Abstract
Objective
Hypospadias is a common congenital problem among male newborns. Both rapid absorbable sutures (polyglactin, Vicryl) and delayed absorbable sutures (polydioxanone, PDO) are used in hypospadias repair based on the surgeon's preference. This study was conducted to compare post-urethroplasty complication rates in pediatric patients with hypospadias using Vicryl or PDO sutures.
Methods
This is a retrospective study which was designed and performed on 583 children aged 1–7 years old who had undergone hypospadias repair from January 2012 to December 2018. Required data were obtained from the patients' medical records.
Results
Overall, post-surgical complications were observed in 60 (10.3%) patients comprising urethro-cutaneous fistula (n=39, 6.7%), meatal stenosis (n=10, 1.7%), urethral stricture (n=7, 1.2%), and glans dehiscence (n=4, 0.7%). The mean age of the children with complications was 3.0±1.3 years. According to Kaplan-Meier estimate, the interval between surgery and development of complications was significantly shorter in the Vicryl group (p=0.037). Overall, complications were more prevalent in Vicryl suture than PDO suture (15.1% vs. 5.3%, p<0.001). Regression model revealed that in comparison to the distal type, proximal hypospadias (odds ratio [OR]:103.9, 95% confidence interval [CI]: 32.2–334.9, p<0.001) and mid-shaft hypospadias (OR: 82.9, 95% CI: 25.9–264.6, p<0.001) while using Vicryl suture instead of PDO suture (OR: 62.4, 95% CI: 21.2–183.8, p<0.001) increased the odds of developing post-urethroplasty complications.
Conclusion
We suggest PDO suture in the repair of hypospadias due to its lower complication rate, especially in cases of proximal and mid-shaft hypospadias which can get more complicated than the distal type.
Keywords: Hypospadias, Urinary fistula, Polyglactin, Polydioxanone
1. Introduction
Hypospadias is a congenital abnormality with the ventral location of the urethral meatus. It occurs roughly in 1/250 male newborns; however, its incidence seems to be increasing [1,2]. The types of this disease are classified as follows: Anterior (glanular and subcoronal), middle (distal penile, midshaft, and proximal penile), and posterior (penoscrotal, scrotal, and perineal) [1].
More than 300 techniques of surgical repair of hypospadias have been introduced in the literature [2]. The classification of surgical techniques is based on advancement techniques, tabularization techniques, and application of grafts or flaps. The factors that determine the success of urethroplasty include the age of repair, type of hypospadias, the intricacy of surgical technique, surgeon's experience, and healing capability of the urethral tissue [3]. The suture material in hypospadias repair should be absorbable with optimal tensile resistance during the healing process. Based on the surgeon's preference, rapid or delayed absorbable sutures may be used.
Some authors indicated that the development of complications, such as fistula, may be reduced by using delayed absorbable suture like polydioxanone (PDO) [4]; however, some surgeons suggested that delayed absorbable sutures might cause urethral stricture due to long-time tissue irritation [5]. Many studies investigated and compared different suture materials, and it was found to be a subject of controversy in many articles [[6], [7], [8], [9], [10]]. Vicryl is a multifilament suture material with a 2-week half-life, and PDO is an absorbable suture with a 6-week half-life which is made of synthetic substance. Both have stronger tensile strength than the surgical chromic gut suture [11,12]. This study was designed and performed to compare post-urethroplasty complication rates in children with hypospadias using Vicryl or PDO sutures.
2. Patients and methods
In this retrospective study, surgical data of 583 children aged 1–7 years old who had undergone primary hypospadias repair from January 2012 to December 2018 in two referral hospitals affiliated to Shiraz University of Medical Sciences, Shiraz, Iran, were investigated. Demographic and surgical data were gathered from the patients' medical records. Complications included urethro-cutaneous fistula, meatal stenosis, urethral stricture, and glans dehiscence.
