Abstract
Treating blood pressure (BP) alone may provide only limited benefits while it is recommendable to manage the total cardiovascular risk. To date, several studies have shown that concomitant treatment of hypertension and dyslipidemia with non-pharmacological approaches and/or metabolically neutral antihypertensive drugs and statins produce a significantly greater reduction of the risk of developing cardiovascular disease. Thus, in this review article, we summarize the available evidence regarding non-pharmacological and pharmacological approaches with a favourable effect on both BP and lipids.
Keywords: Hypertension, Dyslipidemia, Blood pressure, DASH, Statins, PUFA
Introduction
According to the latest estimates of the World Health Organization (WHO), hypertension is a highly prevalent risk factor for the development of cardiovascular disease, affecting 1.13 billion people in the world [1].
Even though hypertension per se has been acknowledged as a leading cause of death and disease burden, hypertensive patients with additional cardiovascular risk factors exhibit even higher morbidity and mortality rates [2]. In this regard, the INTERHEART study has recently showed that single risk factors increase the total cardiovascular risk from 2- to 3-fold, while the coexistence of hypertension, type 2 diabetes mellitus, dyslipidemia and smoking in the same individual can result in a > 20-fold increase in risk compared to patients only affected by hypertension [3]. Based on these observations, treating blood pressure (BP) alone may provide only limited benefits while it is recommendable to manage the total cardiovascular risk. Several studies have shown that concomitant treatment of hypertension and dyslipidemia with non-pharmacological approaches and/or metabolically neutral antihypertensive drugs and statins produce a significantly greater reduction of the risk of developing cardiovascular disease [4, 5]. Thus, in this review article, we summarize the available evidence regarding non-pharmacological and pharmacological approaches with a favourable effect on both BP and lipids.
Diet and Lifestyle
Based on the recommendations of the European Society of Cardiology/European Society of Hypertension (ESC/ESH) guidelines, the treatment of hypertension first involves lifestyle interventions, such as sodium restriction, alcohol moderation, regular exercise and weight control [6]. Most of these recommendations overlap with those of the European guidelines for the management of dyslipidaemias, that advise to reduce the dietary intake of saturated fatty acids, increase the daily consumption of wholegrain product, vegetables, fruit and fish, and practice aerobic physical activity for 3.5–7 h per week [7].
In the last decades, the role of nutrition in cardiovascular prevention has been extensively investigated. Dietary patterns that have been more extensively evaluated are the Dietary Approaches to Stop Hypertension (DASH) diet and the Mediterranean diet, that recommend higher intakes of fruits, vegetables, whole grains, nuts and legumes, low-fat dairy and lower amounts of processed meats and sweetened beverages, with beneficial effect on both blood lipids and BP [8, 9].
Overall, available evidence reinforces the concept that complete eradication of animal products is not necessary for BP reduction and serum lipids control, and also adds that dietary salt reduction is a powerful tool in adjunct with increased plant-food consumption [10, 11].
Combining data from the available literature, a low-salt energy-restricted Mediterranean diet should be considered for patients affected at the same time by high BP and hypercholesterolemia before either starting pharmacological treatment or increasing the number of lipid-lowering and/or anti-hypertensive drugs [12].
Nutraceuticals with Both Antihypertensive and Lipid-Lowering Effects
A large and growing body of evidence supports the potentially protective role in cardiovascular prevention of specific foods and bioactive molecules from natural sources [13, 14].
In the last years, the Italian Society of Hypertension (SIIA) and ESH published statements summarizing the best available evidence of efficacy for nutraceuticals with proved BP-lowering effect [15, 16]. In addition, the Lipid and Blood Pressure Meta-analysis Collaboration Group and the International Lipid Expert Panel (ILEP) released a position paper endorsed by a number of European lipid societies with the aim to provide consensus-based recommendations for the optimal use of nutraceuticals in the management of dyslipidaemias [17].
In the following sub-paragraphs, the attention of the review has been focused on food components and natural bioactive substances with both lipid- and BP-lowering effect [18].
Berberine
Berberine is an alkaloid from different species of plants that acts maily reversibly inhibiting the proprotein convertase subtilisin/kexin type 9 (PCSK9) [19, 20], but also reducing the absorption of cholesterol in the intestine, increasing its excretion and promoting the formation of new bile acids [21]. In addition, berberine reversibly inhibits the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase-mediated oxidative stress and activates 5´ AMP-activated protein kinase (AMPK), and consequently leads to a reduced expression of lipogenic genes, contributes to an increased oxidation of fatty acids, ameliorates insulin-sensitivity and relieves BP levels [22, 23].
The berberine lipid-lowering effect was confirmed in humans by a recent meta-analysis including 16 clinical trials with 2147 participants [24]. Berberine supplementation was effective in improving serum levels of total cholesterol (TC: – 0.47 mmol/L, 95% Confidence Interval (CI): – 0.64, – 0.31, P < 0.00001), LDL-C (– 0.38 mmol/L, 95% CI – 0.53, – 0.22, P < 0.00001), triglycerides (TG: – 0.28 mmol/L, 95% CI – 0.46, – 0.10), P = 0.002) and high-density lipoprotein cholesterol (HDL-C: 0.08 mmol/L, 95% CI 0.03, 0.12, P = 0.001).
The evidence on the BP-lowering effect in humans following supplementation with berberine is less solid and limit to single small clinical trials. To date, no meta-analyses has investigated the effect on BP levels of berberine alone. On the other hand, a number of meta-analyses and large clinical trials have aimed to assess the effect of the supplementation with nutraceutical compounds containing berberine (e.g. Armolipid Plus®) on BP and high BP complications [25]. Mazza et al. found that a nutraceutical compound containing 3 mg monacolin K, 500 mg berberine, 30 mg coenzyme Q10,00 mcg folic acid and 40 mg chrome was effective in preventing the progression to overt hypertension in a cohort of 131 patients with pre-hypertension on a 3-month period follow-up [26]. In another multicenter, randomized, double-blind, placebo controlled clinical trial enrolling 150 patients with metabolic syndrome and increased left ventricular mass (LVM), a nutraceutical combination of berberine, red yeast rice extract and policosanols was shown to reduce LVM compared to the baseline (– 2.7%, P-value < 0.0001) and the placebo (– 4.1%, P-value < 0.0001) [27].
Based on the pooled available evidence, the use of berberine is indicated both in primary and secondary prevention for cardiovascular disease, especially in slightly/moderately hypercholesterolemic patients with high BP levels. The dosages used in clinical practice vary from 500 to 1500 mg/day, with good efficacy on inflammatory markers and tolerable side effects [28].
