Abstract
Background
There are limited data on risk factors for serious outcomes and death from COVID-19 among patients representative of the U.S. population. The objective of this study was to determine risk factors for critical care, ventilation, and death among hospitalized patients with COVID-19.
Methods
This was a cohort study using data from Optum’s longitudinal COVID-19 electronic health record database derived from a network of healthcare provider organizations across the US. The study included patients with confirmed COVID-19 (presence of ICD-10-CM code U07.1 and/or positive SARS-CoV-2 test) between January 2020 and November 2020. Patient characteristics and clinical variables at start of hospitalization were evaluated for their association with subsequent serious outcomes (critical care, mechanical ventilation, and death) using odds ratios (OR) and 95% confidence intervals (CI) from logistic regression, adjusted for demographic variables.
Results
Among 56,996 hospitalized COVID-19 patients (49.5% male and 72.4% ≥ 50 years), 11,967 received critical care, 9136 received mechanical ventilation, and 8526 died. The median duration of hospitalization was 6 days (IQR: 4, 11), and this was longer among patients that experienced an outcome: 11 days (IQR: 6, 19) for critical care, 15 days (IQR: 8, 24) for mechanical ventilation, and 10 days (IQR: 5, 17) for death. Dyspnea and hypoxemia were the most prevalent symptoms and both were associated with serious outcomes in adjusted models. Additionally, temperature, C-reactive protein, ferritin, lactate dehydrogenase, D-dimer, and oxygen saturation measured during hospitalization were predictors of serious outcomes as were several in-hospital diagnoses. The strongest associations were observed for acute respiratory failure (critical care: OR, 6.30; 95% CI, 5.99–6.63; ventilation: OR, 8.55; 95% CI, 8.02–9.11; death: OR, 3.36; 95% CI, 3.17–3.55) and sepsis (critical care: OR, 4.59; 95% CI, 4.39–4.81; ventilation: OR, 5.26; 95% CI, 5.00–5.53; death: OR, 4.14; 95% CI, 3.92–4.38). Treatment with angiotensin-converting enzyme inhibitors/angiotensin receptor blockers during hospitalization were inversely associated with death (OR, 0.57; 95% CI, 0.54–0.61).
Conclusions
We identified several clinical characteristics associated with receipt of critical care, mechanical ventilation, and death among COVID-19 patients. Future studies into the mechanisms that lead to severe COVID-19 disease are warranted.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12879-022-07383-6.
Keywords: Coronavirus, SARS-CoV-2, Risk factors, Death, Biomarkers, Treatments
Introduction
Since coronavirus disease 2019 (COVID-19) first emerged in China in December 2019, there have been over 270 million confirmed cases and 5.3 million deaths worldwide due to COVID-19 as of 15 December 2021, according to the World Health Organization [1]. The United States (US) leads the world in cases (49.8 million) and deaths (792,371) from COVID-19 and these numbers are expected to continue to rise through the start of 2022.
There is significant heterogeneity in the clinical presentation of COVID-19 infection, ranging from patients who are asymptomatic to those with severe disease [2–4]. It is important to determine predictors of serious outcomes as patients may decline rapidly after initially presenting with mild symptoms [5]. Identifying predictors of serious outcomes may enable clinicians to deliver appropriate care to patients early as well as inform interventions to reduce risk of death [6].
The serious outcomes of COVID-19 (e.g., intensive care unit admission, receipt of mechanical ventilation, death) and their preceding risk factors have been identified previously [7–10]. Common factors associated with progression to serious disease include age, male sex, obesity, and comorbid diseases, including diabetes and renal disease. Additionally, it has been recognized that biomarkers, such as C-reactive protein (CRP) and D-dimer, may be associated with serious outcomes. However, studies from early in the pandemic were small and sought to identify the strongest predictors of serious disease and death from a broad set of variables. Further, some of these studies were hospital-based case series and may not be representative of all patients hospitalized with COVID-19 in the United States.
The purpose of this study was to apply an exploratory, data-driven approach to the identification of potential risk factors for serious outcomes among patients with COVID-19 in order to inform clinicians and researchers of characteristics that may be integral to identifying high risk patients. Thus, the objective was to determine demographic and clinical predictors associated with critical care, mechanical ventilation, and death among hospitalized COVID-19 patients in a large electronic health record (EHR) database that is representative of a geographically diverse U.S. population.
Methods
Study design and study population
This was a retrospective cohort study that included patients confirmed with COVID-19 infection between January 2020 and November 2020. Among these patients, a subset of patients hospitalized with COVID-19 was identified from those with an inpatient health care encounter. Confirmation of COVID-19 infection was based on presence of a specific International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) diagnosis code (U07.1) and/or a positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral test. The date of confirmed infection was the earlier of the date of diagnosis or the date of a positive test. The cohort entry date was the earliest date that the patient met both of the following criteria: confirmed COVID-19 infection and admission to the hospital. For patients who were hospitalized prior to contracting COVID-19, the date of cohort entry was the date of confirmed infection. For patients who were confirmed to have COVID-19 before they were admitted to the hospital, the date of cohort entry was date of hospital admission. This approach for assigning cohort entry date allows for the description of clinical characteristics at the time patients were first hospitalized with COVID-19. For clinical characteristics other than death, patients were followed from cohort entry to discharge or 30 days after cohort entry, whichever came first. Deaths were identified in all follow-up available, including during and after hospitalization.
Data source
Patients were identified from Optum’s longitudinal COVID-19 EHR database derived from a network of healthcare provider organizations across the U.S. The COVID-19 EHR database consists of a subset of patients from Optum’s EHR database, which represents a geographically diverse U.S. patient population with more than 85 million patients from 2007 through 2019. Optum’s EHR database includes data collected from tens of thousands of providers and hundreds of hospitals representing more than 60 electronic medical record (EMR)-based provider/hospital networks across the U.S. This database incorporates clinical and medical administrative data from both inpatient and ambulatory EMRs, practice management systems, and numerous other internal systems. Information is processed from across the continuum of care, including acute inpatient stays and outpatient visits. The COVID-19 data captures diagnostics specific to the COVID-19 patient during initial presentation at hospital admission, acute illness, and convalescence with over 500 mapped labs and bedside observations, including COVID-19 specific testing. The data are incorporated into the underlying database on a biweekly basis, allowing for near real-time analysis and assessment of the COVID-19 clinical landscape. The database is certified as de-identified by an independent statistical expert following Health Insurance Portability and Accountability Act statistical de-identification rules.
