Journal of Cancer Research and Therapeutics, 1073. 13(6): p. 1073–1074. [DOI] [PubMed] [Google Scholar]
- 177.Mortaz E., Marashian S. M., Ghaffaripour H., Varahram M., Mehrian P., Dorudinia A., et al., A new ataxia-telangiectasia mutation in an 11-year-old female. Immunogenetics, 2017. 69(7): p. 415–419. doi: 10.1007/s00251-017-0983-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Fukao T., Tashita H., Teramoto T., Inoue R., Kaneko H., Komiyama K., et al., Novel exonic mutation (5319 G to A) resulting in two aberrantly spliced transcripts of the ATM gene in a Japanese patient with ataxia-telangiectasia. Human Mutation, 1998. Suppl 1: p. S223–5. [DOI] [PubMed] [Google Scholar]
- 179.Ates E.T., A; Soylemez MA; Geckinli BB; Ata P; Arman A; Guney AI , A novel intronic ATM gene mutation affecting splicing in a patient with Ataxia-Telangiectasia. European Journal of Human Genetics, 2019. [Google Scholar]
- 180.Landoure G., Mochel F., Meilleur K., Ly M., Sangare M., Bocoum N., et al., Novel mutation in the ATM gene in a Malian family with ataxia telangiectasia. Journal of Neurology, 2013. 260(1): p. 324–6. doi: 10.1007/s00415-012-6738-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Saeidi K.S.G., N ; Mansouri Nejad SE, A Novel Splice Site Mutation of the ATM Gene Associated with Ataxia Telangiectasia. Iranian Journla of Child Neurology, 2018. 12(4). [PMC free article] [PubMed] [Google Scholar]
- 182.Galal N., Meshaal S., Elhawary R., ElAziz D. A., Alkady R., Lotfy S., et al., Patterns of Primary Immunodeficiency Disorders Among a Highly Consanguineous Population: Cairo University Pediatric Hospital’s 5-Year Experience. Journal of Clinical Immunology, 2016. 36(7): p. 649–655. doi: 10.1007/s10875-016-0314-1 [DOI] [PubMed] [Google Scholar]
- 183.Angele S., Lauge A., Fernet M., Moullan N., Beauvais P., Couturier J., et al., Phenotypic cellular characterization of an ataxia telangiectasia patient carrying a causal homozygous missense mutation. Human Mutation, 2003. 21(2): p. 169–70. doi: 10.1002/humu.9107 [DOI] [PubMed] [Google Scholar]
- 184.Khumalo N.P., Joss D. V., Huson S. M., Burge S., Pigmentary anomalies in ataxia—telangiectasia: a clue to diagnosis and an example of twin spotting. British Journal of Dermatology, 2001. 144(2): p. 369–71. [DOI] [PubMed] [Google Scholar]
- 185.Sheikhbahaei S., et al., Pregnancy, child bearing and prevention of giving birth to the affected children in patients with primary immunodeficiency disease; a case-series. BMC Pregnancy Childbirth, 2018. 18(1): p. 299. doi: 10.1186/s12884-018-1927-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Sridharan R., Radhakrishnan K., Ashok P. P., Mousa M. E., Prevalence and pattern of spinocerebellar degenerations in northeastern Libya. Brain, 1985. 108(Pt 4): p. 831–43. doi: 10.1093/brain/108.4.831 [DOI] [PubMed] [Google Scholar]
- 187.Reda S.M., Afifi H. M., Amine M. M., Primary immunodeficiency diseases in Egyptian children: A single-center study. Journal of Clinical Immunology, 2009. 29(3): p. 343–351. doi: 10.1007/s10875-008-9260-x [DOI] [PubMed] [Google Scholar]
- 188.Al-Saud B., et al., Primary Immunodeficiency Diseases in Saudi Arabia: a Tertiary Care Hospital Experience over a Period of Three Years (2010–2013). Journal of Clinical Immunology, 2015. 35(7): p. 651–660. doi: 10.1007/s10875-015-0197-6 [DOI] [PubMed] [Google Scholar]
- 189.Aghamohammadi A., Moein M., Farhoudi A., Pourpak Z., Rezaei N., Abolmaali K., et al., Primary immunodeficiency in Iran: first report of the National Registry of PID in Children and Adults. Journal of Clinical Immunology, 2002. 22(6): p. 375–80. doi: 10.1023/a:1020660416865 [DOI] [PubMed] [Google Scholar]
- 190.Ruggieri M., Arcidiacono G., Tine A., Di Mauro C., Pavone L., Pulmonary valve stenosis in a patient with ataxia telangiectasia. European Heart Journal, 1996. 17(6): p. 968. [DOI] [PubMed] [Google Scholar]
- 191.Porcedda P., Turinetto V., Brusco A., Cavalieri S., Lantelme E., Orlando L., et al., A rapid flow cytometry test based on histone H2AX phosphorylation for the sensitive and specific diagnosis of ataxia telangiectasia. Cytometry Part A: The Journal of the International Society for Analytical Cytology, 2008. 73(6): p. 508–16. doi: 10.1002/cyto.a.20566 [DOI] [PubMed] [Google Scholar]
- 192.Mancebo E., Bernardo I., Castro M. J., Fernandez-Martinez F. J., Barreiro E., De-Pablos P., et al., Rapid molecular prenatal diagnosis of ataxia-telangiectasia by direct mutational analysis. Prenatal Diagnosis, 2007. 27(9): p. 861–4. doi: 10.1002/pd.1787 [DOI] [PubMed] [Google Scholar]
- 193.Nagasravani J., Chacham S., Narayan Reddy U., Narsing Rao J., Rao S. P., Mahmood A., A rare case of ataxia telangiectasia in a 9-year-old female child. Pediatric Neurology, 2014. 51(4): p. 583–4. doi: 10.1016/j.pediatrneurol.2014.06.022 [DOI] [PubMed] [Google Scholar]
- 194.Patiroglu T., Murataldi S., Ozkul Y., Koklu E., Report of a family with Fanconi anemia and ataxia-telangiectasia. Turkish Journal of Haematology, 2004. 21(1): p. 33–37. [PubMed] [Google Scholar]
- 195.Berkun Y., Vilozni D., Levi Y., Borik S., Waldman D., Somech R., et al., Reversible airway obstruction in children with ataxia telangiectasia. Pediatric Pulmonology, 2010. 45(3): p. 230–5. doi: 10.1002/ppul.21095 [DOI] [PubMed] [Google Scholar]
- 196.Ehlayel M., de Beaucoudrey L., Fike F., Nahas S. A., Feinberg J., Casanova J. L., et al., Simultaneous presentation of 2 rare hereditary immunodeficiencies: IL-12 receptor beta1 deficiency and ataxia-telangiectasia. Journal of Allergy & Clinical Immunology, 2008. 122(6): p. 1217–9. doi: 10.1155/2015/213928 [DOI] [PubMed] [Google Scholar]
- 197.Adeli M., Hendaus M., Nisar S., Skin ulcers leading to residual hypo pigmented lesions with failure to thrive in ataxia telangiectasia case: A case report. Journal of Clinical Immunology, 2018. Conference: p. 2018 CIS Annual Meeting: Immune Deficiency and Dysregulation North American Conference. Canada. 38 (3) (pp 405). [Google Scholar]
- 198.Yareeda S., Rupam B., Rukmini M., Ak M., Jabeen S. A. , The spectrum of clinical profile of patients with ataxia telengiectasia: A case series from nims. Annals of Indian Academy of Neurology, 2014. Conference: p. 22nd Annual Conference of the Indian Academy of Neurology, IANCON 2014. Chandigarh India. Conference Publication: (var.pagings). 17 (SUPPL. 2) (pp S173). [Google Scholar]
- 199.De Silva N.R., Gunawardena S., Rathnayake D., Wickramasingha G. D., Spectrum of primary immunodeficiency disorders in Sri Lanka. Allergy, Asthma and Clinical Immunology, 2013. 9(1). doi: 10.1586/eci.12.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Berkel A.I., Ersoy F., Epstein L. B., Spitler L. E., Transfer factor therapy in ataxia—telangiectasia. Clinical & Experimental Immunology, 1977. 29(3): p. 376–84. [PMC free article] [PubMed] [Google Scholar]
- 201.Ersoy F., Berkel A. I., Sanal O., Oktay H., Twenty-year follow-up of 160 patients with ataxia-telangiectasia. Turkish Journal of Pediatrics, 1991. 33(4): p. 205–15. [PubMed] [Google Scholar]
- 202.Unsteady gait—Ataxia-telangiectasia. Postgraduate Medical Journal, 2006. 82(967). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Meyts I., Weemaes C., De Wolf-Peeters C., Proesmans M., Renard M., Uyttebroeck A., et al., Unusual and severe disease course in a child with ataxia-telangiectasia. Pediatric Allergy & Immunology, 2003. 14(4): p. 330–3. [DOI] [PubMed] [Google Scholar]
- 204.Claret Teruel G., et al., Variability of immunodeficiency associated with ataxia telangiectasia and clinical evolution in 12 affected patients. Pediatric Allergy & Immunology, 2005. 16(7): p. 615–8. doi: 10.1111/j.1399-3038.2005.00323.x [DOI] [PubMed] [Google Scholar]
- 205.Amirifar P., et al., The spectrum of ATM gene mutations in Iranian patients with ataxia-telangiectasia. Pediatr Allergy Immunol, 2021. 32(6): p. 1316–1326. doi: 10.1111/pai.13461 [DOI] [PubMed] [Google Scholar]
- 206.Arani M.H., et al., Clinical complications and their management in a child with ataxia-telangiectasia (A-T): A case report study. Clinical Case Reports, 2021. 9(1): p. 556–559. doi: 10.1002/ccr3.3581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Asmari W.N., et al., Novel Genetic Variant of Ataxia Telangiectasia Presenting with Necrotising Pneumonia and Bronchopleural Fistulae at the Age of 4 Years. J Coll Physicians Surg Pak, 2020. 30(10): p. 1102–1104. doi: 10.29271/jcpsp.2020.10.1102 [DOI] [PubMed] [Google Scholar]
- 208.Cao J., et al., Identifying ataxia-telangiectasia in cancer patients: Novel insights from an interesting case and review of literature. Clin Case Rep, 2021. 9(2): p. 995–1009. doi: 10.1002/ccr3.3543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Cekic S., et al., The evaluation of malignancies in Turkish primary immunodeficiency patients; a multicenter study. Pediatr Allergy Immunol, 2020. 31(5): p. 528–536. doi: 10.1111/pai.13231 [DOI] [PubMed] [Google Scholar]
- 210.Dewang S., et al., Cutaneous granulomas in a child with Ataxia telangiectasia—A rare association. Journal of Pakistan Association of Dermatologists, 2021. 30(3): p. 511–515. [Google Scholar]
- 211.Haskologlu Z.S., et al., Does the hyper igm phenotype affect prognosis in ataxia telangiectasia? Asthma Allergy Immunology, 2020. 18(1): p. 38–46. [Google Scholar]
- 212.Lee H.Y., et al., Compound heterozygous variants including a novel copy number variation in a child with atypical ataxia-telangiectasia: a case report. BMC Med Genomics, 2021. 14(1): p. 204. doi: 10.1186/s12920-021-01053-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Mahadevappa M., et al., A clinical profile of 100 patients with ataxia telangiectasia seen at a tertiary care center. Annals of Movement Disorders, 2020. 3(1): p. 33–38. [Google Scholar]
- 214.Marquez W.B., L ; Jaramillo L , Ataxia Telangiectasia and Common Variable Immunodeficiency with B-cell Lymphoma in Adolescent. Journal of Clinical Immunology, 2019. [Google Scholar]
- 215.Mathew M.G., Management of a pediatric patient with ataxia telangiectasia: Report of a rare case in which diagnostic radiographs are contraindicated. J Family Med Prim Care, 2020. 9(2): p. 1199–1201. doi: 10.4103/jfmpc.jfmpc_1095_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Perez Maturo J., et al., Novel Variants in ATM Causing Mild Ataxia-Telangiectasia: From Benchside to Bedside and Back Again. Mov Disord Clin Pract, 2020. 7(6): p. 727–729. doi: 10.1002/mdc3.13013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Scott O., et al., An atypical presentation of ataxia telangiectasia in a school-aged boy secondary to an intronic mutation. Lymphosign Journal-the Journal of Inherited Immune Disorders, 2020. 7(2): p. 57–60. [Google Scholar]
- 218.Shad T.M., et al., Variable Abnormalities in T and B Cell Subsets in Ataxia Telangiectasia. Journal of Clinical Immunology, 2021. 41(1): p. 76–88. doi: 10.1007/s10875-020-00881-9 [DOI] [PubMed] [Google Scholar]
- 219.Szczawińska-Popłonyk A., Ossowska L., and Jończyk-Potoczna K., Granulomatous Liver Disease in Ataxia-Telangiectasia With the Hyper-IgM Phenotype: A Case Report. Front Pediatr, 2020. 8: p. 570330. doi: 10.3389/fped.2020.570330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Tomacinschii C., et al., ABCL-311: The Burden of Non-Hodgkin Lymphoma Developed in an Ataxia Telangiectasia Child. Clinical Lymphoma, Myeloma and Leukemia, 2020. 20(Supplement 1): p. S272–S273. [Google Scholar]
- 221.Villagaray-Pacheco N., Franco-Bustamante K., and Cordova-Calderon W., 8-year experience with ataxia telangiectasia: A series of 7 cases. Romanian Journal of Neurology/ Revista Romana de Neurologie, 2021. 20(2): p. 200–203. [Google Scholar]
- 222.Nowak-Wegrzyn A.H., Lederman H. M., A 7-year-old girl with cerebral palsy and multiple warts. Annals of Allergy, Asthma and Immunology , 1998. 81(3): p. 195–201. doi: 10.1016/S1081-1206(10)62812-8 [DOI] [PubMed] [Google Scholar]
- 223.Datta V., Chaturvedi P., Ataxia telangiectasia. Indian Pediatrics, 1999. 36(12): p. 1278. [PubMed] [Google Scholar]
- 224.Tattersall R., Toghill P. J., Ataxia telangiectasia. Proceedings of the Royal Society of Medicine, 1970. 63(5): p. 453. [PMC free article] [PubMed] [Google Scholar]
- 225.Wong V., Yu Y. L., Chan-Lui W. Y., Woo E., Yeung C. Y., Ataxia telangiectasia in Chinese children. A clinical and electrophysiological study. Clinical Neurology & Neurosurgery, 1987. 89(3): p. 137–44. doi: 10.1016/s0303-8467(87)80045-8 [DOI] [PubMed] [Google Scholar]
- 226.Rondon-Melo S., de Almeida I. J., Andrade C. R. F., Sassi F. C., Molini-Avejonas D. R., Ataxia Telangiectasia in Siblings: Oral Motor and Swallowing Characterization. The American Journal of Case Reports, 2017. 18: p. 783–789. doi: 10.12659/ajcr.903592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Charlesworth G., Mohire M. D., Schneider S. A., Stamelou M., Wood N. W., Bhatia K. P., Ataxia telangiectasia presenting as dopa-responsive cervical dystonia. Neurology, 2013. 81(13): p. 1148–51. doi: 10.1212/WNL.0b013e3182a55fa2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Doshi A., Ryu J., Thornburg C. D., Hershey D., Cherry R., Milligan K., et al., Ataxia telangiectasia presenting as hyper IgM syndrome without neurologic signs. Annals of Allergy, Asthma, & Immunology, 2016. 117(3): p. 221–6. [DOI] [PubMed] [Google Scholar]
- 229.Rao S.R., Iyer R. S., Gladstone B., Advani S. H., Ataxia telangiectasia with acute lymphoblastic leukemia. Indian Pediatrics, 1993. 30(2): p. 257–61. [PubMed] [Google Scholar]
- 230.George S.M., Mathews M. C., Ataxia telangiectasia: Case report from a rural hospital in Nepal and current management recommendation. Journal of Nepal Paediatric Society, 2014. 34(2): p. 138–140. [Google Scholar]
- 231.Dunn H.G., Meuwissen H., Livingstone C. S., Pump K. K., Ataxia-Telangiectasia. Canadian Medical Association Journal, 1964. 91: p. 1106–18. [PMC free article] [PubMed] [Google Scholar]
- 232.Smeby B., Ataxia-Telangiectasia. Acta Paediatrica Scandinavica, 1966. 55(2): p. 239–&. [Google Scholar]
- 233.Leuzzi V., D’Agnano D., Menotta M., Caputi C., Chessa L., Magnani M., Ataxia-telangiectasia A new remitting form with a peculiar transcriptome signature. Neurology-Genetics, 2018. 4(2). doi: 10.1212/NXG.0000000000000228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Siekert R.G., Keith H. M., Dion F. R., Ataxia-Telangiectasia in Children. Proceedings of the Staff Meetings of the Mayo Clinic, 1959. 34(25): p. 581–587. [PubMed] [Google Scholar]
- 235.Fukao T., Song X. Q., Yoshida T., Tashita H., Kaneko H., Teramoto T., et al., Ataxia-telangiectasia in the Japanese population: identification of R1917X, W2491R, R2909G, IVS33+2T—>A, and 7883del5, the latter two being relatively common mutations. Human Mutation, 1998. 12(5): p. 338–43. doi: [DOI] [PubMed] [Google Scholar]
- 236.Navratil M., Duranovic V., Nogalo B., Svigir A., Dumbovic Dubravcic I., Turkalj M., Ataxia-Telangiectasia Presenting as Cerebral Palsy and Recurrent Wheezing: A Case Report. The American Journal of Case Reports, 2015. 16: p. 631–6. doi: 10.12659/AJCR.893995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Gimeno A., Liano H., Kreisler M., Ataxia-telangiectasia with absence of IgG. Journal of the Neurological Sciences, 1969. 8(3): p. 545–54. doi: 10.1016/0022-510x(69)90012-4 [DOI] [PubMed] [Google Scholar]
- 238.Datta H., Datta S., Panja S., Ataxica telengiectasia (Louis-Bar syndrome). Journal of the Indian Medical Association, 2001. 99(2): p. 106–7. [PubMed] [Google Scholar]
- 239.Aygun F.D., Nepesov S., Cokugras H., Camcioglu Y., Bladder Wall Telangiectasia in a Patient with Ataxia-Telangiectasia and How to Manage? Case Reports in Pediatrics, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Shimoda K., Mimaki M., Fujino S., Takeuchi M., Hino R., Uozaki H., et al., Brain edema with clasmatodendrosis complicating ataxia telangiectasia. Brain & Development, 2017. 39(7): p. 629–632. doi: 10.1016/j.braindev.2017.02.007 [DOI] [PubMed] [Google Scholar]
- 241.Greemberg R., Herzog R., A call for an early clinical consideration for ataxia-telangiectasia in infants with low TREC and combined immunodeficiency. Journal of Allergy and Clinical Immunology, 2016. Conference: p. 2016 Annual Meeting of the American Academy of Allergy, Asthma and Immunology, AAAAI 2016. Los Angeles, CA United States. Conference Publication: (var.pagings). 137 (2 SUPPL. 1) (pp AB216). [Google Scholar]
- 242.Sourander P., Bonnevier J. O., Olsson Y., A case of ataxia-telangiectasia with lesions in the spinal cord. Acta Neurologica Scandinavica, 1966. 42(3): p. 354–66. doi: 10.1111/j.1600-0404.1966.tb01187.x [DOI] [PubMed] [Google Scholar]
- 243.Monafo V., Fierro C., Fiocchi S., Maghnie M., Case Report: Ataxia telangiectasia with hyper IgM (ATM) with a complicated clinical course and a hepatic malignancy. Molecular Immunology, 1998. 35(11–12): p. 736–736. [Google Scholar]
- 244.Patino-Nino J.A., Pachajoa H., Perez P., Olaya M., Medina D., Case Report: Novel Mutations Detected in ATM Gene in a 10 Years Old Girl with Ataxia Telangiectasia in Colombia. Journal of Clinical Immunology, 2015. 35: p. S29–S30. [Google Scholar]
- 245.Lohmann E., Krüger S., Hauser A. K., Hanagasi H., Guven G., Erginel-Unaltuna N., et al., Clinical variability in ataxia–telangiectasia. Journal of Neurology, 2015. 262(7): p. 1724–1727. doi: 10.1007/s00415-015-7762-z [DOI] [PubMed] [Google Scholar]
- 246.Ram G., Heimall J., Cutaneous granulomas presenting as primary immune deficiency. Annals of Allergy, Asthma and Immunology, 2013. Conference: p. 2013 Annual Meeting of the American College of Allergy, Asthma and Immunology. Baltimore, MD United States. Conference Publication: (var.pagings). 111 (5 SUPPL. 1) (pp A95). [Google Scholar]
- 247.Folgori L., Scarselli A., Angelino G., Ferrari F., Antoccia A., Chessa L., et al., Cutaneous granulomatosis and combined immunodeficiency revealing Ataxia-Telangiectasia: a case report. Italian Journal of Pediatrics, 2010. 36: p. 29. doi: 10.1186/1824-7288-36-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Renedo M., Robledo M., Arranz E., Infantes F., Roman A., Garcia-Yebenes J., et al., Cytogenetic and molecular studies of siblings with ataxia telangiectasia followed for 7 years. Cancer Genetics & Cytogenetics, 1997. 95(2): p. 178–82. doi: 10.1016/s0165-4608(96)00256-7 [DOI] [PubMed] [Google Scholar]
- 249.Soresina A., Meini A., Lougaris V., Cattaneo G., Pellegrino S., Piane M., et al., Different clinical and immunological presentation of ataxia-telangiectasia within the same family. Neuropediatrics, 2008. 39(1): p. 43–5. doi: 10.1055/s-2008-1076736 [DOI] [PubMed] [Google Scholar]
- 250.van Belzen M.J., Hiel J. A., Weemaes C. M., Gabreels F. J., van Engelen B. G., Smeets D. F., et al., A double missense mutation in the ATM gene of a Dutch family with ataxia telangiectasia. Human Genetics, 1998. 102(2): p. 187–91. doi: 10.1007/s004390050675 [DOI] [PubMed] [Google Scholar]
- 251.Goyal V., Behari M., Dystonia as presenting manifestation of ataxia telangiectasia: a case report. Neurology India, 2002. 50(2): p. 187–9. [PubMed] [Google Scholar]
- 252.Pritchard J., Sandland M. R., Breatnach F. B., Pincott J. R., Cox R., Husband P., The effects of radiation therapy for Hodgkin’s disease in a child with ataxia telangiectasia: a clinical, biological and pathologic study. Cancer, 1982. 50(5): p. 877–86. doi: [DOI] [PubMed] [Google Scholar]
- 253.Woods C.G., Bundey S., Taylor A. M. R., A Genetic-Study of Classical Ataxia Telangiectasia. Journal of Medical Genetics, 1990. 27(10): p. 645–646. [Google Scholar]
- 254.Terplan K.L., Krauss R. F., Histopathologic brain changes in association with ataxia-telangiectasia. Neurology, 1969. 19(5): p. 446–54. doi: 10.1212/wnl.19.5.446 [DOI] [PubMed] [Google Scholar]
- 255.Yalcin B., Kutluk M. T., Sanal O., Akyuz C., Anadol D., Caglar M., et al., Hodgkin’s disease and ataxia telangiectasia with pulmonary cavities. Pediatric Pulmonology, 2002. 33(5): p. 399–403. doi: 10.1002/ppul.10057 [DOI] [PubMed] [Google Scholar]
- 256.An S.H., Li J. Y., Gao W. J., Zhang Y. L., Mo G. L., Tian L. Y., et al., A homozygous nonsense mutation of ATM gene in a Chinese family with five ataxia telangiectasia children: lesson for prenatal diagnosis. International Journal of Clinical and Experimental Pathology, 2016. 9(7): p. 7686–7690. [Google Scholar]
- 257.Huh H.J., Cho K. H., Lee J. E., Kwon M. J., Ki C. S., Lee P. H., Identification of ATM mutations in Korean siblings with ataxia-telangiectasia. Annals of Laboratory Medicine, 2013. 33(3): p. 217–20. doi: 10.3343/alm.2013.33.3.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Lahat N., Zelnik N., Froom P., Kinarty A., Etzioni A., Impaired autologous mixed lymphocyte reaction (AMLR) in patients with ataxia-telangiectasia and their family members. Clinical & Experimental Immunology, 1988. 74(1): p. 32–5. [PMC free article] [PubMed] [Google Scholar]
- 259.Tangsinmankong N., Wayne A. S., Howenstine M. S., Washington K. R., Langston C., Gatti R. A., et al., Lymphocytic interstitial pneumonitis, elevated IgM concentration, and hepatosplenomegaly in ataxia-telangiectasia. Journal of Pediatrics, 2001. 138(6): p. 939–41. [DOI] [PubMed] [Google Scholar]
- 260.Cantarutti N., Claps A., Angelino G., Chessa L., Callea F., El Hachem M., et al., Multi-drugs resistant acne rosacea in a child affected by Ataxia-Telangiectasia: successful treatment with Isotretinoin. Italian Journal of Pediatrics, 2015. 41: p. 23. doi: 10.1186/s13052-015-0125-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Termsarasab P., Yang A. C., Frucht S. J., Myoclonus in ataxia-telangiectasia. Tremor and Other Hyperkinetic Movements, 2015(pagination). doi: 10.7916/D88P5Z9X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Leuzzi V., Elli R., Antonelli A., Chessa L., Cardona F., Marcucci L., et al., Neurological and cytogenetic study in early-onset ataxia-telangiectasia patients. European Journal of Pediatrics, 1993. 152(7): p. 609–12. doi: 10.1007/BF01954092 [DOI] [PubMed] [Google Scholar]
- 263.Ruiz-Botero F., Rodriguez-Guerrero J. T., [New mutation in ATM gen in patient whith Ataxia Telangiectasia: Clinical case]. Revista Chilena de Pediatria, 2017. 88(4): p. 524–528. doi: 10.4067/S0370-41062017000400013 [DOI] [PubMed] [Google Scholar]
- 264.Mallott J., Kwan A., Church J., Gonzalez-Espinosa D., Lorey F., Tang L. F., et al., Newborn screening for SCID identifies patients with ataxia telangiectasia. Journal of Clinical Immunology, 2013. 33(3): p. 540–9. doi: 10.1007/s10875-012-9846-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Liu X.L., Wang T., Huang X. J., Zhou H. Y., Luan X. H., Shen J. Y., et al., Novel ATM mutations with ataxia-telangiectasia. Neuroscience Letters, 2016. 611: p. 112–5. doi: 10.1016/j.neulet.2015.11.036 [DOI] [PubMed] [Google Scholar]
- 266.Chen W.L., SD; Hu HF; Chen G; Zhu SC; Jia B; Sheng W; et al., Novel homozygous ataxia-telangiectasia (A-T) mutated gene mutation identified in a Chinese pedigree with A-T. Molecular Medicine Reports 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Garcia-Perez M.A., et al., Novel mutations and defective protein kinase C activation of T-lymphocytes in ataxia telangiectasia. Clinical & Experimental Immunology, 2001. 123(3): p. 472–80. doi: 10.1046/j.1365-2249.2001.01452.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Jacobs M., et al., The Objective Assessment of Abnormal Eye-Movements in Infants and Young-Children. Australian and New Zealand Journal of Ophthalmology, 1992. 20(3): p. 185–195. doi: 10.1111/j.1442-9071.1992.tb00938.x [DOI] [PubMed] [Google Scholar]
- 269.Nespoli L., Verri A., Taje S., Pellegrini F. P., Marinoni M., A precocious cerebellar ataxia and frequent fever episodes in a 16-month-old infant revealing ataxia-telangiectasia syndrome. Case Reports in Immunology, 2013(pagination). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Bakhtiar S., et al., Pre-emptive Allogeneic Hematopoietic Stem Cell Transplantation in Ataxia Telangiectasia. Front Immunol, 2018. 9: p. 2495. doi: 10.3389/fimmu.2018.02495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Cunlift P.N., Mann J. R., Cameron A. H., Roberts K. D., Ward H. N., Radiosensitivity in ataxia-telangiectasia. British Journal of Radiology, 1975. 48(569): p. 374–6. doi: 10.1259/0007-1285-48-569-374 [DOI] [PubMed] [Google Scholar]
- 272.Ashari N.S.M., Hamid W. Z. W. A., A rare case of ataxia telangiectasia in Malaysia. Bangladesh Journal of Medical Science, 2017. 16(1): p. 154–156. [Google Scholar]
- 273.Ray S., Sidhu R. J. S., Yadav R., Srinivas D., Pal P. K., Refractory status dystonicus in ataxia telangiectasia. Neurology India, 2017. 65(1): p. 169–172. doi: 10.4103/0028-3886.198206 [DOI] [PubMed] [Google Scholar]
- 274.Jain D., Natarajan S., Segmental pigmentary anomaly and ataxia telangiectasia. British Journal of Dermatology, 2015. Conference: p. 95th Annual Meeting of the British Association of Dermatologists. Manchester United Kingdom. Conference Publication: (var.pagings). 173 (SUPPL. 1) (pp 167). [Google Scholar]
- 275.Oxford J.M., Harnden D. G., Parrington J. M., Delhanty J. D. A., Specific Chromosome-Aberrations in Ataxia Telangiectasia. Journal of Medical Genetics, 1975. 12(3): p. 251–262. doi: 10.1136/jmg.12.3.251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Watanabe A., Hanazono H., Sogawa H., Takaya H., Stomach cancer of a 14-year-old boy with ataxia-telangiectasia. Tohoku Journal of Experimental Medicine, 1977. 121(2): p. 127–31. doi: 10.1620/tjem.121.127 [DOI] [PubMed] [Google Scholar]
- 277.Janic D., Dokmanovic L., Jovanovic N., Lazic J., T-cell acute lymphoblastic leukemia in a child with ataxia-telangiectasia: case report. Journal of Pediatric Hematology/Oncology, 2007. 29(10): p. 713–5. doi: 10.1097/MPH.0b013e31814d67f4 [DOI] [PubMed] [Google Scholar]