Hypospadias was classified based on the urethral meatus location in the distal, mid-shaft, and proximal sections. All patients had been operated by one expert surgeon using the tubularized incised plate (TIP) technique. Dartos flap in the distal and mid-shaft hypospadias and tunica vaginalis flap in the proximal hypospadias were harvested and flipped over the neourethra during the TIP method. A 6 Fr urethral catheter was inserted and kept 5–7 days in distal and mid-shaft hypospadias and 10–14 days in proximal hypospadias postoperatively. All patients were individually evaluated at time-table intervals (1 week, 1 month, 6 months, and 2 years postoperatively) in the clinic. The suture material was Vicryl (polyglactin 910) or PDO. From January 2012 to November 2015, we performed urethroplasty procedures using Vicryl, while from December 2015 to December 2018 we have switched the suture to PDO. Vicryl suture was used in 298 (51.1%) patients including 227 distal, 70 mid-shaft, and 30 proximal hypospadias. In addition, PDO suture was applied in 285 (48.9%) patients including 185 distal, 55 mid-shaft, and 51 proximal hypospadias.
Exclusion criteria were recurrent fistula, recurrent hypospadias, two-staged hypospadias, and hypospadias with more than 30° chordee.
Informed consents were obtained from all the children's guardians. The protocol of the study was approved by the ethics committee of Shiraz University of Medical Sciences (IR.SUMS.MED.REC.1398.260). The authors have obtained the permission of using the data for this study from Shiraz University of Medical Sciences. Descriptive data were presented as mean ± standard deviation, frequency, and percentage. Chi-square test and independent sample t-test were used for bivariate analysis. A logistic regression model was applied to assess the independent association of developing complications as a dependent variable, and hypospadias type and suture type are independent factors. Kaplan-Meier estimator and log-rank test were used to analyze time to develop post-urethroplasty complication. The adjusted odds ratio (OR) and its 95% confidence interval (CI) were estimated. A p-value of less than 0.05 was considered statistically significant. IBM SPSS Statistics for Windows, Version 26.0 (IBM Corporation, Armonk, New York, USA) was used for analyses.
3. Results
Overall, post-surgical complications were observed in 60 (10.3%) patients including urethro-cutaneous fistula (n=39, 6.7%), meatal stenosis (n=10, 1.7%), urethral stricture (n=7, 1.2%), and glans dehiscence (n=4, 0.7%). The mean age of the children was 3.0±1.3 years in the complicated group compared to 3.1±1.2 years in the uncomplicated group (p=0.243).
The frequencies of complications based on the hypospadias type and suture type are presented in Table 1. The complication rates were significantly higher in the proximal (26.2%) and mid-shaft hypospadias (17.6%) in comparison with the distal type (4.3%) (p<0.001). Moreover, the complication rate was significantly higher in Vicryl suture than PDO suture (15.1% vs. 5.3%, p<0.001). The frequency of complications was higher in the Vicryl group compared to the PDO group; however, the difference was not statistically significant, possibly due to the small numbers in subgroups (p=0.460) (Table 2).
Table 1.
Comparison of the frequencies of post-hypospadias repair complications based on hypospadias type and suture type.
| Parameter | Complication, n (%) | p-Value |
|---|---|---|
| Hypospadias type | <0.001 | |
| Distal (n=374) | 16 (4.3) | |
| Mid-shaft (n=125) | 22 (17.6) | |
| Proximal (n=84) | 22 (26.2) | |
| Suture type | <0.001 | |
| Vicryl (n=298) | 45 (15.1) | |
| PDO (n=285) | 15 (5.3) |
PDO, polydioxanone.
Table 2.
Comparison of post-surgical complication rates between Vicryl and PDO sutures in children with hypospadias repair.
| Complication | Vicryl, n (%) | PDO, n (%) | p-Valuea |
|---|---|---|---|
| Urethro-cutaneous fistula | 27 (9.1) | 12 (4.2) | 0.460 |
| Glans dehiscence | 4 (1.3) | 0 (0) | |
| Meatal stenosis | 8 (2.7) | 2 (0.7) | |
| Urethral stricture | 6 (2.0) | 1 (0.4) |
PDO, polydioxanone.
Suture types and complications have been compared as two independent qualitative variables.