Ascertainment of covariates
Demographic characteristics were assessed on the date of cohort entry. Comorbidities and medication use were assessed in the 21 days prior to cohort entry. Comorbidities were identified by ICD-10-CM diagnosis code with a diagnosis status of “history of” and medications were mapped according to the Anatomical Therapeutic Chemical (ATC) classification scheme.
Additionally, vital signs, laboratory results, symptoms, diagnoses, and treatments during hospitalization were assessed. For vital signs and laboratory results, the first measurement on or after the date of cohort entry was selected if the patient had multiple measurements. Symptoms and diagnoses were identified by ICD-10-CM diagnosis codes.
Identification of outcomes
The primary outcomes of interest were receipt of critical care, mechanical ventilation, and death. Patients were classified according to the presence or absence of an outcome, and outcome groups were not mutually exclusive.
Receipt of critical care was identified using Current Procedural Terminology, 4th Edition (CPT-4) codes. Receipt of mechanical ventilation was identified by CPT-4 and International Classification of Diseases, 10th Revision, Procedural Coding System (ICD-10-PCS) codes and included intubation, mechanical ventilation, and extracorporeal membrane oxygenation (ECMO). Receipt of critical care and mechanical ventilation were ascertained during hospitalization.
Death was ascertained via linkage to the Social Security Administration’s Death Master File and/or the presence of a death indicator in the structured EHR data within all data available during and after hospitalization.
Statistical analysis
All analyses were conducted using SAS version 9.4 (SAS Institute Inc, Cary, NC). Baseline characteristics were examined overall and according to outcome (critical care, mechanical ventilation, and death). Categorical variables were summarized using frequency and percent while continuous variables were summarized using median and interquartile range (IQR).
For the association analyses, vital signs and laboratory values were transformed into categorical variables. Dichotomous variables were created based on clinically-relevant cutpoints. Additionally, categories based on quintiles were generated to examine the shape of the dose–response relationship of vital signs and laboratory values with each outcome. Quintiles were determined based on the distribution of each biomarker among hospitalized patients overall. Tests for linear trend were computed by using the medians of the quintiles modeled as a continuous variable.
Logistic regression models were used to estimate unadjusted and adjusted odds ratios (OR) and corresponding 95% confidence intervals (CI) for associations between the covariates and each outcome. Adjusted models included age, gender, region, race, and week of cohort entry. Week of cohort entry was included as a covariate to adjust for any potential changes in patient characteristics or treatments over time.
Results
Descriptive analyses
A total of 56,996 hospitalized patients with COVID-19 between January 2020 and November 2020 were identified (Fig. 1). Of these, 11,967 (21.0%) received critical care, 9136 (16.0%) received mechanical ventilation, and 8526 (15.0%) died. Table 1 shows the demographics, comorbidities, and patient-reported medications at baseline overall and according to outcome. The majority of hospitalized patients were aged 50 years and older (72.4%), Caucasian (58.8%), and from the Midwest or Northeast (38.0% and 29.0%, respectively); this was also observed for each outcome. Females comprised 50.5% of hospitalized patients, but males comprised the majority of patients experiencing each outcome (58.8% for critical care, 60.4% for mechanical ventilation, and 57.4% for death). Prior to the cohort entry date, 76.7% of patients received care in the emergency department, while fewer patients received care in the outpatient or inpatient settings. Confirmation of COVID-19 infection was based on both a positive SARS-CoV-2 viral test and presence of a U07.1 diagnosis code for 70.2% of hospitalized patients, a U07.1 diagnosis code only for 26.0% of patients, and a positive SARS-CoV-2 viral test only for 3.8% of patients. The largest proportion of patients were admitted to the hospital in April 2020 (18.3%), followed by November 2020 (17.8%).
Fig. 1.

Flowchart of hospitalized COVID-19 patients: the Optum COVID-19 EHR Database, January–November 2020. *Patients who received critical care and mechanical ventilation were counted in both categories
Table 1.
Baseline characteristics among hospitalized COVID-19 patients, overall and by outcome
| Overall | Critical Care | Mechanical Ventilation | Death | |||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Total patients | 56,996 | 100.0 | 11,967 | 100.0 | 9136 | 100.0 | 8526 | 100.0 |
| Age | ||||||||
| < 10 | 396 | 0.7 | 82 | 0.7 | 29 | 0.3 | 7 | 0.1 |
| 10–19 | 671 | 1.2 | 135 | 1.1 | 46 | 0.5 | 1 | 0.0 |
| 20–29 | 3610 | 6.3 | 293 | 2.4 | 175 | 1.9 | 37 | 0.4 |
| 30–39 | 5123 | 9.0 | 615 | 5.1 | 380 | 4.2 | 110 | 1.3 |
| 40–49 | 5889 | 10.3 | 1,113 | 9.3 | 794 | 8.7 | 285 | 3.3 |
| 50–59 | 9486 | 16.6 | 2,125 | 17.8 | 1605 | 17.6 | 770 | 9.0 |
| 60–69 | 11,871 | 20.8 | 2,926 | 24.5 | 2552 | 27.9 | 1658 | 19.4 |
| 70–79 | 10,396 | 18.2 | 2,621 | 21.9 | 2137 | 23.4 | 2257 | 26.5 |