- 278.Nowak-Wegrzyn A., Crawford T. O., Winkelstein J. A., Carson K. A., Lederman H. M., Immunodeficiency and infections in ataxia-telangiectasia. Journal of Pediatrics, 2004. 144(4): p. 505–11. doi: 10.1016/j.jpeds.2003.12.046 [DOI] [PubMed] [Google Scholar]
- 279.McReynolds E.W., Dabbous M. K., Hanissian A. S., Duenas D., Kimbrell R., Abnormal collagen in ataxia telangiectasia. American Journal of Diseases of Children, 1976. 130(3): p. 305–7. doi: 10.1001/archpedi.1976.02120040083016 [DOI] [PubMed] [Google Scholar]
- 280.Lampert F., [Acute lymphoblastic leukemia in sibblings with progressive cerebellar ataxia (Louis-Bar syndrome)]. Deutsche Medizinische Wochenschrift, 1969. 94(5): p. 217–20. [DOI] [PubMed] [Google Scholar]
- 281.Cohen M.C., Sanchez-Marull R, Drut R, Aneuploid nucleomegaly of bronchial cells in ataxia-telangiectasia: cytologic recognition in bronchial brushings. Diagnostic Cytopathology, 1997. 17(6): p. 484–6. doi: [DOI] [PubMed] [Google Scholar]
- 282.Gershanik J.J., James V., Ataxia telangiectasia and growth failure. American Journal of Diseases of Children, 1971. 122(6): p. 538–40. doi: 10.1001/archpedi.1971.02110060108020 [DOI] [PubMed] [Google Scholar]
- 283.Hosal A.S., Yilmaz T., Ogretmenoglu O., Soylemezoglu F., Ataxia telangiectasia and mucoepidermoid carcinoma of the parotid gland: a case report. International Journal of Pediatric Otorhinolaryngology, 1996. 37(1): p. 79–84. doi: 10.1016/0165-5876(96)01373-0 [DOI] [PubMed] [Google Scholar]
- 284.Fireman P., Boesman M., and Gitlin D., Ataxia Telangiectasis. A Dysgammaglobulinaemia with Deficient Gamma-1-a (Beta-2-a)-Globulin. Lancet, 1964. 1(7344): p. 1193–5. doi: 10.1016/s0140-6736(64)91210-3 [DOI] [PubMed] [Google Scholar]
- 285.Ogawa T., Ataxia Telangiectasia in 2 Slibs—with an Immunological Study of Patients and Their Family. Developmental Medicine and Child Neurology, 1966. 8(5): p. 616–&. [Google Scholar]
- 286.Meshram C.M., Sawhney I. M., Prabhakar S., Chopra J. S, Ataxia telangiectasia in identical twins: unusual features. Journal of Neurology, 1986. 233(5): p. 304–5. doi: 10.1007/BF00314163 [DOI] [PubMed] [Google Scholar]
- 287.Woods C.G., Taylor A. M. R., Ataxia telangiectasis in the British Isles: The clinical and laboratory features of 70 affected individuals. Quarterly Journal of Medicine, 1992. 82(298): p. 169–179. [PubMed] [Google Scholar]
- 288.Shuster J., Hart Z., Stimson C. W., Brough A. J., Poulik M. D., Ataxia telangiectasia with cerebellar tumor. Pediatrics, 1966. 37(5): p. 776–86. [PubMed] [Google Scholar]
- 289.Zeft A., Jackson W. D., Daftary A., Lederman H., Bohnsack J, Ataxia Telangiectasia With Hyper IgM Immunophenotype, Chronic Hepatosplenomegaly, Lymphocytic Pneumonitis, and Enteropathy. Clinical Immunology, 2010. 135(2): p. 330–330. [Google Scholar]
- 290.Opeskin K., Waterston J., Nirenberg A., Hare W. S. C., Ataxia telangiectasia with long survival. Journal of Clinical Neuroscience, 1998. 5(4): p. 471–473. doi: 10.1016/s0967-5868(98)90295-8 [DOI] [PubMed] [Google Scholar]
- 291.Gutmann L., Lemli L., Ataxia-telangiectasia associated with hypogammaglobulinemia. Archives of Neurology, 1963. 8: p. 318–27. doi: 10.1001/archneur.1963.00460030102010 [DOI] [PubMed] [Google Scholar]
- 292.Penchaszadeh V.B., Ataxia-telangiectasia in brother and sister. Birth Defects: Original Article Series, 1971. 7(8): p. 324–5. [PubMed] [Google Scholar]
- 293.Smith L.L. and Conerly S.L., Ataxia-telangiectasia or Louis-Bar syndrome. Journal of the American Academy of Dermatology, 1985. 12(4): p. 681–96. doi: 10.1016/s0190-9622(85)70094-1 [DOI] [PubMed] [Google Scholar]
- 294.Noordzij J.G., Wulffraat N. M., Haraldsson A., Meyts I., van’t Veer L. J., Hogervorst F. B., et al., Ataxia-telangiectasia patients presenting with hyper-IgM syndrome. Archives of Disease in Childhood, 2009. 94(6): p. 448–9. doi: 10.1136/adc.2008.149351 [DOI] [PubMed] [Google Scholar]
- 295.Kumar L., Sehgal S., Ataxia-telangiectasia syndrome in 2 siblings. Indian Journal of Medical Research, 1975. 63(10): p. 1459–63. [PubMed] [Google Scholar]
- 296.Haerer A.F., Jackson J. F., Evers C. G., Ataxia-telangiectasia with gastric adenocarcinoma. JAMA, 1969. 210(10): p. 1884–7. [PubMed] [Google Scholar]
- 297.Brito J.C., da Silva J. A., da Nobrega P. V., [Ataxia-telangiectasia. Report of 4 cases]. Arquivos de Neuro-Psiquiatria, 1979. 37(2): p. 158–64. doi: 10.1590/s0004-282x1979000200006 [DOI] [PubMed] [Google Scholar]
- 298.Ozonoff M.B., Ataxia-telangiectasia: chronic pneumonia, sinusitis, and adenoidal hypoplasia. American Journal of Roentgenology, Radium Therapy & Nuclear Medicine, 1974. 120(2): p. 297–9. [DOI] [PubMed] [Google Scholar]
- 299.Farina L., Uggetti C., Ottolini A., Martelli A., Bergamaschi R., Sibilla L., et al., Ataxia-telangiectasia: MR and CT findings. Journal of Computer Assisted Tomography, 1994. 18(5): p. 724–7. [PubMed] [Google Scholar]
- 300.Curry C.J.R., Tsai J., Hutchison H. T., Painter R., Wara D., Gatti R., Atypical Ataxia Telangiectasia—an Expanding Spectrum of Disorders. Clinical Research, 1987. 35(1): p. A211–A211. [Google Scholar]
- 301.Levitt R., Pierre R. V., White W. L., Siekert R. G., Atypical lymphoid leukemia in ataxia telangiectasia. Blood, 1978. 52(5): p. 1003–11. [PubMed] [Google Scholar]
- 302.Ito M., Nakagawa A., Hirabayashi N., Asai J. , Bronchiolitis obliterans in ataxia-telangiectasia. Virchows Archiv, 1997. 430(2): p. 131–7. doi: 10.1007/BF01008034 [DOI] [PubMed] [Google Scholar]
- 303.Olsen J.H., Hahnemann J. M., Borresen-Dale A. L., Brondum-Nielsen K., Hammarstrom L., Kleinerman R., et al., Cancer in patients with ataxia-telangiectasia and in their relatives in the nordic countries. Journal of the National Cancer Institute, 2001. 93(2): p. 121–7. doi: 10.1093/jnci/93.2.121 [DOI] [PubMed] [Google Scholar]
- 304.Soukupova J., Pohlreich P., Seemanova E., Characterisation of ATM mutations in Slavic Ataxia telangiectasia patients. NeuroMolecular Medicine, 2011. 13(3): p. 204–11. doi: 10.1007/s12017-011-8152-z [DOI] [PubMed] [Google Scholar]
- 305.Scheres J.M., Hustinx T. W., Weemaes C. M., Chromosome 7 in ataxia-telangiectasia. Journal of Pediatrics, 1980. 97(3): p. 440–1. doi: 10.1016/s0022-3476(80)80200-9 [DOI] [PubMed] [Google Scholar]
- 306.Hatcher N.H., Pollara B., Hook E. B., Chromosome Breakage in 2 Siblings with Ataxia-Telangiectasia—Search for Intrafamilial Similarities. American Journal of Human Genetics, 1974. 26(6): p. A39–A39. [Google Scholar]
- 307.Zheng L., Liu X. L., Cao L., Clinical phenotype and genetic characteristics of ataxia-telangiectasia: four cases report. Chinese Journal of Contemporary Neurology and Neurosurgery, 2017. 17(7): p. 519–525. [Google Scholar]
- 308.Sherrington P.D., Fisch P., Taylor A. M. R., Rabbitts T. H., Clonal Evolution of Malignant and Nonmalignant T-Cells Carrying T(1414) and T(X14) in Patients with Ataxia-Telangiectasia. Oncogene, 1994. 9(8): p. 2377–2381. [PubMed] [Google Scholar]
- 309.Cohen L.E., Tanner D. J., Schaefer H. G., Levis W. R., Common and uncommon cutaneous findings in patients with ataxia-telangiectasia. Journal of the American Academy of Dermatology, 1984. 10(3): p. 431–8. doi: 10.1016/s0190-9622(84)80089-4 [DOI] [PubMed] [Google Scholar]
- 310.Mostofsky S.H., Green J. T., Meginley M., Christensen J. R., Woodruff-Pak, D. S., Conditioning in identical twins with ataxia-telangiectasia. Neurocase, 1999. 5(5): p. 425–433. [Google Scholar]
- 311.Petkovic I., Ligutic I., Dominis M., Loffler-Badzak D., M. Cepulic, Nakic M., Cytogenetic analysis in ataxia telangiectasia with malignant lymphoma. Cancer Genetics & Cytogenetics, 1992. 60(2): p. 158–63. doi: 10.1016/0165-4608(92)90009-w [DOI] [PubMed] [Google Scholar]
- 312.Alsaadi, Paluke M., Kumar K., Cytogenetic and Immunological Studies in Ataxia Telangiectasia. American Journal of Human Genetics, 1975. 27(6): p. A78–A78. [Google Scholar]
- 313.Waghray, Gascon G. G., Alsedairy S., Hannan M. A., Cytogenetic Investigations in 3 Cell-Types of a Saudi Family with Ataxia Telangiectasia. Human Genetics, 1991. 87(3): p. 285–289. doi: 10.1007/BF00200905 [DOI] [PubMed] [Google Scholar]
- 314.Cabana M.D., Winkelstein J. A., Christensen J. R., Lederman H. M., Crawford T. O., Delayed diagnosis of ataxia-telangiectasia. Annals of Neurology, 1997. 42(3): p. P42–P42. [Google Scholar]
- 315.Greenberger S., Berkun Y., Ben-Zeev B., Levi Y. B., Barziliai A., Nissenkorn A., Dermatologic manifestations of ataxia-telangiectasia syndrome. Journal of the American Academy of Dermatology, 2013. 68(6): p. 932–6. doi: 10.1016/j.jaad.2012.12.950 [DOI] [PubMed] [Google Scholar]
- 316.Jason J.M. and Gelfand E.W., Diagnostic considerations in ataxia-telangiectasia. Archives of Disease in Childhood, 1979. 54(9): p. 682–6. doi: 10.1136/adc.54.9.682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Neves Forte W.C., Santos De Menezes M. C., Loureiro Dionigi P. C., Fanuchi E. Bastos C. L. A., Different clinical and laboratory evolutions in ataxia-telangiectasia syndrome: Report of four cases. Allergologia et Immunopathologia, 2005. 33(4): p. 199–203. [DOI] [PubMed] [Google Scholar]
- 318.Tamai I., Okuyama M., Aoki T., Ochiai Y., [Disorders of lymphocyte maturation, helper T cells and anti T cell antibody in sisters with ataxia telangiectasia]. No to Hattatsu [Brain & Development], 1986. 18(3): p. 193–8. [PubMed] [Google Scholar]
- 319.Ben-Zvi A., Soffer D., Yatziv S., Disseminated Herpes simplex virus infection in ataxia-telangiectasia. Acta Paediatrica Scandinavica, 1978. 67(5): p. 667–70. doi: 10.1111/j.1651-2227.1978.tb17821.x [DOI] [PubMed] [Google Scholar]
- 320.Vilmer E., Lenoir G. M., Virelizier J. L., Griscelli C., Epstein-Barr serology in immunodeficiencies: an attempt to correlate with immune abnormalities in Wiskott-Aldrich and Chediak-Higashi syndromes and ataxia telangiectasia. Clinical & Experimental Immunology, 1984. 55(2): p. 249–56. [PMC free article] [PubMed] [Google Scholar]
- 321.Joncas J.H., Wills A., Reece E., Fox Z., Epstein-Barr virus antibodies in patients with ataxia-telangiectasia and other immunodeficiency diseases. Canadian Medical Association Journal, 1981. 125(8): p. 845–9. [PMC free article] [PubMed] [Google Scholar]
- 322.Pereira C.T.M., Carvalho B. C., Bichuetti-Silva D. C., Brunialti M. K. C., Ferreira N., Salomao R., Expression of CD40, CD40L and IgM production in patients with ataxiatelangiectasia. World Allergy Organization Journal, 2015. Conference: p. 3rd WAO International Scientific Conference, WISC 2014. Rio de Janeiro Brazil. Conference Publication: (var.pagings). 8 (SUPPL. 1) (no pagination). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Bar R.S., Levis W., Muggeo M., Roth J., Rechler M. M., Podskalny J. M., Extreme Insulin Resistance in Ataxia Telangiectasia—Defect in Affinity of Insulin Receptors. Clinical Research, 1977. 25(3): p. A290–A290. [DOI] [PubMed] [Google Scholar]
- 324.Hyams S.W., Reisner S. H., Neumann E., The eye signs in ataxia-telangiectasia. American Journal of Ophthalmology, 1966. 62(6): p. 1118–24. doi: 10.1016/0002-9394(66)92562-1 [DOI] [PubMed] [Google Scholar]
- 325.Pickup J.D., Pugh R. J., Familial Ataxia-Telangiectasia. Archives of Disease in Childhood, 1961. 36(187): p. 344–&. doi: 10.1136/adc.36.187.344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Degan P., et al., Glutathione levels in blood from ataxia telangiectasia patients suggest in vivo adaptive mechanisms to oxidative stress. Clinical Biochemistry, 2007. 40(9–10): p. 666–70. doi: 10.1016/j.clinbiochem.2007.03.013 [DOI] [PubMed] [Google Scholar]
- 327.Browne R., Ravenscroft J. C., McDermott E. M., Cliffe L., Glover M., Suri M., Granulomatous skin disease in ataxia-telangiectasia. British Journal of Dermatology, 2018. Conference: p. 32nd Annual Meeting of the British Society for Paediatric Dermatology. United Kingdom. 178 (2) (pp e149–e150). [Google Scholar]
- 328.Serizawa M., Sakamoto M., Hirabayashi K., Fujiwara Y., Atsumi T., [Histological and radiobiological study on adult cases with ataxia telangiectasia]. Rinsho Shinkeigaku—Clinical Neurology, 1994. 34(1): p. 38–42. [PubMed] [Google Scholar]
- 329.Wells J.V., Bleumers J.F., and Fudenberg H.H., Human anti-IgM iso-antibodies in subjects with selective IgA deficiency. Clinical & Experimental Immunology, 1972. 12(3): p. 305–13. [PMC free article] [PubMed] [Google Scholar]
- 330.Datta U., Sehgal S., Kumar L., Kaur K. J., Walia B. N., Chopra J. S., et al., Immune status in ataxia telangiectasia. Indian Journal of Medical Research, 1991. 94: p. 252–4. [PubMed] [Google Scholar]
- 331.Hanicki Z., Hanicka M., and Rembiesowa H., Immunologic aspects of ataxia-telangiectasia. International Archives of Allergy & Applied Immunology, 1967. 32(5): p. 436–52. doi: 10.1159/000229955 [DOI] [PubMed] [Google Scholar]
- 332.Eisen A.H., Karpati G., Laszlo T., Andermann F., Robb J. P., Bacal H. L., Immunologic Deficiency in Ataxia Telangiectasia. New England Journal of Medicine, 1965. 272: p. 18–22. [DOI] [PubMed] [Google Scholar]
- 333.Epstein W.L., Fudenberg H. H., Reed W. B., Boder E., Sedgwick R. P., Immunologic studies in ataxia-telangiectasia. I. Delayed hypersensitivity and serum immune globulin levels in probands and first-degree relatives. International Archives of Allergy & Applied Immunology, 1966. 30(1): p. 15–29. [PubMed] [Google Scholar]
- 334.Schultewissermann H., Gutjahr P., Zebisch P., Reitz M., Lemmel E. M., Immunological Investigations in 2 Brothers with Ataxia Telangiectasia Louis-Bar. European Journal of Pediatrics, 1976. 122(2): p. 93–102. doi: 10.1007/BF00466267 [DOI] [PubMed] [Google Scholar]
- 335.Hansen R.L., Marx J. J., Ptacek L. J., Roberts R. C., Immunological studies on an aberrant form of ataxia telangiectasia. American Journal of Diseases of Children, 1977. 131(5): p. 518–21. doi: 10.1001/archpedi.1977.02120180032004 [DOI] [PubMed] [Google Scholar]
- 336.Bordigoni P., Faure G., Bene M. C., Dardenne M., Bach J. F., Duheille J., et al., Improvement of cellular immunity and IgA production in immunodeficient children after treatment with synthetic serum thymic factor (FTS). Lancet, 1982. 2(8293): p. 293–7. doi: 10.1016/s0140-6736(82)90271-9 [DOI] [PubMed] [Google Scholar]
- 337.Suarez F., Mahlaoui N., Canioni D., Andriamanga C., Dubois d’Enghien C., Brousse N., et al., Incidence, presentation, and prognosis of malignancies in ataxia-telangiectasia: a report from the French national registry of primary immune deficiencies. Journal of Clinical Oncology, 2015. 33(2): p. 202–8. doi: 10.1200/JCO.2014.56.5101 [DOI] [PubMed] [Google Scholar]
- 338.Hiel J.A., Weemaes C. M., Smeets D. F., Van de Vlasakker C. J., Horstink M. W., Late-onset ataxia telangiectasia in two brothers presenting with juvenile resting tremor. Movement Disorders, 1994. 9(4): p. 460–2. doi: 10.1002/mds.870090415 [DOI] [PubMed] [Google Scholar]
- 339.Hecht F., Koler R. D., Rigas D. A., Dahnke G. S., Case M. P., Tisdale V., et al., Leukaemia and Lymphocytes in Ataxia-Telangiectasia. Lancet, 1966. 2(7474): p. 1193–&. [Google Scholar]
- 340.Ammann A.J., Good R. A., Bier D., Fudenberg H. H., Long-term plasma infusions in a patient with ataxia-telangiectasia and deficient IGA and IGE. Pediatrics, 1969. 44(5): p. 672–6. [PubMed] [Google Scholar]
- 341.Peterson R.D., Cooper M. D., Good R. A., Lymphoid tissue abnormalities associated with ataxia-telangiectasia. American Journal of Medicine, 1966. 41(3): p. 342–59. doi: 10.1016/0002-9343(66)90080-5 [DOI] [PubMed] [Google Scholar]
- 342.Cirillo E., Del Giudice E., Micheli R., Cappellari A. M., Soresina A., Dellepiane R. M., et al., Minimum effective betamethasone dosage on the neurological phenotype in patients with ataxia-telangiectasia: a multicenter observer-blind study. European Journal of Neurology, 2018. 25(6): p. 833–840. doi: 10.1111/ene.13606 [DOI] [PubMed] [Google Scholar]
- 343.Salman M.S., Chodirker B. N., Neuro-ophthalmological findings in children and adolescents with chronic ataxia. Neuro Ophthalmology, 2015. 39(3): p. 125–131. doi: 10.3109/01658107.2015.1016579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Schmidt D., [Oculomotor signs in cerebellar disease shown in ataxia telangiectasia (Louis Bar) (author’s transl)]. Klinische Monatsblatter fur Augenheilkunde, 1978. 173(3): p. 329–33. [PubMed] [Google Scholar]
- 345.Strich S.J., Pathological Findings in 3 Cases of Ataxia-Telangiectasia. Journal of Neurology Neurosurgery and Psychiatry, 1966. 29(6): p. 489–&. [Google Scholar]
- 346.Morio T., Takahashi N., Watanabe F., Honda F., Sato M., Takagi M., et al., Phenotypic variations between affected siblings with ataxia-telangiectasia: ataxia-telangiectasia in Japan. International Journal of Hematology, 2009. 90(4): p. 455–462. doi: 10.1007/s12185-009-0408-0 [DOI] [PubMed] [Google Scholar]
- 347.Kovacs K., Giannini C., Scheithauer B. W., Stefaneanu L., Lloyd R. V., Horvath E., Pituitary changes in ataxia-telangiectasia syndrome: An immunocytochemical, in situ hybridization, and DNA cytometric study of three cases. Endocrine Pathology, 1997. 8(3): p. 195–203. doi: 10.1007/BF02738786 [DOI] [PubMed] [Google Scholar]
- 348.Hellani A., et al., Pregnancy after preimplantation genetic diagnosis for Ataxia Telangiectasia. Molecular Human Reproduction, 2002. 8(8): p. 785–8. doi: 10.1093/molehr/8.8.785 [DOI] [PubMed] [Google Scholar]
- 349.Devaney R., Pasalodos S., Suri M., Bush A., Bhatt J., Presentation and diagnostic delay in ataxia telangiectasia (A-T). European Respiratory Journal, 2015. Conference: p. European Respiratory Society Annual Congress 2015. Amsterdam Netherlands. Conference Publication: (var.pagings). 46 (SUPPL. 59) (no pagination). [Google Scholar]
- 350.Bodensteiner J.B., Goldblum R. M., Goldman A. S., Progressive dystonia masking ataxia in ataxia-telangiectasia. Archives of Neurology, 1980. 37(7): p. 464–5. doi: 10.1001/archneur.1980.00500560094020 [DOI] [PubMed] [Google Scholar]
- 351.Hernanz-Hermosa J.M., Bueno-Marco C., Gonzalez-Herrada C., Casanova-Seuma J. M., Martin-Moro M., Villanueva-Osorio J., [Prolonged and severe photodermatitis, an early manifestation of ataxia telangiectasia]. Medicina Cutanea Ibero-Latino-Americana, 1987. 15(2): p. 119–22. [PubMed] [Google Scholar]
- 352.Levine C., Vrlenich L., Renal lymphoma in ataxia-telangiectasia: CT contribution. Journal of Computer Assisted Tomography, 1989. 13(3): p. 537–9. doi: 10.1097/00004728-198905000-00039 [DOI] [PubMed] [Google Scholar]
- 353.Aucouturier P., Bremard-Oury C., Griscelli C., Berthier M., Preud’homme J. L., Serum IgG subclass deficiency in ataxia-telangiectasia. Clinical & Experimental Immunology, 1987. 68(2): p. 392–6. [PMC free article] [PubMed] [Google Scholar]
- 354.Chen R.L., Wang P. J., Hsu Y. H., Chang P. Y., Fang J. S., Severe lung fibrosis after chemotherapy in a child with ataxia-telangiectasia. Journal of Pediatric Hematology/Oncology, 2002. 24(1): p. 77–9. doi: 10.1097/00043426-200201000-00021 [DOI] [PubMed] [Google Scholar]
- 355.Verma S., Sharma P. K., Sivanandan S., Rana N., Saini S., Lodha R., et al., Spectrum of primary immune deficiency at a tertiary care hospital. Indian Journal of Pediatrics, 2008. 75(2): p. 143–8. doi: 10.1007/s12098-008-0022-9 [DOI] [PubMed] [Google Scholar]
- 356.Uygungil B., Lederman H., A successful pregnancy and delivery in a patient with ataxia-telangiectasia. Journal of Clinical Immunology, 2013. Conference: p. 2013 Clinical Immunology Society, CIS Annual Meeting: Regulation and Dysregulation of Immunity. Miami, FL United States. Conference Publication: (var.pagings). 33 (3) (pp 688). [Google Scholar]
- 357.Bichuetti-Silva D.C., et al., Transitional B cells and CD21low in patients with ataxia-telangiectasia. World Allergy Organization Journal, 2015. Conference: p. 3rd WAO International Scientific Conference, WISC 2014. Rio de Janeiro Brazil. Conference Publication: (var.pagings). 8 (SUPPL. 1) (no pagination). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Cousineau A.J., Higgins J. V., Kaufman D., Unique Karyotypic Patterns in 3 Sibs with Ataxia Telangiectasia. American Journal of Human Genetics, 1981. 33(6): p. A101–A101. [Google Scholar]
- 359.Ours C., Cunningham A., Afify Z., Unique presentations of ataxia-telangiectasia in two brothers. Pediatric Blood and Cancer, 2018. Conference: p. 2018 American Society of Pediatric Hematology/Oncology, ASPHO 2018. United States. 65 (Supplement 1) (pp S21). [Google Scholar]
- 360.Cipe F., Dogu F., Yildiran A., Yuksek M., Pekacar T., Guriz H., et al., An unusual clinical presentation: invasive Candida non-albicans infections in ataxia telangiectasia. Journal of Investigational Allergology & Clinical Immunology, 2008. 18(6): p. 488–90. [PubMed] [Google Scholar]
- 361.Joncas J., et al., Unusual prevalence of Epstein-Barr virus early antigen (EBV-EA) antibodies in ataxia telangiectasia. Journal of Immunology, 1977. 119(5): p. 1857–9. [PubMed] [Google Scholar]
- 362.Gatti R.A., Nieberg R., Boder E., Uterine tumors in ataxia-telangiectasia. Gynecologic Oncology, 1989. 32(2): p. 257–60. doi: 10.1016/s0090-8258(89)80045-9 [DOI] [PubMed] [Google Scholar]
- 363.Asadollahi R., et al., Severe reaction to radiotherapy provoked by hypomorphic germline mutations in ATM (ataxia-telangiectasia mutated gene). Mol Genet Genomic Med, 2020. 8(10): p. e1409. doi: 10.1002/mgg3.1409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Bucher M., et al., Analysis of chromosomal aberrations and γH2A.X foci to identify radiation-sensitive ataxia-telangiectasia patients. Mutat Res Genet Toxicol Environ Mutagen, 2021. 861–862: p. 503301. doi: 10.1016/j.mrgentox.2020.503301 [DOI] [PubMed] [Google Scholar]
- 365.Cau A.C.A., et al., Case report: papillary thyroid carcinoma in two sisters with ataxia telangiectasia syndrome. Revista Argentina de Endocrinologia y Metabolismo, 2021. 58(SUPPL 1): p. 283. [Google Scholar]
- 366.Chakravorty S., et al., Expanding the genotype-phenotype correlation of childhood sensory polyneuropathy of genetic origin. Sci Rep, 2020. 10(1): p. 16184. doi: 10.1038/s41598-020-73219-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Ritchie A., et al., The importance of phenotypic information to guide genetic testing. Pathology, 2020. 52(Supplement 1): p. S27–S28. [Google Scholar]
- 368.Shalash A.S., et al., Evidence for pathogenicity of variant ATM Val1729Leu in a family with ataxia telangiectasia. Neurogenetics, 2021. 22(2): p. 143–147. doi: 10.1007/s10048-021-00639-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Suspitsin E., et al., ATM mutation spectrum in Russian children with ataxia-telangiectasia. Eur J Med Genet, 2020. 63(1): p. 103630. doi: 10.1016/j.ejmg.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 370.Bernstein R., Pinto M., Jenkins T., Ataxia telangiectasia with evolution of monosomy 14 and emergence of Hodgkin’s disease. Cancer Genetics & Cytogenetics, 1981. 4(1): p. 31–7. doi: 10.1016/0165-4608(81)90005-4 [DOI] [PubMed] [Google Scholar]
- 371.Ramirez Corria C.M., Proposal of a neurosurgical treatment for ataxia telangiectasia (Mme. Louis Bar syndrome). First results obtained. Revista Cubana de Pediatria, 1972. 44(4–5 6): p. 221–228. [Google Scholar]
- 372.Young R. R. A., K.F.M., H. W., Abnormalities of Serum Gamma-1-a Globulin and Ataxia Telangiectasia. 1964. [DOI] [PubMed] [Google Scholar]
- 373.Ussowicz M., et al., Allogeneic Stem Cell Transplantation after Fanconi Anemia Conditioning in Children with Ataxia-Telangiectasia Results in Stable T Cell Engraftment and Lack of Infections despite Mixed Chimerism. Biol Blood Marrow Transplant, 2018. 24(11): p. 2245–2249. doi: 10.1016/j.bbmt.2018.07.001 [DOI] [PubMed] [Google Scholar]
- 374.Hayakawa H., Kobayashi N., Yata J., [Ataxia-telangiectasia in Japan]. Arerugi—Japanese Journal of Allergology, 1984. 33(3): p. 182–93. [PubMed] [Google Scholar]
- 375.Jo K.M., Yang S. Y., Park J. H., Kim T. O., Jeong H. J., Heo C. M., et al., Childhood colon cancer in a patient with ataxia telangiectasia. Annals of Translational Medicine, 2016. 4(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Triki C., Feki I., Meziou M., Turki H., Zahaf A., Mhiri C., [Clinical, biological and genetic study of 24 patients with ataxia telangiectasia from southern Tunisia]. Revue Neurologique, 2000. 156(6–7): p. 634–7. [PubMed] [Google Scholar]
- 377.Kirkpatrick P., Riminton S., Primary immunodeficiency diseases in Australia and New Zealand. Journal of Clinical Immunology, 2007. 27(5): p. 517–524. doi: 10.1007/s10875-007-9105-z [DOI] [PubMed] [Google Scholar]
- 378.Martin-Nalda A., Soler-Palacin P., Espanol Boren T., Caragol Urgelles I., Diaz de Heredia Rubio C., Figueras Nadal C., [Spectrum of primary immunodeficiencies in a tertiary hospital over a period of 10 years]. Anales de Pediatria, 2011. 74(2): p. 74–83. doi: 10.1016/j.anpedi.2010.09.019 [DOI] [PubMed] [Google Scholar]
- 379.Listernick R., A 6-year-old girl with unsteady gait. Pediatric Annals, 2009. 38(8): p. 410–3. doi: 10.3928/00904481-20090723-03 [DOI] [PubMed] [Google Scholar]
- 380.Moynahan E.J., Ataxia Telangiectasia. Proceedings of the Royal Society of Medicine-London, 1963. 56(8): p. 727–728. [PMC free article] [PubMed] [Google Scholar]
- 381.Necpal J., et al., Ataxia Telangiectasia Gene Mutation in Isolated Segmental Dystonia Without Ataxia and Telangiectasia. Movement Disorders Clinical Practice, 2018. 5(1): p. 89–91. doi: 10.1002/mdc3.12564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Sakiyama Y., Takahashi Y., Tsuneta H., Matsumoto S., Ataxia telangiectasia with persistent Epstein-Barr virus infection and malignant lymphoma. Acta Paediatrica Japonica, 1984. 26(1): p. 51–55. [Google Scholar]
- 383.Gupta C., Tewari R., Natu S. M., Tondon P., Mehrotra R., Ataxia telangiectasia: Serological Presentation. Current Pediatric Research, 2012. 16(1): p. 15–18. [Google Scholar]
