Abstract
The anterior talofibular ligament (ATFL) is the most frequently injured lateral ligament of the ankle, and up to 20% of patients with ankle sprains may require surgical intervention to correct chronic lateral ankle instability. There has been increased interest in arthroscopic lateral ankle ligament repair techniques to minimize postoperative pain and expedite recovery. Additionally, the use of suture-tape augmentation may allow for improved recovery in those with ATFL reconstruction. The goal of this Technical Note is to describe the steps to performing in-office needle arthroscopy using suture tape as an internal brace for an ATFL deficient ankle. We also include an accompanying discussion on indications and opportunities afforded by an in-office procedure over the traditional operating room suite.
Technique Video
Operative technique demonstrating in-office nano arthroscopy for anterior talofibular ligament reconstruction with suture-tape augmentation.
Ankle sprains are one of the most common athletic injuries, with nearly 1 in 10,000 Americans experiencing an ankle sprain daily.1 The anterior talofibular ligament (ATFL) is the most frequently injured lateral ligament of the ankle, and up to 20% of patients who have sustained ankle sprains require surgical intervention to correct chronic lateral ankle instability.2 Recently, there has been increased interest in arthroscopic lateral ankle ligament repair to minimize postoperative pain and expedite recovery compared to traditional open approaches. In their 2020 meta-analysis Brown et al.3 found improved AOFAS scores in the patients treated arthroscopically. Several surgical techniques have been proposed for the management of chronic instability of the ankle in the setting of an ATFL tear, with the Brostrom procedure widely accepted as the gold standard. However, despite the excellent efficacy of this procedure, augmentation with suture-tape may provide additional benefits such as earlier postoperative mobilization, decreased risk of reinjury, and faster return to play.4, 5, 6, 7, 8 Additionally, several studies have also evaluated the use of suture-tape augmentation in ATFL repair and found improved functional outcome scores after surgery.4,9,10
In-office needle arthroscopy (IONA) first became available in the 1990s as a tool for visualization and evaluation of anatomic structures with patients under local anesthesia. The technique was never widely accepted in part because of a lack of defined indications, an inability to simultaneously treat identified pathologies, and poor picture resolution. Advancements in IONA have led to the development of a new disposable chip-on-tip camera with 400 × 400 resolution and 120° field of view fed through a 13″ high-definition monitor (Arthrex, Inc., Naples, FL). Even more importantly, this system comes with instrumentation including punches, graspers, scissors, a retractable probe, shavers, burrs, and resectors that allow for surgical intervention for any identified pathology. Work has now focused on describing scenarios where in-office needle arthroscopy can safely and effectively replace arthroscopy performed in a standard operating room suite as surgeons continuously refine their treatment algorithms to provide high quality patient care.
This surgical technique guide describes our method for performing an internal brace fixation of the ATFL with the Arthrex Nanoscope nano-arthroscopy system.11 We present our examination room layout, local anesthesia technique, arthroscopy video guide, and perceived advantages and disadvantages of using a needle arthroscopy system to assist other foot and ankle surgeons with deciding whether to adopt this technique into their clinical practices.
Surgical Technique
Preoperative Planning/Patient Positioning
The complete arthroscopic procedure is performed in the office examination room (Video 1). A mayo stand is sterilely draped for the assistant to organize the instruments during the procedure. The video monitor and additional equipment are placed on a separate tower within the vicinity of the examination table. The patient is asked to lay in the supine position on the examination table to provide access to the operative ankle. Soft padding is provided under the patient’s nonoperative extremity for comfort. Both the assistant and operative surgeon scrub for the procedure and don masks, gowns, and sterile gloves. A solution of chlorhexidine gluconate mixed with isopropyl alcohol is used to sterilely prep the patient’s ankle. Finally, the patient’s ankle is draped to provide a sterile work area on the examination table.
