Abstract
Objective:
To study hydration plans and understanding of exercise-associated hyponatremia (EAH) among current marathon runners.
Design:
Cross-sectional study
Setting:
Southern California 2018 summer marathon
Participants:
210 marathon runners
Interventions:
Survey administered 1–2 days before the race. Race times were obtained from public race website.
Main Outcome Measures:
Planned frequency of hydration; awareness of, understanding of, and preventative strategies for dehydration and EAH; resources used to create hydration plans; drink preferences
Results:
When the participants were split into 3 equal groups by racing speed, the slower tertile intended to drink at every mile/station (60%) while the faster tertile preferred to drink every other mile or less often (60%), though not statistically significant. Most runners (84%) claimed awareness of EAH, but only 32% could list a symptom of the condition. Both experienced marathoners and the faster tertile significantly had greater understanding of hyponatremia compared to first-time marathoners and the slower tertile, respectively. Less than 5% of marathoners offered “drink to thirst” as a prevention strategy for either dehydration or EAH.
Conclusion:
Slower runners plan to drink larger volumes compared to their faster counterparts. Both slower and first-time marathoners significantly lacked understanding of EAH. These groups have plans and knowledge that may put them at higher risk for developing EAH. Most marathon runners did not know of the guidelines to “drink to thirst,” suggesting the 2015 EAH Consensus statement may not have had the desired impact.
Keywords: exercise-associated hyponatremia, thirst, education, dehydration, running
INTRODUCTION
In recent years, marathon running has increased in popularity. In 2018, 781 marathons were held across the US with more than 500,000 finishing times recorded.1 Older guidance advised runners to drink as much as possible to avoid dehydration. As marathoners planned for constant consumption of fluids over the long race, studies estimate that over 10% of runners have some degree of exercise-associated hyponatremia (EAH) by the end of a marathon. 2 EAH is defined as a serum sodium level of less than 135 mmol/L during or after physical activity. Mild EAH can be associated with symptoms such as dizziness, nausea, confusion, seizures and altered mental status. Severe EAH can cause encephalopathy, pulmonary edema, and even death.3
While the pathophysiology of EAH is not completely understood, there are three categories of mechanisms believed to contribute: (1) excess fluid intake during exercise, (2) retention of water due to inappropriate secretion of ADH, and (3) abnormal movement of sodium from an osmotically inactive pool.4 Lack of conditioning can impact any or all of these.5 The primary risk factor implicated is excessive fluid intake and since it is the most readily modifiable of these factors, we have focused on it in our study.
Previous studies have reported that drinking more than 3–3.5L of fluid, weight gain during the race, long racing times, female sex, body mass index (BMI) extremes, and use of non-steroidal anti-inflammatory drugs (NSAIDs) are associated with EAH.6,7,8 Inadequate understanding of hyponatremia was identified as an issue in both experienced and non-experienced marathon runners.9,10
In 2015, the Third International EAH Consensus Development conference released a statement encouraging runners to “drink to thirst.” 11 Similar advice has been echoed by the 2019 Wilderness Medical Society guidelines. Since then, research specifically on marathon runners, their hydration strategies, and their knowledge of EAH has not been conducted.
In this study, we aimed to understand the race hydration strategies of current marathon runners. This included drink preferences. what resources were used in creating these strategies, and whether these strategies were related to racing speed. We also evaluated current runners’ knowledge of EAH. We hypothesized that non-first-time runners and faster marathon runners would plan to hydrate less frequently. We expected that their choice of hydration would tend to be 100% water and water with electrolyte tablets, to avoid added sugars, based on personal previous experience to optimize their nutrition and performance over time. First time runners and slower runners, on the other hand, would be more likely to have a hydration plan involving excessive consumption of fluids, including sports drinks, based on peer recommendations and advertisements to stay hydrated at every opportunity during the race. Given the emphasis on preventing dehydration among runners, we believe both groups were less likely to understand the symptoms of EAH compared to dehydration or have the prevention strategy to “drink to thirst.”
