Abstract
Background
Irritable bowel syndrome (IBS) has become a common public health issue among university students, impairing their physical and mental health. This meta-analysis aimed to examine the pooled prevalence of IBS and its associated factors among Chinese university students.
Methods
Databases of PubMed, EMBASE, MEDLINE (via EBSCO), CINAHL (via EBSCO), Wan Fang, CNKI and Weipu (via VIP) were systematically searched from inception date to May 31, 2021. Meta-analysis was performed using random-effects models. Meta-regression and subgroup analysis were used to detect the potential source of heterogeneity.
Key Results
A total of 22 cross-sectional studies (14 were in Chinese and 8 were in English) with 33,166 Chinese university students were included. The pooled prevalence of IBS was estimated as 11.89% (95% CI = 8.06%, 16.35%). The prevalence was 10.50% (95% CI = 6.80%, 15.87%) in Rome II criteria, 12.00% (95% CI = 8.23%, 17.17%) in Rome III criteria, and 3.66% (95% CI = 2.01%, 6.60%) in Rome IV criteria. The highest prevalence of IBS was 17.66% (95% CI = 7.37%, 36.64%) in North China, and the lowest was 3.18% (95% CI = 1.28%, 7.68%) in South China. Subgroup analyses indicated that gender, major, anxiety and depression symptoms, drinking and smoking behaviors were significantly associated with the prevalence of IBS. Meta-regression analyses suggested that region influenced prevalence estimates for IBS.
Conclusions and Inferences
This meta-analysis illustrated that IBS is very common in Chinese university students. Regular screening, effective prevention, and appropriate treatments should be implemented to reduce the risk of IBS in this population. More future studies should be conducted in Northeastern and Southwestern parts of China.
Keywords: irritable bowel syndrome, prevalence, associated factors, Chinese university students, meta-analysis
Introduction
Irritable bowel syndrome (IBS) is a chronic functional gastrointestinal disease characterized by altered bowel habits, abdominal discomfort or pain, and abdominal distension, without obvious structural or biochemical abnormalities (1) or organic etiology (2). A meta-analysis with 23 studies (n = 74,763) revealed that the prevalence of IBS was 6.5% in the general population in China (3). Though the pathophysiology is still unclear, IBS has been proved to be associated with multiple factors including abnormal gastrointestinal motility, visceral sensory abnormality, abnormal brain-gut regulation, inflammation, gastrointestinal infection, and stressful life events, etc. (4–6). Furthermore, recent evidences supported the negative psycho-influences to be the key role of the biopsychosocial model of IBS (4, 7–9). For instance, a meta-analysis showed the high rates of anxiety symptoms (39.1%) and disorders (23%), depression symptoms (28.8%) and disorders (23.3%) in IBS patients (10). Throughout the years, various criteria including the Manning criteria, the Rome I, Rome II, Rome III and Rome IV criteria, have been applied for diagnosis of IBS. Amongst them, the Rome III criteria (11) and Rome IV criteria (12) are the most commonly used currently.
University students are more likely to experience IBS–varied from 1.18% (13) to 33.3% (14) in China, might due to the psychological problems, unhealthy lifestyles, and a low level of health literacy (15). For instance, they are more prone to suffer from anxiety and depression symptoms, because of difficulties in terms of academic pressures, occupational choices, interpersonal conflict, and life goal decisions (16), which could cause gastrointestinal disorders through the brain-gut axis mechanism (17). A lack of physical exercise, irregular eating habits (i.e., not having breakfast), smoking, and drinking behaviors have also been found common in university students (18), which may contribute to the risk of IBS in this population. Moreover, due to various clinical examinations and constant medical treatment, IBS has been proved to be linked to physical problems like headache, chronic back or neck pain and diabetes (19), mental disorders like anxiety and depression (20) and obsessive-compulsiveness (21), sleep disorder (22), poorer academic achievements (23), lower quality of life (24, 25), social embarrassment due to diarrhea (a symptom of IBS) which restricts the patients being near a bathroom (26), and higher economic cost (24).
There has been a growing number of studies on IBS in Chinese university students, but the prevalence of IBS varied widely in existing studies. Precise epidemiological figures related to IBS prevalence are fundamental to inform preventive strategies in an evidence-based way. This study aimed to quantitatively evaluate the prevalence of IBS and its associated factors among Chinese university students via systematic review and meta-analysis.
Materials and Methods
Search Strategy and Selection Criteria
This study was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) Statement (27) and Meta-analyses Observational Studies in Epidemiology (MOOSE) guidelines (28). A systematic search was conducted in both English (PubMed, EMBASE, MEDLINE via EBSCO, CINAHL via EBSCO) and Chinese databases (Wan Fang, CNKI, Weipu via VIP) from their inception date to May 31, 2021. The searching terms were followed: (((Irritable OR spastic OR Mucous) AND (bowel OR colon OR colonic OR gastrointestinal)) OR IBS) AND (China OR Chinese OR mainland China OR Hong Kong OR Macau OR Macao OR Taiwan) AND (College OR University OR undergrad*). The search strategies in different databases were provided in Supplementary Table 1. The cited references of the identified publications were also searched manually to ascertain additional studies that may have been missed. The corresponding author would be contacted to get the essential information if needed.
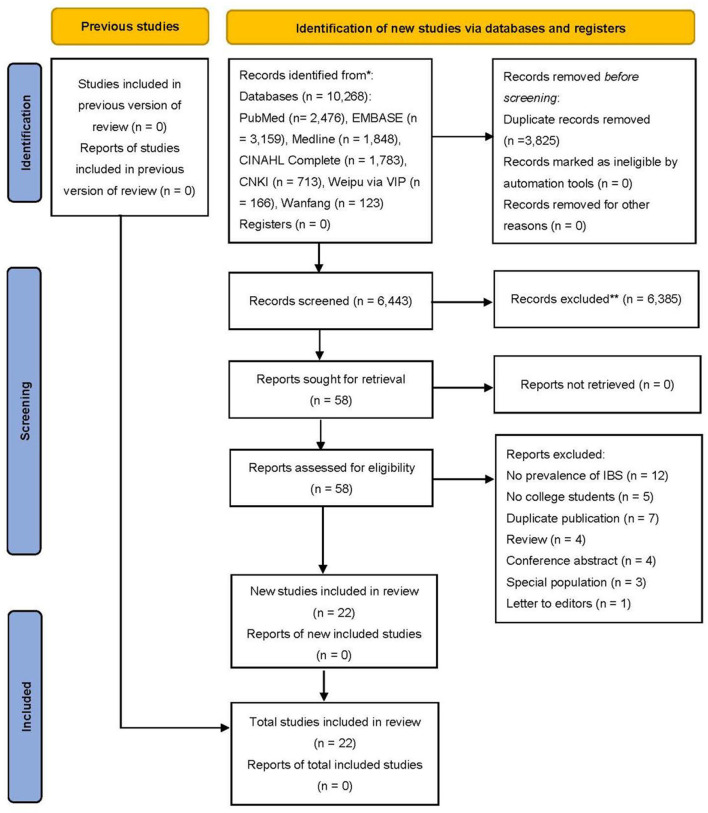
The titles and abstracts were initially screened and those that were obviously irrelevant were excluded. The full texts of the remaining articles were reviewed to find relevant studies that were finally included. The selection above was performed by two researchers (WX Yang and X Yang) independently and any discrepancies were resolved by discussing with the senior researcher (XH Cai). Figure 1 detailed the process of screening articles.
Figure 1.
PRISMA flow chart of literature search and article selection process.
Studies were included if they met the following criteria: (1) original studies including cross-sectional and cohort studies; (2) participants should be full-time undergraduate students, junior college students, or postgraduates in China (including Hong Kong, Macao, and Taiwan); (3) reporting the prevalence of IBS with diagnostic criteria based on validated questionnaires or scales according to Manning or Rome criteria or International Classification of Diseases codes; (4) studies recruiting at least 50 subjects; (5) accessible full texts in English or Chinese. We excluded studies if they met the following criteria: (1) studies focused on special populations with medical conditions like gastritis or hepatitis; (2) studies without the prevalence of IBS reported; (3) full-texts not being available. If two or more papers were published based on the same dataset, only the one with the most complete information was included.
