Abstract
Purpose:
An effective response for a mass-casualty incident requires understanding the relevant basic science and physical impact; detailed preparedness among jurisdictions; and clear, sequential response planning, including formal operational exercises, logistics, interagency, and public-private coordination, rapid activation of resilience, and continual improvement from lessons learned and new knowledge. This ConRad 2021 meeting report describes steps for civilian medical and public health response planning for a nuclear detonation; the utility of this type of planning for broader application; and extension of this planning to the international community.
Conclusion:
A nuclear detonation requires a response within minutes to what will be a large-scale disaster complicated by radiation, including some elements that are similar to a broad range of incidents. The response could be further complicated if multiple incidents occur simultaneously. Required are detailed planning, preparedness and scripting for an immediate operational response, addressing clinical manifestations of evolving radiation illness, and flexibility to adapt to a rapidly changing situation. This need translates into the use of just-in-time information; effective, credible communication; situational awareness on a global scale; and a template upon which to apply capabilities in a multi-sector response. This effort is greatly facilitated using a ‘playbook’ approach, the basics of which are presented.
Keywords: Response, disaster response, mass-casualty, nuclear detonation, radiation accident, emergency playbook
Introduction
Following the terrorist attacks of 11 September 2001, the United States formalized disaster response planning based on 15 National Planning Scenarios (FEMA 2021), including #1 – an improvised nuclear device detonation and #11 – a radiological dispersal device. For nuclear detonation-related civilian preparedness, this planning represented a substantial new effort, given the limited activity following the end of the Cold War and the new emerging threat from terrorism. To foster public health and medical response to nuclear terrorism, as opposed to state-sponsored nuclear war, investments were made in understanding the physical consequences of detonations; modeling the types and numbers of injuries that would result (Knebel et al. 2011); developing diagnostics for assessing individual radiation dose from exposure (e.g. radiation biodosimetry); and identifying, testing, and acquiring potential medical countermeasures to mitigate/treat radiation exposure. These activities required organizing detailed, complex information into a coherent strategy and then applying a granular approach to planning, preparedness, and operational response. Much public health and medical information about nuclear detonation incidents have been made publicly available, both in peer-reviewed scientific journals and in US government publications. This ready availability not only informs the public but also constitutes a credible, accessible body of knowledge with which to address the threat from a nuclear and/or radiation-related disaster.
This report provides details of a presentation at ConRad 2021, regarding the next steps for civilian medical and public health planning, preparedness, and operational response for a nuclear detonation; the utility of this type of planning for broader application; and extension of this planning to collaboration across the international community.
A number of key publications and tools are now available that provide relevant information for leaders, planners, response managers, and responders, including, but not limited to, the following items: (1) Planning guidance for response to a nuclear detonation (EOP 2010; update in progress); (2) the continuously updated, ASPR-produced, Radiation emergency medical management (REMM) website (DHHS 2021a); (3) A decision-makers guide: medical planning and response for a nuclear detonation (ASPR 2017); and (4) Public health and medical preparedness for a nuclear detonation: the nuclear incident medical enterprise (Coleman et al. 2015). In addition, concepts are under development to advance the science behind medical countermeasures needed to respond effectively to chemical, biological, radiological, nuclear, and explosive (CBRNE) incidents and to the identification of C, B, R, N, E medical operations science support expert(s) (CMOSSE) (Coleman et al. 2019).
The complex preparedness and response planning for a nuclear detonation involves many government/jurisdictional (federal, regional, state, tribal, territorial, local) and private (e.g. American Red Cross) entities that will need to cooperate to apply their capabilities to respond to this type of scenario. A project on nuclear preparedness and allocation of scarce resources (DHHS 2021b; Coleman et al. 2011) highlighted important actions for public-private partnerships and collaboration among a broad range of participants. Likewise, taking international considerations into account is also important. Communication strategies for all audiences along all points of the response timeline are key to a successful response.
