Abstract
Background
The COVID-19 pandemic has and will continue to have a tremendous influence on intensive care unit (ICU) nurses’ mental health.
Objectives
The purpose of this study was to describe the impact of COVID-19 on nurse moral distress, burnout, and mental health.
Methods
Between October 2020 and January 2021 this descriptive study recruited a national sample of nurses who worked in the ICU during the COVID-19 pandemic through American Association of Critical Care Nurses newsletters and social media.
Results
A total of 488 survey responses were received from critical care nurses working in the U.S. during the COVID pandemic. Over two thirds of respondents experienced a shortage of personal protective equipment (PPE). Nurse respondents reported moderate/high levels of moral distress and burnout. Symptoms of moderate to severe depression and anxiety were reported by 44.6% and 31.1% of respondents, respectively. Forty-seven percent of respondents were at risk for having posttraumatic stress disorder (PTSD). Lack of perceived support from administration and shortage of PPE were associated with higher levels of burnout, moral distress, and PTSD symptoms.
Conclusions
Respondents had higher anxiety and depression than the general population and higher risk for having PTSD than recent veterans or patients after traumatic injury. High levels of reported burnout and moral distress increase the risk of nurses leaving ICU practice or the profession. This study offers important insights about the mental health of nurses during a global pandemic that can guide the development of customized interventions for ICU nurses related to this health care crisis.
KeyWords: COVID-19, Critical Care, Nurses, Mental Health, Burnout, Moral Distress
Introduction
The coronavirus disease 2019 (COVID-19) global pandemic has put immense strain on frontline healthcare workers (HCWs). This is particularly true for HCWs caring for COVID-19 patients in intensive care units (ICU). Indeed, news reports highlight the extreme stress experienced by HCWs in critical care.1., 2., 3., 4.
This increased strain on critical care nurses during COVID-19 is multifactorial. Critically ill COVID-19 patients have extremely high severity of illness, often with acute respiratory distress syndrome (ARDS) and multi organ failure.5 Patients require longer durations of mechanical ventilation than is typical even in ARDS and reported mortality rates are high (22 to 97%).5 , 6 In the midst of caring for these patients, nurses are experiencing system level barriers to safe and effective care. Challenges include lack of personal protective equipment (PPE),7 , 8 potential shortage of ventilators,8 and limited or no family visitation, leaving nurses to struggle to connect patients with their loved ones.2 Personal safety concerns, fear of infecting oneself and family members1 , 9 add to this stress. Critical care nurses are at significant risk for anxiety, depression, posttraumatic stress disorder (PTSD), moral distress and burnout based on the frequency of death of COVID-19 patients in the ICU and the extreme workload imposed by severe COVID-19 illness.10 , 11
National leaders have raised concerns about the impact of COVID-19 on ICU nurses well-being10 , 11 and the pandemic impact on the existing nursing shortage. Even prior to the pandemic, ICU nurses reported higher levels of moral distress,12 burnout,13 , 14 and symptoms of posttraumatic stress15 when compared to other HCWs. The high acuity and mortality of critically ill COVID-19 patients coupled with inadequate resources (e.g. PPE) increases risk of both moral distress and burnout, which are closely associated.12 , 13 , 16 Moral distress or burnout can occur when nurses experience powerlessness, low levels of control, inadequate support or resources, increased job stress, and high job demands.13 , 17., 18., 19., 20. These factors are likely experienced by nurses working in critical care during the pandemic as HCWs experience shortage of resources, uncertainty around treatment, and personal fears of contracting illness while caring for the critically ill. Overstretched, stressed nurses may not be able to provide the care they would like to critically ill or dying patients or may be overwhelmed by the increased demands during the pandemic, thereby potentially increasing risk of moral distress or burnout, as well as symptoms of PTSD, anxiety, and depression.
Studies from China, the first country to experience the crisis, describe the toll of the pandemic on HCWs. For HCWs in the hospital setting during the onset of the pandemic there was a high incidence of anxiety (45%), depression (50%), and distress related to COVID-19 (71%).21 Furthermore, nurses reported more severe symptoms of depression, anxiety, and distress than other HCWs.21 Even during routine practice prior to the pandemic, 11% of critical care nurses reported symptoms of anxiety, 13% symptoms of depression, and 33% symptoms of PTSD and nurses with PTSD symptoms experienced high levels of burnout.15 Given prepandemic and early pandemic studies, ICU nurses are at high risk to be negatively impacted by the COVID-19 pandemic. However, previous studies have not focused on the impact of the pandemic on mental health and distress of ICU nurses in the United States.
To fully support nurses working on the frontline now and in the future, we must understand the impact of COVID-19 on ICU nurses during the pandemic. The purpose of the current study was:
-
•
to describe the impact of COVID-19 on ICU nurse moral distress, burnout, anxiety, depression and PTSD symptoms
-
•
to identify differences in moral distress, burnout, and mental health measures based on workplace and participant characteristics.
-
•
to describe associations between moral distress, burnout, and mental health measures.
Methods
Design: In this descriptive study a national sample of nurses that worked in ICUs during the COVID-19 pandemic in the United States early October 2020 through early January 2021 was recruited. Survey data was collected using QualtricsXM (Qualtrics, Provo, UT) online data collection platform.