Data Analysis
We used the “Checklist for Prevalence Studies” developed by the Joanna Briggs Institute for quality assessment (29, 30). The checklist consists of nine items, including (1) appropriate sampling frame, (2) appropriate sampling design, (3) adequate sample size, (4) detailed description of study subjects and setting, (5) sufficient coverage of sample, (6) valid methods for identifying the condition, (7) standard and reliable measurement of the condition (8) appropriate statistical analysis, and (9) adequate response rate. Each item was rated as either “yes”, “no”, “unclear”, or “not applicable”. Only the “yes” answer for each item receives a score of 1. Thus, final scores for each study could range from 0 to 9. Study quality was assessed by two researchers (WX Yang and X Yang) independently and any discrepancies were resolved by discussing with a third researcher (XH Cai).
Two researchers (WX Yang and X Yang) independently conducted data extraction, and any inconsistencies in the process were checked and resolved by involving a third investigator (XH Cai). The following information was extracted and tabulated: author, year of publication, sample characteristics {gender[Male/Female (M/F)], age [Mean ± Standard Deviation(SD)], grade, majors, educational level}, survey year, survey province, survey region, sampling method, total subjects, subjects with IBS, the prevalence of IBS, diagnostic criteria of IBS, subgroups, risk factors, and other significant results. Seven regions were identified in China, as shown in Supplementary Data 1. Majors were classified into “medicine” (clinical medicine, nursing, and health-related specialties set in the medical university), “non-medicine” or “mixed”. “Mixed” was defined as a mixture of different majors, which could not extract the specific major data in the paper. Only Rome III prevalence data was extracted if the study contained both Rome II and Rome III criteria.
The pooled prevalence of IBS was calculated as effect size (ES). Given the prevalence of IBS in most included studies (ranging from 0 to 20%) was close to the margins, the variance-stabilizing Freeman-Tukey double arcsine transformation was used to combine rates (31). Raw prevalence estimation was transformed and then multiple meta-analyses were performed with the transformed proportions using the random-effects model. These were then back-transformed to prevalence rates to facilitate interpretation of the outcomes and confidence interval (CI) (32). The I2 statistic was used to assess heterogeneity between the studies (low: I2 <25%, moderate: 25–50%, high: I2 > 50%) (33, 34). The funnel plot and Begg's test (35) were conducted to explore publication bias when there were at least 10 studies in the meta-analysis (36). The “metaninf ” command was used for sensitivity analysis via evaluating the effect of each study on overall estimates.
Subgroup analyses were conducted to examine the possible sources of heterogeneity according to the following categorical variables: (1) educational level: junior college vs. undergraduate vs. postgraduate; (2) gender: female vs. male; (3) majors: medicine vs. non-medicine vs. mixed; (4) regions: Central China vs. East China vs. North China vs. Northwest China vs. South China; (5) survey year: 2005–2010 vs. > 2010; (6) criteria: Rome II vs. Rome III vs. Rome IV; (7) anxiety: yes vs. no; (8) depression: yes vs. no; (9) drinking: yes vs. no; and (10) smoking: yes vs. no. To identify the factors associated with the prevalence of IBS in Chinese university students, pooled odd ratios (ORs) for potential influencing factors were calculated with a random-effects model.
Univariate meta-regression was performed to identify sources of between-study heterogeneity according to the following variables: educational level, gender ratio (M/F), major, region, survey year, criteria, anxiety proportion, depression proportion, drinking proportion, smoking proportion, and quality score. The significance level was set at p < 0.05 (two-tailed) for all analyses.
The Stata 14.0 (Stata Corporation, College Station, TX, USA) and Comprehensive Meta-Analysis Version 2.0 (Biostat, Inc., Englewood, New Jersey, USA) were administered to synthesize data.
Results
Study Characteristics
A total of 10,268 citations were initially searched in the databases, with 6,443 remaining after the removal of duplicates. After evaluating the title and/or abstract, 6,385 citations were removed for non-compliance with inclusion criteria. The full text of the remaining 58 citations was evaluated, and a total of 22 citations that met the criteria were included. Two citations with the same data were both included due to the different content in subgroup analyses and significant results, and the sample size of one citation was included when calculating the number of participants in this review. Finally, a total of 22 citations (14 in Chinese and 8 in English) with 33,166 Chinese university students were included in the analysis (Figure 1). All 22 studies reported the prevalence of IBS in university students, 20 reported risk factors for IBS, and 21 reported other significant results. A list of all included studies was presented in Supplementary Data 2. The characteristics of the study were summarized in Table 1.
Table 1.
Characteristics of included studies.
| References | Survey year | Region, province | Sampling method | Quality score | Criteria of IBS |
Gender (M/F) |
Age (mean ±SD) | Major | Educational level and grade | Total subjects | Prevalence (%) | Other significant results |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kong (37) | 2006 | East China, Shanghai | Random, stratified | 8 | Rome II | 155/158 | 23.48 ± 2.46 | Medicine | Undergraduate, postgraduate | 313 | 13.42 | • With the Rome II criteria, 8 cases were IBS-C (19.05%), 24 cases were IBS-D (57.14%), and 10 cases were IBS-M (23.81%). • Compared with the non-IBS group, scores of anxiety and depression were higher in the IBS group (p < 0.001). |
| Shen (38) | 2006 | Central China, Hubei | Stratified | 9 | Rome II | 166/165 | 24.69 ± 2.10 | Mixed | Undergraduate year 1, postgraduate year 1–2 | 331 | 15.4 | • IBS was detected in 19.7% of the non-medical professional group, and 10.5% of the medical professional group, with significant differences seen between groups (p = 0.022). • Compared with the non-IBS group, scores of anxiety and depression were higher in the IBS group. |
| Dai (39) | 2007 | East China, Zhejiang | Cluster | 9 | Rome II, Rome III | 517/604 | 21.8 ± 3.2 | Mixed | Undergraduate | 1,121 | 4.7 (Rome II), 10.4 (Rome III) | • With the Rome II criteria, 8 cases were c-IBS (14.81%), 12 cases were d-IBS (22.22%), and 34 cases were a-IBS (62.96%). With the Rome III criteria, 18 cases were IBS-C (14.63%), 30 cases were IBS-D (24.39%), 59 cases were IBS-M (47.97%), and 16 cases were IBS-U (13.01%). |
| Shen (5) | 2006 | Central China, Hubei | Stratified | 9 | Rome II | 241/250 | 24.13 ± 2.069 | Mixed | Undergraduate year 1 | 491 | 15.7 | • IBS was associated with anxiety (p < 0.001) and depression (p < 0.001). |
| Dong (40) | 2009 | East China, Shandong | Random | 9 | Rome II | 917/1209 | 20.64 ± 1.593 | Mixed | Undergraduate | 2,126 | 7.85 | • The IBS group scored higher in anxiety (p < 0.001), depression (p < 0.001) and lower in exercise frequency (p = 0.007) compared to the non-IBS group. • With the Rome III criteria, 61 cases were IBS-C (36.5%), 51 cases were IBS-D (31.1%), 40 cases were IBS-M (23.9%), and 25 were non-IBS cases (8.5%). |
| Liu (41) | 2009 | East China, Jiangxi | Cluster | 8 | Rome III | 392/568 | 19.68 ± 2.14 | Mixed | Junior college year 1–2 | 960 | 12.81 | • With the Rome III criteria, 58 cases were IBS-C (47.51%), 23 cases were IBS-D (18.34%), and 42 cases were IBS-M (34.25%). • IBS was associated with health-related majors (p < 0.01) and higher grade (p < 0.01). • Compared with the non-IBS group, the IBS group has a higher prevalence of anxiety and depression. |