METHODS
We recruited marathon runners at the pre-race exposition one and two days before a Southern California marathon in summer 2018. All runners were required by marathon organizers to be 18 years or older and to pick up their race bib number at the expo without exception. There were no exclusion criteria. Posters advertising the study were set up outside the expo. Members of the research team invited runners to participate as they were leaving the bib pick-up area.
The pre-marathon survey (Supplement Survey) consisted of 33 questions regarding demographics, training, hydration plan, drink preferences, resources used, hydration beliefs, and knowledge of EAH and dehydration. This survey was based on previous studies2,7,10 with a new section for hydration knowledge. In understanding participants’ fluid intake plans, we asked runners to estimate frequency and amounts of planned fluid intake as well as their fluid preferences from the choices of sports drinks, 100% water, water with added electrolytes, and coconut water. For resources used, we asked runners what they referenced in creation of their hydration plan from a list that included prior experiences, books/magazines, scientific research/journals, commercials/ads, online/internet search, YouTube, word of mouth/other runners, and coach.
For the knowledge of hydration disorders section, runners were asked to respond “Yes/No/Don’t know” if they were aware of the conditions of “hyponatremia/water overload/water intoxication” and “dehydration”. Two free response questions followed, which required runners to write-in symptoms of “hyponatremia/water overload/water intoxication” and “dehydration” to check for understanding and knowledge of these conditions. We validated answers using the current consensus in the medical literature.3,12 Knowledge or understanding was determined as ability to list at least one of the correct symptoms of the respective conditions. We deliberately designed our final strategy questions regarding prevention of hydration disorders to be free response in hopes of eliciting the participants’ own input rather than offering “drink to thirst” as an option. The runners took the survey in either identical digital or paper format. Bib numbers of each runner were noted to allow access to publicly available race time data after the marathon.
Initially as a surrogate for risk of developing hyponatremia, we had planned to collect participant weights before and after the race. All participants were weighed on digital scales at the time of survey for pre-race weights, but we were unable to collect all the post-race weights at the finish line due to a safety threat that forced the research team to evacuate. The race resumed after a delay and finishing times were adjusted by officials. Due to incomplete collection of the weight data, we were unable to finish this part of the analysis.
We analyzed the participants’ hydration plans and knowledge of hyponatremia and dehydration through dividing the cohort by speed as well as by racing experience. For racing experience, we compared the participants by those who had never run a marathon and those who had run one or more. We also examined the demographics, resources, and plans of runners divided by knowledge: those who knew only about dehydration, both EAH and dehydration, and neither. The BMI was calculated using reported weight and height using the following formula: weight (lbs) / [height (in)]2 × 703. The study qualified for UCSD IRB-exempt status as it did not collect any personal health information (PHI) and race times were pulled from a publicly available database.
We reported participant responses to the survey categorized by finish times and compared the variables using chi-square tests for categorical and discrete variables and ANOVA for continuous variables. SAS version 9.4, SAS enterprise version 7.1, and JMP Version 15.2 were used to perform the analysis and a p-value <0.05 was considered statistically significant.
RESULTS
Baseline characteristics:
We enrolled 210 marathon runners, 133 men and 77 women with mean (SD) age of 40 (11). Table 1 shows the 210 enrolled runners, divided into tertiles by race times. Those who were in the faster tertile had significantly lower BMI and tended to have less health co-morbidities, run marathons previously, and trained specifically for this marathon for less time compared to the slower tertile. NSAID use in the past week was lower, but not significantly, in faster runners.
Table 1.