Portal Placement
The locations for standard anteromedial and anterolateral portals are identified and the skin and subcutaneous tissues are anesthetized using 1% lidocaine with epinephrine. The location for an accessory portal located 1 cm anterior to the tip of the fibula is similarly anesthetized. The accessory portal is made adjacent to the footprint of the ATFL on the Talus when the Talus is in Neutral dorsiflexion (Figs 1 and 2). After 5 to 10 minutes 5 mL of a solution of 0.5% bupivacaine with epinephrine and 1% lidocaine with epinephrine in a 1:1 ratio is injected into the ankle joint. Emphasis is placed on providing sufficient anesthetic to the lateral malleolar region. We have found that including epinephrine in the local anesthesia assists with hemostasis. The portals are created by first incising the skin only, then spreading the subcutaneous tissues to avoid injury to superficial nerves, and then inserting a blunt cannula for the nanoscope.
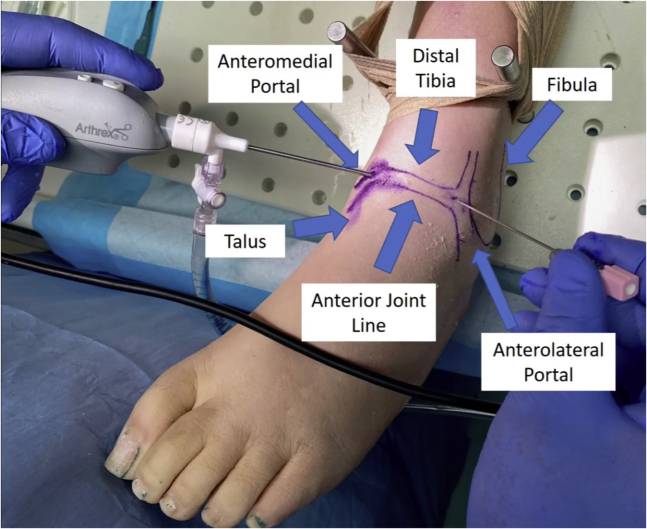
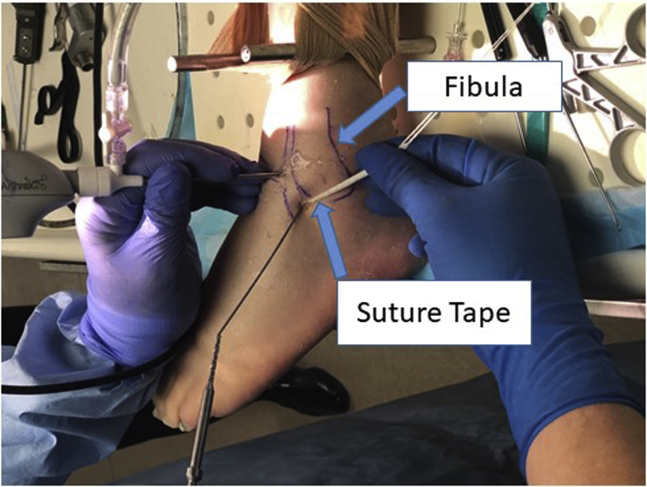
Fig 1.
The patient is in the supine position. Standard arthroscopic approach to the left ankle via the anterolateral and anteromedial portals. Relevant surface anatomy markings including the anterior joint line and portal locations are shown. The anteromedial portal, which is the primary viewing portal, is placed lateral to the medial malleolus and medial to the tibialis anterior tendon. One should be cautious to avoid the saphenous nerve and vein, as well as the tibialis anterior tendon. The anterolateral portal is made under direct visualization medial to the lateral malleolus. One should be cautious to avoid the superficial peroneal nerve, which is the most common neurovascular injury from ankle arthroscopy.