- 384.Miller R.C., Ataxia-Telangiectasia. Archives of Dermatology, 1968. 98(2): p. 207–&. [Google Scholar]
- 385.Massad M., Uthman S., Obeid S., Majjar F., Ataxia-telangiectasia and stomach cancer. American Journal of Gastroenterology, 1990. 85(5): p. 630–1. [PubMed] [Google Scholar]
- 386.Batista da Silva A., Antonio de Moraes A., Goncalves de Medeiros J. E., Pires F. A., Zerlotti Filho E., [Ataxia-telangiectasia syndrome]. Arquivos de Neuro-Psiquiatria, 1971. 29(2): p. 219–26. doi: 10.1590/s0004-282x1971000200011 [DOI] [PubMed] [Google Scholar]
- 387.Ye F., et al., Ataxia-telangiectasia with a novel ATM gene mutation and Burkitt leukemia: A case report. Mol Clin Oncol, 2018. 9(5): p. 493–498. doi: 10.3892/mco.2018.1721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Jeong H., et al., Ataxia-telangiectasia with novel splicing mutations in the ATM gene. Annals of Laboratory Medicine, 2014. 34(1): p. 80–4. doi: 10.3343/alm.2014.34.1.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Paula-Barbosa M.M., Ruela C., Tavares M. A., Pontes C., Saraiva A., Cruz C., Cerebellar cortex ultrastructure in ataxia-telangiectasia. Annals of Neurology, 1983. 13(3): p. 297–302. doi: 10.1002/ana.410130312 [DOI] [PubMed] [Google Scholar]
- 390.Zagami A.S., Colebatch H. J., Wakefield D., Chronic eosinophilic pneumonia in a patient with ataxia telangiectasia. Australian & New Zealand Journal of Medicine, 1987. 17(6): p. 592–5. [DOI] [PubMed] [Google Scholar]
- 391.Otabor I.A., Abdessalam S. F., Erdman S. H., Hammond S., Besner G. E., Gastric outlet obstruction due to adenocarcinoma in a patient with Ataxia-Telangiectasia syndrome: a case report and review of the literature. World Journal of Surgical Oncology, 2009. 7: p. 29. doi: 10.1186/1477-7819-7-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Rohatgi A., Pardasani V., Sharma S. K., Gupta A. K., Gurtoo A., Louis Bar syndrome. Journal of the Association of Physicians of India, 2003. 51: p. 286. [PubMed] [Google Scholar]
- 393.Brasseur B., Beauloye V., Chantrain C., Daumerie C., Vermylen C., Waignein F., et al., Papillary thyroid carcinoma in a 9-year-old girl with ataxia-telangiectasia. Pediatric Blood & Cancer, 2008. 50(5): p. 1058–60. [DOI] [PubMed] [Google Scholar]
- 394.Pump K.K., Dunn H. G., Meuwissen H., A Study of the Bronchial and Vascular Structures of a Lung: From a Case of Ataxia-Telangiectasia. Diseases of the Chest, 1965. 47: p. 473–86. doi: 10.1378/chest.47.5.473 [DOI] [PubMed] [Google Scholar]
- 395.Zhang L., et al., Trihexyphenidyl for treatment of dystonia in ataxia telangiectasia: a case report. Childs Nerv Syst, 2020. 36(4): p. 873–875. doi: 10.1007/s00381-019-04399-3 [DOI] [PubMed] [Google Scholar]
- 396.Worth P.F., Srinivasan V., Smith A., Last J. I., Wootton L. L., Biggs P. M., et al., Very mild presentation in adult with classical cellular phenotype of ataxia telangiectasia. Movement Disorders, 2013. 28(4): p. 524–8. doi: 10.1002/mds.25236 [DOI] [PubMed] [Google Scholar]
- 397.Li X.L. and Wang Y.L., Ataxia-telangiectasia complicated with Hodgkin’s lymphoma: A case report. World J Clin Cases, 2020. 8(11): p. 2387–2391. doi: 10.12998/wjcc.v8.i11.2387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Maturo J.P., et al., Adult ataxia-telangiectasia: A case report and description of genetic and functional findings. Movement Disorders Clinical Practice, 2020. 7(Supplement 1): p. S14. [Google Scholar]
- 399.Rosen F.S., Harris N. L., Weber A. L., Mark E. J., Freehling D. J., Tepper R. I., et al., A 30-Year-Old Man with Ataxia-Telangiectasia and Dysphagia—Malignant-Lymphoma, Diffuse, Large-Cell, B-Immunoblastic Type, Involving Right Tonsil and Lungs—Ataxia-Telangiectasia. New England Journal of Medicine, 1987. 316(2): p. 91–100. [DOI] [PubMed] [Google Scholar]
- 400.Karpati G., Eisen A. H., Andermann F., Bacal H. L., Robb P., Ataxia-Telangiectasia. Further Observations and Report of Eight Cases. American Journal of Diseases of Children, 1965. 110: p. 51–63. [PubMed] [Google Scholar]
- 401.Itatsu Y., Uno Y., An autopsy case of ataxia-telangiectasia. Acta Pathologica Japonica, 1969. 19(2): p. 229–39. doi: 10.1111/j.1440-1827.1969.tb00705.x [DOI] [PubMed] [Google Scholar]
- 402.Baloh R.W., Yee R. D., Boder E., Eye movements in ataxia-telangiectasia. Neurology, 1978. 28(11): p. 1099–1104. doi: 10.1212/wnl.28.11.1099 [DOI] [PubMed] [Google Scholar]
- 403.Solitare G.B., Louis-Bar’s syndrome (ataxia-telangiectasia). Anatomic considerations with emphasis on neuropathologic observations. Neurology, 1968. 18(12): p. 1180–6. doi: 10.1212/wnl.18.12.1180 [DOI] [PubMed] [Google Scholar]
- 404.Loeb D.M., Lederman H. M., Winkelstein J. A., Lymphoid malignancy as a presenting sign of ataxia-telangiectasia. Journal of Pediatric Hematology/Oncology, 2000. 22(5): p. 464–7. doi: 10.1097/00043426-200009000-00017 [DOI] [PubMed] [Google Scholar]
- 405.Danby C.S., Allen L., Moharir M. D., Weitzman S., Dumont T., Non-hodgkin B-cell lymphoma of the ovary in a child with Ataxia-telangiectasia. Journal of Pediatric & Adolescent Gynecology, 2013. 26(2): p. e43–5. [DOI] [PubMed] [Google Scholar]
- 406.Lopukhin Y., Morosov Y., Petrov R., Transplantation of neonate thymus-sternum complex in ataxia-teleangiectasia. Transplantation Proceedings, 1973. 5(1): p. 823–7. [PubMed] [Google Scholar]
- 407.Pascual-Pascual S.I., Pascual-Castroviejo I., Fontan G., Lopez-Martin V., Ataxia-telangiectasia (A-T). Contribution with eighteen personal cases. Brain & Development, 1981. 3(3): p. 289–96. doi: 10.1016/s0387-7604(81)80051-4 [DOI] [PubMed] [Google Scholar]
- 408.Goetz D.M., Spahr J. E., 16 Year old male with cough and dysphagia. American Journal of Respiratory and Critical Care Medicine, 2010. Conference: p. American Thoracic Society International Conference, ATS 2010. New Orleans, LA United States. Conference Publication: (var.pagings). 181 (1 MeetingAbstracts) (no pagination). [Google Scholar]
- 409.Ciemins J.J., Horowitz A. L., Abnormal white matter signal in ataxia telangiectasia. Ajnr: American Journal of Neuroradiology, 2000. 21(8): p. 1483–5. [PMC free article] [PubMed] [Google Scholar]
- 410.Viniou N., Terpos E., Rombos J., Vaiopoulos G., Nodaros K., Stamatopoulos K., et al., Acute myeloid leukemia in a patient with ataxia-telangiectasia: a case report and review of the literature. Leukemia, 2001. 15(10): p. 1668–70. doi: 10.1038/sj.leu.2402210 [DOI] [PubMed] [Google Scholar]
- 411.Braga-Neto P., Dutra L. A., Pedroso J. L., Barsottini O. G. P., Alpha-fetoprotein as a biomarker for recessive ataxias. Arquivos de Neuro Psiquiatria, 2010. 68(6): p. 953–955. doi: 10.1590/s0004-282x2010000600022 [DOI] [PubMed] [Google Scholar]
- 412.Sauma L., Teixeira K.C., and Montenegro M.A., Ataxia telangiectasia. Arquivos de Neuro-Psiquiatria, 2015. 73(7): p. 638. doi: 10.1590/0004-282X20150067 [DOI] [PubMed] [Google Scholar]
- 413.Pasini A.M., Gagro A., Roic G., Vrdoljak O., Lujic L., Zutelija-Fattorini M., Ataxia Telangiectasia and Juvenile Idiopathic Arthritis. Pediatrics, 2017. 139(2). doi: 10.1542/peds.2016-1279 [DOI] [PubMed] [Google Scholar]
- 414.Milligan K.L., Schirm K., Leonard S., Hussey A. A., Agharahimi A., Kleiner D. E., et al., Ataxia telangiectasia associated with nodular regenerative hyperplasia. Journal of Clinical Immunology, 2016. 36(8): p. 739–742. doi: 10.1007/s10875-016-0334-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Hosking K.A., Leung H., Andrews I., Sachdev R., Ataxia telangiectasia in a three-year-old-girl. Pediatric Neurology, 2014. 50(3): p. 279–80. doi: 10.1016/j.pediatrneurol.2013.11.011 [DOI] [PubMed] [Google Scholar]
- 416.Rawat A., Imai K., Suri D., Gupta A., Bhisikar S., Saikia B., et al., Ataxia Telangiectasia Masquerading as Hyper IgM Syndrome. Indian Journal of Pediatrics, 2016. 83(3): p. 270–1. doi: 10.1007/s12098-015-1852-x [DOI] [PubMed] [Google Scholar]
- 417.Spaull R.V.V., Majumdar A., Babiker M. O. E., Ataxia telangiectasia masquerading as partially l-dopa responsive dystonia. Developmental Medicine and Child Neurology, 2017. Conference: p. 44th Annual Conference of the British Paediatric Neurology Association, BPNA 2018. United Kingdom. 59 (Supplement 4) (pp 73). [Google Scholar]
- 418.Korah-Sedgwick M., Paris K., Ataxia telangiectasia presenting with absent IgG, IgA, and elevated IgM. Journal of Allergy and Clinical Immunology, 2016. Conference: p. 2016 Annual Meeting of the American Academy of Allergy, Asthma and Immunology, AAAAI 2016. Los Angeles, CA United States. Conference Publication: (var.pagings). 137 (2 SUPPL. 1) (pp AB222). [Google Scholar]
- 419.Snyder S., Newland J., Shinawi M., Pearson T., Nieman E., Coughlin C., et al., Ataxia telangiectasia presenting with severe neutropenia and invasive actinomyces infection. Pediatric Blood and Cancer, 2018. Conference: p. 2018 American Society of Pediatric Hematology/Oncology, ASPHO 2018. United States. 65 (Supplement 1) (pp S24–S25). [Google Scholar]
- 420.Kaneko H., Inoue R., Yamada Y., Kasahara K., Takami T., Kondo N., Ataxia telangiectasia syndrome with B cell lymphoma. Clinical Genetics, 1996. 49(6): p. 331–2. doi: 10.1111/j.1399-0004.1996.tb03803.x [DOI] [PubMed] [Google Scholar]
- 421.Abadir R., Hakami N., Ataxia telangiectasia with cancer. An indication for reduced radiotherapy and chemotherapy doses. British Journal of Radiology, 1983. 56(665): p. 343–5. doi: 10.1259/0007-1285-56-665-343 [DOI] [PubMed] [Google Scholar]
- 422.Patil M.M., Patil S. V., Ataxia telangiectasia with hepatocellular carcinoma. Indian Pediatrics, 2009. 46(6): p. 546. [PubMed] [Google Scholar]
- 423.Manglani M., Pulliyel M., Gabhale Y., Chate S., Wade M., Ataxia telangiectasia with malignant melanoma. Pediatric Blood & Cancer, 2007. 49(4): p. 531–531. [Google Scholar]
- 424.Mandigers C.M., et al., Ataxia telangiectasia: the consequences of a delayed diagnosis. Radiotherapy & Oncology, 2011. 99(1): p. 97–8. doi: 10.1016/j.radonc.2011.02.007 [DOI] [PubMed] [Google Scholar]
- 425.Alohan A.O., Falade A. G., Ataxia telangiectasia-diagnostic and management challenge in a developing country. American Journal of Respiratory and Critical Care Medicine, 2015. Conference: p. American Thoracic Society International Conference, ATS 2015. Denver, CO United States. Conference Publication: (var.pagings). 191 (MeetingAbstracts) (no pagination). [Google Scholar]
- 426.Gotz A., Eckert F., Landthaler M., Ataxia-telangiectasia (Louis-Bar syndrome) associated with ulcerating necrobiosis lipoidica. Journal of the American Academy of Dermatology, 1994. 31(1): p. 124–6. doi: 10.1016/s0190-9622(09)80245-4 [DOI] [PubMed] [Google Scholar]
- 427.Cantu-Maltos H., Saez-De-Ocariz M., Duran-McKinster C., Orozco-Covarrubias L., Palacios-Lopez C., Garcia-Romero M. T., Ataxia-telangiectasia associated granulomas in a girl. a case report. Pediatric Dermatology, 2017. Conference: p. 13th World Congress of Pediatric Dermatology. United States. 34 (Supplement 1) (pp S128). [Google Scholar]
- 428.Fleck R.M., Myers L. K., Wasserman R. L., Tigelaar R. E., Freeman R. G., Ataxia-telangiectasia associated with sarcoidosis. Pediatric Dermatology, 1986. 3(4): p. 339–43. doi: 10.1111/j.1525-1470.1986.tb00537.x [DOI] [PubMed] [Google Scholar]
- 429.Moreno L., Cox A., Ponda P., LoGalbo P., Bonagura V., Ataxia-Telangiectasia diagnosed after adenoidectomy: A case report. Clinical Immunology, 2005. 116(3): p. 295–296. [Google Scholar]
- 430.Pohl K.R., Farley J. D., Jan J. E., Junker A. K., Ataxia-telangiectasia in a child with vaccine-associated paralytic poliomyelitis. Journal of Pediatrics, 1992. 121(3): p. 405–7. [DOI] [PubMed] [Google Scholar]
- 431.Narita T., Takagi K., Ataxia-telangiectasia with dysgerminoma of right ovary, papillary carcinoma of thyroid, and adenocarcinoma of pancreas. Cancer, 1984. 54(6): p. 1113–6. doi: [DOI] [PubMed] [Google Scholar]
- 432.Goldsmith C.I., Hart W. R., Ataxia-telangiectasia with ovarian gonadoblastoma and contralateral dysgerminoma. Cancer, 1975. 36(5): p. 1838–42. doi: [DOI] [PubMed] [Google Scholar]
- 433.Alyasin S., Khoshkhui M., Abolnezhadian F., Autoimmune hemolytic anemia in a patient with probable ataxia telangiectasia: a case report. Iranian Journal Of Immunology: IJI, 2014. 11(3): p. 217–20. doi: IJIv11i3A8 [PubMed] [Google Scholar]
- 434.Yamashita S., Tanaka Y., Akagi K., An autopsy case of ataxia telangiectasia. Neuropathology, 2012. Conference: p. 53rd Annual Meeting of the Japanese Society of Neuropathology. Niigata Japan. Conference Publication: (var.pagings). 32 (3) (pp 361). [Google Scholar]
- 435.Sharma L.M., Kashyap R., Gupta S., Bhargava M., B-cell acute lymphoblastic leukemia in a child with ataxia telangiectasia. Pediatric Hematology & Oncology, 2008. 25(5): p. 473–6. [DOI] [PubMed] [Google Scholar]
- 436.Kropshofer G., Wehl G., Klein-Franke A., Hogler W., Meister B., B-cell lymphoma in a girl with ataxia teleangiectasia (A-T) treated with rituximab monotherapy. Pediatric Blood & Cancer, 2006. 46(4): p. 528–9. [DOI] [PubMed] [Google Scholar]
- 437.Bahadir A., et al., Bladder Artery Embolization for Massive Hematuria Treatment in a Patient With Ataxia-Telangiectasia Acute Lymphoblastic Leukemia. J Pediatr Hematol Oncol, 2020. 42(4): p. 316–318. doi: 10.1097/MPH.0000000000001471 [DOI] [PubMed] [Google Scholar]
- 438.Cohen J.M., Cuckow P., Davies E. G., Bladder wall telangiectasis causing life-threatening haematuria in ataxia-telangiectasia: a new observation. Acta Paediatrica, 2008. 97(5): p. 667–9. doi: 10.1111/j.1651-2227.2008.00736.x [DOI] [PubMed] [Google Scholar]
- 439.Rampur L., Shliozberg J., A Case of Ataxia Telangiectasia with Immunodeficiency Due to a Rare Vriant. Journal of Clinical Immunology, 2016. 36(3): p. 276–277. [Google Scholar]
- 440.Ferraris A.M., Melani C., Canepa L., Meloni T., Forteleoni G., Gaetani G. F., A case of ataxia telangiectasia with unbalanced glucose 6-phosphate dehydrogenase mosaicism in the granulocytic/monocytic lineages. American Journal of Human Genetics, 1987. 40(1): p. 32–8. [PMC free article] [PubMed] [Google Scholar]
- 441.Bell B.N, H.N., Patel M, A case of clandestine cancer: Increasing awareness of non-hematologic cancers in patients with ataxiatelangiectasia. [Google Scholar]
- 442.Zupanic E., Sega Jazbec S., Case report: Ataxia-telangiectasia: Cerebral abnormalities in: A case of long survival. European Journal of Neurology, 2016. Conference: p. 2nd Congress of the European Academy of Neurology. Copenhagen Denmark. Conference Publication: (var.pagings). 23 (SUPPL. 2) (pp 149). [Google Scholar]
- 443.Langhagen T., Blaschek A., Rettinger N., Muller-Felber W., Jahn K., Case report: Oculomotor apraxia in ataxia telangiectasia. Neuropediatrics, 2013. Conference: p. 39th Annual Meeting of the Society of Neuropediatrics. Innsbruck Austria. Conference Publication: (var.pagings). 44 (2) (no pagination). [Google Scholar]
- 444.Liu H.S., Chen Y. C., Chen C. Y., Cerebral microbleeds and iron depletion of dentate nuclei in ataxia-telangiectasia. Neurology, 1062. 87(10): p. 1062–1063. doi: 10.1212/WNL.0000000000003066 [DOI] [PubMed] [Google Scholar]
- 445.Lin C.H., Lin W. C., Wang C. H., Ho Y. J., Chiang I. P., Peng C. T., et al., Child with ataxia telangiectasia developing acute myeloid leukemia. Journal of Clinical Oncology, 2010. 28(14): p. e213–4. doi: 10.1200/JCO.2009.25.5067 [DOI] [PubMed] [Google Scholar]
- 446.Kazaz I.C., F; Teoman AS; Karaguzel E, A Child with Ataxia Telangiectasia with Persistent Hematuria due to Bladder Wall Telangiectasia. JOURNAL OF ACADEMIC RESEARCH IN MEDICINE, 2018. [Google Scholar]
- 447.Murakawa G.J., McCalmot T., Frieden I. J., Chronic plaques in a patient with ataxia telangiectasia. Cutaneous granulomatous lesions in a patient with AT. Archives of Dermatology, 1998. 134(9): p. 1145, 1148. doi: 10.1001/archderm.134.9.1145 [DOI] [PubMed] [Google Scholar]
- 448.Duhrsen U., Uppenkamp M., Uppenkamp I., Becher R., Engelhard M., Konig E., et al., Chronic T cell leukemia with unusual cellular characteristics in ataxia telangiectasia. Blood, 1986. 68(2): p. 577–85. [PubMed] [Google Scholar]
- 449.van Os N.J.H., et al., Classic ataxia-telangiectasia: the phenotype of long-term survivors. J Neurol, 2020. 267(3): p. 830–837. doi: 10.1007/s00415-019-09641-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Doshi A., Rosenzweig S. D., Leonard S., A COMPLEX CASE OF HYPER IgM IMMUNODEFICIENCY AND LATE PRESENTATION OF ATAXIA TELANGIECTASIA WITHOUT NEUROLOGIC SIGNS. Journal of Clinical Immunology, 2016. 36(3): p. 251–251. [Google Scholar]
- 451.Mitra A., Pollock B., Gooi J., Darling J. C., Boon A., Newton-Bishop J. A., Cutaneous granulomas associated with primary immunodeficiency disorders. British Journal of Dermatology, 2005. 153(1): p. 194–9. doi: 10.1111/j.1365-2133.2005.06619.x [DOI] [PubMed] [Google Scholar]
- 452.Corbisier A., Eschard C., Motte J., Munzer M., Barhoum K., Kalis B., et al., [Cutaneous granulomatous lesions disclosing ataxia-telangiectasia]. Annales de Dermatologie et de Venereologie, 1999. 126(8–9): p. 608–11. [PubMed] [Google Scholar]
- 453.Beaulieu-Boire I., Aquino C. C., Fasano A., Poon Y. Y., Fallis M., Lang A. E., et al., Deep Brain Stimulation in Rare Inherited Dystonias. Brain Stimulation, 2016. 9(6): p. 905–910. doi: 10.1016/j.brs.2016.07.009 [DOI] [PubMed] [Google Scholar]
- 454.Kapoor G., Albrecht R. J., Craver R., Duncan C., Warrier R. P., Diffuse large cell lymphoma presenting as inflammatory bowel disease in an adolescent with ataxia telangiectasia. Leukemia Research, 1996. 20(11–12): p. 997–8. doi: 10.1016/s0145-2126(96)00033-1 [DOI] [PubMed] [Google Scholar]
- 455.Abdulhag U.N., Liebster D., Eisenstein E. M., Berkun Y., Efficacy of Rituximab in Refractory Cold Agglutinin Hemolytic Anemia in a Patient with Ataxia-Telangiectasia. Israel Medical Association Journal: Imaj, 2015. 17(7): p. 455–6. [PubMed] [Google Scholar]
- 456.Reyes C., Abuzaitoun O., De Jong A., Hanson C., Langston C., Epstein-Barr virus-associated smooth muscle tumors in ataxia-telangiectasia: a case report and review. Human Pathology, 2002. 33(1): p. 133–6. doi: 10.1053/hupa.2002.30214 [DOI] [PubMed] [Google Scholar]
- 457.Kruger R., Zappe S. M., Stolzel K., von Bernuth H., Wahn V., Knopke S., Fatal case of ataxia-telangiectasia complicated by severe epistaxis due to nasal telangiectasia in a 12-year-old boy. Pediatric Allergy & Immunology, 2017. 28(7): p. 711–712. [DOI] [PubMed] [Google Scholar]
- 458.Irsfeld H., Korholz D., Janssen G., Wahn V., Schroten H., Fatal outcome in two girls with hodgkin disease complicating ataxia-telangiectasia (Louis-Bar syndrome) despite favorable response to modified-dose chemotherapy. Medical & Pediatric Oncology, 2000. 34(1): p. 62–4. doi: [DOI] [PubMed] [Google Scholar]
- 459.Matsuoka M., et al., Follow-up studies of immunological disorders in patients with ataxia-telangiectasia I. Clinical and pathological observations of two cases. Japanese Journal of Clinical Immunology, 1983. 6(4): p. 235–248. [Google Scholar]
- 460.Barmettler S., Farmer J., Abraham R., Smith M. J., Hale J. E., Comeau A. M., et al., Functional diagnosis of ataxia telangiectasia in a female infant identified via newborn screening for SCID (NBS SCID). Journal of Clinical Immunology, 2017. Conference: p. 2017 CIS Annual Meeting: Immune Deficiency and Dysregulation North American Conference. United States. 37 (2) (pp 236–237). [Google Scholar]
- 461.Kolbel H., Kaiser O., Andres B., Taylor A. F. M., Kieslich M., Hoche F., et al., Gait disturbances and unspecific white matter hyperintensity in T2-weighted imaging as the first manifestation of an ataxia telangiectasia. Neuropediatrics, 2016. Conference: p. 42nd Annual Meeting of the Society for Neuropediatrics. Germany. 47 (Supplement 1) (no pagination). [Google Scholar]
- 462.Galvez-Cuitiva E.A., Ridaura-Sanz C., Yamazaki-Nakashimada M. A., Leal-Leal C., Zapata-Tarres M., Germ cell ovarian tumor in an adolescent with ataxia-telangiectasia. Acta Pediatrica De Mexico, 2015. 36(6): p. 464–472. [Google Scholar]
- 463.Laurel R., Yamazaki-Nakashimada M. A., Lopez-Ugalde M., Scheffler-Mendoza S. C., Hepatic disease in ataxia-telangiectasia, diagnosed in institutonacional de pediatria in Mexico City. Journal of Clinical Immunology, 2017. Conference: p. 7th Meeting of the Latin American Society for Immunodeficiencies, LASID 2017. Brazil. 37 (1 Supplement 1) (pp S25). [Google Scholar]
- 464.Srisirirojanakorn N., Finegold M. J., Gopalakrishna G. S., Klish W. J., Hepatic veno-occlusive disease in ataxia-telangiectasia. Journal of Pediatrics, 1999. 134(6): p. 786–8. doi: 10.1016/s0022-3476(99)70301-x [DOI] [PubMed] [Google Scholar]
- 465.Jacobs M.F., et al., Hepatosplenic alphabeta T-Cell Lymphoma as Second Malignancy in Young Adult Patient With Previously Undiagnosed Ataxia-Telangiectasia. J Pediatr Hematol Oncol, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 466.Kutukculer N. and Aksu G., Is there an association between autoimmune hemolytic anemia and ataxia-telangiectasia? Autoimmunity, 2000. 32(2): p. 145–7. doi: 10.3109/08916930008994084 [DOI] [PubMed] [Google Scholar]
- 467.Pedroza-Flores K.P., Nunez-Nunez M. E., Rios-Aguirre A., Gonzalez-Cruz M. J., Barron-Balderas A., Pere J. L., et al., Late diagnosis in a patient with ataxia-telangiectasia and review of literature. Journal of Clinical Immunology, 2013. Conference: p. 3rd Meeting of the Latin American Society for Immunodeficiencies, LASID 2013. Santiago Chile. Conference Publication: (var.pagings). 33 (SUPPL. 3) (pp S108). [Google Scholar]
- 468.Agarwal S., Gupta R. K., Gora A., Gupta M. L., Sadasivan S., Bhandari A., et al., Late presentation of autoimmune hepatitis as end-stage liver disease in a diagnosed case of celiac disease with ataxia telangiectasia. Indian Journal of Gastroenterology, 2016. Conference: p. 57th Annual Conference of Indian Society of Gastroenterology, ISGCON 2016. India. 35 (1 Supplement) (pp A105). [Google Scholar]
- 469.Eyre J.A., Gardner-Medwin D., Summerfield G. P., Leukoencephalopathy after prophylactic radiation for leukaemia in ataxia telangiectasia. Archives of Disease in Childhood, 1988. 63(9): p. 1079–80. doi: 10.1136/adc.63.9.1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Bodemer C., et al., Live rubella virus vaccine long-term persistence as an antigenic trigger of cutaneous granulomas in patients with primary immunodeficiency. Clinical Microbiology and Infection, 2014. 20(10): p. O656–O663. doi: 10.1111/1469-0691.12573 [DOI] [PubMed] [Google Scholar]
- 471.Ussowicz M., Musial J., Duszenko E., Haus O., Kalwak K., Long-term survival after allogeneic-matched sibling PBSC transplantation with conditioning consisting of low-dose busilvex and fludarabine in a 3-year-old boy with ataxia-telangiectasia syndrome and ALL. Bone Marrow Transplantation, 2013. 48(5): p. 740–1. [DOI] [PubMed] [Google Scholar]
- 472.Miller S.J.H., Gooddy W., Madame louis-bar’s syndrome; a case record, with comments upon the name, classification and significance of this disorder. Brain, 1964. 87(4): p. 581–588. doi: 10.1093/brain/87.4.581 [DOI] [PubMed] [Google Scholar]
- 473.Rosas-Salazar C., Gunawardena S. W., Spahr J. E., Malignant pleural mesothelioma in a child with ataxia-telangiectasia. Pediatric Pulmonology, 2013. 48(1): p. 94–7. doi: 10.1002/ppul.22535 [DOI] [PubMed] [Google Scholar]
- 474.De Souza M.T., Vera-Lozada G., Othman M., Marques-Salles T. J., Pinto L. W., da Rocha M. M., et al., Molecular and Cytogenetic Studies in a Child with Burkitt Lymphoma and Ataxia-Telangiectasia Syndrome Harboring MYC Overexpression and Partial Trisomy 8. Annals of Laboratory Medicine, 2018. 38(1): p. 63–66. doi: 10.3343/alm.2018.38.1.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.McDonald P.S., Cora-Bramble D., De Palma L., Monoclonal gammopathy of the immunoglobulin A class in a two-year-old girl with ataxia telangiectasia. Pediatric & Developmental Pathology, 1998. 1(4): p. 319–21. [DOI] [PubMed] [Google Scholar]
- 476.Nakayama T., Sato Y., Uematsu M., Takagi M., Hasegawa S., Kumada S., et al., Myoclonic axial jerks for diagnosing atypical evolution of ataxia telangiectasia. Brain & Development, 2015. 37(3): p. 362–5. doi: 10.1016/j.braindev.2014.06.001 [DOI] [PubMed] [Google Scholar]
- 477.Purkait R., et al., Neurocutaneous syndrome: A prospective study. Indian Journal of Dermatology, 2011. 56(4): p. 375–379. doi: 10.4103/0019-5154.84721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Kifer N A.T., Sestan M, Frkovic M, Vinuesa C.G, Jelusic M, New ATM variants and a rare association of juvenile idiopathic arthritis and ataxia-telangiectasia: Coincidence or relationship? Pediatric Rheumatology, 2019. [Google Scholar]
- 479.Roohi J., Crowe J., Loredan D., Anyane-Yeboa K., Mansukhani M. M., Omesi L., et al., New diagnosis of atypical ataxia-telangiectasia in a 17-year-old boy with T-cell acute lymphoblastic leukemia and a novel ATM mutation. Journal of Human Genetics, 2017. 62(5): p. 581–584. doi: 10.1038/jhg.2017.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Shankar T., Chen X., Szabolcs P., Vander Lugt M. T., Chong H. J., Newborn screening for severe combined immunodeficiency (SCID) leads to early identification of ataxia-telangiectasia (AT) complicated by neutropenia: A case report. Journal of Allergy and Clinical Immunology, 2015. Conference: p. 2015 Annual Meeting of the American Academy of Allergy, Asthma and Immunology, AAAAI 2015. Houston, TX United States. Conference Publication: (var.pagings). 135 (2 SUPPL. 1) (pp AB13). [Google Scholar]
- 481.Minto H.B., Rubtsova K., Reynolds P. R., Gelfand E. W., Ataxia telangiectasia presenting with hypogammaglobulinemia and high igm levels, cutaneous granulomas, and expansion of CD21(LO) T-bet(+) b cells. Journal of Allergy and Clinical Immunology, 2017. Conference: p. Annual Meeting of the American Academy of Allergy, Asthma and Immunology, AAAAI 2017. United States. 139 (2 Supplement 1) (pp AB105). [Google Scholar]
