Abstract
Background:
Raised blood pressure (BP) is the leading global risk factor for cardiovascular diseases and a major cause of premature death. Worldwide, one in four men and one in five women are hypertensive. For effective preventive strategy, understanding of predictors of hypertension is necessary.
Objective:
To assess prevalence and predictors of hypertension in the rural adult Indian population.
Material and Methods:
This cross-sectional study was carried out on 425 rural subjects (25–64 years) of the Varanasi district in India selected through multistage sampling. Blood pressure of each subject was measured using a standard technique. Sociodemographic data and predictors of hypertension were assessed by interviewing subjects with help of a predesigned and pretested proforma.
Results:
Prevalence of hypertension was 31.5% (95% CI: 27.1–35.9). There existed a significant (P < 0.05) association of BP with age, educational status, occupation, socioeconomic class, tobacco consumption, waist circumference, waist-hip ratio, and nutritional status. No significant association was found with gender, religion, caste, marital status, type and size of family, family without NCDs, awareness of screening camps for NCDs and national program for prevention and control of cancer, diabetes, cardiovascular diseases and stroke, and alcohol consumption. Significant association of education, nutritional, and occupational status obtained in univariate analysis got eliminated in the logistic model. Risk of hypertension was higher in the 45–64 years age group (AOR: 3.06; 95% CI: 1.75–5.35) and in socioeconomic class IV and V (AOR: 2.24; 95% CI: 1.17–4.31).
Conclusion:
Prevalence of hypertension in the rural population was high and most of the observed predictors were modifiable.
Keywords: BMI, cardiovascular diseases and stroke, diabetes, hypertension, national program for prevention and control of cancer, noncommunicable diseases, waist circumference, waist-hip ratio
Introduction
Globally, more than 41 million people die annually from noncommunicable diseases (NCDs) (71% of total global deaths), including among 15 million individuals who dies between ages 30-70 years, many have premature death.[1] In India, risk of premature death due to NCDs is 23%, and is slightly more in males (27%) compared to females (20%).[2] Elevated blood pressure (BP) or hypertension is the leading global modifiable risk factor for cardiovascular diseases and is a major cause of premature death. It has modifiable risk factors such as tobacco use, unhealthy diet, physical inactivity, and high alcohol consumption; moreover, an unbreakable bond also prevails between obesity (general as well as central) and hypertension. Nonmodifiable risk factors are family history of hypertension, age above 65 years, and coexisting comorbid conditions.[3] In 2015, one in four men and one in five women had hypertension.[4] According to the WHO NCD country profile (2018), the prevalence of raised blood pressure among Indian adults aged 18+ was 24%. It was almost the same in both the sexes, with 24% men and 23% women having hypertension.[5]
There is a continuous relationship between the level of blood pressure and the risk of complications. With each increment of 20/10 mm Hg in the blood pressure range, CVD risk doubles with starting blood pressure of 115/75 mm Hg.[6] In 2019, ischemic heart disease and stroke (sequelae of hypertension) were the top-ranked causes of DALYs in 50 years and older age groups. Of all death globally, 19.2% was attributed to high systolic blood pressure.[4] Currently, the world is facing a syndemic of coronavirus infection along with NCDs, and one of the worldwide focuses for NCDs is the target to decrease the prevalence of hypertension by 25% by 2025 (baseline: 2010).[7,8]
Hypertension is easily diagnosable and controllable with effective medicines. Unfavorable health outcomes associated with hypertension could be lessened through strategies that include early identification, treatment, and control by providing timely access to primary healthcare providers to expedite the process to alleviate the expense of medications for those in treatment through insurance coverage, cost-sharing, and benefit designs, and finally to support hypertension control by expanding worksite wellbeing and quality control measures.[9]
Low healthcare literacy, poor patient self-care, high self-medication rate, inconsistent hypertension management guidelines, and nonadherence to treatment plans and medical regimens leads to poor blood pressure control and high healthcare costs, thus intensifying the problem in India.[10] In fact, the role of primary healthcare physicians is pivotal in the prevention and management of hypertension. Furthermore, this is a cost-effective and scalable approach in tackling the problem of hypertension.
To curb the rising trend of hypertension and to establish new policy implications, one must be first aware of the prevalence and predictors of hypertension. With this background, the present study was undertaken on a representative adult population of rural Varanasi in India, with the objectives to assess prevalence, associates, and predictors of hypertension.