| Shi (42) | 2008 | Central China, Henan | Cluster | 8 | Rome III | 414/1,520 | 19.7 ± 1.4 | Medicine | Undergraduate | 1,934 | 32.1 | • With the Rome III criteria, 203 cases were IBS-C (32.69%), 168 cases were IBS-D (27.05%), and 250 cases were IBS-M (40.26%). • Higher height (p = 0.018), shorter sleep time (p = 0.024) and weight loss (p < 0.001) were related to IBS in females. |
| Jiang (13) | / | South China, Guangdong | Stratified | 7 | Rome III | 161/178 | 20.12 ± 0.63 | Mixed | Junior college, undergraduate | 339 | 1.18 | • Mental factors were related to functional gastroenteropathy (p < 0.05). |
| Lin (43) | / | North China, Hebei | Stratified | 8 | Rome III | 388/1,370 | 18–24 (age range) | Medicine | Junior college, undergraduate | 1,758 | 8.99 | • IBS was associated with female (p = 0.049), educational level (p < 0.001), major (p = 0.026). |
| Wu (44) | 2011 | Central China, Hubei | Stratified | 6 | Rome III | 86/137 | 20.26 | Medicine | Undergraduate | 223 | 6.7 | • IBS was associated with lack of physical exercise (p = 0.035), spicy diet (p = 0.009), anxiety (p = 0.049), gastrointestinal infection (p = 0.002), antibiotics taking (p = 0.046), painkillers taking (p = 0.009), lack of amusement (p = 0.017) and parents having the same symptoms (p = 0.012). |
| Dong (45) | 2012 | East China, Shandong | Random | 9 | Rome III | 2,215/2,423 | 20.768 ± 1.509 | Mixed | Undergraduate | 4,638 | 8.34 | • IBS was associated with anxiety (p = 0.002) and depression (p = 0.045). • With the Rome III criteria, 150 cases were IBS-C (38.76%), 189 cases were IBS-D (48.84%), and 48 cases were IBS-M (12.40%). |
| Li (46) | 2010–2011 | East China, Zhejiang | / | 8 | Rome III | 967/903 | 21.34 ± 2.56 | Mixed | Undergraduate year 1–4, postgraduate year 1 | 1,870 | 6.9 | / |
| Liu (14) | 2014 | North China, Beijing | Stratified | 8 | Rome III | 196/571 | 23.26 ± 2.88 | Medicine | Undergraduate and postgraduate, year 1–7 | 767 | 33.3 | • For females, the IBS participants scored higher in anxiety (p = 0.015). • The IBS group scored higher in emotional neglect than the non-IBS group (p = 0.045). • Medical students with IBS scored higher on the PSQI than those without IBS (p < 0.001 in females, p = 0.014 in males). • With the Rome III criteria, 15 cases were IBS-C (5.88%), 79 cases were IBS-D (30.98%), 112 cases were IBS-M (43.92%), and 49 cases were IBS-U (19.22%). |
| Yang (47) | 2014 | North China, Beijing | Stratified, cluster | 7 | Rome III | 196/571 | 23.26 ± 2.88 | Medicine | Undergraduate and postgraduate, year 1–7 | 767 | 33.3 | • With the Rome III criteria, 15 cases were IBS-C (5.88%), 79 cases were IBS-D (30.98%), 112 cases were IBS-M (43.92%), and 49 cases were IBS-U (19.22%). • Compared with the non-IBS group, the score of the life stress questionnaire was higher in the IBS group (p < 0.05). |
| Zhang (48) | 2012–2013 | Northwest China, Xinjiang | Stratified | 9 | Rome III | 248/193 | 24.57 ± 2.02 | Mixed | Postgraduate year 1-3 | 441 | 11.56 | • IBS prevalence was higher in groups of females (p = 0.021), eating cold food frequency ≥ 3 times a week (p < 0.001), eating dairy product frequency ≥3 times a week (p = 0.001), eating high-fiber foods frequency <4 times a week (p = 0.011), physical activity time <4 h a week (p = 0.029), insomnia frequency ≥ 3 times a week (p < 0.001), anxiety (p = 0.013) and depression (p = 0.002). |
| Li (49) | 2015 | North China, Beijing | Stratified | 8 | Rome III | 425/282 | 20.28 ± 1.46 | Mixed | Undergraduate year 1–4 | 707 | 16.7 | • With the Rome III criteria, 16 cases were IBS-C (13.6%), 40 cases were IBS-D (33.9%), 54 cases were IBS-M (45.8%), and 8 cases were IBS-U (6.8%). • IBS was detected differently in females (20.2%) and males (14.4%, p = 0.041). • Compared to the healthy control group, participants in the IBS group reported higher scores of somatization symptom (p < 0.001), test anxiety (p = 0.026), negative life events (p = 0.002), and lower scores of physical symptoms and organ function (p < 0.001), psychological symptoms and negative emotions (p = 0.036), role activities and social adaptation (p = 0.008), social resources and social contact (p = 0.027) of SRHMS. • Gender, smoking, eating chilies, high physical-sensitive independently related to IBS. |
| Wang (50) | 2013 | Northwest China, Inner Mongolia | Stratified | 7 | Rome III | 1,667/4,438 | 21 ± 1.5 | Mixed mixed |
Undergraduate year 1–3 | 6,105 | 29.5 | • With the Rome III criteria, 364 cases were IBS-C (20.22%), 866 cases were IBS-D (48.11%), 322 cases were IBS-M (17.89%), and 248 cases were IBS-U (13.78%). • IBS was detected differently in females (31.3%) and males (24.8%, p < 0.001). • IBS was associated with lose weight (p < 0.001), anxiety (p < 0.001) and depression (p = 0.026). |
| Yang (51) | 2014–2015 | South China, Guangdong | Stratified | 7 | Rome III | / | / | Mixed | Undergraduate year 1–3 | 2,847 | 7.38 | • With the Rome III criteria, 76 cases were IBS-C (36.19%), 101 cases were IBS-D (48.10%), and 33 cases were IBS-M (15.71%). |
| Chen (52) | 2016 | East China, Shanghai | Stratified, cluster | 7 | Rome III | 0/468 | 19.60 ± 1.20 | Nursing | Junior college year 1–3 | 468 | 17.31 | • With the Rome III criteria, 43 cases were IBS-C (53.09%), 19 cases were IBS-D (23.46%), 14 cases were IBS-M (17.28%), and 5 cases were IBS-U (6.17%). • IBS was associated with spicy diet (p = 0.014), sleep disorder (p = 0.047) and lower grade (p = 0.008). |
| Liu (53) | 2019 | South China, Guangxi | Cluster | 8 | Rome IV | 593/2,033 | 19.22 ± 1.03 | Health related | Junior college year 1 | 2,626 | 2.7 | • IBS was associated with alcohol consumption (p = 0.021), dairy intake (p = 0.001), fatigue (p = 0.003), poor mood situation (p < 0.001) in healthy freshmen. |
| Chen (54) | 2016 | East China, Taiwan | Convenience | 7 | Rome III | 0/1,894 | 21.59 ± 1.40 | Medicine, non-medicine | Undergraduate year 2–4 | 1,894 | 10.1 | • Compared with the non-IBS female students, IBS female students had higher levels of stress and lower QoL. • IBS in females was associated with dysmenorrhea (p < 0.001), food avoidance (p < 0.001), class absenteeism (p < 0.001), and the lower physical domain of QoL (p < 0.001). |
| Zhang (55) | 2018–2019 | East China, Jiangsu | Cluster | 8 | Rome IV | 533/674 | / | Medicine, non-medicine | Undergraduate year 1–4 | 1,207 | 5.1 | • IBS was associated with irregular menstruation (p < 0.05) and previous history of gastroenteritis (p < 0.05). |
Gender (M/F), Gender (Male/Female); Junior college students, students studying in 3-year college degree: Undergraduate students, students studying in 4-year or 5-year bachelor degree; Postgraduate students, students studying in master degree; Under Rome II criteria, IBS-C, irritable bowel syndrome with constipation; IBS-D, irritable bowel syndrome with diarrhea; IBS-M, irritable bowel syndrome mixed; IBS-U, irritable bowel syndrome un-subtyped; Under Rome III criteria: c-IBS, constipation predominant irritable bowel syndrome; d-IBS, diarrhea predominant irritable bowel syndrome; a-IBS, alternative irritable bowel syndrome; SRHMS, self-rated health measurement scale; PSQI, Pittsburgh sleep quality index; QoL, The World Health Organization Quality of Life-BREF Questionnaire.
Quality Assessment and Publication Bias
The scores of study quality assessment ranged from 6 to 9 with a mean score of 7.8. The most common missing items in the studies included the reports of detailed information about the study subjects and the detailed descriptions of the process of collecting data or the professionalism of the person collecting the data (Supplementary Table 2).
No significant publication bias was found by the funnel plot (Supplementary Figure 1) in the 21 studies. Begg's test (z = 1.48, p = 0.139) also did not detect significant bias.