Baseline characteristics of marathon participants across tertiles of race times.
| Race Times: | Slower Tertile | Middle Tertile | Faster Tertile | p-value |
|---|---|---|---|---|
| Number of runners | 68 | 69 | 68 | |
| Average race time (SD in minutes) | 6 hrs, 17 min (32) | 5 hrs, 13 min (23) | 3 hrs, 51 min (23) | |
| Age | 41.6 (11) | 39.6 (11) | 37.3 (10) | 0.06 |
| Gender (% male) | 50% | 68% | 69% | 0.03 |
| Ethnicity | 0.40 | |||
| White | 52% | 42% | 57% | |
| Black | 6% | 6% | 0% | |
| Hispanic | 24% | 29% | 29% | |
| Asian | 15% | 16% | 9% | |
| Other | 4% | 7% | 4% | |
| Body-mass index | 25.7 (3.8) | 24.2 (2.9) | 22.8 (2.8) | <0.0001 |
| Previous marathons ever | 47% | 64% | 74% | 0.01 |
| Previous marathons | 0.01 | |||
| 0 | 53% | 36% | 26% | |
| 1 to 5 | 24% | 35% | 26% | |
| > 5 | 24% | 29% | 47% | |
| Training period | 0.06 | |||
| 0 | 7% | 6% | 5% | |
| 1 to 3 months | 15% | 31% | 38% | |
| > 3 months | 78% | 63% | 58% | |
| Reason for running | ||||
| Fun | 79% | 71% | 65% | 0.16 |
| Fitness | 71% | 72% | 68% | 0.82 |
| charity | 16% | 9% | 4% | 0.06 |
| recreational | 25% | 28% | 44% | 0.03 |
| competition | 7% | 13% | 28% | 0.00 |
| Past Medical History | ||||
| hypertension | 10% | 3% | 7% | 0.22 |
| arthritis | 22% | 13% | 4% | 0.01 |
| asthma or COPD | 3% | 1% | 0% | 0.36 |
| Other | 3% | 0% | 1% | 0.36 |
| Prior injuries | 12% | 9% | 13% | 0.69 |
| NSAIDS in last week | 50% | 32% | 34% | 0.06 |
| Prescription Medications | 26% | 16% | 13% | 0.11 |
| Supplements | 44% | 28% | 31% | 0.10 |
| Fuel during Race | ||||
| “Gu” gels | 80% | 81% | 93% | 0.07 |
| Bars | 30% | 19% | 16% | 0.21 |
| nothing | 7% | 9% | 1% | 0.16 |
| Other | 18% | 16% | 9% | 0.29 |
| Caffeine on Race Morning | 50% | 43% | 57% | 0.26 |
| Alcohol in Last Week | 50% | 54% | 57% | 0.69 |
| Part of Running Club | 70% | 77% | 75% | 0.57 |
| Physician Consult Prior to Race | 31% | 19% | 15% | 0.06 |
Hydration planning:
Table 2 displays the hydration plans of the runners, divided by race times. Most runners across all groups claimed to have hydration plans for the race. The faster tertile relied significantly on scientific journals to create their hydration plan in comparison to the rest of the group. While not statistically significant, 60% of slower runners favored drinking every mile/station while 60% of faster runners planned to drink every other mile or less frequently. When asked what amount of fluids a theoretical marathon runner needed to consume at minimum, the slower tertile significantly believed in a greater baseline amount than the faster and middle tertiles.
Table 2.
Hydration plan of marathon participants across tertiles of race times.