Material and Methods
Study design and study setting
This community-based snapshot study was undertaken in one (viz. Chiraigaon) of the eight community development blocks of Varanasi district, India. The region lies in the eastern part of the Uttar Pradesh territory of North India. As per census 2011, the population of Varanasi district and Chiraigaon Community Development block were 3,676,841 and 2,62,324, respectively. Sex ratio for the district and block was 913 and 899, respectively. Overall literacy rate was 67.1%, whereas for males and females, this was 76.1% and 57.1%, respectively.[11,12]
Participants of the study
This study was conducted on an adequate and representative sample of the rural adult population belonging to the age group 25–64 years. Prevalence of hypertension was taken to be 21% in the rural adult population.[13] Considering the permissible level of error of 5% (absolute), the required sample size worked out to be 254.9, which after adjusting for design effect of 1.5 became 382.4. Furthermore, giving due allowance to nonresponse of 10% the final sample size was fixed at 425.
The following stages were adopted for the selection of study subjects: In the first stage, the Chiraigaon community development block was selected by simple random sampling from eight community development blocks of the Varanasi district. Villages were selected in the next stage by stratified sampling; stratification was done based on distance from block headquarter and from the first stratum of villages within 5 km; one village, that is, Narayanpur was selected by simple random sampling. Applying the identical approach, one village, that is, Umraha was selected from the second stratum (5–10 km), and the last village, Chittauna, was selected from the third stratum (>10 km). Required numbers of families from each village were computed adopting probability proportion to size (PPS) and the estimated families from a particular village were selected by systemic random sampling. One adult (25–64 years) from the selected family was picked up by lottery method.
Inclusion and exclusion criteria
Adults of the age group of 25–64 years consenting for the study were considered as subjects of the study. Pregnant women, subjects with serious mental abnormality or terminal illness, and individuals having duration of stay in the study area less than 6 months were excluded from the study.
Tools and techniques
Sociodemographic information: Information pertaining to age, sex, religion, caste, literacy, marital status, occupation, total family income, family size, socioeconomic status, and family history of diseases and comorbid conditions were obtained by interviewing individuals using predesigned and pretested proforma.[14]
Assessment of prevalence of hypertension in study subjects and its predictors: Hypertension was defined according to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (Seventh report). A fully automatic, digital blood pressure measuring device (Dr. Morepen BP One; model no: BP-16) was used twice over the right arm of the selected subjects with the interval of 5 minutes to get the average of the two blood pressure readings.[15] Information regarding predictors of hypertension in an individual was obtained by anthropometric measurements. All the anthropometric measurements were done by following a standardized technique. Anthropometric measurements such as weight (accuracy of 0.1 kg) were measured by a Libra weighing machine, height (accuracy of 0.1 cm) was assessed by steel anthropometry rod with parallel bars, waist circumferences (in cm) was taken at the end of expiration by a nonstretchable measuring tape in the smallest point between the costal margins and the iliac crest and lastly hip circumferences (in cm) were measured by wrapping nonstretchable measuring tape over the hips at the widest part.[16] Based on the body mass index (BMI) obtained, Asian classification was used for classifying subjects into different categories.[17] Waist-to-hip circumference (WHR) was determined by taking the ratio of waist circumference to hip circumference.[18] Particulars regarding tobacco use as well as alcohol consumption were also noted by the interview schedule developed by modifying and pretesting the WHO chronic disease risk factor surveillance STEPS tool.[19]
Ethical approval
Ethical approval was obtained from Institutional Ethical Committee. Hindi consent form was used for obtaining consent from the individual participants.
Statistical analysis
Data thus generated were analyzed using IBM-SPSS version 23.0. Confidence Intervals (95%) were computed for inferential purpose. Associates and predictors (adjusted odds ratios) of hypertension among individuals were obtained through univariate and logistic regression analysis.