Prevalence of IBS
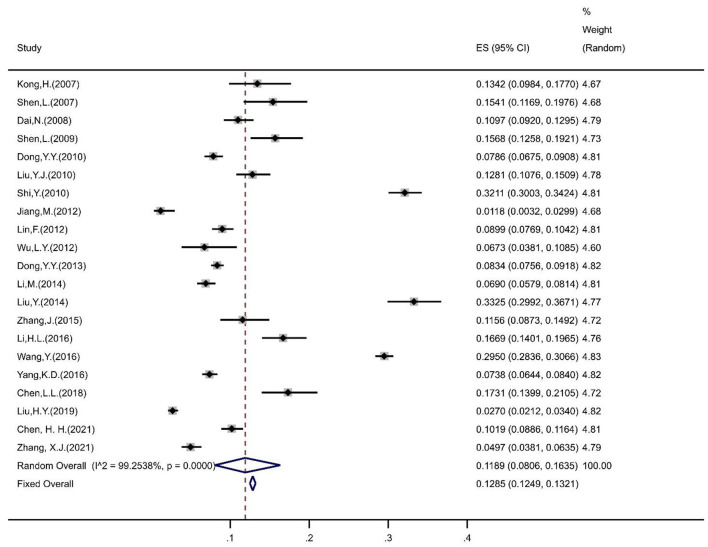
The pooled prevalence of IBS in Chinese university students was estimated to be 11.89% (95% CI = 8.06%, 16.35%) based on the random-effects model (Figure 2). The sensitivity analysis indicated that no study affected the prevalence estimate by more than 1%, suggesting that the overall prevalence estimate was powered to the methodological quality of each research study included.
Figure 2.
Forest plot of prevalence of IBS in Chinses university students. ES, effect size.
Among them, the prevalence of IBS was 8.18% (95% CI = 3.66%, 17.26%) for junior college students, 12.14% (95% CI = 8.02%, 17.96%) for undergraduate students, and 12.74% (95% CI = 10.10%, 15.94%) for postgraduate students. The prevalence of IBS was 13.14% (95% CI = 9.22%, 18.39%) in females and 10.17% (95% CI = 6.39%, 15.80%) in males. The prevalence of IBS in medical, non-medical, and mixed majors were 11.91% (95% CI = 8.13%, 17.12%), 11.35% (95% CI = 8.90%, 14.37%), and 6.48% (95% CI = 2.13%, 18.05%), respectively. In terms of regions, the prevalence of IBS among university students was 15.93% (95% CI = 8.28%, 28.47%) in Central China, 10.50% (95% CI = 8.40%, 13.06%) in East China, 17.66% (95% CI = 7.37%, 36.64%) in North China, 19.10% (95% CI = 7.02%, 42.46%) in Northwest China, and 3.18% (95% CI = 1.28%, 7.68%) in South China. Under different diagnostic criteria, the prevalence of IBS was 10.50% (95% CI = 6.80%, 15.87%) in Rome II, 12.00% (95% CI = 8.23%, 17.17%) in Rome III, and 3.66% (95% CI = 2.01%, 6.60%) in Rome IV.
The prevalence of IBS in people with anxiety and depression symptoms was 17.31% (95% CI = 8.36%, 32.44%) and 17.34% (95% CI = 8.32%, 32.68%), respectively. The prevalence of IBS was 11.11% (95% CI = 6.40%, 18.60%) in people who drank, 18.10% (95% CI = 5.59%, 45.18%) in people who smoke.
Associated Factors With IBS
Subgroup analysis found that a higher prevalence of IBS was significantly associated with postgraduate students, females, medical majors, anxiety, and depression symptoms, drinking and smoking behaviors (all P < 0.001) (Table 2, Supplementary Table 3). The survey region, survey year, diagnostic criteria were also significantly associated with the prevalence of IBS (all P < 0.001) (Table 2, Supplementary Table 3).
Table 2.
Subgroup analyses of the pooled prevalence of IBS.
| Subgroup analysis | Studies (n) | Sample size (n) | Pooled prevalence (%) | 95% CI | I2(%) within subgroup | p-value across subgroups | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Educational level | <0.001 | ||||||
| Junior college | 4 | 5,063 | 8.18 | 3.66 | 17.26 | 98.24 | |
| Undergraduate | 13 | 24,202 | 12.14 | 8.02 | 17.96 | 99.27 | |
| Postgraduate | 3 | 925 | 12.74 | 10.10 | 15.94 | 40.36 | |
| Gender | <0.001 | ||||||
| Female | 16 | 18,252 | 13.14 | 9.22 | 18.39 | 98.72 | |
| Male | 14 | 9,279 | 10.17 | 6.39 | 15.80 | 98.02 | |
| Major | <0.001 | ||||||
| Medicine | 15 | 10,046 | 11.91 | 8.13 | 17.12 | 98.02 | |
| Non-medicine | 10 | 11,077 | 11.35 | 8.90 | 14.37 | 93.49 | |
| Mixed | 5 | 12,061 | 6.48 | 2.13 | 18.05 | 99.55 | |
| Region | <0.001 | ||||||
| Central China | 4 | 2,979 | 15.93 | 8.28 | 28.47 | 97.39 | |
| East China | 7 | 14,597 | 10.50 | 8.40 | 13.06 | 92.56 | |
| North China | 3 | 3,232 | 17.66 | 7.37 | 36.64 | 99.03 | |
| Northwest China | 2 | 6,546 | 19.10 | 7.02 | 42.46 | 98.30 | |
| South China | 3 | 5,812 | 3.18 | 1.28 | 7.68 | 97.00 | |
| Survey year | <0.001 | ||||||
| 2005–2010 | 7 | 7,276 | 14.42 | 8.48 | 23.46 | 98.65 | |
| 2010–2021 | 12 | 23,793 | 10.60 | 6.42 | 17.00 | 99.38 | |
| Criteria | <0.001 | ||||||
| Rome II | 5 | 4,382 | 10.50 | 6.80 | 15.87 | 94.58 | |
| Rome III | 15 | 26,072 | 12.00 | 8.23 | 17.17 | 99.21 | |
| Rome IV | 2 | 3,833 | 3.66 | 2.01 | 6.60 | 92.00 | |
| Anxiety | <0.001 | ||||||
| No | 6 | 11,058 | 8.61 | 3.72 | 18.66 | 99.31 | |
| Yes | 6 | 2,640 | 17.31 | 8.36 | 32.44 | 98.02 | |
| Depression | <0.001 | ||||||
| No | 5 | 10,743 | 9.11 | 3.60 | 21.19 | 99.43 | |
| Yes | 5 | 2,798 | 17.34 | 8.32 | 32.68 | 98.10 | |
| Drinking | <0.001 | ||||||
| No | 4 | 3,570 | 10.78 | 3.51 | 28.62 | 99.05 | |
| Yes | 4 | 970 | 11.11 | 6.40 | 18.60 | 85.58 | |
| Smoking | <0.001 | ||||||
| No | 4 | 2,815 | 14.70 | 6.09 | 31.43 | 98.65 | |
| Yes | 4 | 307 | 18.10 | 5.59 | 45.18 | 87.47 | |
Boldface indicates statistical significance (p < 0.05).
CI, confidence interval.
In the univariate meta-regression, region (p = 0.01) was identified as a significant moderator that contributed to heterogeneity between the studies. However, educational level (p = 0.66), gender ratio (p = 0.19), major (p = 0.05), survey year (p = 0.57) criteria (p = 0.41), anxiety proportion (p = 0.29), depression proportion (p = 0.14), drinking proportion (p = 0.64), smoking proportion (p = 0.71) and quality score (p = 0.48) were non-significant moderators (Table 3).
Table 3.
Univariate meta-regression analyses of prevalence of IBS.
| Variable | Coefficient | SE | T | P > |t| | 95%CI | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Univariate analysis | Educational level | 0.02 | 0.04 | 0.45 | 0.66 | −0.07 | 0.11 |
| Gender ratio (M/F) | −0.09 | 0.06 | −1.36 | 0.19 | −0.23 | 0.05 | |
| Major | −0.09 | 0.04 | −2.06 | 0.05 | −0.18 | 0.00 | |
| Region | 0.03 | 0.01 | 2.84 | 0.01 | 0.01 | 0.06 | |
| Survey year | −0.03 | 0.05 | −0.58 | 0.57 | −0.12 | 0.07 | |
| Criteria | −0.03 | 0.04 | −0.84 | 0.41 | −0.01 | 0.05 | |
| Anxiety proportion | −0.21 | 0.17 | −1.23 | 0.29 | −0.68 | 0.26 | |
| Depression proportion | −0.35 | 0.18 | −1.96 | 0.14 | −0.92 | 0.22 | |
| Drinking proportion | −0.16 | 0.32 | −0.51 | 0.64 | −1.17 | 0.84 | |
| Smoking proportion | −0.15 | 0.33 | −0.43 | 0.71 | −1.59 | 1.30 | |
| Quality score | 0.02 | 0.02 | 0.72 | 0.48 | −0.03 | 0.06 | |
Boldface indicates statistical significance (p < 0.05). CI, confidence interval; M/F, male/female.