- 482.Piane M., Molinaro A., Soresina A., Costa S., Maffeis M., Germani A., et al., Novel compound heterozygous mutations in a child with Ataxia-Telangiectasia showing unrelated cerebellar disorders. Journal of the Neurological Sciences, 2016. 371: p. 48–53. doi: 10.1016/j.jns.2016.10.014 [DOI] [PubMed] [Google Scholar]
- 483.McLaughlin M., Saad A. G., Ophthalmic pathology of ataxia-telangiectasia: Description of the first case. Laboratory Investigation, 2006. 86: p. 6A–6A. [Google Scholar]
- 484.Win P.H. and Wedner H.J., Partial immune system reconstitution ina patient with ataxia-telangiectasia. Annals of Allergy Asthma & Immunology, 2007. 98(1): p. A17–A17. [Google Scholar]
- 485.Brioli A., Parisi S., Iacobucci I., Cavo M., Papayannidis C., Anna Zannetti B., et al., Patient with ataxia telangiectasia who developed acute myeloid leukemia. Leukemia & Lymphoma, 2011. 52(9): p. 1818–20. doi: 10.3109/10428194.2011.577256 [DOI] [PubMed] [Google Scholar]
- 486.Myers G P.K., PREVIOUSLY HEALTHY 15-MONTH OLD FEMALE WITH RAPIDLY PROGRESSIVE ATAXIA AND MILESTONE REGRESSION. Annals of Allergy, Asthma and Immunology, 2018. [Google Scholar]
- 487.Mansouri D., et al., Primary immune deficiencies presenting in adults: seven years of experience from Iran. Journal of Clinical Immunology, 2005. 25(4): p. 385–91. doi: 10.1007/s10875-005-4124-0 [DOI] [PubMed] [Google Scholar]
- 488.Amin O.S., Progressive gait instability in a young girl; what will happen at the end? BMJ Case Reports, 2012. 17: p. 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Morgan J.L., Holcomb T. M., Morrissey R. W., Radiation reaction in ataxia telangiectasia. American Journal of Diseases of Children, 1968. 116(5): p. 557–8. doi: 10.1001/archpedi.1968.02100020561022 [DOI] [PubMed] [Google Scholar]
- 490.DeWire M.D., Pananandiker A. S. P., Ellison D. E., McKinnon P. J., Kastan M. B., Gajjar A., Radiation Therapy and Adjuvant Chemotherapy in a Patient with a High Grade Glioma and Underlying Ataxia Telangiectasia. Neuro-Oncology, 2010. 12(6): p. II87–II87. [Google Scholar]
- 491.Hilmi F.A., Soliman D.S., Al Sabbagh A., Alkuwari E., Taha R.Y., Al Battah A., et al., A rare case of marginal zone lymphoma in a 15-year old ataxia telangiectasia patient with massive bone marrow involvement and a challenging nodal diagnosis. Human Pathology: Case Reports, 2019. [Google Scholar]
- 492.Kumar G., et al., Rare Cause of Bright Red Gross Hematuria in a Child. Indian J Nephrol, 2018. 28(4): p. 327–328. doi: 10.4103/ijn.IJN_147_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493.Chakravarthi S., Goyal M. K., Spontaneous pneumothorax in ataxia telangectasia. Indian Journal of Medical Research, 2014. 140(2): p. 321–2. [PMC free article] [PubMed] [Google Scholar]
- 494.Sandlund J.T., Kastan M. B., Kennedy W., Behm F., Entrekin E., Pui C. H., et al., A subtle t(3;8) results in plausible juxtaposition of MYC and BCL6 in a child with Burkitt lymphoma/leukemia and ataxia-telangiectasia. Cancer Genetics & Cytogenetics, 2006. 168(1): p. 69–72. [DOI] [PubMed] [Google Scholar]
- 495.Onoda T., Kanno M., Meguro T., Sato H., Takahashi N., Kawakami T., et al., Successful treatment of acute myeloid leukaemia in a patient with ataxia telangiectasia. European Journal of Haematology, 2013. 91(6): p. 557–60. doi: 10.1111/ejh.12186 [DOI] [PubMed] [Google Scholar]
- 496.Hersby D.S., Sehested A., Kristensen K., Schmiegelow K., T-cell ALL in ataxia telangiectasia cured with only 7 weeks of anti-leukemic therapy. Journal of Pediatric Hematology/Oncology, 2015. 37(2): p. 154–5. doi: 10.1097/MPH.0000000000000151 [DOI] [PubMed] [Google Scholar]
- 497.Ortega—Lopez M.C., Leon—Quintero A., Telangiectasia ataxia new functional defect. Journal of Clinical Immunology, 2013. Conference: p. 3rd Meeting of the Latin American Society for Immunodeficiencies, LASID 2013. Santiago Chile. Conference Publication: (var.pagings). 33 (SUPPL. 3) (pp S106). [Google Scholar]
- 498.Schoenaker M.H.D., Van Os N. J. H., Van der Flier M., Van Deuren M., Seyger M. M., Taylor A. M. R., et al., Telangiectasias in Ataxia Telangiectasia: Clinical significance, role of ATM deficiency and potential pathophysiological mechanisms. European Journal of Medical Genetics, 2018. 61(5): p. 284–287. doi: 10.1016/j.ejmg.2017.12.012 [DOI] [PubMed] [Google Scholar]
- 499.Ivonye C., Jamched U., Anderson D., Adesunloye B., Uncommon skin lesion in a patient with ataxia-telangiectasia. International Journal of Dermatology, 2008. 47(10): p. 1051–2. doi: 10.1111/j.1365-4632.2008.03745.x [DOI] [PubMed] [Google Scholar]
- 500.Metin A K.C.I.Y.E.A.V.E.O.D., An unexpected malignancy in children with ataxia telangiectasis: Intracerebellar hemangiopericytoma. Allergy, 2019. [Google Scholar]
- 501.Ulusoy E., Edeer-Karaca N., Ozen S., Ertan Y., Goksen D., Aksu G., et al., An unusual manifestation: Papillary thyroid carcinoma in a patient with ataxia-telengiectasia. Turkish Journal of Pediatrics, 2016. 58(4): p. 442–445. [DOI] [PubMed] [Google Scholar]
- 502.Suzuki K., Tsugawa K., Oki E., Morio T., Ito E., Tanaka H., Vesical varices and telangiectasias in a patient with ataxia telangiectasia. Pediatric Nephrology, 2008. 23(6): p. 1005–8. doi: 10.1007/s00467-007-0710-0 [DOI] [PubMed] [Google Scholar]
- 503.Synofzik M., et al., Videogame-based coordinative training can improve advanced, multisystemic early-onset ataxia. Journal of Neurology, 2656. 260(10): p. 2656–2658. doi: 10.1007/s00415-013-7087-8 [DOI] [PubMed] [Google Scholar]
- 504.Kozina A F.I., Borisevich D, Schatalov P, Okuneva E, Korostin D, Krasnenko A, et al., Whole exome sequencing identifies a novel ATM mutation resulting ataxia-teleangiectasia. European Journal of Human Genetics, 2019. [Google Scholar]
- 505.Nandhagopal R and Krishnamoorthy S. G, Unsteady gait. Postgrad Med J, 2006. 82(967): p. e7–8. doi: 10.1136/pgmj.2005.040774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 506.Cosper A. and Eisenberg R., Early Diagnosis of Ataxia Telangiectasia Identified through Low T-Cell Receptor Excision Circles. Annals of Allergy, Asthma and Immunology, 2020. 125(5 Supplement): p. S82. [Google Scholar]
- 507.Carles M.E., et al., Central Precocious Puberty in a Boy with down Syndrome and Ataxia Telangiectasia: A Rare Association. Hormone Research in Paediatrics, 2021. 93(SUPPL 2): p. 31–31. [Google Scholar]
- 508.Goldgraben M.A., et al., Genomic profiling of acute myeloid leukaemia associated with ataxia telangiectasia identifies a complex karyotype with wild-type TP53 and mutant KRAS, G3BP1 and IL7R. Pediatr Blood Cancer, 2020. 67(9): p. e28354. doi: 10.1002/pbc.28354 [DOI] [PubMed] [Google Scholar]
- 509.Zannolli R., Buoni S., Betti G., Salvucci S., Plebani A., Soresina A., et al., A randomized trial of oral betamethasone to reduce ataxia symptoms in ataxia telangiectasia. Movement Disorders, 2012. 27(10): p. 1312–6. doi: 10.1002/mds.25126 [DOI] [PubMed] [Google Scholar]
- 510.Jacob C.M.A., Pastorino A. C., Santos V. Z. C., Chong A. K., Dorna M., Fomin A. B. F., et al., Ataxia-telangiectasia: Clinical, laboratorial and mutational analysis of patients from a reference center for primary immunodeficiency. Journal of Allergy and Clinical Immunology, 2008. 121(2): p. S164–S164. [Google Scholar]
- 511.Dantas E.L. J; Mazzucchelli JTL; Aranda CS; Serrano MEG; Bezrodnik L; Moreira I; et al., Ataxia-Telangiectasia: Epidemiological Survey in Latin America. Journal of Allergy and Clinical Immunology, 2018. [Google Scholar]
- 512.Chessa L., Leuzzi V., Plebani A., Soresina A., Micheli R., D’Agnano D., et al., Intra-erythrocyte infusion of dexamethasone reduces neurological symptoms in ataxia teleangiectasia patients: results of a phase 2 trial. Orphanet Journal Of Rare Diseases, 2014. 9: p. 5. doi: 10.1186/1750-1172-9-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 513.Bott L., Lebreton J., Thumerelle C., Cuvellier J., Deschildre A., Sardet A., Lung disease in ataxia-telangiectasia. Acta Paediatrica, 2007. 96(7): p. 1021–4. doi: 10.1111/j.1651-2227.2007.00338.x [DOI] [PubMed] [Google Scholar]
- 514.Mirzaee A.Z., Darougar S., Chavoshzadeh Z., Mesdaghi M., Mansouri M., Babaie D., et al., Registry of clinical data and laboratory findings in 80 patients with primary immunodeficiencies in mofid children hospital. Journal of Comprehensive Pediatrics, 2018. [Google Scholar]
- 515.Almeida A.G., Marques-Dias M. J., Jacob C. M. A., Duarte A. S., Grumach A. S. , Ataxia-telangiectasia (AT) clinical and laboratorial evaluation of 11 patients. Journal of Allergy and Clinical Immunology, 1999. 103(1): p. S142–S142. [Google Scholar]
- 516.Kolbel H., Kaiser O., Andres B., Moller-Hartmann C., Taylor A. F. M., Kieslich M., et al., Unspecific white matter hyperintensity in T2-weighted imaging and dystonia as the first manifestations of ataxia telangiectasia. European Journal of Paediatric Neurology, 2017. Conference: p. 12th European Paediatric Neurology Society Congress, EPNS 2017. France. 21 (Supplement 1) (pp e214). [Google Scholar]
- 517.Seghezzo S.F., D; Shah SD; Mathes EF; Dorsey MJ; Puck J, Ataxia Telangiectasia with Chronic Skin Granulomas Preventable with SCID Newborn Screening? 2019. [Google Scholar]
- 518.Robinson A., Ataxia-telangiectasia presenting with craniostenosis. Archives of Disease in Childhood, 1962. 37: p. 652–5. doi: 10.1136/adc.37.196.652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.van Egmond M.E., Elting J. W., Kuiper A., Zutt R., Heineman K. R., Brouwer O. F., et al., Myoclonus in childhood-onset neurogenetic disorders: The importance of early identification and treatment. European Journal of Paediatric Neurology, 2015. 19(6): p. 726–9. doi: 10.1016/j.ejpn.2015.07.003 [DOI] [PubMed] [Google Scholar]
- 520.Madaan P., Mukherjee S., Reddy C., Yadav J., Saini L., Multiple café-au-lait macules and movement disorder: Think beyond neurofibromatosis. Archives of Diseases in Childhood, 2019. doi: 10.1136/archdischild-2019-317497 [DOI] [PubMed] [Google Scholar]
- 521.Madaan P., et al., Multiple café-au-lait macules and movement disorder: think beyond neurofibromatosis. Arch Dis Child, 2021. 106(1): p. 73. doi: 10.1136/archdischild-2019-317497 [DOI] [PubMed] [Google Scholar]
- 522.Devaney R., Pasalodos S., Suri M., Bush A., Bhatt J. M., Ataxia telangiectasia: presentation and diagnostic delay. Archives of Disease in Childhood, 2017. 102(4): p. 328–330. doi: 10.1136/archdischild-2016-310477 [DOI] [PubMed] [Google Scholar]
- 523.Moreira D., Teixeira C., Santos M., Neves E., Vasconcelos J., Marques L., Ataxia telangiectasia-report of six cases. Journal of Clinical Immunology, 2012. Conference: p. 15th Biennial Meeting of the European Society for Immunodeficiency, ESID 2012. Florence Italy. Conference Publication: (var.pagings). 32 (SUPPL. 1) (pp S241). [DOI] [PubMed] [Google Scholar]
- 524.Bellanti J.A., Artenste.Ms, Buescher, E. L., Ataxia-Telangiectasia—Immunologic and Virologic Studies of Serum and Respiratory Secretions. Pediatrics, 1966. 37(6): p. 924–&. [Google Scholar]
- 525.Silva R., Santos M., Barbot C., Vasconcelos J., Neves E., Gomes E., et al., Ataxia-telangiectasia—review of five cases. Allergy, 2010. 65: p. 471–471. doi: 10.1097/BPB.0b013e32833cb764 [DOI] [PubMed] [Google Scholar]
- 526.Rudenskaya G.E., et al., [Ataxia-telangiectasia with rare phenotype and unusual pedigree]. Zh Nevrol Psikhiatr Im S S Korsakova, 2019. 119(6): p. 101–106. doi: 10.17116/jnevro2019119061101 [DOI] [PubMed] [Google Scholar]
- 527.Scarpini C., Mondelli M., Guazzi G. C., Federico A., Ataxia-telangiectasia: somatosensory, brainstem auditory and motor evoked potentials in six patients. Developmental Medicine & Child Neurology, 1996. 38(1): p. 65–73. [DOI] [PubMed] [Google Scholar]
- 528.Cao J, Shen R., Zhang W, Mao B, Shi Q, Zhou R, et al., Clinical diagnosis and genetic counseling of atypical ataxia‑telangiectasia in a Chinese family. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 529.Catal F., Topal E., Celiksoy M. H., Ermistekin H., Kutluturk K., Yildirim N., et al., Demographic and systemic manifestations of patients diagnosed with ataxia-telangiectasia. Asim, Allerji, Immunoloji, 2014. 12(2): p. 83–90. [Google Scholar]
- 530.Keklik M., Koker M. Y., Sivgin S., Camlica D., Pala C., Cetin M., et al., Detection of Acute Lymphoblastic Leukemia Involvement in Pleural Fluid in an Adult Patient with Ataxia Telangiectasia by Flow Cytometry Method. Indian Journal of Hematology and Blood Transfusion, 2014. 30(Supplement 1): p. 73–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 531.Grant S.G., Reeger W., Wenger S. L., Diagnosis of ataxia telangiectasia with the glycophorin A somatic mutation assay. Genetic Testing, 1997. 1(4): p. 261–7. doi: 10.1089/gte.1997.1.261 [DOI] [PubMed] [Google Scholar]
- 532.Henderson L., Cole H., Arlett C., James S. E., Cole J., Lehmann A., et al., Diagnosis of ataxia-telangiectasia by T-lymphocyte cloning assay. Lancet, 1985. 2(8466): p. 1242. doi: 10.1016/s0140-6736(85)90766-4 [DOI] [PubMed] [Google Scholar]
- 533.Privette E.D., Ram G., Treat J. R., Yan A. C., Heimall J. R., Healing of granulomatous skin changes in ataxia-telangiectasia after treatment with intravenous immunoglobulin and topical mometasone 0.1% ointment. Pediatric Dermatology, 2014. 31(6): p. 703–7. doi: 10.1111/pde.12411 [DOI] [PubMed] [Google Scholar]
- 534.Grau I.M., Diaz J. V., Immunodeficiency with ataxia telangiectasia. Case report. Inmunologia, 2009. 28(1): p. 12–18. [Google Scholar]
- 535.Strober W., Wochner R. D., Barlow M. H., McFarlin D. E., Waldmann T. A., Immunoglobulin metabolism in ataxia telangiectasia. Journal of Clinical Investigation, 1968. 47(8): p. 1905–15. doi: 10.1172/JCI105881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 536.Keklik M., Sivgin S., Kalin B. S., Akyol G., Pala C., Solmaz M., et al., The management of hyperleukocytosis in an adult patient with acute lymphoblastic leukemia and ataxia-telangiectasia. Transfusion & Apheresis Science, 2013. 48(3): p. 293–5. [DOI] [PubMed] [Google Scholar]
- 537.Nissenkorn A., Levi Y. B., Vilozni D., Berkun Y., Efrati O., Frydman M., et al., Neurologic presentation in children with ataxia-telangiectasia: is small head circumference a hallmark of the disease? Journal of Pediatrics, 2011. 159(3): p. 466–471.e1. doi: 10.1016/j.jpeds.2011.02.005 [DOI] [PubMed] [Google Scholar]
- 538.Miller M.E., Chatten J., Ovarian changes in ataxia telangiectasia. Acta Paediatrica Scandinavica, 1967. 56(5): p. 559–61. doi: 10.1111/j.1651-2227.1967.tb15424.x [DOI] [PubMed] [Google Scholar]
- 539.Meneret A., Ahmar-Beaugendre Y., Rieunier G., Mahlaoui N., Gaymard B., Apartis E., et al., The pleiotropic movement disorders phenotype of adult ataxia-telangiectasia. Neurology, 2014. 83(12): p. 1087–95. doi: 10.1212/WNL.0000000000000794 [DOI] [PubMed] [Google Scholar]
- 540.Chen Z., Ye W., Long Z., Ding D., Peng H., Hou X., et al., Targeted Next-Generation Sequencing Revealed Novel Mutations in Chinese Ataxia Telangiectasia Patients: A Precision Medicine Perspective. PLoS ONE [Electronic Resource], 2015. 10(10): p. e0139738. doi: 10.1371/journal.pone.0139738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 541.Kuznetsova M.V., Trofimov D. Y., Shubina E. S., Kochetkova T. O., Karetnikova N. A., Barkov I. Y., et al., Two novel mutations associated with ataxia-telangiectasia identified using an ion ampliSeq inherited disease panel. Frontiers in Neurology, 2017. 8(OCT). doi: 10.3389/fneur.2017.00570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 542.Ramcharan J., Balkaran B., Basdeo-Maharaj K., Narinesingh D., Ramlackhansingh A., Ataxia Telangiectasia. A case report. West Indian Medical Journal, 2001. 50(4): p. 336–8. [PubMed] [Google Scholar]
- 543.Teller W.M., Millichap J. G., Ataxia-telangiectasia (Louis-Bar syndrome) with prominent sinopulmonary disease. JAMA, 1961. 175: p. 779–82. doi: 10.1001/jama.1961.03040090039007 [DOI] [PubMed] [Google Scholar]
- 544.Skoglund R.R., Ataxia-telangiectasia. Archives of Neurology, 1984. 41(2): p. 137. doi: 10.1001/archneur.1984.04050140035014 [DOI] [PubMed] [Google Scholar]
- 545.Tachi N., Agatzuma K., Motomura S., A case of ataxia-telangiectasia with dystonia. Sural nerve biopsy findings. No To Hattatsu, 1982. 14(5): p. 504–510. [Google Scholar]
- 546.Bodensteiner J.B., Goldblum R. M., Goldman A. S., Enlarging Neurological Spectrum of Ataxia-Telangiectasia. Clinical Research, 1978. 26(6): p. A821–A821. [Google Scholar]
- 547.Bowden D.H., Danis P. G., Sommers S. C., Ataxia-Telangiectasia. A Case with Lesions of Ovaries and Adenohypophysis. Journal of Neuropathology & Experimental Neurology, 1963. 22: p. 549–54. [PubMed] [Google Scholar]
- 548.Aslanov A.M., [Coordination disorders in children with the Louis-Bar syndrome]. Zhurnal Nevropatologii i Psikhiatrii Imeni S—S—Korsakova, 1979. 79(10): p. 1375–9. [PubMed] [Google Scholar]
- 549.Henrich M., Lutz S., Busse M., Schara U., Ataxia telangiectasia in dizygotic two year old twins. Neuropediatrics, 2011. Conference: p. 37th Annual Meeting of the Society of Neuropediatrics. Garmisch-Partenkirchen Germany. Conference Publication: (var.pagings). 42 (SUPPL. 1) (no pagination). [Google Scholar]
- 550.Schaffer F.M., Virella-Lowell I., Gatti R. A., Gossage D. L., Ataxia-Telangiectasia, Associated with a Rare 1339C > T ATM mutation, presenting in infancy with Pneumocystis carinii pneumonia, and an elevated serum IgM. Journal of Immunology, 2007. 178. [Google Scholar]
- 551.Rubinstein J.D., et al., EBV-directed viral-specific T-lymphocyte therapy for the treatment of EBV-driven lymphoma in two patients with primary immunodeficiency and DNA repair defects. Pediatr Blood Cancer, 2020. 67(3): p. e28126. doi: 10.1002/pbc.28126 [DOI] [PubMed] [Google Scholar]
- 552.Seidemann K., Henze G., Beck J. D., Sauerbrey A., Kuhl J., Mann G., et al., Non-Hodgkin’s lymphoma in pediatric patients with chromosomal breakage syndromes (AT and NBS): experience from the BFM trials. Annals of Oncology, 2000. 11 Suppl 1: p. 141–5. [PubMed] [Google Scholar]
- 553.Dörr J.R., et al., Germline Mutations Including the Rare Pathogenic Variant c.3206delC in the ATM Gene Cause Ataxia Teleangiectasia-Associated Primary Central Nervous System Lymphoma. Children (Basel), 2021. 8(6). doi: 10.3390/children8060469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 554.Al-Herz W., Nanda A., Skin manifestations in primary immunodeficient children. Pediatric Dermatology, 2011. 28(5): p. 494–501. doi: 10.1111/j.1525-1470.2011.01409.x [DOI] [PubMed] [Google Scholar]
- 555.Kyong C.U., Galbraith G., Fudenberg H. H., The Effects of Isoprinosine in a Patient with Ataxia Telangiectasia. Pediatric Research, 1985. 19(4): p. A277–A277. [Google Scholar]
- 556.Gelfand E.W., Minto H., Mensah K., Reynolds P. R., Meffre E., Rubtsov K., A novel atm mutation associated with elevated atypical lymphocyte populations, hyper-IgM, and cutaneous granulomas. Journal of Clinical Immunology, 2018. Conference: p. 2018 CIS Annual Meeting: Immune Deficiency and Dysregulation North American Conference. Canada. 38 (3) (pp 431–432). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 557.Chung E.O., Bodensteiner J. B., Noorani P. A., Schochet S. S. Jr., Cerebral white-matter changes suggesting leukodystrophy in ataxia telangiectasia. Journal of Child Neurology, 1994. 9(1): p. 31–5. doi: 10.1177/088307389400900106 [DOI] [PubMed] [Google Scholar]
- 558.Jin J.J., Smith M. J., Lagerstedt S. A., Cousin M. A., Boczek N. J., Klee E. W., et al., Flow Cytometry-Based Radiosensitivity Assay: Application in Patient with Heterozygous Atm Mutation and Clinical Ataxia Telangiectasia Phenotype. Journal of Clinical Immunology, 2016. 36(3): p. 246–246. [Google Scholar]
- 559.Bechis M., et al., Severe combined immune deficiency (SCID): Need for universal newborn screening (NBS) in pennsylvania (PA). Journal of Clinical Immunology, 2017. Conference: p. 2017 CIS Annual Meeting: Immune Deficiency and Dysregulation North American Conference. United States. 37 (2) (pp 258). [Google Scholar]
- 560.Shaham M., Voss R., Becker Y., Yarkoni S., Ornoy A., Kohn G., Prenatal diagnosis of ataxia telangiectasia. Journal of Pediatrics, 1982. 100(1): p. 134–7. doi: 10.1016/s0022-3476(82)80253-9 [DOI] [PubMed] [Google Scholar]
- 561.Barmettler S., et al., Functional Confirmation of DNA Repair Defect in Ataxia Telangiectasia (AT) Infants Identified by Newborn Screening for Severe Combined Immunodeficiency (NBS SCID). J Allergy Clin Immunol Pract, 2021. 9(2): p. 723–732.e3. doi: 10.1016/j.jaip.2020.08.008 [DOI] [PubMed] [Google Scholar]
- 562.Ziino O., Rondelli R., Micalizzi C., Luciani M., Conter V., Arico M., Acute lymphoblastic leukemia in children with associated genetic conditions other than Down’s syndrome. The AIEOP experience. Haematologica, 2006. 91(1): p. 139–40. [PubMed] [Google Scholar]
- 563.Gazulla J., Benavente I., Sarasa Barrio M., [Adult-onset ataxia-telangiectasia. A clinical and therapeutic observation]. Neurologia, 2006. 21(8): p. 447–51. [PubMed] [Google Scholar]
- 564.Stray-Pedersen A., Borresen-Dale A. L., Paus E., Lindman C. R., Burgers T., Abrahamsen T. G., Alpha fetoprotein is increasing with age in ataxia-telangiectasia. European Journal of Paediatric Neurology, 2007. 11(6): p. 375–80. doi: 10.1016/j.ejpn.2007.04.001 [DOI] [PubMed] [Google Scholar]
- 565.Nissenkorn A., Levi Y., Vilozni D., Hassin S., Menascu S., Ben-Zeev B., Amantadine Sulfate for Treatment of Movement Disorder in Ataxia-Telangiectasia. Annals of Neurology, 2010. 68(4): p. S115–S115. [Google Scholar]
- 566.Terasawa K., et al., Ataxia Telangiectasia—Reduced Pyruvate-Dehydrogenase Activity with Lipid Storage in Type-1 Muscle-Fibers. Brain & Development, 1984. 6(2): p. 257–257. [Google Scholar]
- 567.Guenther D.M., Smith W. B., Wara W. W., Santora T. R., Sachs R. L., Kronish D. T., et al., Ataxia Telangiectasia with Burkitts-Lymphoma. Journal of Allergy and Clinical Immunology, 1979. 63(3): p. 189–189. [Google Scholar]
- 568.Cox R., Hosking G. P., Wilson J., Ataxia telangiectasia. Evaluation of radiosensitivity in cultured skin fibroblasts as a diagnostic test. Archives of Disease in Childhood, 1978. 53(5): p. 386–90. doi: 10.1136/adc.53.5.386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 569.Kumar N., Aggarwal P., Dev N., Kumar G., Ataxia telangiectasia: learning from previous mistakes. BMJ Case Reports, 2012. 14: p. 14. doi: 10.1136/bcr-2012-007246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 570.Huang K.Y., Shyur S. D., Wang C. Y., Shen E. Y., Liang D. C., Ataxia telangiectasia: report of two cases. Journal of Microbiology, Immunology & Infection, 2001. 34(1): p. 71–5. [PubMed] [Google Scholar]
- 571.Valbuena O., Poo P., Campistol J., Vernet A., Fernandez-Alvarez E., Sierra I., et al., [Ataxia telangiectasia: review of 13 new cases]. Revista de Neurologia, 1996. 24(125): p. 77–80. [PubMed] [Google Scholar]
- 572.Centerwall W.R., Miller M. M., Ataxia, telangiectasia, and sinopulmonary infections; a syndrome of slowly progressive deterioration in childhood. A.M.A. Journal of Diseases of Children, 1958. 95(4): p. 385–96. doi: 10.1001/archpedi.1958.02060050387007 [DOI] [PubMed] [Google Scholar]
- 573.Boder E., Sedgewick R., Ataxia-Telangiectasia—a Familial Syndrome of Progressive Cerebellar Ataxia, Oculocutaneous Telangiectasia, and Frequent Pulmonary Infection. Archives of Dermatology, 1958. 78(3): p. 402–405. [PubMed] [Google Scholar]
- 574.Toledano S.R., Lange B. J., Ataxia-telangiectasia and acute lymphoblastic leukemia. Cancer, 1980. 45(7): p. 1675–8. doi: [DOI] [PubMed] [Google Scholar]
- 575.Sugimoto T., Kidowaki T., Sawada T., Ohtsukaurano T., Kusunoki T., Ataxia-Telangiectasia Associated with Non-T, Non-B Cell Acute Lymphocytic-Leukemia. Acta Paediatrica Scandinavica, 1982. 71(3): p. 509–510. doi: 10.1111/j.1651-2227.1982.tb09462.x [DOI] [PubMed] [Google Scholar]
- 576.Jeddane L., Ailal F., Dubois-D’Enghien C., Abidi O., Benhsaien I., Kili A., et al., Ataxia-telangiectasia in Moroccan patients. Journal of Clinical Immunology, 2014. Conference: p. 16th Biennial Meeting of the European Society for Immunodeficiency, ESID 2014. Prague Czech Republic. Conference Publication: (var.pagings). 34 (2 SUPPL. 1) (pp S452–S453). [Google Scholar]
- 577.Pietrucha B.M., Heropolitanska-Pliszka E., Wakulinska A., Skopczynska H., Gatti R. A., Bernatowska E., Ataxia-telangiectasia with hyper-IgM and Wilms tumor: fatal reaction to irradiation. Journal of Pediatric Hematology/Oncology, 2010. 32(1): p. e28–30. doi: 10.1097/MPH.0b013e3181bfd3d9 [DOI] [PubMed] [Google Scholar]
- 578.Beatty D.W., Arens L.J., and Nelson M.M., Ataxia-telangiectasia. X,14 translocation, progressive deterioration of lymphocyte numbers and function, and abnormal in vitro immunoglobulin production. South African Medical Journal. Suid-Afrikaanse Tydskrif Vir Geneeskunde, 1986. 69(2): p. 115–8. [PubMed] [Google Scholar]
- 579.Yanofsky R.A., Seshia S. S., Dawson A. J., Stobart K., Greenberg C. R., Booth F. A., et al., Ataxia-telangiectasia: atypical presentation and toxicity of cancer treatment. Canadian Journal of Neurological Sciences, 2009. 36(4): p. 462–7. doi: 10.1017/s0317167100007794 [DOI] [PubMed] [Google Scholar]
- 580.Mitui M., et al., ATM gene founder haplotypes and associated mutations in Polish families with ataxia-telangiectasia. Annals of Human Genetics, 2005. 69(Pt 6): p. 657–64. doi: 10.1111/j.1529-8817.2005.00199.x [DOI] [PubMed] [Google Scholar]
- 581.Willems P.J., Van Roy B. C., Kleijer W. J., Van der Kraan M., Martin J. J., Atypical clinical presentation of ataxia telangiectasia. American Journal of Medical Genetics, 1993. 45(6): p. 777–82. doi: 10.1002/ajmg.1320450624 [DOI] [PubMed] [Google Scholar]