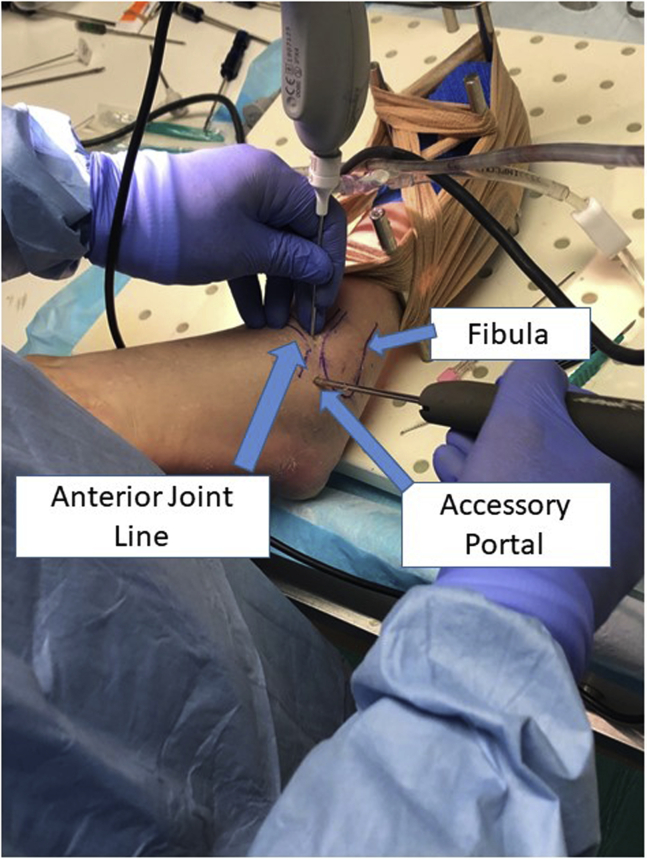
Fig 2.
The patient is in the supine position. Arthroscopic approach to the left ankle for a third, accessory, portal is made 1 cm anterior to the tip of the fibula to protect the sural nerve. This portal is adjacent to the footprint of the anterior talofibular ligament (ATFL) on the talus, when the talus is in neutral dorsiflexion.
Operative Technique
To facilitate visualization, begin by resecting part of the AITFL to identify the anatomic foot print of the ATFL on the fibula (Fig 3). Debridement of the area around the anatomic footprint is also recommended to enhance visibility of the area. Elevate the attachment of the ATFL off of the distal fibula. Mark an area 1 cm anterior to the tip of the fibula which will serve as the third portal site (Fig 2). This corresponds to the anatomic foot print of the Talar attachment of the ATFL. Through the accessory portal, a guide pin is placed at the talar footprint, and it is over drilled with a cannulated 3.5 mm drill to the laser line (Fig 3). Introduce the FiberTape suture anchor (Arthrex) and seat it into the talus (Fig 4). The anchor is tapped gently until the threads engage the subchondral bone (Fig 5). Through the anteromedial portal, we then turn our attention to the fibula. The periosteum is shaved to unveil a clean bed of subchondral bone and a guide wire is introduced. With a 3.5 mm cannulated drill, the guide pin is over drilled to the laser line (Fig 6). A knotless suture anchor is placed, with the suture tape, into the prepared fibular site (Fig 7). Check suture tension using a probe before final seating (Figs 8 and 9). At the end of the procedure, the patient is asked to actively range his or her ankle to ensure smooth tendon gliding and stability. Any remaining arthroscopy fluid is removed with suction, and the portals are closed with Steri-Strips (3M Corp, St. Paul, MN). Throughout the procedure, the patient is encouraged to watch the viewing monitor and ask questions to learn about their pathology. A sterile soft dressing is applied at the end of the procedure. Patients are allowed to bear weight as tolerated with early range of motion. Because there is no incision, patients can reduce the bandage on day 3 after surgery and are encouraged to use an Ace compressive bandage for an additional 1 week.