Items of sleep disorders (OR = 1.48, 95% CI = 1.02, 2.15), anxiety (OR = 2.35, 95% CI = 2.03, 2.72), depression (OR = 2.15, 95% CI = 1.88, 2.47), and gender (OR = 1.36, 95% CI = 1.08, 1.69) were statistically associated with the development of IBS in Chinese university students (Supplementary Table 4), which was also found in the corresponding subgroup analyses.
Discussion
To the best of our knowledge, this is the first systematic review and meta-analysis to estimate the pooled prevalence of IBS among Chinese university students, including 22 studies with 33,166 subjects. The major findings are: (1) the pooled prevalence of IBS among Chinese university students was 11.89% (95% CI = 8.06%, 16.35%); (2) the prevalence of IBS was significantly associated with educational level, gender, major, region, survey year, diagnostic criteria, anxiety, depression, drinking, smoking, and sleep disorders.
The prevalence of IBS in our study was approximate to that of 10.9% in American university students (56) and 10.7% in Japanese university students (57), but higher than that in Korean college students (5.7%) (58), lower than that in Pakistan college students (34%) (59). The possible explanations might be the difference in culture, diet habits, physical characteristics, academic and socioeconomic stress across countries.
Students with psychological disorders such as anxiety and depression had an increased likelihood of IBS comorbidity compared to those without. The link between psychosocial factors and gastrointestinal function (motility, sensation, inflammation) could be explained by the brain-gut axis (17). Specifically, this implies a bidirectional connection system between the gastrointestinal tract and the brain, through neural, neuroimmune and neuroendocrine pathways. In this model, individuals with increased central nervous system (CNS) arousal such as those with anxiety and depression, could experience gastrointestinal distress and increased gastrointestinal motility via CNS-mediated sympathetic outflow (60), leading to the destruction in the intestinal mucosal barrier (61) and the change of transport in the small intestine and even the entire gastrointestinal tract (62) and, resulting in gastrointestinal symptoms (cramping and pain, etc.) of IBS.
Our study found that the prevalence of IBS was higher among female students. This discrepancy could be attributed to several factors. First, the difference in the secretion of sex hormones contributes to the gender difference in the modulation of IBS. For example, androgens, higher in males, possibly could reduce visceral pain through enhancing TRPM8 expression and/or activity (63). TRPM8 is suggested to possess anti-nociceptive roles in the intestine (64) and ligands of TRPM8 such as peppermint are believed to possess analgesic effects in IBS patients (65, 66). As for females, the higher level of hormones like estrogen contributes to the development of IBS. It is reported that estrogens inhibit colonic smooth muscle contraction via a non-genomic mechanism involving cell membrane coupling (67), leading to the higher occurrence of IBS-related symptoms including abdominal distension, bloating, infrequent stools and hard stools (68). Estrogens promote activation of mast cells (68), which are found to be associated with IBS through increasing intestinal nerve sensitization (69). Second, for females, increased prostaglandins during the menstrual cycle could induce diarrhea syndrome, one of the IBS symptoms, through enhanced intestinal secretion and altered electrolyte absorption (70). Third, women are more vulnerable to experience life stress, anxiety, and depression symptoms (71, 72), which are associated with a higher incidence of IBS.
In terms of majors, a higher prevalence of IBS was estimated in the medical students. This might be due to the long length of schooling, high load from the academy and clinical practice, high level of psychological stress exposure like severe anxiety and depression (73) and sleep disturbances (74). It was proved that the stress was associated with the development of IBS through stimulating the hypothalamic-pituitary-adrenal (HPA) axis and triggering the release of some substances including corticotrophin-releasing factor (CRF), adreno-cortico-tropic-hormone (ACTH), and cortisol, which affect gut function through the composition and the growth of microbiota, and stimulate the sympathetic nervous system (SNS) (75). Sleep disorder, such as insomnia, was associated with a 24-h increase of ACTH and cortisol secretion (76). Furthermore, the symptoms of IBS, such as abdominal pain, might activate the SNS and then reduce sleep efficiency (76, 77).
Our results revealed that the prevalence of IBS in university students was higher in Northwest China (19.10%, 95% CI: 7.02–42.46%), North China (17.66%, 95% CI: 7.37–36.64%) and Central China (15.93%, 95% CI: 8.28–28.47%), followed by East China (10.50%, 95% CI: 8.40–13.06%) and South China (3.18%, 95% CI: 1.28–7.68%). This might be due to the varied territory, climate, diet, traditional customs, the development of socioeconomic and employment prospects across China (48). In the coastal regions–East China and South China, the relatively more moderate climate might benefit people's health and the superior socioeconomic conditions effectively alleviate the psychological stress for university students there (78), leading to a lower prevalence of IBS.
Be consistent with the results of previous studies (79, 80), the prevalence estimation in the Rome III criteria group (12.00%) was higher than groups of Rome II (10.50%) and Rome IV criteria (3.66%). Diagnosis of IBS can be challenging. Compared to Rome III, Rome II criteria examine a 12-week period duration in the past 12 months, less than a continuous 6-month period, thus expanding the scope of diagnosis and being more stringent (81). Rome IV criteria requires that abdominal pain occurs on average at least 1 day per week while only 3 days a month were required in Rome III criteria. This might be the most important factor accounting for a reduction in the estimated prevalence of IBS from Rome III to Rome IV (82). Dai et al. (39) suggested that the choice between Rome II and Rome III criteria may affect the IBS diagnosis in females more than males. Another diagnosis of IBS–Manning criteria was regarded to be applied to the private housing group rather than the public housing group (83). Studies showed that Manning criteria was more appropriate for females (84), but less sensitive for males (85, 86). The applicable diagnostic criteria seem different according to the research population.
Furthermore, university students with drinking and smoking behaviors were more likely to report IBS. It was explained that alcohol could decrease muscle movements, which helps retain the food for further digestion in the small intestine and reduce the frequency and strength of muscle contractions in a segment of the rectum. This could further reduce the transit time and the compaction of the intestinal content. In addition, alcohol interferes with the activity of lactase, which breaks down the milk sugar lactose, resulting in lactose intolerance. Thus, diarrhea was frequently observed in alcoholics. Alcohol also inhibits some enzymes that participate in the metabolism of foreign organic substances in the gut. It directly disturbs the integrity of the mucosal epithelium and induces the release of noxious signaling molecules, which could damage the small blood vessels of capillaries in the intestinal mucosa and induce blood clotting. The resulting lesions allow large molecules, such as endotoxins and other bacterial toxins, to enter the bloodstream and the lymph. Therefore, alcohol-induced digestive disorders and mucosal damage in the gastrointestinal (GI) tract cause the change in the frequency and appearance of the stool, abdominal pain and bloating (87), which were the symptoms of IBS. For smokers, nicotine stimulates the sympathetic nerve to inhibit the movement of the disinfectant tract and the secretion of the gland, resulting in gastrointestinal emptying delay and absorption dysfunction. Another explanation could be that oxygen-free radicals from smoking could enhance lipid peroxidation, implicated with gastrointestinal dysfunction (88).
The results of this meta-analysis have implications for future research. The prevalence of IBS among university students in certain regions such as Northeast and Southwest China, needs further study for the overall estimation with greater precision. More population-based studies using Rome IV criteria are required to explore the appropriateness of this criteria on Chinese university students. Future longitudinal studies are needed to be adopted to establish the causal relationships between IBS and potential influencing factors, which are greatly warranted for intervention development.
