Abstract
The WHO recently included Gaming Disorder as a psychiatric diagnosis. Whether there are distinct groups of adolescents who differ based on severity of gaming disorder and their relationships with other mental health and addictive behavior outcomes, including problematic smartphone use (PSU), remains unclear. The current study explored and identified subtypes of Internet Gaming Disorder (IGD) severity and estimated the association between these subtypes and other disorders. Participants completed online questionnaires assessing the severity of IGD, PSU, depression, and anxiety during COVID-19. We conducted a latent class analysis of IGD symptoms among 1,305 Chinese adolescents (mean age = 15.2; male = 58.5%) from 11 secondary schools in Macao (SAR), China. Multinomial logistic regression estimated correlates of latent class membership and PSU. A 4-class model adequately described the sample subgroups. Classes were labeled as normative gamers (30.9%), occasional gamers (42.4%), problematic gamers (22.7%), and addictive gamers (4.1%). Relative to normative gamers, PSU severity, depression, and being male were significantly higher among problematic gamers, addictive gamers, and occasional gamers. Only problematic gamers showed significant positive associations with anxiety severity compared to the other groups. The study revealed the differences in severity of gaming disorder and its association with psychopathology outcomes. Application in screening for IGD and comorbidity is discussed.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12144-022-03133-8.
Keywords: Latent class analysis, Internet gaming disorder, Problematic smartphone use, Adolescent
Introduction
Due to the concerning repercussion resulting from maladaptive gaming, Internet gaming disorder (IGD) was listed under 6C51 in the most recent edition of the International Classification of Diseases (ICD-11) as an official psychiatric diagnosis (World Health Organization, 2019) and was also proposed for inclusion in the DSM-5 (American Psychiatric Association, 2013). IGD is defined by symptoms including loss of control over gaming, prioritizing gaming over other relevant daily activities and continuing gaming despite negative consequences over a time course of 12 months. IGD impairs people’s social, academic, and occupational functioning (American Psychiatric Association, 2013; Macao Association for Internet Research, 2020; Petry et al., 2015; Wichstrøm et al., 2019), including poor relationships with peers or family (Dreier et al., 2017; Hwang et al., 2020; Schneider et al., 2017; Strittmatter et al., 2015; Sugaya et al., 2019; Yang et al., 2020) and lower academic performance (Hawi et al., 2018; Ko et al., 2020; Müller et al., 2015; Wang et al., 2014; Zhang et al., 2019).
Because of the ubiquity of the Internet and the easy access to mobile phones among youth, subsequently, their risk of internet-related behavioral problems also increased exponentially (Anderson & Jiang, 2018; Chia et al., 2020; Geisel et al., 2021). Around the globe, a recent meta-analysis (Stevens et al., 2021) revealed a prevalence of gaming disorder was 3.1% worldwide. A high prevalence of Internet addition among youth in Asia were previously observed. The prevalence was 21.2% in Vietnam (Tran et al., 2017), 21% in Philippines (Mak et al., 2014), 20% in Korea (Ha et al., 2006), 17.9% in Taiwan (Tsai et al., 2009); 17.1% in Singapore (Mythily et al., 2008), 16.4% in Hong Kong (Mak et al., 2014), 14.1% in Malaysia (Mak et al., 2014), 6.2% in Japan (Mak et al., 2014), and 13% among adolescents in China (Yang et al., 2020). Across Asia, children and adolescents in East Asian countries, such as China, reported the highest prevalence rates (Paulus et al., 2018). The high prevalence of IGD among Chinese youth is concerning, particularly in the coronavirus disease (COVID-19) context, children and adolescents spent most of their time at home using the Internet during the lockdown, and this might increase video game use and probable IGD (Teng et al., 2021).
IGD and Psychopathological Outcomes
IGD demonstrates high comorbidity with PSU, in which the two problems share similar characteristics (Lin et al., 2017). However, only IGD is classified as an addictive disorder in the psychiatric nosology. It is also difficult to disentangle the purpose of smartphone use whether it is to engage in gaming behavior or other activities (Montag et al., 2021). Smartphones allow gamers to stay in touch with each other either within the game platform or through other gaming-related activities including social media, which is associated with greater IGD severity (King & Delfabbro, 2018). This relationship is also bidirectional such that some studies found that smartphone gaming is a risk factor for PSU (Fischer-Grote et al., 2019; Jeong et al., 2016).
IGD is also associated or comorbid with other mental health problems, including depression (Liu et al., 2016; Yuan et al., 2021), anxiety (Schou Andreassen et al., 2016; Wu et al., 2018), and stress symptoms (Andreetta et al., 2020; Yen et al., 2019), which are considered as predictive factors of gaming-related behavior (Hyun et al., 2015; Laconi et al., 2017). Cross-sectional studies that adopted different measurements for gaming problems found positive association with depression (Gaming Addiction Scale; Männikkö et al., 2015) and anxiety (Problematic Videogame Playing; Fumero et al., 2020) in adolescents. Symptoms of anxiety and depression before the pandemic predicted later IGD and videogame use (Teng et al., 2021). IGD is also associated with psychiatric disorders in young people including attention deficit and hyperactivity disorder and alcohol misuse (Ho et al., 2014) as well as illicit drug use (Sun et al., 2012). Internet used as a coping strategy for psychiatric comorbidity may perpetuate IGD because young people suffering from IGD often avoid socialization with other people (Zhang et al., 2018). IGD was found to affect sleep quality (Zhang et al., 2017) and lead to negative impact on health-related quality of life (Tran et al., 2017) among adolescents in Asia.
The COVID-19 pandemic has a vital impact on adolescents’ mental health. Compared to Chinese adults, adolescents were more affected in the beginning of COVID-19 outbreak, and it showed higher impact on youth mental health (i.e., depression, anxiety, and stress) (Wang et al., 2020a, 2020b). After one month of COVID-19 outbreak in China, Chinese adolescents were impacted more than before. This may be due to their long-term online study from home (Wang et al., 2020a, 2020b). In a cross-sectional study conducted during the COVID-19 outbreak in China among adolescents from grade 7 to grade 12 and first year in university, Ren et al. (2021) found that among them, the prevalence of anxiety was 28.3%, and 2.1% of them presented with severe anxiety, whereas the prevalence of depression was 30.8%, and 1.3% was severe. The comorbidity of anxiety and depression was also high, and estimated to be around 20.1% of the Chinese adolescents. With the increasing risk of psychopathology (e.g., depression and anxiety) and academic stress during COVID-19 (Cullen et al., 2020; Pfefferbaum & North, 2020), adolescents may be more susceptible to gaming-related behavior.
Theoretical Frameworks
This study is guided by two theoretical models. First, the Interaction of Person-Affect-Cognition-Execution model (I-PACE) (Brand et al., 2016, 2019) suggests that core personal characteristics (e.g., psychopathology, biopsychological constitution), cognitive and affective responses to perceived situations, decision-making behavior about using a certain application, and the consequences of using it drives some people to excessively use the internet. When individuals experience high levels of depression and anxiety (psychopathology factors), and high levels of stress (stimuli) trigger the cognitive and affective responses, they may be motivated to use certain applications more to gain gratification, which then reinforces more use. Second, Compensatory Internet Use Theory (Kardefelt-Winther, 2014) explains the underlying mechanism of how negative life events or negative emotion give rise to compensatory internet use, which helps to mitigate negative affect. Through the process of gratification-seeking, once an individual’s internet use becomes excessive, negative consequences may lead to a higher degree of stabilization of psychopathology factors. In other words, in individuals who are experiencing depression, anxiety or stress, these negative emotions may motivate them, to seek an escape from their daily life struggles (Melodia et al., 2020), by playing more Internet games in order to compensate for negative emotions. Once they gain gratification, those negative emotions may decrease, but it can result in more long-term negative outcomes.