Results
Out of 425 subjects, 52.9% and 47.1% subjects were male and female, respectively. Overall sex ratio in the study group was 1000:889. As many as 39.3%, 29.2%, 21.6%, and 9.9% of subjects were from the age group of 25–34, 35–44, 45–54, and 55–64 years, respectively. As many as 84.9% and 15.1% of subjects were from the Hindu and Muslim religions, respectively. In all 24.7%, 52.7%, and 22.6% subjects were from SC/ST, OBC, and other caste categories, respectively. Overall, 82.6% of subjects were married. Twenty-six (6.1%) subjects were without spouses whereas 11 (2.6%) subjects were either separated or deserted. In the case of 201 (47.3%) subjects, highest education in the family was intermediate and above. As many as 52.2%, 41.2%, and 6.6% of subjects were from nuclear, joint, and three-generation families, respectively. There were 6 (1.41%) subjects where higher education in the family was as illiterate, just literate, and literate. In the case of 68.8% of subjects, family size was 4–6, whereas 26.6% of subjects had a family size of >6.
As many as 8.9%, 14.8%, and 2.6% of subjects were illiterate, just-illiterate, and literate, respectively; whereas subjects with educational status as primary, middle, and high school were 21.3%, 19.5%, and 16.5%, respectively. In the case of 11.8% and 4.7% of subjects, educational status was intermediate and graduate and above, respectively. Out of all illiterates, 34.2% and 65.8% were male and female. Out of all males, 5.8% were illiterate. Out of all females, 12.5% were illiterate. In the case of 25.3% and 6.5% female subjects had educational level was intermediate and above. Subjects engaged in agriculture, labor, and business were 17.2%, 25.2%, and 10.6%, respectively. Out of 200 female subjects, 148 (74.0%) were homemakers. In all, 2.1% of subjects were students and 4.9% were unemployed. As many as 4.5%, 16.9%, 64.0% of subjects were from social class II, social class III, and social IV, respectively. Sixty-two (14.6%) subjects were in class V as per Modified B.G. Prasad classification, 2019 [Table 1].
Table 1.
Socioeconomic profile of study subjects (n=425)
| Particulars | Frequency (n) | Percentage | |
|---|---|---|---|
| Educational status | Illiterate | 38 | 8.9 |
| Just literate | 63 | 14.8 | |
| Literate | 11 | 2.6 | |
| Primary | 90 | 21.2 | |
| Middle | 83 | 19.5 | |
| High school | 70 | 16.5 | |
| Intermediate | 50 | 11.8 | |
| Graduate | 19 | 4.5 | |
| Postgraduate and above | 1 | 0.2 | |
| Occupation | Agriculturist | 73 | 17.2 |
| Laborer | 107 | 25.2 | |
| Business | 45 | 10.6 | |
| Service | 22 | 5.2 | |
| Homemaker | 148 | 34.8 | |
| Student | 9 | 2.1 | |
| Unemployed | 21 | 4.9 | |
| Classification according to modified B.G. Prasad for year 2019 | Social class I | - | - |
| Social class II | 19 | 4.5 | |
| Social class III | 72 | 16.9 | |
| Social class IV | 272 | 64.0 | |
| Social class V | 62 | 14.6 | |
Family history of hypertension and diabetes was present in 26.4% and 23.8% of subjects, respectively. Family history of chronic respiratory diseases (CRDs), cancer, and heart attack were present in 3.8%, 4.0%, and 2.8% of subjects, respectively. Self-reported hypertension was present in 12.0% of subjects [Figure 1].
Figure 1.
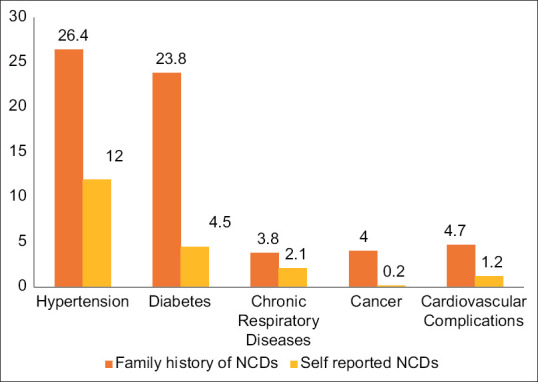
Distribution of family history of NCDs and self-reported NCDs
In the case of 27.1% male and 25.0% female subjects, diastolic blood pressure was >90 mm Hg; overall, this value was 26.1% (95% CI: 21.9–30.5). In all, 20.9% (95% CI: 17.1–24.8) of subjects had systolic blood pressure ≥140 mm Hg [Table 2]. As much as 31.5% (95% CI: 27.1–35.9) were categorized as hypertensive when criteria of diastolic blood pressure >90 mm Hg and/or systolic blood pressure ≥140 mm Hg was applied.