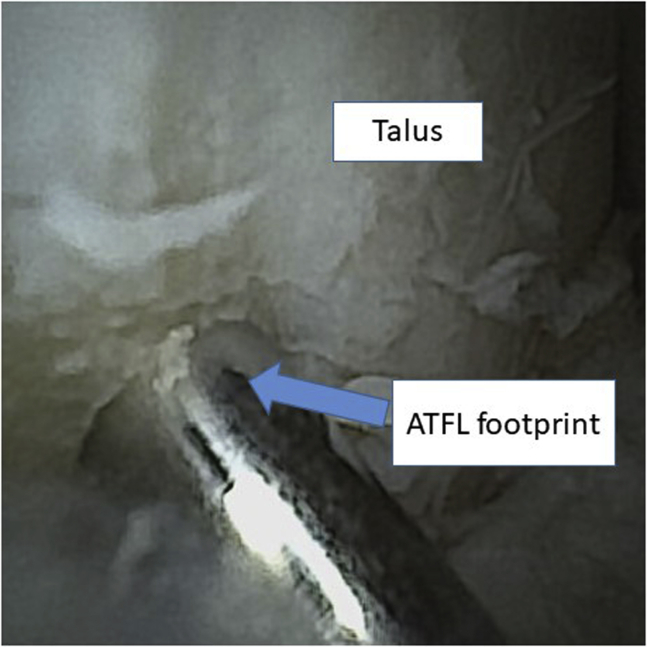
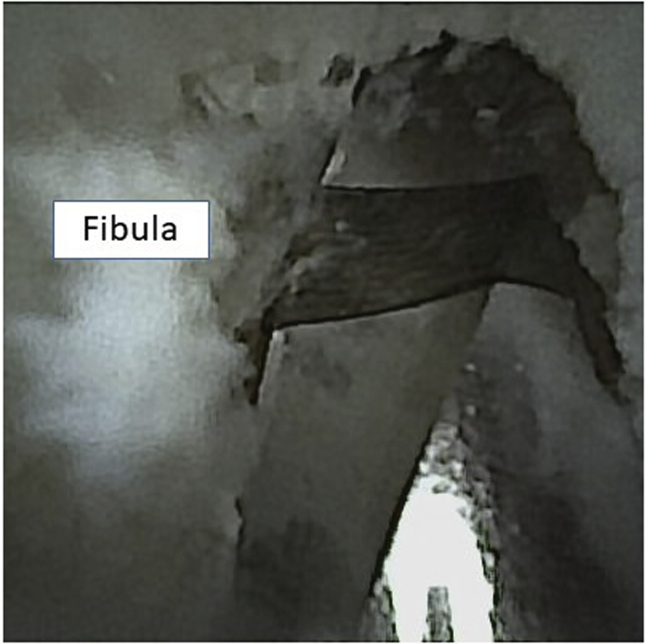
Fig 3.
This is an arthroscopic view of the left ankle through the anterolateral portal. Through the accessory portal, a 2.0 mm shaver is introduced. The working area is debrided using the 2.0 mm shaver to remove scar, soft tissue synovial hyperplasia, and remnant anterior talofibular ligament (ATFL) to optimize visualization. In some cases, there is an accessory ATFL that is also resected. The anatomic footprint of the ATFL on the talus is drilled through the accessory portal with a 3.5mm guide wire to the laser line.
Fig 4.
The patient is in the supine position. Through the accessory portal on the left ankle, introduce the suture tape anchor. Through the anterolateral portal, visualize the predrilled anterior talofibular ligament (ATFL) insertion site foot print. Gently guide the suture tape anchor into the talus at the predrilled ATFL insertion site foot print.
Fig 5.
The patient is in the supine position and this is the left ankle. The suture-tape anchor is already seated at the predrilled anterior talofibular ligament (ATFL) insertion site foot print. Tap the suture anchor into the talus until it engages subchondral bone, and tension sutures accordingly to secure the anchor.
Fig 6.
This is an arthroscopic view of the left ankle. Through the anteromedial portal we can properly visualize the anterior talofibular ligament (ATFL) insertion at the fibula. Through the anterolateral portal a 2.0 mm shaver is introduced. The working area is debrided, and the periosteum is shaved using a 2.0 mm shaver to unveil a clean bed of subchondral bone, and a guidewire is introduced using a 3.5 mm cannulated drill.