A Person-Centered Approach to Understand IGD
Different from a data-centered approach, latent class analysis (LCA), is a statistical approach used to identify heterogeneous sub-groups within a larger population according to their item responses, which can identify types of IGD based on symptom patterns. It can also incorporate data from observed covariates to understand their correlation with latent class subgroup membership. LCA assumes that the structure of the observed multivariate data results from a categorical latent (class membership) variable.
Several studies applied LCA among adolescents with IGD using different scales to measure the heterogeneity of IGD in terms of symptom endorsement severity. A 4-class model of latent classes of PVP (Problem Video Game Playing), which classified participants as “Severe PVP” (1.9%), “High PVP” (12.2%), “Low PVP” (36%), and “Normative” (50%) due to the lowest probabilities of PVP scale item endorsement in Canadian young people (Faulkner et al., 2015). Myrseth and Notelaers (2018) found a 5-class model of Gaming Addiction, including a “never symptoms of addiction” (46.2%), “rarely symptoms of addiction” (22.3%), “occasionally symptoms of addiction” (23.5%), “problem gamers” (6.9%), and “disordered gamers” (1.2%) among Norwegian adolescents, while another 5-class model was identified from Scale for the Assessment of Internet and Computer Game Addiction—Gaming Module (AICA-S), with the majority being in a “Normative” class (61.8%), followed by “Concerned” (23.6%), “Engaged” (7.3%), “At-Risk” (5.1%), and “IGD” (2.2%), among European young gamers (Colder Carras & Kardefelt-Winther, 2018).
These studies were based on symptom items of gaming-related scales, classifying subtypes of gamers using the person-centered (LCA) approach, and measuring subtype associations with psychopathological variables (e.g., depression), but did not study other problematic use of digital technology, such as PSU, which is often associated with gaming (Elhai et al., 2020; Fischer-Grote et al., 2019; Jeong et al., 2016; Yuan et al., 2021). Meanwhile, to our knowledge, there has not been studies that have conducted LCA of IGD symptoms in Chinese youth.
Study Aim
The study explored the subtypes of IGD and its relationship with PSU, depression, and anxiety using a person-centered approach. Due to the inconsistent findings, and lack of investigations among Chinese youth, we have also investigated covariates (age and gender) to understand which individuals may be associated with the different subgroups of IGD among Chinese adolescents (Dreier et al., 2017; Hawi et al., 2018; Macur & Pontes, 2021; Schou Andreassen et al., 2016; Su et al., 2020). Based on previous studies (Colder Carras & Kardefelt-Winther, 2018; Faulkner et al., 2015; Myrseth & Notelaers, 2018), we hypothesized that there will be an optimal model with 4 to 6-classes. We expect that some of the IGD subtypes will be associated with PSU, depression, anxiety and stress. Finally, a positive association between IGD and PSU are hypothesized.
Method
Participants and Procedure
Thirty-eight secondary schools in Macao (SAR), China were invited and eleven agreed to participate in this study by a local student association from June to July 2020. Informed consent from parents and assent from children was obtained electronically. The online survey took around 15 min to complete.
In our final sample, a total of 1,785 valid responses with both parent consents and student assents were collected using Qualtrics. Among them, 78 (4.36%) were removed due to missing data, and 402 (22.5%) were excluded because they did not report playing video games. Therefore, the final sample includes 1,305 participants between 13–21 years old (M = 15.16, SD = 1.66). Demographic information of the participants is shown in Table 1.
Table 1.
Descriptive statistics of demographic characteristics, IGD, PSU, depression, anxiety, and stress
| N(%) | Mean | SD | |||
|---|---|---|---|---|---|
| Age | 1305 | 15.16 | 1.66 | ||
| Gender | Male | 763 (58.5%) | |||
| Female | 542 (41.5%) | ||||
| Grade | Junior High | 781 (59.8%) | |||
| Senior High | 524 (40.2%) | ||||
| Have smartphone | Yes | 1275 (97.7%) | |||
| No | 30 (2.3%) | ||||
| IGD | 2.51 | 2.30 | |||
| Cumulative scores | 0 | 313 (24.0%) | |||
| 1 | 226 (17.3%) | ||||
| 2 | 210 (16.1%) | ||||
| 3 | 170 (13%) | ||||
| 4 | 121 (9.3%) | ||||
| 5 | 106 (8.1%) | ||||
| 6 | 69 (5.3%) | ||||
| 7 | 43 (3.3%) | ||||
| 8 | 27 (2.1%) | ||||
| 9 | 20 (1.5%) | ||||
| PSU | 31.35 | 10.86 | |||
| Male | < 31 | 369 (28.3%) | |||
| ≥ 31 | 374 (28.7%) | ||||
| Female | < 33 | 224 (17.2%) | |||
| ≥ 33 | 308 (23.6%) | ||||
| Depression | 8.80 | 8.81 | |||
| 0–9 | 790 (60.5%) | ||||
| > 9 | 515 (39.5%) | ||||
| Anxiety | |||||
| 0–7 | 694 (53.2%) | ||||
| > 7 | 611 (46.8%) | ||||
| Stress | 10.95 | 8.82 | |||
| 0–14 | 913 (70.0%) | ||||
| > 14 | 392 (30.0%) |
Measures
Internet Gaming Disorder Scale (IGDS)
The IGDS is a 9-item self-report scale developed according to the DSM-5 diagnostic criteria of IGD measuring Internet gaming activities in the past 12 months by a dichotomous response format, 0 = No and 1 = Yes (Lemmens et al., 2015). The Chinese version has demonstrated excellent reliability (KR-20 = 0.91) and criterion and structural validity among Chinese sample (Sigerson et al., 2017). A higher total score indicates greater IGD severity. In the current study, KR-20 (i.e. internal consistency) was 0.77.
Short Version of the Smartphone Addiction Scale (SAS-SV)
The 10-item SAS-SV was designed to measure severity of PSU in terms of associated health and social impairment, withdrawal, and tolerance, using a 6-point Likert scale from 1 = strongly disagree to 6 = strongly agree (Kwon et al., 2013). The cut-off scores of 31 for male and 33 for female were used for adolescents (Kwon et al., 2013). Higher total scores indicated greater PSU. The Chinese version demonstrated good internal consistency (Cronbach’s α = 0.86) and convergent validity among Chinese adolescents (Cheung et al., 2019). Internal consistency in our sample was 0.90.
Depression, Anxiety, Stress Scale-21 (DASS-21)
The Chinese version of DASS-21 is a 21-item self-report measure with three subscales measuring depression, anxiety, and stress in the past week (Lovibond & Lovibond, 1995; Moussa et al., 2001). Each subscale comprises 7 items with a rating from 0 = did not apply to me at all to 3 = applied to me very much, or most of the time. The cut-off scores are 9, 7, and 14 for the depression, anxiety, and stress sub-scales, respectively (Lovibond & Lovibond, 1995). The scale showed good internal consistency, convergent and discriminant validity among Chinese youth (Wang et al., 2016). Cronbach’s α of depression, anxiety, and stress in our sample were 0.86, 0.81 and 0.83, respectively.
