Abstract
Despite growing availability, HIV pre-exposure prophylaxis (PrEP) uptake and adherence remains suboptimal among female sex workers (FSW) in the United States. Using cross-sectional data from a survey of 236 street-based cisgender FSW in Baltimore, Maryland, we examined interest in event-driven and long-acting PrEP formulations. Latent class analysis identified discrete patterns of interest in five novel PrEP agents. Multinomial latent class regression then examined factors associated with probabilistic class membership. A three-class solution emerged as the best-fit latent class model: Injectable Acceptors (~ 24% of sample), Universal Acceptors (~ 18%), and Non-Acceptors (~ 58%). Compared to Non-Acceptors, Universal Acceptors had significantly (p < 0.05) higher odds of reporting condomless vaginal sex with clients, client condom coercion, and client-perpetrated physical violence. Relative to Non-Acceptors, Injectable Acceptors were distinguished by significantly higher rates of condomless vaginal sex with clients and injection drug use. Expanding PrEP options for FSW could help overcome barriers to PrEP initiation and persistence.
Keywords: HIV pre-exposure prophylaxis, Sex work, Injection drug use, Biomedical HIV prevention, United States
Introduction
Pre-exposure prophylaxis (PrEP) is an empowering biomedical HIV prevention tool for women experiencing elevated occupational risk of HIV infection, including female sex workers (FSW). In 2018, women accounted for one of every five new HIV diagnoses in the United States [1] but fewer than 5% of all PrEP prescription recipients [2]. PrEP is optimally suited for FSW, who experience overlapping burdens of substance use [3, 4], violence and sexual coercion [5–7] that synergistically elevate HIV [8] and sexually transmitted infection (STI) risks [9]. In the United States, FSW are nearly nine times more likely to be living with HIV relative to women in the general population [10]. Increasing PrEP coverage in this population through tailored interventions is, therefore, an urgent HIV prevention priority.
While willingness to use PrEP has been widely documented among FSW globally [11–15], PrEP uptake and persistence (9–30% at 12 months) remain suboptimal [16–18]. Large multi-site trials have attributed attenuations in the effectiveness of daily oral PrEP among women to poor adherence [16, 19–22]. Daily pill burdens [23–26], healthcare inaccessibility [27, 28], layered stigma (i.e., sex work, drug use) [28–30], limited opportunities for safe medication storage [29], and concerns about side effects [14, 27, 31] are frequently cited barriers to oral PrEP uptake and persistence among FSW. These barriers are further amplified by high levels of structural vulnerability among FSW, specifically homelessness [32, 33], food insecurity [33], and lack of health insurance [34]. Given the competing survival needs and healthcare access barriers experienced by FSW, the attributes of currently available PrEP formulations (i.e., pills requiring near-daily adherence for optimal protection) could render this HIV prevention tool undesirable or infeasible for the women who could benefit from it most.
Promising evidence shows alternative PrEP formulations in the development pipeline have comparable, even improved, protective efficacy compared to daily oral PrEP. Novel PrEP agents include long-acting injectables (in the arm or abdomen); topical microbicidal gels (administered vaginally or rectally); passive antibody transfer through intravenous infusion; vaginal rings; and subdermal implants [35, 36]. These non-oral and non-daily PrEP formulations have generated considerable scientific attention, given their potential to increase uptake and adherence in women with elevated HIV risk, such as FSW, for whom daily oral PrEP may be clinically indicated [37] but infeasible in practice. For example, in a preliminary study, long-acting injectable cabotegravir (administered bimonthly) demonstrated superior protection against HIV acquisition (> 80%) relative to daily oral PrEP [38]. In studies measuring acceptance of hypothetical event-driven and long-acting PrEP agents, injectable formulations have garnered the most interest among FSW [27, 39, 40].
Given attribute heterogeneities of these novel PrEP technologies, situating FSW’s formulation preferences in the context of competing priorities, health needs, and risks is crucial for identifying suitable and acceptable HIV prevention alternatives to daily oral PrEP. In addition to injectables, multipurpose technologies like vaginal rings and subdermal implants may appeal to women seeking dual protection against HIV and pregnancy [41–43]. Likewise, topicals gels appeal to women with episodic/intermittent HIV risk who may gravitate towards event-driven HIV prevention options [23, 44]. However, interest among FSW, whose HIV risk may be more consistent, is insufficiently characterized in the literature, particularly in concentrated HIV epidemic settings like the US. In addition to protective duration (e.g., long-acting or shorter-term methods), product attributes like application site, point of service delivery, and partner awareness are salient factors shaping women’s interest in novel PrEP agents [45–48]. Understanding how FSW’s interests in these hypothetical PrEP formulations maps onto the everyday HIV vulnerabilities and risks environments, from unstable housing to intimate partner violence, can help guide development and introduction of products with greatest potential to address persistent PrEP uptake and adherence challenges among FSW.
Responding to these evidence gaps, this study compares interest in various non-oral and non-daily PrEP formulations among street-based FSW in Baltimore, Maryland. Specifically, this study examines multilevel factors associated with interest in five hypothetical event-driven and long-acting PrEP formulations. Findings will inform which combinations of PrEP formulations are most appealing to FSW and how these identified patterns of PrEP interest may vary among FSW with different social, occupational, and structural vulnerability characteristics.
Methods
Study Population and Recruitment
Data are derived from the baseline assessment of The Sex Workers And Police Promoting Health In Risky Environments (SAPPHIRE) study in Baltimore, Maryland [32]. Between April 2016 and August 2017, a prospective cohort of 312 cisgender and transgender women engaged in street-based sex work were recruited via targeted sampling in Baltimore City. Recruitment zones were selected through triangulation of primary and secondary data sources—including geospatial analyses of prostitution charge data, heatmapping of emergency call center reports, unstructured observations (“windshield tours”), ridealongs with Baltimore City Police Department, and key informant interviews—to identify public spaces of possible sex work activity [49]. Women were approached in recruitment zones and invited to participate in the study if they met the following eligibility criteria: (1) were aged 15 years or older; (2) sold or traded oral, vaginal, and/or anal sex for money, material goods (i.e., food or drugs), or favors; (3) picked up clients on the street or in public spaces (e.g., parks) 3+ times in the past 3 months; and (4) expressed willingness to undergo HIV and STI testing [50]. The analytic sample for this study includes only cisgender participants (participants who were assigned female at birth and who currently identify as women), as the PrEP formulations included in the survey differed between cisgender and transgender participants to account for distinct biological mechanisms underpinning HIV risk and routes of PrEP administration.
