Never before has the field of heart failure seen such accelerated advancements in medical and device therapies. The expansion of knowledge, albeit progressively over the last 5 decades with more rapid recent advances, provides heart failure specialists with a multitude of treatment options supported by a strong foundation of evidence. Nonetheless, the concurrent increasing prevalence of heart failure challenges the cardiology workforce to provide adequate care. Recently, the Journal of Cardiac Failure featured an article by Chuzi and Reza1 highlighting the need to cultivate interest in heart failure careers, rightfully suggesting the need to strengthen the advanced heart failure workforce. However, as it stands, heart failure is still an all-consuming cardiovascular disease, advancing much faster than the advanced heart failure workforce can handle. In addition, many advanced heart failure and transplant training programs remained unfilled to date. Thus, the need for dedicated specialized training to achieve the demanding competencies of heart failure may require further strategic development of training programs to manage preventive, early, and symptomatic heart failure stages.
Advanced practice practitioner (APP), pharmacy, and nursing programs have revolutionized heart failure management for several decades now. A recent systematic review evaluating studies including a total of 43,754 patients concluded the involvement of advanced practice nurses significantly decreased hospital admissions and the mortality of patients with heart failure, thereby increasing the cost effectiveness of care.2 Many APPs contribute to heart failure research efforts, emphasizing the need to improve health literacy, patient-reported outcomes, and self-care and education of patients with heart failure. Thus, the inclusion of the APP role in heart failure management has significantly improved the field.
Pharmacist-led interventions also contribute powerful benefits to patients receiving heart failure care, with associations of significantly decreased heart failure readmissions in several studies.3 Pharmacists have also become increasingly important in managing diabetes, hypertension, and other chronic diseases that share similar treatment goals and therapies with heart failure. As the evidence builds for the benefits of drug classes with multiple treatment effects in heart failure, such as sodium-glucose cotransporter-2 inhibitors, pharmacists are essential in providing information to patients and other health care professionals to improve evidence-based management. Thus, the laudable expansions of provider-care models are critical for the optimization of heart failure management.
Training of Heart Failure–Focused General Cardiologists
The heart failure burden is steadily increasing, projected to affect >8 million Americans by 2030.4 However, fewer than 3700 patients in the United States will receive a cardiac transplant in any given year.5 Although transplant numbers have increased over time, the availability is modest compared to the number of people who develop end-stage heart failure each year. Ventricular assist devices (VADs) offer bridge support to orthotopic heart transplantation (OHT) and end-stage therapy in others. Still, these treatments are not routinely offered as optimal therapy to a large number of patients for a multitude of reasons, including health care access and social support systems. Even so, the spectrum of heart failure includes patients at risk, those with asymptomatic cardiac dysfunction, and those with symptomatic or advanced disease. One-third of all US adults have at least 1 heart failure risk factor (ie, hypertension, diabetes, coronary heart disease, obesity, and smoking), accounting for more than 50% of the overall population-attributable risk.3 Although the prevalence of heart failure stages is unique to the observed population, stage A or B heart failure significantly increases the lifetime risk of worsening heart failure stages and morbidity. Despite an ever-present emphasis on the disparities in heart failure care, underrepresented populations continue to suffer worse outcomes.6–9
The American College of Cardiology Core Cardiology (ACC) Training Symposium, currently in its fourth iteration as of 2015, issued a potential competency pathway for level II heart failure training, rendering certain physicians the ability to provide more specialized care in this specific area.10 Depending on one’s interests or career goals, a trainee can develop the skills to care for a wide range of patients with heart failure after fellowship. A recent statement by Yancy et al concerning the lifelong learning of an advanced heart failure cardiologist also serves as an excellent guide to define the role of a general heart failure (GEN-HF) cardiologist. While serving as a report of the ACC Competency Management Committee, the statement fittingly complements the Core Cardiovascular Training Statements of advanced heart failure training. Based on these training reports, there are more than enough data to guide the education and development of the GEN-HF cardiologist.
Training programs should also consider collaboration with the Accreditation Council for Graduate Medical Education to develop nontransplant and mechanical support heart failure tracks, including tracks with an interventional focus. The GEN-HF fellowship track should include the management of patients with advanced heart failure, thereby strengthening the conviction of a trainee to emphasize preventive strategies to less severely ill patients with heart failure. Adamson et al11 published an interesting viewpoint discussing the possibility of an interventional heart failure training track to increase the competencies of a GEN-HF cardiologist in device implant and management. Specifically, this track recommended 2 years of a general cardiology curriculum before advancing to the interventional training track. Innovative training pathways such as this may require exploration to diversify heart failure training and the overall workforce. This type of innovative heart failure training is essential as heart failure care extends to focus on preventive strategies and patient-related outcomes.