- 582.Noroski L.M., Rosenblatt H. M., Hanson I. C., Abramson S. L., Paul M. E., Shearer W. T., Atypical presentation of ataxia-telangiectasia (AT) with features of non-x-linked HyperIgM (HIGM). Journal of Allergy and Clinical Immunology, 1996. 97(1): p. 844–844. [Google Scholar]
- 583.Gioia L.V., Bonsall D., Moffett K., Leys M., Bilateral maculopathy in a patient with ataxia telangiectasia. Journal of Aapos: American Association for Pediatric Ophthalmology & Strabismus, 2016. 20(1): p. 85–8. [DOI] [PubMed] [Google Scholar]
- 584.Friend D., Hadjivassiliou M., and Baxter P., BPNSU study of chronic childhood ataxia in the UK and Ireland. Developmental Medicine and Child Neurology, 2013. Conference: p. 2013 Annual Meeting of the British Paediatric Neurology Association. Manchester United Kingdom. Conference Publication: (var.pagings). 55 (SUPPL. 1) (pp 2). [DOI] [PubMed] [Google Scholar]
- 585.Lin D.D., Barker P. B., Lederman H. M., Crawford T. O., Cerebral abnormalities in adults with ataxia-telangiectasia. Ajnr: American Journal of Neuroradiology, 2014. 35(1): p. 119–23. doi: 10.3174/ajnr.A3646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 586.Mutlu-Albayrak H., Kirat E., and Gurbuz G., Childhood-onset autosomal recessive ataxias: a cross-sectional study from Turkey. Neurogenetics, 2020. 21(1): p. 59–66. doi: 10.1007/s10048-019-00597-y [DOI] [PubMed] [Google Scholar]
- 587.Marchetti F., Businco L., Finocchi M., Clinical and immunological observations in 13 patients suffering from ataxia-telangiectasia. Folia Allergologica et Immunologica Clinica, 1977. 24(6): p. 598–601. [Google Scholar]
- 588.Lukanov T., Nedkova V., Gecheva S., Veleva G., Slavcheva V., Clinical case of a child with ataxia-telangiectasia. Pediatriya, 2009. 49(1): p. 47–50+6. [Google Scholar]
- 589.Fuhrmann E., Pfeiffer L., Zschenderlein R., Leonhardt T., Melster U., Kolmel H. W., [Clinico-genetic diagnosis of ataxia telangiectatica (Louis-Bar syndrome)]. Nervenarzt, 1993. 64(2): p. 140–2. [PubMed] [Google Scholar]
- 590.Hoche F., Frankenberg E., Rambow J., Theis M., Harding J. A., Qirshi M., et al., Cognitive phenotype in ataxia-telangiectasia. Pediatric Neurology, 2014. 51(3): p. 297–310. doi: 10.1016/j.pediatrneurol.2014.04.027 [DOI] [PubMed] [Google Scholar]
- 591.Young R., Davis P., Schomer M., Tucker J., Compound Heterozygotes with Three Disparate Orphan Diseases: Pyridoxine Dependent Epilepsy, Ataxia Telangiectasia, and Tay Sachs Disease. Neurology, 2018. Conference: p. 70th Annual Meeting of the American Academy of Neurology, AAN 2018. United States. 90 (15 Supplement 1) (no pagination). [Google Scholar]
- 592.Cabana M.D., Crawford T. O., Winkelstein J. A., Christensen J. R., Lederman H. M., Consequences of the delayed diagnosis of ataxia-telangiectasia. Pediatrics, 1998. 102(1 Pt 1): p. 98–100. doi: 10.1542/peds.102.1.98 [DOI] [PubMed] [Google Scholar]
- 593.Demaerel P., Kendall B. E., Kingsley D., Cranial CT and MRI in diseases with DNA repair defects. Neuroradiology, 1992. 34(2): p. 117–21. doi: 10.1007/BF00588156 [DOI] [PubMed] [Google Scholar]
- 594.Okano M., Sakiyama Y., Matsumoto S., Mizuno F., Osato T., Decreased cytoplasmic immunoglobulin A production during Epstein-Barr virus immortalization on lymphocytes from patients with ataxia-telangiectasia. Journal of Clinical Laboratory Analysis, 1995. 9(1): p. 77–9. doi: 10.1002/jcla.1860090115 [DOI] [PubMed] [Google Scholar]
- 595.Waldmann T.A., Broder S., Goldman C. K., Frost K., Korsmeyer S. J., Medici M. A., Disorders of B cells and helper T cells in the pathogenesis of the immunoglobulin deficiency of patients with ataxia telangiectasia. Journal of Clinical Investigation, 1983. 71(2): p. 282–95. doi: 10.1172/jci110768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 596.Shaikh A.G., Marti S., Tarnutzer A. A., Palla A., Crawford T. O., Zee D. S., et al., Effects of 4-aminopyridine on nystagmus and vestibulo-ocular reflex in ataxia-telangiectasia. Journal of Neurology, 2013. 260(11): p. 2728–35. doi: 10.1007/s00415-013-7046-4 [DOI] [PubMed] [Google Scholar]
- 597.Broccoletti T., Del Giudice E., Cirillo E., Vigliano I., Giardino G., Ginocchio V. M., et al., Efficacy of very-low-dose betamethasone on neurological symptoms in ataxia-telangiectasia. European Journal of Neurology, 2011. 18(4): p. 564–70. doi: 10.1111/j.1468-1331.2010.03203.x [DOI] [PubMed] [Google Scholar]
- 598.Ammann A.J., Duquesnoy R. J., Good R. A., Endocrinological studies in ataxiatelangiectasia and other immunological deficiency diseases. Clinical & Experimental Immunology, 1970. 6(4): p. 587–95. [PMC free article] [PubMed] [Google Scholar]
- 599.Huang Y., Yang L., Wang J., Yang F., Xiao Y., Xia R., et al., Erratum: Twelve novel atm mutations identified in chinese ataxia telangiectasia patients (NeuroMolecular Medicine (2013) 15 (536–540) doi: 10.1007/s12017-013-8240-3). NeuroMolecular Medicine, 2014. 16(1): p. 216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 600.Fievet A., et al., Functional classification of ATM variants in ataxia-telangiectasia patients. Hum Mutat, 2019. 40(10): p. 1713–1730. doi: 10.1002/humu.23778 [DOI] [PubMed] [Google Scholar]
- 601.Mesci L., et al., H2AX gene does not have a modifier effect on ataxia-telangiectasia phenotype. International Journal of Immunogenetics, 2011. 38(3): p. 209–13. doi: 10.1111/j.1744-313X.2010.00989.x [DOI] [PubMed] [Google Scholar]
- 602.Amirmoini M., Chavoshzadeh Z., Mansouri M., Armin S., Fahimzad A., Hyper IGM syndrome as a presenting sign of ataxia telangiectasia and A.T like diseases (report of three cases). Journal of Clinical Immunology, 2014. Conference: p. 100th J Project Meeting. Antalya Turkey. Conference Publication: (var.pagings). 34 (6) (pp 720–721). [Google Scholar]
- 603.Golomb A., Sandbank U., Letter: Negri bodies in a case of ataxia telangiectasia. Archives of Neurology, 1976. 33(4): p. 306. [DOI] [PubMed] [Google Scholar]
- 604.Taylor M.J., Chan-Lui W. Y., Logan W. J., Longitudinal evoked potential studies in hereditary ataxias. Canadian Journal of Neurological Sciences, 1985. 12(2): p. 100–5. doi: 10.1017/s0317167100046783 [DOI] [PubMed] [Google Scholar]
- 605.Bearzoti P., Abreu J. M. Q., Maudonnet O. Q., The Louis-Bar syndrome: Ataxia—Telangiectasia. Revista Brasileira de Oftalmologia, 1978. 37(4): p. 489–494. [Google Scholar]
- 606.Sahama I., Sinclair K., Fiori S., Doecke J., Pannek K., Reid L., et al., Motor pathway degeneration in young ataxia telangiectasia patients: A diffusion tractography study. NeuroImage Clinical, 2015. 9: p. 206–15. doi: 10.1016/j.nicl.2015.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 607.Shaikh A.G., Crawford T. O., Zee D. S., Jinnah H. A., Movement disorders in ataxia-telangiectasia. Movement Disorders, 2009. 24: p. S21–S22. [Google Scholar]
- 608.Elfaituri S.S., Matoug I., Elsalheen H., Belrasali Y., Emaetig F., Mucocutaneous leishmaniasis in an 11-year-old girl with ataxia telangectasia—case report. Libyan Journal of Medicine, 2015. 10: p. 26432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 609.Jiang H., Tang B., Xia K., Hu Z., Shen L., Tang J., et al., Mutation analysis of the ATM gene in two Chinese patients with ataxia telangiectasia. Journal of the Neurological Sciences, 2006. 241(1–2): p. 1–6. doi: 10.1016/j.jns.2005.09.001 [DOI] [PubMed] [Google Scholar]
- 610.Demuth I., Dutrannoy V., Marques W. Jr., Neitzel H., Schindler D., Dimova P. S., et al., New mutations in the ATM gene and clinical data of 25 AT patients. Neurogenetics, 2011. 12(4): p. 273–82. doi: 10.1007/s10048-011-0299-0 [DOI] [PubMed] [Google Scholar]
- 611.Riise R., Ygge J., Lindman C., Stray-Pedersen A., Bek T., Rodningen O. K., et al., Ocular findings in Norwegian patients with ataxia-telangiectasia: a 5 year prospective cohort study. Acta Ophthalmologica Scandinavica, 2007. 85(5): p. 557–62. doi: 10.1111/j.1600-0420.2007.00890.x [DOI] [PubMed] [Google Scholar]
- 612.Gungor T., Buhring I., Cremer R., Gartenschlager M., Zielen S., [Pathogenesis, diagnosis, clinical and therapeutic aspects of ataxia telangiectasia]. Klinische Padiatrie, 1997. 209(5): p. 328–35. doi: 10.1055/s-2008-1043972 [DOI] [PubMed] [Google Scholar]
- 613.Rajoor U.G., Kashinakunti M. D., Progressive ataxia in an 11 year child—A case report. Indian Journal of Public Health Research and Development, 2013. 4(1): p. 208–210. [Google Scholar]
- 614.Burkhardt B., Modlich S., Meyer U., Moricke A., Bienemann K., Mauz-Korholz C., et al., Promising therapy results for lymphoid malignancies in children with chromosomal breakage syndromes (Ataxia teleangiectasia or Nijmegen-breakage syndrome): A retrospective survey. British Journal of Haematology, 2011. 155(4): p. 468–476. doi: 10.1111/j.1365-2141.2011.08863.x [DOI] [PubMed] [Google Scholar]
- 615.Dmenska H., Pietrucha B., Heropolitanska-Pliszka E., Pulmonary manifestations in patients with ataxia—telangiectasia [A-T]. European Respiratory Journal, 2017. 50. [Google Scholar]
- 616.Firat A.K., Karakas H. M., Firat Y., Yakinci C., Quantitative evaluation of brain involvement in ataxia telangiectasia by diffusion weighted MR imaging. European Journal of Radiology, 2005. 56(2): p. 192–6. doi: 10.1016/j.ejrad.2005.04.009 [DOI] [PubMed] [Google Scholar]
- 617.Kaur N., Campbell D., Mehr S., A rare case of pulmonary lymphomatoid granulomatosis in a patient with ataxia telangiectasia. Internal Medicine Journal, 2017. Conference: p. 28th Annual Conference of the Australasian Society of Clinical Immunology and Allergy, ASCIA 2017. New Zealand. 47 (Supplement 5) (pp 38). [Google Scholar]
- 618.Kretschmer R.R., Lopez Osuna M., Valenzuela R. H., Reversible neutrophil defect in ataxia telangiectasia. Pediatrics, 1972. 50(1): p. 147–50. [PubMed] [Google Scholar]
- 619.Quarantelli M., Giardino G., Prinster A., Aloj G., Carotenuto B., Cirillo E., et al., Steroid treatment in Ataxia-Telangiectasia induces alterations of functional magnetic resonance imaging during prono-supination task. European Journal of Paediatric Neurology, 2013. 17(2): p. 135–40. doi: 10.1016/j.ejpn.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 620.Broccoletti T., Del Giudice E., Amorosi S., Russo I., Di Bonito M., Imperati F., et al., Steroid-induced improvement of neurological signs in ataxia-telangiectasia patients. European Journal of Neurology, 2008. 15(3): p. 223–8. doi: 10.1111/j.1468-1331.2008.02060.x [DOI] [PubMed] [Google Scholar]
- 621.Kang E., Jung J. W., Sugammadex reversal of rocuronium-induced neuromuscular block in a patient with ataxia-telangiectasia. Rawal Medical Journal, 2015. 40(4): p. 486–488. [Google Scholar]
- 622.Tachi N., Fujiwara M., Wagatsuma K., Motomura S., Nakao T., Sural Nerve Findings of 2 Cases with Ataxia-Telangiectasia. Brain & Development, 1983. 5(2): p. 172–172. [Google Scholar]
- 623.Sugie H., et al., Therapeutic trial of TRH in cerebellar ataxia in childhood. Brain and Development, 1980. 2(3): p. 270. [Google Scholar]
- 624.Watson H.G., et al., Transfusion-associated graft-versus-host disease in ataxia telangiectasia. Lancet, 1997. 349(9046): p. 179. doi: 10.1016/s0140-6736(05)60980-4 [DOI] [PubMed] [Google Scholar]
- 625.Meister M.T., Voss S., Schwabe D., Treatment of EBV-associated nodular sclerosing Hodgkin lymphoma in a patient with ataxia telangiectasia with brentuximab vedotin and reduced COPP plus rituximab. Pediatric Blood & Cancer, 2015. 62(11): p. 2018–20. [DOI] [PubMed] [Google Scholar]
- 626.Sandoval C., Swift M., Treatment of lymphoid malignancies in patients with ataxia-telangiectasia. Medical & Pediatric Oncology, 1998. 31(6): p. 491–7. doi: [DOI] [PubMed] [Google Scholar]
- 627.Jiang H., Tang B. S., Hu Z. M., Xia K., Xu B., Tang J. G., Research on clinical characteristics and ATM gene mutations in Chinese patients with ataxiatelangiectasia. National Medical Journal of China, 1117. 85(16): p. 1117–1120. [PubMed] [Google Scholar]
- 628.Kelaidi C., Tzotzola V., and Polychronopoulou S., The paradigm of hematological malignant versus non-malignant manifestations, driven by primary immunodeficiencies: a complex interplay. Fam Cancer, 2021. 20(4): p. 363–380. doi: 10.1007/s10689-021-00266-w [DOI] [PubMed] [Google Scholar]
- 629.Khan N.C., et al., Free-Living Motor Activity Monitoring in Ataxia-Telangiectasia. Cerebellum, 2021: p. 1–12. doi: 10.1007/s12311-020-01184-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 630.Nunez-Nunez M.E., et al., Survival of pediatric patients with primary immunodeficiencies in a public hospital in Western Mexico. Archivos Argentinos de Pediatria, 2021. 119(3): p. 202–207. doi: 10.5546/aap.2021.eng.202 [DOI] [PubMed] [Google Scholar]
- 631.Soler J.A., Pulido S.A., and Cordero R.H.A., Ataxia Telangiectasia: A View from the Lung. American Journal of Respiratory and Critical Care Medicine, 2020. 201. [Google Scholar]
- 632.Chaiban R., Tarabishy A., Yilmaz Demirdag Y., A rare cns complication of ataxia telangiectasia. Annals of Allergy, Asthma and Immunology, 2013. Conference: p. 2013 Annual Meeting of the American College of Allergy, Asthma and Immunology. Baltimore, MD United States. Conference Publication: (var.pagings). 111 (5 SUPPL. 1) (pp A64). [Google Scholar]
- 633.Battisti C., Formichi P., Federico A., Vitamin E serum levels are normal in ataxia telangiectasia (Louis-Bar disease). Journal of the Neurological Sciences, 1996. 141(1–2): p. 114–6. doi: 10.1016/0022-510x(96)00158-x [DOI] [PubMed] [Google Scholar]
- 634.Amariglio N., Hirshberg A., Scheithauer B. W., Cohen Y., Loewenthal R., Trakhtenbrot L., et al., Donor-derived brain tumor following neural stem cell transplantation in an ataxia telangiectasia patient. PLoS Medicine / Public Library of Science, 2009. 6(2): p. e1000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 635.Felix E., Gimenes A. C., Costa-Carvalho B. T., Effects of inspiratory muscle training on lung volumes, respiratory muscle strength, and quality of life in patients with ataxia telangiectasia. Pediatric Pulmonology, 2014. 49(3): p. 238–44. doi: 10.1002/ppul.22828 [DOI] [PubMed] [Google Scholar]
- 636.Nissenkorn A., Levy-Shraga Y., Banet-Levi Y., Lahad A., Sarouk I., Modan-Moses D., Endocrine abnormalities in ataxia telangiectasia: findings from a national cohort. Pediatric Research, 2016. 79(6): p. 889–94. doi: 10.1038/pr.2016.19 [DOI] [PubMed] [Google Scholar]
- 637.Vilozni D., Lavie M., Sarouk I., Bar-Aluma B. E., Dagan A., Ashkenazi M., et al., FVC deterioration, airway obstruction determination, and life span in Ataxia telangiectasia. Respiratory Medicine, 2015. 109(7): p. 890–6. doi: 10.1016/j.rmed.2015.05.013 [DOI] [PubMed] [Google Scholar]
- 638.Vilozni D., Lavie M., Sarouk I., Bar Aluma B. E., Dagan A., Levi Y., et al., Late-breaking abstract: The Effect of lung volume deterioration on tidal volume, airway flows and life span in ataxia telangiectasia. European Respiratory Journal, 2014. Conference: p. European Respiratory Society Annual Congress 2014. Munich Germany. Conference Publication: (var.pagings). 44 (SUPPL. 58) (no pagination). [Google Scholar]
- 639.McGrath-Morrow S.A., Sterni L., McGinley B., Lefton-Greif M. A., Rosquist K., Lederman H., Polysomnographic values in adolescents with ataxia telangiectasia. Pediatric Pulmonology, 2008. 43(7): p. 674–9. doi: 10.1002/ppul.20838 [DOI] [PubMed] [Google Scholar]
- 640.Chang Y., et al., Ataxia Telangiectasia with Recurrent urinary tract infections and Sepsis. Journal of Clinical Immunology, 2020. 40(SUPPL 1): p. S150–S150. [Google Scholar]
- 641.Woelke S., et al., Altered Cerebrospinal Fluid (CSF) in Children with Ataxia Telangiectasia. Cerebellum, 2021. 20(1): p. 31–40. doi: 10.1007/s12311-020-01175-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 642.Wölke S., et al., Immune competence and respiratory symptoms in patients with ataxia telangiectasia: A prospective follow-up study. Clin Immunol, 2020. 217: p. 108491. doi: 10.1016/j.clim.2020.108491 [DOI] [PubMed] [Google Scholar]
- 643.Zaki-Dizaji M., et al., Dystonia in Ataxia Telangiectasia: A Case Report with Novel Mutations. Oman Med J, 2020. 35(1): p. e93. doi: 10.5001/omj.2020.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 644.Speers L., Al-Sayegh H., Parveen S., The effect of ataxia telangiectasia in pregnancy and delivery: A case report. BJOG: An International Journal of Obstetrics and Gynaecology, 2013. Conference: p. RCOG World Congress 2013. Liverpool United Kingdom. Conference Publication: (var.pagings). 120 (SUPPL. 1) (pp 60). [Google Scholar]
- 645.Iodice A., Galli J., Molinaro A., Franzoni A., Micheli R., Pinelli L., et al., Neurovisual Assessment in Children with Ataxia Telangiectasia. Neuropediatrics, 2018. 49(1): p. 26–34. doi: 10.1055/s-0037-1607216 [DOI] [PubMed] [Google Scholar]
- 646.Farr A.K., Shalev B., Crawford T. O., Lederman H. M., Winkelstein J. A., Repka M. X., Ocular manifestations of ataxia-telangiectasia. American Journal of Ophthalmology, 2002. 134(6): p. 891–6. doi: 10.1016/s0002-9394(02)01796-8 [DOI] [PubMed] [Google Scholar]
- 647.Spang S., Lindermuth R., Kasmann B., Ruprecht K. W., Clinical Aspects of Ataxia-Telangiectasia (Louis-Bar Syndrome). Klinische Monatsblatter Fur Augenheilkunde, 1995. 206(4): p. 273–276. doi: 10.1055/s-2008-1035439 [DOI] [PubMed] [Google Scholar]
- 648.Pascualpascual S.I., Pascualcastroviejo I., Fontan G., Lopezmartin V., Ataxia-Telangiectasia (a-T)—Contribution with 18 Personal Cases. Brain & Development, 1981. 3(3): p. 289–296. [DOI] [PubMed] [Google Scholar]
- 649.Shaikh A.G., Marti S., Tarnutzer A. A., Palla A., Crawford T. O., Straumann D., et al., Gaze fixation deficits and their implication in ataxia-telangiectasia. Journal of Neurology, Neurosurgery & Psychiatry, 2009. 80(8): p. 858–64. doi: 10.1136/jnnp.2008.170522 [DOI] [PubMed] [Google Scholar]
- 650.Harris C.M., Shawkat F., Russell-Eggitt I., Wilson J., Taylor D., Intermittent horizontal saccade failure (’ocular motor apraxia’) in children. British Journal of Ophthalmology, 1996. 80(2): p. 151–8. doi: 10.1136/bjo.80.2.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 651.Zamora C., Yahyavi-Firouz-Abadi N., Kuyumcu G., Kontzialis M., Magnetic resonance imaging of ataxia-telangiectasia. Neurology India, 2016. 64(pp S129). doi: 10.4103/0028-3886.178058 [DOI] [PubMed] [Google Scholar]
- 652.Lewis R.F., Crawford T. O., Slow target-directed eye movements in ataxia-telangiectasia. Investigative Ophthalmology & Visual Science, 2002. 43(3): p. 686–91. [PubMed] [Google Scholar]
- 653.Pommerening H., van Dullemen S., Kieslich M., Schubert R., Zielen S., Voss S., Body composition, muscle strength and hormonal status in patients with ataxia telangiectasia: a cohort study. Orphanet Journal Of Rare Diseases, 2015. 10: p. 155. doi: 10.1186/s13023-015-0373-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 654.Lefton-Greif M.A., Perlman A. L., He X., Lederman H. M., Crawford T. O., Assessment of impaired coordination between respiration and deglutition in children and young adults with ataxia telangiectasia. Developmental Medicine & Child Neurology, 2016. 58(10): p. 1069–75. doi: 10.1111/dmcn.13156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 655.Paulino T.L., Rafael M. N., Hix S., Ajzen S. A., de Souza F. I. S., Kochi C., et al., Risk of Atherosclerosis and Diabetes in Patients with Ataxia Telangiectasia. Journal of Clinical Immunology, 2015. 35: p. S28–S28. [Google Scholar]
- 656.Velazquez-Perez L., et al., Hereditary Ataxias in Cuba: A Nationwide Epidemiological and Clinical Study in 1001 Patients. Cerebellum, 2020. 19(2): p. 252–264. doi: 10.1007/s12311-020-01107-9 [DOI] [PubMed] [Google Scholar]
- 657.Tsukahara M., Masuda M., Ohshiro K., Kobayashi K., Kajii T., Ejima Y., et al., Ataxia telangiectasia with generalized skin pigmentation and early death. European Journal of Pediatrics, 1986. 145(1–2): p. 121–4. doi: 10.1007/BF00441871 [DOI] [PubMed] [Google Scholar]
- 658.de Araujo A.C., de los Santos-Fortuna E., Carneiro-Sampaio M. M., Grumach A. S., Primary immunodeficiency diseases: a presentation of 6 cases. Brazilian Journal of Medical & Biological Research, 1988. 21(5): p. 915–7. [PubMed] [Google Scholar]
- 659.Judge S.J.P., Trevor A.; Bateni, Cyrus P.; Darrow, Morgan A; Evans, Christopher P.; Canter, Robert J., Retroperitoneal extramedullary hematopoietic pseudotumor in ataxia-telangiectasia. Rare tumors, 2018. doi: 10.1177/2036361318789724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 660.Dooling E.C., Schoene W. C., Richardson E. P., Ataxia-Telangiectasia—Clinicopathological Findings. Journal of Neuropathology and Experimental Neurology, 1978. 37(5): p. 608–608. [Google Scholar]
- 661.Kieslich M., Hoche F., Reichenbach J., Weidauer S., Porto L., Vlaho S., et al., Extracerebellar MRI-lesions in ataxia telangiectasia go along with deficiency of the GH/IGF-1 axis, markedly reduced body weight, high ataxia scores and advanced age. Cerebellum, 2010. 9(2): p. 190–7. doi: 10.1007/s12311-009-0138-0 [DOI] [PubMed] [Google Scholar]
- 662.Churchyard A., Stell R., Mastaglia F. L., Ataxia telangiectasia presenting as an extrapyramidal movement disorder and ocular motor apraxia without overt telangiectasia. Clinical & Experimental Neurology, 1991. 28: p. 90–6. [PubMed] [Google Scholar]
- 663.Koepp M., Schelosky L., Cordes I., Cordes M., Poewe W., Dystonia in ataxia telangiectasia: report of a case with putaminal lesions and decreased striatal [123I]iodobenzamide binding. Movement Disorders, 1994. 9(4): p. 455–9. doi: 10.1002/mds.870090414 [DOI] [PubMed] [Google Scholar]
- 664.Sanger T.D. and Ferman D., Similarity of Involuntary Postures between Different Children with Dystonia. Movement Disorders Clinical Practice, 2017. 4(6): p. 870–874. doi: 10.1002/mdc3.12533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 665.Shaikh A.G., Zee D. S., Mandir A. S., Lederman H. M., Crawford T. O., Disorders of Upper Limb Movements in Ataxia-Telangiectasia. PLoS ONE [Electronic Resource], 2013. 8(6): p. e67042. doi: 10.1371/journal.pone.0067042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 666.Shaikh A.G., Zee D. S., Meyer A. E., Lederman H. M., Crawford T. O., Involuntary movements in ataxia-telangiectasia: Natural history and quantitative characteristics. Movement Disorders, 2007. 22: p. S13–S13. [Google Scholar]
- 667.Keene E.J., Diagnostic dental radiographs not allowed! A child with ataxia telangiectasia. European Archives of Paediatric Dentistry: Official Journal of the European Academy of Paediatric Dentistry, 2014. 15(1): p. 55–7. [DOI] [PubMed] [Google Scholar]
- 668.Kutluk M.T., Yalcin B., Buyukpamukcu M., Ataxia telangiectasia and Hodgkin disease. Medical & Pediatric Oncology, 2000. 35(5): p. 509. doi: [DOI] [PubMed] [Google Scholar]
- 669.Amromin G.D., Boder E., Teplitz R., Ataxia-telangiectasia with a 32 year survival. A clinicopathological report. Journal of Neuropathology & Experimental Neurology, 1979. 38(6): p. 621–43. doi: 10.1097/00005072-197911000-00007 [DOI] [PubMed] [Google Scholar]
- 670.Agamanolis D.P., Greenstein J. I., Ataxia-telangiectasia. Report of a case with Lewy bodies and vascular abnormalities within cerebral tissue. Journal of Neuropathology & Experimental Neurology, 1979. 38(5): p. 475–89. doi: 10.1097/00005072-197909000-00003 [DOI] [PubMed] [Google Scholar]
- 671.Habek M., Brinar V. V., Rados M., Zadro I., Zarkovic K., Brain MRI abnormalities in ataxia-telangiectasia. Neurologist, 2008. 14(3): p. 192–5. doi: 10.1097/NRL.0b013e31815fa5a7 [DOI] [PubMed] [Google Scholar]
- 672.Scharnetzky M., Kohlschutter A., Krtsch H., Computerized tomographic findings in a case of ataxia-telangiectasia (Louis-Bar syndrome). Neuropediatrics, 1980. 11(4): p. 384–7. doi: 10.1055/s-2008-1071405 [DOI] [PubMed] [Google Scholar]
- 673.Sardanelli F., Parodi R. C., Ottonello C., Renzetti P., Saitta S., Lignana E., et al., Cranial MRI in ataxia-telangiectasia. Neuroradiology, 1995. 37(1): p. 77–82. doi: 10.1007/BF00588526 [DOI] [PubMed] [Google Scholar]
- 674.D’Arrigo S., Vigano L., Bruzzone M. G., Marzaroli M., Nikas I., Riva D., et al., Diagnostic approach to cerebellar disease in children. Journal of Child Neurology, 2005. 20(11): p. 859–866. doi: 10.1177/08830738050200110101 [DOI] [PubMed] [Google Scholar]
- 675.Al-Maawali A., Blaser S., Yoon G., Diagnostic approach to childhood-onset cerebellar atrophy: a 10-year retrospective study of 300 patients. Journal of Child Neurology, 2012. 27(9): p. 1121–32. doi: 10.1177/0883073812448680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 676.Gupta K., Rawat A., Agrawal P., Jindal A., Nada R., Saikia B., et al., Infectious and non-infectious complications in primary immunodeficiency disorders: An autopsy study from North India. Journal of Clinical Pathology, 2018. 71(5): p. 425–435. doi: 10.1136/jclinpath-2017-204708 [DOI] [PubMed] [Google Scholar]
- 677.Salman M.S., Chodirker B. N., Bunge M., Neuroimaging Findings and Repeat Neuroimaging Value in Pediatric Chronic Ataxia. Canadian Journal of Neurological Sciences, 2016. 43(6): p. 824–832. doi: 10.1017/cjn.2016.7 [DOI] [PubMed] [Google Scholar]
- 678.Wallet-Faber N., Bodemer C., Blanche S., Delabesse E., Eschard C., Brousse N., et al., Primary cutaneous Epstein-Barr virus-related lymphoproliferative disorders in 4 immunosuppressed children. Journal of the American Academy of Dermatology, 2008. 58(1): p. 74–80. doi: 10.1016/j.jaad.2007.08.013 [DOI] [PubMed] [Google Scholar]
- 679.Lin D.D., Crawford T. O., Lederman H. M., Barker P. B., Proton MR spectroscopic imaging in ataxia-telangiectasia. Neuropediatrics, 2006. 37(4): p. 241–6. doi: 10.1055/s-2006-924722 [DOI] [PubMed] [Google Scholar]
- 680.Wallis L.I., Griffiths P. D., Ritchie S. J., Romanowski C. A., Darwent G., Wilkinson I. D., Proton spectroscopy and imaging at 3T in ataxia-telangiectasia. Ajnr: American Journal of Neuroradiology, 2007. 28(1): p. 79–83. [PMC free article] [PubMed] [Google Scholar]