| Race Times: | Slower Tertile | Middle Tertile | Faster Tertile | p-value |
|---|---|---|---|---|
| Number of Runners | 68 | 69 | 68 | |
| Have a hydration plan (Y/N) | 70% | 62% | 79% | 0.09 |
| Resources for Hydration Plan Creation | ||||
| prior experience | 71% | 77% | 84% | 0.19 |
| books, magazines | 21% | 13% | 16% | 0.49 |
| science | 7% | 12% | 25% | 0.01 |
| Ads | 3% | 3% | 1% | 0.82 |
| Web | 32% | 28% | 24% | 0.52 |
| word of mouth | 35% | 38% | 25% | 0.24 |
| YouTube | 3% | 3% | 3% | 1.00 |
| coach | 18% | 22% | 20% | 0.83 |
| other | 7% | 7% | 6% | 0.93 |
| Drink Type | ||||
| sports | 63% | 59% | 57% | 0.78 |
| 100% water | 65% | 77% | 57% | 0.05 |
| H2O + electrolytes | 49% | 48% | 53% | 0.81 |
| coconut water | 10% | 13% | 4% | 0.21 |
| other | 10% | 4% | 7% | 0.41 |
| Hydration Frequency during race | 0.07 | |||
| every mile/station | 60% | 36% | 40% | |
| every other mile | 21% | 33% | 31% | |
| every third mile/less often | 19% | 30% | 29% | |
| Checking hydration status during race | ||||
| thirst | 75% | 61% | 51% | 0.02 |
| urine | 57% | 45% | 47% | 0.30 |
| feel | 62% | 75% | 62% | 0.15 |
| skin changes | 7% | 6% | 13% | 0.27 |
| no idea | 4% | 1% | 15% | 0.44 |
| other | 3% | 4% | 10% | 0.15 |
Knowledge of water overload and dehydration:
Table 3 shows the knowledge and understanding of dehydration and EAH in marathon runners, divided by race times. The majority of participants (>90%) reported that they had heard of dehydration. When asked to list a symptom of dehydration, approximately 70% of participants wrote in at least one symptom (e.g., dizziness, nausea, fatigue, cramps). Similar to the awareness of dehydration, >80% of participants reported they were aware of “hyponatremia/water overload/water intoxication”. However, when asked to write in at least one symptom (e.g., nausea, confusion, seizures), only 34% of total participants were able to list an answer. Out of the participants who wrote in at least one symptom of EAH, the faster runners demonstrated understanding more frequently, with 41% of the faster runners able to list at least one symptom compared to the other two groups (32%, 22%).
Table 3.
Knowledge of EAH and dehydration across race time tertiles.
| Race Times: | Slower Tertile | Middle Tertile | Faster Tertile | p-value |
|---|---|---|---|---|
| Number of Runners | 68 | 69 | 68 | |
| EAH, water overload, water intoxication: | ||||
| Awareness | 81% | 83% | 88% | 0.47 |
| Symptoms | 32% | 22% | 41% | 0.05 |
| mild | 26% | 20% | 43% | 0.01 |
| moderate | 7% | 7% | 4% | 0.73 |
| severe | 3% | 1% | 1% | 0.77 |
| Prevent via salt ingestion | 21% | 10% | 18% | 0.23 |
| Prevent via drink strategy modification | 38% | 29% | 34% | 0.52 |
| Prevent with “drink to thirst” | 0% | 3% | 3% | 0.36 |
| Dehydration: | ||||
| Awareness | 97% | 91% | 96% | 0.32 |
| Symptoms | 65% | 75% | 74% | 0.34 |
| Prevent via drink strategy modification | 87% | 88% | 81% | 0.43 |
| Prevent with “drink to thirst” | 0% | 3% | 4% | 0.24 |
When asked how to prevent dehydration, many runners wrote in to “drink more fluids” and when asked how to prevent EAH, countered with “drink less fluids.” Only 4 runners (2 in the faster tertile and 2 in the middle tertile) wrote to prevent EAH by “drink[ing] to thirst.” No runners in the slower tertile listed “drink to thirst” as a prevention strategy.
First Time vs Experienced Marathon Runners
In addition to comparing runners by finishing times, we compared marathon runners’ hydration plans and knowledge of EAH by racing experience (first time vs. non-first time).
Greater than 50% of the experienced runners had run at least 5 marathons previously, with 20% having run more than 10 marathons. Experienced runners were significantly more likely to have a hydration plan and significantly use both previous experience and scientific journals in creating it. First-time runners, on the other hand, were significantly more likely to reference the internet in creating their hydration plan. Experienced marathoners reported significant investment in recreational racing or competition lifestyle while first-time marathoners were significantly more likely to be in a running club (supplemental Table S1).