Table 2.
Distribution of study subjects according to their Blood pressure
| Particulars | Male (n=225) | Female (n=200) | Total (n=425) | 95% CI | Test of Significance χ2, df, P |
|||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| No. | % | No. | % | No. | % | |||
| Diastolic Blood pressure | ||||||||
| <90 mm of Hg | 164 | 72.9 | 150 | 75.0 | 314 | 73.9 | 69.7-78.1 | 0.25, 1, 0.62 |
| ≥90 mm of Hg | 61 | 27.1 | 50 | 25.0 | 111 | 26.1 | 21.9-30.5 | |
| Systolic Blood pressure | ||||||||
| <140 mm of Hg | 176 | 78.2 | 160 | 80.0 | 336 | 79.1 | 75.2-82.9 | 0.2, 1, 0.65 |
| ≥140 mm of Hg | 49 | 21.8 | 40 | 20.0 | 89 | 20.9 | 17.1-24.8 | |
Associates of raised blood pressure of study subjects with their socioeconomic variables are given in Table 3. As much as 20.6% and 55.2% of subjects from the age group 25–44 and 45–64 years had raised BP (P < 0.01). There existed a significant (P < 0.01) association between blood pressure of study subjects with their educational status. All the subjects were clubbed in three educational categories and individual category wise blood pressure were determined. There existed a significant (p < 0.01) association between blood pressure of study subjects with their educational categories. Category wise prevalence of hypertension were illiterate + just literate + literate – 46.4 %, primary + middle + high – 29.2 % and intermediate and above – 15.7 %. There also existed a significant (P < 0.05) association of BP status of subjects with their occupation and socioeconomic class. Hypertension was maximum in subjects involved in labor (37.4%) and from socioeconomic class IV and V (34.4%). There existed no significant (P > 0.0) association of the subject’s blood pressure status with their gender, religion, caste, residing village, and marital status.
Table 3.
Associates of raised blood pressure of study subjects with their socio-economic variables
| Particulars | Total (n) | Blood pressure within range | Raised Blood pressure | Test of Significance | |||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| No. | % | No. | % | χ 2 | df | P | |||
| Age in years | 25-44 years | 291 | 231 | 79.4 | 60 | 20.6 | 50.89 | 1 | 0.00 |
| 45-64 years | 134 | 60 | 44.8 | 74 | 55.2 | ||||
| Residing Village | Narayanpur | 169 | 117 | 69.2 | 52 | 30.8 | 0.13 | 2 | 0.94 |
| Umrahan | 144 | 97 | 67.4 | 47 | 32.6 | ||||
| Chittauna | 112 | 77 | 68.8 | 35 | 31.3 | ||||
| Marital status | With Spouse | 351 | 243 | 69.2 | 108 | 30.8 | 0.54 | 1 | 0.46 |
| Without Spouse | 74 | 48 | 64.9 | 26 | 35.1 | ||||
| Educational status | Illiterate + Just literate + Literate | 112 | 60 | 53.6 | 52 | 46.4 | 20.23 | 2 | 0.00 |
| Primary + Middle + High | 243 | 172 | 70.8 | 71 | 29.2 | ||||
| Intermediate and above | 70 | 59 | 84.3 | 11 | 15.7 | ||||
| Occupational status | Agriculture | 73 | 46 | 63.0 | 27 | 37.0 | 9.79 | 3 | 0.02 |
| Labor | 107 | 67 | 62.6 | 40 | 37.4 | ||||
| Business + Service | 67 | 56 | 83.6 | 11 | 16.4 | ||||
| Not engaged in gainful employment | 178 | 122 | 68.5 | 56 | 31.5 | ||||
| Socioeconomic Class | II + III | 91 | 72 | 79.1 | 19 | 20.9 | 6.08 | 1 | 0.01 |
| IV + V | 334 | 219 | 65.6 | 115 | 34.4 | ||||
Association of raised blood pressure of study subjects with their familial, programmatic, and risk factor attributes is shown below in Table 4. As many as 44.9% of subjects consuming tobacco and 23.8% of subjects without tobacco consumption were hypertensive (P < 0.01). As many as 60.0% of subjects with higher waist circumference, 50.4% with high WHR, and 58.3% of subjects characterized as overweight + pre-obese + obese based on Asian classification using BMI as a parameter were hypertensive; corresponding values in their counterpart were significantly less. There was no significant association of the subject’s blood pressure status with their type and size of family, family without NCDs, awareness of screening camps and NPCDCS program, and status of alcohol consumption.