- 681.Osetowska E., Traczynska H., Sur l’ataxie avec télangiectasie, une observation anatomoclinique. Acta Neuropathologica, 1964. 3(4): p. 319–325. [DOI] [PubMed] [Google Scholar]
- 682.Dineen R.A., et al., Accumulation of Brain Hypointense Foci on Susceptibility-Weighted Imaging in Childhood Ataxia Telangiectasia. AJNR Am J Neuroradiol, 2021. 42(6): p. 1144–1150. doi: 10.3174/ajnr.A7107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 683.Dunn H.G., Nerve conduction studies in children with Friedreich’s ataxia and ataxia-telangiectasia. Developmental Medicine & Child Neurology, 1973. 15(3): p. 324–37. doi: 10.1111/j.1469-8749.1973.tb04889.x [DOI] [PubMed] [Google Scholar]
- 684.McKinney J.L. and Islam M.P., Neurophysiologic intraoperative monitoring (NIOM) in pediatric patients with polyneuropathy. Childs Nerv Syst, 2020. 36(11): p. 2801–2805. doi: 10.1007/s00381-020-04571-0 [DOI] [PubMed] [Google Scholar]
- 685.Rivat L., Ropartz C., Burtin P., Karitzky D., Abnormalities in synthesis of some subclasses of gamma-G in a family with two cases of ataxia telangiectasia. Vox Sanguinis, 1969. 17(1): p. 5–10. doi: 10.1111/j.1423-0410.1969.tb00536.x [DOI] [PubMed] [Google Scholar]
- 686.Ornellas L., Matos J., Carvalho B., Alteration of humoral and cellular immunity in patients with ataxia-telangiectasia at reference center in Sao Paulo, Brazil. World Allergy Organization Journal, 2012. Conference: p. 22nd World Allergy Congress. Cancun Mexico. Conference Publication: (var.pagings). 5 (SUPPL. 2) (pp S189). [Google Scholar]
- 687.Pyun K.H., Ochs H. D., Yang X., Wedgwood R. J., Antibody Deficiency in Ataxia Telangiectasia, a Defect in Heavy-Chain Constant Gene Rearrangement. Clinical Research, 1987. 35(1): p. A218–A218. [Google Scholar]
- 688.Ammann A.J., Hong R., Ataxia-Telangiectasia and Autoimmunity. Pediatric Research, 1970. 4(5): p. 435–&. [Google Scholar]
- 689.Diaconu G., Grigore I., Moisa S. M., Burlea M., [Ataxia-telangiectasia syndrome. Clinical and diagnostic aspects]. Revista Medico-Chirurgicala a Societatii de Medici Si Naturalisti Din Iasi, 2007. 111(2): p. 386–90. [PubMed] [Google Scholar]
- 690.Salinas F., Ortega G., Molina M., Garre J., Navarrete A., Pérez V., et al., Ataxia-telangiectasia with immunodeficiency and malignant lymphoma. Report of two cases. Medicina Clinica, 1981. 76(3): p. 109–112. [PubMed] [Google Scholar]
- 691.Hayakawa H., Kobayashi N., Blasts in Ataxia-Telangiectasia. Lancet, 1967. 1(7502): p. 1279–+. [Google Scholar]
- 692.Katsura T., Ohta S., Shimada M., Shima A., Chishiro H., Kasahara Y., Cell Biological Diagnosis of Ataxia-Telangiectasia. Brain & Development, 1984. 6(2): p. 236–236. [PubMed] [Google Scholar]
- 693.Jiang H., Tang B., Yan X., The clinical characteristic and diagnosis of 7 cases of ataxia- telangiectasia. Chinese Journal of Neurology, 2000. 33(2): p. 98–100. [Google Scholar]
- 694.Ghiasy S., Parvaneh L., Azizi G., Sadri G., Zaki Dizaji M., Abolhassani H., Aghamohammadi A., The clinical significance of complete class switching defect in Ataxia telangiectasia patients. Expert Review of Clinical Immunology, 2017. 13(5): p. 499–505. doi: 10.1080/1744666X.2017.1292131 [DOI] [PubMed] [Google Scholar]
- 695.Chiam L.Y., Verhagen M. M., Haraldsson A., Wulffraat N., Driessen G. J., Netea M. G., et al., Cutaneous granulomas in ataxia telangiectasia and other primary immunodeficiencies: reflection of inappropriate immune regulation? Dermatology, 2011. 223(1): p. 13–9. doi: 10.1159/000330335 [DOI] [PubMed] [Google Scholar]
- 696.Llamas B.A., Hernandez A. G., Diaz L., Descriptive analysis of the immunological behavior of patients with ataxia telangiectasia attended in the national institute of pediatrics in the past 30 years. World Allergy Organization Journal, 2012. Conference: p. 22nd World Allergy Congress. Cancun Mexico. Conference Publication: (var.pagings). 5 (SUPPL. 2) (pp S189). [Google Scholar]
- 697.Waldmann T.A., Broder S., Goldman C., Frost K., Medici M., Disorders of Immunoglobulin (Ig) Biosynthesis in Patients with Ataxia Telangiectasia (at). Clinical Research, 1982. 30(2): p. A564–A564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 698.Berkel A.I., Henle W., Henle G., Klein G., Ersoy F., Sanal O., Epstein-Barr virus-related antibody patterns in ataxia-telangiectasia. Clinical & Experimental Immunology, 1979. 35(2): p. 196–201. [PMC free article] [PubMed] [Google Scholar]
- 699.Bobba N., Kaplan M. S., Immunodeficiency and infections in ataxia-telangiectasia. Pediatrics, 2005. 116(2). [Google Scholar]
- 700.McFarlin D.E., Strober W., Wochner R. D., Waldmann T. A., Immunoglobulin A production in ataxia telangiectasia. Science, 1965. 150(3700): p. 1175–7. doi: 10.1126/science.150.3700.1175 [DOI] [PubMed] [Google Scholar]
- 701.Eidelman S., Davis S. D., Immunoglobulin Content of Intestinal Plasma Cells in Ataxia Telangiectasia. Journal of Clinical Investigation, 1967. 46(6): p. 1051–&. [Google Scholar]
- 702.Ammann A.J., Cain W. A., Ishizaka K., Hong R., Good R. A., Immunoglobulin E deficiency in ataxia-telangiectasia. New England Journal of Medicine, 1969. 281(9): p. 469–72. doi: 10.1056/NEJM196908282810904 [DOI] [PubMed] [Google Scholar]
- 703.Grumach A.S., Moraes-Vasconcelos D., Jacob C. M. A., Kok F., Duarte A. J. S., Immunological evaluation in Brazilian ataxia telangiectasia patients. Allergy and Clinical Immunology International, 2002. 14(3): p. 102–108. [Google Scholar]
- 704.Stray-Pedersen A., et al., The impact of an early truncating founder ATM mutation on immunoglobulins, specific antibodies and lymphocyte populations in ataxia-telangiectasia patients and their parents. Clinical & Experimental Immunology, 2004. 137(1): p. 179–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 705.Sanal O., Ersoy F., Yel L., Tezcan I., Metin A., Ozyurek H., et al., Impaired IgG antibody production to pneumococcal polysaccharides in patients with ataxia-telangiectasia. Journal of Clinical Immunology, 1999. 19(5): p. 326–34. doi: 10.1023/a:1020599810261 [DOI] [PubMed] [Google Scholar]
- 706.Schroeder S.A., Swift M., Sandoval C., Langston C., Interstitial lung disease in patients with ataxia-telangiectasia. Pediatric Pulmonology, 2005. 39(6): p. 537–43. doi: 10.1002/ppul.20209 [DOI] [PubMed] [Google Scholar]
- 707.Stobo J.D. and Tomasi T.B., A Low Molecular Weight Immunoglobulin Antigenically Related to Igm—Studies in Ataxia Telangiectasia. Arthritis and Rheumatism, 1966. 9(3): p. 543–&. [Google Scholar]
- 708.Kashiwa H., Kishi T., Kittaka E., Hyodo S., Karakawa T., Okada M., et al., Natural killer activity in two cases of ataxia telangiectasia. Acta Paediatrica Scandinavica, 1985. 74(5): p. 819–23. doi: 10.1111/j.1651-2227.1985.tb10042.x [DOI] [PubMed] [Google Scholar]
- 709.Shoimer I., Wright N., Haber R. M., Noninfectious Granulomas: A Sign of an Underlying Immunodeficiency? Journal of Cutaneous Medicine & Surgery, 2016. 20(3): p. 259–62. doi: 10.1177/1203475415626085 [DOI] [PubMed] [Google Scholar]
- 710.Stray-Pedersen A., Aaberge I. S., Fruh A., Abrahamsen T. G., Pneumococcal conjugate vaccine followed by pneumococcal polysaccharide vaccine; immunogenicity in patients with ataxia-telangiectasia. Clinical & Experimental Immunology, 2005. 140(3): p. 507–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 711.McGrath-Morrow S., Lefton-Greif M., Rosquist K., Crawford T., Kelly A., Zeitlin P., et al., Pulmonary function in adolescents with ataxia telangiectasia. Pediatric Pulmonology, 2008. 43(1): p. 59–66. doi: 10.1002/ppul.20738 [DOI] [PubMed] [Google Scholar]
- 712.Lefton-Greif M.A., Crawford T. O., McGrath-Morrow S., Carson K. A., Lederman H. M., Safety and caregiver satisfaction with gastrostomy in patients with Ataxia Telangiectasia. Orphanet Journal Of Rare Diseases, 2011. 6: p. 23. doi: 10.1186/1750-1172-6-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 713.Uygungil B., Minka E., Crawford T., Lederman H., Safety of live viral vaccines and retrospective review of immunologic status of 329 patients with ataxia telangiectasia. Journal of Clinical Immunology, 2012. Conference: p. 2012 Clinical Immunology Society, CIS Annual Meeting: Primary Immune Deficiency Diseases North American Conference. Chicago, IL United States. Conference Publication: (var.pagings). 32 (2) (pp 366). [Google Scholar]
- 714.Sanal O., Ozaltin F., Tezcan I., Ersoy F., Serum IgD concentrations in patients with ataxia telangiectasia and with selective IgA deficiency. International Archives of Allergy & Immunology, 1998. 116(3): p. 246. doi: 10.1159/000023951 [DOI] [PubMed] [Google Scholar]
- 715.Woelke S., Valesky E., Bakhtiar S., Bader P., Schubert R., Zielen S., Treatment of granulomas in patients with ataxia telangiectasia. Allergy: European Journal of Allergy and Clinical Immunology, 2017. Conference: p. 36th Annual Congress of the European Academy of Allergy and Clinical Immunology, EAACI 2017. Finland. 72 (Supplement 103) (pp 255). [Google Scholar]
- 716.Joncas J., Lapointe N., Gervais F., Leyritz M., Wills A., Unusual prevalence of antibodies to Epstein-Barr virus early antigen in ataxia telangiectasia. Lancet, 1977. 1(8022): p. 1160. [DOI] [PubMed] [Google Scholar]
- 717.Meyer A.K., et al., Vasculitis in a Child With the Hyper-IgM Variant of Ataxia-Telangiectasia. Frontiers in Pediatrics, 2019. 7 (no pagination)(390). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 718.Minto H., et al., A novel ATM mutation associated with elevated atypical lymphocyte populations, hyper-IgM, and cutaneous granulomas. Clin Immunol, 2019. 200: p. 55–63. doi: 10.1016/j.clim.2019.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 719.Overberg-Schmidt U., Wegner R. D., Baumgarten E., Gunther A., Ebell W., Stein H., et al., Low-grade non-Hodgkin’s lymphoma after high-grade non-Hodgkin’s lymphoma in a child with ataxia telangiectasia. Cancer, 1994. 73(5): p. 1522–5. doi: [DOI] [PubMed] [Google Scholar]
- 720.Amirifar P., et al., Effect of Class Switch Recombination Defect on the Phenotype of Ataxia-Telangiectasia Patients. Immunol Invest, 2021. 50(2–3): p. 201–215. doi: 10.1080/08820139.2020.1723104 [DOI] [PubMed] [Google Scholar]
- 721.Guiducci C. and Marchetti F., Iga deficiency. Medico e Bambino, 2020. 39(6): p. 365–369. [Google Scholar]
- 722.Szczawinska-Poplonyk A., et al., Cutaneous and systemic granulomatosis in ataxia-telangiectasia: A clinico-pathological study. Postepy Dermatologii i Alergologii, 2020. 37(5): p. 760–765. doi: 10.5114/ada.2020.100485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 723.Stefano A., et al., Flow cytometry as an important tool in the diagnosis of immunodeficiencies demonstrated in a patient with ataxia-telangiectasia. Laboratoriumsmedizin-Journal of Laboratory Medicine, 2016. 40(4): p. 255–261. [Google Scholar]
- 724.Algahtani H., et al., A novel mutation in ATM gene in a Saudi female with ataxia telangiectasia. Int J Neurosci, 2021. 131(2): p. 206–211. doi: 10.1080/00207454.2020.1736582 [DOI] [PubMed] [Google Scholar]
- 725.Sadighi Akha A.A., Humphrey R. L., Winkelstein J. A., Loeb D. M., Lederman H. M., Oligo-/monoclonal gammopathy and hypergammaglobulinemia in ataxia-telangiectasia. A study of 90 patients. Medicine, 1999. 78(6): p. 370–81. doi: 10.1097/00005792-199911000-00002 [DOI] [PubMed] [Google Scholar]
- 726.Hernandez-Trujillo V., Blouin W., Calderon J., Tolerability of subcutaneous gamma globulin in two patients with ataxia telangiectasia. Journal of Clinical Immunology, 2014. Conference: p. 16th Biennial Meeting of the European Society for Immunodeficiency, ESID 2014. Prague Czech Republic. Conference Publication: (var.pagings). 34 (2 SUPPL. 1) (pp S285). [Google Scholar]
- 727.Sanal O., Ersoy F., Tezcan I., Metin A., Turul T., Gariboglu S., et al., Antibody response to a seven-valent pneumococcal conjugated vaccine in patients with ataxia-telangiectasia. Journal of Clinical Immunology, 2004. 24(4): p. 411–7. doi: 10.1023/B:JOCI.0000029109.15355.ba [DOI] [PubMed] [Google Scholar]
- 728.Mori P.G., et al., Human serum thymic factor in antaxia-telangiectasia. New England Journal of Medicine, 1978. 298(11): p. 628–9. doi: 10.1056/NEJM197803162981113 [DOI] [PubMed] [Google Scholar]
- 729.Mohammadinejad P., Abolhassani H., Aghamohammadi A., Pourhamdi S., Ghosh S., Sadeghi B., et al., Class switch recombination process in ataxia telangiectasia patients with elevated serum levels of IgM. Journal of Immunoassay & Immunochemistry, 2015. 36(1): p. 16–26. doi: 10.1080/15321819.2014.891525 [DOI] [PubMed] [Google Scholar]
- 730.Lee W.I., et al., Clinical features and genetic analysis of Taiwanese patients with the hyper IgM syndrome phenotype. Pediatric Infectious Disease Journal, 2013. 32(9): p. 1010–6. doi: 10.1097/INF.0b013e3182936280 [DOI] [PubMed] [Google Scholar]
- 731.Buchbinder D., et al., Rubella Virus-Associated Cutaneous Granulomatous Disease: a Unique Complication in Immune-Deficient Patients, Not Limited to DNA Repair Disorders. Journal of Clinical Immunology, 2019. 39(1): p. 81–89. doi: 10.1007/s10875-018-0581-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 732.Fekrvand S., et al., Evaluation of Radiation Sensitivity in Patients with Hyper IgM Syndrome. Immunological Investigations, 2020: p. 1–17. doi: 10.1080/08820139.2020.1779288 [DOI] [PubMed] [Google Scholar]
- 733.Amirifar P., et al., Cutaneous Granulomatosis and Class Switching Defect as a Presenting Sign in Ataxia-Telangiectasia: First Case from the National Iranian Registry and Review of the Literature. Immunol Invest, 2020. 49(6): p. 597–610. doi: 10.1080/08820139.2019.1692864 [DOI] [PubMed] [Google Scholar]
- 734.Buckley R.H., Fiscus S. A., Serum IgD and IgE concentrations in immunodeficiency diseases. Journal of Clinical Investigation, 1975. 55(1): p. 157–65. doi: 10.1172/JCI107906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 735.Biggar D., Lapointe N., Ishizaka K., Meuwissen H., Good, Robert A, Frommel D. , IgE IN ATAXIA-TELANGIECTASIA AND FAMILY MEMBERS. The Lancet, 1970. 296(7682): p. 1089. doi: 10.1016/s0140-6736(70)90326-0 [DOI] [PubMed] [Google Scholar]
- 736.Aghamohammadi A., Farhoudi A., Nikzad M., Moin M., Pourpak Z., Rezaei N., et al., Adverse reactions of prophylactic intravenous immunoglobulin infusions in Iranian patients with primary immunodeficiency. Annals of Allergy, Asthma, & Immunology, 2004. 92(1): p. 60–4. doi: 10.1016/S1081-1206(10)61711-5 [DOI] [PubMed] [Google Scholar]
- 737.Bakhtiar S.S., J; Jarisch A; Rettinger E; Schubert R; Hauck FH; Zielen S; et al., Allogeneic hematopoietic stem cell transplantation in ataxia telangiectasia patients without malignancy. 2019. [Google Scholar]
- 738.Verhagen M.M., van Deuren M., Willemsen M. A., Van der Hoeven H. J., Heijdra Y. F., Yntema J. B., et al., Ataxia-Telangiectasia and mechanical ventilation: a word of caution.[Erratum appears in Pediatr Pulmonol. 2009 Feb;44(2):202–3]. Pediatric Pulmonology, 2009. 44(1): p. 101–2. doi: 10.1002/ppul.20957 [DOI] [PubMed] [Google Scholar]
- 739.Hernandez-Trujillo V.P., Blouin W. R., Calderon J. G., Case series of tolerability of SCIg in young adults with ataxia telangiectasia. Journal of Allergy and Clinical Immunology, 2016. Conference: p. 2016 Annual Meeting of the American Academy of Allergy, Asthma and Immunology, AAAAI 2016. Los Angeles, CA United States. Conference Publication: (var.pagings). 137 (2 SUPPL. 1) (pp AB227). [Google Scholar]
- 740.Malkocoglu G., Gencer H., Kaya A., Dalgic N., Bulut M. E., Aktas E., Corynebacterium propinquum bronchopneumonia in a child with ataxia telangiectasia. Turkish Journal of Pediatrics, 2016. 58(5): p. 558–561. [DOI] [PubMed] [Google Scholar]
- 741.Biswas N., Wheller L., Melo M., Casey T., Peake J., Cutaneous granulomas arising in a patient with ataxia telangiectasia. Australasian Journal of Dermatology, 2016. Conference: p. 49th Annual Scientific Meeting of the Australasian College of Dermatologists. Perth, WA Australia. Conference Publication: (var.pagings). 57 (SUPPL. 1) (pp 39–40). [Google Scholar]
- 742.Ortega-López M.C., Garay J., and Pinilla M.L., Efficacy, safety and quality of life in patients receiving subcutaneous IgG treatment: experience in Bogotá, Colombia. Immunotherapy, 2018. 10(10): p. 861–869. doi: 10.2217/imt-2018-0038 [DOI] [PubMed] [Google Scholar]
- 743.Krauthammer A., Lahad A., Goldberg L., Sarouk I., Weiss B., Somech R., et al., Elevated IgM levels as a marker for a unique phenotype in patients with Ataxia telangiectasia. BMC Pediatrics, 2018. 18(1). doi: 10.1186/s12887-018-1156-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 744.Heath J., Goldman F. D., Idiopathic thrombocytopenic purpura in a boy with ataxia telangiectasia on immunoglobulin replacement therapy. Journal of Pediatric Hematology/Oncology, 2010. 32(1): p. e25–7. doi: 10.1097/MPH.0b013e3181bf29b6 [DOI] [PubMed] [Google Scholar]
- 745.Bichuetti-Silva D.C., Furlan F. P., Nobre F. A., Pereira C. T. M., Goncalves T. R. T., Gouveia-Pereira M., et al., Immediate infusion-related adverse reactions to intravenous immunoglobulin in a prospective cohort of 1765 infusions. International Immunopharmacology, 2014. 23(2): p. 442–446. doi: 10.1016/j.intimp.2014.09.015 [DOI] [PubMed] [Google Scholar]
- 746.Pinzon-Charry A., Kimble R., Peake J., Intralesional Steroids for the Treatment of Cutaneous Granulomas in Ataxia Telangiectasia. Internal Medicine Journal, 2013. 43: p. 25–25. [Google Scholar]
- 747.Paulino T.L., Rafael M. N., Hix S., Shigueoka D. C., Ajzen S. A., Kochi C., et al., Is age a risk factor for liver disease and metabolic alterations in ataxia Telangiectasia patients? Orphanet Journal Of Rare Diseases, 2017. 12(1): p. 136. doi: 10.1186/s13023-017-0689-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 748.Soresina A., Micheli R., Leuzzi V., Molinaro A., Maffeis M., D’Agnano D., et al., Long-term continuous intra-erythrocyte infusion of dexamethasone reduces neurological symptoms in ataxia telangiectasia patients. Journal of Clinical Immunology, 2014. Conference: p. 16th Biennial Meeting of the European Society for Immunodeficiency, ESID 2014. Prague Czech Republic. Conference Publication: (var.pagings). 34 (2 SUPPL. 1) (pp S152–S153). [Google Scholar]
- 749.Bhatt J., Bush A., The microbiology of lung disease in ataxia telangiectasia (AT). European Respiratory Journal, 2012. Conference: p. European Respiratory Society Annual Congress 2012. Vienna Austria. Conference Publication: (var.pagings). 40 (SUPPL. 56) (no pagination). [Google Scholar]
- 750.Amatuni G.S., Currier R.J., Church J.A., Bishop T., Grimbacher E., Nguyen A.A.-C., et al., Newborn screening for severe combined immunodeficiency and T-cell lymphopenia in California, 2010–2017. Pediatrics in Review, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 751.Perelygina L., et al., Outcomes for Nitazoxanide Treatment in a Case Series of Patients with Primary Immunodeficiencies and Rubella Virus-Associated Granuloma. Journal of Clinical Immunology, 2019. 39(1): p. 112–117. doi: 10.1007/s10875-019-0589-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 752.Maalej B., et al., Primary immunodeficiencies (PID) of the child: About 16 cases. Archives of Disease in Childhood, 2019. 104(Supplement 3): p. A397. [Google Scholar]
- 753.Lamia S., Aloulou H., Kamoun T., Chabchoub I., Ben Moustapha I., Barbouch R., et al., [Primary immunodeficiency disorders in 51 cases]. Tunisie Medicale, 2013. 91(1): p. 38–43. [PubMed] [Google Scholar]
- 754.McGrath-Morrow S.A., Lederman H. M., Aherrera A. D., Lefton-Greif M. A., Crawford T. O., Ryan T., et al., Pulmonary function in children and young adults with ataxia telangiectasia. Pediatric Pulmonology, 2014. 49(1): p. 84–90. doi: 10.1002/ppul.22760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 755.McGrath-Morrow S.A., Collaco J. M., Detrick B., Lederman H. M., Serum Interleukin-6 Levels and Pulmonary Function in Ataxia-Telangiectasia. Journal of Pediatrics, 2016. 171: p. 256–61.e1. doi: 10.1016/j.jpeds.2016.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 756.Patel N.C., et al., Subcutaneous Immunoglobulin Replacement Therapy with Hizentra is Safe and Effective in Children Less Than 5 Years of Age. Journal of Clinical Immunology, 2015. 35(6): p. 558–565. doi: 10.1007/s10875-015-0190-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 757.Dashti-Khavidaki S., et al., Adverse reactions of prophylactic intravenous immunoglobulin: A 13-year experience with 3004 infusions in Iranian patients with primary immunodeficiency diseases. Journal of Investigational Allergology and Clinical Immunology, 2009. 19(2): p. 139–145. [PubMed] [Google Scholar]
- 758.Ribeiro L.G., et al., Clinical features of patients with primary immunodeficiency under immunoglobulin replacement therapy at the hospital da crianca de brasilia jose alencar. Journal of Clinical Immunology, 2017. Conference: p. 7th Meeting of the Latin American Society for Immunodeficiencies, LASID 2017. Brazil. 37 (1 Supplement 1) (pp S58). [Google Scholar]
- 759.Méndez-Echevarría A., et al., The Role of Respiratory Viruses in Children with Ataxia-Telangiectasia. Viruses, 2021. 13(5). doi: 10.3390/v13050867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 760.Weitering T.J., et al., Normal Numbers of Stem Cell Memory T Cells Despite Strongly Reduced Naive T Cells Support Intact Memory T Cell Compartment in Ataxia Telangiectasia. Front Immunol, 2021. 12: p. 686333. doi: 10.3389/fimmu.2021.686333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 761.Glazer S., et al., The Role of Chest MRI in Guiding Treatment Decisions in Ataxia Telangiectasia: A Case Report. Pediatric Pulmonology, 2021. 56: p. S181–S182. [Google Scholar]
- 762.Ferreira C., et al., New human immunoglobulin in Brazil: should we use? Journal of Allergy and Clinical Immunology, 2021. 147(2): p. AB13–AB13. [Google Scholar]
- 763.Yeo A.J., et al., Increased susceptibility of airway epithelial cells from ataxia-telangiectasia to S. pneumoniae infection due to oxidative damage and impaired innate immunity. Scientific reports, 2019. 9(1): p. 2627. doi: 10.1038/s41598-019-38901-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 764.Peterson R.D., Kelly W. D., Good R. A., Ataxia-Telangiectasia. Its Association with a Defective Thymus, Immunological-Deficiency Disease, and Malignancy. Lancet, 1964. 1(7344): p. 1189–93. doi: 10.1016/s0140-6736(64)91209-7 [DOI] [PubMed] [Google Scholar]
- 765.Lobo-Sanahuja F., Barrantes M., Garcia I., Porras O., Gonzalez M., Ataxia-telangiectasia and cancer of the childhood in Costa Rica. Boletin Medico del Hospital Infantil de Mexico, 1995. 52(12): p. 685–689. [Google Scholar]
- 766.Truman J.T., Richardson E. P., Dvorak H. F., Case 22–1975: Young Man with Telangiectases, Glioma and Peripheral Lymphadenopathy. New England Journal of Medicine, 1975. 292(23): p. 1231–1237. [Google Scholar]
- 767.Lefton-Greif M.A., Perlman A. L., Rosquist K. J., McGrath-Morrow S., Crawford T. O., Lederman H. M. , Coordination between respiration and deglutition in children with Ataxia-Telangiectasia (A-T). Dysphagia, 2007. 22(4): p. 400–400. [Google Scholar]
- 768.Kozielewicz D D.D., Ataxia telangiectasia as a rare cause of non-alcoholic steatohepatitis. Clinical and Experimental Hepatology, 2018. [Google Scholar]
- 769.De Lima Honorio Dumas C., Tavares F. S., De Paula Ramos Netto H., Campos V. S. P., Valente C. F. C., Pereira L. L. D., Ataxia-telangiectasia: Immunologic profile and clinical outcome. World Allergy Organization Journal, 2015. Conference: p. 3rd WAO International Scientific Conference, WISC 2014. Rio de Janeiro Brazil. Conference Publication: (var.pagings). 8 (SUPPL. 1) (no pagination). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 770.Keseru M., Knospe V., Menz A., Richard G., Meyer-Rusenberg H. W., Green S., et al., [Bilateral conjunctival manifestation of a generalized Kaposi’s sarcoma in a patient with ataxia teleangiectatica (Louis-Bar-Syndrome)]. Klinische Monatsblatter fur Augenheilkunde, 2012. 229(3): p. 255–6. doi: 10.1055/s-0031-1281838 [DOI] [PubMed] [Google Scholar]
- 771.Krauthammer A., Lahad A., Sarouk Y., Somech R., Nissenkorn A., Modan-Moses D., et al., Long-term nutritional and gastrointestinal aspects in patients with ataxia telangiectasia. Nutrition, 2018. 46(pp 48–52). doi: 10.1016/j.nut.2017.08.008 [DOI] [PubMed] [Google Scholar]
- 772.Montella S., Mollica C., Finocchi A., Pession A., Pietrogrande M. C., Trizzino A., et al., Non invasive assessment of lung disease in ataxia telangiectasia by high-field magnetic resonance imaging. Journal of Clinical Immunology, 2013. 33(7): p. 1185–91. doi: 10.1007/s10875-013-9933-y [DOI] [PubMed] [Google Scholar]
- 773.Oren O., Discovery at the bedside. Annals of Internal Medicine, 2011. 155(9): p. 643. doi: 10.7326/0003-4819-155-9-201111010-00017 [DOI] [PubMed] [Google Scholar]
- 774.Perez Gonzalez J., Delgado A., Martinez J. M., Ataxia telangiectasia (Spanish). Revista Espanola de Pediatria, 1976. 32(187): p. 77–88. [Google Scholar]
- 775.Micol R., Benslama L., Beaute J., Mahlaoui N., Hall J., Lauge A., et al., Clinical, biological, and genetic characteristics of 242 patients affected with Ataxia-Telangiectasia: a retrospective analysis from the French primary immunodeficiency registry (CEREDIH). Clinical and Experimental Immunology, 2008. 154: p. 18–19. [Google Scholar]
- 776.Patiroglu T., Gungor H. E., Baz H., Unal E. , Ataxia telangiectasia and secondary diseases. Turk Pediatri Arsivi, 2012. 47(1): p. 40–44. [Google Scholar]
- 777.Prayle A.T., M; Youle C; Safavi S; Alenazi S; Paul JA; Cooper A; et al., Early experience of oxygen enhanced magnetic resonance imaging (OE-MRI) in ataxia telangiectasia (A-T). European Respiratory Journal, 2018. [Google Scholar]