| 80 + | 9554 | 16.8 | 2,057 | 17.2 | 1418 | 15.5 | 3401 | 39.9 |
| Gender | ||||||||
| Female | 28,782 | 50.5 | 4925 | 41.2 | 3620 | 39.6 | 3636 | 42.6 |
| Male | 28,214 | 49.5 | 7042 | 58.8 | 5516 | 60.4 | 4890 | 57.4 |
| Race | ||||||||
| African American | 11,694 | 20.5 | 2282 | 19.1 | 1873 | 20.5 | 1529 | 17.9 |
| Asian | 1336 | 2.3 | 329 | 2.7 | 250 | 2.7 | 206 | 2.4 |
| Caucasian | 33,524 | 58.8 | 7125 | 59.5 | 5227 | 57.2 | 5536 | 64.9 |
| Other/Unknown | 10,442 | 18.3 | 2231 | 18.6 | 1786 | 19.5 | 1255 | 14.7 |
| Ethnicity | ||||||||
| Hispanic | 8497 | 14.9 | 1711 | 14.3 | 1271 | 13.9 | 814 | 9.5 |
| Not Hispanic | 42,881 | 75.2 | 9079 | 75.9 | 6910 | 75.6 | 6908 | 81.0 |
| Unknown | 5618 | 9.9 | 1177 | 9.8 | 955 | 10.5 | 804 | 9.4 |
| Region | ||||||||
| Midwest | 21,647 | 38.0 | 4979 | 41.6 | 3851 | 42.2 | 2995 | 35.1 |
| Northeast | 16,548 | 29.0 | 3621 | 30.3 | 2516 | 27.5 | 2616 | 30.7 |
| South | 12,654 | 22.2 | 2094 | 17.5 | 1583 | 17.3 | 2114 | 24.8 |
| West | 4378 | 7.7 | 947 | 7.9 | 949 | 10.4 | 560 | 6.6 |
| Other/Unknown | 1769 | 3.1 | 326 | 2.7 | 237 | 2.6 | 241 | 2.8 |
| Care settings prior to admission date | ||||||||
| Inpatient | 4684 | 8.2 | 747 | 6.2 | 736 | 8.1 | 945 | 11.1 |
| Outpatient | 10,479 | 18.4 | 2121 | 17.7 | 1554 | 17.0 | 1253 | 14.7 |
| Emergency department | 43,724 | 76.7 | 9819 | 82.1 | 7615 | 83.4 | 7194 | 84.4 |
| Insurance type on admission date | ||||||||
| Multiple | 16,266 | 28.5 | 3790 | 31.7 | 2831 | 31.0 | 3274 | 38.4 |
| Commercial | 15,775 | 27.7 | 2916 | 24.4 | 2193 | 24.0 | 1134 | 13.3 |
| Medicare | 12,364 | 21.7 | 2854 | 23.8 | 2258 | 24.7 | 2888 | 33.9 |
| Medicaid | 5111 | 9.0 | 1107 | 9.3 | 801 | 8.8 | 354 | 4.2 |
| Other payer type | 2936 | 5.2 | 483 | 4.0 | 364 | 4.0 | 275 | 3.2 |
| Uninsured | 973 | 1.7 | 156 | 1.3 | 109 | 1.2 | 68 | 0.8 |
| Unknown | 3571 | 6.3 | 661 | 5.5 | 580 | 6.3 | 533 | 6.3 |
| Confirmatory event | ||||||||
| Positive SARS-CoV-2 viral test only | 2166 | 3.8 | 258 | 2.2 | 215 | 2.4 | 318 | 3.7 |
| U07.1 diagnosis code only | 14,822 | 26.0 | 3027 | 25.3 | 2367 | 25.9 | 1989 | 23.3 |
| Positive SARS-CoV-2 viral test and U07.1 diagnosis code | 40,008 | 70.2 | 8682 | 72.5 | 6554 | 71.7 | 6219 | 72.9 |
| Month of cohort entry | ||||||||
| January 2020 through March 2020 | 4497 | 7.9 | 1389 | 11.6 | 1397 | 15.3 | 1040 | 12.2 |
| April 2020 | 10,422 | 18.3 | 2924 | 24.4 | 2205 | 24.1 | 2360 | 27.7 |
| May 2020 | 5,859 | 10.3 | 1472 | 12.3 | 994 | 10.9 | 1028 | 12.1 |
| June 2020 | 4611 | 8.1 | 908 | 7.6 | 594 | 6.5 | 593 | 7.0 |
| July 2020 | 6082 | 10.7 | 1136 | 9.5 | 840 | 9.2 | 916 | 10.7 |
| August 2020 | 5013 | 8.8 | 856 | 7.2 | 644 | 7.0 | 721 | 8.5 |
| September 2020 | 4318 | 7.6 | 824 | 6.9 | 575 | 6.3 | 623 | 7.3 |
| October 2020 | 6028 | 10.6 | 1102 | 9.2 | 858 | 9.4 | 776 | 9.1 |
| November 2020 | 10,166 | 17.8 | 1356 | 11.3 | 1029 | 11.3 | 469 | 5.5 |
| Comorbidities | ||||||||
| Diabetes | 16,826 | 29.5 | 4851 | 40.5 | 3918 | 42.9 | 3375 | 39.6 |
| Obesity | 13,544 | 23.8 | 3861 | 32.3 | 3183 | 34.8 | 1893 | 22.2 |
| Pulmonary disease | ||||||||
| COPD | 5830 | 10.2 | 1,812 | 15.1 | 1582 | 17.3 | 1498 | 17.6 |
| Asthma | 4948 | 8.7 | 1,121 | 9.4 | 916 | 10.0 | 510 | 6.0 |
| Cardiovascular disease | ||||||||
| Hypertension | 23,229 | 40.8 | 5855 | 48.9 | 4495 | 49.2 | 4029 | 47.3 |
| Coronary artery disease | 8407 | 14.8 | 2477 | 20.7 | 1986 | 21.7 | 2228 | 26.1 |
| Congestive heart failure | 7242 | 12.7 | 2425 | 20.3 | 2058 | 22.5 | 2246 | 26.3 |
| Kidney disease* | 17,694 | 31.0 | 6103 | 51.0 | 5110 | 55.9 | 5257 | 61.7 |
| Liver disease | 2671 | 4.7 | 985 | 8.2 | 830 | 9.1 | 681 | 8.0 |
| Cancer | 4369 | 7.7 | 1080 | 9.0 | 780 | 8.5 | 1029 | 12.1 |
| Patient-reported medications | ||||||||
| Statins | 14,933 | 26.2 | 3631 | 30.3 | 2975 | 32.6 | 2733 | 32.1 |
| ACEs/ARBs | 11,517 | 20.2 | 2695 | 22.5 | 2256 | 24.7 | 1879 | 22.0 |
| NSAIDS | 5908 | 10.4 | 1092 | 9.1 | 873 | 9.6 | 618 | 7.2 |
| Steroids | 6827 | 12.0 | 1556 | 13.0 | 1144 | 12.5 | 882 | 10.3 |
| PPIs | 9966 | 17.5 | 2269 | 19.0 | 1878 | 20.6 | 1749 | 20.5 |
COPD chronic obstructive pulmonary disease, ACE angiotensin-converting enzyme, ARB angiotensin II receptor blocker, NSAIDS non-steroidal anti-inflammatory drugs, PPIs proton-pump inhibitors, SARS-CoV-2 severe acute respiratory syndrome coronavirus 2
*Includes acute and chronic kidney disease
The most common comorbidities among the patients hospitalized with COVID-19 overall were hypertension (40.8%), kidney disease (31.0%), diabetes (29.5%), and obesity (23.8%) (Table 1). In general, the prevalence of these comorbidities was higher among patients who experienced one of the outcomes of interest, compared to the broader hospitalized population. Among patients who received critical care, 48.9% had hypertension, 51.0% had kidney disease, 40.5% had diabetes, and 32.3% were obese. Among patients who received mechanical ventilation, 49.2% had hypertension, 55.9% had kidney disease, 42.9% had diabetes, and 34.8% were obese. Among patients who died, 47.3% had hypertension, 61.7% had kidney disease, and 39.6% had diabetes; 22.2% were obese, slightly less than hospitalized patients overall. Statins and angiotensin-converting enzyme inhibitors (ACEs)/angiotensin receptor blockers (ARBs) were the most prevalent patient-reported medications (26.2% and 20.2%, respectively, overall).