Recruitment:AACN member participants were recruited through the AACN weekly e-newsletter. Information in the e-newsletter briefly described the study, provided a hyperlink to access the electronic survey, and provided a contact from the study team should potential participants have questions. On the survey landing and conclusion page nurses were given a link to the survey that they could share with other critical care nurses. Additionally, the survey was advertised on Facebook and the survey link was shared by researchers and colleagues on Twitter. For Facebook, we created a new account that was used only for study recruitment.
The survey landing page provided a brief description of the study purpose, inclusion criteria, procedures, risks and benefits, voluntary nature of participation, and researcher contact information. Completion of the survey indicated consent.
Sample and Sample Size: Our previous surveys of critical care nurses with recruitment through AACN have yielded a sample size of 177 to 423.22 , 23 For this descriptive study, we did not calculate a required sample size a-priori. We included any nurse working in the ICU during the pandemic. Nurses working outside of the United States were excluded.
Measures: Sample demographics collected in the survey included respondent characteristics (e.g. years of experience), work setting and location (e.g. region of U.S.), and description of challenges during the pandemic (e.g. shortage of PPE). Measure of moral distress, burnout, PTSD symptoms, anxiety, and depression were selected based on the following criteria: validity and reliability of the instrument, past use with nursing or HCW samples, and length of the instrument to minimize response burden.
Moral Distress was measured with the Measure of Moral Distress in Healthcare Professionals (MMD-HP).18 The 30 item MMD-HP has respondents rate the frequency (0 Never to 4 Very Frequently) and level of distress (0 none to 4 very distressing) related to care situations. Scores range from 0 to 432 with higher scores indicating greater moral distress.18
The MMD-HP has high internal reliability (0.93); construct validity, and discriminant validity as evidenced by correlations between intent to leave the workplace and higher scores.18
Burnout was measured with the burnout subscale of the Professional Quality of Life Scale (PROQOL-5). On 10 items, respondents rate how often they have had positive and negative experiences related to work in the last 30 days from never (1) to very often (5).24 Scores range from 10 to 50 with ≤22 indicating low levels, 23 to 42 indicating high levels, and ≥ 42 indicating high levels of burnout.42 The ProQOL has demonstrated validity with decreased burnout scores after interventions to increase resilience 25 , 26 and acceptable internal reliability (Cronbach's alpha >0.8).24 , 25
PTSD symptoms were measured by the Trauma Screening Questionnaire (TSQ), a 10-item symptom screen that was designed for use with survivors of all types of traumatic stress. Respondents endorse those items that they have experienced at least twice in the past week. 27 Scores range from 0 to 10 with a score of 6 indicating risk for PTSD.26 , 27 The TSQ has excellent sensitivity (0.86) and specificity (0.93) in predicting PTSD (overall efficiency = 0.90 when using a cut-score of at least 6 re-experiencing or arousal symptoms in any combination).27 , 28
The Patient Health Questionnaire Anxiety and Depression Scale (PHQ-ADS) was used to measure anxiety and depression. The PHQ-ADS has 9 anxiety and 7 depression items. Respondents rate how much symptoms have bothered them in last two weeks from ‘not at all’ (0) to ‘nearly every day’ (3).29 Subscale scores range from 0 to 27 (depression subscale) and 0 to 21 (anxiety subscale).29 Depression Subscale Scores of 5, 10, 15, and 20 represent mild, moderate, moderately severe, and severe depression, respectively.30 Anxiety Subscale Scores reflect anxiety that is minimal (0-4), mild (5-9), moderate (10-14), and severe (15-21).31 Subscales have strong internal (Cronbach's alpha 0.8 to 0.9) and construct validity (correlations range from 0.4 to 0.6 with quality of life and disability measures).29
Incentive: At the end of the survey, individuals interested in entering a drawing for a $50 VISA gift card were connected to a separate Qualtrics page that allowed them to enter their email contact information. Contact information was not connected to survey responses. Ten individuals were randomly selected from those who provided contact information.
Analysis: Demographic and survey response data were analyzed with appropriate descriptive statistics. Differences in nurse responses based on demographic or workplace characteristics (e.g. age, type of ICU) were analyzed with Kruskal-Wallis or Mann-Whitney U tests. Pair-wise comparisons were calculated for any significant Kruskal-Wallis analyses. Associations between scales were calculated with Spearman's correlations.
Ethical Considerations. IRB approval was obtained through XXX University prior to recruitment. Completion of the survey was voluntary and indicated consent for participation, respondents could stop answering survey items, and exit the survey at any time. Contact information for incentives were not connected to survey responses to maintain anonymity. On the landing Page and final Page of the survey, contact information for the Disaster Distress Helpline (1-800-985-5990) was provided. This confidential helpline is available 24/7 to all United States residents and provides counseling for individuals experiencing emotional distress related to a disaster.