The findings of this meta-analysis should be interpreted with caution due to several limitations. First, the 22 included studies involved only 14 of 34 provincial-level administrative regions in China, which limited the generalizability of the findings to all university students in China. Second, although subgroup analyses somewhat mitigated this limitation (89), heterogeneity was impossible to avoid in the meta-analysis of epidemiological studies. Third, the potential association between IBS and some factors, such as frequency of exercise, could not be examined in the subgroup analyses due to incomplete data or inconsistent reporting forms in most included studies. The miss of studies only exploring the associated factors without the prevalence of IBS might lead to the insufficiency of data on the analyses of associated factors of IBS. Therefore, our results of associated factors of IBS needed to be treated with caution. Finally, the causal inference between IBS and other factors was not allowed because of the cross-sectional design in all included studies.
Conclusions
This systematic review and meta-analysis showed that IBS was common (11.89%) in Chinese university students. The prevalence varied considerably in some instances, according to educational levels, geographic region, criteria used to define IBS. There are many associated factors of IBS, including female gender, majoring in medicine, anxiety, depression, drinking and smoking behavior. Further research should build on our findings and develop effective strategies for preventing and treating IBS in this population.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
PX: conceptualization, methodology, software, resources, writing-original draft, writing-review and editing, supervision, project administration, and funding acquisition. TZ: conceptualization, methodology, and funding acquisition. WY: methodology, validation, formal analysis, investigation, data curation, and writing–original. XY: validation, formal analysis, investigation, data curation, writing-original draft, and visualization. XC: methodology, investigation, draft, and visualization. ZZ and HY: methodology, investigation, and visualization. XS: review and revision. All authors contributed to the article and approved the submitted version.
Funding
PX was supported by grants Moral Education Research Project for Teaching Science of Education Department of Guangdong Province (NO. 2019JKDY005) and National Natural Science Foundation of China (NO. 31970990). TZ was supported by grants Guangzhou Institute of Pediatrics/Guangzhou Women and Children's Medical Center funds (NO. GCP-2018-001) and Program of Guangzhou Municipal Science and Technology Bureau (NO. 201803010025). The funding body had no role in the study design, data collection, data analysis, data interpretation, the writing of the manuscript and the decision to submit the paper for publication. The research presented in this paper is that of the authors and does not reflect the official policy of Department of Public Health and Preventive Medicine, School of Medicine, Jinan University, Guangzhou, China. PX has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.864721/full#supplementary-material
References
- 1.Saha L. Irritable bowel syndrome: pathogenesis, diagnosis, treatment, and evidence-based medicine. World J Gastroenterol. (2014) 20:6759–73. 10.3748/wjg.v20.i22.6759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schoenfeld PS. Advances in IBS 2016: A Review of Current and Emerging Data. Gastroenterol Hepatol. (2016) 12:1–11. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5210026/ [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang L, Duan LP, Liu YX, Leng YX, Zhang H, Liu ZJ, et al. Meta analysis of prevalence and related risk factors of irritable bowel syndrome in Chinese population [In Chinese]. Zhonghua Nei Ke Za Zhi. (2014) 53:969–75. 10.3760/cma.j.issn.0578-1426.2014.12.011 [DOI] [PubMed] [Google Scholar]
- 4.Choung RS, Locke GR, 3rd, Zinsmeister AR, Schleck CD, Talley NJ. Psychosocial distress and somatic symptoms in community subjects with irritable bowel syndrome: a psychological component is the rule. Am J Gastroenterol. (2009) 104:1772–9. 10.1038/ajg.2009.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shen L, Kong H, Hou X. Prevalence of irritable bowel syndrome and its relationship with psychological stress status in Chinese university students. J Gastroenterol Hepatol. (2009) 24:1885–90. 10.1111/j.1440-1746.2009.05943.x [DOI] [PubMed] [Google Scholar]
- 6.Enck P, Aziz Q, Barbara G, Farmer AD, Fukudo S, Mayer EA, et al. Irritable bowel syndrome. Nat Rev Dis Primers. (2016) 2:16014. 10.1038/nrdp.2016.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fadgyas-Stanculete M, Buga AM, Popa-Wagner A, Dumitrascu DL. The relationship between irritable bowel syndrome and psychiatric disorders: from molecular changes to clinical manifestations. J Mol Psychiatry. (2014) 2:4. 10.1186/2049-9256-2-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jang SH Ryu HS, Choi SC, Lee SY. Psychological factors influence the irritable bowel syndrome and their effect on quality of life among firefighters in South Korea. Psychiatry Investig. (2017) 14:434–40. 10.4306/pi.2017.14.4.434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Midenfjord I, Polster A, Sjövall H, Törnblom H, Simrén M. Anxiety and depression in irritable bowel syndrome: Exploring the interaction with other symptoms and pathophysiology using multivariate analyses. Neurogastroenterol Motil. (2019) 31:e13619. 10.1111/nmo.13619 [DOI] [PubMed] [Google Scholar]
- 10.Zamani M, Alizadeh-Tabari S, Zamani V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment Pharmacol Ther. (2019) 50:132–43. 10.1111/apt.15325 [DOI] [PubMed] [Google Scholar]
- 11.Drossman DA. Rome III: the new criteria. Chin J Dig Dis. (2006) 7:181–5. 10.1111/j.1443-9573.2006.00265.x [DOI] [PubMed] [Google Scholar]
- 12.Fau DD, Hasler WL. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology. (2016) 150:1257–61. 10.1053/j.gastro.2016.03.035 [DOI] [PubMed] [Google Scholar]
- 13.Jiang M, Wang L, Liu X, Hu HX, Liang ZX, Zhang JA. The distribution and influencing factors of functional gastrointestinal diseases in college students [In Chinese]. Chin J Clinicians. (2012) 6:5281–2. 10.3877/cma.j.issn.1674-0785.2012.17.069 [DOI] [Google Scholar]
- 14.Liu Y, Liu L, Yang Y, He Y, Zhang Y, Wang M, et al. A school-based study of irritable bowel syndrome in medical students in Beijing, China: prevalence and some related factors. Gastroenterol Res Pract. (2014) 2014:124261. 10.1155/2014/124261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou WW, Luo CH, Fan CX, Li YF, Ma SB. A study on the status and influential factors of health literacy among undergraduate students in Guangzhou City [In Chinese]. Chinese Journal of Disease Control & Prevention. (2014) 18:654–8. Available online at: http://zhjbkz.ahmu.edu.cn/article/id/JBKZ201407021 [Google Scholar]
- 16.Jiang CX Li ZZ, Chen P, Chen LZ. Prevalence of depression among college-goers in mainland China: a methodical evaluation and meta-analysis. Medicine. (2015) 94:e2071. 10.1097/MD.0000000000002071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Surdea-Blaga T, Fau BA, Dumitrascu DL. Psychosocial determinants of irritable bowel syndrome. World J Gastroenterol. (2012) 18:616–26. 10.3748/wjg.v18.i7.616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mao CF, Zhou WJ, Ma HY, Wang XP, Weng XY, Zhuo YN, et al. A survey on cognitive attitude and behavior of chronic diseases among college students in Hangzhou [In Chinese]. Zhongguo jian kang jiao yu. (2015) 31:15–9. 10.16168/j.cnki.issn.1002-9982.2015.01.04 [DOI] [Google Scholar]