The certification process of a GEN-HF cardiologist remains undefined. Before the American Board of Internal Medicine (ABIM) advanced heart failure certification, the cardiovascular disease certification provided by the ABIM was the acceptable benchmark for any cardiologist pursuing a career in heart failure. However, as therapies and evidence-based management continue to build, the heart failure community rightfully developed the advanced training pathway and certification to achieve competency over time.12 Thus, the advanced heart failure physician is equipped with the complex knowledge to serve patients requiring VAD/OHT therapies to optimize survival and other spectrums of the condition. Many of the competencies achieved with advanced heart failure training are also very necessary for the GEN-HF cardiologist. Although it is entirely possible to outfit one’s fellowship training to a dedicated GEN-HF career, the Heart Failure Society of America (HFSA) and the European Society of Cardiology now provide additional certification opportunities for physicians who desire a career in non-VAD/OHT heart failure.
The HFSA Heart Failure Certification (HF-Cert) program is currently under development to recognize providers who have demonstrated specialized knowledge and skill to provide competent heart failure services in the United States.13 The HF-Cert program is set to launch and was recently discussed at the 2021 HFSA national conference. This certification process is available to physicians and registered nurses, pharmacists, and APPs. However, the question remains whether this certification program is adequate for an ABIM board-certified physician in cardiovascular disease. The Heart Failure Association of the European Society of Cardiology also provides similar certification, although only Heart Failure Association physician members with national board certification in cardiology (diploma) or a physician in cardiology training are eligible to take the examination.14 Additional advanced heart failure training does not seem to be a prerequisite for the examination. Further discussions of non-VAD/OHT certification for ABIM cardiologists are likely to evolve to ensure proper recognition and, more important, recognize the competency to support the scope of work for these cardiologists.
Suggestions to Broaden the Criteria of a Heart Failure Cardiologist
In reality, the GEN-HF cardiologist role occurs already, yet some of these clinicians may not feel recognized within the larger heart failure community. Reasons for this belief may be related to the board certification for advanced heart failure specialists, possibly conveying an ostracized perception for cardiologists who do not practice VAD/OHT or mechanical circulatory support management. Yet, GEN-HF cardiologists have dedicated their careers to preventing and managing heart failure across the disease spectrum. Therefore, as the HFSA continues to support the diversity and inclusion of all who specialize in the multidisciplinary management of heart failure, recognition of the GEN-HF cardiologist will further these efforts.
The GEN-HF career trajectory may also be attractive to many training cardiologists who desire a broader focus on heart failure management (Fig. 1). There is potential to specialize in non-VAD/OHT/mechanical circulatory support heart failure training during cardiology fellowship, which may be better suited to manage aspects of heart failure such as heart failure with preserved ejection fraction, ambulatory telehealth hemodynamic management, and many others. A non-VAD/OHT heart failure trained physician will indeed need to have a working knowledge of both current and future advancements in the field, which is why lifelong learning for all heart failure physicians should be the standard.