Study Procedures
After providing written informed consent, participants completed a 50-min interviewer-administered, computer-assisted survey assessing FSW demographics, sex work history, police and client interactions, housing and finances, sexual and drug use behaviors, and healthcare access. A rapid HIV test was administered following survey completion, and results were shared with participants. Referrals to case management, counseling, healthcare, and drug treatment programs were made for participants who expressed interest in health and social services. Biological specimens (vaginal swabs and urine collection) were collected for gonorrhea, chlamydia, and trichomonas serology on the van and sent to the Johns Hopkins International STD Research Infectious Diseases Laboratory for testing. Positive STI results were forwarded to disease intervention specialists at the Baltimore City Health Department, who notified participants and their partners of the results and referred them to treatment services. Participants received a $70 pre-paid gift card for completing the baseline survey and HIV/STI testing.
Measures
Outcomes
Acceptability of various event-driven and long-acting PrEP formulations was assessed by asking women, “Would you be interested in using PrEP in the form of any of the following?” Interest in each modality was measured dichotomously, with affirmative responses captured as endorsement of interest in a particular modality compared to all other response options (i.e., “no”, “not sure”, “refused”). Queried hypothetical PrEP formulations, routes and frequency of administration, and delivery settings are described in Table 1.
Table 1.
Event-driven and long-acting pre-exposure prophylaxis formulations assessed among female sex workers, by administration site, use/replacement frequency, and dispensing venue—Baltimore, Maryland (N = 236)
| Formulation | Duration of protection | Site of administration | Frequency of use/replacement | Dispensing venue | % Endorsing interest |
|---|---|---|---|---|---|
| Injection | Long-acting | Arm | Quarterly (4x/year) | Health facility | 55.9 |
| Injection | Long-acting | Abdomen | Quarterly (4x/year) | Health facility | 29.2 |
| Ring | Long-acting | Vagina | Monthly (12x/year) | Self-administered | 25.4 |
| Gel | Event-driven | Vagina | Episodic (before sex) | Self-administered | 24.6 |
| Intravenous infusion | Long-acting | Unspecified | Quarterly (4x/year) | Health facility | 20.3 |
Independent Variables
The risk environment framework [51], coupled with our previous work with sex workers [15, 27, 32, 52] and other marginalized populations [53, 54] in Baltimore City, guided the selection of multi-level, mutually reinforcing factors to assess in relation to HIV risk and subsequent interest in event-driven and long-acting PrEP formulations. These covariates are operationalized below.
Socio-demographics
Demographic characteristics assessed included age (in continuous years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic or other), educational attainment (completed high school/GED vs. did not), and relationship status (married or in a partnership vs. single).
Structural Vulnerabilities
Numerous indicators assessed recent (past 3 months) structural factors heightening FSW’s vulnerability to risky sexual and drug use behaviors with potential to amplify HIV risk. These dichotomized measures included housing instability (living in ≥ 3 places), arrest or incarceration, unemployment (no formal full- or part-time employment), having financial dependents (any-one who relies on the participant for financial support), and food insecurity (going to bed hungry because there was not enough food at least one day in the past week).
Sex Work Characteristics
Variables assessing entry into and sex work characteristics included entering sex work as minor (started sex work before age 18), being trafficked into sex work (being tricked, misled, coerced/threatened, or physically forced into sex work), duration in sex work (< 1, 1–5, 5+ years), daily sex work (sells/trades sex every day vs. not every day), and number of clients in the past 3 months (dichotomized at the median response of 30 clients).
Condom Use
Four dichotomous indicators were created to indicate any condomless vaginal or anal sex with clients (i.e., partners with whom participants had oral, vaginal, or anal sex for money, food, drugs, or favors) and non-paying (i.e., romantic) partners in the past 3 months.
Violence
Recent (past 3 months) experiences of any physical and sexual violence, by clients and non-paying partners, were assessed via six dichotomous indicators using items adapted from the Revised Conflict Tactics Scale, a widely used validated measure of intimate partner violence [55]. Sexual violence was defined as being pressured, coerced, or forced into having sex. Physical violence was defined as being hit, punched, slapped, physically hurt, or threatened/hurt with a weapon. Condom coercion was defined as any experience where a client or non-paying partner refused a condom before sex or removed a condom during sex after initially agreeing to use one.
Police Avoidance Strategies
Policing practices, including targeted stopping and perceived threat of arrest, have been shown to influence sex workers’ decision-making around spaces where they sell/trade sex, clients to whom they sell/trade sex, and practices for screening clients and negotiating sex [52]. Responses to the following indicators of police avoidance strategies in the previous year were captured dichotomously: (1) avoided carrying condoms; (2) moved to an unfamiliar area for clients; and (3) rushed negotiations with clients.
Substance Use
A number of survey items assessed injection drug use behaviors. Responses were used to create the following categories of injection related HIV risk behaviors in the past 3 months: no injection drug use, injected drugs without sharing syringes, and injected drugs and shared syringes. Daily binge drinking was captured dichotomously from “daily or almost daily” responses to a single item measuring alcohol consumption frequency, adapted from the Alcohol Use Disorders Identification Test–Concise (AUDIT-C)—a validated, widely used instrument assessing hazardous drinking behaviors in adults [56].
Analysis
The analytic sample was restricted to HIV-seronegative cisgender participants at baseline (N = 236), verified by rapid HIV testing. Descriptive statistics were first calculated to explore covariate distributions in the study population, including frequency measures for socio-demographic characteristics, HIV risk environment factors, and endorsement of interest in event-driven and long-acting PrEP formulations.
To examine whether FSW’s interest in event-driven and long-acting PrEP agents clustered around product attributes (e.g., formulation type, site of administration, use frequency, dispensing venues), latent class analysis was used to identify mutually exclusive and discrete response patterns in items measuring FSW’s interest in various PrEP formulations. Compared to traditional covariate-driven regression approaches, latent class analysis estimates unobservable (latent) subgroups from item-response patterns for specific variables, specified a priori [57]. This subject-oriented approach to data analysis helps identify homogenous subgroups of FSW, characterized by interest in hypothetical PrEP formulations, that would be otherwise unobservable using classical regression techniques on individual variables.
Using dichotomous items measuring FSW’s interest in five event-driven and long-acting PrEP formulations (Table 1), two-, three-, and four-class models were iteratively estimated. Model fit indices and distinguishability of item-response probabilities, conditioned on predicted probability of latent class membership, guided selection of the final latent class solution [57, 58]. Inspected fit indices included the chi-square likelihood ratio test (χ2 LRT) [59], Akaike and Bayesian Information Criteria (AIC and BIC, respectively) [57], entropy [60], Vong–Lo–Mendell–Rubin likelihood ratio test (VLMR-LRT) [61], and bootstrap likelihood ratio test (BLRT) [62, 63].