Statistical Analysis
The statistical analyses were conducted in three steps. First, Pearson correlations among covariates and IGD were analyzed with SPSS version 24 (IBM Corp, 2016). Second, latent class analysis was conducted to determine the number of latent classes based on the IGD item responses. Optimal model fit (i.e., the number of latent classes) was determined by comparing the Bayesian information criterion (BIC), Akaike’s information criterion (AIC), and sample-size adjusted Bayesian information criterion (SABIC). Lower values indicate better model fit. The Vuong Lo-Mendell-Rubin likelihood ratio test (V-LMR), adjusted Lo-Mendell-Rubin likelihood ratio (ALMR LR), and Bootstrapped likelihood ratio test (BLRT) were used to compare model fit improvement between models with k vs. k-1 classes, with statistical significance indicating improved fit when adding the additional class (Wang & Wang, 2019). Entropy values were used to determine better quality of model classification, with larger values close to 1 indicating improved quality of model classification. Third, multinomial logistic regression analysis was conducted to determine the association between covariates (i.e., PSU, depression, anxiety, stress, and gender) and latent class membership. LCA and multinomial logistic regression were performed by Mplus software version 7.4 (Muthén & Muthén, 1998–2015). We used odds ratios to determine the relationship between covariates and class membership. Odds ratios represent the odds of how the covariate is associated with membership in the index class when compared to the reference class (Wang & Wang, 2019).
Ethics
All procedures of the present study were carried out in accordance with the Helsinki Declaration. The ethical approval was obtained from the Research Ethics Committee of the University of Macau. Informed consent was provided and obtained from all participants in the study. Parental consent was obtained for those younger than 18 years of age.
Results
Correlations
Bivariate Pearson correlations among covariates and IGD are presented in Table 2.
Table 2.
Bivariate Pearson Correlations among study variables
| age | gender | IGD | PSU | depression | anxiety | stress | |
|---|---|---|---|---|---|---|---|
| Age | 1 | ||||||
| Gender | .000 | 1 | |||||
| IGD | -.055* | .161** | 1 | ||||
| PSU | -.046 | .015 | .065* | 1 | |||
| Depression | .088** | -.088** | .301** | .061* | 1 | ||
| Anxiety | .081** | -.087** | .258** | .013 | .752** | 1 | |
| Stress | .087** | -.076** | .311** | .015 | .783** | .800** | 1 |
Note. IGD = Internet gaming disorder; PSU = Problematic smartphone use
*p < .05. ** p < .01
LCA Model of IGD
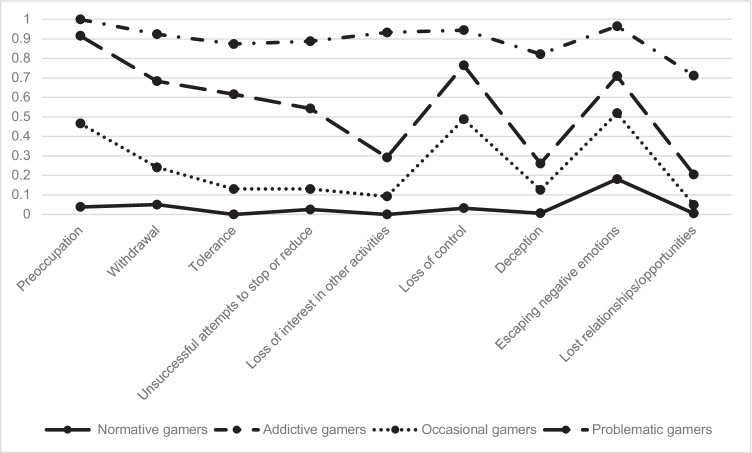
Table 3 shows results of the 2-, 3-, and 4-class models. The probability distribution and endorsement on IGDS items of the four classes are presented in Table A.1 and Fig. 1. The 3-class model had smaller BIC (11,208.103) and higher entropy (0.717) than the 4-class model (BIC = 11,233.042; entropy = 0.686); however, the 4-class model had smaller AIC (11,031.257) and SABIC (11,109.157). Although LMR-LR and VLMR were not significant in the 4-class model, the BLRT (p < 0.0001) was statistically significant, which meant that the 4-class model is superior (Nylund et al., 2007; Wang & Wang, 2019). Therefore, the 4-class model was selected.
Table 3.
The number of latent IGD classes
| Classification criterion | Number of latent class | ||
|---|---|---|---|
| 2 | 3 | 4 | |
| BIC | 11,338.408 | 11,208.103 | 11,233.042 |
| AIC | 11,240.103 | 11,058.058 | 11,031.257 |
| SABIC | 11,278.054 | 11,115.984 | 11,109.157 |
| Vuong-LMR test | p = 0.0000 | p = 0.0001 | p = 0.1555 |
| LMR-LR | Value = 1576.115 (p = 0.0000) | Value = 199.267 (p = 0.0001) | Value = 46.158 (p = 0.1590) |
| ***BLRT | p = 0.0000 | p = 0.0000 | p = 0.0000 |
| Entropy | 0.780 | 0.717 | 0.686 |
Note. LMR = Lo-Mendell-Rubin likelihood ratio test; BLRT = Bootstrapped likelihood ratio test; statistically significant: p < .05
Fig. 1.
Latent Class Model Profiles Based On IGDS Symptom Items. Note. X-Axis: Symptom Items Of IGD; Y-Axis: Probability Of Item Endorsement
Overall, the four classes vary across each other based on the severity of IGD symptoms. We labeled Class 1 as Normative Gamers (30.9%) that the lowest probabilities of endorsing all symptom items (near 0%), apart from a greater tendency to endorse escaping negative emotions (18.1%) than other symptom items. Class 2 was labeled as Addictive Gamers (4.1%) due to the highest endorsement on all symptom items, which ranged from 0.712 for the item of loss of relationships/opportunities to 1 for the item of preoccupation. We labeled Class 3 as Occasional Gamers (42.4%) due to elevated symptoms of IGD relative to Normative Gamers; meanwhile, Class 4 was labeled as Problematic Gamers (22.7%), which were differentiated from Addictive Gamers by having a lower probability on symptom items of unsuccessful attempts to stop or reduce gaming behavior (54.3%) and loss of interest in other activities (29.2%).
Multinomial Logistic Regression Model
In the multinomial logistic regression analysis, 30 participants were excluded due to missing values (2.3%) from the smartphone use responses (i.e., having no smartphone). Normative Gamers was the reference group because this class showed the lowest probabilities of IGD symptom endorsement.
Compared to Normative Gamers, gender, PSU, and depression were statistically significant and positively associated with the Addictive Gamers, Occasional Gamers and Problematic Gamers. Also, only anxiety was statistically significant and positively associated with the Problematic Gamers class (Table 4).
Table 4.