- 19.Grover M, Kolla BP, Pamarthy R, Mansukhani M, Breen-Lyles M, He JP, et al. Psychological, physical, and sleep comorbidities and functional impairment in irritable bowel syndrome: Results from a national survey of US adults. PLoS ONE. (2021) 16:e0245323. 10.1371/journal.pone.0245323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frändemark Å, Törnblom H, Jakobsson S, Simrén M. Work productivity and activity impairment in irritable bowel syndrome (IBS): a multifaceted problem. Am J Gastroenterol. (2018) 113:1540–9. 10.1038/s41395-018-0262-x [DOI] [PubMed] [Google Scholar]
- 21.Sertbas Y, Fau BH, Fau PN, Fau UC, Fau AM, Fau SM, et al. Assesment of psychiatric symptoms and co-morbidities in patients with irritable bowel syndrome. West Indian Med J. (2012) 61:544–8. 10.7727/wimj.2012.166 [DOI] [PubMed] [Google Scholar]
- 22.Wang B, Duan R, Duan L. Prevalence of sleep disorder in irritable bowel syndrome: a systematic review with meta-analysis. Saudi J Gastroenterol. (2018) 24:141–50. 10.4103/sjg.SJG_603_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gralnek IM. Health care utilization and economic issues in irritable bowel syndrome. Eur J Surg. (1998) 164:73–6. 10.1080/11024159850191283 [DOI] [PubMed] [Google Scholar]
- 24.Gulewitsch MD, Fau EP, Fau HM, Schlarb AA. Irritable bowel syndrome symptoms among German students: prevalence, characteristics, and associations to somatic complaints, sleep, quality of life, and childhood abdominal pain. Eur J Gastroenterol Hepatol. (2011) 23:311–6. 10.1097/MEG.0b013e3283457b1e [DOI] [PubMed] [Google Scholar]
- 25.Tan YM, Goh KL, Muhidayah R, Ooi CL, Salem O. Prevalence of irritable bowel syndrome in young adult Malaysians: a survey among medical students. J Gastroenterol Hepatol. (2003) 18:1412–6. 10.1046/j.1440-1746.2003.03212.x [DOI] [PubMed] [Google Scholar]
- 26.Drossman DA, Fau CL, Fau SS, Fau BC, Fau NW, Norton NJ, et al. A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. Dig Dis Sci. (2009) 54:1532–41. 10.1007/s10620-009-0792-6 [DOI] [PubMed] [Google Scholar]
- 27.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiologya proposal for reporting. JAMA. (2000) 283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 29.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int J Evid Based Healthc. (2015) 13:147–53. 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 30.Santoso AMM, Jansen F, de Vries R, Leemans CR, van Straten A, Verdonck-de Leeuw IM. Prevalence of sleep disturbances among head and neck cancer patients: a systematic review and meta-analysis. Sleep Med Rev. (2019) 47:62–73. 10.1016/j.smrv.2019.06.003 [DOI] [PubMed] [Google Scholar]
- 31.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. (2013) 67:974–8. 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- 32.Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Statist. (1950) 21:607–11. 10.1214/aoms/1177729756 [DOI] [Google Scholar]
- 33.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 35.Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. (2018) 74:785–94. 10.1111/biom.12817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dalton JE, Fau BS, Mascha EJ. Publication bias: the elephant in the review. Anesth Analg. (2016) 123:812–3. 10.1213/ANE.0000000000001596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kong H, Shen L, Hou XH. Prevalence of irritable bowel syndrome among medical students in different grades: the effect of anxiety and depression. J Clin Intern Med. (2007) 24:825–7. 10.3969/j.issn.1001-9057.2007.12.011 [DOI] [Google Scholar]
- 38.Shen L, Kong H, Hou X. An epidemiologic study of irritable bowel syndrome in graduates of different specialties. Chin J Gastroenterol. (2007) 12:14–8. 10.3969/j.issn.1008-7125.2007.01.004 [DOI] [Google Scholar]
- 39.Dai N, Cong Y, Yuan H. Prevalence of irritable bowel syndrome among undergraduates in Southeast China. Dig Liver Dis. (2008) 40:418–24. 10.1016/j.dld.2008.01.019 [DOI] [PubMed] [Google Scholar]
- 40.Dong YY, Zuo XL, Li CQ, Yu YB, Zhao QJ, Li YQ. Prevalence of irritable bowel syndrome in Chinese college and university students assessed using Rome III criteria. World J Gasentrol. (2010) 16:4221–6. 10.3748/wjg.v16.i33.4221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu Y, Xiong L, Cui M. The prevalence and influencing factors of irritable bowel syndrome among students in a vocational college in Jiangxi Province. Chin J Sch Health. (2010) 31:1393–4. 10.16835/j.cnki.1000-9817.2010.11.049 [DOI] [Google Scholar]
- 42.Shi Y, Liu L, Zhang Z. Current situation of irritable bowel syndrome in nursing and clinical medicine undergraduates. J Zhengzhou Univers. (2010) 45:829–31. 10.13705/j.issn.1671-6825.2010.05.025 [DOI] [Google Scholar]
- 43.Lin F, Li Z. Investigation of functional gastrointestinal diseases among students of Tangshan Medical College. Seek Medical and Ask The Medicine (2012) 10:281. Available online at: http://www.cnki.com.cn/Article/CJFDTotal-QYWA201211302.htm [Google Scholar]
- 44.Wu L, Xu X, Ma H. Investigation and analysis of influencing factors of irritable bowel syndrome among internal medical students in Wuhan City. Chin Med Hearald. (2012) 9:125–7. 10.3969/j.issn.1673-7210.2012.33.048 [DOI] [Google Scholar]
- 45.Dong YY, Chen FX, Yu YB, Du C, Qi QQ, Liu H, et al. A school-based study with rome iii criteria on the prevalence of functional gastrointestinal disorders in chinese college and university students. PLoS ONE (2013) 8:e54183. 10.1371/journal.pone.0054183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li M, Lu B, Chu L, Zhou H, Chen MY. Prevalence and characteristics of dyspepsia among college students in Zhejiang province. World J Gastroentrol. (2014) 20:3649–54. 10.3748/wjg.v20.i13.3649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang Y, Liu L, He Y, Zhao H, Yao S, Zhang Y. Gender differences in the prevalence of irritable bowel syndrome and related factors in medical students. J China-Japan Friendship Hosp. (2015) 29:177–9. 10.3969/j.issn.1001-0025.2015.03.01524707150 [DOI] [Google Scholar]
- 48.Zhang J, Zhang GL, Liu H, Liu F, Chen WG, Zheng Y. Morbidity of IBS and its related factors in different major postgraduates [In Chinese]. Chin J Gastroenterol Hepatol. (2015) 24:291–5. 10.3969/j.issn.1006-5709.2015.03.016 [DOI] [Google Scholar]
- 49.Li H, Liu L, Ren W, Li Y, Liu Y, Zhang Y, et al. A school-based study of irritable bowel syndrome in college students in Beijing: prevalence and some relative factors. Chin J Gastroenterol Hepatol. (2016) 25:448–51. 10.3969/j.issn.1006-5709.2016.04.025 [DOI] [Google Scholar]
- 50.Wang Y, Jin F, Chi B, Duan S, Zhang Q, Liu Y, et al. Gender differences in irritable bowel syndrome among medical students at Inner Mongolia Medical University, China: a cross-sectional study. Psychol Health Med. (2016) 21:964-74. 10.1080/13548506.2016.1144890 [DOI] [PubMed] [Google Scholar]
- 51.Yang K, Jin Y, Yang T. Investigation and syndrome differentiation of Irritable bowel syndrome among students in a university in Guangzhou [In Chinese]. J New Chin Med. (2016) 48:74–5. 10.13457/j.cnki.jncm.2016.08.032 [DOI] [Google Scholar]
- 52.Chen L, Shen F, Hong L, Jin Q, Jin Y, Zhu D, et al. The association of sleep quality with prevalence of irritable bowel syndrome in female college students from the faculty of nursing. Nurs. Integ. Trad. Chin West Med. (2018) 4:23–6. 10.11997/nitcwm.201805007 [DOI] [Google Scholar]
- 53.Liu H, Jiang L, Wei X, Liang H, Chen Y, Long S, et al. Investigation analysis of the prevalence situation and risk factors for irritable bowel syndrome of students in a higher vocational college in Guangxi based on the Rome IV standard . Intern Med Chin. (2019) 14:16-8. 10.16121/j.cnki.cn45-1347/r.2019.05.02 [DOI] [Google Scholar]
- 54.Chen HH, Hung CH, Kao AW, Hsieh HF. Exploring quality of life, stress, and risk factors associated with irritable bowel syndrome for female university students in Taiwan. Int J Environ Res Public Health. (2021) 18:3888. 10.3390/ijerph18083888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang X, Ma S, Li R. Prevalence of irritable bowel syndrome and analysis of related factors in Soochow University. Contemp Med. (2021) 27:120–3. 10.3969/j.issn.1009-4393.2021.08.048 [DOI] [Google Scholar]