Coenzyme Q10
CoQ10 is a potent lipid phase antioxidant, particularly concentrated in fish red meat. At molecular level, CoQ10 reduces the oxidation of low-density lipoproteins (LDL) and the oxidative stress. CoQ10 is also a co-factor and co-enzyme in mitochondrial oxidative phosphorylation, contributing to modulate BP and being often reduced in hypertensive patients [29]. In the past decade, a number of controlled clinical trials sustained the BP and lipid-lowering effect of CoQ10 supplementation, alone or in addition to other natural substances [30, 31]. A meta-analysis of 17 randomized controlled clinical trials (648 participants overall) showed that CoQ10 significantly decreased SBP (standardized mean difference (SMD): – 0.3, 95% CI – 0.52, – 0.08) without affecting DBP in patients with metabolic syndrome [32]. In addition, a number of meta-analyses showed promising effects of CoQ10 supplementation on lowering serum lipids levels among patients with metabolic disorders of affected by coronary artery disease [33–35]. To date, the main issue of CoQ10 use is related to its low bioavailability in humans, that could be improved by the use of CoQ10 nanoemulsion [36].
Green Tea
Green tea extract is particularly rich in polyphenols, including the epigallocatechin-3-gallate (EPCG), a flavan-3-ol with powerful cardioprotective and antioxidant activities. The antioxidant activity of the EPCG is responsible for the green tea effect on reducing the lipid peroxidation and the number of oxidized LDL (oxy-LDL). In addition, green tea is an activator of AMPK, inhibits the β-Hydroxy β-methylglutaryl-CoA (HMG-CoA) reductase and interferes with the micellar solubilization and absorption of endogenous cholesterol. Finally, catechins seem to enhance the expression of hepatic LDL-receptor (LDL.R) and increase the biliary excretion of cholesterol [37, 38].
A meta-analysis of 10 randomized controlled clinical trials has recently revealed that tea consumption associates with improvement in LDL-C (SMD: – 0.63, 95% CI – 1.06, – 0.2, P-value = 0.0057) and DBP (SMD: – 0.89, 95% CI – 1.73, – 0.05, P-value = 0.0388) with a trend toward decrease in SBP (SMD: – 0.83, 95% CI – 1.75, 0.09, P-value = 0.769) [39]. Over the years, green tea has also been associated to improvements in endothelial function and arterial stiffness [40, 41], and to a significant decrease in the risk of morbidity and mortality for cardiovascular disease [42].
Cocoa
An updated Cochrane meta-analysis of 20 double-blind, placebo-controlled randomized clinical trials involving 856 mainly healthy participants revealed a statistically significant BP reducing effect of flavanol-rich cocoa products in short-term trials of 2–18 weeks duration [43]. The meta-analysis pooled data from clinical trials that provided participants with a daily average 545.5 mg flavanols in 3.6–105 g of cocoa products per day, and found impressive effect sizes on SBP and DBP (SBP: MD: – 2.8 mmHg, 95% CI – 4.7, – 0.8 mmHg, P = 0.005; DBP: MD: − 2.2 mmHg, 95% CI – 3.5, – 0.9 mmHg, P = 0.006). More recently, another meta-analysis of 8 randomized controlled clinical trials and 433 participants with diabetes found that cocoa consumption exerts a significant reduction in LDL-C levels (SMD: – 15.49 mg/dl, 95% CI – 24.56, – 6.42, P = 0.001) [44].
Dark chocolate flavanols increase NO bioavailability, protect vascular endothelium, and modulate a number of risk factors for the development of cardiovascular disease [45, 46]. The final evidence on the benefit of cocoa polyphenols in improving cardiovascular health and preventing cardiovascular disease will be provided by the ongoing study, coordinated by the Department of Epidemiology of the Brigham and Women University, Boston, US and supported by MARS Symbioscience. This study is investigating 18.000 individuals randomized either to placebo capsules or to the isolated cocoa extract with a 4 year long follow-up, in order to evaluate the effect of cocoa flavanoids in reducing the risk of major cardiovascular events [47].
Aged Garlic Extract
Garlic-derived polysulfides (in particular S-allylcysteine) enhance the regulation of endothelial NO, inducing vasodilation and BP reduction [18]. Aged dry garlic extract has also calcium channel blocking and angiotensin-converting enzyme (ACE) inhibitory activity, reduces sensitivity to catecholamines, increases bradykinin and NO, and finally improves arterial compliance [48].
Pooling data from 12 clinical trials and 553 hypertensive patients, a meta-analysis has recently confirmed that in humans aged garlic extract lower SBP by 8.3 ± 1.9 mmHg and DBP by 5.5 ± 1.9 mmHg, and found that this reduction in BP associates with a 16–40% reduction in the risk of developing cardiovascular events [49]. Moreover, garlic extract seems to have mild though clinically significant antiaggrengant and lipid-lowering actions [50, 51]. One of the latest meta-analyses on this issue included 39 randomized controlled clinical studies and 2300 adults treated with aged garlic extract for at least 2 weeks [52]. This meta-analysis confirmed that aged garlic extract was effective in reducing total cholesterol (TC) and LDL-C by 10% when the supplementation was continued for at least 2 months and the concentrations of cholesterol were slightly elevated at baseline. Another meta-analysis of 6 randomized controlle clinical trials found that garlic extract exert had significant effect on TC also in patients with CAD (WMD: – 16.32 mg/dL, 95% CI – 31.22, – 1.43, P-value = 0.032) [53].
Anti-hypertensive Drugs with Effect on Serum Lipids
Some antihypertensive drugs have a neutral or beneficial effect on the lipid profile, while others have an adverse effect that is not necessarily outweighed by the beneficial clinical effects of BP-lowering on cardiovascular risk. Drug-induced changes in lipid levels may be particularly important in hypertensive patients since up to 45% of untreated patients with primary hypertension are also affected by lipid abnormalities a priori, such as high serum levels of LDL-C [54].
To date, there is general consensus that thiazide diuretics and nonselective β-blockers adversely affect lipid levels, but many areas of disagreement exist about the effects of other antihypertensive agents on lipids. This disagreement is partially due to the impossibility of judging the results from clinical trials with heterogeneous designs and that have been carried out on different study population cohorts. However, metabolic effects of antihypertensive drugs are of great importance in long-term treatment of hypertension, as the Oslo Study clearly confirmed [55].
Anti-hypertensive Drugs with Beneficial or Neutral Effect on Lipids
Through the investigation of the effects of 85 antihypertensive drugs on lipids and BP in over 65.000 patients, the meta-analysis by Kasiske et al. [56] found that β-blockers with intrinsic sympathomimetic activity and cardioselectivity favorably affected serum lipids through reducing both TC (– 0.14 mmol/L, 95% CI – 0.24, – 0.04 mmol/L) and LDL-C (– 0.17 mmol/L, 95% CI – 0.28, – 0.07 mmol/L); α-blockers beneficially affected TC (– 0.23 mmol/L, 95% CI – 0.28, – 0.18 mmol/L), LDL-C (– 0.20 mmol/L, 95% CI – 0.25, 0.15 mmol/L), TG (– 0.07 mmol/L, 95% CI – 0.11, – 0.03 mmol/L), and, in younger individuals, HDL-C (0.02 mmol/L, 95% CI 0.01, 0.04 mmol/L). ACE inhibitors reduced TG (– 0.07 mmol/L, 95% CI – 0.12, – 0.02 mmol/L), and, in diabetics, TC (– 0.22 mmol/L, 95% CI – 0.34, – 0.10 mmol/L). Direct vasodilators reduced TC (– 0.22 mmol/l, 95% CI – 0.30, – 0.10 mmol/L) and LDL-C (– 0.22 mmol/L, 95% CI – 0.29, – 0.11 mmol/L) and increased HDL-C (0.06 mmol/L, 95% CI 0.02, 0.09 mmol/L).