Comparing both groups, the runners displayed no significant differences in drink type preference or in planned frequency of hydration. More first-time marathoners significantly claimed to check thirst (73%) as a reflection of hydration status than experienced marathoners (55%) (supplemental Table S2).
Experienced marathoners were significantly more knowledgeable about mild hyponatremia symptoms (35%) compared to first-time runners (22%). Only a few more experienced marathoners versus first time marathoners responded with “drink to thirst” for prevention strategies for EAH (3 vs. 1) and dehydration (6 vs. 2) respectively (supplemental Table S3).
Knowledge of Dehydration & EAH
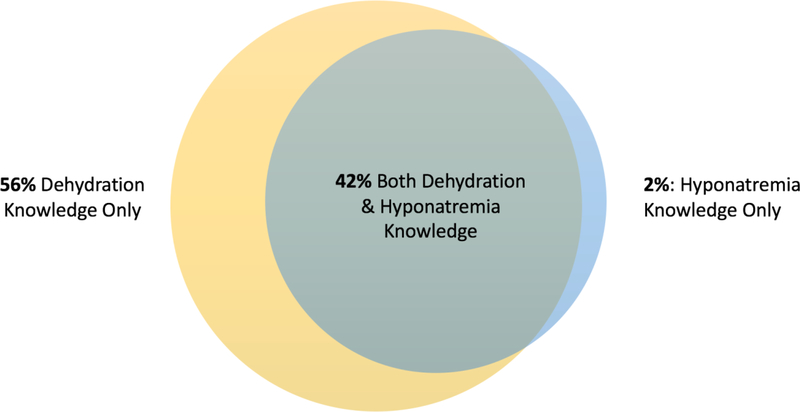
In order to understand to whom education on EAH would be best targeted, we compared the hydration plans between those who proved to have accurate knowledge of the symptoms of both EAH and dehydration versus knowledge of just dehydration symptoms versus knowledge of neither (Figure 1). Only 3 runners claimed to have knowledge of only hyponatremia, so they were excluded from this specific analysis.
Figure 1.
Knowledge of Dehydration and EAH among 152 participants. 58 participants (28% of total) had knowledge of neither dehydration nor EAH.
Those with knowledge of both dehydration and EAH had significantly more marathon experience and significantly used scientific journals and articles to inform their hydration plans compared to the other two groups (supplemental Table S4). Those with knowledge of only dehydration significantly relied on word of mouth from other runners as a resource in contrast to the other two groups. Runners with knowledge of neither preferred, but not significantly, the internet in creation of their hydration plan.
Women
As female sex is a known risk factor for developing EAH and the women were on average significantly slower compared to the men (5 hrs vs 6 hrs 24 min), we performed a subset analysis of the 77 women in the study by creating tertiles by the women’s racing speed. (supplemental Table S5, Table S6, and Table S7).
In comparing these three groups of women, the faster tertile was significantly lighter than slower tertile. There was a trend of more marathon experience with faster female runners, though not significant. No significant differences were found in resources used to create hydration plans. Women in the slower tertile planned to consume more fluids during the race compared to their faster counterparts. Similarly, when asked about the minimum amount of fluids a marathoner should drink during the marathon, women in the slower tertile significantly expected runners to drink more at a minimum. There were no significant differences in drink preference, with the most popular choice (>65% in each tertile) being 100% water across the groups (supplemental Table S6). The faster tertile (69%) significantly claimed to check their hydration status via urine color compared to the other two tertiles. Faster women were also significantly able to name the subset of moderate symptoms of EAH compared to their slower counterparts. No women stated to drink to thirst for EAH prevention.
DISCUSSION
We surveyed how current marathoners hydrate and found that slower runners had strategies that involved more frequent hydration. Regarding creation of their hydration plans, faster runners relied significantly on scientific studies compared to slower runners and first-time runners significantly used the internet in comparison to their experienced counterparts. Both faster and experienced runners significantly expressed greater knowledge and understanding of EAH compared to slower and first-time runners respectively. These findings suggest that slower and less experienced runners may be at a higher risk of developing EAH. Above all, more than 95% of runners in this study did not use “drink to thirst” as an effective prevention strategy to combat dehydration and EAH. To our knowledge, this is the first such study done after the 2015 EAH consensus conference promulgation regarding cautious hydration and knowledge.