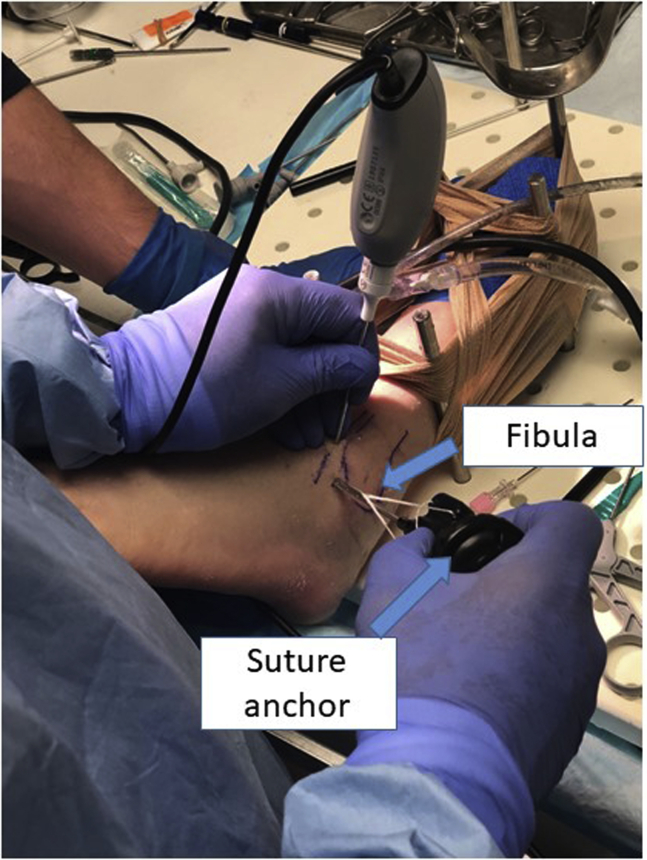
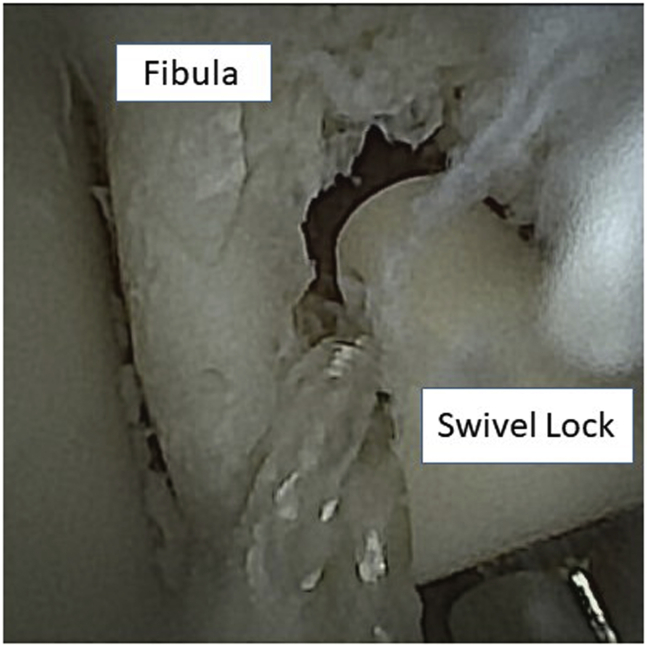
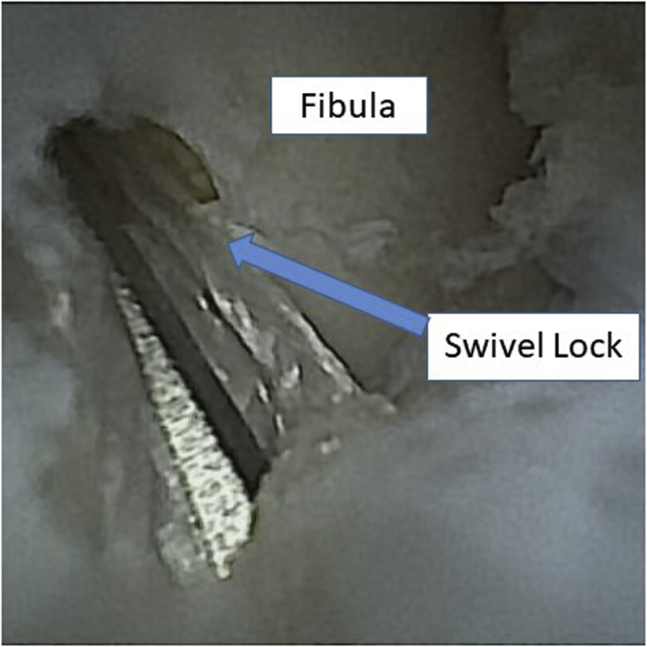
Fig 7.