After identifying the optimal latent class model fit for the data, post-estimation multinomial latent class regression using the R3STEP method identified associations of HIV risk environment characteristics with probabilistic latent class membership. Compared to two-step (fit-then-analyze) approaches, where subjects are assigned to a single latent class based on their most likely (highest) predicted probability of class membership [57, 64], the R3STEP procedure evaluates covariate differences between enumerated latent classes without altering fitted latent class model parameters [65]. Because latent class analysis enumerates subgroups based on item-response probabilities conditioned on posterior probabilities of class membership, both of which are measured with error, the R3STEP method accounts for measurement error from latent class enumeration when regressing probabilistic latent class membership onto specified covariates, yielding more accurate standard errors. HIV risk environment covariates significantly associated with latent class membership at the p < 0.05 level were further inspected in multivariable analysis, adjusting for socio-demographics and sex work characteristics. Data were managed and descriptively analyzed in Stata/IC 15.1 (StataCorp®, College Station, TX). Latent class analyses and regressions were implemented in MPlus 8.3 (Muthen & Muthen®, Los Angeles, CA).
Results
Sample Characteristics
Table 2 presents descriptive sample statistics. The median age was 35 years (range 18–61 years). Most FSW were non-Hispanic white (66%), and nearly one-fourth (23%) identified as non-Hispanic black. Half did not complete high school (52%). With respect to structural vulnerabilities, over half reported unstable housing (56%), unemployment (92%), and weekly food insecurity (53%) in the past 3 months. Past-year arrest/incarceration (46%) was frequently reported. Over one-third (39%) had financial dependents. About half of FSW reported selling sex for 5 years or longer (50%). Few reported initiating sex work as minors (20%) or being trafficked into sex work (8%). Most FSW reported selling sex daily (66%). About half of participants (55%) reported having 30 or more sex work clients in the past 3 months.
Table 2.
Descriptive sample statistics of female sex workers at baseline assessment—Baltimore, Maryland (N = 236)
| N | % | |
|---|---|---|
| Socio-demographics | ||
| Age, in years (median, range) | 34.5 | 18–61 |
| Race/ethnicity | ||
| Non-Hispanic white | 155 | 65.7 |
| Non-Hispanic black | 55 | 23.3 |
| Hispanic or other | 26 | 11.0 |
| Educational attainment | ||
| Did not complete high school | 123 | 52.1 |
| Completed high school/GED or higher | 113 | 47.9 |
| Structural vulnerabilities | ||
| Housing instability, past 3 months | 149 | 55.9 |
| Arrest or incarceration, past 12 months | 109 | 46.4 |
| Unemployment, past 3 months | 216 | 91.9 |
| Have financial dependents | 93 | 39.4 |
| Food insecurity (≥ 1 weekly), past 3 months | 125 | 53.0 |
| Sex work characteristics | ||
| Entered sex work as a minor (< 18 years) | 47 | 19.9 |
| Trafficked into sex work | 19 | 8.1 |
| Duration in sex work | ||
| <1 year | 43 | 18.2 |
| 1–5 years | 75 | 31.8 |
| 5+ years | 118 | 50.0 |
| Daily sex work | 156 | 66.1 |
| Number of clients, past 3 months | ||
| < 30 | 106 | 44.9 |
| 30+ | 130 | 55.1 |
| Condom use (past 3 months) | ||
| Condomless vaginal sex | ||
| With clients | 88 | 37.5 |
| With non-paying partners | 104 | 44.1 |
| Condomless anal sex | ||
| With clients | 19 | 8.1 |
| With non-paying partners | 40 | 17.0 |
| Violence (past 3 months) | ||
| Condom coercion | ||
| By clients | 99 | 41.5 |
| By non-paying partners | 24 | 10.1 |
| Sexual violence | ||
| By clients | 71 | 30.1 |
| By non-paying partners | 20 | 8.5 |
| Physical violence | ||
| By clients | 45 | 19.1 |
| By non-paying partners | 35 | 14.8 |
| Police avoidance strategies (past 12 months) | ||
| Avoided carrying condoms | 33 | 14.0 |
| Moved to an unfamiliar area for clients | 54 | 22.9 |
| Rushed negotiations with (potential) clients | 134 | 56.8 |
| Substance use | ||
| Injection drug use, past 3 months | ||
| None | 70 | 29.7 |
| Injected drugs without sharing syringes | 74 | 31.3 |
| Injected drugs and shared syringes | 92 | 39.0 |
| Daily binge drinking | 21 | 8.9 |
Sexual risks and violence were prevalent among FSW. Over one-third of participants reported condomless vaginal sex with clients (38%) and non-paying partners (44%). Relative to vaginal sex, condomless anal sex in the past 3 months was reported less frequently with clients (8%) and non-paying partners (17%). Recent condom coercion (by clients: 42%, by non-paying partners: 10%), sexual violence (by clients: 30%, by non-paying partners: 9%), and physical violence (by clients: 19%, by non-paying partners: 15%) were disconcertingly high.
Police avoidance strategies were endorsed with notable frequency among FSW. In the past 12 months, over half (57%) reported rushing negotiations with potential clients to avert police detection. Furthermore, 23% and 14%, respectively, reported moving to an unfamiliar area to sell sex and avoided carrying condoms. Finally, in terms of substance use, a majority of FSW (70%) reported injection drug use in the past 3 months, over half of whom (39%) shared syringes.
Acceptability of Event-Driven and Long-Acting PrEP Formulations
Interest in novel event-driven and long-acting PrEP agents fluctuated widely (Table 1). Quarterly arm injections were the most popular (56%). Interest dipped substantially when FSW were queried about quarterly abdomen injections (29%), vaginal rings (replaced monthly) (25%), gels applied topically to the vagina before penetrative sex (25%), and quarterly intravenous infusions of broadly neutralizing antibodies against HIV (20%). Approximately two-thirds (67%) reported interest in at least one event-driven or long-acting PrEP formulation.
Identifying Clusters of Interest in Event-Driven and Long-Acting PrEP Using Latent Class Analysis
Table 3 presents fit indices for the two-, three-, and four-class models of event-driven and long-acting PrEP formulation acceptability. Three model fit indices (χ2 LRT: 37.260, p < 0.001; BIC: 1273.372; entropy: 0.841) favored selection of a three-class solution, relative to other enumerated latent class models. The three-class model was also preferred because of meaningful and interpretable differences in item-response probabilities between enumerated classes.
Table 3.