Multinomial logistic regression between latent class membership and covariates
| Covariates | B | SE of B | p | Odds ratio | |
|---|---|---|---|---|---|
| Class 2 | Intercept | -4.777 | 0.534 | 0.000 | |
| Age | 0.241 | 0.320 | 0.452 | 1.272 | |
| Gender | 1.405 | 0.382 | 0.000 | 4.076 | |
| PSU | 1.375 | 0.364 | 0.000 | 3.953 | |
| Depression | 1.473 | 0.402 | 0.000 | 4.361 | |
| Anxiety | 0.012 | 0.454 | 0.978 | 1.012 | |
| Stress | 0.450 | 0.371 | 0.225 | 1.569 | |
| Class 3 | Intercept | -0.835 | 0.146 | 0.000 | |
| Age | 0.221 | 0.138 | 0.108 | 1.248 | |
| Gender | 0.517 | 0.138 | 0.000 | 1.678 | |
| PSU | 1.138 | 0.143 | 0.000 | 3.120 | |
| Depression | 0.383 | 0.192 | 0.046 | 1.466 | |
| Anxiety | 0.172 | 0.177 | 0.332 | 1.188 | |
| Stress | -0.234 | 0.204 | 0.251 | 0.791 | |
| Class 4 | Intercept | -3.065 | 0.239 | 0.000 | |
| Age | -0.129 | 0.178 | 0.468 | 0.879 | |
| Gender | 1.452 | 0.188 | 0.000 | 4.273 | |
| PSU | 2.043 | 0.195 | 0.000 | 7.714 | |
| Depression | 0.802 | 0.230 | 0.000 | 2.230 | |
| Anxiety | 0.430 | 0.218 | 0.048 | 1.537 | |
| Stress | 0.134 | 0.229 | 0.558 | 1.143 |
Note. Class 2 = Addictive gamers; Class 3 = Occasional gamers; Class 4 = Problematic gamers; Reference group: Class 1 = Normative gamers; Statistically significant: p < .05
Discussion
The present study investigated latent subgroups of IGD and its relationship with demographic and psychopathological variables among adolescents in Macao, China during the COVID-19 pandemic.
LCA of IGD
We found that the 4-class model had the best fit. Aligned with Faulkner et al. (2015) our results identified Normative Gamers group who showed little or no IGD symptoms, Problematic Gamers group and Occasional Gamers group, which are two types of gamers with parallel symptom patterns but different severity, and the Addictive Gamers group, who reported the highest level of symptoms. When examining the differences closely across the four groups, the different level of loss of interest in other activities and unsuccessful attempts to stop or reduce differentiate Addictive Gamers and Problematic Gamers. Consistent with Wichstrøm et al. (2019)’s findings, our study found that loss of interest might serve as a central symptom in the assessment of IGD and its related impairment. Gamers are usually fed with intensive and short-term stimuli which could engender gamers’ quick gratification or pleasure at the present. Therefore, gamers are habituated to respond to only certain types of stimulations, meaning that their attention is actually trapped or narrowed down to a very limited and fixed area (Berardi, 2015), rather than deferring their immediate relief to explore other activities and think more deeply (Moore, 2018). Biologically, such a trap of attention or interest also hinders the development of new synaptic pathways in prefrontal cortex, which is a region crucial for learning (Lewis, 2015). As a result, the loss of interest makes it more difficult for gamers to create new neural connections and learn new knowledge. To differentiate clinically problematic gamers from other gamers, symptoms of withdrawal, tolerance, and unsuccessful attempts to stop or reduce gaming are also suggested as potential symptoms or criteria in this study, which is also consistent with previous research among Norwegian youth (Wichstrøm et al., 2019).
Problematic Gamers showed higher probabilities of IGD symptoms than Occasional Gamers on all symptoms, especially in withdrawal, tolerance, and unsuccessful attempts to stop or reduce gaming, despite their parallel patterns of IGD symptoms. Previous studies showed that these three symptoms were associated with gaming involvement (Wichstrøm et al., 2019) and gaming-related negative outcomes (Colder Carras & Kardefelt-Winther, 2018), including impairments in relationships and school achievement. This is consistent with the theory of psychosocial dislocation (Alexander, 2010) that those who are dislocated socially and psychologically depend heavily on certain activities to compensate their feelings of alienation or dislocation, even knowing that these activities are harmful to them.
Furthermore, in addition to the symptom of loss of interest, withdrawal and tolerance were also important criteria in measuring IGD (Rehbein et al., 2015). However, the current results did not suggest that withdrawal, tolerance, and unsuccessful attempts to stop or reduce have a strong association with the Occasional Gamers. Since similar symptoms were found in other substance use or addictive behaviors, further studies on IGD assessment criteria of withdrawal are still needed (Kaptsis et al., 2016). In current study, these three symptoms indicate that differences in the assessment of IGD also are important criteria for differentiating subgroups of IGD.
Latent Class and Psychopathological Variables
Previous studies found that mobile games or social platforms for game interaction are associated with PSU (Cha & Seo, 2018; Fischer-Grote et al., 2019; Liu et al., 2016; Rozgonjuk et al., 2020) and noted that the economic models of current game industry and social platforms tend to create some online functions which could exploit users' cognitive and affective mechanisms (Moore, 2017; Parisi, 2016). Greater internet social interaction had lower awareness of problematic gaming, and a higher level of problems related to mental health, whereas awareness of their IGD could be a protective factor against PSU (Cha & Seo, 2018; Colder Carras et al., 2017). However, these studies are limited to mobile gaming/social media. The current research extended the literature to IGD and showed PSU was significantly positively associated with all subgroups of gamers, relative to Normative Gamers. Among them, Problematic Gamers showed a strong relationship with PSU severity, which revealed a relationship between PSU and IGD severity. Previous studies (Fischer-Grote et al., 2019; Jeong et al., 2016) showed that gaming was the risk factor for PSU, whereas the current study supported an opposite direction, which might indicate the relationship between IGD and PSU is bidirectional.
We found that different subgroups of gamers were associated with different mental health problems during the pandemic when local in-person school suspension occurred. Depression and anxiety were associated with IGD (Schou Andreassen et al., 2016; Wu et al., 2018; Yuan et al., 2021). Preexisting anxiety and depression before the COVID-19 pandemic predicted IGD severity during the pandemic (Teng et al., 2021). Our results showed that compared with Normative Gamers, there was a significant positive association between all subgroups (especially Addictive Gamers) with depression severity. However, only Problematic Gamers showed significant positive association with anxiety severity compared to other subgroups of gamers. In other words, Problematic Gamers showed more PSU and anxiety symptoms whereas Addictive Gamers showed more depressive symptoms, which contradicted previous work that showed no associated between gaming symptoms and poorer mental health (Colder Carras & Kardefelt-Winther, 2018; Faulkner et al., 2015). The result also revealed an inconsistent relationship between anxiety and IGD subgroups, in that anxiety symptoms were not a risk factor for Addictive Gamers (Wichstrøm et al., 2019). These findings are in line with the I-PACE model (Brand et al., 2016) and can be explained such that gamers experiencing higher levels of depression or anxiety (as psychopathological factors in I-PACE), and then played more games to gain more satisfaction and mitigate negative outcomes or emotions. Moreover, consistent with previous studies (Macur & Pontes, 2021; Su et al., 2020), our results indicate that male adolescents were more likely to participate in gaming behavior.
Limitations and Future Directions
The study has limitations. First, data from a convenience sample of middle school students may not be representative of the broader population. Second, causal relationships between the variables might not be inferred due to cross-sectional design of the study. Therefore, further research is needed to explore the longitudinal relationships. Third, because of the differences between the diagnostic criteria of IGD established by the WHO and those by APA, the present study design might benefit from being repeated using assessment tools that include the framework of the APA and explore this concerning newly derived criteria in the WHO ICD-11, for instance with the Gaming Disorder Test, which is also readily available in Chinese language (Pontes et al., 2021). Although there are overlaps when diagnosing Gaming Disorder and Internet Gaming Disorder according to the WHO/APA, applying both framework in the same sample also led to differences in prevalence (Montag, Lachmann, et al., 2019; Montag, Schivinski, et al., 2019).