Table 4.
Association of raised blood pressure of study subjects with their familial, programmatic, and risk factor attributes
| Particulars | Total (n) | Blood pressure within range | Raised Blood pressure | Test of Significance | |||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| No. | % | No. | % | χ 2 | df | P | |||
| Type of family | Nuclear | 222 | 157 | 70.7 | 65 | 29.3 | 1.09 | 1 | 0.30 |
| Joint/3-Gen | 203 | 134 | 66.0 | 69 | 34.0 | ||||
| Family size | ≤3 | 28 | 22 | 78.6 | 6 | 21.4 | 2.61 | 2 | 0.27 |
| 4-6 | 284 | 197 | 69.4 | 87 | 30.6 | ||||
| >6 | 113 | 72 | 63.7 | 41 | 36.3 | ||||
| 4 + 5 | 334 | 219 | 65.6 | 115 | 34.4 | ||||
| Family history of NCDs | Absent | 200 | 135 | 67.5 | 65 | 32.5 | 0.17 | 1 | 0.69 |
| Present | 225 | 156 | 69.3 | 69 | 30.7 | ||||
| Awareness regarding NPCDCS Program | No | 385 | 265 | 68.8 | 120 | 31.2 | 0.25 | 1 | 0.62 |
| Yes | 40 | 26 | 65.0 | 14 | 35.0 | ||||
| Awareness of Health promotional/Screening Camps | No | 346 | 237 | 68.5 | 109 | 31.5 | 0.00 | 1 | 0.98 |
| Yes | 79 | 54 | 68.4 | 25 | 31.6 | ||||
| Tobacco consumption | No | 269 | 205 | 76.2 | 64 | 23.8 | 20.32 | 1 | 0.00 |
| Yes | 156 | 86 | 55.1 | 70 | 44.9 | ||||
| Alcohol consumption | No | 332 | 233 | 70.2 | 99 | 29.8 | 2.06 | 1 | 0.15 |
| Yes | 93 | 58 | 62.4 | 35 | 37.6 | ||||
| Waist circumference | Normal | 320 | 249 | 77.8 | 71 | 22.2 | 52.36 | 1 | 0.00 |
| Higher than normal range | 105 | 42 | 40.0 | 63 | 60.0 | ||||
| Waist Hip ratio | Normal | 302 | 230 | 76.2 | 72 | 23.8 | 28.57 | 1 | 0.00 |
| Higher than normal range | 123 | 61 | 49.6 | 62 | 50.4 | ||||
| BMI (Asian criteria) | Underweight | 40 | 33 | 82.5 | 7 | 17.5 | 48.70 | 2 | 0.00 |
| Normal | 277 | 213 | 76.9 | 64 | 23.1 | ||||
| Overweight + Pre-obese + Obese | 108 | 45 | 41.7 | 63 | 58.3 | ||||
Significant association of education, nutritional status according to Asian BMI, and occupational status of subjects with raised BP obtained in univariate analysis got eliminated in the logistic model. Taking age 25–44 years as reference, risk of hypertension was higher in the age group 45–64 years (AOR: 3.06; 95% CI: 1.75–5.35). In comparison to socioeconomic class II + III, risk of hypertension was more in socioeconomic class IV + V (AOR: 2.24; 95% CI: 1.17–4.31). AORs in subjects consuming tobacco, with high waist circumference, and high WHR were 1.73 (95% CI: 1.02–2.93), 2.93 (95% CI: 1.17–4.60), and 1.98 (95% CI: 1.08–3.62), respectively [Table 5].
Table 5.