Table 2 presents the distributions of vital signs, laboratory values, symptoms, diagnoses, and treatments received during hospitalization among COVID-19 patients. The median duration of hospitalization overall was 6 days (IQR: 4, 11). The duration was longer among patients that experienced an outcome: 11 days (IQR: 6, 19) for critical care, 15 days (IQR: 8, 24) for mechanical ventilation, and 10 days (IQR: 5, 17) for death. Among hospitalized patients overall, 6.6% had a temperature > 38 degrees Celsius and 10.1% had an oxygen saturation < 90%. Markers of inflammation and coagulation were elevated for many patients, including 85.7% of patients with C-reactive protein (CRP) > 10 mg/L and 76.8% of patients with D-dimer > 250 ng/mL (DDU).
Table 2.
Laboratory results, symptoms, diagnoses, and interventions during hospitalization among hospitalized COVID-19 patients, overall and by outcome
| Overall | Critical Care | Mechanical ventilation | Death | |||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Duration of Hospitalization (median, IQR) | 6.0 | (4, 11) | 11.0 | (6, 19) | 15.0 | (8, 24) | 10.0 | (5, 17) |
| Observations (median, IQR) | ||||||||
| Temperature, °C | 36.8 | (36.5, 37.1) | 36.8 | (36.5, 37.2) | 36.8 | (36.5, 37.3) | 36.8 | (36.4, 37.4) |
| > 38 | 3,609 | 6.6 | 971 | 8.3 | 929 | 10.4 | 981 | 11.9 |
| Oxygen saturation (SpO2), % | 95.0 | (93.0, 97.3) | 95.0 | (92.0, 97.2) | 95.0 | (92.0, 97.4) | 95.0 | (91.0, 97.0) |
| < 90 | 2457 | 10.1 | 1193 | 14.9 | 1107 | 14.7 | 1051 | 17.6 |
| Platelet count × 109 per L | 224.0 | (169.0, 298.0) | 228.0 | (165.0, 309.0) | 225.0 | (161.0, 306.0) | 200.0 | (143.0, 271.0) |
| < 150 | 9355 | 17.0 | 2324 | 19.7 | 1,879 | 20.8 | 2334 | 28.1 |
| C-reactive protein, mg/L | 60.5 | (21.1, 124.0) | 86.3 | (34.1, 163.0) | 97.7 | (40.3, 178.0) | 107.9 | (51.0, 181.3) |
| > 10 | 30,979 | 85.7 | 8353 | 90.5 | 6469 | 92.1 | 5773 | 94.1 |
| Ferritin, ng/mL | 478.0 | (219.1, 942.0) | 632.0 | (309.0, 1175.5) | 673.1 | (338.0, 1284.7) | 689.0 | (339.1, 1309.9) |
| > 300 | 22,216 | 66.3 | 6371 | 75.6 | 5141 | 78.0 | 4394 | 78.3 |
| Lactate dehydrogenase, U/L | 310.0 | (232.0, 428.0) | 377.0 | (277.0, 526.0) | 406.0 | (294.0, 566.0) | 405.0 | (285.0, 571.0) |
| > 280 | 19,726 | 58.9 | 6235 | 73.9 | 5266 | 78.4 | 4384 | 75.8 |
| D-Dimer, ng/mL | 465.0 | (264.0, 880.0) | 680.0 | (376.5, 1345.0) | 773.8 | (429.5, 1616.0) | 855.0 | (480.0, 1695.0) |
| > 250 | 19,021 | 76.8 | 5024 | 87.2 | 4006 | 89.7 | 3587 | 92.5 |
| Fibrinogen, mg/dL | 529.0 | (403.0, 667.0) | 546.0 | (400.0, 700.0) | 557.0 | (403.0, 700.0) | 537.0 | (394.0, 693.0) |
| > 400 | 12,116 | 75.5 | 3750 | 74.9 | 3309 | 75.2 | 2501 | 74.2 |
| Symptoms | ||||||||
| Hypoxemia | 14,718 | 25.8 | 3968 | 33.2 | 3231 | 35.4 | 2719 | 31.9 |
| Fever | 9158 | 16.1 | 2617 | 21.9 | 2035 | 22.3 | 1641 | 19.2 |
| Cough | 7182 | 12.6 | 1656 | 13.8 | 1266 | 13.9 | 1032 | 12.1 |
| Nausea/Vomiting | 3711 | 6.5 | 814 | 6.8 | 547 | 6.0 | 345 | 4.0 |
| Malaise and fatigue | 7483 | 13.1 | 2242 | 18.7 | 1723 | 18.9 | 1484 | 17.4 |
| Dyspnea or shortness of breath | 15,979 | 28.0 | 4472 | 37.4 | 3781 | 41.4 | 2971 | 34.8 |
| Diagnoses | ||||||||
| Acute respiratory failure | 25,525 | 44.8 | 9472 | 79.2 | 7825 | 85.7 | 6187 | 72.6 |
| Pneumonia | 33,946 | 59.6 | 9771 | 81.6 | 7738 | 84.7 | 6565 | 77.0 |
| Sepsis | 12,646 | 22.2 | 5812 | 48.6 | 4995 | 54.7 | 4168 | 48.9 |