Latent class model goodness-of-fit statistics, by number of classes specified a priori
| No. of classes | No. of free parameters | Log-likelihood (df) | χ2 LRT (p-value) | AIC | BIC | Entropy | VLMR-LRT (p-value) | BLRT (p-value) |
|---|---|---|---|---|---|---|---|---|
| 2 | 11 | − 605.662 (20) | 68.097 (p < 0.001) | 1233.323 | 1271.426 | 0.762 | 161.974 (p < 0.001) | 166.914 (p < 0.001) |
| 3 | 17 | − 590.243 (14) | 37.260 (p < 0.001) | 1214.487 | 1273.372 | 0.841 | 29.924 (p = 0.005) | 30.836 (p < 0.001) |
| 4 | 23 | − 576.469 (8) | 9.712 (p = 0.286) | 1198.939 | 1278.607 | 0.841 | 26.733 (p = 0.009) | 27.548 (p < 0.001) |
χ2 LRT Chi-square likelihood ratio test, AIC Akaike Information Criteria, BIC Bayesian Information Criteria, VLMR-LRT Vuong–Lo–Mendell–Rubin likelihood ratio test, BLRT bootstrap likelihood ratio test
Figure 1 illustrates posterior class membership probabilities and item response probabilities, conditioned on class membership, for the three-class model. Class 1 (24% sample prevalence, Injectable Acceptors) was characterized by high interest (> 60%) in only injectable PrEP formulations (arm: 93%; abdomen: 71%) but lower interest in other formulations, including vaginal gels (15%), intravenous infusion (34%), and vaginal rings (0%). Class 2 (18% sample prevalence, Universal Acceptors) was characterized by high interest (> 60%) across event-driven and long-acting PrEP formulations (arm injectable: 94%, abdomen injectable: 64%, vaginal gel: 63%, intravenous infusion: 67%, vaginal ring: 100%). Lastly, Class 3 (58% sample prevalence, Non-Acceptors) was characterized by generally low acceptance (< 50%) across PrEP formulations (range 0–29%). The most popular hypothetical PrEP formulations in this class were arm injectables (29%), vaginal gels (17%), and vaginal rings (12%).
Fig. 1.
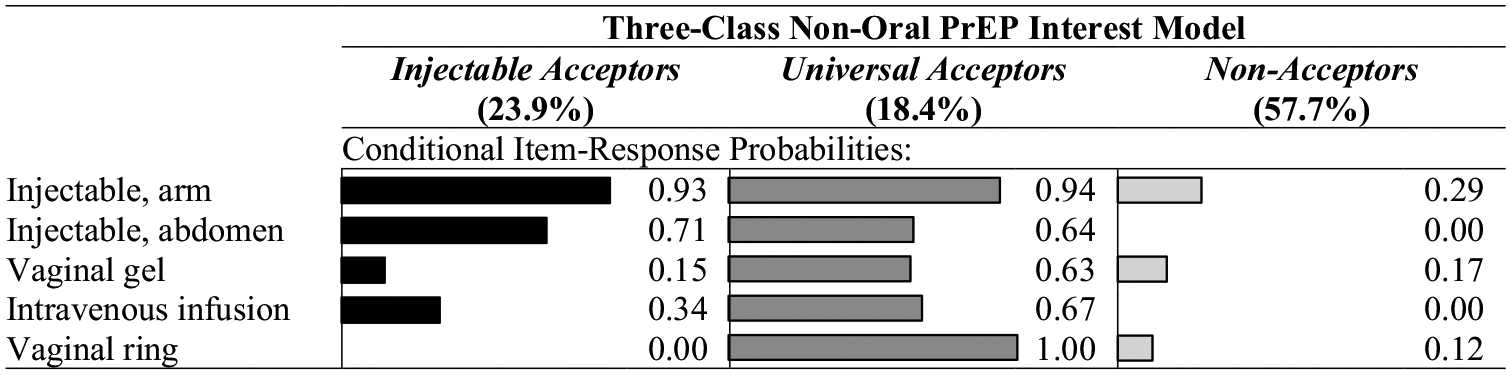
Probability of expressing interest in event-driven and long-acting pre-exposure prophylaxis formulations among female sex workers, by posterior probability of latent class membership—Baltimore, Maryland (N = 236)
Multilevel Factors Associated with Probabilistic Latent Class Membership
Table 4 presents adjusted (multivariable) associations between probabilistic latent class membership and HIV risk environment characteristics, identified in multinomial latent class regression. Relative to Non-Acceptors, Injectable Acceptors had significantly higher odds of condomless vaginal sex with clients [adjusted odds ratio (aOR) 2.35, 95% confidence interval (CI) 1.01–5.45, p = 0.047] and injection drug use (aOR 3.64, 95% CI 1.23–10.77, p = 0.020). Injectable Acceptors class membership was only marginally associated with avoiding carrying condoms to avert police detection (aOR 3.18, 95% CI 0.88–11.49, p = 0.077) compared to Non-Acceptors.
Table 4.
Adjusted odds ratios (aOR) and 95% confidence intervals (95% CI) from multinomial latent class regression of predicted latent class probabilities on correlates of event-driven and long-acting pre-exposure prophylaxis interest (N = 236) (only covariates significantly associated with probabilistic latent class membership in bivariate analysis are presented in the table)
| Injectable Acceptors (vs. Non-Acceptors) | Universal Acceptors (vs. Non-Acceptors) | Universal Acceptors (vs. Injectable Acceptors) | ||||
|---|---|---|---|---|---|---|
| aOR (95% CI) | p | aOR (95% CI) | p | aOR (95% CI) | p | |
| Condom use (past 3 months) | ||||||
| Condomless vaginal sex | ||||||
| With clientsa | 2.35 (1.01, 5.45) | 0.047 | 2.28 (1.02, 5.11) | 0.044 | 0.97 (0.40, 2.38) | 0.953 |
| Violence (past 3 months) | ||||||
| Condom coercion | ||||||
| By clientsa | 1.23 (0.55, 2.77) | 0.616 | 2.66 (1.18, 5.78) | 0.018 | 2.12 (0.85, 5.26) | 0.106 |
| Sexual violence | ||||||
| By clientsa | 0.97 (0.39, 2.44) | 0.953 | 3.18 (1.38, 7.29) | 0.006 | 3.27 (1.25, 8.57) | 0.016 |
| Physical violence | ||||||
| By clientsa | 0.57 (0.19, 1.74) | 0.322 | 2.44 (0.97, 6.18) | 0.059 | 4.30 (1.42, 12.98) | 0.010 |
| Police avoidance strategies (past 12 months) | ||||||
| Avoided carrying condomsa | 3.18 (0.88, 11.49) | 0.077 | 3.17 (0.90, 11.23) | 0.073 | 1.00 (0.35, 2.88) | 0.996 |
| Rushed negotiations with (potential) clientsa | 1.31 (0.59, 2.92) | 0.504 | 2.15 (0.95, 4.87) | 0.066 | 1.61 (0.65, 3.98) | 0.305 |
| Substance use | ||||||
| Injection drug use, past 3 monthsb | 3.64 (1.23, 10.77) | 0.020 | 1.81 (0.72, 4.53) | 0.204 | 0.50 (0.15, 1.66) | 0.258 |
Bolded values represent regression coefficients that were statisitcally significant (p < 0.05)
Adjusted for age, race/ethnicity, education, duration (years) in sex work, and entering sex work as a minor
Adjusted for age, race/ethnicity, education, and entering sex work as a minor
Likewise, relative to Non-Acceptors, Universal Acceptors exhibited significantly higher odds of condomless vaginal sex with clients (aOR 2.28, 95% CI 1.02–5.11, p = 0.044) as well as client-perpetrated condom coercion (aOR 2.66, 95% CI 1.18–5.78, p = 0.018) and sexual violence (aOR 3.18, 95% CI 1.38–7.29, p = 0.006), respectively. Although significantly higher among Universal Acceptors in bivariate analysis, client-perpetrated physical violence (aOR 2.44, 95% CI 0.97–6.18, p = 0.059), avoiding carrying condoms to avert police detection, (aOR 3.17, 95% CI 0.90–11.23, p = 0.073), and rushing negotiations with potential clients as a police avoidance strategy (aOR 2.15, 95% CI 0.95–4.87, p = 0.066) were only marginally associated with membership in the Universal Acceptors class, compared to Non-Acceptors, in multivariable analysis. Lastly, the adjusted odds of client-perpetrated sexual (aOR 3.27, 95% CI 1.25–8.57, p = 0.016) and physical (aOR 4.30, 95% CI 1.42–12.98, p = 0.010) violence, respectively, was significantly higher among Universal Acceptors compared to Injectable Acceptors.