Fig. 1.
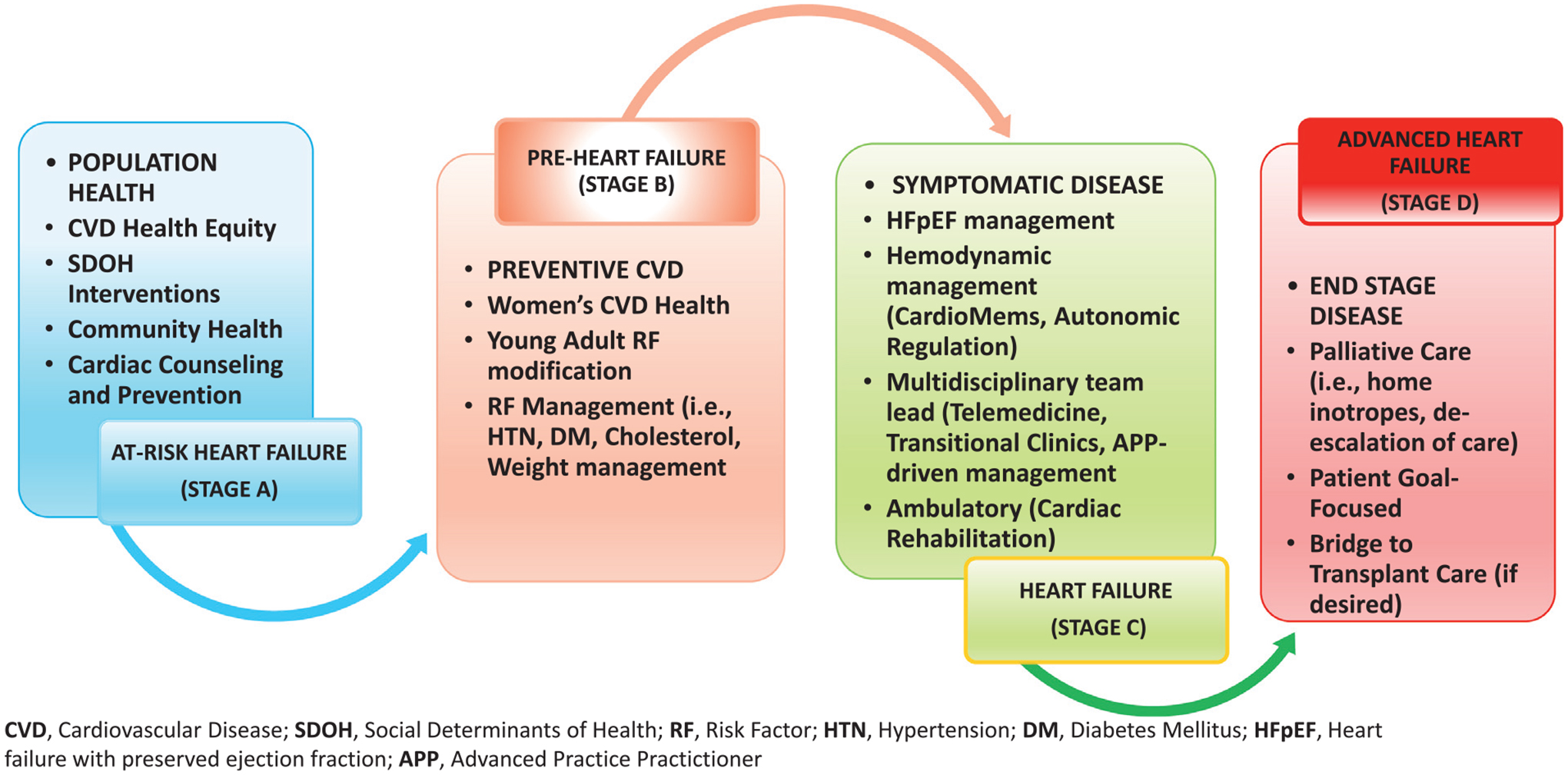
Clinical opportunities for the nontransplant heart failure cardiologist. CVD, cardiovascular disease; SDOH, social determinants of health; RF, risk factor; HTN, hypertension; DM, diabetes mellitus; HFpEF, heart failure with preserved ejection fraction; APP, advanced practice practitioner.
Prevention
The GEN-HF cardiologists who contribute to preventive strategies are essential as well. Only 5% of the 6.2 million patients with heart failure will progress to advanced or stage D disease per year,8 which equates to approximately 300,000 additional patients with heart failure. As suggested, even with the increased therapies for advanced heart failure, this per year increase is still significantly more than the current advanced heart failure workforce can handle. Owing to hospitalizations and end-stage care, patients with stage D heart failure consume a significant percentage of the health care expenditures for heart failure.15 Therefore, management should emphasize primary and secondary prevention strategies in the majority of patients with heart failure (stages A–C) and identification of patients suffering from progressive symptoms (stage D)9 who require earlier referrals to advanced heart failure centers.
Heart Failure Research
The inclusion of the GEN-HF cardiologist in the leadership, design, planning, and execution of heart failure clinical trials is essential. Often, general cardiologists take care of most patients with heart failure eligible for clinical trials. Thus, the participation of the GEN-HF cardiologist will expand the scope and the diversity of recruited clinical trial participants; most of the trials enroll patients with stage C heart failure. The collegial relationship and a high level of trust between the GEN-HF cardiologist and other internal medicine practitioners (ie, hospitalists, primary care physicians, APPs) may further facilitate patient enrollment in these settings. The rapidly advancing heart failure research in heart failure with preserved ejection fraction is also an emerging area of interest for GEN-HF cardiologists interested in pursuing innovative research pathways. Ultimately, there is a need to produce clinical researchers and clinicians in the heart failure field who will dedicate time to these promising areas, which is often a challenge for some advanced heart failure physicians, considering the demanding clinical effort required for their patients.
Patient-reported Outcomes and Value-focused Health Care
Attention to patient quality of life is essential in heart failure management. As patients experience progressive symptoms, it is vital to recognize their life values in relation to health and disease management. A care model should incorporate patient-centered care and patient-reported outcomes in a manner that considers the individual patient’s preferences and goals and ensures that informed clinical decisions align with patient values. The GEN-HF cardiologists can attain these primary skills, including palliative care management. These cardiologists should initiate early advanced care planning discussions with patients and their families, because these discussions are best received in an ambulatory care setting with a familiar provider. A GEN-HF cardiologist must also have the skills to discuss non-OHT/VAD/mechanical circulatory support options with advanced patients with heart failure if they do not prefer or cannot pursue more advanced options.