Evidence-based interventions could be used to address IGD in the digital age and during COVID-19. Cognitive-behavioral therapy (CBT) was found efficacious in reducing IGD symptoms and factors associated with IGD (i.e., depressive and anxiety symptoms), with moderate to large effect sizes (Stevens et al., 2019). Digital interventions (e.g., internet-based CBT; iCBT) delivered through mobile app or the Internet could be an ideal clinical practice due to the increasing use of telehealth therapy during the pandemic. Thus, the use of the Internet and socialization through the Internet is more frequent than before. Evidence from previous studies on digital or internet CBT showed that technology-supported CBT can effectively improve the psychopathological factors associated with IGD such as level of anxiety and depression (Ho et al., 2020), maladaptive coping skills (Ho et al., 2020), and sleep-related issues such as insomnia (Soh et al., 2020). In addition, the delivery of CBT through the Internet or smartphone is low-cost and easy to access with minimal geographical constraints. Clinical professionals could provide CBT content through a learning platform to people with IGD in educational settings (Zhang & Ho, 2017a, 2017b). Furthermore, virtual reality therapy was found effective, although it requires the use of screens and devices, such as virtual machines (Zhang & Ho, 2017a, 2017b). To conclude, digital evidence-based interventions are low-cost and effective to reduce IGD and mood symptoms in people with IGD and, therefore, promising to address mental health problems in the midst of COVID-19 (Sit et al., 2021).
Conclusions
The present study used the person-centered approach (LCA) to identify 4 classes of IGD that were differentiated based on IGDS symptoms. Gender (i.e., being male). PSU and depression were associated with all classes of IGD while anxiety was only positively associated with the Problematic Gamers class, which contributes to the framework of clinical assessment of gaming-related behavior and indicated that different classes of gamers might present different mental health problems. Clinical professionals should emphasize the relationship between IGD and PSU, to evaluate, prevent, and intervene in adolescents with IGD. Moreover, continued mental health support is needed in school settings, and interventions need to be developed to address digital-related behavioral addition, especially among male adolescents. Other policy strategies to consider may include the promotion of ethical gaming designs, in particular Freemium games, on the smartphone, to foster healthy gameplay (Montag, Lachmann, et al., 2019; Montag, Schivinski, et al., 2019).
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the General Association of Chinese Students for collecting data from the schools and students who participated in the study.
Authors’ Contribution
CIC: Writing – Original Draft, Formal analysis. HFS: Writing – Original Draft, Data
Curation, Investigation. TC: Writing- Original Draft. CC: Writing – Review & Editing. JS: Writing – Review & Editing. BC: Writing – Review & Editing. CM: Writing – Review & Editing. JE: Writing – Review & Editing. BJH: Conceptualization, Methodology, Supervision, Writing – Original Draft. All the authors contributed to the manuscript and have approved the final version of the manuscript.
Funding sources
Funding for this project was from the Macao SAR Government project: MYRG2019-00120-FSS. The funding source had no role in the study design, collection, analysis, or interpretation of data, writing the manuscript, and decision to submit the manuscript for publication.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
Portions of these findings were presented as e-poster in the 20th WPA World Congress of Psychiatry. All other authors declare that they have no conflicts of interest.
Ethics
All procedures of the present study were carried out in accordance with the Helsinki Declaration. The ethical approval was obtained from the Research Ethics Committee of University of Macau Informed consent was provided and obtained from all participants in the study. Parental consent was obtained for those younger than 18 years of age.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alexander, B. (2010). The Globalization Of Addiction: A Study In Poverty Of The Spirit. Oxford University Press.
- American Psychiatric Association. (2013). Diagnostic And Statistical Manual Of Mental Disorders (Dsm-5®). American Psychiatric Pub.
- Anderson M, Jiang J. Teens, Social Media & Technology 2018. Pew Research Center. 2018;31(2018):1673–1689. [Google Scholar]
- Andreetta J, Teh MJ, Burleigh TL, Gomez R, Stavropoulos V. Associations Between Comorbid Stress And Internet Gaming Disorder Symptoms: Are There Cultural And Gender Variations? Asia-Pacific Psychiatry. 2020;12(2):E12387. doi: 10.1111/Appy.12387. [DOI] [PubMed] [Google Scholar]
- Berardi F. And: Phenomenology Of The End. Semiotext; 2015. [Google Scholar]
- Brand M, Wegmann E, Stark R, Müller A, Wölfling K, Robbins TW, Potenza MN. The Interaction Of Person-Affect-Cognition-Execution (I-Pace) Model For Addictive Behaviors: Update, Generalization To Addictive Behaviors Beyond Internet-Use Disorders, And Specification Of The Process Character Of Addictive Behaviors. Neuroscience and Biobehavioral Reviews. 2019;104:1–10. doi: 10.1016/J.Neubiorev.2019.06.032. [DOI] [PubMed] [Google Scholar]
- Brand M, Young KS, Laier C, Wölfling K, Potenza MN. Integrating Psychological And Neurobiological Considerations Regarding The Development And Maintenance Of Specific Internet-Use Disorders: An Interaction Of Person-Affect-Cognition-Execution (I-Pace) Model. Neuroscience and Biobehavioral Reviews. 2016;71:252–266. doi: 10.1016/J.Neubiorev.2016.08.033. [DOI] [PubMed] [Google Scholar]
- Cha SS, Seo BK. Smartphone Use And Smartphone Addiction In Middle School Students In Korea: Prevalence, Social Networking Service and Game Use. Health Psychol Open. 2018;5(1):2055102918755046. doi: 10.1177/2055102918755046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung T, Lee RLT, Tse ACY, Do CW, So BCL, Szeto GPY, Lee PH. Psychometric Properties And Demographic Correlates Of The Smartphone Addiction Scale-Short Version Among Chinese Children And Adolescents In Hong Kong. Cyberpsychology, Behavior and Social Networking. 2019;22(11):714–723. doi: 10.1089/Cyber.2019.0325. [DOI] [PubMed] [Google Scholar]