Planning for response to a nuclear detonation incorporates the following key concepts: (1) the best available science and technical underpinnings are used and continuously updated; (2) a nuclear detonation scenario is a complex system in which changing one parameter, requirement, or capability can have broad implications across many sectors, regions, and countries (Coleman et al. 2009; Coleman and Lurie 2012); and (3) subject matter experts in various fields assess many complexities and produce practical tools and useful documents to address the question, ‘What do I do?!’, as it applies to all levels of participants in preparedness and response. These experts include planners, government leaders, medical care providers, public health officials, and first responders.
Current project
Murrain-Hill et al. (2011) described the need for playbooks for providing medical response capabilities in response to a nuclear detonation. The approach includes a detailed time- and functional area-based playbook template for state and local responders that parallels the playbooks used by federal partners, enabling responders at all levels to literally be on the same page and line. The entire State and Local Planners Playbook is publicly available (ASPR 2011).
These and other preparedness activities are fundamental to a successful response. For example, the benefit of detailed preparedness activities was experienced by the subject matter experts in Japan involved in response to the Fukushima nuclear power plant crisis (see Simon et al. 2012). Now, with the proposed update of the planning guidance for response to a nuclear detonation (EOP 2010), the changing face of global nuclear capabilities including nuclear-capable nations, and the experience with COVID-19 demonstrate the need for advanced planning and global collaboration before and during a large-scale disaster, a major effort is in progress to develop a playbook, similar to that referenced above (Murrain-Hill et al. 2011; ASPR 2011), for public health and medical preparedness collaboration among members of the Global Health Security Initiative (GHSI). GHSI is an informal, international partnership of Canada, the European Commission, France, Germany, Italy, Japan, Mexico, the United Kingdom, and the United States, with the World Health Organization and International Atomic Energy Agency serving as technical advisors, to strengthen public health preparedness and response globally to threats of chemical, biological, radiological, and nuclear (CBRN) terrorism, as well as pandemic influenza (GHSI 2021).
Experience from the last two decades of disaster preparedness and response has highlighted the need for subject-matter experts to be essential members of operational response. This led a group of subject-matter experts, including authors of this report, to propose a new competency: chemical, biological, radiological, nuclear, and explosive (CBRNE) medical operations science support expert(s) (CMOSSE) (Coleman et al. 2019). The updated playbook considerations described in the present article provide a potential opportunity to foster implementing this CMOSSE concept.
Science as a basis for planning, preparedness, response, and recovery
Figure 1 is a general schema as to when particular phases of emergency management – preparedness, response, and recovery – may be active, along with associated activities. Scientific guidance should be applied throughout and updated based on emerging knowledge and experience, as was done during the COVID-19 response. Preparedness should begin well before an incident, with ongoing planning remaining a critical component of the response as situational awareness evolves. While the response has its dominant role immediately after an incident (or possibly before, if some advanced warning occurs), recovery should begin early. A great number of incident-related, albeit indirect, casualties can occur nationwide, including far from the epicenter, as resources are directed toward the disaster and routine healthcare elsewhere thereby is delayed. The statuses of three cross-cutting capabilities, among other factors, influence every stage of the emergency from preparedness to recovery: (1) operational coordination, including consideration of operational capacity; (2) situational awareness, based on information management and knowledge sharing; and (3) resilience, lessons learned, and shared experience with other incidents, including formal projects with disaster science. The better that these coalesce, the more effective the response.
Figure 1.