| Coagulation defects or hemorrhagic conditions | 3490 | 6.1 | 1715 | 14.3 | 1456 | 15.9 | 1101 | 12.9 |
| Arrhythmia | 4799 | 8.4 | 2112 | 17.6 | 1772 | 19.4 | 1439 | 16.9 |
| Heart failure | 7934 | 13.9 | 2775 | 23.2 | 2380 | 26.1 | 2441 | 28.6 |
| MI | 3437 | 6.0 | 1535 | 12.8 | 1293 | 14.2 | 1251 | 14.7 |
| Kidney disease* | 17,694 | 31.0 | 6103 | 51.0 | 5110 | 55.9 | 5257 | 61.7 |
| Liver disease | 2671 | 4.7 | 985 | 8.2 | 830 | 9.1 | 681 | 8.0 |
| Treatments | ||||||||
| Chloroquine/Hydroxychloroquine | 8852 | 15.5 | 2805 | 23.4 | 2632 | 28.8 | 2084 | 24.4 |
| Lopinavir/Ritonavir | 427 | 0.7 | 205 | 1.7 | 181 | 2.0 | 166 | 1.9 |
| Remdesivir | 12,990 | 22.8 | 3274 | 27.4 | 2829 | 31.0 | 1901 | 22.3 |
| Dexamethasone | 16,698 | 29.3 | 3968 | 33.2 | 3582 | 39.2 | 2520 | 29.6 |
| ACEs/ARBs | 12,313 | 21.6 | 2492 | 20.8 | 2112 | 23.1 | 1546 | 18.1 |
| Anticoagulants | 45,509 | 79.8 | 10,569 | 88.3 | 8286 | 90.7 | 7362 | 86.3 |
| Immunosuppressants | 3009 | 5.3 | 1409 | 11.8 | 1344 | 14.7 | 799 | 9.4 |
| Antibacterials for systemic use | 38,050 | 66.8 | 9373 | 78.3 | 7927 | 86.8 | 6967 | 81.7 |
| Antivirals for systemic use | 1847 | 3.2 | 633 | 5.3 | 555 | 6.1 | 434 | 5.1 |
| Corticosteroids for systemic use | 26,615 | 46.7 | 6897 | 57.6 | 6320 | 69.2 | 4699 | 55.1 |
MI myocardial infarction, ACE angiotensin-converting enzyme, ARB angiotensin II receptor blocker, ICU intensive care unit
*Includes acute and chronic kidney disease
The most common symptoms during hospitalization among COVID-19 patients were dyspnea (28.0%) and hypoxemia (25.8%) (Table 2). Prevalence of these symptoms was higher among patients who received critical care (37.4% and 33.2%, respectively), those who received ventilation (41.4% and 35.4%, respectively), and those who died (34.8% and 31.9%, respectively). Relatedly, the most prevalent diagnoses during hospitalization among patients overall were pneumonia (59.6%) and acute respiratory failure (44.8%). These diagnoses were even more common among those with an outcome, with the highest prevalence observed among patients that received mechanical ventilation (acute respiratory failure, 85.7%; pneumonia, 84.7%). Anticoagulants were the most prevalent treatment, received by 79.8% of hospitalized patients with COVID-19 overall during their hospitalization. Among other treatments, 15.5% of patients received chloroquine or hydroxychloroquine, 29.3% received dexamethasone, and 22.8% received remdesivir.
Associations between covariates and serious outcomes
Baseline demographics and comorbidities
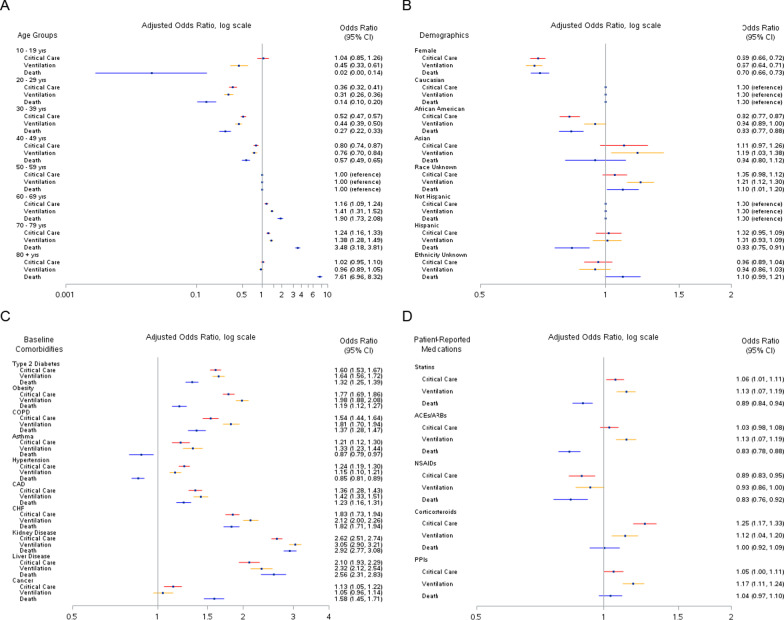
Figure 2 presents the associations between baseline characteristics and receipt of critical care, ventilation, and death adjusted for age, gender, region, race, and week of cohort entry. Unadjusted ORs for the associations between covariates and outcomes are provided in Additional file 1: Tables S1–S3. Age was associated with all 3 outcomes, particularly death; the OR for patients ≥ 80 years of age compared to those 50–59 years of age was 7.61 (95% CI, 6.96–8.32) (Fig. 2A). Female patients were less likely to experience any of the 3 outcomes compared to males. Regarding race, hospitalized patients that received critical care, ventilation, or died were less likely to be African American compared to Caucasian (critical care: OR, 0.82; 95% CI, 0.77–0.87; mechanical ventilation: OR, 0.94; 95% CI, 0.89–1.00; death: OR, 0.83; 95% CI, 0.77–0.88) (Fig. 2B).
Fig. 2.