Results
Demographics. Although 648 nurses accessed the survey, only 488 nurses responded to the survey and completed at least some demographic questions. Respondents reported learning about the survey through Facebook (51.8%), the AACN newsletter (22.5%), and information shared by colleagues (20.9%). Respondents were primarily staff nurses (92.5%), female (88.1%), and had a BSN degree (71.7%) (Table 1 ). Over two-thirds of nurse respondents experienced shortages of personal protective equipment (PPE) at some point during the pandemic (Table 2 ).
Table 1.
Workplace and Respondent Characteristics (N=488)
| Characteristic | n (%) or Median | |
|---|---|---|
| Region of United States [n (%)] (n = 485) | ||
| Midwest | 255 (52.6) | |
| Northeast | 78 (16.0) | |
| Southeast | 67 (13.8) | |
| West | 48 (9.9) | |
| Southwest | 31 (6.4) | |
| Other (e.g. Mid-Atlantic, South Central) | 4 (0.8) | |
| Multiple Regions as Travel Nurse | 2 (0.4) | |
| Nursing Position [n (%)] (n = 488) | ||
| Staff Nurse | 457 (93.6) | |
| Nurse Manager/Supervisor | 13 (2.7) | |
| Nurse Practitioner | 7 (1.4) | |
| Other (e.g. care coordinator, faculty, educator, CNS) | 11 (2.2) | |
| Type of Hospital [n (%)] (n =484) | ||
| Community Hospital | 242 (50.0) | |
| University medical center | 163 (33.7) | |
| Non-Academic Teaching | 29 (6.0) | |
| Veterans Affairs (VA) or Military | 16 (3.3) | |
| County | 17 (3.5) | |
| Other (e.g. type unclear, travel nurse at multiple sites) | 17 (3.5) | |
| Age years [n (%)] (n = 488) | ||
| 20-30 | 192 (39.3) | |
| 31-40 | 140 (28.7) | |
| 41-50 | 67 (13.7) | |
| 51-60 | 65 (13.3) | |
| >60 | 24 (4.9) | |
| Gender [n (%)] (n =488) | ||
| Female | 430 (88.1) | |
| Male | 56 (11.5) | |
| Nonbinary | 1 (0.2) | |
| Prefer not to respond | 1 (0.2) | |
| Highest Nursing Degree [n(%)] (n =487) | ||
| Bachelors | 353 (72.5) | |
| Associate | 81 (16.6) | |
| Masters | 38 (7.8) | |
| Diploma | 11 (2.3) | |
| PhD or DNP | 4 (0.8) | |
| Years of ICU Experience [Median (Range)] (n =457) | 5 (0-44) | |
| CCRN certification [n(%)] (n =486) | 169(34.6) | |
CNS (clinical nurse specialist); CCRN (critical care nurse certification); PhD (Doctor of Philosophy); DNP (Doctor of Nursing Practice)
Table 2.
COVID-19 Workplace Characteristics (N=488)
| Workplace Characteristic | n (%) | |
|---|---|---|
| Worked on COVID-19 Designated Unit (n= 481) | 416 (86.5) | |
| Number of Patients Assigned during pandemic (n= 457) | ||
| One to two | 268 (58.6) | |
| Three to four | 179 (39.2) | |
| 5 or more | 10 (2.2) | |
| Shortage of Equipment/Supplies | ||
| Experienced shortages of PPE (n=465) | 331 (71.2) | |
| Experienced shortage of ventilators (n=463) | 86 (18.6) | |
| Changed Units during COVID-19 (n=402) | 117 (29.1) | |
| Patient family allowed to visit (n=463) | ||
| Yes | 14 (3.0) | |
| No | 244 (52.7) | |
| Under some circumstances (e.g. end of life) | 205 (44.3) | |
| Supported by Hospital Administration During pandemic (n=464) | ||
| Yes, fully supported | 86 (18.5) | |
| Yes, partially supported | 204 (44.0) | |
| No | 174 (37.5) | |
PPE: personal protective equipment.
Of the 488 nurses who completed demographic data, not all respondents completed every measure. Sample sizes for each measure are as follows: MMD-HP (N=481), PRQOL-5 (N=452), TSQ (N=360), PHQ-ADS Anxiety Questions (N=354), and PHQ-ADS Depression questions (N =357).
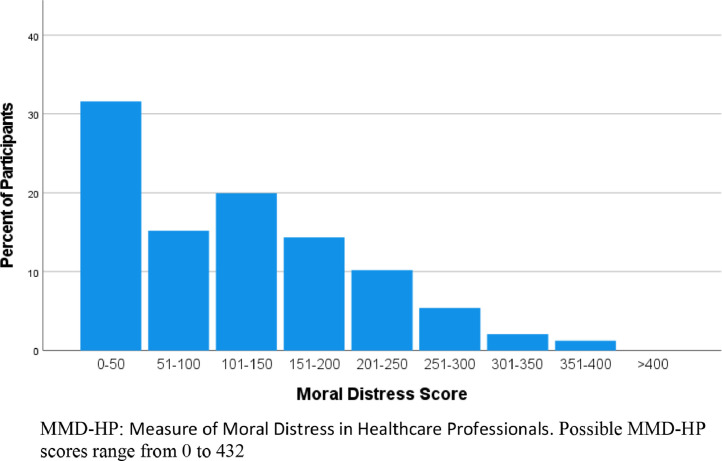
Moral Distress and Burnout. Critical care nurses in our sample reported moderate levels of burnout (Mdn. 30, range 10 to 44; 84.7% moderate levels). Respondents had moderate levels of moral distress (Mdn. 106, range 0 to 400) (fig 1 ).