Finally, the thiazides-like diuretic indapamide does not have any impact on serum lipids and lipoproteins [57].
Anti-hypertensive Drugs with Negative Effect on Lipids
According to available evidence from early controlled clinical trials, diuretics were believed to increase TG and TC on average by 30% and 6–8% respectively, with a negative impact also on LDL-C and very LDL-C (VLDL-C). β-1 selective and nonselective β-blockers were believed to increase TG by 30% and lower HDL-C by 5–15% [58].
Although in past decades findings from several randomised, controlled clinical trials corroborated the hypothesis that antihypertensive drugs may influence serum lipid levels, in general population no significant association for single antihypertensive drug was observed over time, except for the combination of a beta-blocker and a diuretic associated to higher lipids levels [59].
The above large meta-analysis by Kasiske et al. concluded that, in absence of statin treatment, patients using beta-blockers had lower HDL-C concentrations and higher cholesterol ratios than untreated hypertensives, while patients on diuretics had higher TC and HDL-C levels compared to untreated hypertensives. However, after adjustment for potential confounders, these differences were smaller and the effect size on HDL-C for users of both beta-blocker and diuretic only persisted [57].
Data from the Framingham Heart Study suggest that for the same amount of BP reduction, BP-lowering agents that have a negative impact on serum lipids cause less reduction in the risk of cardiovascular disease [56]. Actually, this may at least partially explain why prospective clinical trials with diuretics and β-blockers failed to prove to reduce the incidence of cardiovascular events as much as would have been expected based on the BP reduction [56].
Even though the persistence of prespecified lipid changes during extended therapy is unresolved due to fragmentary observations, considerable data suggest that it continues on the long term [58].
Lipid-Lowering Drugs with Effect on Blood Pressure
Indirect evidence from several clinical trials investigating lipid-lowering regimens suggests that lowering cholesterol may simultaneously reduce BP by 2–5 mmHg [60]. The mechanism Most of these observations refer to clinical studies testing traditional lipid-lowering drugs [i.e. statins and omega-3 polyunsaturated fatty acids (PUFAs)], while evidence from the emerging drugs are few and definitely inconsistent. Based on the available evidence, ezetimibe and bempedoic acid seem not to exert any clinically relevant effect on BP [61, 62]. In addition, according to the results of a meta-analysis from the Cochrane Collaboration’s Group, treatment with PCSK9 inhibitors alirocumab and evolocumab has no significant effect on the risk of new onset of hypertension (alirocumab: OR: 0.92, 95% CI 0.72, 1.18 versus placebo, and OR = 1.01, 95% CI 0.57, 1.79 versus other comparator; evolocumab: OR = 1.51, 95% CI 0.06, 37.04 versus comparator) [63].
Statins
Among the first observations regarding that the addition of statin treatment to conventional antihypertensive therapy might improve BP control in hypertensive patients with hypercholesterolemia, there are those from the Brisighella Heart Study (BHS) group [64]. Then, the University of California San Diego (UCSD) Statin Study prospectively evaluated the impact of statins on BP in 1016 patients with increased levels of serum cholesterol [65]. This study was one of the first large randomized clinical trials on the topic and provided evidence that there was a significant decrease in BP with statin therapy compared to placebo, even though the effect on DBP in the simvastatin group and the effect on SBP in the pravastatin group disappeared in a 2-month period.
The effect on BP of statins—as suggested by the available literature- is dependent upon well-known and recognized mechanism [66]. As a matter of fact, statins up-regulate the expression and activity of endothelial nitric oxide synthase (eNOS) through the activation of phosphatidylinositol 3-kinase, the inhibition of geranylgeranylation of the small G-protein Rho, and of vascular Rac1-mediated activation of NADPH-oxidase [67–69]. In addition, statins have also been found to down-regulate the expression of AT1 receptors for angiotensin-II and to inhibit several angiotensin II–activated intracellular signaling systems, delay hypertension-induced vascular alterations, reduce large artery stiffness, and improve systemic arterial compliance [70].
According to a meta-analysis pooling data from 20 controlled clinical trials and 828 patients with and without hypertension, the antihypertensive effect of statins seems to be more pronounced when the mean pre-treatment SBP is > 130 mmHg [60]. The meta-analysis also provided evidence that in statin-treated patients seems to be a tendency toward decrease in DBP (mean difference 0.9 mmHg, 95% CI 2.0, 0.2 compared with controls), with the greatest improvement that has to be expected in patients with baseline DBP > 80 mmHg. Based on these evidences, the impact of statins on BP should to be considered as dependent on the initial BP values, and a greater antihypertensive effect should be expected for higher initial values of BP.
More recently, a meta-analysis of 5 randomized controlled clinical trials testing rosuvastatin, demonstrated a modest—though significant- improvement in DBP (– 2.12 mmHg, 95% CI – 3.72, – 0.52) and a trend toward improvement in SBP (– 2.27 mmHg, 95% CI − 4.75 to 0.25) in hypertensive patients. This has corroborated the hypothesis that also treatment with rosuvastatin is beneficial to control hypertension and, consequently, contribute toward reducing the risk of cardiovascular events in patients with dyslipidemia and hypertension [71].
Over the years, all these evidence raised some concerns as regard the risk of adverse events related to effect of statins on BP. Then, 5.9 million clinical reports submitted to FDA Adverse Events Reporting System (FAERS) from 2004 to 2015 were retrieved and reviewed [72]. By the comparison of the reporting rate of hypotension event, atorvastatin and simvastatin were found to be significantly associated with reduction in BP (atorvastatin: pooled ROR = 1.26, adjusted P-value = 8.60 × 10 –4; simvastatin: pooled ROR = 1.94, adjusted P-value = 4.16 × 10 –45). On the other hand, the association between rosuvastatin and hypotension was proved to be nonsignificant (adjusted P-value = 0.65).
In the future, further studies evaluating the magnitude of the antihypertensive effects of statins should: not change the dosages of the antihypertensive drugs during the study, consider BP changes as one of the primary endopoints, use 24-h ambulatory monitoring (ABPM) measurements to accurately determine the extent and duration of antihypertensive effects, evaluate the effect of statins on specific subgroup of hypertensive patients (e.g., dippers vs. nondippers), assess the effects of different statin dosages and determine the onset and duration of antihypertensive actions of statins.