Associations between Baseline Characteristics and Critical Care, Mechanical Ventilation, and Death among Hospitalized COVID-19 Patients. A Age groups; B Demographics; C Baseline comorbidities; D Patient-reported medications. COPD, chronic obstructive pulmonary disease; CAD, coronary artery disease; CHF, congestive heart failure; ACE, angiotensin-converting enzyme; ARB, angiotensin II receptor blocker; NSAIDS, non-steroidal anti-inflammatory drugs; PPIs, proton-pump inhibitors. Logistic regression models were used to estimate odds ratios (OR) and corresponding 95% confidence intervals (CI) adjusted for age, gender, region, race, and week of cohort entry
After adjusting for demographic variables, several comorbidities at baseline were associated with serious outcomes (Fig. 2C). Comorbidities associated with higher odds of all 3 outcomes included diabetes, obesity, chronic obstructive pulmonary disease, coronary artery disease, congestive heart failure, kidney disease, and liver disease. Asthma, hypertension, and cancer showed varying associations with each outcome. In the unadjusted model, hypertension was positively associated with death (OR, 1.37; 95% CI, 1.30–1.43; Additional file 1: Table S3). However, once adjusted for demographic variables, there was an inverse association between hypertension and death (OR, 0.85; 95% CI, 0.81–0.89). Asthma was associated with higher odds of critical care (OR, 1.21; 95% CI, 1.12–1.30) and ventilation (OR, 1.33; 95% CI, 1.23–1.44), but lower odds of death (OR, 0.87; 95% CI, 0.79–0.97).
Among select patient-reported medications at baseline, use of statins, corticosteroids, and PPIs was positively associated with receipt of critical care and ventilation, but not death (Fig. 2D). Statins, ACEs/ARBs, and NSAIDs showed inverse associations with death.
Vital signs and laboratory values
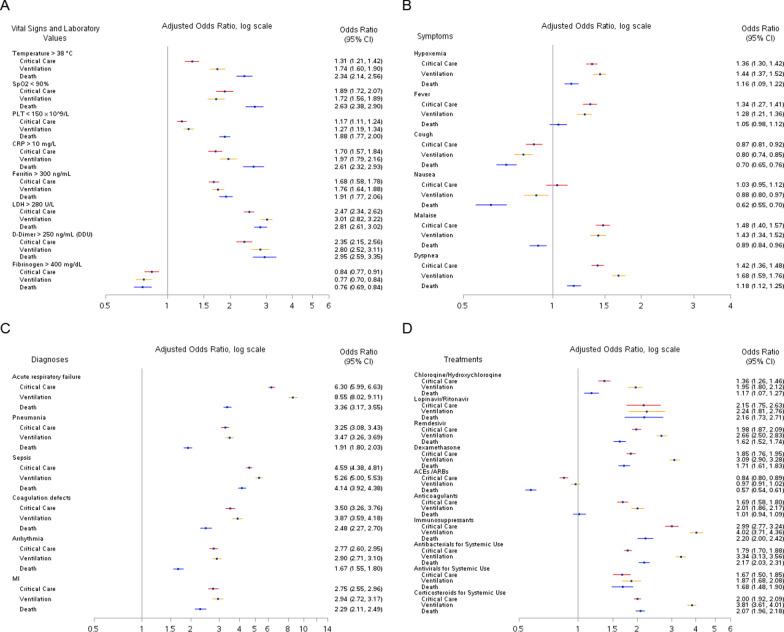
Figure 3 presents the adjusted ORs for the associations between clinical characteristics during hospitalization and receipt of critical care, ventilation, and death among hospitalized patients with COVID-19. Measurements of temperature, CRP, ferritin, lactate dehydrogenase (LDH), and D-dimer that exceeded the clinically-relevant cutpoint were significantly associated with an increased risk of all 3 serious outcomes in adjusted models (Fig. 3A). Likewise, measurements of oxygen saturation and platelets that were less than the clinically-relevant cutpoint were also significantly associated with an increased risk of all 3 serious outcomes. D-dimer and LDH measured during hospitalization had the highest adjusted ORs for the association with death: OR, 2.95 (95% CI, 2.59–3.35) for D-dimer > 250 ng/mL (DDU) and OR, 2.81 (95% CI, 2.61–3.02) for LDH > 280 U/L. Fibrinogen > 400 mg/dL was associated with a lower risk of all 3 outcomes.
Fig. 3.
Associations between Clinical Variables During Hospitalization and Critical Care, Mechanical Ventilation, and Death among Hospitalized COVID-19 Patients. A Vital signs and laboratory values; B Symptoms; C Diagnoses; D Treatments. SpO2, oxygen saturation; PLT, platelet count; CRP, C-reactive protein; LDH, lactate dehydrogenase; MI, myocardial infarction; ACE, angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor blocker Logistic regression models were used to estimate odds ratios (OR) and corresponding 95% confidence intervals (CI) adjusted for age, gender, region, race, and week of cohort entry
The associations between each biomarker in quintiles and serious outcomes are shown in Fig. 4. For CRP, D-dimer, ferritin, and LDH, the relationships appeared linear for all 3 outcomes (p values for linear trend < 0.0001, Additional file 1: Tables S1–S3). For temperature, oxygen saturation, and platelets, the relationships were less linear, although many of the p values for linear trend were < 0.0001. For fibrinogen, the associations with all 3 outcomes were non-linear, with p values of 0.44 for critical care, 0.92 for mechanical ventilation, and 0.09 for death. The biomarkers that showed the strongest associations with outcomes were LDH and D-dimer. The ORs for the 5th (> 466 U/L) versus 1st (< 215 U/L) quintiles of LDH were 4.75 (95% CI, 4.35–5.19) for critical care, 6.84 (95% CI, 6.16–7.58) for ventilation, and 6.97 (95% CI, 6.23–7.79) for death. Likewise, for D-dimer, the ORs for the 5th (> 1030 ng/mL) versus 1st quintile (< 230 ng/mL) were 4.34 (95% CI, 3.89–4.84) for critical care, 5.90 (95% CI, 5.19–6.71) for ventilation, and 6.07 (95% CI, 5.21–7.08) for death (Additional file 1: Tables S1–S3).
Fig. 4.