Figure 1.
Moral Distress scores on MMD-HP (n=481)
MMD-HP: Measure of Moral Distress in Healthcare Professionals. Possible MMD-HP scores range from 0 to 432
Anxiety, Depression, and PTSD Symptoms. Nearly a third of respondents met criteria for moderate to severe anxiety (31.1%) (overall Mdn. 9.0 (range 0-27) while 44.6% of respondents met criteria for moderate to severe depression (overall Mdn. 6.0 (range 0-21) (Table 3). Almost half (46.7%) of nurse respondents were at risk for developing PTSD (overall Mdn. 5 range (0-10). Over half of respondents (55.6%) reported feeling their life was threatened or they might die as a consequence of caring for COVID-19 patients.
Table 3.
PTSD Risk, Anxiety, and Depression (N=488)
| n (%) | ||
|---|---|---|
| At Risk for PTSD (n = 360) | 168 (46.7) | |
| Felt life in danger/might die due to caring for COVID-19 patients (n =363) | 202 (55.6) | |
| Depression (n = 357) | ||
| Minimal Depression | 97(27.2) | |
| Mild Depression | 101 (28.3) | |
| Moderate Depression | 86 (24.1) | |
| Moderately Severe Depression | 47 (13.2) | |
| Severe Depression | 26 (7.3) | |
| Anxiety (n =354) | ||
| Minimal Anxiety | 126 (35.6) | |
| Mild Anxiety | 118 (33.3) | |
| Moderate Anxiety | 64 (18.1) | |
| Severe Anxiety | 46 (13.0 | |
PTSD: post-traumatic stress disorder.
Respondents that felt that their life was threatened or that they might die as a consequence of COVID-19 had higher PTSD risk (U = 22863.5, p<.001; Mdn. 6 vs. 3), depression (U=19544.5, p<.001; Mdn. 10 vs. 7), and anxiety (U=19833.0, p < .001; Mdn. 7 vs. 5) scores. Of those respondents that felt their life was threatened, 61.4% were at risk for PTSD compared to 27.8% for those that did not feel threatened. Similarly, there was a higher percentage of respondents with moderate to severe depression (52.6% versus 34.5%) and moderate to severe anxiety (38.3% versus 22.2%) for those that felt their life had been at risk due to COVID-19 compared to those who did not.
Differences by Respondent and Workplace Characteristics
There was no difference in any measure of emotional or psychological distress related to region of the country, race/ethnicity, family visitation policies, CCRN certification, or having to change to a different unit during the pandemic. Burnout scores varied based on age, ICU experience, PPE shortages, and perceived support from administration (Table 4 and 5 ). Younger nurses (20-30 years old) had higher reported burnout than either nurses aged 41-50 (p=.031) or nurses aged 51-60 (p=.023). Similarly, nurses with experience of five years or less had significantly higher reported burnout than nurses with more than 20 years of experience (p=.019). Scores for burnout, PTSD risk, and anxiety varied by gender with respondents identifying as female having higher burnout (p=.005), PTSD risk (p=.013), and anxiety (p=.014) than respondents identifying as male.
Table 4.
Differences by Respondent Characteristics
| Burnout [median (range)] | Statistica | p | ||
|---|---|---|---|---|
| Age (years) | 10.136 | .038 | ||
| 20-30 | 51.0 (25.1-73.6)b | |||
| 31-40 | 51.0 (21.8-72.0) | |||
| 41-50 | 47.7 (21.8-65.5) | |||
| 51-60 | 47.7 (18.6-67.2) | |||
| ICU Experience (years) | 10.687 | .014 | ||
| 0-5 | 52.6 (21.8-73.6)c | |||
| 6-10 | 51.0 (29.9-67.2) | |||
| 11-30 | 47.7 (21.9-65.5) | |||
| >20 | 46.1 (18.6-67.2) | |||
| Genderd | 9.133 | .028 | ||
| Male | 47.7 (21.9-70.4) | |||
| Female | 51.0 (18.6-73.6) | |||
| TSQ [median (range)] | 8.738 | .033 | ||
| Male | 3 (0-10) | |||
| Female | 5 (0-10) | |||
| Anxiety [median (range)] | 8.484 | .037 | ||
| Male | 4 (0-21) | |||
| Female | 7 (0-21) | |||
Kruskal-Wallis H
higher burnout for 20-30 age group than 51-60 (p=.023) and 41-50 (p=.031);
Higher burnout for ICU experience 0-5 years versus >20 years (p=.019)
No differences seen in pairwise comparisons between male and female reported gender with respondents that preferred to self-describe or preferred to not report gender. TSQ: Trauma Screening Questionnaire.
Table 5.