- Chia DXY, Ng CWL, Kandasami G, Seow MYL, Choo CC, Chew PKH, Lee C, Zhang MWB. Prevalence Of Internet Addiction And Gaming Disorders In Southeast Asia: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2020;17(7):2582. doi: 10.3390/ijerph17072582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder Carras M, Kardefelt-Winther D. When Addiction Symptoms And Life Problems Diverge: A Latent Class Analysis Of Problematic Gaming In A Representative Multinational Sample Of European Adolescents. European Child and Adolescent Psychiatry. 2018;27(4):513–525. doi: 10.1007/S00787-018-1108-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder Carras M, Van Rooij AJ, Van De Mheen D, Musci R, Xue QL, Mendelson T. Video Gaming In A Hyperconnected World: A Cross-Sectional Study Of Heavy Gaming, Problematic Gaming Symptoms, And Online Socializing In Adolescents. Comput Human Behav. 2017;68:472–479. doi: 10.1016/J.Chb.2016.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen W, Gulati G, Kelly BD. Mental Health In The Covid-19 Pandemic. Qjm: An International Journal Of Medicine. 2020;113(5):311–312. doi: 10.1093/Qjmed/Hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreier M, Wölfling K, Duven E, Giralt S, Beutel ME, Müller KW. Free-To-Play: About Addicted Whales, At Risk Dolphins And Healthy Minnows. Monetarization Design And Internet Gaming Disorder. Addictive Behaviors. 2017;64:328–333. doi: 10.1016/J.Addbeh.2016.03.008. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Mckay D, Yang H, Minaya C, Montag C, Asmundson GJG. Health Anxiety Related To Problematic Smartphone Use And Gaming Disorder Severity During Covid-19: Fear Of Missing Out As A Mediator. Hum Behav Emerg Technol. 2020 doi: 10.1002/Hbe2.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner G, Irving H, Adlaf EM, Turner N. Subtypes Of Adolescent Video Gamers: A Latent Class Analysis. International Journal of Mental Health and Addiction. 2015;13(1):1–18. doi: 10.1007/S11469-014-9501-6. [DOI] [Google Scholar]
- Fischer-Grote L, Kothgassner OD, Felnhofer A. Risk Factors For Problematic Smartphone Use In Children And Adolescents: A Review Of Existing Literature. Neuropsychiatrie. 2019;33(4):179–190. doi: 10.1007/S40211-019-00319-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fumero A, Marrero RJ, Bethencourt JM, Peñate W. Risk Factors Of Internet Gaming Disorder Symptoms In Spanish Adolescents. Computers in Human Behavior. 2020;111:106416. doi: 10.1016/J.Chb.2020.106416. [DOI] [Google Scholar]
- Geisel O, Lipinski A, Kaess M. Non-Substance Addiction In Childhood And Adolescence-The Internet, Computer Games And Social Media. Deutsches Ärzteblatt International. 2021;118(1–2):14–22. doi: 10.3238/Arztebl.M2021.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha JH, Yoo HJ, Cho IH, Chin B, Shin D, Kim JH. Psychiatric Comorbidity Assessed In Korean Children And Adolescents Who Screen Positive For Internet Addiction. Journal of Clinical Psychiatry. 2006;67(5):821–826. doi: 10.4088/Jcp.V67n0517. [DOI] [PubMed] [Google Scholar]
- Hawi NS, Samaha M, Griffiths MD. Internet Gaming Disorder In Lebanon: Relationships With Age, Sleep Habits and Academic Achievement. Journal of Behavioral Addictions. 2018;7(1):70–78. doi: 10.1556/2006.7.2018.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho CS, Chee CY, Ho RC. Mental Health Strategies To Combat The Psychological Impact Of Coronavirus Disease 2019 (Covid-19) Beyond Paranoia And Panic. Ann Acad Med Singap. 2020;49(3):155–160. doi: 10.47102/annals-acadmedsg.202043. [DOI] [PubMed] [Google Scholar]
- Ho RC, Zhang MW, Tsang TY, Toh AH, Pan F, Lu Y, Cheng C, Yip PS, Lam LT, Lai CM, Watanabe H, Mak KK. The Association Between Internet Addiction And Psychiatric Co-Morbidity: A Meta-Analysis. BMC Psychiatry. 2014;14:183. doi: 10.1186/1471-244x-14-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang H, Hong J, Kim SM, Han DH. The Correlation Between Family Relationships And Brain Activity Within The Reward Circuit In Adolescents With Internet Gaming Disorder. Science and Reports. 2020;10(1):9951. doi: 10.1038/S41598-020-66535-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyun GJ, Han DH, Lee YS, Kang KD, Yoo SK, Chung U-S, Renshaw PF. Risk Factors Associated With Online Game Addiction: A Hierarchical Model. Computers in Human Behavior. 2015;48:706–713. doi: 10.1016/J.Chb.2015.02.008. [DOI] [Google Scholar]
- Ibm Corp . Ibm Spss Statistics For Windows, Version 240. Ibm Corp; 2016. [Google Scholar]
- Jeong S-H, Kim H, Yum J-Y, Hwang Y. What Type Of Content Are Smartphone Users Addicted To?: Sns Vs. Games. Computers in Human Behavior. 2016;54:10–17. doi: 10.1016/J.Chb.2015.07.035. [DOI] [Google Scholar]
- Kaptsis D, King DL, Delfabbro PH, Gradisar M. Withdrawal Symptoms In Internet Gaming Disorder: A Systematic Review. Clinical Psychology Review. 2016;43:58–66. doi: 10.1016/J.Cpr.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Kardefelt-Winther D. A Conceptual And Methodological Critique Of Internet Addiction Research: Towards A Model Of Compensatory Internet Use. Computers in Human Behavior. 2014;31:351–354. doi: 10.1016/J.Chb.2013.10.059. [DOI] [Google Scholar]
- King, D., & Delfabbro, P. (2018). Internet Gaming Disorder: Theory, Assessment, Prevention, And Treatment (1st Edition). 10.1016/C2016-0-04107-4
- Ko CH, Lin HC, Lin PC, Yen JY. Validity, Functional Impairment And Complications Related To Internet Gaming Disorder In The Dsm-5 And Gaming Disorder In The Icd-11. Australian and New Zealand Journal of Psychiatry. 2020;54(7):707–718. doi: 10.1177/0004867419881499. [DOI] [PubMed] [Google Scholar]
- Kwon M, Kim DJ, Cho H, Yang S. The Smartphone Addiction Scale: Development And Validation Of A Short Version For Adolescents. PLoS ONE. 2013;8(12):E83558. doi: 10.1371/Journal.Pone.0083558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laconi S, Pirès S, Chabrol H. Internet Gaming Disorder, Motives, Game Genres And Psychopathology. Computers in Human Behavior. 2017;75:652–659. doi: 10.1016/J.Chb.2017.06.012. [DOI] [Google Scholar]
- Lemmens JS, Valkenburg PM, Gentile DA. The Internet Gaming Disorder Scale. Psychological Assessment. 2015;27(2):567–582. doi: 10.1037/Pas0000062. [DOI] [PubMed] [Google Scholar]
- Lewis M. The Biology Of Desire: Why Addiction Is Not A Disease. Publicaffairs; 2015. [Google Scholar]
- Lin YH, Lin YC, Lin SH, Lee YH, Lin PH, Chiang CL, Chang LR, Yang CC, Kuo TB. To Use Or Not To Use? Compulsive Behavior And Its Role In Smartphone Addiction. Translational Psychiatry. 2017;7(2):E1030. doi: 10.1038/Tp.2017.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CH, Lin SH, Pan YC, Lin YH. Smartphone Gaming And Frequent Use Pattern Associated With Smartphone Addiction. Medicine (baltimore) 2016;95(28):E4068. doi: 10.1097/Md.0000000000004068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The Structure Of Negative Emotional States: Comparison Of The Depression Anxiety Stress Scales (Dass) With The Beck Depression And Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Macao Association For Internet Research. (2020). Internet Usage Trends In Macao 2020. Macao: Mair.