This is an arthroscopic view of the left ankle joint through the anteromedial portal. The suture tape is introduced into the swivel lock. Through the anterolateral portal, the swivel lock is deployed at the predrilled site on the fibula.
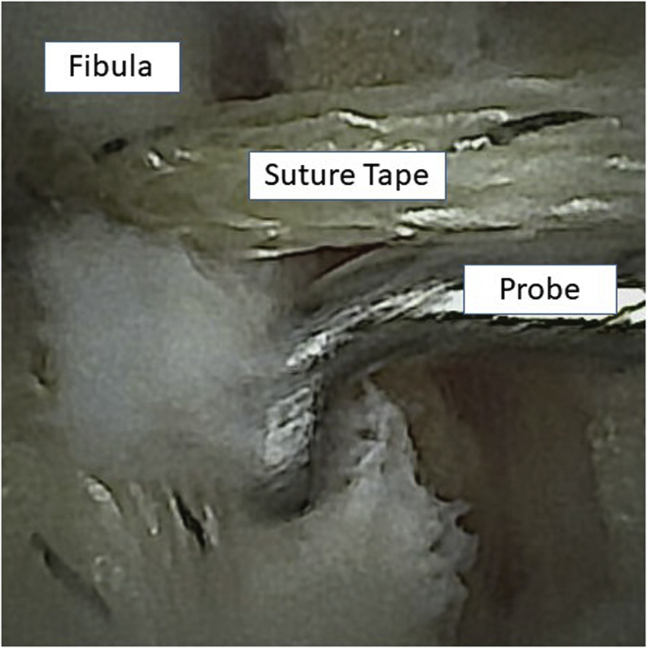
Fig 8.
This is an arthroscopic view of the left fibula through the anteromedial portal. The swivel lock is secured, and tension is tested with a probe. This is done before the swivel lock is secured into the fibula. It is critical to not over tension, because this will restrict motion.
Fig 9.
This is an arthroscopic view of the fibula through the anteromedial portal. Here we demonstrate the final swivel lock position after excess suture is excised.
Postoperative Protocol
Formal physical therapy consisting of strengthening, range of motion, balance, and proprioceptive exercises is begun immediately after arthroscopy involving only debridement. Ice and elevation are encouraged when patients are not ambulating. We have typically provided pain medication for up to 4 days after the procedure. Patients are expected to return on day 5 after their arthroscopy for the first follow-up appointment (Table 1, Table 2, Table 3).
Table 1.
Advantages and Disadvantages of Proposed Technique
| Advantages |
| Minimally invasive procedure with smaller instruments than standard arthroscopy |
| Allows for rapid post-operative recovery due to its minimally invasive approach |
| Decreased cost and resource utilization without the need for a full operating room suite |
| Patient is wide awake and allowed to learn about their condition in real-time |
| Improved ability to diagnose anatomic variants compared to magnetic resonance imaging |
| Less-invasive procedure provides opportunity for quicker recovery, minimal scarring, and limited wound complications |
| Disadvantages |
| Dependent on local anesthesia for pain control during procedure |
| Learning curve with wide-awake patient present |
| Only a 0° camera is currently available with the needle arthroscopy system |
Table 2.
Pearls and Pitfalls of the Proposed Technique
| Pearls |
| Ensure proper support for the patient’s head and non-operative extremity to limit movement during the procedure |
| Inject lidocaine at both portal sites |
| Use a mixture of lidocaine with epinephrine and bupivacaine to limit bleeding |
| Help to prevent overtightening by having the patient plantarflex the ankle to about 30°. |
| Insert an instrument under the suture tape construct to ensure there is physiological laxity |
| Pitfalls |
| Incorrect placement of inferior and superior portal may cause Sural nerve injury |
| Overtightening of the suture tape which may lead to altering the normal integrity of the ligament complex, as well as restricting the motion of the subtalar joint |
| Debridement before a full diagnostic evaluation may lead to iatrogenic injury |
Table 3.