Covariates that were not significantly associated (p ≥ 0.05) with probabilistic latent class membership were excluded from Table 4. These included: socio-demographics, structural vulnerability factors, sex work characteristics, condomless vaginal sex with non-paying partners, condomless anal sex (across partner types), any violence perpetrated by non-paying partners, moving to an unfamiliar area to avoid police in the past 12 months, and daily binge drinking.
Discussion
We sought to understand which combinations of acceptable hypothetical PrEP modalities exist among FSW and how these preferences differ by socio-demographic characteristics and structural vulnerabilities influential in the HIV risk environment. FSW’s interest in novel event-driven and long-acting PrEP formulations was high and clustered around specific modalities. We identified three subgroups with distinct patterns of interest in hypothetical PrEP formulations: Universal Acceptors, Injectable Acceptors, and Non-Acceptors. Nearly half of surveyed FSW were willing to use various event-driven or long-acting PrEP agents or exhibit specific preferences for injectable formulations (arm or abdomen). Injectable Acceptors were distinguishable from Non-Acceptors by higher odds of condomless vaginal sex with clients and injection drug use but lower odds of client-perpetrated sexual and physical violence, relative to FSW who expressed broad interest across hypothetical PrEP formulations. Likewise, Universal Acceptors exhibited significantly higher odds of HIV risks—including condomless vaginal sex, condom coercion, and sexual violence—than Non-Acceptors. Given a majority (> 66%) of FSW expressed interest in at least one event-driven or long-acting PrEP formulation, the availability of numerous PrEP modalities could offer FSW more choice and agency in their HIV prevention options over the life course.
In both descriptive analysis and latent class modeling, injectable PrEP outshined other formulations in terms of interest among FSW. In the global literature on PrEP acceptability, women express substantial interest in injectable PrEP because of reduced dosing requirements [23, 27, 47, 48, 66] and its multipurpose potential (i.e., combination administration with injectable contraception for dual HIV and pregnancy prevention) [45]. Despite exclusive provision in healthcare settings, injectable PrEP may appeal to FSW who experience barriers to healthcare access, which ultimately reduce their frequency of healthcare interactions [67]. Innovative service-delivery strategies, including PrEP provision outside of health facilities (e.g., in pharmacies or community settings), can address the accessibility challenges that bottleneck the PrEP care continuum for FSW.
Injection drug use uniquely characterized FSW who expressed interest in injectable PrEP but lower interest in other event-driven and long-acting PrEP formulations (i.e., Injectable Acceptors). Globally, sex workers who inject drugs are more likely to experience homelessness and incarceration [34, 68], lack health insurance [34], report client violence [69, 70], and engage in higher-risk sex (i.e., unprotected anal sex or consent to higher payment for condomless sex) [71, 72]. Although the association between injection drug use and these aforementioned characteristics was not examined in this study, product attributes and service-delivery characteristics of injectable PrEP may better accommodate competing needs and interests of FSW who inject drugs than currently available PrEP modalities: by requiring minimal contact (four times annually) with the healthcare system and long-acting protection, it averts the adherence burdens and concerns about safe storage that dissuade women who inject drugs from using daily oral PrEP [73–75]. By design, other event-driven PrEP formulations, for example topical gels, offer intermittent HIV prevention at physiological sites of potential exposure; compared to injectable PrEP, these other non-oral formulations could be perceived as providing incomplete systemic protection from HIV infection [23, 27, 76] and may, therefore, be less desirable among FSW who experience repeated potential HIV exposures from their injection behaviors. This was reaffirmed by how the interests of FSW who inject drugs in event-driven and long-acting PrEP clustered almost exclusively around injectable formulations.
By comparison, Universal Acceptors experienced violence at significantly higher rates relative to Injectable Acceptors and Non-Acceptors, respectively. Various formulations, from injectable PrEP to vaginal rings, have infrequent dosing requirements and can be administered or used discretely, without detection by controlling or violent partners [45]. Other formulations, like topical gels, may appeal to FSW who manage intermittent HIV risk, including inconsistent condom use with paying or non-paying partners. While some studies have shown that experiences with violence may attenuate interest in event-based HIV prevention modalities like microbicides [77–79], others showed topical microbicides were highly acceptable, particularly when they could be used discretely without partner knowledge [80]. These inconsistencies may reflect fundamental differences in sex workers’ abilities to control the context and spaces in which they adopt HIV prevention behaviors. Ultimately, expanding choices can support PrEP initiation among street-based FSW, who can benefit from various options supporting their shifting needs, thus advancing HIV prevention efforts.
Non-Acceptors in this study reported lower rates of condomless vaginal sex compared to Injectable Acceptors and Universal Acceptors, which aligns with findings from the extant literature that perceived HIV risk is a critical facilitator of PrEP interest and willingness [11, 12]. For FSW who can safely negotiate condom use with clients and, therefore, report infrequent (or no) condomless sex with paying partners, any formulation of PrEP may be deemed unnecessary. Communicating the availability of biomedical HIV prevention options, including post-exposure prophylaxis, to FSW who consistently use condoms with clients and, thus, exhibit diminished interest in PrEP would close HIV prevention gaps in this population, especially for FSW who experience an unanticipated (potential) HIV exposure or whose condom negotiation capacities and use patterns shift.