Logistic regression analysis for raised blood pressure of study subjects
| Particulars | Estimation of β | SE of β | P | AOR | 95% CI |
||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Age | 45-64 | 1.12 | 0.258 | 0.000 | 3.06 | 1.75 | 5.35 |
| 25-44* | - | - | - | - | - | - | |
| Education | Illiterate + Just Literate + Literate | 0.54 | 0.45 | 0.22 | 1.73 | 0.71 | 4.19 |
| Primary + Middle + High school | 0.59 | 0.41 | 0.14 | 1.80 | 0.81 | 4.00 | |
| Intermediate and above * | - | - | - | - | - | - | |
| Occupation | Labor | 0.81 | 0.44 | 0.06 | 2.24 | 0.95 | 5.33 |
| Agriculture | 0.81 | 0.46 | 0.08 | 2.25 | 0.92 | 5.52 | |
| Not engaged in gainful employment | 0.91 | 0.44 | 0.84 | 1.09 | 0.46 | 2.58 | |
| Business + Service* | - | - | - | - | - | - | |
| Socioeconomic Class | Social class IV + V | 0.778 | 0.313 | 0.013 | 2.177 | 1.179 | 4.017 |
| Social class II + III* | - | - | - | - | - | - | |
| BMI (Asian Criteria) | Overweight + Pre-obese + Obese | 0.76 | 0.53 | 0.15 | 2.13 | 0.76 | 5.99 |
| Normal | 0.11 | 0.47 | 0.82 | 1.11 | 0.45 | 2.78 | |
| Underweight | - | - | - | - | - | - | |
| Tobacco consumption | Consumed | 0.55 | 0.27 | 0.04 | 1.73 | 1.02 | 2.93 |
| Not consumed* | - | - | - | - | - | - | |
| Central obesity as per Waist circumference | Present | 0.84 | 0.35 | 0.02 | 2.32 | 1.17 | 4.60 |
| Normal* | - | - | - | - | - | - | |
| Central obesity as per Waist Hip ratio | Present | 0.68 | 0.31 | 0.03 | 1.98 | 1.08 | 3.62 |
| Normal* | - | - | - | - | - | - | |
*Reference. NOTE: The appropriateness of fitted model was 76.2%
Discussion
In India, mortality from NCDs accounted for 65% of total deaths in 2019, and hypertension among all NCDs is a major contributor to death in general and premature mortality in particular.[20]
According to this study, nearly one out of three subjects were hypertensive. In a cross-sectional study conducted by Chow et al.[21] (2007) in rural Andhra Pradesh, the overall prevalence was lower (one out of five) than in the present study. Krishnan et al.[22] (2008) in rural Haryana also showed a lower prevalence in male and female subjects. Todkar et al.[23] (2009) in a cross-sectional study in Aurangabad, Maharashtra also predicted an overall prevalence much lower than the current study. Stratified multistage sampling design of Stage I of the Indian Council of Medical Research-India Diabetes (ICMR-INDIAB) study conducted over three states (Tamil Nadu, Maharashtra, and Jharkhand) and one union territory (Chandigarh) depicted also an overall prevalence of 26.3% in subjects of age group above 20 years.[24] Oommen et al.[25] (2016) concluded the prevalence of hypertension as 17.2% in a cross-sectional study in rural Tamil Nadu. According to a national-level survey by Ramakrishnan et al.[26] (2019) for blood pressure conducted on fixed one-day camps under the aegis of the Cardiological Society of India showed the prevalence of hypertension as 30.7%. Findings of overall blood pressure higher than the present study were shown by Thankappan et al.[27] (2010) in rural Kerala (32.5%), by Singh et al.[28] (2016) in rural Andhra Pradesh (36.4%), by Swaminathan et al.[29] (2017) in rural Tamil Nadu (37.8%), by Tushi et al.[30] (2018) in rural Nagaland (43.2%), and by Mohanraj et al.[31] (2019) in Suburban Tamil Nadu (47.1%).