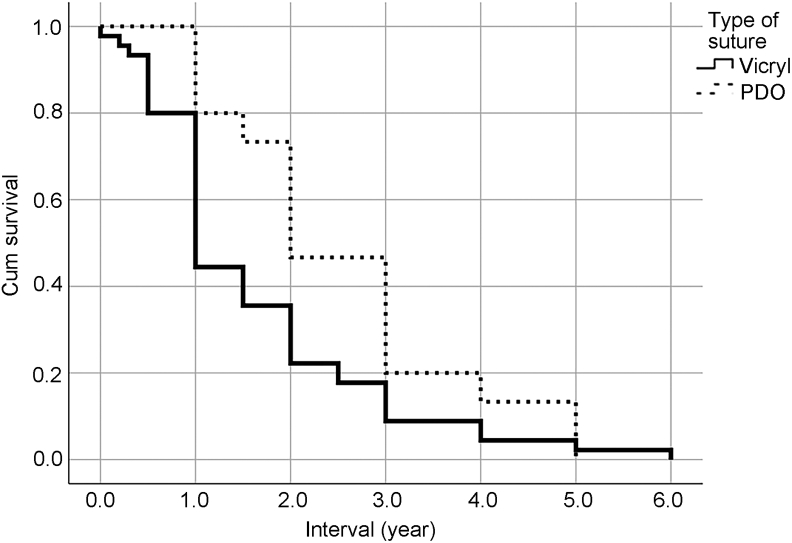
In addition, the interval between surgery and development of complications was significantly shorter in the Vicryl group (1.63±1.27 years vs. 2.56±1.32, p<0.018). This finding was also confirmed by Kaplan-Meier model (p=0.037) (Fig. 1). According to the multivariable analyses, hypospadias type and suture type were independently associated with developing complications (Table 3).
Figure 1.
Kaplan-Meier survival plot showing time to develop post-surgical complications in the Vicryl and PDO groups. PDO, polydioxanone.
Table 3.
Results of binary logistic regression.a
| Parameter | Regression coefficient | Standard error | p-Value | OR | 95% CI of OR |
|---|---|---|---|---|---|
| Intercept | −6.883 | 0.6043 | <0.001 | 0.001 | 0.000–0.003 |
| Hypospadias type (distal as reference) | |||||
| Proximal | 4.644 | 0.5971 | <0.001 | 103.9 | 32.2–334.9 |
| Mid-shaft | 4.418 | 0.5921 | <0.001 | 82.9 | 25.9–264.6 |
| Suture type (PDO as reference) | |||||
| Vicryl | 4.135 | 0.5507 | <0.001 | 62.4 | 21.2–183.8 |
PDO, polydioxanone; CI, confidence interval; OR, odds ratio.
Developing complication was regarded as the dependent variable.
4. Discussion
Post-urethroplasty complications in children with hypospadias are an important issue that happens inevitably regardless of the surgeon's expertise. Over the last three decades, many operational techniques have been introduced to improve the outcomes and decrease the complications of the surgery. In addition to the surgical method, many factors have been reported which can influence the result of the repair. These factors include the age, severity of the disease, surgeon's expertise, hypospadias type, and suture materials.
Of all participants, 10.3% had postoperative complications in our study which was lower than the previous reports [13,14]. The mean interval between hypospadias repair and complication development was 1.63±1.27 years in the Vicryl group and 2.56±1.32 years in the PDO group. Snodgrass et al. [15] reported that the majority of the complications were apparent at the first post-urethroplasty visit or within the first year following TIP hypospadias repair. Despite the surgeon's advice, some patients referred with delay to the clinic postoperatively. This could justify the interval difference in the Snodgrass and colleaguesʼ study [15].
In this study, we found that proximal and mid-shaft hypospadias increased the odds of developing post-urethroplasty complications. A previous study done by Chung et al. [16] reported that more proximal hypospadias was a risk factor for the development of urethro-cutaneous fistula after hypospadias repair. In addition, Pfistermuller et al. [17] showed a higher complications rate in primary proximal hypospadias repair using the TIP technique in their meta-analysis. Moreover, in two other studies, the proximal type has been cited as a risk factor for repair failure [18,19]. The smallness of the glans, the lesser penile skin shaft, and the severity of chordee account for the increase in the complication rates of hypospadias repair in more proximal types than the distal ones. All the aforementioned points can jeopardize the outcome of the surgery.