- Macur M, Pontes HM. Internet Gaming Disorder In Adolescence: Investigating Profiles And Associated Risk Factors. BMC Public Health. 2021;21(1):1547. doi: 10.1186/S12889-021-11394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak KK, Lai CM, Watanabe H, Kim DI, Bahar N, Ramos M, Young KS, Ho RC, Aum NR, Cheng C. Epidemiology Of Internet Behaviors And Addiction Among Adolescents In Six Asian Countries. Cyberpsychology, Behavior and Social Networking. 2014;17(11):720–728. doi: 10.1089/Cyber.2014.0139. [DOI] [PubMed] [Google Scholar]
- Männikkö N, Billieux J, Kääriäinen M. Problematic Digital Gaming Behavior And Its Relation To The Psychological, Social And Physical Health Of Finnish Adolescents And Young Adults. Journal of Behavioral Addictions. 2015;4(4):281–288. doi: 10.1556/2006.4.2015.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melodia F, Canale N, Griffiths MD. The Role Of Avoidance Coping And Escape Motives In Problematic Online Gaming: A Systematic Literature Review. International Journal of Mental Health and Addiction. 2020 doi: 10.1007/S11469-020-00422-W. [DOI] [Google Scholar]
- Montag, C., Lachmann, B., Herrlich, M., & Zweig, K. (2019a). Addictive Features Of Social Media/Messenger Platforms And Freemium Games Against The Background Of Psychological And Economic Theories. International Journal of Environmental Research and Public Health, 16(14). 10.3390/Ijerph16142612 [DOI] [PMC free article] [PubMed]
- Montag, C., Schivinski, B., Sariyska, R., Kannen, C., Demetrovics, Z., & Pontes, H. M. (2019b). Psychopathological Symptoms And Gaming Motives In Disordered Gaming-A Psychometric Comparison Between The Who And Apa Diagnostic Frameworks. Journal of Clinical Medicine, 8(10). 10.3390/Jcm8101691 [DOI] [PMC free article] [PubMed]
- Montag C, Wegmann E, Sariyska R, Demetrovics Z, Brand M. How To Overcome Taxonomical Problems In The Study Of Internet Use Disorders And What To Do With "Smartphone Addiction"? Journal of Behavioral Addictions. 2021;9(4):908–914. doi: 10.1556/2006.8.2019.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, G. (2017). Dopamining And Disadjustment: Addiction And Digital Capitalism.
- Moore G. The Pharmacology Of Addiction. Parrhesia, 29, pp. 190–211. In: Bowden-Jones Henrietta., editor. Are We All Addicts Now? Digital Dependence. Liverpool University Press; 2018. pp. 69–75. [Google Scholar]
- Moussa MT, Lovibond PF, Laube R. Psychometric Properties Of A Chinese Version Of The 21-Item Depression Anxiety Stress Scales (Dass21) Transcultural Mental Health Centre. Cumberland Hospital; 2001. [Google Scholar]
- Müller KW, Janikian M, Dreier M, Wölfling K, Beutel ME, Tzavara C, Richardson C, Tsitsika A. Regular Gaming Behavior And Internet Gaming Disorder In European Adolescents: Results From A Cross-National Representative Survey Of Prevalence, Predictors, And Psychopathological Correlates. European Child and Adolescent Psychiatry. 2015;24(5):565–574. doi: 10.1007/S00787-014-0611-2. [DOI] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (1998–2015). Mplus User’s Guide, Seventh Edn, Los Angeles, Ca: Muthén & Muthé N.
- Myrseth H, Notelaers G. A Latent Class Approach For Classifying The Problem And Disordered Gamers In A Group Of Adolescence. Frontiers in Psychology. 2018;9:2273. doi: 10.3389/Fpsyg.2018.02273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mythily S, Qiu S, Winslow M. Prevalence And Correlates Of Excessive Internet Use Among Youth In Singapore. Ann Acad Med Singap. 2008;37(1):9–14. [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding On The Number Of Classes In Latent Class Analysis And Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- Parisi, L. (2016). Automated Cognition And Capital In The Psychopathologies Of Cognitive Capitalism Part Iii. Warren Neidich (Eds.), Berlin, Archive Books. Pp 49–84.
- Paulus FW, Ohmann S, Von Gontard A, Popow C. Internet Gaming Disorder In Children And Adolescents: A Systematic Review. Developmental Medicine and Child Neurology. 2018;60(7):645–659. doi: 10.1111/Dmcn.13754. [DOI] [PubMed] [Google Scholar]
- Petry NM, Rehbein F, Ko CH, O’Brien CP. Internet Gaming Disorder In The Dsm-5. Curr Psychiatry Rep. 2015;17(9):72. doi: 10.1007/S11920-015-0610-0. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B, North CS. Mental Health And The Covid-19 Pandemic. New England Journal of Medicine. 2020;383(6):510–512. doi: 10.1056/Nejmp2008017. [DOI] [PubMed] [Google Scholar]
- Pontes HM, Schivinski B, Sindermann C, Li M, Becker B, Zhou M, Montag C. Measurement And Conceptualization Of Gaming Disorder According To The World Health Organization Framework: The Development Of The Gaming Disorder Test. International Journal of Mental Health and Addiction. 2021;19(2):508–528. doi: 10.1007/S11469-019-00088-Z. [DOI] [Google Scholar]
- Rehbein F, Kliem S, Baier D, Mößle T, Petry NM. Prevalence Of Internet Gaming Disorder In German Adolescents: Diagnostic Contribution Of The Nine Dsm-5 Criteria In A State-Wide Representative Sample. Addiction. 2015;110(5):842–851. doi: 10.1111/Add.12849. [DOI] [PubMed] [Google Scholar]
- Ren Z, Xin Y, Wang Z, Liu D, Ho RCM, Ho CSH. What Factors Are Most Closely Associated With Mood Disorders In Adolescents During The Covid-19 Pandemic? A Cross-Sectional Study Based On 1,771 Adolescents In Shandong Province China. Front Psychiatry. 2021;12:728278. doi: 10.3389/Fpsyt.2021.728278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozgonjuk D, Sindermann C, Elhai JD, Christensen AP, Montag C. Associations Between Symptoms Of Problematic Smartphone, Facebook, Whatsapp, And Instagram Use: An Item-Level Exploratory Graph Analysis Perspective. Journal of Behavioral Addictions. 2020;9(3):686–697. doi: 10.1556/2006.2020.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider LA, King DL, Delfabbro PH. Family Factors In Adolescent Problematic Internet Gaming: A Systematic Review. Journal of Behavioral Addictions. 2017;6(3):321–333. doi: 10.1556/2006.6.2017.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schou Andreassen C, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, Pallesen S. The Relationship Between Addictive Use Of Social Media And Video Games And Symptoms Of Psychiatric Disorders: A Large-Scale Cross-Sectional Study. Psychology of Addictive Behaviors. 2016;30(2):252–262. doi: 10.1037/Adb0000160. [DOI] [PubMed] [Google Scholar]
- Sigerson L, Li AY, Cheung MW, Luk JW, Cheng C. Psychometric Properties Of The Chinese Internet Gaming Disorder Scale. Addictive Behaviors. 2017;74:20–26. doi: 10.1016/J.Addbeh.2017.05.031. [DOI] [PubMed] [Google Scholar]
- Sit HF, Hong IW, Burchert S, Sou EKL, Wong M, Chen W, Lam AIF, Hall BJ. A Feasibility Study Of The Who Digital Mental Health Intervention Step-By-Step To Address Depression Among Chinese Young Adults. Front Psychiatry. 2021;12:812667. doi: 10.3389/Fpsyt.2021.812667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soh HL, Ho RC, Ho CS, Tam WW. Efficacy Of Digital Cognitive Behavioural Therapy For Insomnia: A Meta-Analysis Of Randomised Controlled Trials. Sleep Medicine. 2020;75:315–325. doi: 10.1016/J.Sleep.2020.08.020. [DOI] [PubMed] [Google Scholar]