As one of the few studies examining HIV prevention preferences among street-based FSW in the United States, a strength of this study is its use of latent class analysis to unearth patterns of interest in numerous event-driven and long-acting PrEP formulations. Findings from this study, nonetheless, are subject to at least five limitations. First, interest in various available and hypothetical PrEP formulations were measured independently and, therefore, do not capture ranked modality preferences among participants. Second, interest in hypothetical PrEP formulations may not align with uptake intentions or adherence outcomes. Third, given the relatively small sample size, observed effect estimates and magnitudes of association in this study may not capture relationships that would be observed with a larger sample of street-based FSW. In latent class analysis, the moderately sized sample also posed challenges for model estimability, as reflected by the presence of boundary and ceiling values (i.e., conditional item-response probabilities of 0 or 1) in the latent class model. Fourth, the study’s observational design is susceptible to recall and response biases. Lastly, because questions regarding interest in hypothetical PrEP formulations were asked only at the baseline visit, associations of PrEP interest with multilevel factors could only be examined cross-sectionally, rather than over time and potentially as a consequence of time-varying covariates.
Conclusions
In this cross-sectional study of women engaged in street-based sex work in Baltimore, most FSW endorsed interest in at least one event-driven or long-acting PrEP formulations. Latent class analysis uncovered interest patterns in novel PrEP agents that clustered around specific product attributes (i.e., formulation, frequency of use/replacement, administration venue) were associated with specific social, occupational, and structural risks, including condomless sex, physical and sexual violence, and injection drug use. Given the heterogeneity of interests in event-driven and long-acting PrEP formulations in this population, availing multiple formulations can close gaps in PrEP interest and uptake among FSW, whose HIV prevention needs and preferences are highly variable. Expanding choice in HIV prevention commodities, in addition to counseling on the benefits and constraints of specific PrEP formulations, can more effectively link FSW to the appropriate PrEP options that complement, rather than compete with, their financial, social, and health priorities.
Acknowledgements
We thank all the women who participated in this study as well as study staff who oversaw data collection.
Funding
This study was supported by the National Institute on Drug Abuse (R01DA038499-01) and the Johns Hopkins University Center for AIDS Research (1P30AI094189). KES was supported by a Training Grant from the National Institute on Drug Abuse (5T32DA007292).
Footnotes
Conflict of interest The authors have no conflicts to declare.
Ethical Approval The study was approved by the Johns Hopkins Bloomberg School of Public Health IRB.
Informed Consent Participants provided written informed consent prior to study procedures.
Data Availability
The data presented in this manuscript are available from the corresponding author upon request.
References
- 1.Centers for Disease Control and Prevention (CDC). HIV in the United States and dependent areas. Atlanta: CDC; 2020. https://www.cdc.gov/hiv/statistics/overview/ataglance.html. Accessed July 7, 2020. [Google Scholar]
- 2.Huang YA. HIV preexposure prophylaxis, by race and ethnicity—United States, 2014–2016. Morb Mortal Wkly Rep. 2018;67. https://www.cdc.gov/mmwr/volumes/67/wr/mm6741a3.htm. Accessed July 7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuteesa MO, Seeley J, Weiss HA, Cook S, Kamali A, Webb EL. Alcohol misuse and illicit drug use among occupational groups at high risk of HIV in Sub-Saharan Africa: a systematic review. AIDS Behav. 2019;23(12):3199–225. [DOI] [PubMed] [Google Scholar]
- 4.Kuteesa MO, Seeley J, Cook S, Webb EL. Multi-level experiences and determinants of alcohol misuse and illicit drug use among occupational groups at high-risk of HIV in Sub-Saharan Africa: a thematic synthesis of qualitative findings. Glob Public Health. 2020;15(5):715–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldenberg SM, Duff P, Krusi A. Work environments and HIV prevention: a qualitative review and meta-synthesis of sex worker narratives. BMC Public Health. 2015;15:1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Footer KH, Silberzahn BE, Tormohlen KN, Sherman SG. Policing practices as a structural determinant for HIV among sex workers: a systematic review of empirical findings. J Int AIDS Soc. 2016;19(4 Suppl 3):20883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Platt L, Grenfell P, Meiksin R, Elmes J, Sherman SG, Sanders T, et al. Associations between sex work laws and sex workers’ health: a systematic review and meta-analysis of quantitative and qualitative studies. PLoS Med. 2018;15(12):e1002680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(7):538–49. [DOI] [PubMed] [Google Scholar]
- 9.Dubbink JH, Verweij SP, Struthers HE, Ouburg S, McIntyre JA, Morré SA, et al. Genital Chlamydia trachomatis and Neisseria gonorrhoeae infections among women in Sub-Saharan Africa: a structured review. Int J STD AIDS. 2018;29(8):806–24. [DOI] [PubMed] [Google Scholar]
- 10.Nerlander LM, Handanagic S, Hess KL, Lutnick A, Agnew-Brune CB, Hoots BE, et al. HIV prevalence among women who exchange sex for money or drugs-4 U.S. cities. J Acquir Immune Defic Syndr 1999. 2020;84(4):345–54. [DOI] [PubMed] [Google Scholar]
- 11.Wang Z, Lau JTF, Yang X, Cai Y, Gross DL, Ma T, et al. Acceptability of daily use of free oral pre-exposure prophylaxis (PrEP) among transgender women sex workers in Shenyang, China. AIDS Behav. 2017;21(12):3287–98. [DOI] [PubMed] [Google Scholar]
- 12.Bazzi AR, Yotebieng K, Otticha S, Rota G, Agot K, Ohaga S, et al. PrEP and the syndemic of substance use, violence, and HIV among female and male sex workers: a qualitative study in Kisumu, Kenya. J Int AIDS Soc. 2019;22(4):e25266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glick JL, Russo R, Jivapong B, Rosman L, Pelaez D, Footer KHA, et al. The PrEP care continuum among cisgender women who sell sex and/or use drugs globally: a systematic review. AIDS Behav. 2019;24(5):1312–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poteat T, Wirtz A, Malik M, Cooney E, Cannon C, Hardy WD, et al. A gap between willingness and uptake: findings from mixed methods research on HIV prevention among Black and Latina transgender women. J Acquir Immune Defic Syndr 1999. 2019;82(2):131–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tomko C, Park JN, Allen ST, Glick J, Galai N, Decker MR, et al. Awareness and interest in HIV pre-exposure prophylaxis among street-based female sex workers: results from a US context. AIDS Patient Care STDs. 2019;33(2):49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deutsch MB, Glidden DV, Sevelius J, Keatley J, McMahan V, Guanira J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2(12):e512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eakle R, Gomez GB, Naicker N, Bothma R, Mbogua J, Cabrera Escobar MA, et al. HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: results from a prospective observational demonstration project. PLoS Med. 2017;14(11):e1002444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kagaayi J, Batte J, Nakawooya H, Kigozi B, Nakigozi G, Strömdahl S, et al. Uptake and retention on HIV pre-exposure prophylaxis among key and priority populations in South-Central Uganda. J Int AIDS Soc. 2020;23(8):e25588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mutua G, Sanders E, Mugo P, Anzala O, Haberer JE, Bangsberg D, et al. Safety and adherence to intermittent pre-exposure prophylaxis (PrEP) for HIV-1 in African men who have sex with men and female sex workers. PLoS ONE. 2012;7(4):e33103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Lond Engl. 2013;381(9883):2083–90. [DOI] [PubMed] [Google Scholar]