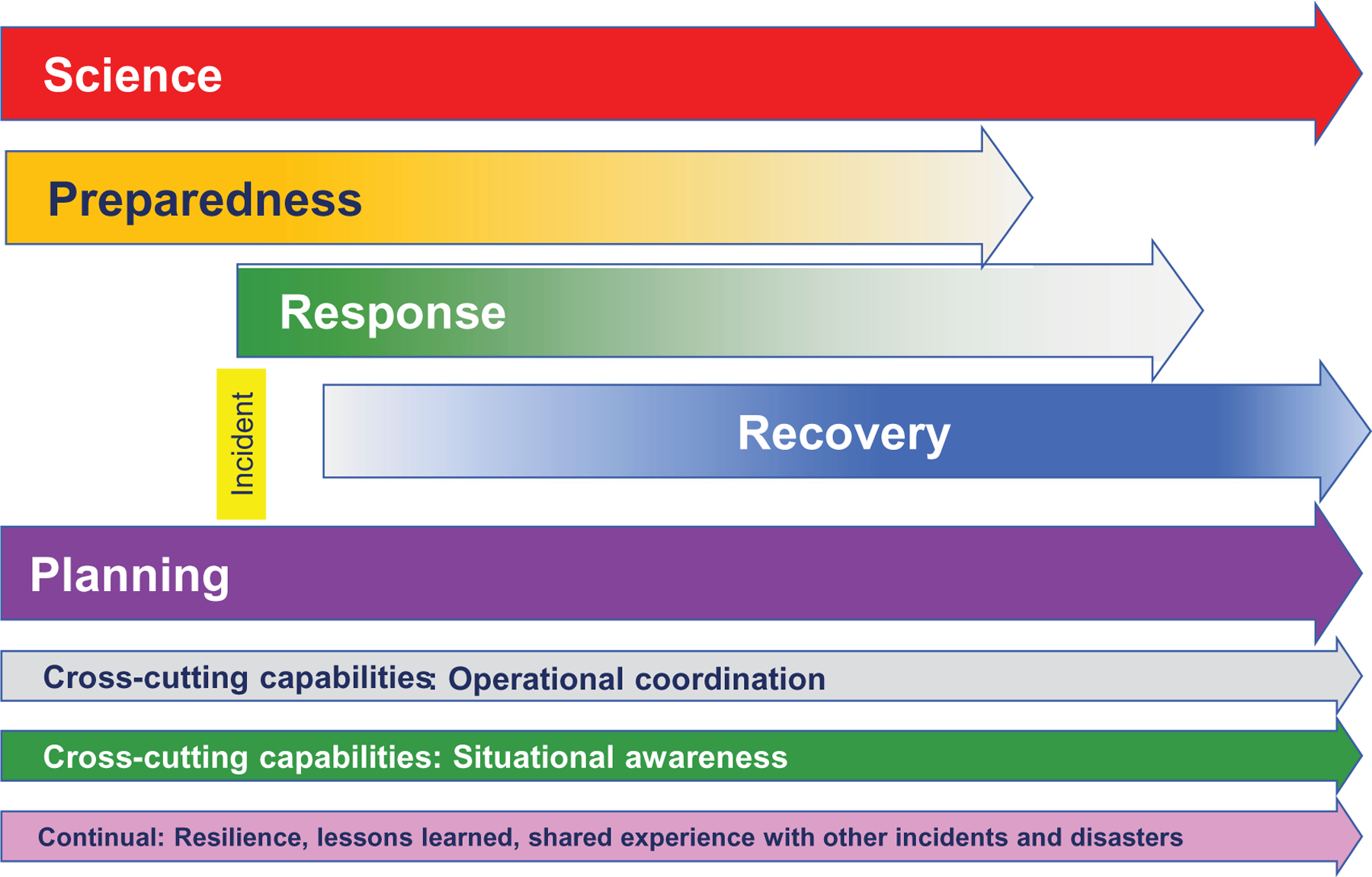
Operational phases and need for science expertise, planning, and cross-cutting capabilities relative to the incident.
In all cases, the acute phase of a disaster ends, but the impact lingers, often for a long time. Therefore, recovery requires extensive preparedness as well. Lessons observed and learned from exercises and actual disasters are keys to ongoing improvement in preparedness, response, and recovery, as is the new knowledge that comes from disaster science that derives from information across the emergency response field.
Essential information for preparedness, response, and recovery
Playbooks, as detailed above, can serve as important guides to key planning, preparedness, and operational response activities, particularly with respect to public health and medical response activities that can save lives and mitigate negative health consequences. They should be available in both an electronic version and printed versions in case access to electronics is unavailable. Because a no-notice nuclear incident will require a rapid, immediate review of background information, succinct sections are included after the detailed time phases and steps. Table 1 identifies proposed topics for essential information. Table 2 identifies some key references.