Differences by Workplace Characteristics
| Burnout [median (range)] | Statistica | p | ||
|---|---|---|---|---|
| Shortage of PPE | 15009 | <.001 | ||
| Yes | 52.6 (18.6-73.6) | |||
| No | 47.7 (21.9-68.8) | |||
| Support of Administration | 81.15b | <.001 | ||
| Yes | 42.9 (18.6-65.5) | |||
| Partial | 49.4 (21.9-72.0) | |||
| No | 55 (31.6-73.6) | |||
| Moral Distress [median (range)] | Statistica | p | ||
| Shortage of Ventilators | 13123 | .018 | ||
| Yes | 139.5 (0-400) | |||
| No | 106.5 (0-397) | |||
| Shortage of PPE | 15206 | <.001 | ||
| Yes | 126 (0-400) | |||
| No | 83.5 (0-255) | |||
| Support of Administration | 46.68b | <.001 | ||
| Yes | 61 (0-240) | |||
| Partial | 104 (0-327) | |||
| No | 166 (0–400) | |||
| TSQ [median (range)] | Statistica | p | ||
| Shortage of PPE | 10418 | .020 | ||
| Yes | 6 (0-10) | |||
| No | 4 (0-10) | |||
| Support of Administration | 34.52b | <.001 | ||
| Yes | 3 (0-10) | |||
| Partial | 5 (0-10) | |||
| No | 6 (0-10) | |||
| Depression [median (range)] | Statistica | p | ||
| Shortage of PPE | 9921 | .010 | ||
| Yes | 9 (0-27) | |||
| No | 7 (0-23) | |||
| Support of Administration | 31.01c | <.001 | ||
| Yes | 5 (0-24) | |||
| Partial | 8 (0-27) | |||
| No | 11 (0-27) | |||
| Anxiety [median (range)] | Statistica | p | ||
| Shortage of PPE | 9445 | .004 | ||
| Yes | 7 (0-21) | |||
| No | 5 (0-21) | |||
| Support of Administration | 28.17c | <.001 | ||
| Yes | 4 (0-21) | |||
| Partial | 6 (0-20) | |||
| No | 8 (0-21) | |||
Kruskal Wallis (H) for greater than two categories or Mann-Whitney (U) for two category comparisons
Pairwise comparisons: significant differences between ‘yes, fully supported’ and ‘partially supported’ and ‘not supported’ respectively and significant differences between ‘partially supported’ and not supported’
Pairwise comparisons: significant differences between ‘not supported’ and ‘partially’ or ‘yes, fully supported’. TSQ: Trauma Screening Questionnaire.
Scores for moral distress varied based on ventilator shortages, ICU experience, PPE shortage, and perceived support from administration (Table 4 and 5). Measures of PTSD, depression, and anxiety varied based on PPE shortage and perceived support from administration. Nurses that reported experiencing shortages of PPE had higher burnout (p<.001), moral distress (p<.001), anxiety (p=.004), depression (p=.010), and symptoms of PTSD (p=.020). Respondents who reported a shortage of ventilators had higher levels of moral distress (p=.018).
In pairwise comparisons, respondents who felt fully supported by administration had lower burnout, moral distress, and symptoms of PTSD than those who felt only partially supported (p=.002; p=.006; p=.016 respectively) or not supported (p<.001; p<.001; p<.001 respectively). Additionally, nurses that felt partially supported also had lower burnout (p<.001), moral distress (p<.001) and symptoms of PTSD (p=.001) than respondents that felt not supported by administration. Nurses that felt fully supported or partially supported by administration had lower anxiety (p<.001) and depression (p<.001) than those reporting they were not supported.
Correlations
Burnout and Moral Distress were both moderately to highly correlated with anxiety, depression, and PTSD symptoms (Table 6 ).
Table 6.
Correlations Moral Distress, Burnout, and Psychologic Measures (Spearman's rho)
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. Moral Distress | — | |||
| 2. Burnout | .451 | — | ||
| 3. PTSD Risk | .431 | .551 | — | |
| 4. Anxiety | .451 | .631 | .681 | — |
| 5. Depression | .431 | .661 | .681 | .801 |
p<.001
Discussion
Our national survey sought to understand the impact of the pandemic on mental health, burnout, and moral distress of critical care nurses in the United States. Anxiety, depression, and risk for PTSD impacted a third to nearly half of nurses in our sample. Our respondents reported moderate to high levels of burnout and moral distress. All measures of distress, burnout, and mental health were moderately to highly correlated in our sample highlighting the interconnectedness and complexity of challenges critical care nurses may face as a result of the pandemic.
Levels of burnout in our sample are higher than those reported by emergency department and trauma nurses32 , 33 prior to the pandemic. Moral Distress levels in our sample are similar but slightly higher than previously reported in a sample of acute and critical care nurses prior to the pandemic18 and a sample of ICU nurses from Romania during the pandemic.34
Concerningly, the prevalence of moderate to severe anxiety (31%) and depression (44.6%), and PTSD risk (46.7%) in this sample is markedly higher in comparison to the prevalence of these disorders in the US when measured prior to the pandemic. For instance, up to 28% of traumatic injury survivors35 and 17% of veterans develop PTSD,36 while approximately 19% and 8% of US adults live with anxiety37 and depression,38 respectively.