The heart failure workforce requires expansion to manage the increased prevalence of symptomatic and advanced stage disease. More than ever before, heart failure management involves a complex process of monitoring through device implantation and clinical pathways. Expanding clinical careers in heart failure may ultimately provide a range of heart failure training pathways and diversify the cardiology workforce. We strongly feel this discussion requires more focus in the future as the heart failure field continues to evolve in management and approach. This article also supports current and future fellows in training who desire to incorporate a heart failure focus within their general cardiology careers.
Footnotes
Disclosures
Melvin R. Echols: Advisory Board/Consultant: Abbott
Institutional Research Grants from Association of Black Cardiologists, Georgia Clinical and Translational Science Alliance, Truist Foundation, Morehouse School of Medicine TX Program
Modele O. Ogunniyi: Institutional Research Grants from AstraZeneca, Boehringer Ingelheim, Zoll Advisory Board/ Consultant: Pfizer
References
- 1.Chuzi S, Reza N. Cultivating interest in heart failure careers: can we reverse the current trend? Cultivating interest in heart failure careers. J Card Fail 2021;27:819–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ordóñez-Piedra J, Ponce-Blandón JA, Robles-Romero JM, Gómez-Salgado J, Jiménez-Picón N, Romero-Martín M. Effectiveness of the advanced practice nursing interventions in patients with heart failure: a systematic review. Nurs Open 2021;8:1879–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKay C, Park C, Chang J, Brackbill M, Choi JY, Lee JH, et al. Systematic review and meta-analysis of pharmacist-led transitions of care services on the 30-day all-cause readmission rate of patients with congestive heart failure. Clin Drug Investig 2019;39:703–12. [DOI] [PubMed] [Google Scholar]
- 4.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bitten-court MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation 2021;143:e254–743. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. Organ procurement and transplantation network. 2021. Available at: https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/#. Accessed September 11, 2021.
- 6.Vasan RS, Musani SK, Matsushita K, Beard W, Obafemi OB, Butler KR, et al. Epidemiology of heart failure stages in middle-aged black people in the community: prevalence and prognosis in the Atherosclerosis Risk in Communities Study. J Am Heart Assoc 2021;10:e016524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng PP, Yao SM, Guo D, Cui LL, Miao GB, Dong W, et al. Prevalence and prognostic value of heart failure stages: an elderly inpatient based cohort study. Front Med (Lausanne) 2021;8:639453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalogeropoulos AP, Samman-Tahhan A, Hedley JS, McCue AA, Bjork JB, Markham DW, et al. Progression to stage D heart failure among outpatients with stage C heart failure and reduced ejection fraction. JACC Heart Fail 2017;5:528–37. [DOI] [PubMed] [Google Scholar]
- 9.Bozkurt B, Coats AJ, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail 2021. Mar 1 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 10.Jessup M, Ardehali R, Konstam MA, Manno BV, Mathier MA, McPherson JA, et al. COCATS 4 Task Force 12: training in heart failure. J Am Coll Cardiol 2015;65:1866–76. [DOI] [PubMed] [Google Scholar]
- 11.Adamson PB, Abraham WT, Love C, Reynolds D. The evolving challenge of chronic heart failure management: a call for a new curriculum for training heart failure specialists. J Am Coll Cardiol 2004;44:1354–7. [DOI] [PubMed] [Google Scholar]
- 12.Yancy CW, Drazner MH, Coffin ST, Cornwell W 3rd, Desai S, Erwin JP 3rd, et al. 2020 ACC/HFSA/ISHLT lifelong learning statement for advanced heart failure and transplant cardiology specialists: a report of the ACC Competency Management Committee. J Card Fail 2020;26:254–69. [DOI] [PubMed] [Google Scholar]
- 13.HFSA Heart Failure Certification (HF-Cert). 2021. Available at: https://hfsa.org/professional-development/hfsa-heart-failure-certification-hf-cert. Accessed September 26, 2021.
- 14.HFA Heart Failure Certification. Certification organised by the Heart Failure Association of the ESC (HFA). 2021. Available at: https://www.escardio.org/Education/Career-Development/Certification/Heart-Failure.
- 15.Norton C, Georgiopoulou VV, Kalogeropoulos AP, Butler J. Epidemiology and cost of advanced heart failure. Prog Cardiovasc Dis 2011;54:78–85. [DOI] [PubMed] [Google Scholar]