Table 1.
Proposed topics for essential information.
| 1 | Scenarios and concept of operations (CONOPs) |
| 2 | Science, technology, and diagnostics |
| 3 | Medical countermeasures |
| 4 | Triage and evacuation |
| 5 | Crisis standards of care |
| 6 | International collaboration potential |
| 7 | Psychosocial support |
| 8 | Fatality management |
| 9 | Recovery |
| 10 | Definition/ certification of expertise (CMOSSE) |
| 11 | Time periods and action steps |
Table 2.
Key references.
Planning and response guides
|
System elements
|
Knowledge library
|
Time periods and steps
A nuclear detonation results in complex and evolving response requirements in time periods early after the detonation, given that the physical environment changes so rapidly. Figure 2 indicates four time periods, from before an incident to post-detonation, recognizing that the impact will last beyond 72 h. Tools, such as playbooks and models, may help quantify potential needs and address the inevitable scarce resources situation. Needs and response capabilities will likely vary dramatically based on distance from the epicenter and based on city- or region-specific resource and transportation considerations. Operations within the blast site and surrounding region will be disrupted for months to years, and planning and recovery will be ongoing.
Figure 2.
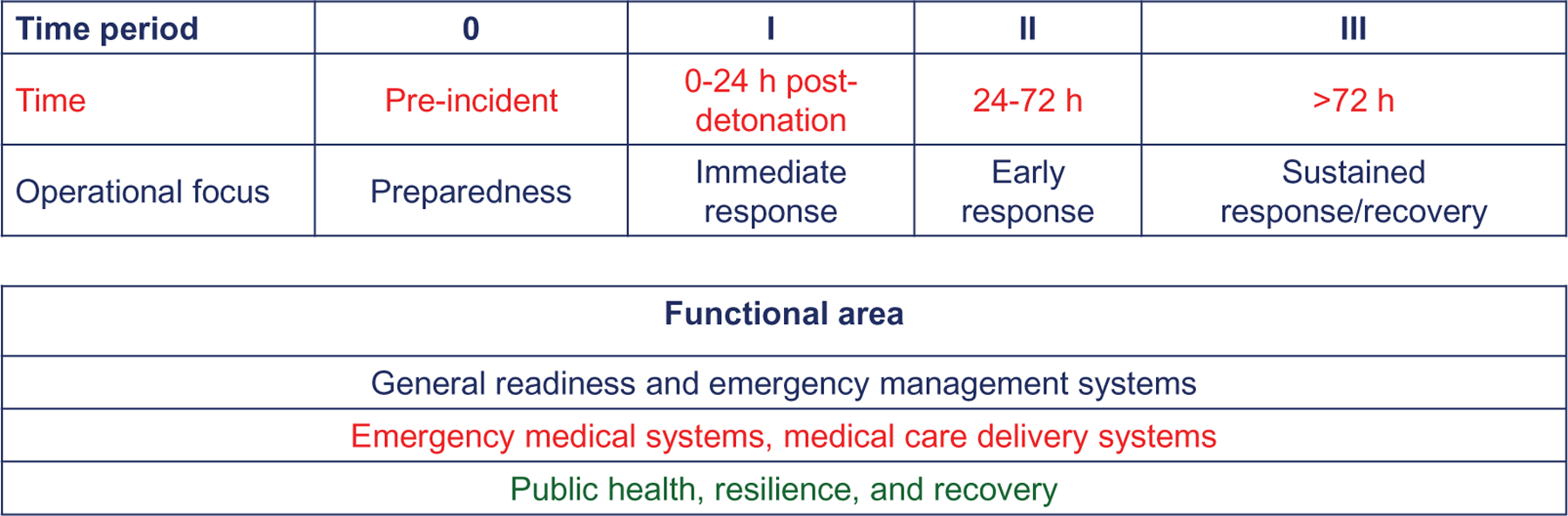
Time periods and functional areas. *The time periods as listed here can be considered to correspond to FEMA phases (FEMA 2016): phase 1 (pre-incident), phase 2a (immediate response), phase 2b (deployment), and phases 2c/3 (sustained response/recovery).