Associations between Vital Signs and Laboratory Markers During Hospitalization and Critical Care, Mechanical Ventilation, and Death among Hospitalized COVID-19 Patients. A C-reactive protein; B D-dimer; C Ferritin; D Fibrinogen; E Lactate dehydrogenase; F Platelets; G Oxygen saturation; H Temperature. SpO2, oxygen saturation; CRP, C-reactive protein; LDH, lactate dehydrogenase; Logistic regression models were used to estimate odds ratios (OR) and corresponding 95% confidence intervals (CI) adjusted for age, gender, region, race, and week of cohort entry
Symptoms and diagnoses during hospitalization
Dyspnea and hypoxemia were positively associated with all 3 serious outcomes in adjusted models, with both showing the strongest association with receipt of ventilation (dyspnea: OR, 1.68; 95% CI, 1.59–1.76; hypoxemia: OR, 1.44; 95% CI, 1.37–1.52) (Fig. 3B). In contrast, cough was associated with lower odds of all 3 outcomes (critical care: OR, 0.87; 95% CI, 0.81–0.92; mechanical ventilation: OR, 0.80; 95% CI, 0.74–0.85; death: OR, 0.70; 95% CI, 0.65–0.76). Patients with nausea and vomiting as well as malaise also had lower odds of death.
All selected in-hospital diagnoses showed positive associations with each of the 3 serious outcomes (Fig. 3C). The strongest associations were observed for acute respiratory failure (critical care: OR, 6.30; 95% CI, 5.99–6.63; ventilation: OR, 8.55; 95% CI, 8.02–9.11; death: OR, 3.36; 95% CI, 3.17–3.55) and sepsis (critical care: OR, 4.59; 95% CI, 4.38–4.81; ventilation: OR, 5.26; 95% CI, 5.00–5.53; death: OR, 4.14; 95% CI, 3.92–4.38).
Treatments received during hospitalization
With the exception ACEs/ARBs, all of the selected treatments were associated with higher odds of serious outcomes (Fig. 3D). The highest ORs were observed for the associations between treatments and receipt of ventilation, ranging from 1.87 (95% CI, 1.68–2.08) for antivirals to 4.02 (95% CI, 3.71–4.36) for immunosuppressants. Treatment with ACEs/ARBs was inversely associated with receipt of critical care (OR, 0.84; 95% CI, 0.80–0.89) and death (OR, 0.57; 95% CI, 0.54–0.61).
Discussion
In this study, we identified and described patients who experienced a serious outcome (critical care, mechanical ventilation, and death) among 56,996 hospitalized patients with COVID-19 within a large, EHR database. We conducted an evaluation of the association of many demographic and clinical characteristics with these outcomes in order to identify potential signals for experiencing a serious outcome. As was observed in prior studies [7–10], older age and male gender were associated with higher risk of serious outcomes, along with comorbidities such as diabetes and kidney disease. We also observed associations with clinical characteristics measured during hospitalization, including several laboratory markers, symptoms, and diagnoses.
In this study of hospitalized patients with COVID-19, we found that African-Americans and women were at lower risk of experiencing a serious outcome compared to Caucasians and men, respectively. Since the start of the pandemic, African-Americans have been more likely than Caucasians to contract and be hospitalized with COVID-19 [11]. Nonetheless, evidence suggests that once hospitalized, they do not have a higher risk of adverse outcomes [10, 12–14]. In contrast, there does not appear to be sex difference in number of confirmed cases of COVID-19, but the death rate has been higher in men than women [15]. The reason for the sex difference in rate of mortality among patients with COVID-19 remains unknown, but it has been suggested that the mechanism involves a combination of biological and psychosocial factors [16].
Hypertension was the most prevalent comorbidity among hospitalized COVID-19 patients in this study and its prevalence was even higher among patients with a serious outcome. Hypertension was positively associated with receipt of critical care and mechanical ventilation, but inversely associated with mortality after adjusting for age and other demographics. Findings in this study are consistent with previous studies that have found hypertension to be common among adults diagnosed with COVID-19, but not associated with mortality after adjusting for covariates [14, 17]. Thus, while there may be overrepresentation of hypertension among adults with COVID-19, it appears this association may be confounded by age and other covariates, and possibly affected by treatment.
In the current study, treatment with ACEs/ARBs during hospitalization was associated with lower odds of critical care and mortality. It is recommended that patients who are prescribed ACEs/ARBs for cardiovascular disease continue taking these medications if hospitalized with COVID-19 [18, 19]. With the exception of ACEs/ARBs, we observed that many treatments received during hospitalization were associated with higher odds of receipt of critical care, mechanical ventilation, or death. An explanation for this finding may be that most medications, particularly those that were investigational, were only recommended for use among patients with severe disease. For example, remdesivir and dexamethasone are recommended for hospitalized COVID-19 patients that require supplemental oxygen [19]. As of 15 December 2021, remdesivir is the only FDA-approved drug for the treatment of COVID-19, although emergency use authorizations have been issued for multiple anti-SARS-CoV-2 monoclonal antibody products (i.e., bamlanivimab plus etesevimab, casirivimab plus imdevimab, and sotrovimab) [19]. Other medications are under investigation.
Several vital signs and laboratory results were associated with serious outcomes in COVID-19 patients in this study, with the strongest associations observed for LDH, D-dimer, and CRP. LDH is an enzyme found within cells in almost all organ systems [20]. Its levels rise when the body’s tissues are damaged. Recent studies have found that high levels of LDH may be predictive of COVID-19 severity and death [17, 20]. Similarly, increased D-dimer, an indicator of coagulopathy, has been linked to higher risk of mortality in COVID-19 patients [8, 21]. CRP is an inflammatory marker and has been shown to be elevated in patients with severe COVID-19 disease [9, 12, 22]. The findings in the current study are consistent with these smaller studies and, taken together, suggest these laboratory markers, if measured soon after admission, may help clinicians triage patients who may be at higher risk of progression to severe disease.
The current study was based on an analysis of EHR data, which are valuable for the examination of clinical health outcomes and treatment patterns. Nonetheless, all EHR databases have inherent limitations because the data are collected for the purpose of clinical patient management, not research. Unlike in clinical trials, where the collection of clinical and laboratory measures is standardized, the Optum EHR includes real-world clinical data obtained from multiple medical and laboratory settings used for patient care. Because data are not collected in a systematic way, clinical measurements (e.g., vital signs and laboratory results) were not available for all patients.