- 56.Hazlett-Stevens H, Craske MG, Mayer EA, Chang L, Naliboff BD. Prevalence of irritable bowel syndrome among university students: the roles of worry, neuroticism, anxiety sensitivity and visceral anxiety. J Psychosom Res. (2003) 55:501–5. 10.1016/S0022-3999(03)00019-9 [DOI] [PubMed] [Google Scholar]
- 57.Shiotani A, Miyanishi T, Takahashi T. Sex differences in irritable bowel syndrome in Japanese university students. J Gastroenterol. (2006) 41:562–8. 10.1007/s00535-006-1805-2 [DOI] [PubMed] [Google Scholar]
- 58.Kim YJ, Ban DJ. Prevalence of irritable bowel syndrome, influence of lifestyle factors and bowel habits in Korean college students. Int J Nurs Stud. (2005) 42:247–54. 10.1016/j.ijnurstu.2004.06.015 [DOI] [PubMed] [Google Scholar]
- 59.Jafri W, Yakoob J, Jafri N, Islam M, Ali QM. Frequency of irritable bowel syndrome in college students. J Ayub Med Coll Abbottabad. (2005) 17:9–11. Available online at: https://ecommons.aku.edu/pakistan_fhs_mc_med_gastroenterol/56/ [PubMed] [Google Scholar]
- 60.Lydiard RB. Irritable bowel syndrome, anxiety, and depression: what are the links? J Clin Psychiatry. (2001) 62:38–45. Available online at: https://www.psychiatrist.com/jcp/medical/comorbidity/irritable-bowel-syndrome-anxiety-depression-are-links/ [PubMed] [Google Scholar]
- 61.Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. (2011) 62:591–9. Available online at: http://www.jpp.krakow.pl/journal/archive/12_11/pdf/591_12_11_article.pdf [PubMed] [Google Scholar]
- 62.Pellissier S, Bonaz B. The place of stress and emotions in the irritable bowel syndrome. Vitam Horm. (2017) 103:327–54. 10.1016/bs.vh.2016.09.005 [DOI] [PubMed] [Google Scholar]
- 63.So SY, Savidge TC. Sex-bias in irritable bowel syndrome: linking steroids to the gut-brain axis. Front Endocrinol. (2021) 12:684096. 10.3389/fendo.2021.684096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Harrington AM, Fau HP, Fau MC, Fau YJ, Fau CJ, Fau IN, et al. A novel role for TRPM8 in visceral afferent function. Pain. (2011) 152:1459–68. 10.1016/j.pain.2011.01.027 [DOI] [PubMed] [Google Scholar]
- 65.Cappello G, Spezzaferro M, Fau-Grossi L, Grossi L, Fau-Manzoli L, Manzoli L, et al. Peppermint oil (Mintoil) in the treatment of irritable bowel syndrome: a prospective double blind placebo-controlled randomized trial. Dig Liver Dis. (2007) 39:530–6. 10.1016/j.dld.2007.02.006 [DOI] [PubMed] [Google Scholar]
- 66.Ford AC, Fau TN, Fau SB, Fau F-OA, Fau SL, Fau QE, et al. Effect of fibre, antispasmodics, and peppermint oil in the treatment of irritable bowel syndrome: systematic review and meta-analysis. BMJ. (2008) 337:a2313. 10.1136/bmj.a2313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hogan AM, Fau KR, Fau CD, Fau BA, Winter DC. Oestrogen inhibits human colonic motility by a non-genomic cell membrane receptor-dependent mechanism. Br J Surg. (2009) 96:817–22. 10.1002/bjs.6612 [DOI] [PubMed] [Google Scholar]
- 68.Meleine M, Matricon J. Gender-related differences in irritable bowel syndrome: potential mechanisms of sex hormones. World J Gastroenterol. (2014) 20:6725–43. 10.3748/wjg.v20.i22.6725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Uranga J, Martínez V, Abalo R. Mast cell regulation and irritable bowel syndrome: effects of food components with potential nutraceutical use. Molecules. (2020) 25:4314. 10.3390/molecules25184314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kane SV, Sable K, Hanauer SB. The menstrual cycle and its effect on inflammatory bowel disease and irritable bowel syndrome: a prevalence study. Am J Gastroenterol. (1998) 93:1867–72. 10.1111/j.1572-0241.1998.540_i.x [DOI] [PubMed] [Google Scholar]
- 71.Young E, Korszun A. Sex, trauma, stress hormones and depression. Mol Psychiatry. (2010) 15:23–8. 10.1038/mp.2009.94 [DOI] [PubMed] [Google Scholar]
- 72.Altemus M. Sex differences in depression and anxiety disorders: potential biological determinants. Horm Behav. (2006) 50:534–8. 10.1016/j.yhbeh.2006.06.031 [DOI] [PubMed] [Google Scholar]
- 73.Mao Y, Zhang N, Liu J, Zhu B, He R, Wang X, et al. A systematic review of depression and anxiety in medical students in China. BMC Med Educ. (2019) 19:327. 10.1186/s12909-019-1744-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. (2015) 11:69–74. 10.5664/jcsm.4370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Qin HY, Cheng CW, Tang XD, Bian ZX. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol. (2014) 20:14126–31. 10.3748/wjg.v20.i39.14126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vgontzas AN, Chrousos GP. Sleep, the hypothalamic-pituitary-adrenal axis, and cytokines: multiple interactions and disturbances in sleep disorders. Endocrinol Metab Clin North Am. (2002) 31:15–36. 10.1016/S0889-8529(01)00005-6 [DOI] [PubMed] [Google Scholar]
- 77.Schlereth T, Birklein F. The sympathetic nervous system and pain. Neuromolecular Med. (2008) 10:141–7. 10.1007/s12017-007-8018-6 [DOI] [PubMed] [Google Scholar]
- 78.Zhang L, Che WB, Li B, Zhang XD. An epidemiological survey of psychological stress among undergraduates in 13 Universities in China [In Chinese]. Chinese Journal of Epidemiology. (2006) 27:387–91. 10.3760/j.issn:0254-6450.2006.05.006 [DOI] [Google Scholar]
- 79.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. (2012) 10:712–21. 10.1016/j.cgh.2012.02.029 [DOI] [PubMed] [Google Scholar]
- 80.Oka P, Parr H, Barberio B, Black CJ, Savarino EV, Ford AC. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. (2020) 5:908–17. 10.1016/S2468-1253(20)30217-X [DOI] [PubMed] [Google Scholar]
- 81.Sperber AD, Fau SP, Fau FM, Fich A. A comparative reappraisal of the Rome II and Rome III diagnostic criteria: are we getting closer to the 'true' prevalence of irritable bowel syndrome? Eur J Gastroenterol Hepatol. (2007) 19:441–7. 10.1097/MEG.0b013e32801140e2 [DOI] [PubMed] [Google Scholar]
- 82.Whitehead WE, Palsson OS, Simrén M. Irritable bowel syndrome: what do the new Rome IV diagnostic guidelines mean for patient management? Expert Rev Gastroenterol Hepatol. (2017) 11:281–3. 10.1080/17474124.2017.1292130 [DOI] [PubMed] [Google Scholar]
- 83.Gwee KA, Lu CL, Ghoshal UC. Epidemiology of irritable bowel syndrome in Asia: something old, something new, something borrowed. J Gastroenterol Hepatol. (2009) 24:1601–7. 10.1111/j.1440-1746.2009.05984.x [DOI] [PubMed] [Google Scholar]
- 84.Gwee KA, Wee S, Wong ML, Png DJ. The prevalence, symptom characteristics, and impact of irritable bowel syndrome in an asian urban community. Am J Gastroenterol. (2004) 99:924–31. 10.1111/j.1572-0241.2004.04161.x [DOI] [PubMed] [Google Scholar]
- 85.Talley NJ, Phillips SF, Melton LJ, Mulvihill C, Wiltgen C, Zinsmeister AR. Diagnostic value of the Manning criteria in irritable bowel syndrome. Gut. (1990) 31:77–81. 10.1136/gut.31.1.77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Smith RC, Greenbaum DS, Vancouver JB, Henry RC, Reinhart MA, Greenbaum RB, et al. Gender differences in Manning criteria in the irritable bowel syndrome. Gastroenterology. (1991) 100:591–5. 10.1016/0016-5085(91)80002-Q [DOI] [PubMed] [Google Scholar]
- 87.Bode C, Bode JC. Effect of alcohol consumption on the gut. Best Pract Res Clin Gastroenterol. (2003) 17:575–92. 10.1016/S1521-6918(03)00034-9 [DOI] [PubMed] [Google Scholar]
- 88.Kim YJ, Fau KE, Hahm KB. Oxidative stress in inflammation-based gastrointestinal tract diseases: challenges and opportunities. J Gastroenterol Hepatol. (2012) 27:1004–10. 10.1111/j.1440-1746.2012.07108.x [DOI] [PubMed] [Google Scholar]
- 89.Patsopoulos NA, Fau EE, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. (2008) 37:1148–57. 10.1093/ije/dyn065 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.