To guide preparedness, response, and recovery, detailed steps need to be developed and described. For example, steps may be organized by functional areas; each time period should have detailed steps for each of the three functional areas in Figure 2: general readiness and emergency management systems; emergency medical systems, medical care delivery systems; public health and resilience. The four time periods and three functional areas create a 4 × 3 matrix, recognizing that functions go across all the time periods. To facilitate subject-matter experts finding steps critical to their areas, the steps are being grouped and indexed by type of action: (1) educate, (2) prepare, (3) inform (situational awareness), (4) activate, and (5) communicate.
Conclusions
Activities promoting effective preparedness, response, and recovery are needed. In addition, preparing for a nuclear detonation has a more general positive impact, not only for preparedness, response, and recovery but for health care and public health in general. For example, advances in burn care products spurred by investments for enhancing disaster preparedness are applicable to general burn care, including products supported by the Biomedical Advanced Research and Development Authority (e.g. FDA 2021). Scientific research into medical countermeasures and biodosimetry is producing knowledge applicable to cancer care (Weinstock et al. 2008). Subject-matter experts in oncology with bone marrow transplantation expertise have created the Radiation Injury Treatment Network (RITN 2021) to assist with treatment for severe acute radiation syndrome after radiation disasters. Similar types of networks have been formed by professional entities, such as the Health Physics Society (HPS 2021) and other organizations, including the National Council for Radiation Protection and Measurements (NCRP 2021), and the American Burn Association (ABA 2021). A capability that is mobilized rapidly to address a substantial, multi-sector public and private response enhances preparedness for other potential large-scale disasters, such as earthquakes or fires and requires much of the solution of the complex system described as the nuclear incident medical enterprise (NIME) (Coleman et al. 2015). Although some large-scale incidents such as pandemics evolve much more slowly, the planning and management of resources and personnel have many components in common with those for a nuclear detonation.
The specifics and density of information within playbooks will vary with country and jurisdiction, but a scripted common template upon which to prepare, plan, exercise, and execute coordinated operations will enable and enhance the capabilities of varied partners to assist and learn from one another. The current projects under consideration include piloting a version of the public playbook (ASPR 2011; Murrain-Hill et al. 2011) and exploring potential capabilities for enhancing responses to mass-casualty incidents.
Acknowledgments
The authors acknowledge that many additional participants are and will be involved in this overall project, too numerous to include in this meeting-related report.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
Notes on contributors
C. Norman Coleman, MD, is Associate Director of the Radiation Research Program, National Cancer Institute; Senior Medical Advisor in the Office of the Assistant Secretary for Preparedness and Response; and a co-chair of the Radiological-Nuclear Threats Working Group of the Global Health Security Initiative.
Kenneth D. Cliffer, PhD, is a Senior Program Analyst in the Planning Division of the Office of Strategy, Policy, Planning, and Requirements, the Office of Incident Command and Control, the Office of the Assistant Secretary of Preparedness and Response, Office of the Secretary, the U.S. Department of Health and Human Services, Washington, DC.
Andrea L. DiCarlo, PhD, is the Director of the Radiation and Nuclear Countermeasures Program, Division of Allergy, Immunology, and Transplantation, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, MD.
Mary J. Homer, PhD, is the Chief of the Radiological and Nuclear Countermeasures program, Division of Chemical, Biological, Radiological, and Nuclear Countermeasures, Biomedical Advanced Research and Development Authority (BARDA), Office of the Assistant Secretary of Preparedness and Response, Office of the Secretary, the U.S. Department of Health and Human Services, Washington, DC.
Brian R. Moyer, MS, CNMT, is a Senior Science Advisor for the Radiological and Nuclear Countermeasures program, Division of Chemical, Biological, Radiological, and Nuclear Countermeasures, Biomedical Advanced Research and Development Authority (BARDA), Office of the Assistant Secretary of Preparedness and Response, Office of the Secretary, the U.S. Department of Health and Human Services, Washington, DC.