While are findings are in-line with some prior reports from China21 and Africa,39 the incicence of of PTSD, depression, and anxiety is much higher than other studies of healthcare workers during COVID-19. For instance, a study from China reported a 28.7% incidence of PTSD symptoms among healthcare workers.40 Additionally, a recent review that summarized findings from seven studies on mental health of COVID-19 healthcare workers found the incidence of depression and anxiety to be approximately 24% across studies that included participants in China, Brazil, the United Kingdom, and India.41 Of note, these reports include HCWs across settings and disciplines while our study focused on critical care nurses who experienced and cared for the sickest patients during the pandemic.
Younger nurses with less experience in our sample had higher levels of burnout raising concerns for the critical care workforce if large numbers of young nurses consider leaving practice. Nurse respondents that reported a shortage of PPE and perceived lack of support from administration had higher levels for all measures of distress and mental health—burnout, moral distress, risk for PTSD, depression, and anxiety. This mirrors findings from other studies39 and from a recent review42 which found PTSD risk was increased with low social support at work, working in unsafe settings, and lack of PPE. This link between administrative support, shortage of PPE with mental health, burnout, and moral distress is especially concerning for two reasons: the high percentages of nurses that reported shortage of PPE (71.2%) and not feeling fully supported by hospital administration (77.5%) and the link between system related factors such as lack of resources and administrative support and intent to leave practice.34
Interventions are needed to support critical care nurses during the remainder of the pandemic and continue post-pandemic to ensure a healthy workforce. Nurse reported concerns about lack of administrative support and resources need to be addressed by healthcare organizations. Understanding what type of support nurses want from leadership should be a priority research question in future studies. Current recommendations for organizational-based support of healthcare workers include providing: adequate supplies,42 ongoing training and updates on best practices for treating COVID-19,42 available leaders who empower staff to share their challenges and emotions,43 accessible peer debriefing,43 and counseling services.42 Partnering with mental health experts to address the complex mental health needs of critical care nurses and all healthcare workers currently and after the pandemic should be a priority for practice and policy. Ensuring that hospitals have adequate funding to meet the increasing mental health support needs of staff will require advocacy at both national and state levels. Additional factors that may decrease stress experienced critical care nurses include: high levels of support from other disciplines in the care of patients and families,9 , 43 high quality teamwork and social support at work, 9 , 42 and increased support from the community or social networks.9
Limitations to our study include a focus on a United States population of critical care nurses. While our findings mirror those found in other countries, there may be variations based on region that are not identified in this study. It is also important to note, that while we focused on critical care nurses, the challenges found in our sample are also present across other HCWs and settings.44 , 45 Additionally, our survey was conducted while COVID cases were still high in many parts of the country which may have impacted sample size and account for some of the incomplete surveys. As this study was completed October 2020 through early January 2021, results account for neither the impact of subsequent COVID surges nor the effect of vaccination availability on the ICU nurse experience. Follow up, after the pandemic is crucial to fully understand the long-term impact on critical care nurses and other healthcare workers. In particular, future work should focus on the interaction between moral distress, burnout, and mental health—anxiety, depression, and PTSD—given the high concordance among these measures.
Conclusion
This study offers important insights about the mental health of U.S. critical care nurses during a global pandemic and sheds light on incidence of anxiety, depression, and PTSD in this population. Findings from this national study can guide the development of interventions customized to needs of ICU nurses as it relates to mental health. Notably, nurses who perceived to be supported by hospital administration had a better mental health profile than those who did not. Future studies of leadership styles and approaches during the pandemic may offer insights into this finding. ICU workforce health must be a priority in healthcare organizations as a healthy workforce is integrally linked to the well-being of the patients we serve. Failure to suppport the mental health of critical care nurses, as well as ensure availability of PPE, may result in an exodus of nurses from the bedside ultimately compromising the safety and quality of patient care.
Declaration of Competing Interest
The authors have no conflicts of interest.