- 778.Christmann M., Pietzner J., Schmitz N., Voss S., Dresel R., Schubert R., et al., Effects of growth hormone on dystrophy and immune status in a patient with ataxia telangiectasia. Allergy: European Journal of Allergy and Clinical Immunology, 2010. Conference: p. 29th Congress of the European Academy of Allergy and Clinical Immunology, EAACI. London United Kingdom. Conference Publication: (var.pagings). 65 (SUPPL. 92) (pp 741). [Google Scholar]
- 779.Kaymaz N.E., Kupeli S., Yalcin B., Buyukpamukcu M., Hemorrhagic cystitis in a child with Hodgkin lymphoma and ataxia-telangiectasia after cyclophosphamide. Pediatric Blood & Cancer, 2009. 53(3): p. 516. [DOI] [PubMed] [Google Scholar]
- 780.Ammendola R.M., Barchetti G., Ceravolo I., Fiorelli A., Carbone I., Diagnosis of pneumothorax without exposure to ionising radiation. Thorax, 2016. 71(11): p. 1068–1069. doi: 10.1136/thoraxjnl-2016-208667 [DOI] [PubMed] [Google Scholar]
- 781.Handzel Z.T., Dolfin Z., Levin S., Altman Y., Hahn T., Trainin N., et al., Effect of thymic humoral factor on cellular immune factors of normal children and of pediatric patients with ataxia telangiectasia and Down’s syndrome. Pediatric Research, 1979. 13(7): p. 803–6. doi: 10.1203/00006450-197907000-00002 [DOI] [PubMed] [Google Scholar]
- 782.Upadhyaya S.A., Mody R., Walkovich K., Hutchinson R. J., Sandlund J. T., Connelly J. A., Ataxia Telangiectasia and Cancer Predisposition: Challenges in Management. Journal of Pediatric Hematology/Oncology., 2017. 01. [DOI] [PubMed] [Google Scholar]
- 783.Filipovich A.H., Spector B. D., Immunodeficiency (Id) as a Susceptibility Factor for Malignancy in Ataxia-Telangiectasia (a-T)—Report from the Immunodeficiency-Cancer-Registry (Icr). Pediatric Research, 1981. 15(4): p. 577–577. [Google Scholar]
- 784.Kobayashi N., Malignant neoplasms in registered cases of primary immunodeficiency syndrome. Japanese Journal of Clinical Oncology, 1985. 15 Suppl 1: p. 307–12. [PubMed] [Google Scholar]
- 785.Morrell D., Cromartie E., Swift M., Mortality and cancer incidence in 263 patients with ataxia-telangiectasia. Journal of the National Cancer Institute, 1986. 77(1): p. 89–92. [PubMed] [Google Scholar]
- 786.Groot-Loonen J.J., Slater R., Taminiau J., Voute P. A., [A patient with an immunodeficiency and consecutively 3 primary malignancies]. Tijdschrift voor Kindergeneeskunde, 1989. 57(2): p. 67–70. [PubMed] [Google Scholar]
- 787.Maffeis M., et al., Primary immunodeficiencies and oncological risk: The experience of the Children’s Hospital of Brescia. Frontiers in Pediatrics, 2019. 7(MAY) (no pagination)(232). doi: 10.3389/fped.2019.00232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 788.Jonkman-Berk B.M., van den Berg J. M., ten Berge I. J. M., Bredius R. G. M., Driessen G. J., Dalm V. A. S. H., et al., Primary immunodeficiencies in the Netherlands: National patient data demonstrate the increased risk of malignancy. Clinical Immunology. 156 (2) (pp 154–162), 2015, 2015. Date of Publication: p. February 01. doi: 10.1016/j.clim.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 789.Hayakawa H., Kobayashi N., Yata J., Primary immunodeficiency diseases and malignancy in Japan. Japanese Journal of Cancer Research, 1986. 77(1): p. 74–9. [PubMed] [Google Scholar]
- 790.Pietrucha B., Skopczynska H., Kmiec T., Chrzanowska K., Bernatowska E., Proneness to cancer in Polish Ataxia-Telangiectasia and Nijmegen breakage syndrome families. Molecular Immunology, 1998. 35(11–12): p. 797–797. [Google Scholar]
- 791.Kersey J.H., Shapiro R. S., Filipovich A. H., Relationship of immunodeficiency to lymphoid malignancy. Pediatric Infectious Disease Journal, 1988. 7(5 Suppl): p. S10–2. [PubMed] [Google Scholar]
- 792.Zielen S., Voss S., Buecker A., Hintze C., Pommerening H., Schubert R., Susceptibility to infections in patients with ataxia-telangiectasia (AT): A prospective follow-up study. Allergy: European Journal of Allergy and Clinical Immunology, 2016. Conference: p. 35th Annual Congress of the European Academy of Allergy and Clinical Immunology, EAACI 2016. Austria. 71 (Supplement 102) (pp 309–310). [Google Scholar]
- 793.Barycheva L.Y.U., et al., Congenital defects in the immune system in the Stavropol Region. Medical News of North Caucasus, 2021. 16(2): p. 153–158. [Google Scholar]
- 794.Hart R.M., Kimler B. F., Evans R. G., Park C. H., Radiotherapeutic management of medulloblastoma in a pediatric patient with ataxia telangiectasia. International Journal of Radiation Oncology, Biology, Physics, 1987. 13(8): p. 1237–40. doi: 10.1016/0360-3016(87)90200-8 [DOI] [PubMed] [Google Scholar]
- 795.Varan A., Buyukpamukcu M., Ersoy F., Sanal O., Akyuz C., Kutluk T., Yalcin B., Malignant solid tumors associated with congenital immunodeficiency disorders. Pediatric Hematology & Oncology, 2004. 21(5): p. 441–51. doi: 10.1080/08880010490457231 [DOI] [PubMed] [Google Scholar]
- 796.Bakhtiar S., et al., The incidence and type of cancer in patients with ataxia-telangiectasia via a retrospective single-centre study. Br J Haematol, 2021. 194(5): p. 879–887. doi: 10.1111/bjh.17736 [DOI] [PubMed] [Google Scholar]
- 797.Suarez F., Beaute J., Mahlaoui N., Micol R., Hermine O., Stoppa-Lyonnet D., et al., Malignancies and Outcome in Patients with Ataxia-Telangiectasia: Results From the French National Registry for Primary Immune Deficiencies. Blood, 2009. 114(22): p. 452–453.19351955 [Google Scholar]
- 798.Mijalovsky A., et al., Malignant Peritoneal Mesothelioma in an Infant With Familial ATM Mutations. Journal of Pediatric Hematology Oncology, 2018. 40(8): p. e511–e515. [DOI] [PubMed] [Google Scholar]
- 799.Halperin D., Mijalovsky A., and Birk O., Peritoneal mesothelioma in an infant with familial ATM mutations. European Journal of Human Genetics, 2019. 26(Supplement 1): p. 973–974. [Google Scholar]
- 800.Boga S., Altundag O., Ozyilkan O., Pleural Mesothelioma in a Patient with Ataxia Telangiectasia. Annals of Oncology, 2009. 20: p. 31–31. [Google Scholar]
- 801.Sandoval C., Schantz S., Posey D., Swift M., Parotid and thyroid gland cancers in patients with ataxia-telangiectasia. Pediatric Hematology & Oncology, 2001. 18(8): p. 485–90. doi: 10.1080/088800101753328448 [DOI] [PubMed] [Google Scholar]
- 802.Gotoff S.P., Amirmokri E., Liebner E. J., Ataxia telangiectasia. Neoplasia, untoward response to x-irradiation, and tuberous sclerosis. American Journal of Diseases of Children, 1967. 114(6): p. 617–25. doi: 10.1001/archpedi.1967.02090270073006 [DOI] [PubMed] [Google Scholar]
- 803.Miller R.W., Childhood cancer and congenital defects a study of U.S. Death certificates during the period 1960–1966. Pediatric Research, 1969. 3(5): p. 389–397. doi: 10.1203/00006450-196909000-00001 [DOI] [PubMed] [Google Scholar]
- 804.Phillips H.A., Howard G. C., Testicular seminoma in a patient with ataxia-telangiectasia. Clinical Oncology (Royal College of Radiologists), 1999. 11(1): p. 63–4. [DOI] [PubMed] [Google Scholar]
- 805.De Leon G.A., Grover W. D., Huff D. S., Neuropathologic changes in ataxia-telangiectasia. Neurology, 1976. 26(10): p. 947–51. doi: 10.1212/wnl.26.10.947 [DOI] [PubMed] [Google Scholar]
- 806.Koksal Y., Caliskan U., Ucar C., Yurtcu M., Artac H., Ilerisoy-Yakut Z., et al., Dysgerminoma in a child with ataxia-telangiectasia. Pediatric Hematology & Oncology, 2007. 24(6): p. 431–6. [DOI] [PubMed] [Google Scholar]
- 807.Duffy R., et al., Dermatofibrosarcoma protuberans in a pediatric patient with ataxia telangiectasia syndrome. Pediatric Dermatology, 2019. 36(3): p. 400–401. doi: 10.1111/pde.13779 [DOI] [PubMed] [Google Scholar]
- 808.Murphy R.C., Berdon W. E., Ruzal-Shapiro C., Hall E. J., Kornecki A., Daneman A., et al., Malignancies in pediatric patients with ataxia telangiectasia. Pediatric Radiology, 1999. 29(4): p. 225–30. doi: 10.1007/s002470050578 [DOI] [PubMed] [Google Scholar]
- 809.Patiroglu T., Eke Gungor H., Arslan D., Deniz K., Unal E., Coskun A., Gastric signet ring carcinoma in a patient with ataxia-telangiectasia: a case report and review of the literature. Journal of Pediatric Hematology/Oncology, 2013. 35(8): p. e341–3. doi: 10.1097/MPH.0b013e318279b3f7 [DOI] [PubMed] [Google Scholar]
- 810.Patiroglu T., Akar H. H., Unal E., Ozdemir M. A., Karakukcu M., Patiroglu T. E., Malignancies in Primary Immunodeficiencies: A Single Center Experience. Pediatric, Allergy, Immunology, and Pulmonology, 2015. 28(1): p. 47–54. [Google Scholar]
- 811.López Tobaruela J.M., Librero Jiménez M., and Heredia Carrasco C., Intestinal-type gastric adenocarcinoma in a patient with ataxia-telangiectasia syndrome. Rev Esp Enferm Dig, 2020. 112(9): p. 742–743. [DOI] [PubMed] [Google Scholar]
- 812.Salazar-Marcelino A.E., Mendoza-Torres Ma, Fernandez-Tamayo N., Martinez-Maya H. J., 23-year-old female patient with ataxia telangiectasia and metastatic clear cell hepatocellular carcinoma. Medicina Interna de Mexico, 2016. 32(1): p. 152–156. [Google Scholar]
- 813.Yoshitomi F., Zaitsu Y., Tanaka K., Ataxia-telangiectasia with renal cell carcinoma and hepatoma. Virchows Archiv. A, Pathological Anatomy & Histology, 1980. 389(1): p. 119–25. doi: 10.1007/BF00428672 [DOI] [PubMed] [Google Scholar]
- 814.Deschildre A., Vallee L., Croquette M. F., Nelken B., Nuyts J. P., [Oncologic complications and cytogenetic features of ataxia telangiectasia]. Archives Francaises de Pediatrie, 1990. 47(3): p. 203–5. [PubMed] [Google Scholar]
- 815.Cecinati V., Arcamone G., Mattia D. D., Santoro N., Martire B., Hepatic non-Hodgkin lymphoma and hepatoblastoma complicating ataxia-telangiectasia. Immunopharmacology & Immunotoxicology, 2012. 34(1): p. 1–3. doi: 10.3109/08923973.2011.567989 [DOI] [PubMed] [Google Scholar]
- 816.Cosentini M.L., et al., Pediatric hepatocellular carcinoma: A 23-year experience at a single institution in Argentina. Pediatric Blood and Cancer, 2015. Conference: p. 47th Congress of the International Society of Paediatric Oncology, SIOP 2015. South Africa. 62 (Supplement 4) (pp S308–S309). [Google Scholar]
- 817.Hayakawa H., Kobayashi N., Yata J., Primary immunodeficiency diseases and malignancy-Asummary of the cases reported to the All Japan lmmunodeficiency Registry. Japanese Journal of Clinical Immunology, 1985. 8(5): p. 265–269. [Google Scholar]
- 818.Woelke S., Hess U., Knop V., Krausskopf D., Kieslich M., Schubert R., et al., Progressive liver disease in patients with ataxia telangiectasia. Allergy: European Journal of Allergy and Clinical Immunology, 2017. Conference: p. 36th Annual Congress of the European Academy of Allergy and Clinical Immunology, EAACI 2017. Finland. 72 (Supplement 103) (pp 255–256). [Google Scholar]
- 819.Krishna Kumar G., Al Saadi A., Yang S. S., McCaughey R. S., Ataxia-telangiectasia and hepatocellular carcinoma. American Journal of the Medical Sciences, 1979. 278(2): p. 157–60. doi: 10.1097/00000441-197909000-00008 [DOI] [PubMed] [Google Scholar]
- 820.Tamminga R.Y., Dolsma W. V., Leeuw J. A., Kampinga H. H., Chemo- and radiosensitivity testing in a patient with ataxia telangiectasia and Hodgkin disease. Pediatric Hematology & Oncology, 2002. 19(3): p. 163–71. [DOI] [PubMed] [Google Scholar]
- 821.Armata J., Grzeskowiak-Melanowska J., Pekacki A., Hnatko-Kolacz M., Chemotherapy alone as a treatment of Hodgkin’s disease in two children with ataxia teleangiectasia. Nowotwory, 1991. 41(3): p. 189–191. [Google Scholar]
- 822.Sandoval C., Swift M., Cytomegalovirus pneumonitis in a patient with Hodgkin disease and ataxia-telangiectasia. Pediatric Pulmonology, 2004. 37(6): p. 559–60. doi: 10.1002/ppul.10422 [DOI] [PubMed] [Google Scholar]
- 823.Spector B.D., Perry G. S., Kersey J. H., Filipovich A. H., Descriptive Epidemiology of Malignancy in Ataxia-Telangiectasia (a-T)—an Immunodeficiency-Cancer Registry (Icr) Report. Pediatric Research, 1981. 15(4): p. 523–523. [Google Scholar]
- 824.Cekic S., Aytekin C., Metin A., Karaca N., Demirkaya M., Sevinir B., et al., The evaluation of malignancies in Turkish pid patients; A multicenter study. Journal of Clinical Immunology, 2018. Conference: p. 2018 CIS Annual Meeting: Immune Deficiency and Dysregulation North American Conference. Canada. 38 (3) (pp 409–410). doi: 10.1111/pai.13231 [DOI] [PubMed] [Google Scholar]
- 825.Szudy A., Litak J., Zawitkowska J., Kowalczyk J., Hematological malignancies in children with ataxia-telangiectasia—A diffi cult clinical problem. Acta Haematologica Polonica, 2012. 43(3): p. 291–295. [Google Scholar]
- 826.Canioni D., Mahlaoui N., Andriamanga C., D’Enghien C. D., Jais J. P., Fischer A., et al., Histological characteristics of ataxia telangiectasia associated lymphoproliferative diseases. Results of the french registry of primary immune deficiencies. Blood, 2014. Conference: p. 56th Annual Meeting of the American Society of Hematology, ASH 2014. San Francisco, CA United States. Conference Publication: (var.pagings). 124 (21) (no pagination). [Google Scholar]
- 827.Sandoval C., Swift M., Hodgkin disease in ataxia-telangiectasia patients with poor outcomes. Medical & Pediatric Oncology, 2003. 40(3): p. 162–6. doi: 10.1002/mpo.10251 [DOI] [PubMed] [Google Scholar]
- 828.Tanyildiz H.G., et al., Lymphoma Secondary to Congenital and Acquired Immunodeficiency Syndromes at a Turkish Pediatric Oncology Center. Journal of Clinical Immunology, 2016. 36(7): p. 667–76. doi: 10.1007/s10875-016-0324-z [DOI] [PubMed] [Google Scholar]
- 829.Tallon Garcia M., Cobelas Cobelas M., Fernandez Sanmartin M., Cabo Perez M., Garcia Burriel I., Fiano Valverde C., [Sclerosing cholangitis, ataxia-telangiectasia and Hodgkin’s disease]. Anales de Pediatria, 2011. 75(2): p. 141–3. doi: 10.1016/j.anpedi.2011.02.011 [DOI] [PubMed] [Google Scholar]
- 830.Ben Arush M.W., Rosenthal J., Dale J., Horovitch Y., Herzl G., Arie J. B., et al., Ataxia telangiectasia and lymphoma: An indication for individualized chemotherapy dosing—report of treatment in a highly inbred arab family. Pediatric Hematology and Oncology, 1995. 12(2): p. 163–169. doi: 10.3109/08880019509029550 [DOI] [PubMed] [Google Scholar]
- 831.Amromin G.D., Boder E., Ataxia-Telangiectasia—Autopsy Findings in a 31-Year-Old Woman. Journal of Neuropathology and Experimental Neurology, 1977. 36(3): p. 591–591. [DOI] [PubMed] [Google Scholar]
- 832.Mouchet F., Ninane J., Gosseye S., Verellen C., Bonnier C., Evrard P., et al., Leiomyoma of the suprarenal gland in a child with ataxia-telangiectasia. Pediatric Hematology & Oncology, 1991. 8(3): p. 235–41. [DOI] [PubMed] [Google Scholar]
- 833.Jindal A.K., et al., Primary immunodeficiency disorders in India-A situational review. Frontiers in Immunology, 2017. 8(JUN). doi: 10.3389/fimmu.2017.00714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 834.Oguzkurt P., Senocak M. E., Akcoren Z., Kale G., Hicsonmez A., Splenic leiomyoma: an uncommon localization. European Journal of Pediatric Surgery, 1996. 6(4): p. 235–7. doi: 10.1055/s-2008-1066517 [DOI] [PubMed] [Google Scholar]
- 835.Becher R., Duhrsen C., Distinct chromosome abnormalities in ataxia telangiectasia with chronic T-cell lymphocytic leukemia. Cancer Genetics & Cytogenetics, 1987. 26(2): p. 217–25. doi: 10.1016/0165-4608(87)90055-0 [DOI] [PubMed] [Google Scholar]
- 836.Taylor A.M. and Butterworth S.V., Clonal evolution of T-cell chronic lymphocytic leukaemia in a patient with ataxia telangiectasia. International Journal of Cancer, 1986. 37(4): p. 511–6. doi: 10.1002/ijc.2910370407 [DOI] [PubMed] [Google Scholar]
- 837.Sparkes R.S., Como R., Golde D. W., Cytogenetic abnormalities in ataxia telangiectasia with T-cell chronic lymphocytic leukemia. Cancer Genetics and Cytogenetics, 1980. 1(4): p. 329–336. [Google Scholar]
- 838.Saxon A., Stevens R.H., and Golde D.W., Helper and suppressor t-lymphocyte leukemia in ataxia telangiectasia. New England Journal of Medicine, 1979. 300(13): p. 700–4. doi: 10.1056/NEJM197903293001303 [DOI] [PubMed] [Google Scholar]
- 839.Espana C., Lugo-Reyes S., Yamazaki M. A., Malignancies associated to primary immunodeficiencies. A 40 year review. World Allergy Organization Journal, 2012. Conference: p. 22nd World Allergy Congress. Cancun Mexico. Conference Publication: (var.pagings). 5 (SUPPL. 2) (pp S190). [Google Scholar]
- 840.Saxon A., Stevens R. H., Golde D. W., T-cell leukemia in ataxia telangiectasia. New England Journal of Medicine, 1979. 301(17): p. 945. doi: 10.1056/NEJM197910253011719 [DOI] [PubMed] [Google Scholar]
- 841.Hoche F., et al., Ataxia Telangiectasia (AT) as a radiation sensitivity syndrom and limits of radiotherapeutic intervention. Neuropediatrics, 2012. Conference: p. 38th Annual Meeting of the Society of Neuropediatrics. Munster Germany. Conference Publication: (var.pagings). 43 (2) (no pagination). [Google Scholar]
- 842.Pastore G., Cordero di Montezemolo L., Madon E., Ataxia telangiectasia and acute lymphoblastic leukemia: report of a case. Tumori, 1981. 67(6): p. 585–7. [DOI] [PubMed] [Google Scholar]
- 843.Wake N., Minowada J., Park B., Sandberg A. A., Chromosomes and causation of human cancer and leukemia. XLVIII. T-cell acute leukemia in ataxia telangiectasia. Cancer Genetics & Cytogenetics, 1982. 6(4): p. 345–7. doi: 10.1016/0165-4608(82)90091-7 [DOI] [PubMed] [Google Scholar]
- 844.Keklik M., Sivgin S., Kalin B. S., Akyol G., Pala C., Solmaz M., et al., The control of acute lymphoblastic leukaemia caused hyperleukocytosis with leukopheresis on an adult ataxia-telangiectasia patient. Transfusion and Apheresis Science, 2012. Conference: p. 14th International Congress of the World Apheresis Association and 7th National Congress of Turkish Society of Apheresis. Istanbul Turkey. Conference Publication: (var.pagings). 47 (SUPPL. 1) (pp S41). [Google Scholar]
- 845.Christmann M., Vos S., Rosewich M., Pietzner J., Schubert R., Zielen S., Effects of Growth Hormone treatment on dystrophy and immune status in patients with Ataxia telangiectasia. Allergy: European Journal of Allergy and Clinical Immunology, 2012. Conference: p. 31st Congress of the European Academy of Allergy and Clinical Immunology. Geneva Switzerland. Conference Publication: (var.pagings). 67 (SUPPL. 96) (pp 274). [Google Scholar]
- 846.Thibaud M., et al., Hematologic Malignancies in Children and Adolescents with Ataxia Telangiectasia: 20 Years of Nationwide Experience in France. Pediatric Blood & Cancer, 2019. 66: p. S259–S259. [Google Scholar]
- 847.Ali S.K., Bowman W. P., Aur R. J., Increased radiation sensitivity of fibroblasts in ataxia telangiectasia with acute lymphocytic leukemia. American Journal of Diseases of Children, 1981. 135(12): p. 1142–3. doi: 10.1001/archpedi.1981.02130360046017 [DOI] [PubMed] [Google Scholar]
- 848.Mselati J.C., Buriot D., Nezelof C., Primary immunodeficiency and cancer. 5 case reports. Archives Francaises de Pediatrie, 1983. 40(3): p. 163–169. [PubMed] [Google Scholar]
- 849.Ferreira L.B., Dias D. K., Castro A. P. B. M., Pastorino A. C., De Barros Dorna M., Zamperlini G., et al., Ataxia-telangiectasia and CD8 + T cells acute lymphoid leukemia in a Brazilian Patient: A Case Report. Journal of Clinical Immunology, 2012. Conference: p. 2012 Clinical Immunology Society, CIS Annual Meeting: Primary Immune Deficiency Diseases North American Conference. Chicago, IL United States. Conference Publication: (var.pagings). 32 (2) (pp 381). [Google Scholar]
- 850.Minegishi M., et al., Functional and molecular characteristics of acute lymphoblastic leukemia cells with a mature T-cell phenotype from a patient with ataxia telangiectasia. Leukemia, 1991. 5(1): p. 88–9. [PubMed] [Google Scholar]
- 851.Thick J., Sherrington P. D., Fisch P., Taylor A. M., Rabbitts T. H., Molecular analysis of a new translocation, t(X;14)(q28;q11), in premalignancy and in leukaemia associated with ataxia telangiectasia. Genes, Chromosomes & Cancer, 1992. 5(4): p. 321–5. [DOI] [PubMed] [Google Scholar]
- 852.Paul R.N., Alizadeh L., Ajayi O. I., Karpurapu H., Ganesan C., Taddesse-Heath L., et al., A Case Report of T Cell Prolymphocytic Leukemia and Kaposi Sarcoma and a Review of T Cell Prolymphocytic Leukemia. Acta Haematologica, 2012. 127(4): p. 235–243. doi: 10.1159/000336241 [DOI] [PubMed] [Google Scholar]
- 853.Thick J.A., Sherrington P. D., Rabbitts T. H., Taylor A. M. R., Clonal Evolution of T-Cell Leukemia in an Ataxia Telangiectasia Patient with a T(X-14) (Q28-Q11) Translocation. American Journal of Human Genetics, 1991. 49(4): p. 458–458. [Google Scholar]
- 854.Taylor A.M., Lowe P. A., Stacey M., Thick J., Campbell L., Beatty D., et al., Development of T-cell leukaemia in an ataxia telangiectasia patient following clonal selection in t(X;14)-containing lymphocytes. Leukemia, 1992. 6(9): p. 961–6. [PubMed] [Google Scholar]
- 855.Thick J., Mak Y. F., Metcalfe J., Beatty D., Taylor A. M., A gene on chromosome Xq28 associated with T-cell prolymphocytic leukemia in two patients with ataxia telangiectasia. Leukemia, 1994. 8(4): p. 564–73. [PubMed] [Google Scholar]
- 856.Brito-Babapulle V., Catovsky D., Inversions and tandem translocations involving chromosome 14q11 and 14q32 in T-prolymphocytic leukemia and T-cell leukemias in patients with ataxia telangiectasia. Cancer Genetics & Cytogenetics, 1991. 55(1): p. 1–9. doi: 10.1016/0165-4608(91)90228-m [DOI] [PubMed] [Google Scholar]
- 857.Brummel B., Bernbeck B., Schneider D. T., Complicated but successful treatment of a patient with ataxia telangiectasia and pre-B-acute lymphoblastic leukemia. Klinische Padiatrie, 2010. 222(6): p. 391–4. doi: 10.1055/s-0030-1267151 [DOI] [PubMed] [Google Scholar]
- 858.Ussowicz M., Musial J., Owoc-Lempach J., Gorczynska E., Chybicka A., Kalwak K., Allogeneic matched sibling donor bone marrow transplantation after low-dose busilvex-fludarabine conditioning in a 3 year old boy with ataxia-telangiectasia syndrome and acute lymphoblastic leukaemia: A case report. Bone Marrow Transplantation, 2012. Conference: p. 38th Annual Meeting of the European Group for Blood and Marrow Transplantation, EBMT 2012. Geneva Switzerland. Conference Publication: (var.pagings). 47 (SUPPL. 1) (pp S395–S396). [Google Scholar]
- 859.Özyörük D., et al., The Development of Chylothorax in a Child With T-Cell Lymphoblastic Lymphoma and Ataxia Telangiectasia During Induction Therapy. J Pediatr Hematol Oncol, 2020. Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 860.Donath H., et al., Diabetes in Patients With Ataxia Telangiectasia: A National Cohort Study. Frontiers in Pediatrics, 2020. 8 (no pagination)(317). doi: 10.3389/fped.2020.00317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 861.Leclerc-Mercier S., et al., Cutaneous granulomas with primary immunodeficiency in children: a report of 17 new patients and a review of the literature. Journal of the European Academy of Dermatology and Venereology, 2019. 33(7): p. 1412–1420. doi: 10.1111/jdv.15568 [DOI] [PubMed] [Google Scholar]
- 862.Martinez-Leon M.I., Ceres-Ruiz L., Cuesta M. A., Garcia-Martin F. J., Imaging study of lymphoreticular tumor development in ataxia-telangiectasia and Nijmegen breakage syndrome. Radiologia, 2003. 45(3): p. 151–155. [Google Scholar]
- 863.Kurucu N., et al., Primary cutaneous lymphoma: A report of 15 cases from single center. Pediatric Blood and Cancer, 2016. Conference: p. 48th Congress of the International Society of Paediatric Oncology, SIOP 2016. Ireland. 63 (Supplement 3) (pp S181). [Google Scholar]
- 864.Mellouli F., et al., Report of the Tunisian Registry of Primary Immunodeficiencies: 25-Years of Experience (1988–2012). Journal of Clinical Immunology, 2015. 35(8): p. 745–753. doi: 10.1007/s10875-015-0206-9 [DOI] [PubMed] [Google Scholar]
- 865.Bennett J.A., Bayerl M. G., Epstein-barr virus-associated extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT Lymphoma) arising in the parotid gland of a child with ataxia telangiectasia. Journal of Pediatric Hematology/Oncology, 2015. 37(2): p. e114–7. doi: 10.1097/MPH.0b013e31829f3496 [DOI] [PubMed] [Google Scholar]
- 866.Kozlova O., Kostyuchenko L., Polishchuk R., Cimbalyuk I., Dorosh O., Troyanovska O., et al., Non-hodgkin lymphomas in children with chromosome instability syndromes. Haematologica, 2011. Conference: p. 16th Congress of the European Hematology Association. London United Kingdom. Conference Publication: (var.pagings). 96 (SUPPL. 2) (pp 570). [Google Scholar]
- 867.Yoshikawa T, et al., Large B-Cell Lymphoma in a 14-Year-Old Girl with Ataxia-Telangiectasia. Pediatric Blood & Cancer, 2018. 65: p. S43–S43. [Google Scholar]
- 868.Shabbat S., et al., Rituximab as monotherapy and in addition to reduced CHOP in children with primary immunodeficiency and non-Hodgkin lymphoma. Pediatric Blood & Cancer, 2009. 52(5): p. 664–6. doi: 10.1002/pbc.21808 [DOI] [PubMed] [Google Scholar]
- 869.Yamada Y., Inoue R., Fukao T., Kaneko H., Isogai K., Fukuda S., et al., Ataxia telangiectasia associated with B-cell lymphoma: the effect of a half-dose of the drugs administered according to the acute lymphoblastic leukemia standard risk protocol. Pediatric Hematology & Oncology, 1998. 15(5): p. 425–9. [DOI] [PubMed] [Google Scholar]
- 870.Christmann M., Heitkamp S., Lambrecht E., Doerries K., Schubert R., Zielen S., Haemorrhagic cystitis and polyomavirus JC infection in ataxia telangiectasia. Journal of pediatric urology, 2009. 5(4): p. 324–6. doi: 10.1016/j.jpurol.2009.02.198 [DOI] [PubMed] [Google Scholar]
- 871.Nelson M., Schore R., Jacobs S., Mature B-Cell Lymphoma in a Pediatric Patient with Ataxia-Telangiectasia: An Uncertain Frontier. Pediatric Blood & Cancer, 2016. 63: p. S83–S83. [Google Scholar]
- 872.Attarbaschi A., Carraro E., Abla O., Barzilai-Birenboim S., Bomken S., Brugieres L., et al., Non-Hodgkin lymphoma and pre-existing conditions: spectrum, clinical characteristics and outcome in 213 children and adolescents. Haematologica, 2016. 101(12): p. 1581–1591. doi: 10.3324/haematol.2016.147116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 873.Sherkat R., Reisi N., and Nazem M., Enigmas left in diagnosis: Chronic epstein barr virus lymphoproliferation or lymphoma. Journal of Clinical Immunology, 2014. Conference: p. 16th Biennial Meeting of the European Society for Immunodeficiency, ESID 2014. Prague Czech Republic. Conference Publication: (var.pagings). 34 (2 SUPPL. 1) (pp S374). [Google Scholar]