Shannon G. Loelius, PhD, is a Biologist in the Radiological and Nuclear Countermeasures program, Division of Chemical, Biological, Radiological, and Nuclear Countermeasures, Biomedical Advanced Research and Development Authority (BARDA), Office of the Assistant Secretary of Preparedness and Response, Office of the Secretary, the U.S. Department of Health and Human Services, Washington, DC.
Adam W. Tewell is an Emergency Management Specialist supporting international health operations in the Office of Emergency Management and Medical Operations, Office of the Assistant Secretary of Preparedness and Response, Office of the Secretary, the U.S. Department of Health and Human Services, Washington, DC., and serves in the Executive Secretariat of the Radiological-Nuclear Threats Working Group of the Global Health Security Initiative.
Judith L. Bader, MD, has been a contractor supporting the Radiological and Nuclear Countermeasures program, Division of Chemical, Biological, Radiological, and Nuclear Countermeasures, Biomedical Advanced Research and Development Authority (BARDA), Office of the Assistant Secretary of Preparedness and Response, Office of the Secretary, the U.S. Department of Health and Human Services, Washington, DC. She has served as the managing editor of the ASPR-sponsored web site REMM (DHHS 2021a).
John F. Koerner, MPH, CIH, is a Senior Program Analyst in the Planning Division of the Office of Strategy, Policy, Planning, and Requirements, the Office of Incident Command and Control, the Office of the Assistant Secretary of Preparedness and Response, Office of the Secretary, the U.S. Department of Health and Human Services, Washington, DC.
Footnotes
Disclosure statement
This communication is an extended description of a presentation by Dr. Coleman at the Conference on Radiation Topics (ConRad) 2021 meeting held virtually in Munich, Germany, 10–12 May 2021. The content represents the personal opinions of the authors and is not the opinion or policy of their institutions, including the Office of the Assistant Secretary for Preparedness and Response, the National Cancer Institute, the National Institute of Allergy and Infectious Diseases, and the Department of Health and Human Services. The authors report no conflicts of interest.
References
- ABA. 2021. Disaster response. Chicago (IL): American Burn Association; [accessed 2021 Jul 1]. https://ameriburn.org/quality-care/disaster-response/. [Google Scholar]
- ASPR. 2011. Public health emergency: state and local planners playbook for medical response to a nuclear detonation. Washington (DC): Assistant Secretary for Preparedness and Response; [accessed 2021 Oct 18]. https://www.phe.gov/Preparedness/planning/playbooks/stateandlocal/nuclear/Documents/statelocalplaybook-v1.pdf. [Google Scholar]
- ASPR. 2017. A decision makers guide: medical planning and response for a nuclear detonation: second edition, November 2017. Washington (DC): Assistant Secretary for Preparedness and Response; [accessed 2021 Oct 18]. https://remm.hhs.gov/IND_Decision_Makers_Guide_2017_guides.pdf. [Google Scholar]
- Coleman CN, Bader JL, Koerner JF, Hrdina C, Cliffer KD, Hick JL, James JJ, Mansoura MK, Livinski AA, Nystrom SV, et al. 2019. Chemical, biological, radiological, nuclear, and explosive (CBRNE) science and the CBRNE science medical operations science support expert (CMOSSE). Disaster Med Public Health Prep. 13(5–6): 995–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman CN, Hrdina C, Bader JL, Norwood A, Hayhurst R, Forsha J, Yeskey K, Knebel A. 2009. Medical response to a radiologic/nuclear event: integrated plan from the Office of the Assistant Secretary for Preparedness and Response, Department of Health and Human Services. Ann Emerg Med. 53(2):213–222. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Knebel AR, Hick JL, Weinstock DM, Casagrande R, Caro JJ, DeRenzo EG, Dodgen D, Norwood AE, Sherman SE, et al. 2011. Scarce resources for nuclear detonation: project overview and challenges. Disaster Med Public Health Prep. 5(1):S13–S19. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Lurie N. 2012. Emergency medical preparedness for radiological/nuclear incidents in the United States. J Radiol Prot. 32(1):N27–N32. [DOI] [PubMed] [Google Scholar]