Omega-3 PUFAs
The dietary intake of omega-3 PUFAs has been inversely associated with cardiovascular disease morbidity and mortality in several epidemiological studies. Recent evidence suggests that this protective effect is—at least in part—mediated by a relatively small though significant decrease in BP [73]. Actually, omega-3 PUFAs exhibit wide-ranging biological actions that include regulating both vasomotor tone and renal sodium excretion, partly competing with omega-6 PUFAs for common metabolic enzymes and thereby decreasing the production of vasoconstrictor rather than vasodilator and anti-inflammatory eicosanoids. PUFAs also reduce Tumor Growth Factor-beta (TGF-beta) expression, angiotensin II formation and angiotensin-converting enzyme (ACE) activity, activate the parasympathetic nervous system and enhance endothelial nitric oxide (NO) generation. The final results are improved vasodilation and arterial compliance of both large and small arteries [73].
Following early observations suggesting a possible anti-hypertensive effect of omega-3 PUFAs in humans [74], their effect on BP was investigated in several observational and prospective clinical studies. Most of these studies used fish oil as a source of omega-3 PUFAs, and enrolled healthy normotensive subjects and patients with dyslipidemia, hypertension, diabetes or obesity. Many of these clinical trials examined the effects of omega-3 PUFAs on BP by the use of the 24-h ABPM [75–77].
Over the last decades, prospective studies on the topic have been included in a number of systematic reviews and meta-analyses. Early findings supported the BP-lowering effect of omega-3 PUFA only in hypertensive patients [78–80]. More recently, another meta-analysis pooled data from 17 randomized controlled clinical trials and 1524 normotensive and hypertensive subjects treated with 0.8–13.3 g/day fish oil for 8–56 weeks [81]. According to the findings of this meta-analysis, fish oil do not exert any effect on BP in normotensive subjects, whereas BP mildly decreases in patients with hypertension (– 2.6 mmHg in SBP and − 1.5 mmHg in DBP), without any dose-related trend.
The last comprehensive systematic review and meta-analysis on the effects of omega-3 PUFAs on BP was published by Miller et al. and includes data from 70 randomized controlled clinical trials, testing an average daily dose of 3.8 g omega-3 PUFA and considering a 3-month average follow-up [82]. Decrease in BP induced by omega-3 PUFA resulted to be statistically significant in both hypertensive (SBP: – 4.5 mmHg, 95% CI – 2.8, – 6.1; DBP: – 3.0 mmHg, 95% CI – 1.7, – 4.3) and normotensive (SBP: – 1.2 mmHg, 95% CI – 0.5, – 2.0; DBP: – 0.6 mmHg, 95% CI 0.0, – 1.2) individuals, though it was clinically relevant only in the former group. In agreement with previous meta-analyses, no dose–response relationship was observed.
Current evidence supports the hypothesis that omega-3 PUFAs significantly decreases the BP levels only in hypertensive patients and that they might prevent the development of new-onset hypertension, with potentially great implications for the clinical management of the patients with hypertension or at high risk for it. The effect of omega-3 PUFAs on BP is rather mild and not dose related.
Discussion
In the last decades, there has been significant progress in concomitant hypertension and hypercholesterolemia control, even though patients compliance with antihypertensive regimens continues being generally better than lipid-lowering treatments [83]. In keeping with this, the inclusion of statins and BP-lowering agents into a fixed combination might even double the effectiveness of statin therapy, and thereby achieve significantly greater reduction of cardiovascular risk, as supported by the findings of the CORAL study [84].
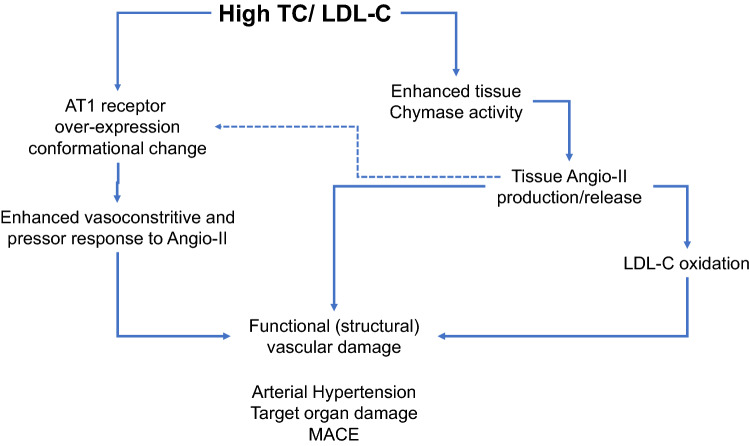
It must also be recognized that, up to date, only 2 broad-based studies have assessed the effect of statins specifically in hypertensive patients, with conflicting results. The Anglo-Scandinavian Cardiac Outcomes Trial—Lipid-Lowering Arm (ASCOT-LLA) evaluated the effect of adding a statin to BP-lowering treatment regimen in patients with hypertension and no clinically evident CHD, average total cholesterol levels ≤ 250 mg/dl at baseline, and at least 3 cardiovascular risk factors other than hypertension [85]. Statin addition in the ASCOT-LLA was associated with a 36% decrease in nonfatal myocardial infarction (NFMI) and fatal CHD and a 27% decrease in the incidence of fatal and nonfatal stroke compared to placebo [85]. On the contrary, in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial—Lipid Lowering Trial (ALLHAT-LLT), the administration of 40 mg pravastatin to hypertensive patients ≥ 65 years old did not lead to a significant difference versus standard of care in all-cause mortality and CHD events [86]. Definitely, the evidence of the efficacy of statins in decreasing cardiovascular morbidity and mortality in hypertensives are conflicting [87]. However, genetic studies in humans suggest that a predisposition for the development of both hypertension and dyslipidemia may result from the inheritance of shared genetic risk factors [88]. For this reason, the use of non-pharmacological and pharmacological approaches with a favourable effect on both BP and lipids hold promise of much greater gains against cardiovascular disease (Fig. 1).
Fig. 1.
Mechanisms involved in the interaction between hypercholesterolemia and Renin-Angiotensin system and hypertension. (from Ref. [70], mod)
Declarations
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement.
Conflict of interest
Claudio Borghi has served as a consultant for Servier, Menarini Corporate, Novartis Pharma, Novo Nordisk, Astra Zeneca, Alfasigma. Federica Fogacci, Arrigo F.G.Cicero and Davide Agnoletti have no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
7/19/2022
Missing Open Access funding information has been added in the Funding Note.
References
- 1.World Health Organization. Hypertension fact sheet. 2019 [cited 2021 10 October]. https://www.who.int/news-room/fact-sheets/detail/hypertension. Accessed 3 Jan 2022.