Step-by-Step Guide to Performing In-Office ATFL Repair With Suture Tape Augmentation
| Step 1: Position the patient supine on an examination table to make the operative ankle easily accessible. |
| Step 2: Use a chlorhexidine gluconate/isopropyl alcohol sponge-stick to sterilely prepare the ankle and drape the ankle to create a sterile field along the distal half of the examination table. |
| Step 3: Inject local anesthesia superficially into the anticipated portals. |
| Step 4: Establish portals with a superficial stab incision followed by blunt dissection Insert the scope into the anteromedial portal initially. Insert shaver into anterolateral portal. |
| Step 5: Resect part of the AITFL to identify the anatomic foot print of the ATFL on the fibula. |
| Step 6: Elevate the attachment of the ATFL ligament off of the distal fibula and shave down to bone. |
| Step 7: Make third portal 1 cm anterior to the tip of the fibula. |
| Step 8: Insert wire into the fibula and laser line into talus. Introduce FiberTape suture and overdrill with cannulated 3.5 drill to secure into talus. |
| Step 9: Overdrill fibula with 3.5 drill through anterolateral portal. |
| Step 10: Pass suture from third portal to the anterolateral portal. |
| Step 11: Advance swivel lock anchor while maintaining tensions in suture. |
| Step 12: Check suture tension using a probe before final seating. |
| Step 13: Ask the patient to actively range their ankle to assess ligament tension. |
| Step 14: Perform wound closure with Steri-Strips and apply soft dressing or splint as indicated. |
ATFL, anterior talofibular ligament.
Discussion
Advancements in needle arthroscopy have allowed for foot and ankle surgeons to treat patients in the office under local anesthesia via a minimally invasive approach. We prepared this article to describe a technique for performing wide-awake needle arthroscopy for the management of lateral ankle instability in the setting of an ATFL tear. We believe that a less-invasive in-office procedure that can further decrease postoperative recovery time will be of increased interest to today’s athletic population.
Various studies have indicated a mechanical superiority of an augmented ATFL reconstruction using suture-tape that facilitates a faster return to play compared to traditional repair.8,12 Yoo and Yang9 compared return to sport in patients treated with and without suture-tape augmentation and found that 18 patients (81.8%) in the suture-tape group returned to sports activity without limitations whereas only 17 patients (27%) in the Brostrom group were able to do so at 12 weeks after surgery. Additionally, Coetzee et al.13 reported that motivated athletes were able to return to play at an accelerated rate, highlighting the ability of suture tape augmentation to contribute to a faster return to sports at a mean of 84 days or 2.77 months. Functional outcome measures have also been favorable for patients treated with suture-tape augmentation. Martin et al.4 reported on 93 patients treated with Brostrom procedure augmented with a suture-tape construct. In this cohort the visual analogue scale score decreased from 4.8 to 1.3 at 12-week follow-up, and the Foot and Ankle Disability Index increased from 67 to 90 at 12-week follow-up.
Patients have shown an increased interest in undergoing procedures that minimize time spent in the operating room. Recently patients have also demonstrated positive feedback thus far in response to treatment with in-office needle arthroscopy with a high rate of willingness to undergo a similar treatment.14,15 The current article describes a procedure that has the potential to facilitate early mobilization after ATFL surgery This will be beneficial to all patients but particularly athletes with an accelerated return to play. Advancements in needle arthroscopy have the potential to redefine minimally invasive procedures and may influence future practice paradigms for specific pathologies.
Footnotes
The authors report the following potential conflict of interest or source of funding: J.G.K. reports grants from Isto Biologics; board or committee membership for the American Orthopaedic Foot and Ankle Society, Arthroscopy Association of North America, European Society for Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA), Ankle and Foot Associates (AFAS), and International Society for Cartilage Repair of the Ankle; receives support from Ohnell Family Foundation and Mr. and Mrs. Michael J. Levitt, and is a consultant for Isto Biologics and Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Operative technique demonstrating in-office nano arthroscopy for anterior talofibular ligament reconstruction with suture-tape augmentation.