- Stevens MW, Dorstyn D, Delfabbro PH, King DL. Global Prevalence Of Gaming Disorder: A Systematic Review And Meta-Analysis. Australian and New Zealand Journal of Psychiatry. 2021;55(6):553–568. doi: 10.1177/0004867420962851. [DOI] [PubMed] [Google Scholar]
- Stevens MWR, King DL, Dorstyn D, Delfabbro PH. Cognitive-Behavioral Therapy For Internet Gaming Disorder: A Systematic Review And Meta-Analysis. Clinical Psychology & Psychotherapy. 2019;26(2):191–203. doi: 10.1002/Cpp.2341. [DOI] [PubMed] [Google Scholar]
- Strittmatter E, Kaess M, Parzer P, Fischer G, Carli V, Hoven CW, Wasserman C, Sarchiapone M, Durkee T, Apter A, Bobes J, Brunner R, Cosman D, Sisask M, Värnik P, Wasserman D. Pathological Internet Use Among Adolescents: Comparing Gamers And Non-Gamers. Psychiatry Research. 2015;228(1):128–135. doi: 10.1016/J.Psychres.2015.04.029. [DOI] [PubMed] [Google Scholar]
- Su W, Han X, Yu H, Wu Y, Potenza MN. Do Men Become Addicted To Internet Gaming And Women To Social Media? A Meta-Analysis Examining Gender-Related Differences In Specific Internet Addiction. Computers in Human Behavior. 2020;113:106480. doi: 10.1016/J.Chb.2020.106480. [DOI] [Google Scholar]
- Sugaya N, Shirasaka T, Takahashi K, Kanda H. Bio-Psychosocial Factors Of Children And Adolescents With Internet Gaming Disorder: A Systematic Review. Biopsychosoc Med. 2019;13:3. doi: 10.1186/S13030-019-0144-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun P, Johnson CA, Palmer P, Arpawong TE, Unger JB, Xie B, Rohrbach LA, Spruijt-Metz D, Sussman S. Concurrent And Predictive Relationships Between Compulsive Internet Use And Substance Use: Findings From Vocational High School Students In China And The Usa. International Journal of Environmental Research and Public Health. 2012;9(3):660–673. doi: 10.3390/Ijerph9030660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng Z, Pontes HM, Nie Q, Griffiths MD, Guo C. Depression And Anxiety Symptoms Associated With Internet Gaming Disorder Before And During The Covid-19 Pandemic: A Longitudinal Study. Journal of Behavioral Addictions. 2021;10(1):169–180. doi: 10.1556/2006.2021.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran BX, Huong LT, Hinh ND, Nguyen LH, Le BN, Nong VM, Thuc VT, Tho TD, Latkin C, Zhang MW, Ho RC. A Study On The Influence Of Internet Addiction And Online Interpersonal Influences On Health-Related Quality Of Life In Young Vietnamese. BMC Public Health. 2017;17(1):138. doi: 10.1186/S12889-016-3983-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai HF, Cheng SH, Yeh TL, Shih CC, Chen KC, Yang YC, Yang YK. The Risk Factors Of Internet Addiction–A Survey Of University Freshmen. Psychiatry Research. 2009;167(3):294–299. doi: 10.1016/J.Psychres.2008.01.015. [DOI] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020a). Immediate Psychological Responses And Associated Factors During The Initial Stage Of The 2019 Coronavirus Disease (Covid-19) Epidemic Among The General Population In China. International Journal of Environmental Research and Public Health, 17(5). 10.3390/Ijerph17051729 [DOI] [PMC free article] [PubMed]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Mcintyre RS, Choo FN, Tran B, Ho R, Sharma VK, Ho C. A Longitudinal Study On The Mental Health Of General Population During The Covid-19 Epidemic In China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/J.Bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang CW, Chan CL, Mak KK, Ho SY, Wong PW, Ho RT. Prevalence And Correlates Of Video And Internet Gaming Addiction Among Hong Kong Adolescents: A Pilot Study. Scientificworldjournal. 2014;2014:874648. doi: 10.1155/2014/874648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Wang X. Structural Equation Modeling: Applications Using Mplus. John Wiley & Sons; 2019. [Google Scholar]
- Wang K, Shi HS, Geng FL, Zou LQ, Tan SP, Wang Y, Neumann DL, Shum DH, Chan RC. Cross-Cultural Validation Of The Depression Anxiety Stress Scale-21 In China. Psychological Assessment. 2016;28(5):E88–E100. doi: 10.1037/Pas0000207. [DOI] [PubMed] [Google Scholar]
- Wichstrøm L, Stenseng F, Belsky J, Von Soest T, Hygen BW. Symptoms Of Internet Gaming Disorder In Youth: Predictors And Comorbidity. Journal of Abnormal Child Psychology. 2019;47(1):71–83. doi: 10.1007/S10802-018-0422-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. ( 2019). International Classification Of Diseases,11th Revision. 2018.
- Wu AMS, Chen JH, Tong KK, Yu S, Lau JTF. Prevalence And Associated Factors Of Internet Gaming Disorder Among Community Dwelling Adults In Macao China. Journal of Behavioral Addictions. 2018;7(1):62–69. doi: 10.1556/2006.7.2018.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, X., Jiang, X., Mo, P. K., Cai, Y., Ma, L., & Lau, J. T. (2020). Prevalence And Interpersonal Correlates Of Internet Gaming Disorders Among Chinese Adolescents. International Journal of Environmental Research and Public Health, 17(2). 10.3390/Ijerph17020579 [DOI] [PMC free article] [PubMed]
- Yen, J. Y., Lin, H. C., Chou, W. P., Liu, T. L., & Ko, C. H. (2019). Associations Among Resilience, Stress, Depression, And Internet Gaming Disorder In Young Adults. International Journal of Environmental Research and Public Health, 16(17). 10.3390/Ijerph16173181 [DOI] [PMC free article] [PubMed]
- Yuan G, Elhai JD, Hall BJ. The Influence Of Depressive Symptoms And Fear Of Missing Out On Severity Of Problematic Smartphone Use And Internet Gaming Disorder Among Chinese Young Adults: A Three-Wave Mediation Model. Addictive Behaviors. 2021;112:106648. doi: 10.1016/J.Addbeh.2020.106648. [DOI] [PubMed] [Google Scholar]
- Zhang MW, Ho RC. Moodle: The Cost Effective Solution For Internet Cognitive Behavioral Therapy (I-Cbt) Interventions. Technology and Health Care. 2017;25(1):163–165. doi: 10.3233/Thc-161261. [DOI] [PubMed] [Google Scholar]
- Zhang MWB, Ho RCM. Smartphone Applications For Immersive Virtual Reality Therapy For Internet Addiction And Internet Gaming Disorder [Journal Article] Technology & Health Care. 2017;25(2):367–372. doi: 10.3233/Thc-161282. [DOI] [PubMed] [Google Scholar]
- Zhang MWB, Lim RBC, Lee C, Ho RCM. Prevalence Of Internet Addiction In Medical Students: A Meta-Analysis. Academic Psychiatry. 2018;42(1):88–93. doi: 10.1007/S40596-017-0794-1. [DOI] [PubMed] [Google Scholar]
- Zhang MWB, Tran BX, Huong LT, Hinh ND, Nguyen HLT, Tho TD, Latkin C, Ho RCM. Internet Addiction And Sleep Quality Among Vietnamese Youths. Asian Journal of Psychiatry. 2017;28:15–20. doi: 10.1016/J.Ajp.2017.03.025. [DOI] [PubMed] [Google Scholar]
- Zhang MX, Wang X, Yu SM, Wu AMS. Purpose In Life, Social Support, And Internet Gaming Disorder Among Chinese University Students: A 1-Year Follow-Up Study. Addictive Behaviors. 2019;99:106070. doi: 10.1016/J.Addbeh.2019.106070. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.