- 874.Rossi G., et al., Modified chop-chemotherapy plus rituximab for diffuse large b-cell lymphoma complicating ataxia-telangiectasia. British Journal of Haematology, 2003. 120(2): p. 369–71. doi: 10.1046/j.1365-2141.2003.04041_4.x [DOI] [PubMed] [Google Scholar]
- 875.Arico M., et al., Non-Hodgkin lymphoma in children with an associated inherited condition: A retrospective analysis of the Associazione Italiana Ematologia Oncologia Pediatrica (AIEOP). Pediatric Blood & Cancer, 2015. 62(10): p. 1782–9. doi: 10.1002/pbc.25565 [DOI] [PubMed] [Google Scholar]
- 876.Jastaniah W., Aljefri A., Ayas M., Alharbi M., Alkhayat N., Al-Anzi F., et al., Prevalence of hereditary cancer susceptibility syndromes in children with cancer in a highly consanguineous population. Cancer Epidemiology, 2018. 55(pp 88–95). doi: 10.1016/j.canep.2018.05.006 [DOI] [PubMed] [Google Scholar]
- 877.Machida S., Tomizawa D., Tamaichi H., Okawa T., Endo A., Imai K., et al., Successful treatment of diffuse large B-cell lymphoma in a patient with ataxia telangiectasia using rituximab. Journal of Pediatric Hematology/Oncology, 2013. 35(6): p. 482–5. doi: 10.1097/MPH.0b013e3182804d59 [DOI] [PubMed] [Google Scholar]
- 878.Mann G., et al., Clinical characteristics and treatment outcome of infants with non-Hodgkin lymphoma. British Journal of Haematology, 2007. 139(3): p. 443–449. doi: 10.1111/j.1365-2141.2007.06796.x [DOI] [PubMed] [Google Scholar]
- 879.Beier R., Sykora K. W., Woessmann W., Maecker-Kolhoff B., Sauer M., Kreipe H. H., et al., Allogeneic-matched sibling stem cell transplantation in a 13-year-old boy with ataxia telangiectasia and EBV-positive non-Hodgkin lymphoma. Bone Marrow Transplantation, 2016. 51(9): p. 1271–4. doi: 10.1038/bmt.2016.93 [DOI] [PubMed] [Google Scholar]
- 880.Pippard E.C., Hall A. J., Barker D. J., Bridges B. A., Cancer in homozygotes and heterozygotes of ataxia-telangiectasia and xeroderma pigmentosum in Britain. Cancer Research, 1988. 48(10): p. 2929–32. [PubMed] [Google Scholar]
- 881.Koleva M., Bojinova V., Savov A., Case of Ataxia-teleangiectasia (Louis Bar Syndrome) in 5-years Old Girl with Non-Hodgkin Lymphoma. Pediatriya, 2017. 2017-January(1): p. 54–57. [Google Scholar]
- 882.Emir S., Vezir E., Azkur D., Demir H. A., Metin A., Characteristics of children with non-hodgkin lymphoma associated with primary immune deficiency diseases: descriptions of five patients. Pediatric Hematology & Oncology, 2013. 30(6): p. 544–53. doi: 10.3109/08880018.2013.792893 [DOI] [PubMed] [Google Scholar]
- 883.Arias D.P., Casas A. A., Cajal M. D., Ramon M. L., Montanes L. J., Complete heart block and asystole in a child with ataxia-telangiectasia. Archivos Argentinos de Pediatria, 2017. 115(5): p. e291–e293. doi: 10.5546/aap.2017.e291 [DOI] [PubMed] [Google Scholar]
- 884.Ataseven E, et al., Non-Hodgkin lymphoma- single center experience. British Journal of Haematology, 2018. 182: p. 5–109. doi: 10.1111/bjh.15536 [DOI] [PubMed] [Google Scholar]
- 885.Makis A., Polychronopoulou S., and Haidas S. , Osteosarcoma as a second tumor after treatment for primary non-Hodgkin’s lymphoma in a child with ataxia-telangiectasia: presentation of a case and review of possible pathogenetic mechanisms. Journal of Pediatric Hematology/Oncology, 2004. 26(7): p. 444–6. doi: 10.1097/00043426-200407000-00009 [DOI] [PubMed] [Google Scholar]
- 886.Sciuca S., Tomacinschi C., and Selevestru R., Polymorphism of pulmonary manifestations in children with Louis bar syndrome. Allergy, 2018. 73: p. 770–770. [Google Scholar]
- 887.Kilic S.S., Ozel M., Hafizoglu D., Karaca N. E., Aksu G., Kutukculer N., The prevalences [correction] and patient characteristics of primary immunodeficiency diseases in Turkey—two centers study. Journal of Clinical Immunology, 2013. 33(1): p. 74–83. doi: 10.1007/s10875-012-9763-3 [DOI] [PubMed] [Google Scholar]
- 888.Seidemann K., Tiemann M., Henze G., Sauerbrey A., Muller S., Reiter A., Therapy for non-Hodgkin lymphoma in children with primary immunodeficiency: Analysis of 19 patients from the BFM trials. Medical and Pediatric Oncology, 1999. 33(6): p. 536–544. doi: [DOI] [PubMed] [Google Scholar]
- 889.Uner A., Caliskan U., Ugras N. S., Reisli I., Artac H., Kose D., et al., Unusual non-hodgkin lymphoma subtypes in children with primary immunodeficiency. Pediatric Blood and Cancer, 2013. Conference: p. 45th Congress of the International Society of Paediatric Oncology, SIOP 2013. Hong Kong China. Conference Publication: (var.pagings). 60 (SUPPL. 3) (pp 83). [Google Scholar]
- 890.Ghoshal A., Salins N., Damani A., Deodhar J., Muckaden M. A., Medical Management of Pediatric Malignant Bowel Obstruction in a Patient with Burkitt’s Lymphoma and Ataxia Telangiectasia Using Continuous Ambulatory Drug Delivery System. Journal of Pain & Palliative Care Pharmacotherapy, 2016. 30(1): p. 44–8. [DOI] [PubMed] [Google Scholar]
- 891.Sandlund J.T., Hudson M. M., Kennedy W., Onciu M., Kastan M. B., Pilot study of modified LMB-based therapy for children with ataxia-telangiectasia and advanced stage high grade mature B-cell malignancies. Pediatric Blood & Cancer, 2014. 61(2): p. 360–2. doi: 10.1002/pbc.24696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 892.Baysal B., et al., Childhood cancers and heredity: A single center experience. Pediatric Blood and Cancer. Conference: 52th Congress of the International Society of Paediatric Oncology, SIOP. Virtual., 2020. 67(SUPPL 4). [DOI] [PubMed] [Google Scholar]
- 893.deVries C.R., Kaplan G. W., An unusual case of urinary incontinence, ataxia-telangiectasia, and metastatic dysgerminoma: case report and review of the literature. Urology, 1997. 50(3): p. 453–5. doi: 10.1016/S0090-4295(97)00244-6 [DOI] [PubMed] [Google Scholar]
- 894.Perez-Villena A., Cormenzana M., de Prada I., Perez-Martinez A., Aleo E., Ataxia-telangiectasia and wilms tumor: reduced treatment but early relapse. Journal of Pediatric Hematology/Oncology, 2013. 35(4): p. 308–10. doi: 10.1097/MPH.0b013e31828fccdf [DOI] [PubMed] [Google Scholar]
- 895.Nissenkorn A., et al., Secondary enuresis and urological manifestations in children with ataxia telangiectasia. European Journal of Paediatric Neurology, 2018. 22(6): p. 1118–1123. doi: 10.1016/j.ejpn.2018.07.006 [DOI] [PubMed] [Google Scholar]
- 896.Feigin R.D., Vietti T. J., Wyatt R. G., Kaufman D. G., Smith C. H. Jr., Ataxia telangiectasia with granulocytopenia. Journal of Pediatrics, 1970. 77(3): p. 431–8. doi: 10.1016/s0022-3476(70)80011-7 [DOI] [PubMed] [Google Scholar]
- 897.Oska S., et al., 18303 Ataxia telangiectasia and melanoma: The role of dermatology in ataxia telangiectasia. Journal of the American Academy of Dermatology, 2020. 83(6 Supplement): p. AB209. [Google Scholar]
- 898.Eswaran M.K., Kennedy J. W., Ataxia telangiectasia and follicular cancer- to radiate or not. Endocrine Reviews, 2013. Conference: p. 95th Annual Meeting and Expo of the Endocrine Society, ENDO 2013. San Francisco, CA United States. Conference Publication: (var.pagings). 34 (3 SUPPL. 1) (no pagination). [Google Scholar]
- 899.Simons M.J. and Hosking C.S., Letter: A.F.P. and ataxia-telangiectasia. Lancet, 1974. 1(7868): p. 1234. doi: 10.1016/s0140-6736(74)91052-6 [DOI] [PubMed] [Google Scholar]
- 900.Waldmann T.A., McIntire K. R., Serum-alpha-fetoprotein levels in patients with ataxia-telangiectasia. Lancet, 1972. 2(7787): p. 1112–5. doi: 10.1016/s0140-6736(72)92717-1 [DOI] [PubMed] [Google Scholar]
- 901.Volkow N.D., Tomasi D., Wang G. J., Studentsova Y., Margus B., Crawford T. O., Brain glucose metabolism in adults with ataxia-telangiectasia and their asymptomatic relatives. Brain, 2014. 137(Pt 6): p. 1753–61. doi: 10.1093/brain/awu092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 902.Schubert R., Reichenbach J., and Zielen S., Deficiencies in CD4+ and CD8+ T cell subsets in ataxia telangiectasia. Clinical & Experimental Immunology, 2002. 129(1): p. 125–32. doi: 10.1046/j.1365-2249.2002.01830.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 903.Sun X., Becker-Catania S. G., Chun H. H., Hwang M. J., Huo Y., Wang Z., et al., Early diagnosis of ataxia-telangiectasia using radiosensitivity testing. Journal of Pediatrics, 2002. 140(6): p. 724–31. doi: 10.1067/mpd.2002.123879 [DOI] [PubMed] [Google Scholar]
- 904.Anheim M., Fleury M., Monga B., Laugel V., Chaigne D., Rodier G., et al., Epidemiological, clinical, paraclinical and molecular study of a cohort of 102 patients affected with autosomal recessive progressive cerebellar ataxia from Alsace, Eastern France: implications for clinical management. Neurogenetics, 2010. 11(1): p. 1–12. doi: 10.1007/s10048-009-0196-y [DOI] [PubMed] [Google Scholar]
- 905.Schubert R., Reichenbach J., Zielen S., Growth factor deficiency in patients with ataxia telangiectasia. Clinical & Experimental Immunology, 2005. 140(3): p. 517–9. doi: 10.1111/j.1365-2249.2005.02782.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 906.Schindler D., Seyschab H., Poot M., Hoehn H., Schinzel A., Fryns J. P., et al., Screening test for ataxia telangiectasia. Lancet, 1987. 2(8572): p. 1398–9. doi: 10.1016/s0140-6736(87)91288-8 [DOI] [PubMed] [Google Scholar]
- 907.Bernatowska E., Michakiewicz J., Gregorek H., Madalinski K., Skopczynska H., Pietrucha B., et al., Twenty years of investigations into primary immunodeficiency diseases in the Department of Immunology of the Children’s Memorial Health Institute, Warsaw. Central European Journal of Immunology, 2000. 25(3): p. 119–126. [Google Scholar]
- 908.Welsh K., Diabetes and Ataxia Telangiectasia. Journal of Pediatric Nursing-Nursing Care of Children & Families, 2018. 40: p. 95–95. [Google Scholar]
- 909.Rafael M., Paulino T., Hix S., Ajzen S., Shigueoka D., Souza F., et al., Hepatic Steatosis in Patients with Ataxia-Telangiectasia: Association with Biomarkers Related to Glucose Metabolism. Journal of Clinical Immunology, 2015. 35: p. S29–S29. [Google Scholar]
- 910.Blevins L.S. Jr., Gebhart S. S., Insulin-resistant diabetes mellitus in a black woman with ataxia-telangiectasia. Southern Medical Journal, 1996. 89(6): p. 619–21. doi: 10.1097/00007611-199606000-00013 [DOI] [PubMed] [Google Scholar]
- 911.Schalch D.S., McFarlin D. E., Barlow M. H., An unusual form of diabetes mellitus in ataxia telangiectasia. New England Journal of Medicine, 1970. 282(25): p. 1396–402. doi: 10.1056/NEJM197006182822503 [DOI] [PubMed] [Google Scholar]
- 912.Cruz J.R.S., et al., Assessment of vitamin D status in common variable immunodeficiency or ataxia-telangiectasia patients. Allergol Immunopathol (Madr), 2019. 47(5): p. 499–505. doi: 10.1016/j.aller.2019.03.004 [DOI] [PubMed] [Google Scholar]
- 913.Ehlayel M., Soliman A. T., De Sanctis V., Linear growth and endocrine function in children with ataxia telangiectasia. Indian Journal of Endocrinology and Metabolism, 2014. 18(Supplement 1): p. S93–S96. doi: 10.4103/2230-8210.145079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 914.Prayle A.P., Bush A., Suri M., Bhatt J., Low Vitamin D levels in children with ataxiatelangiectasia. Archives of Disease in Childhood, 2017. Conference: p. Annual Conference of the Royal College of Paediatrics and Child Health, RCPCH 2017. United Kingdom. 102 (Supplement 1) (pp A158). [Google Scholar]
- 915.Da Silva R., Santos Valente E. C., Carvalho B. C., Vieira D. G., Ferreira C. A., Andrade I. G. A., et al., Nutritional condition related to vitamin D in patients with primary immunodeficiency. Journal of Clinical Immunology, 2012. Conference: p. 2012 Clinical Immunology Society, CIS Annual Meeting: Primary Immune Deficiency Diseases North American Conference. Chicago, IL United States. Conference Publication: (var.pagings). 32 (2) (pp 355). [Google Scholar]
- 916.Weiss B., Krauthammer A., Soudack M., Lahad A., Sarouk I., Somech R., et al., Liver Disease in Pediatric Patients With Ataxia Telangiectasia: A Novel Report. Journal of Pediatric Gastroenterology & Nutrition, 2016. 62(4): p. 550–5. doi: 10.1097/MPG.0000000000001036 [DOI] [PubMed] [Google Scholar]
- 917.Barreto T.L.N., et al., Agreement of cardiovascular risk in ataxia-telangiectasia mutated heterozygotes and their children with Ataxia-telangiectasia. Expert Opinion on Orphan Drugs, 2020. 8(6): p. 209–213. [Google Scholar]
- 918.Jiang H., Tang B. S., Hu Z. M., Xia K., Xu B., Tang J. G., et al., ATM gene mutations in Chinese patients with ataxia-telangiectasia. Chinese Journal of Medical Genetics, 2005. 22(2): p. 121–124. [PubMed] [Google Scholar]
- 919.Tennstedt A., [Contribution to the Louis-Bar syndrome (ataxia telangiectasia) (author’s transl)]. Zentralblatt fur Allgemeine Pathologie und Pathologische Anatomie, 1978. 122(5): p. 485–95. [PubMed] [Google Scholar]
- 920.Elfaituri S.S., Matoug I., Bujlawi K., Elteer A., Elsalheen H., Belrasali Y., Cutaneous manifestations of primary immunodeficiency diseases in Libyan children. JDDG—Journal of the German Society of Dermatology, 2014. Conference: p. 12th Congress of European Society for Pediatric Dermatology, ESPD 2014. Kiel Germany. Conference Publication: (var.pagings). 12 (SUPPL. 2) (pp 5). [Google Scholar]
- 921.Korting G.W., Bork K., [Overall progeroid aspect of the Louis-Bar syndrome: pigmentary and keratotic phenomena]. Hautarzt, 1979. 30(5): p. 273–5. [PubMed] [Google Scholar]
- 922.Dzieciatkowska M., Qi G., You J., Bemis K. G., Sahm H., Lederman H. M., et al., Proteomic characterization of cerebrospinal fluid from ataxia- telangiectasia (A-T) patients using a LC/MS-based label-free protein quantification technology. International Journal of Proteomics, 2011(pagination). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 923.Berkel A.I., Ersoy F., Ozsoy G., Transfer-Factor Therapy in Ataxia-Telangiectasia. Pediatric Research, 1977. 11(1): p. 53–53. [PMC free article] [PubMed] [Google Scholar]
- 924.Akarsu O.P., Atilgan C. U., Guven D., Conjunctival telangiectasia in a patient with ataxia telangiectasia: A case report. Turk Oftalmoloiji Dergisi, 2012. 42(1): p. 75–77. [Google Scholar]
- 925.Aql M.M.F., et al., Telomerase Dysfunction in the Tumorigenesis of Genetic Disorders. International Journal of Molecular and Cellular Medicine, 2021. 10(1): p. 56–67. doi: 10.22088/IJMCM.BUMS.10.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 926.Marie D., Bertille B., Geraldine J., Laurence F., Pierre V., Following and diagnostic outcome of multiple cafe-au-lait macules of chil. Pediatric Dermatology, 2018. Conference: p. 18th Annual Meeting of the European Society for Pediatric Dermatology, ESPD 2018. United Kingdom. 35 (Supplement 2) (pp S13). [Google Scholar]
- 927.Brett E.M., Ataxia Telangiectasia with Unusual Features. Proceedings of the Royal Society of Medicine, 1965. 58: p. 128–30. [PMC free article] [PubMed] [Google Scholar]
- 928.Neven B., et al., Cutaneous and visceral chronic granulomatous disease triggered by a rubella virus vaccine strain in children with primary immunodeficiencies. Clinical Infectious Diseases, 2017. 64(1): p. 83–86. doi: 10.1093/cid/ciw675 [DOI] [PubMed] [Google Scholar]
- 929.Amirifar P., et al., Ataxia-telangiectasia: A review of clinical features and molecular pathology. Pediatric Allergy and Immunology, 2019. 30(3): p. 277–288. doi: 10.1111/pai.13020 [DOI] [PubMed] [Google Scholar]
- 930.Paller A.S., Massey R. B., Curtis M. A., Pelachyk J. M., Dombrowski H. C., Leickly F. E., et al., Cutaneous granulomatous lesions in patients with ataxia-telangiectasia. Journal of Pediatrics, 1991. 119(6): p. 917–22. doi: 10.1016/s0022-3476(05)83043-4 [DOI] [PubMed] [Google Scholar]
- 931.Mitra A., Gooi J., Darling J., Boon A., Newton-Bishop J. A., Infliximab in the treatment of a child with cutaneous granulomas associated with ataxia telangiectasia. British Journal of Dermatology, 2008. 159: p. 123–123. [DOI] [PubMed] [Google Scholar]
- 932.Leung J., et al., Prevalence of Granulomas in Patients With Primary Immunodeficiency Disorders, United States: Data From National Health Care Claims and the US Immunodeficiency Network Registry. Journal of Clinical Immunology, 2018. 38(6): p. 717–726. doi: 10.1007/s10875-018-0534-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 933.Buchbinder D., Hauck F., Shcherbina A., Sullivan K. E., Perelygina L., Eloit M., et al., Rubella virus associated cutaneous granulomatous disease: A unique complication in patients with dna repair disorders. Journal of Clinical Immunology, 2018. Conference: p. 2018 CIS Annual Meeting: Immune Deficiency and Dysregulation North American Conference. Canada. 38 (3) (pp 402–403). [Google Scholar]
- 934.Goraya J.S. and Kaur S., Spectrum of Neurocutaneous Syndromes in Children in Neurology Practice. Journal of Pediatric Neurology., 2017. 22. [Google Scholar]
- 935.Davila V., et al., Rubella vaccine induced cutaneous granulomas in a patient with ataxia telangiectasia. Pediatric Dermatology, 2021. 38(SUPPL 1): p. 45–46.32767593 [Google Scholar]
- 936.Sari A., Okuyaz C., Adiguzel U., Ates N. A., Uncommon associations with ataxia-telangiectasia: vitiligo and optic disc drusen. Ophthalmic Genetics, 2009. 30(1): p. 19–22. doi: 10.1080/13816810802415256 [DOI] [PubMed] [Google Scholar]
- 937.Dhouib N.G., et al., Cutaneous Manifestations of Primary Immunodeficiency Diseases in Tunisian Children. Mediterranean Journal of Hematology and Infectious Diseases, 2018. 10. doi: 10.4084/MJHID.2018.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 938.Ong M.T., Chow G., Suri M., Whitehouse W. P., Scoliosis in children with Ataxia-Telangiectasia. Developmental Medicine and Child Neurology, 2017. Conference: p. 43rd Annual Conference of the British Paediatric Neurology Association, BPNA 2017. United Kingdom. 59 (Supplement 1) (pp 63). [Google Scholar]
- 939.Itri M., Hachim J., Mikou N., Hadj Khalifa K. K., Ataxia telangiectasia. On 4 personal cases. Pediatre, 1995. 31(147): p. 4–8. [Google Scholar]
- 940.Lefton-Greif M.A., Crawford T. O., Winkelstein J. A., Loughlin G. M., Koerner C. B., Zahurak M., et al., Oropharyngeal dysphagia and aspiration in patients with ataxia-telangiectasia. Journal of Pediatrics, 2000. 136(2): p. 225–31. doi: 10.1016/s0022-3476(00)70106-5 [DOI] [PubMed] [Google Scholar]
- 941.Stillman A.E., Larter W., Goldman D. S., Longitudinal esophageal bands associated with esophageal aperistalsis: speculations on pathogenesis. Gastroenterology, 1978. 74(3): p. 592–4. [PubMed] [Google Scholar]
- 942.Abdullah A.M., Aetiology of chronic diarrhoea in children: experience at King Khalid University Hospital, Riyadh, Saudi Arabia. Annals of Tropical Paediatrics, 1994. 14(2): p. 111–7. doi: 10.1080/02724936.1994.11747702 [DOI] [PubMed] [Google Scholar]
- 943.Ross L.J., Capra S., Baguley B., Sinclair K., Munro K., Lewindon P., et al., Nutritional status of patients with ataxia-telangiectasia: A case for early and ongoing nutrition support and intervention. Journal of Paediatrics & Child Health, 2015. 51(8): p. 802–7. doi: 10.1111/jpc.12828 [DOI] [PubMed] [Google Scholar]
- 944.Stewart E., Prayle A. P., Tooke A., Pasalodos S., Suri M., Bush A., et al., Growth and nutrition in children with ataxia telangiectasia. Archives of Disease in Childhood, 2016. 101(12): p. 1137–1141. doi: 10.1136/archdischild-2015-310373 [DOI] [PubMed] [Google Scholar]
- 945.Jauhari P., et al., Aetiology of intellectual disability in paediatric outpatients in Northern India. Developmental Medicine and Child Neurology, 2011. 53(2): p. 167–172. doi: 10.1111/j.1469-8749.2010.03823.x [DOI] [PubMed] [Google Scholar]
- 946.Casaril M., Gabrielli G. B., Capra F., Falezza G. C., [Ataxia telangiectasia. Description of a case with multiple cerebral hemorrhages and liver cirrhosis]. Minerva Medica, 1982. 73(34): p. 2183–8. [PubMed] [Google Scholar]
- 947.Boder E., Ataxia-telangiectasia: an overview. Kroc Foundation Series, 1985. 19: p. 1–63. [PubMed] [Google Scholar]
- 948.Miyata R., Kaneko S., Hayashi M., Itoh M., Basal ganglia lesion in two autopsy cases of ataxia telangiectasia. Neuropathology, 2012. Conference: p. 53rd Annual Meeting of the Japanese Society of Neuropathology. Niigata Japan. Conference Publication: (var.pagings). 32 (3) (pp 361). [Google Scholar]
- 949.Mitui M., Castellvi-Bel S., Coutinho G., Huo Y., Sun X., Gatti R. A., Common founder mutations among Hispanic patients with ataxia-telangiectasia (A-T). American Journal of Human Genetics, 2001. 69(4): p. 415–415. [Google Scholar]
- 950.Bottini A.R., Gatti R. A., Wirenfeldt M., Vinters H. V., Heterotopic Purkinje cells in ataxia-telangiectasia. Neuropathology, 2012. 32(1): p. 23–9. doi: 10.1111/j.1440-1789.2011.01210.x [DOI] [PubMed] [Google Scholar]
- 951.Hecht F. and McCaw B.K., Letter: Chromosomally marked lymphocyte clones in ataxia-telangiectasia. Lancet, 1974. 1(7857): p. 563–4. doi: 10.1016/s0140-6736(74)92747-0 [DOI] [PubMed] [Google Scholar]
- 952.Fares F., Axelord Ran S., David M., Zelnik N., Hecht Y., Khairaldeen H., et al., Identification of two mutations for ataxia telangiectasia among the Druze community. Prenatal Diagnosis, 2004. 24(5): p. 358–62. doi: 10.1002/pd.874 [DOI] [PubMed] [Google Scholar]
- 953.Perry T.L., Kish S. J., Hinton D., Hansen S., Becker L. E., Gelfand E. W., Neurochemical abnormalities in a patient with ataxia-telangiectasia. Neurology, 1984. 34(2): p. 187–91. doi: 10.1212/wnl.34.2.187 [DOI] [PubMed] [Google Scholar]
- 954.Severi F., Ugazio A. G., Magrini U., Bianchi E., Pedroni E., Burgio V. L., Unusual combination of immune and endocrine deficiencies. A possible case of early-onset Louis-Bar syndrome. Helvetica Paediatrica Acta, 1976. 31(4–5): p. 395–405. [PubMed] [Google Scholar]
- 955.Zielen S., Comment on: Treatment of EBV-Associated Nodular Sclerosing Hodgkin Lymphoma in a Patient With Ataxia Telangiectasia With Brentuximab Vedotin and Reduced COPP Plus Rituximab. Pediatric Blood & Cancer, 2016. 63(5): p. 946. [DOI] [PubMed] [Google Scholar]
- 956.Selevestru R, Tomacinschi C, and Sciuca S, Pulmonary infections in primary immunodeficiencies to children. Allergy, 2018. 73. [Google Scholar]
- 957.Salman M.S., Lee E. J., Tjahjadi A., Chodirker B. N., The epidemiology of intermittent and chronic ataxia in children in Manitoba, Canada. Developmental Medicine & Child Neurology, 2013. 55(4): p. 341–7. doi: 10.1111/dmcn.12081 [DOI] [PubMed] [Google Scholar]
- 958.Gathmann B., et al., The German national registry for primary immunodeficiencies (PID). Clinical and Experimental Immunology, 2013. 173(2): p. 372–380. doi: 10.1111/cei.12105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 959.Schroeder S.A., Zielen S., Infections of the respiratory system in patients with ataxia-telangiectasia. Pediatric Pulmonology, 2014. 49(4): p. 389–99. doi: 10.1002/ppul.22817 [DOI] [PubMed] [Google Scholar]
- 960.Crawford T.O., Skolasky R. L., Fernandez R., Rosquist K. J., Lederman H. M., Survival probability in ataxia telangiectasia. Archives of Disease in Childhood, 2006. 91(7): p. 610–1. doi: 10.1136/adc.2006.094268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 961.Donath H., et al., Progressive Liver Disease in Patients With Ataxia Telangiectasia. Frontiers in Pediatrics, 2019. 7 (no pagination)(458). doi: 10.3389/fped.2019.00458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 962.Yildiran A., Celiksoy M. H., Guner S. N., Borte S., Unusual Clinical Presentation and Hemophagocytosis of Ataxia-Telangiectasia in Two Siblings with a Rare Mutation. Journal of Clinical Immunology, 2014. 34(6): p. 732–732. [Google Scholar]
- 963.Saha K., Chopra K., Primary immune disorders in children and their diagnosis. Journal of Communicable Diseases, 1984. 16(1): p. 11–7. [PubMed] [Google Scholar]
- 964.Cawley L.P., Schenken J. R., Monoclonal hypergammaglobulinemia of the gamma M type in a nine-year-old girl with ataxia-telangiectasia. American Journal of Clinical Pathology, 1970. 54(6): p. 790–801. doi: 10.1093/ajcp/54.6.790 [DOI] [PubMed] [Google Scholar]
- 965.Kumar G.K., Amjad H., Hageman factor deficiency in ataxia telangiectasia. American Journal of the Medical Sciences, 1976. 272(3): p. 353–5. doi: 10.1097/00000441-197611000-00014 [DOI] [PubMed] [Google Scholar]
- 966.Vos S., Christmann M., Pietzner J., Hoche F., Schubert R., Zielen S., Growth hormone deficiency and immune status in patients with ataxia telangiectasia. Allergy: European Journal of Allergy and Clinical Immunology, 2012. Conference: p. 31st Congress of the European Academy of Allergy and Clinical Immunology. Geneva Switzerland. Conference Publication: (var.pagings). 67 (SUPPL. 96) (pp 274). [Google Scholar]
- 967.Sute M.B., et al., Cytogenetic studies in chromosome instability syndromes. Indian Journal of Human Genetics, 2014. Conference: p. International Symposium on ’Genomics in Health and Disease’ and 40th Annual Conference of Indian Society of Human Genetics. Mumbai India. Conference Publication: (var.pagings). 20 (5 SUPPL. 1) (pp S76). [Google Scholar]
- 968.Celiksoy M.H., et al., A Case of Ataxia-telangiectasia Presented With Hemophagocytic Syndrome. Journal of Pediatric Hematology Oncology, 2018. 40(8): p. e547–e549. doi: 10.1097/MPH.0000000000001134 [DOI] [PubMed] [Google Scholar]
- 969.Arkel Y.S., Kinchelow T. E., Oleske J., Searle B. M., Desposito F., Ataxia telangiectasia with thrombasthenia, platelet dysfunction, and a chromosomal translocation. A monoclonal defect? American Journal of Pediatric Hematology/Oncology, 1981. 3(1): p. 27–33. [PubMed] [Google Scholar]
- 970.Kudryashov S., et al., Rheumatologic diseases as presentations of primary immunodeficiency diseases. Annals of the Rheumatic Diseases, 2021. 80(SUPPL 1): p. 969. [Google Scholar]