- 2.Williams B, Masi S, Wolf J, Schmieder RE. Facing the challenge of lowering blood pressure and cholesterol in the same patient: report of a Symposium at the European Society of Hypertension. Cardiol Ther. 2020;9(1):19–34. doi: 10.1007/s40119-019-00159-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L, INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 4.Multiple Risk Factor Intervention Trial Risk factor changes and mortality results. Multiple Risk Factor Intervention Trial Research Group. JAMA. 1982;248(12):1465–77. doi: 10.1001/jama.1982.03330120023025. [DOI] [PubMed] [Google Scholar]
- 5.Schwalm JD, McKee M, Huffman MD, Yusuf S. Resource effective strategies to prevent and treat cardiovascular disease. Circulation. 2016;133(8):742–55. doi: 10.1161/CIRCULATIONAHA.115.008721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2019;37(2):456. doi: 10.1097/HJH.0000000000002026. [DOI] [PubMed] [Google Scholar]
- 7.Authors/Task Force Members; ESC Committee for Practice Guidelines (CPG); ESC National Cardiac Societies 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205. doi: 10.1016/j.atherosclerosis.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER, 3rd, Lin PH, Karanja NM, Most-Windhauser MM, Moore TJ, Swain JF, Bales CW, Proschan MA, DASH Research Group Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial. Am J Clin Nutr. 2001;74(1):80–9. doi: 10.1093/ajcn/74.1.80. [DOI] [PubMed] [Google Scholar]
- 9.Antoniazzi L, Arroyo-Olivares R, Bittencourt MS, Tada MT, Lima I, Jannes CE, Krieger JE, Pereira AC, Quintana-Navarro G, Muñiz-Grijalvo O, Díaz-Díaz JL, Alonso R, Mata P, Santos RD. Adherence to a Mediterranean diet, dyslipidemia and inflammation in familial hypercholesterolemia. Nutr Metab Cardiovasc Dis. 2021;31(7):2014–22. doi: 10.1016/j.numecd.2021.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Gibbs J, Gaskin E, Ji C, Miller MA, Cappuccio FP. The effect of plant-based dietary patterns on blood pressure: a systematic review and meta-analysis of controlled intervention trials. J Hypertens. 2021;39(1):23–37. doi: 10.1097/HJH.0000000000002604. [DOI] [PubMed] [Google Scholar]
- 11.Rees K, Al-Khudairy L, Takeda A, Stranges S. Vegan dietary pattern for the primary and secondary prevention of cardiovascular diseases. Cochrane Database Syst Rev. 2021;2(2):CD013501. doi: 10.1002/14651858.CD013501.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cicero AFG, Veronesi M, Fogacci F. Dietary intervention to improve blood pressure control: beyond salt restriction. High Blood Press Cardiovasc Prev. 2021;28(6):547–53. doi: 10.1007/s40292-021-00474-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fogacci F, Borghi C, Cicero AFG. Diets, foods and food components’ effect on dyslipidemia. Nutrients. 2021;13(3):741. doi: 10.3390/nu13030741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strilchuk L, Cincione RI, Fogacci F, Cicero AFG. Dietary interventions in blood pressure lowering: current evidence in 2020. Kardiol Pol. 2020;78(7–8):659–66. doi: 10.33963/KP.15468. [DOI] [PubMed] [Google Scholar]
- 15.Cicero AFG, Grassi D, Tocci G, Galletti F, Borghi C, Ferri C. Nutrients and nutraceuticals for the management of high normal blood pressure: an evidence-based consensus document. High Blood Press Cardiovasc Prev. 2019;26(1):9–25. doi: 10.1007/s40292-018-0296-6. [DOI] [PubMed] [Google Scholar]
- 16.Borghi C, Tsioufis K, Agabiti-Rosei E, Burnier M, Cicero AFG, Clement D, Coca A, Desideri G, Grassi G, Lovic D, Lurbe E, Kahan T, Kreutz R, Jelakovic B, Polonia J, Redon J, Van De Borne P, Mancia G. Nutraceuticals and blood pressure control: a European Society of Hypertension position document. J Hypertens. 2020;38(5):799–812. doi: 10.1097/HJH.0000000000002353. [DOI] [PubMed] [Google Scholar]
- 17.Cicero AFG, Colletti A, Bajraktari G, Descamps O, Djuric DM, Ezhov M, Fras Z, Katsiki N, Langlois M, Latkovskis G, Panagiotakos DB, Paragh G, Mikhailidis DP, Mitchenko O, Paulweber B, Pella D, Pitsavos C, Reiner Ž, Ray KK, Rizzo M, Sahebkar A, Serban MC, Sperling LS, Toth PP, Vinereanu D, Vrablík M, Wong ND, Banach M. Lipid-lowering nutraceuticals in clinical practice: position paper from an International Lipid Expert Panel. Nutr Rev. 2017;75(1):731–67. doi: 10.1093/nutrit/nux047. [DOI] [PubMed] [Google Scholar]
- 18.Cicero AFG, Fogacci F, Colletti A. Food and plant bioactives for reducing cardiometabolic disease risk: an evidence based approach. Food Funct. 2017;8(6):2076–88. doi: 10.1039/c7fo00178a. [DOI] [PubMed] [Google Scholar]
- 19.Abidi P, Zhou Y, Jiang JD, Liu J. Extracellular signal-regulated kinase-dependent stabilization of hepatic low-density lipoprotein receptor mRNA by herbal medicine berberine. Arterioscler Thromb Vasc Biol. 2005;25(10):2170–6. doi: 10.1161/01.ATV.0000181761.16341.2b. [DOI] [PubMed] [Google Scholar]
- 20.Li H, Dong B, Park SW, Lee HS, Chen W, Liu J. Hepatocyte nuclear factor 1alpha plays a critical role in PCSK9 gene transcription and regulation by the natural hypocholesterolemic compound berberine. J Biol Chem. 2009;284(42):28885–95. doi: 10.1074/jbc.M109.052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li XY, Zhao ZX, Huang M, Feng R, He CY, Ma C, Luo SH, Fu J, Wen BY, Ren L, Shou JW, Guo F, Chen Y, Gao X, Wang Y, Jiang JD. Effect of Berberine on promoting the excretion of cholesterol in high-fat diet-induced hyperlipidemic hamsters. J Transl Med. 2015;13:278. doi: 10.1186/s12967-015-0629-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qiang X, Xu L, Zhang M, Zhang P, Wang Y, Wang Y, Zhao Z, Chen H, Liu X, Zhang Y. Demethyleneberberine attenuates non-alcoholic fatty liver disease with activation of AMPK and inhibition of oxidative stress. Biochem Biophys Res Commun. 2016;472(4):603–9. doi: 10.1016/j.bbrc.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 23.Kim WS, Lee YS, Cha SH, Jeong HW, Choe SS, Lee MR, Oh GT, Park HS, Lee KU, Lane MD, Kim JB. Berberine improves lipid dysregulation in obesity by controlling central and peripheral AMPK activity. Am J Physiol Endocrinol Metab. 2009;296(4):E812-9. doi: 10.1152/ajpendo.90710.2008. [DOI] [PubMed] [Google Scholar]
- 24.Ju J, Li J, Lin Q, Xu H. Efficacy and safety of berberine for dyslipidaemias: a systematic review and meta-analysis of randomized clinical trials. Phytomedicine. 2018;50:25–34. doi: 10.1016/j.phymed.2018.09.212. [DOI] [PubMed] [Google Scholar]
- 25.Suadoni MT, Atherton I. Berberine for the treatment of hypertension: A systematic review. Complement Ther Clin Pract. 2021;42:101287. doi: 10.1016/j.ctcp.2020.101287. [DOI] [PubMed] [Google Scholar]