Our investigation of drink preferences failed to show significant differences across participants regardless of speed or experience. Since most fluid replacement options are hypotonic, they remain inadequate replacement for solute loss during the race. Rather, the volume of fluid and planned frequent hydration combined with lack of knowledge about EAH can potentially endanger slower and first-time runners. A study at the 2002 Boston Marathon2 showed that individuals who drink every mile or station and those who drink more than 3L of fluid are more likely to develop EAH. At the 2016 London Marathon, change in serum sodium was inversely correlated with change in body mass and estimated fluid intake.13 Previous studies have shown concern that NSAIDs can increase the risk of developing EAH.8 In our study, while not significant, we found that slower, first time runners used more NSAIDs within the week leading up to marathon when compared to their faster counterparts.
As for knowledge of EAH, a 2010 London Marathon 9 study concluded that 65% of runners were aware of hyponatremia, with about half (35%) able to list the cause and effects.9 A follow up 2014 London marathon study showed comparable numbers, with 63.8% of runners claiming awareness of hyponatremia and 40% of total runners able to demonstrate basic understanding.14 Both these studies were conducted before the 2015 EAH consensus statement. In our study, we found 84% of runners reporting they had heard of hyponatremia/water intoxication/water overload but only 32% of the total group, a comparable percentage found in the London marathon studies, able to list symptoms. While awareness of EAH may have increased in the last decade, we observed no change in understanding.
We expected and found that most of the runners did not know to “drink to thirst.” However, slower runners and first-time runners surprised us by significantly reporting to check hydration status by thirst. Still, runners in this group planned frequent hydration during the race and did not list “drink to thirst” as a general hydration strategy. Yet, if less experienced, slower runners recognize their hydration status by thirst, the broad education of the message “drink to thirst” may be effective in translating a natural instinct to optimal hydration actions. Experienced marathoners were more cognizant of the risks of EAH and planned less frequent fluid intake, informed mostly by personal running experience. Only a few non-first-time marathoners knew to “drink to thirst.” Overall, few runners across the range of speed and experience spontaneously generated “drink to thirst” as a hydration strategy, signifying a need for high quality safety and hydration education. Further research regarding the impact of conditioning to sensitivity of disorders of water balance is also indicated.
Limitations of our study include self-reporting bias with surveys, lack of blood tests to confirm EAH or dehydration, and inability to complete the originally planned weight analysis. Of note, while the current guidance is “drink to thirst,” there is no data that proves this advice helps combat hydration disorders. Our study’s strengths lie in a current understanding of runners’ hydration plans and a novel connection between hydration strategies to actual race times and knowledge of dehydration and EAH. Although we recruited a convenience sample at the pre-race bib pick up area, our runners required no qualification time to race, making the sample more likely to be representative of a general marathon runner population. Our study is one of the few in the literature that studied a non-elite marathon population.
This study demonstrates that the 2015 EAH Consensus guidelines to “drink to thirst” may not yet have had the intended impact on knowledge. Looking ahead, as marathon running continues to grow in popularity, a focus should be placed on tailoring effective educational interventions especially for high-risk groups.
Supplementary Material
Acknowledgements:
The authors would like to thank the athletes that volunteered for this study, fellow colleagues Shruti Dubey, Mary Gamboa, Victoria Speck, Michael Paap, and Kilian Burke who assisted in recruitment, and the marathon race organizers who helped with logistics.
Conflicts of Interest and Source of Funding:
Neeharika Namineni received the UAB-UCSD O’Brien Grant for Summer Research. The other authors have no conflicts of interest to declare.