References
- 1.Hayman J., Prasad S., Stulberg D. Help patients prevent repeat ankle injury. J Fam Pract. 2010;59:32–34. [PMC free article] [PubMed] [Google Scholar]
- 2.de Vries J.S., Krips R., Sierevelt I.N., Blankevoort L., van Dijk C.N. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011;8:CD004124. doi: 10.1002/14651858.CD004124.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Brown A.J., Shimozono Y., Hurley E.T., Kennedy J.G. Arthroscopic versus open repair of lateral ankle ligament for chronic lateral ankle instability: A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2020;28:1611–1618. doi: 10.1007/s00167-018-5100-6. [DOI] [PubMed] [Google Scholar]
- 4.Martin K.D., Andres N.N., Robinson W.H. Suture tape augmented Broström procedure and early accelerated rehabilitation. Foot Ankle Int. 2021;42:145–150. doi: 10.1177/1071100720959015. [DOI] [PubMed] [Google Scholar]
- 5.Ulku T.K., Kocaoglu B., Tok O., Irgit K., Nalbantoglu U. Arthroscopic suture-tape internal bracing is safe as arthroscopic modified Broström repair in the treatment of chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020;28:227–232. doi: 10.1007/s00167-019-05552-w. [DOI] [PubMed] [Google Scholar]
- 6.Xu D.L., Gan K.F., Li H.J., et al. Modified Broström repair with and without augmentation using suture tape for chronic lateral ankle instability. Orthop Surg. 2019;11:671–678. doi: 10.1111/os.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho B.K., Park J.K., Choi S.M., SooHoo N.F. A randomized comparison between lateral ligaments augmentation using suture-tape and modified Broström repair in young female patients with chronic ankle instability. Foot Ankle Surg. 2019;25:137–142. doi: 10.1016/j.fas.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 8.Lee K., Jegal H., Chung H., Park Y. Return to play after modified Broström operation for chronic ankle instability in elite athletes. Clin Orthop Surg. 2019;11:126–130. doi: 10.4055/cios.2019.11.1.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoo J.S., Yang E.A. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17:353–360. doi: 10.1007/s10195-016-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schuh R., Benca E., Willegger M., et al. Comparison of Broström technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2016;24:1101–1107. doi: 10.1007/s00167-015-3631-7. [DOI] [PubMed] [Google Scholar]
- 11.Hand Held Arthroscopic Instruments. https://www.arthrex.com/knee/hand-held-arthroscopic-instruments Available at:
- 12.Theodore B.R., Mayer T.G., Gatchel R.J. Cost-effectiveness of early versus delayed functional restoration for chronic disabling occupational musculoskeletal disorders. J Occup Rehabil. 2015;25:303–315. doi: 10.1007/s10926-014-9539-0. [DOI] [PubMed] [Google Scholar]
- 13.Coetzee J.C., Ellington J.K., Ronan J.A., Stone R.M. Functional results of open Brostrom ankle ligament repair augmented with a suture tape. Foot Ankle Int. 2018;39:304–310. doi: 10.1177/1071100717742363. [DOI] [PubMed] [Google Scholar]
- 14.Gunasagaran J., Sean E.S., Shivdas Amir S., Ahmad T.S. Perceive comfort during minor hand surgeries with wide awake local anesthesia no tourniquet (WALANT) versus local anesthesia (LA)/tourniquet. J Orthop Surg. 2017;25(3):1–4. doi: 10.1177/2309499017739499. [DOI] [PubMed] [Google Scholar]
- 15.Rhee P.C., Fischer M.M., Rhee L.A., et al. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: A critical analysis of the first 100 procedures. J Hand Surg. 2017;42:139–147. doi: 10.1016/j.jhsa.2016.11.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Operative technique demonstrating in-office nano arthroscopy for anterior talofibular ligament reconstruction with suture-tape augmentation.
Operative technique demonstrating in-office nano arthroscopy for anterior talofibular ligament reconstruction with suture-tape augmentation.