- Coleman CN, Sullivan JM, Bader JL, Murrain-Hill P, Koerner JF, Garrett AL, Weinstock DM, Case C Jr, Hrdina C, Adams SA. 2015. Public health and medical preparedness for a nuclear detonation: the nuclear incident medical enterprise. Health Phys. 108(2): 149–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DHHS. 2021a. Radiation emergency medical management: REMM. Washington (DC): Department of Health and Human Services; [accessed 2021 Oct 18]. https://remm.hhs.gov/index.html. [Google Scholar]
- DHHS. 2021b. Nuclear detonation scarce resources project working group publications. Washington (DC): Department of Health and Human Services; [accessed 2021 Oct 18]. https://remm.hhs.gov/triagetool_intro.htm. [Google Scholar]
- EOP. 2010. Planning guidance for response to a nuclear detonation: second edition, June 2010. Washington (DC): Executive Office of the President; [accessed 2021 Oct 18]. https://remm.hhs.gov/PlanningGuidanceNuclearDetonation.pdf. [Google Scholar]
- FDA. 2021. FDA approves StrataGraft for the treatment of adults with thermal burns. Silver Spring (MD): U.S. Food and Drug Administration; [accessed 2021 Jul 7]. https://www.fda.gov/news-events/press-announcements/fda-approves-stratagraft-treatment-adults-thermal-burns. [Google Scholar]
- FEMA. 2016. Response federal interagency operational plan: second edition: August 2016. Washington (DC): Federal Emergency Management Agency; [accessed 2021 Nov 3]. https://www.fema.gov/sites/default/files/documents/fema_response-fiop.pdf. [Google Scholar]
- FEMA. 2021. FEMA fact sheet: national planning scenarios. Washington (DC): Federal Emergency Management Agency; [accessed 2021 Jun 27]. https://www.hsdl.org/?view&did=683091. [Google Scholar]
- GHSI. 2021. Ottawa (Canada): Global Health Security Initiative; [accessed 2021 Jun 27]. http://ghsi.ca/.
- HPS. 2021. HPS: specialists in radiation protection. McLean (VA): Health Physics Society; [accessed 2021 Jun 27]. https://hps.org/ [Google Scholar]
- Knebel AR, Coleman CN, Cliffer KD, Murrain-Hill P, McNally R, Oancea V, Jacobs J, Buddemeier B, Hick JL, Weinstock DM, et al. 2011. Allocation of scarce resources after a nuclear detonation: setting the context. Disaster Med Public Health Prep. 5(S1):S20–S31. [DOI] [PubMed] [Google Scholar]
- Murrain-Hill P, Coleman CN, Hick JL, Redlener I, Weinstock DM, Koerner JF, Black D, Sanders M, Bader JL, Forsha J, et al. 2011. Medical response to a nuclear detonation: creating a playbook for state and local planners and responders. Disaster Med Public Health Prep. 5(S1):S89–S97. [DOI] [PubMed] [Google Scholar]
- NCRP. 2021. Bethesda (MD): National Council on Radiation Protection and Measurements; [accessed 2021 Jun 27]. https:ncrponline.org/.
- RITN. 2021. Radiation Injury Treatment Network; [accessed 2021 Jun 27]. https://ritn.net/.
- Simon SL, Coleman CN, Noska MA, Bowman T. 2012. Response of the U.S. Department of Health and Human Services in protecting civilian Americans in Japan during the Fukushima nuclear crisis. Health Phys. 102(5):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock DM, Case C Jr, Bader JL, Chao NJ, Coleman CN, Hatchett RJ, Weisdorf DJ, Confer DL. 2008. Radiologic and nuclear events: contingency planning for hematologists/oncologists. Blood. 111(12): 5440–5445. [DOI] [PMC free article] [PubMed] [Google Scholar]