- 22.Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372(6):509–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mack N, Evens EM, Tolley EE, Brelsford K, Mackenzie C, Milford C, et al. The importance of choice in the rollout of ARV-based prevention to user groups in Kenya and South Africa: a qualitative study. J Int AIDS Soc. 2014;17(3 Suppl 2):19157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ye L, Wei S, Zou Y, Abdullah AS, Zhong X, Ruan Y, et al. HIV pre-exposure prophylaxis interest among female sex workers in Guangxi, China. PLoS ONE. 2014;9(1):e86200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reza-Paul S, Lazarus L, Doshi M, Hafeez Ur Rahman S, Ramaiah M, Maiya R, et al. Prioritizing risk in preparation for a demonstration project: a mixed methods feasibility study of oral pre-exposure prophylaxis (PREP) among female sex workers in South India. PLoS ONE. 2016;11(11):e0166889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eakle R, Bourne A, Mbogua J, Mutanha N, Rees H. Exploring acceptability of oral PrEP prior to implementation among female sex workers in South Africa. J Int AIDS Soc. 2018;21(2):e25081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Footer KHA, Lim S, Rael CT, Greene GJ, Carballa-Diéguez A, Giguere R, et al. Exploring new and existing PrEP modalities among female sex workers and women who inject drugs in a U.S. city. AIDS Care. 2019;31(10):1207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Emmanuel G, Folayan M, Undelikwe G, Ochonye B, Jayeoba T, Yusuf A, et al. Community perspectives on barriers and challenges to HIV pre-exposure prophylaxis access by men who have sex with men and female sex workers access in Nigeria. BMC Public Health. 2020;20(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van der Elst EM, Mbogua J, Operario D, Mutua G, Kuo C, Mugo P, et al. High acceptability of HIV pre-exposure prophylaxis but challenges in adherence and use: qualitative insights from a phase I trial of intermittent and daily PrEP in at-risk populations in Kenya. AIDS Behav. 2013;17(6):2162–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eakle R, Bothma R, Bourne A, Gumede S, Motsosi K, Rees H. “I am still negative”: female sex workers’ perspectives on uptake and use of daily pre-exposure prophylaxis for HIV prevention in South Africa. PLoS ONE. 2019;14(4):e0212271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chakrapani V, Shunmugam M, Rawat S, Baruah D, Nelson R, Newman PA. Acceptability of HIV pre-exposure prophylaxis among transgender women in India: a qualitative investigation. AIDS Patient Care STDs. 2020;34(2):92–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sherman SG, Park JN, Galai N, Allen ST, Huettner SS, Silberzahn BE, et al. Drivers of HIV infection among cisgender and transgender female sex worker populations in Baltimore City: results from the SAPPHIRE Study. J Acquir Immune Defic Syndr 1999. 2019;80(5):513–21. [DOI] [PubMed] [Google Scholar]
- 33.Lim S, Park JN, Kerrigan DL, Sherman SG. Severe food insecurity, gender-based violence, homelessness, and HIV risk among street-based female sex workers in Baltimore, Maryland. AIDS Behav. 2019;23(11):3058–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nerlander LM, Hess KL, Rose CE, Sionean C, Thorson A, Broz D, et al. Exchange sex and HIV infection among women who inject drugs-20 US cities, 2009. J Acquir Immune Defic Syndr 1999. 2017;75(Suppl 3):S333–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hendrix CW. HIV antiretroviral pre-exposure prophylaxis: development challenges and pipeline promise. Clin Pharmacol Ther. 2018;104(6):1082–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coelho LE, Torres TS, Veloso VG, Landovitz RJ, Grinsztejn B. Pre-exposure prophylaxis 2.0: new drugs and technologies in the pipeline. Lancet HIV. 2019;6(11):e788–99. [DOI] [PubMed] [Google Scholar]
- 37.United States Public Health Service. Pre-exposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. Atlanta: Centers for Disease Control and Prevention (CDC); 2017. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Accessed July 7, 2020. [Google Scholar]
- 38.HIV Prevention Trials Network. HPTN 084 study demonstrates superiority of CAB LA to oral FTC/TDF for the prevention of HIV. HPTN; 2020. https://www.hptn.org/news-and-events/press-releases/hptn-084-study-demonstrates-superiority-of-cab-la-to-oral-ftctdf-for. [Google Scholar]
- 39.Luecke EH, Cheng H, Woeber K, Nakyanzi T, Mudekunye-Mahaka IC, van der Straten A, et al. Stated product formulation preferences for HIV pre-exposure prophylaxis among women in the VOICE-D (MTN-003D) study. J Int AIDS Soc. 2016;19(20875):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harling G, Muya A, Ortblad KF, Mashasi I, Dambach P, Ulenga N, et al. HIV risk and pre-exposure prophylaxis interest among female bar workers in Dar es Salaam: cross-sectional survey. BMJ Open. 2019;9(3):e023272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hynes JS, Sales JM, Sheth AN, Lathrop E, Haddad LB. Interest in multipurpose prevention technologies to prevent HIV/STIs and unintended pregnancy among young women in the United States. Contraception. 2018;97(3):277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minnis AM, Browne EN, Boeri M, Agot K, van der Straten A, Ahmed K, et al. Young women’s stated preferences for biomedical HIV prevention: results of a discrete choice experiment in Kenya and South Africa. J Acquir Immune Defic Syndr 1999. 2019;80(4):394–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shapley-Quinn MK, Manenzhe KN, Agot K, Minnis AM, van der Straten A. “We are not the same”: African women’s view of multipurpose prevention products in the TRIO clinical study. Int J Womens Health. 2019;11:97–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.van den Berg JJ, Rosen RK, Bregman DE, Thompson LA, Jensen KM, Kiser PF, et al. “Set it and forget it”: women’s perceptions and opinions of long-acting topical vaginal gels. AIDS Behav. 2014;18(5):862–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Govender E, Abdool KQ. Understanding women and men’s acceptability of current and new HIV prevention technologies in KwaZulu-Natal, South Africa. AIDS Care. 2018;30(10):1311–4. [DOI] [PubMed] [Google Scholar]