- 26.Mazza A, Schiavon L, Rigatelli G, Torin G, Lenti S. The effects of a new generation of nutraceutical compounds on lipid profile and glycaemia in subjects with pre-hypertension. High Blood Press Cardiovasc Prev. 2019;26(4):345–350. doi: 10.1007/s40292-019-00332-6. [DOI] [PubMed] [Google Scholar]
- 27.Mercurio V, Pucci G, Bosso G, Fazio V, Battista F, Iannuzzi A, Brambilla N, Vitalini C, D’Amato M, Giacovelli G, Vaudo G, Schillaci G, Galletti F, Bonaduce D. A nutraceutical combination reduces left ventricular mass in subjects with metabolic syndrome and left ventricular hypertrophy: a multicenter, randomized, double-blind, placebo-controlled trial. Clin Nutr. 2020;39(5):1379–84. doi: 10.1016/j.clnu.2019.06.026. [DOI] [PubMed] [Google Scholar]
- 28.Derosa G, Maffioli P, Cicero AF. Berberine on metabolic and cardiovascular risk factors: an analysis from preclinical evidences to clinical trials. Expert Opin Biol Ther. 2012;12(8):1113–24. doi: 10.1517/14712598.2012.704014. [DOI] [PubMed] [Google Scholar]
- 29.Langsjoen PH, Langsjoen AM. Overview of the use of CoQ10 in cardiovascular disease. BioFactors. 1999;9(2–4):273–84. doi: 10.1002/biof.5520090224. [DOI] [PubMed] [Google Scholar]
- 30.Cicero AFG, Fogacci F, Colletti A. Commentary to: “The Effects of Coenzyme Q10 Supplementation on Blood Pressures Among Patients with Metabolic Diseases: A Systematic Review and Meta-analysis of Randomized Controlled Trials". High Blood Press Cardiovasc Prev. 2018;25(1):51–2. doi: 10.1007/s40292-018-0248-1. [DOI] [PubMed] [Google Scholar]
- 31.Cicero AF, Colletti A, Fogacci F, Bove M, Rosticci M, Borghi C. Effects of a combined nutraceutical on lipid pattern, glucose metabolism and inflammatory parameters in moderately hypercholesterolemic subjects: a double-blind, cross-over, randomized clinical trial. High Blood Press Cardiovasc Prev. 2017;24(1):13–18. doi: 10.1007/s40292-016-0163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tabrizi R, Akbari M, Sharifi N, Lankarani KB, Moosazadeh M, Kolahdooz F, Taghizadeh M, Asemi Z. The Effects of Coenzyme Q10 Supplementation on blood pressures among patients with metabolic diseases: a systematic review and meta-analysis of randomized controlled trials. High Blood Press Cardiovasc Prev. 2018;25(1):41–50. doi: 10.1007/s40292-018-0247-2. [DOI] [PubMed] [Google Scholar]
- 33.Sharifi N, Tabrizi R, Moosazadeh M, Mirhosseini N, Lankarani KB, Akbari M, Chamani M, Kolahdooz F, Asemi Z. The effects of coenzyme Q10 supplementation on lipid profiles among patients with metabolic diseases: a systematic review and meta-analysis of randomized controlled trials. Curr Pharm Des. 2018;24(23):2729–42. doi: 10.2174/1381612824666180406104516. [DOI] [PubMed] [Google Scholar]
- 34.Jorat MV, Tabrizi R, Mirhosseini N, Lankarani KB, Akbari M, Heydari ST, Mottaghi R, Asemi Z. The effects of coenzyme Q10 supplementation on lipid profiles among patients with coronary artery disease: a systematic review and meta-analysis of randomized controlled trials. Lipids Health Dis. 2018;17(1):230. doi: 10.1186/s12944-018-0876-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sahebkar A, Simental-Mendía LE, Stefanutti C, Pirro M. Supplementation with coenzyme Q10 reduces plasma lipoprotein(a) concentrations but not other lipid indices: a systematic review and meta-analysis. Pharmacol Res. 2016;105:198–209. doi: 10.1016/j.phrs.2016.01.030. [DOI] [PubMed] [Google Scholar]
- 36.Ankola DD, Viswanad B, Bhardwaj V, Ramarao P, Kumar MN. Development of potent oral nanoparticulate formulation of coenzyme Q10 for treatment of hypertension: can the simple nutritional supplements be used as first line therapeutic agents for prophylaxis/therapy? Eur J Pharm Biopharm. 2007;67(2):361–9. doi: 10.1016/j.ejpb.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 37.Way TD, Lin HY, Kuo DH, Tsai SJ, Shieh JC, Wu JC, Lee MR, Lin JK. Pu-erh tea attenuates hyperlipogenesis and induces hepatoma cells growth arrest through activating AMP-activated protein kinase (AMPK) in human HepG2 cells. J Agric Food Chem. 2009;57(12):5257–64. doi: 10.1021/jf900730e. [DOI] [PubMed] [Google Scholar]
- 38.Shishikura Y, Khokhar S, Murray BS. Effects of tea polyphenols on emulsification of olive oil in a small intestine model system. J Agric Food Chem. 2006;54(5):1906–13. doi: 10.1021/jf051988p. [DOI] [PubMed] [Google Scholar]
- 39.Liu W, Wan C, Huang Y, Li M. Effects of tea consumption on metabolic syndrome: a systematic review and meta-analysis of randomized clinical trials. Phytother Res. 2020;34(11):2857–66. doi: 10.1002/ptr.6731. [DOI] [PubMed] [Google Scholar]
- 40.Park CS, Kim W, Woo JS, Ha SJ, Kang WY, Hwang SH, Park YW, Kim YS, Ahn YK, Jeong MH, Kim W. Green tea consumption improves endothelial function but not circulating endothelial progenitor cells in patients with chronic renal failure. Int J Cardiol. 2010;145(2):261–262. doi: 10.1016/j.ijcard.2009.09.471. [DOI] [PubMed] [Google Scholar]
- 41.Lin QF, Qiu CS, Wang SL, Huang LF, Chen ZY, Chen Y, Chen G. A cross-sectional study of the relationship between habitual tea consumption and arterial stiffness. J Am Coll Nutr. 2016;35(4):354–61. doi: 10.1080/07315724.2015.1058197. [DOI] [PubMed] [Google Scholar]
- 42.Zhang C, Qin YY, Wei X, Yu FF, Zhou YH, He J. Tea consumption and risk of cardiovascular outcomes and total mortality: a systematic review and meta-analysis of prospective observational studies. Eur J Epidemiol. 2015;30(2):103–13. doi: 10.1007/s10654-014-9960-x. [DOI] [PubMed] [Google Scholar]
- 43.Ried K, Sullivan TR, Fakler P, Frank OR, Stocks NP. Effect of cocoa on blood pressure. Cochrane Database Syst Rev. 2012;8:CD008893. doi: 10.1002/14651858.CD008893.pub2. [DOI] [PubMed] [Google Scholar]
- 44.Darand M, Hajizadeh Oghaz M, Hadi A, Atefi M, Amani R. The effect of cocoa/dark chocolate consumption on lipid profile, glycemia, and blood pressure in diabetic patients: a meta-analysis of observational studies. Phytother Res. 2021;35(10):5487–501. doi: 10.1002/ptr.7183. [DOI] [PubMed] [Google Scholar]
- 45.Grassi D, Desideri G, Necozione S, Lippi C, Casale R, Properzi G, Blumberg JB, Ferri C. Blood pressure is reduced and insulin sensitivity increased in glucose-intolerant, hypertensive subjects after 15 days of consuming high-polyphenol dark chocolate. J Nutr. 2008;138(9):1671–6. doi: 10.1093/jn/138.9.1671. [DOI] [PubMed] [Google Scholar]
- 46.Grassi D, Desideri G, Necozione S, Ruggieri F, Blumberg JB, Stornello M, Ferri C. Protective effects of flavanol-rich dark chocolate on endothelial function and wave reflection during acute hyperglycemia. Hypertension. 2012;60(3):827–32. doi: 10.1161/HYPERTENSIONAHA.112.193995. [DOI] [PubMed] [Google Scholar]
- 47.http://www.brighamandwomens.org/About_BWH/publicaffairs/news/publications/DisplayBulletin.aspx?issueDate=3/28/2014%2012:00:00%20AM. Access 31 Jan 2021.