Suture composition is an important factor in the outcome of the hypospadias repair. Based on the surgeon's preference, any kind of absorbable suture with enough tensile strength can be used for hypospadias repair. Urethral stricture, meatal stenosis, urethro-cutaneous fistula, and glans dehiscence were more prevalent in the Vicryl group; however, the differences were not statistically significant. In contrast to our result, Cimador et al. [20] and Chung et al. [16] stated that suture material did not affect the outcome of hypospadias repair.
DiSandro and Palmer [5] compared rapidly absorbable sutures with PDO suture and showed a higher incidence rate of urethral stricture in the latter group. However, they did not find any significant difference in postoperative fistula formations based on the suture material [5]. In their study, different surgical methods were used, while we used the same surgical method for all patients. This may be the reason for the discrepancy.
Another study performed by Guarino et al. [21] revealed no association between the suture material and development of post-urethroplasty fistula, wound dehiscence, and infection in children with distal hypospadias. The reason for the difference may be that they only investigated the patients with distal hypospadias which is known for the least post-operative complication formation of another hypospadias type.
Shirazi et al. [22] investigated the outcome of hypospadias repair based on the suture materials in a study conducted on animals. They found better outcomes in the Monocryl and PDO groups. A higher percentage of vessel density and a higher volume of the urethral lumen in the PDO group may explain lower complications in their study. This is in line with results of the present study. The nature of PDO suture which is a long-term absorbable suture with a less inflammatory response in comparison to the Vicryl suture can explain this significant difference.
Similar to the result of the present study, Ulman et al. [4] reported that using Vicryl suture caused more urethro-cutaneous fistula in children who had undergone perimeatal-based flap urethroplasty (Mathieu procedure) for distal hypospadias than PDO suture (16.0% vs. 4.9%, p<0.001).
There are two limitations in our study. This study is a one center case-control study, and we believe that multicenter studies might be more conclusive. In addition, regarding the method, we suggest randomized control trial studies with enough sample size.
5. Conclusion
We suggest PDO suture in the repair of hypospadias due to lower complication rate, especially in the cases of proximal and mid-shaft hypospadias repair; however, multicenter randomized control trial studies with enough sample size are necessary to support our results.
Author contributions
Study concept and design: Mehdi Shirazi, Abdolreza Haghpanah.
Data acquisition: Mehdi Shirazi, Anahita Dehghani, Abdolreza Haghpanah, Mehdi Ghahartars.
Data analysis: Sezaneh Haghpanah, Mahdi Rahmanian.
Drafting of manuscript: Abdolreza Haghpanah, Anahita Dehghani, Sezaneh Haghpanah, Mehdi Ghahrtars, Mahdi Rahmanian.
Critical revision of the manuscript: Abdolreza Haghpanah, Mehdi Shirazi.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Footnotes
Peer review under responsibility of Tongji University.
References
- 1.Kraft K.H., Shukla A.R., Canning D.A. Hypospadias. Urol Clin. 2010;37:167–181. doi: 10.1016/j.ucl.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Baskin L.S., Ebbers M.B. Hypospadias: Anatomy, etiology, and technique. J Pediatr Surg. 2006;41:463–472. doi: 10.1016/j.jpedsurg.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 3.Gilliver S.C., Ashcroft G.S. Sex steroids and cutaneous wound healing: The contrasting influences of estrogens and androgens. Climacteric. 2007;10:276–288. doi: 10.1080/13697130701456630. [DOI] [PubMed] [Google Scholar]
- 4.Ulman I., Erikci V., Avanoglu A., Gokdemir A. The effect of suturing technique and material on complication rate following hypospadias repair. Eur J Pediatr Surg. 1997;7:156–157. doi: 10.1055/s-2008-1071079. [DOI] [PubMed] [Google Scholar]