Additionally, the presence of a diagnosis code in EHR data may not represent the actual presence of disease, as the diagnosis code may be incorrectly coded, or included as rule-out criteria rather than actual disease. We assumed the absence of a diagnosis code meant the patient did not have the disease. This assumption may be a reason why we observed an inverse association between cough and serious outcomes; in a patient who is very ill, severe symptoms like dyspnea and hypoxemia may be more likely to be recorded than minor symptoms such as cough. Furthermore, it is possible that some comorbidities and medications may not have been captured as health care encounters with medical providers who do not contract with Optum would not be observed.
The median duration of hospitalization among patients who died was 10 days. However, deaths were identified within all data available, not only during hospitalization. As such, it is possible that duration of hospitalization may have been shorter among patients that died during hospitalization. An additional limitation of the EHR database is the data lag at the time of data extraction, which likely resulted in an underestimation of the number of deaths. Finally, residual confounding is a concern as we only adjusted for demographic covariates.
Conclusion
In summary, we utilized an exploratory, data-driven approach to identify many clinical characteristics that were associated with receipt of critical care, mechanical ventilation, and death among patients hospitalized with COVID-19. As more continues to be learned about COVID-19 by clinicians and researchers, future studies should move toward causal inference and focus on identifying the etiologic factors and mechanisms responsible for some patients experiencing more severe COVID-19 disease.
Supplementary Information
Acknowledgements
The authors would like to acknowledge Katherine Reed for her technical assistance in preparing the manuscript.
Abbreviations
- ACE
Angiotensin-converting enzyme inhibitor
- ARB
Angiotensin receptor blockers
- ATC
Anatomical therapeutic chemical
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
- CPT-4
Current Procedural Terminology, 4th Edition
- CRP
C-reactive protein
- ECMO
Extracorporeal membrane oxygenation
- EHR
Electronic health record
- EMR
Electronic medical record
- ICD-10-CM
International Classification of Diseases, 10th Revision, Clinical Modification
- ICD-10-PCS
International Classification of Diseases, 10th Revision, Procedural Coding System
- IQR
Interquartile range
- LDH
Lactate dehydrogenase
- NSAID
Nonsteroidal anti-inflammatory drug
- OR
Odds ratio
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- US
United States
Author contributions
AKC, CL, NDL, FTW, JDS contributed to the study concept and design. NDL, FTW, and JDS acquired the data. AKC and CL drafted the manuscript. MCD, CRC, RPO, RVG, JNS, CE, NDL, FTW, and JDS critically revised the manuscript for important intellectual content. All authors contributed to the analysis and interpretation of data. All authors read and approved the final manuscript.
Funding
This work was funded by Optum Epidemiology.
Availability of data and materials
The de-identified database used for the current study is not publicly available, but is available from Optum through a data license agreement. More information can be found at the following website: https://www.optum.com/business/solutions/life-sciences/real-world-data/ehr-data.html.
Declarations
Ethics approval and consent to participate
Not applicable because this study utilized a commercially available, de-identified database. No administrative permissions were required for this study as this database has been certified as de-identified by an independent statistical expert following Health Insurance Portability and Accountability Act statistical de-identification rules and managed according to Optum® customer data use agreements. As no study team members had access to patient identifiers linked to the data, review by an ethics committee or institutional review board was not required, nor was consent to participate.
Consent for publication
Not applicable.
Competing interests
AKC, CL, MCD, CRC, RPO, RVG, JNS, CE, FTW, and JDS are employees of Optum receiving stock and/or stock options in UnitedHealth Group. NDL was formerly an employee of Optum and is currently an employee of IQVIA.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Andrea K. Chomistek and Caihua Liang contributed equally as first authors
References
- 1.WHO Coronavirus Disease (COVID-19) Dashboard. [cited 2021 December 15]; Available from: https://covid19.who.int/.
- 2.Chen N, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson S, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Traversi D, et al. Precision medicine and public health: new challenges for effective and sustainable health. J Pers Med. 2021;11(2):135. doi: 10.3390/jpm11020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liang W, et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. 2020;180(8):1081–1089. doi: 10.1001/jamainternmed.2020.2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou F, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berenguer J, et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain. Clin Microbiol Infect. 2020. [DOI] [PMC free article] [PubMed]
- 10.Kim L, et al. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the U.S. coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET) Clin Infect Dis. 2020;72:e206. doi: 10.1093/cid/ciaa1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVID-19 Hospitalization and Death by Race/Ethnicity. [cited 2020 November 17]; Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html.
- 12.Garibaldi BT et al. Patient trajectories among persons hospitalized for COVID-19: a cohort study. Ann Intern Med. 2020. [DOI] [PMC free article] [PubMed]
- 13.Price-Haywood EG, et al. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suleyman G, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan detroit. JAMA Netw Open. 2020;3(6):e2012270. doi: 10.1001/jamanetworkopen.2020.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The COVID-19 Sex-Disaggregated Data Tracker. [cited 2020 December 12]; Available from: https://globalhealth5050.org/the-sex-gender-and-covid-19-project/.
- 16.Griffith DM, et al. Men and COVID-19: a biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Prev Chronic Dis. 2020;17:E63. doi: 10.5888/pcd17.200247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao Z, et al. Prediction model and risk scores of ICU admission and mortality in COVID-19. PLoS ONE. 2020;15(7):e0236618. doi: 10.1371/journal.pone.0236618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lopes R, o.b.o.t.B.C.I. Continuing versus suspending ACE inhibitors and ARBs: impact of adverse outcomes in hospitalized patients with COVID-19—the BRACE CORONA Trial. in European Society of Cardiology 2020 Congress. 2020.
- 19.Panel C-TG. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. [cited 2021 December 15]; Available from: https://www.covid19treatmentguidelines.nih.gov/. [PubMed]
- 20.Henry BM, et al. Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: a pooled analysis. Am J Emerg Med. 2020;38(9):1722–1726. doi: 10.1016/j.ajem.2020.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang N, et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manson JJ, et al. COVID-19-associated hyperinflammation and escalation of patient care: a retrospective longitudinal cohort study. Lancet Rheumatol. 2020;2(10):e594–e602. doi: 10.1016/S2665-9913(20)30275-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The de-identified database used for the current study is not publicly available, but is available from Optum through a data license agreement. More information can be found at the following website: https://www.optum.com/business/solutions/life-sciences/real-world-data/ehr-data.html.