Footnotes
Ethics Approval:
This study was conducted with the approval of the Institutional Review Board, University of California San Diego, La Jolla, CA, USA.
REFERENCES
- 1.Marathon Statistics. FindMyMarathon.com.
- 2.Almond CSD, Shin AY, Fortescue EB, et al. Hyponatremia among runners in the Boston Marathon. N Engl J Med. 2005;352(15):1550–1556. doi: 10.1056/NEJMoa043901 [DOI] [PubMed] [Google Scholar]
- 3.Hew-Butler T, Loi V, Pani A, Rosner MH. Exercise-Associated Hyponatremia: 2017 Update. Front Med. 2017;4. doi: 10.3389/fmed.2017.00021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Noakes TD, Sharwood K, Speedy D, et al. Three independent biological mechanisms cause exercise-associated hyponatremia: evidence from 2,135 weighed competitive athletic performances. Proc Natl Acad Sci U S A. 2005;102(51):18550–18555. doi: 10.1073/pnas.0509096102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shibasaki M, Wilson TE, Crandall CG. Neural control and mechanisms of eccrine sweating during heat stress and exercise. J Appl Physiol Bethesda Md 1985. 2006;100(5):1692–1701. doi: 10.1152/japplphysiol.01124.2005 [DOI] [PubMed] [Google Scholar]
- 6.Küster M, Renner B, Oppel P, Niederweis U, Brune K. Consumption of analgesics before a marathon and the incidence of cardiovascular, gastrointestinal and renal problems: a cohort study. BMJ Open. 2013;3(4). doi: 10.1136/bmjopen-2012-002090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winger JM, Dugas JP, Dugas LR. Beliefs about hydration and physiology drive drinking behaviours in runners. Br J Sports Med. 2011;45(8):646–649. doi: 10.1136/bjsm.2010.075275 [DOI] [PubMed] [Google Scholar]
- 8.Whatmough S, Mears S, Kipps C. Serum sodium changes in marathon participants who use NSAIDs. BMJ Open Sport Exerc Med. 2018;4(1):e000364. doi: 10.1136/bmjsem-2018-000364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams J, Tzortziou Brown V, Malliaras P, Perry M, Kipps C. Hydration strategies of runners in the London Marathon. Clin J Sport Med Off J Can Acad Sport Med. 2012;22(2):152–156. doi: 10.1097/JSM.0b013e3182364c45 [DOI] [PubMed] [Google Scholar]
- 10.O’Neal EK, Wingo JE, Richardson MT, Leeper JD, Neggers YH, Bishop PA. Half-marathon and full-marathon runners’ hydration practices and perceptions. J Athl Train. 2011;46(6):581–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hew-Butler T, Rosner MH, Fowkes-Godek S, et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin J Sport Med Off J Can Acad Sport Med. 2015;25(4):303–320. doi: 10.1097/JSM.0000000000000221 [DOI] [PubMed] [Google Scholar]
- 12.Shaheen NA, Alqahtani AA, Assiri H, Alkhodair R, Hussein MA. Public knowledge of dehydration and fluid intake practices: variation by participants’ characteristics. BMC Public Health. 2018;18. doi: 10.1186/s12889-018-6252-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whatmough S, Mears S, Kipps C. Exercise Associated Hyponatremia (EAH) and Fluid Intake During the 2016 London Marathon. Br J Sports Med. 2017;51(4):409.1–409. doi: 10.1136/bjsports-2016-097372.316 [DOI] [Google Scholar]
- 14.Leggett T, Williams J, Daly C, Kipps C, Twycross-Lewis R. Intended Hydration Strategies and Knowledge of Exercise-Associated Hyponatraemia in Marathon Runners: A Questionnaire-Based Study. J Athl Train. 2018;53(7):696–702. doi: 10.4085/1062-6050-125-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson PB. Nutrition behaviors, perceptions, and beliefs of recent marathon finishers. Phys Sportsmed. 2016;44(3):242–251. doi: 10.1080/00913847.2016.1177477 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.