- 5.DiSandro M., Palmer J.M. Stricture incidence related to suture material in hypospadias surgery. J Pediatr Surg. 1996;31:881–884. doi: 10.1016/s0022-3468(96)90402-9. [DOI] [PubMed] [Google Scholar]
- 6.Snodgrass W. Tubularized, incised plate urethroplasty for distal hypospadias. J Urol. 1994;151:464–465. doi: 10.1016/s0022-5347(17)34991-1. [DOI] [PubMed] [Google Scholar]
- 7.Smith D.P. A comprehensive analysis of a tubularized incised plate hypospadias repair. Urology. 2001;57:778–781. doi: 10.1016/s0090-4295(00)01062-1. discussion 81–2. [DOI] [PubMed] [Google Scholar]
- 8.Sugarman I.D., Trevett J., Malone P.S. Tubularization of the incised urethral plate (Snodgrass procedure) for primary hypospadias surgery. BJU Int. 1999;83:88–90. doi: 10.1046/j.1464-410x.1999.00910.x. [DOI] [PubMed] [Google Scholar]
- 9.Uygur M.C., Erol D., Germiyanoğlu C. Lessons from 197 Mathieu hypospadias repairs performed at a single institution. Pediatr Surg Int. 1998;14:192–194. doi: 10.1007/s003830050484. [DOI] [PubMed] [Google Scholar]
- 10.Koyle M.A. Hypospadias: A 30-year personal journey. Scand J Surg. 2011;100:250–255. doi: 10.1177/145749691110000404. [DOI] [PubMed] [Google Scholar]
- 11.Bellenger C.R. Sutures. Part I. The purpose of sutures and available suture materials. Compend Continuing Educ Pract Vet. 1982;4:507–515. [Google Scholar]
- 12.Boothe H.W. Selecting suture materials for small animal surgery. Compend Continuing Educ Pract Vet. 1998;20:155–163. [Google Scholar]
- 13.Castagnetti M., El-Ghoneimi A. Surgical management of primary severe hypospadias in children: Systematic 20-year review. J Urol. 2010;184:1469–1474. doi: 10.1016/j.juro.2010.06.044. [DOI] [PubMed] [Google Scholar]
- 14.Lu W., Tao Y., Wisniewski A.B., Frimberger D., Kropp B.P. Different outcomes of hypospadias surgery between North America, Europe and China: Is patient age a factor? Nephro-Urol Mon. 2012;4:609–612. doi: 10.5812/numonthly.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snodgrass W., Villanueva C., Bush N.C. Duration of follow-up to diagnose hypospadias urethroplasty complications. J Pediatr Urol. 2014;10:208–211. doi: 10.1016/j.jpurol.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Chung J.-W., Choi S.H., Kim B.S., Chung S.K. Risk factors for the development of urethrocutaneous fistula after hypospadias repair: A retrospective study. Kor J Urol. 2012;53:711–715. doi: 10.4111/kju.2012.53.10.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pfistermuller K.L., McArdle A.J., Cuckow P.M. Meta-analysis of complication rates of the tubularized incised plate (TIP) repair. J Pediatr Urol. 2015;11:54–59. doi: 10.1016/j.jpurol.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Castagnetti M., Zhapa E., Rigamonti W. Primary severe hypospadias: Comparison of reoperation rates and parental perception of urinary symptoms and cosmetic outcomes among 4 repairs. J Urol. 2013;189:1508–1513. doi: 10.1016/j.juro.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 19.Long C.J., Chu D.I., Tenney R.W., Morris A.R., Weiss D.A., Shukla A.R., et al. Intermediate-term followup of proximal hypospadias repair reveals high complication rate. J Urol. 2017;197:852–858. doi: 10.1016/j.juro.2016.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cimador M., Castagnetti M., Milazzo M., Sergio M., De Grazia E. Suture materials: Do they affect fistula and stricture rates in flap urethroplasties? Urol Int. 2004;73:320–324. doi: 10.1159/000081592. [DOI] [PubMed] [Google Scholar]
- 21.Guarino N., Vallasciani S.A., Marrocco G. A new suture material for hypospadias surgery: A comparative study. J Urol. 2009;181:1318–1322. doi: 10.1016/j.juro.2008.10.056. discussion 22–3. [DOI] [PubMed] [Google Scholar]
- 22.Shirazi M., Noorafshan A., Serhan A. Effects of different suture materials used for the repair of hypospadias: A stereological study in a rat model. Urol Int. 2012;89:395–401. doi: 10.1159/000343423. [DOI] [PubMed] [Google Scholar]