However, according to National Family Health Survey-4 (NFHS-4), prevalence of hypertension was low compared to our study. NFHS-4 data has revealed that 11% of women and 14.8% of men aged 15–49 have hypertension. There was a consistent and steep increase in the prevalence of hypertension with increases in BMI for both sexes;.29% of obese women and 38% of obese men were found to be hypertensive in NFHS-4.[32] In Uttar Pradesh, 9.2% of women and 11.1% of men were having hypertension. However, prevalence of hypertension in Varanasi district was below the national level. Only 5.1% of women (urban: 5.6%, rural: 4.8%) and 6.4% (urban: 7.4%, rural: 5.6%) of men were hypertensive.[33] A major limitation of the NFHS-4 survey is the inclusion of adults only up to the age of 49 years. Analysis of a cross-sectional survey data from the fourth round (2015–2016) of National Family Health Survey (NFHS) by Ghosh et al.[34] (2019) and Kumar and Misra[35] (2021) also showed advancing age, obesity/overweight, male sex, consumption of alcohol, and contrarily high socioeconomic status as the major predictors of hypertension. In coherence with the present study findings, a multivariate regression analysis done in ICMR-INDIAB study by Bhansali et al.[36] (2015) and a quantitative analysis by Rao et al.[37] (2013) in coastal Karnataka also identified advancing age, central obesity, overweight, and obesity as defined by BMI as significantly correlated for hypertension by multivariate logistic regression. A study conducted in nine villages of a rural block of Vellore district, Tamil Nadu by Oommen et al.[25] (2016) also revealed that hypertension was significantly associated with increasing age, male sex, urban residence, use of alcohol, scheduled caste status, low physical activity, BMI ≥25 kg/m2, central obesity, and a family history of hypertension. In contrast to a present result, studies by Parthaje[38] (2016), Bhise and Patra[39] (2018), Corsi and Subramanian[40] (2019), Prenissl et al.[41] (2019), Patel et al.[42] (2020) showed higher odds for hypertension for higher household economic status and higher educational status. The possible explanations for the lower prevalence of hypertensive subjects among higher education and higher socioeconomic class in this study may be attributed to better awareness of hypertension prevention and control measures, better adherence to medical advice, including lifestyle modifications among higher socioeconomic status groups, as well as possible higher job strain among lower socioeconomic status groups.
Variations in the extent of hypertension in the abovementioned studies may be due to disparity in settings, attributes of study subjects, and differences in time frame. In India, Primary Health Care facilities happen to be the first point of contact of the population with health services. This is also valid for detection and management of NCDs in general and hypertension in particular. The findings of this study provide significant inputs for prevention, screening, and focused attention of subjects from rural India.
Globally, 51% of men and 41% of women, that is, 580 million individuals in total were unaware of their condition because they were never diagnosed with hypertension.[43] This calls for concerted efforts by primary healthcare physicians in the early diagnosis and timely management of the condition.
Well representative sample of adults and use of pretested and validated tools stands out to be the strength of the study. However, the cross-sectional nature of the survey only provides the burden of hypertension at a point in time. The study focuses only on the rural adult population; thus, the nation-based estimates are desirable. A large community-based study including both rural and urban populations is required to ascertain the exact prevalence and predictors of hypertension in the community. Social desirability bias may have led to over or under-reporting related to tobacco and alcohol.
This study reflects three out of ten study subjects as hypertensive; subjects in higher age range, from lower socioeconomic class, tobacco consumer and with high waist circumference as well as WHR as predictors for hypertension.
The study refutes the age-old concept that hypertension is not a major problem in rural India. There is a big chunk of the population unaware of their hypertension status. The findings of the study give the message that focus should shift from expensive tertiary care to primary health care settings for combating lifelong management of hypertension.
Conclusion
Three out of ten subjects were hypertensive. Advancing age, tobacco dependence, socioeconomic adversities, and high central obesity predisposed individuals to hypertension.
These findings call for targeted attention for maximum risk reduction in terms of dietary modification, optimum nutrition, and increased physical activity for curbing hypertension in rural subjects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to thank all the subjects for their participation in the study.
References
- 1.World Health Organization. Global action plan for the prevention and control of noncommunicable diseases, 2013-2020. [Last assessed on 2021 Feb 02]. pp. 1–103. Available from:https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf;jsessionid=993FD743F06FE0D93E3183921550AD73?sequence=1 .
- 2.World Health Organization. Noncommunicable Diseases Country Profiles 2018. [Last accessed on 2021 Mar 01]. Available from:https://www.who.int/nmh/countries/ind_en.pdf?ua=1 .
- 3.World health organization. Hypertension key facts. [Updated 2021 May 17]. [Last accessed on 2021 May 20]. Available from:https://www.who.int/news-room/fact-sheets/detail/hypertension .