- 48.Butt MS, Sultan MT, Butt MS, Iqbal J. Garlic: nature’s protection against physiological threats. Crit Rev Food Sci Nutr. 2009;49(6):538–51. doi: 10.1080/10408390802145344. [DOI] [PubMed] [Google Scholar]
- 49.Ried K. Garlic lowers blood pressure in hypertensive subjects, improves arterial stiffness and gut microbiota: a review and meta-analysis. Exp Ther Med. 2020;19(2):1472–8. doi: 10.3892/etm.2019.8374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ried K, Toben C, Fakler P. Effect of garlic on serum lipids: an updated meta-analysis. Nutr Rev. 2013;71(5):282–99. doi: 10.1111/nure.12012. [DOI] [PubMed] [Google Scholar]
- 51.Steiner M, Lin RS. Changes in platelet function and susceptibility of lipoproteins to oxidation associated with administration of aged garlic extract. J Cardiovasc Pharmacol. 1998;31(6):904–8. doi: 10.1097/00005344-199806000-00014. [DOI] [PubMed] [Google Scholar]
- 52.Ried K. Garlic lowers blood pressure in hypertensive individuals, regulates serum cholesterol, and stimulates immunity: an updated meta-analysis and review. J Nutr. 2016;146(2):389S–396S. doi: 10.3945/jn.114.202192. [DOI] [PubMed] [Google Scholar]
- 53.Kheirmandparizi M, Keshavarz P, Nowrouzi-Sohrabi P, Hosseini-Bensenjan M, Rezaei S, Kashani SMA, Zeidi N, Tabrizi R, Alkamel A. Effects of garlic extract on lipid profile in patients with coronary artery disease: a systematic review and meta-analysis of randomised clinical trials. Int J Clin Pract. 2021;75(12):e14974. doi: 10.1111/ijcp.14974. [DOI] [PubMed] [Google Scholar]
- 54.Egan BM, Li J, Qanungo S, Wolfman TE. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients: national health and nutrition examination surveys 1988–2010. Circulation. 2013;128(1):29–41. doi: 10.1161/CIRCULATIONAHA.112.000500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leren P, Eide I, Foss OP, Helgeland A, Hjermann I, Holme I, Kjeldsen SE, Lund-Larsen PG. Antihypertensive drugs and blood lipids: the Oslo study. Br J Clin Pharmacol. 1982;13(Suppl 2):441S–444S. doi: 10.1111/j.1365-2125.1982.tb01954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kasiske BL, Ma JZ, Kalil RS, Louis TA. Effects of antihypertensive therapy on serum lipids. Ann Intern Med. 1995;15(2):133–41. doi: 10.7326/0003-4819-122-2-199501150-00010. [DOI] [PubMed] [Google Scholar]
- 57.Ames R. Effects of diuretic drugs on the lipid profile. Drugs. 1988;36(Suppl 2):33–40. doi: 10.2165/00003495-198800362-00007. [DOI] [PubMed] [Google Scholar]
- 58.Ames RP. Antihypertensive drugs and lipid profiles. Am J Hypertens. 1988;1(4 Pt 1):421–7. doi: 10.1093/ajh/1.4.421. [DOI] [PubMed] [Google Scholar]
- 59.Maitland-van der Zee AH, Klungel OH, Kloosterman JM, Seidell JC, Leufkens HG, de Boer A. The association between antihypertensive drug therapies and plasma lipid levels in the general population. J Hum Hypertens. 2001;15(10):701–5. doi: 10.1038/sj.jhh.1001197. [DOI] [PubMed] [Google Scholar]
- 60.Strazzullo P, Kerry SM, Barbato A, Versiero M, D’Elia L, Cappuccio FP. Do statins reduce blood pressure?: a meta-analysis of randomized, controlled trials. Hypertension. 2007;49(4):792–8. doi: 10.1161/01.HYP.0000259737.43916.42. [DOI] [PubMed] [Google Scholar]
- 61.Cicero AFG, Fogacci F, Hernandez AV, Banach M, Lipid, Blood Pressure Meta-Analysis Collaboration (LBPMC) Group and the International Lipid Expert Panel (ILEP) Efficacy and safety of bempedoic acid for the treatment of hypercholesterolemia: A systematic review and meta-analysis. PLoS Med. 2020;17(7):e1003121. doi: 10.1371/journal.pmed.1003121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Correa V, Jr, Gus M, Fuchs FD. Does the blood pressure-lowering effect of statins contribute to their beneficial cardiovascular effects? Expert Rev Cardiovasc Ther. 2010;8(6):775–9. doi: 10.1586/erc.10.59. [DOI] [PubMed] [Google Scholar]
- 63.Schmidt AF, Carter JL, Pearce LS, Wilkins JT, Overington JP, Hingorani AD, Casas JP. PCSK9 monoclonal antibodies for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2020;10(10):CD011748. doi: 10.1002/14651858.CD011748.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Borghi C, Dormi A, Veronesi M, Sangiorgi Z, Gaddi A, Brisighella Heart Study Working Party Association between different lipid-lowering treatment strategies and blood pressure control in the Brisighella Heart Study. Am Heart J. 2004;148(2):285–92. doi: 10.1016/j.ahj.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 65.Golomb BA, Dimsdale JE, White HL, Ritchie JB, Criqui MH. Reduction in blood pressure with statins: results from the UCSD Statin Study, a randomized trial. Arch Intern Med. 2008;168(7):721–7. doi: 10.1001/archinte.168.7.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Briasoulis A, Agarwal V, Valachis A, Messerli FH. Antihypertensive effects of statins: a meta-analysis of prospective controlled studies. J Clin Hypertens. 2013;15(5):310–20. doi: 10.1111/jch.12081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sun W, Lee TS, Zhu M, Gu C, Wang Y, Zhu Y, Shyy JY. Statins activate AMP-activated protein kinase in vitro and in vivo. Circulation. 2006;114(24):2655–62. doi: 10.1161/CIRCULATIONAHA.106.630194. [DOI] [PubMed] [Google Scholar]
- 68.Laufs U, Liao JK. Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by Rho GTPase. J Biol Chem. 1998;273:24266–71. doi: 10.1074/jbc.273.37.24266. [DOI] [PubMed] [Google Scholar]