- 46.Eisingerich AB, Wheelock A, Gomez GB, Garnett G, Dybul MR, Piot PK. Attitudes and acceptance of oral and parenteral HIV preexposure prophylaxis among potential user groups: a multinational study. PLoS ONE. 2012;7(1):e28238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Minnis AM, Roberts ST, Agot K, Weinrib R, Ahmed K, Manenzhe K, et al. Young women’s ratings of three placebo multipurpose prevention technologies for HIV and pregnancy prevention in a randomized, cross-over study in Kenya and South Africa. AIDS Behav. 2018;22(8):2662–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van der Straten A, Agot K, Ahmed K, Weinrib R, Browne EN, Manenzhe K, et al. The Tablets, Ring, Injections as Options (TRIO) study: what young African women chose and used for future HIV and pregnancy prevention. J Int AIDS Soc. 2018;21(3):e25094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Allen ST, Footer KHA, Galai N, Park JN, Silberzahn B, Sherman SG. Implementing targeted sampling: lessons learned from recruiting female sex workers in Baltimore, MD. J Urban Health Bull N Y Acad Med. 2019;96(3):442–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Silberzahn BE, Morris MB, Riegger KE, White RH, Tomko CA, Park JN, et al. Barriers and facilitators to retaining a cohort of street-based cisgender female sex workers recruited in Baltimore, Maryland, USA: results from the SAPPHIRE study. BMC Public Health. 2020;20(1):585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rhodes T. The, “risk environment”: a framework for understanding and reducing drug-related harm. Int J Drug Policy. 2002;13(2):85–94. [Google Scholar]
- 52.Footer KHA, Park JN, Allen ST, Decker MR, Silberzahn BE, Huettner S, et al. Police-related correlates of client-perpetrated violence among female sex workers in Baltimore City, Maryland. Am J Public Health. 2019;109(2):289–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brantley M, Kerrigan D, German D, Lim S, Sherman S. Identifying patterns of social and economic hardship among structurally vulnerable women: a latent class analysis of HIV/STI risk. AIDS Behav. 2017;21(10):3047–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Footer KHA, Lim S, Brantley MR, Sherman SG. Structural risk and limits on agency among exotic dancers: HIV risk practices in the exotic dance club. Cult Health Sex. 2018;20(3):321–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS2): development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 56.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95. [DOI] [PubMed] [Google Scholar]
- 57.Collins LM, Lanza ST. Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences. New York: Wiley; 2009. [Google Scholar]
- 58.Lanza ST, Collins LM, Lemmon DR, Schafer JL. PROC LCA: a SAS procedure for latent class analysis. Struct Equ Model Multidiscip J. 2007;14(4):671–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goodman LA. Exploratory latent structure analysis using both identifiable and unidentifiable models. Biometrika. 1974;61(2):215–31. [Google Scholar]
- 60.Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. J Classif. 1996;13(2):195–212. [Google Scholar]
- 61.Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–78. [Google Scholar]
- 62.McCutcheon AL. Latent class analysis. Thousand Oaks: SAGE; 1987. [Google Scholar]
- 63.McLachlan GJ. Mahalanobis distance. Resonance. 1999;4(6):20–6. [Google Scholar]
- 64.Nagin D Group-based modeling of development. Cambridge: Harvard University Press; 2009. [Google Scholar]
- 65.Vermunt JK. Latent class modeling with covariates: two improved three-step approaches. Polit Anal Undefined/ed. 2017;18(4):450–69. [Google Scholar]
- 66.Rael CT, Martinez M, Giguere R, Bockting W, MacCrate C, Mellman W, et al. Transgender women’s concerns and preferences on potential future long-acting biomedical HIV prevention strategies: the case of injections and implanted medication delivery devices (IMDDs). AIDS Behav. 2019;24(5):1452–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ma PHX, Chan ZCY, Loke AY. The socio-ecological model approach to understanding barriers and facilitators to the accessing of health services by sex workers: a systematic review. AIDS Behav. 2017;21(8):2412–38. [DOI] [PubMed] [Google Scholar]
- 68.Croxford S, Platt L, Hope VD, Cullen KJ, Parry JV, Ncube F. Sex work amongst people who inject drugs in England, Wales and Northern Ireland: findings from a National Survey of Health Harms and Behaviours. Int J Drug Policy. 2015;26(4):429–33. [DOI] [PubMed] [Google Scholar]
- 69.Girchenko P, King EJ. Correlates of double risk of HIV acquisition and transmission among women who inject drugs in St. Petersburg, Russia. AIDS Behav. 2017;21(4):1054–8. [DOI] [PubMed] [Google Scholar]
- 70.Park JN, Footer KHA, Decker MR, Tomko C, Allen ST, Galai N, et al. Interpersonal and structural factors associated with receptive syringe-sharing among a prospective cohort of female sex workers who inject drugs. Addict Abingdon Engl. 2019;114(7):1204–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Adelekan AL, Omoregie PI, Edoni ER. Sexual practices of female sex workers who inject drugs in Osogbo, Nigeria. Int Sch Res Not. 2014;2014. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4897494/(cited 1 Oct 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wirtz AL, Peryshkina A, Mogilniy V, Beyrer C, Decker MR. Current and recent drug use intensifies sexual and structural HIV risk outcomes among female sex workers in the Russian Federation. Int J Drug Policy. 2015;26(8):755–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Biello KB, Bazzi AR, Mimiaga MJ, Biancarelli DL, Edeza A, Salhaney P, et al. Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm Reduct J. 2018;15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233595/(cited 1 Oct 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Allen ST, O’Rourke A, White RH, Smith KC, Weir B, Lucas GM, et al. Barriers and facilitators to PrEP use among people who inject drugs in rural Appalachia: a qualitative study. AIDS Behav. 2020;24(6):1942–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schneider KE, White RH, O’Rourke A, Kilkenny ME, Perdue M, Sherman SG, et al. Awareness of and interest in oral pre-exposure prophylaxis (PrEP) for HIV prevention and interest in hypothetical forms of PrEP among people who inject drugs in rural West Virginia. AIDS Care. 2020;21:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Atujuna M, Newman PA, Wallace M, Eluhu M, Rubincam C, Brown B, et al. Contexts of vulnerability and the acceptability of new biomedical HIV prevention technologies among key populations in South Africa: a qualitative study. PLoS ONE. 2018;13(2):e0191251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Woodsong C, Alleman P. Sexual pleasure, gender power and microbicide acceptability in Zimbabwe and Malawi. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2008;20(2):171–87. [DOI] [PubMed] [Google Scholar]
- 78.Gafos M, Pool R, Mzimela MA, Ndlovu HB, McCormack S, Elford J. Communication about microbicide use between couples in KwaZulu-Natal, South Africa. AIDS Behav. 2015;19(5):832–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Robertson AM, Syvertsen JL, Martinez G, Rangel MG, Palinkas LA, Stockman JK, et al. Acceptability of vaginal microbicides among female sex workers and their intimate male partners in two Mexico–US border cities: a mixed methods analysis. Glob Public Health. 2013;8(5):619–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Giguere R, Frasca T, Dolezal C, Febo I, Cranston RD, Mayer K, et al. Acceptability of three novel HIV prevention methods among young male and transgender female sex workers in Puerto Rico. AIDS Behav. 2016;20(10):2192–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this manuscript are available from the corresponding author upon request.