Funding
This work was supported by the Wallace Research Award, a Marquette University College of Nursing Internal Grant
References
- 1.Jervis R. Death is our greeter’: Doctors, nurses struggle with mental health as coronavirus cases grow. USA Today. 2020 https://www.usatoday.com/story/news/nation/2020/05/03/coronavirus-death-count-has-doctors-struggling-mental-health/3063081001/ Published May 3, 2020. Accessed May 4. [Google Scholar]
- 2.Washburn L. If you think too much, you cry’: Nurse shares what it's like to care for the sickest coronavirus patients. USA Today. 2020 https://www.usatoday.com/story/news/nation/2020/03/28/nurses-caring- covid-19- patients-ventilators-tell-what-its-like/2925359001/. Published March 28, 2020Accessed May 4. [Google Scholar]
- 3.Jacobs A. Frontline health care workers aren't feeling the ‘Summer of Joy. New York Times. 2021 https://www.nytimes.com/2021/07/01/health/covid-nurses-doctors-burnout.html Published July 1, 2021. Accessed December 27. [Google Scholar]
- 4.Mejia B. ICU doctors, nurses demoralized over ‘needless’ COVID-19 misery. ‘Patients are still dying’. Los Angeles Times. 2021 https://www.adn.com/nation-world/2021/12/25/icu-doctors-nurses-demoralized-over-needless-covid-19-misery-patients-are-still-dying/ Published: December 25, 2021. Accessed December 27. [Google Scholar]
- 5.Murthy S, Gomersall CD, Fowler RA. Care for critically ill patients with COVID-19. JAMA Insights. 2020;323:1499–1500. doi: 10.1001/jama.2020.3633. [DOI] [PubMed] [Google Scholar]
- 6.Wang Y, Lu X, Li Y, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;20(11):1430–1434. doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernstein L, Boburg S, Sacchetti M, Brown E. Covid-19 hits doctors, nurses and EMTs, threatening health system. Washington Post. 2020 https://www.washingtonpost.com/health/covid-19-hits-doctors-nurses-emts-threatening-health-system/2020/03/17/f21147e8-67aa-11ea-b313-df458622c2cc_story.html Published March 17, 2020Accessed May 4. [Google Scholar]
- 8.Society of Critical Care Medicine SCCM COVID-19 rapid-cycle survey 2 report. Critical Connections Blog. 2020 https://sccm.org/Blog/May-2020/SCCM-COVID-19-Rapid-Cycle-Survey-2-Report. Published May 5, 2020Accessed May 6. [Google Scholar]
- 9.Guttormson J, Calkins K, McAndrew N, Fitzgerald J, Losuredo H, Loonsfoot D. Critical care nurses experiences during the COVID-19 pandemic: A US national survey. Am J Crit Care. 2021:e1–e7. doi: 10.4037/ajcc2022312. [DOI] [PubMed] [Google Scholar]
- 10.Goodyear C. COVID-19: How nurse managers can mitigate nurse PTSD. American Association of Critical-Care Nurses Blog. 2020 https://www.aacn.org/blog/covid-19-how-nurse-managers-can-mitigate-nurse-ptsd Published April 3, 2020. Accessed May 4. [Google Scholar]
- 11.Thew J. COVID-19 is affecting critical care nurses: What nurse leaders need to know. Health Leaders. 2020 https://www.healthleadersmedia.com/nursing/covid-19-affecting-critical-care-nurses-what-nurse-leaders-need-know Published April 8, 2020. Accessed May 4. [Google Scholar]
- 12.Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. Am J Crit Care. 2015;24:412–421. doi: 10.4037/ajcc2015291. [DOI] [PubMed] [Google Scholar]
- 13.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement—Burnout syndrome in critical care health-care professionals. Chest. 2016;150(1):17–26. doi: 10.1016/j.chest.2016.02.649. [DOI] [PubMed] [Google Scholar]
- 14.Young JL, Derr DM, Cicchillo VJ, Bressler S. Compassion satisfaction, burnout, and secondary traumatic stress in heart and vascular nurses. Crit Care Nurs Quart. 2011;34(3):227–234. doi: 10.1097/CNQ.0b013e31821c67d5. [DOI] [PubMed] [Google Scholar]
- 15.Mealer M, Burnham EL, Goode CJ, Rothbaum B, Moss M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depress Anxiety. 2009;26(12):1118–1126. doi: 10.1097/CNQ.0b013e31821c67d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Epp K. Burnout in critical care nurses: A literature review. Dynamics. 2012;23(4):25–31. [PubMed] [Google Scholar]
- 17.Browning AM. Moral distress and psychological empowerment in critical care nurses caring for adults at end of Life. Am J Crit Care. 2013;22(2):143–151. doi: 10.4037/ajcc2013437. [DOI] [PubMed] [Google Scholar]
- 18.Epstein EG, Whitehead PB, Prompahakul C, Thacker L R, Hamric AB. Enhancing understanding of moral distress: The measure of moral distress for health care professionals. AJOB Empir Bioeth. 2019;10(2):113–124. doi: 10.1080/23294515.2019.1586008. 2019. [DOI] [PubMed] [Google Scholar]
- 19.Huffman DM, Rittenmeyer L. How professional nurses working in hospital environments experience moral distress: A systematic review. Crit Care Nurs Clin North Am. 2012;24(1):91–100. doi: 10.1016/j.ccell.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 20.McAndrew N, Leske J, Schroeter K. Moral distress in critical care nursing: The state of the science. Nurs Ethics. 2018;25(5):552–570. doi: 10.1177/0969733016664975. [DOI] [PubMed] [Google Scholar]
- 21.Lai J, Ma S, Wang Y., et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease. JAMA Network Open. 2019;3(3) doi: 10.1001/jamanetworkopen.2020.3976. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guttormson JL, Chlan L, Savik K, Weinert CR. Factors influencing nurse sedation practices with mechanically ventilated patients: A U.S. national survey. Intens Crit Care Nurs. 2010;26:44–50. doi: 10.1016/j.iccn.2009.10.004. 2010. [DOI] [PubMed] [Google Scholar]