- 69.Antoniades C, Bakogiannis C, Leeson P, Guzik TJ, Zhang MH, Tousoulis D, Antonopoulos AS, Demosthenous M, Marinou K, Hale A, Paschalis A, Psarros C, Triantafyllou C, Bendall J, Casadei B, Stefanadis C, Channon KM. Rapid, direct effects of statin treatment on arterial redox state and nitric oxide bioavailability in human atherosclerosis via tetrahydrobiopterin-mediated endothelial nitric oxide synthase coupling. Circulation. 2011;124(3):335–45. doi: 10.1161/CIRCULATIONAHA.110.985150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Borghi C, Urso R, Cicero AF. Renin-angiotensin system at the crossroad of hypertension and hypercholesterolemia. Nutr Metab Cardiovasc Dis. 2017;27(2):115–20. doi: 10.1016/j.numecd.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 71.Lee S, Yang S, Chang MJ. Antihypertensive effects of rosuvastatin in patients with hypertension and dyslipidemia: a systemic review and meta-analysis of randomized studies. PLoS One. 2021;16(11):e0260391. doi: 10.1371/journal.pone.0260391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.You T, Liu XG, Hou XD, Wang XK, Xie HH, Ding F, Yi K, Zhang P, Xie XD. Effect of statins on blood pressure: analysis on adverse events released by FDA. Clin Exp Hypertens. 2017;39(4):325–9. doi: 10.1080/10641963.2016.1254224. [DOI] [PubMed] [Google Scholar]
- 73.Cicero AF, Ertek S, Borghi C. Omega-3 polyunsaturated fatty acids: their potential role in blood pressure prevention and management. Curr Vasc Pharmacol. 2009;7(3):330–7. doi: 10.2174/157016109788340659. [DOI] [PubMed] [Google Scholar]
- 74.Bønaa KH, Bjerve KS, Straume B, Gram IT, Thelle D. Effect of eicosapentaenoic and docosahexaenoic acids on blood pressure in hypertension. A population-based intervention trial from the Tromsø study. N Engl J Med. 1990;22(12):795–801. doi: 10.1056/NEJM199003223221202. [DOI] [PubMed] [Google Scholar]
- 75.Liu JC, Conklin SM, Manuck SB, Yao JK, Muldoon MF. Long-chain omega-3 fatty acids and blood pressure. Am J Hypertens. 2011;24(10):1121–6. doi: 10.1038/ajh.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Park Y, Oh SH, Rhee MY. Association between 24-hour ambulatory blood pressure and erythrocyte n-3 polyunsaturated fatty acids in Korean subjects with hypertension. Nutr Res. 2010;30(12):807–14. doi: 10.1016/j.nutres.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 77.Russo C, Olivieri O, Girelli D, Azzini M, Stanzial AM, Guarini P, Friso S, De Franceschi L, Corrocher R. Omega-3 polyunsaturated fatty acid supplements and ambulatory blood pressure monitoring parameters in patients with mild essential hypertension. J Hypertens. 1995;13(12 Pt 2):1823–6. [PubMed] [Google Scholar]
- 78.Appel LJ, Miller ER, 3rd, Seidler AJ, Whelton PK. Does supplementation of diet with ‘fish oil’ reduce blood pressure? A meta-analysis of controlled clinical trials. Arch Intern Med. 1993;28(12):1429–38. doi: 10.1001/archinte.1993.00410120017003. [DOI] [PubMed] [Google Scholar]
- 79.Morris MC, Sacks F, Rosner B. Does fish oil lower blood pressure? A meta-analysis of controlled trials. Circulation. 1993;88(2):523–33. doi: 10.1161/01.cir.88.2.523. [DOI] [PubMed] [Google Scholar]
- 80.Geleijnse JM, Giltay EJ, Grobbee DE, Donders AR, Kok FJ. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. J Hypertens. 2002;20(8):1493–9. doi: 10.1097/00004872-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 81.Campbell F, Dickinson HO, Critchley JA, Ford GA, Bradburn M. A systematic review of fish-oil supplements for the prevention and treatment of hypertension. Eur J Prev Cardiol. 2013;20(1):107–20. doi: 10.1177/2047487312437056. [DOI] [PubMed] [Google Scholar]
- 82.Miller PE, Van Elswyk M, Alexander DD. Long-chain omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid and blood pressure: a meta-analysis of randomized controlled trials. Am J Hypertens. 2014;27(7):885–96. doi: 10.1093/ajh/hpu024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Leslie KH, McCowan C, Pell JP. Adherence to cardiovascular medication: a review of systematic reviews. J Public Health (Oxf). 2019;41(1):e84–e94. doi: 10.1093/pubmed/fdy088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Simon A, Dézsi CA. Treatment of hypertensive and hypercholesterolaemic patients with the triple fixed combination of atorvastatin, perindopril and amlodipine: the results of the CORAL Study. Adv Ther. 2019;36(8):2010–20. doi: 10.1007/s12325-019-01002-8. [DOI] [PubMed] [Google Scholar]
- 85.Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O’Brien E, Ostergren J, ASCOT investigators Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361(9364):1149–58. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 86.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT) JAMA. 2002;288:2998–3007. doi: 10.1001/jama.288.23.2998. [DOI] [PubMed] [Google Scholar]
- 87.Messerli FH, Pinto L, Tang SS, Thakker KM, Cappelleri JC, Sichrovsky T, Dubois RW. Impact of systemic hypertension on the cardiovascular benefits of statin therapy–a meta-analysis. Am J Cardiol. 2008;101(3):319–25. doi: 10.1016/j.amjcard.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 88.Williams RR, Hunt SC, Hopkins PN, Stults BM, Wu LL, Hasstedt SJ, Barlow GK, Stephenson SH, Lalouel JM, Kuida H. Familial dyslipidemic hypertension. Evidence from 58 Utah families for a syndrome present in approximately 12% of patients with essential hypertension. JAMA. 1988;259(24):3579–86. doi: 10.1001/jama.259.24.3579. [DOI] [PubMed] [Google Scholar]