- 23.Guttormson J, Chlan L, Tracy MF, Hetland B, Mandrekar J. Nurses’ attitudes and practices related to sedation: A national survey. Am J Crit Care. 2019;28:255–263. doi: 10.4037/ajcc2019526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stamm BH. 2nd Ed. Pocatello, ID; 2010. The Concise ProQOL Manual.https://proqol.org/proqol-manual Accessed May 8, 2020. [Google Scholar]
- 25.Flarity K, Gentry JE, Mesnikoff N. The effectiveness of an educational program on preventing and treating compassion fatigue in emergency nurses. Adv Emerg Nurs J. 2013;35(3):247–258. doi: 10.1097/TME.0b013e31829b726f. [DOI] [PubMed] [Google Scholar]
- 26.Weidlich CP, Ugarriza DN. A pilot study examining the impact of care provider support program on resiliency, coping, and compassion fatigue in military health care providers. Mil Med. 2015;180(3):290–295. doi: 10.7205/MILMED-D-14-00216. [DOI] [PubMed] [Google Scholar]
- 27.Brewin CR, Rose S, Andrews B, Green J, Tata P, McEvedy C, Turner S, Foa EB. Brief screening instrument for post-traumatic stress disorder. Br J Psychiatry. 2002;181:158–162. doi: 10.1017/s0007125000161896. [DOI] [PubMed] [Google Scholar]
- 28.Walters JTR, Bisson JI, Shepherd JP. Predicting post-traumatic stress disorder: Validation of the trauma screening questionnaire in victims of assault. Psychol Med. 2007;37:143–150. doi: 10.1017/S0033291706008658. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Wu J, Yu Z, Blair MJ, Kean J, Stump T, Monahan PO. The Patient Health Questionnaire Anxiety and Depression Scale (PHQ-ADS): Initial validation in three clinical trials. Psychosom Med. 2016;78:716–727. doi: 10.1097/PSY.0000000000000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 32.Hunsaker S, Chen H, Maughan D, Heaston S. Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. J Nurs Scholarsh. 2015;47(2):186–194. doi: 10.1111/jnu.12122. [DOI] [PubMed] [Google Scholar]
- 33.Hinderer KA, VonRueden KT, Friedmann E, et al. Burnout, compassion fatigue, compassion satisfaction, and secondary traumatic stress in trauma nurses. J Trauma Nurs. 2014;21(4):160–169. doi: 10.1097/JTN.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 34.Petriosor C, Breazu C, Doroftei M, Maries I, Popescu C. Association of moral distress with anxiety, depression, and an intention to leave among nurses working in intensive care units during the COVID-19 pandemic. Healthcare. 2021;9:1377. doi: 10.3390/healthcare9101377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shih RA, Schell TL, Hambarsoomian K, Marshall BN, Belzberg H. Prevalence of PTSD and major depression following trauma-center hospitalization. J Trauma. 2010;69(6):1560–1566. doi: 10.1097/TA.0b013e3181e59c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lk Richardson, Frueh BC, Acierno R. Prevalence estimates of combat-related PTSD: A critical review. Aust N Z J Psychiatry. 2010;44(1):4–19. doi: 10.3109/00048670903393597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harvard Medical School. National Comorbidity Survey (NCS). Data Table 2: 12-month prevalence DSM-IV/WMH-CIDI disorders by sex and cohort. https://www.hcp.med.harvard.edu/ncs/index.php. Published July 19, 2007. Accessed December 20, 2021.
- 38.Substance Abuse and Mental Health Services Administration. National survey on drug use and health. https://www.samhsa.gov/data/report/2019-methodological-summary-and-definitions. Published September 11, 2020. Accessed December 20, 2021.
- 39.Asnakew S, Getasew L, Liyeh TM, et al. Prevalence of post-traumatic stress disorder on health professionals in the era of COVID-19 pandemic, Northwest Ethiopia, 2020: A multi-centered cross-sectional study. PLoS ONE. 2021;16(9) doi: 10.1371/journal.pone.0255340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen H, Wang B, Cheng Y, et al. Prevalence of posttraumatic stress symptoms in health care workers after exposure to patients with COVID-19. Neurobiol Stress. 2020;13 doi: 10.1016/j.ynstr.2020.100261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sahebi A, Nejati-Zarnaqui B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.d'Ettorre G, Ceccarelli G, Santinelli L, et al. Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: A systematic review. Int J Environ Res Public Health. 2021;18(12):601. doi: 10.3390/ijerph18020601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Donkers MA, Gillissen VJHS, Candel MJJM, et al. Moral distress and ethical climate in intensive care medicine during COVID-19: a nationwide survey. BMC Med Ethics. 2021;22:73. doi: 10.1186/s12910-021-00641-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carmassi C, Dell'Oste V, Bui E, et al. The interplay between acute post-traumatic stress, depressive and anxiety symptoms on healthcare workers functioning during the COVID-19 emergency: A multicenter study comparing regions with increasing pandemic incidence. J Affect Disord. 2022;298:209–216. doi: 10.1016/j.jad.2021.10.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mediavilla R, Fernandez-Jimenez E, Martinez-Ales G, et al. Role of access to personal protective equipment, treatment prioritization decisions, and changes in job functions on health workers’ mental health outcomes during the initial outbreak of the COVID-19 pandemic. J Affect Disord. 2021;295:405–409. doi: 10.1016/j.jad.2021.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]