- 4.Global health:Time for radical change? Lancet. 2020;396:1129. doi: 10.1016/S0140-6736(20)32131-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization [Internet] Geneva: [Updated 2018 April 24]. [Last accessed on 2021 Jan 20]. Noncommunicable diseases country profiles 2018 Licence:CC BY-NC-SA 3.0 IGO. Available from:https://www.who.int/publications/i/item/9789241514620 . [Google Scholar]
- 6.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality:A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 7.Fronteira I, Sidat M, Magalhães JP, de Barros FPC, Delgado AP, Correia T, et al. The SARS-CoV-2 pandemic:A syndemic perspective. One Health. 2021;12:100228. doi: 10.1016/j.onehlt.2021.100228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Hypertension Fact Sheet. [Last assessed on 2020 Nov 28]. Available from:https://www.who.int/news-room/fact-sheets/detail/hypertension .
- 9.Washington (DC): National Academies Press (US).; 2010. Institute of Medicine (US) Committee on Public Health Priorities to Reduce and Control Hypertension. A Population-Based Policy and Systems Change Approach to Prevent and Control Hypertension. Bookshelf ID:NBK220087;PMID:25032370. DOI:10.17226/12819. [PubMed] [Google Scholar]
- 10.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019:Update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Registrar General and Census Commission of India. Census of India (2011). Ministry of Home Affairs, Government of India. [Last assessed on 2021 Jan 12]. Available from:https://censusindia.gov.in.
- 12.District Statistical magazine Internet based Data entry and retrieval system, National Information Centre Ministry of Electronics and Information Technology (MeitY), Govt of India. Available from:http://updes.up.nic.in/spideradmin/Hpag|ne1.jsp .
- 13.Gupta R, Ram CVS. Hypertension epidemiology in India:Emerging aspects. Curr Opin Cardiol. 2019;34:331–41. doi: 10.1097/HCO.0000000000000632. [DOI] [PubMed] [Google Scholar]
- 14.Pandey VK, Aggarwal P, Kakkar R. Modified BG Prasad socio-economic classification, update –2019. Indian J Comm Health. 2019;31:123–5. [Google Scholar]
- 15.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure:The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 16.Jelliffe DB. Geneva: World Health Organisation; 1966. The Assessment of the Nutritional Status of the Community; pp. 50–77. Monograph series No. 53. [Google Scholar]
- 17.National Centre for Disease Control, Training Module for Medical Officers for Prevention Control and Population Level Screening of Hypertension, Diabetes and Common Cancer. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke. 2017. pp. 1–47. Available from:http://nhsrcindia.org/sites/default/files/Module%20for%20MOs%20for%20Prevention%2CControl%20%26%20PBS%20of%20Hypertension%2CDiabetes%20%26%20Common%20Cancer.pdf.
- 18.World Health Organization (WHO) World Health Organization; Geneva, Switzerland: 1998. “Obesity:Preventing and managing the global epidemic,”WHO Technical Report Series 894. [PubMed] [Google Scholar]
- 19.World Health Organization. World Health Organization; Geneva, Switzerland: 2005. “WHO STEPS surveillance manual:The WHO STEP wise approach to chronic disease risk factor surveillance, ”Tech. Rep. TOC-1 to 7-2-3. Available from:http://www.who.int/chp/steps/manual/en/index.html. [Google Scholar]
- 20.Mathur P, Kulothungan V, Leburu S, Krishnan A, Chaturvedi HK, Salve HR, et al. National noncommunicable disease monitoring survey (NNMS) in India:Estimating risk factor prevalence in adult population. PLoS One. 2021;16:e0246712. doi: 10.1371/journal.pone.0246712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chow C, Cardona M, Raju PK, Iyengar S, Sukumar A, Raju R, et al. Cardiovascular disease and risk factors among 345 adults in rural India--The Andhra Pradesh Rural Health Initiative. Int J Cardiol. 2007;116:180–5. doi: 10.1016/j.ijcard.2006.03.043. [DOI] [PubMed] [Google Scholar]
- 22.Krishnan A, Shah B, Lal V, Shukla DK, Paul E, Kapoor SK. Prevalence of risk factors for non-communicable disease in a rural area of Faridabad district of Haryana. Indian J Public Health. 2008;52:117–24. [PubMed] [Google Scholar]
- 23.Todkar SS, Gujarathi VV, Tapare VS. Period prevalence and sociodemographic factors of hypertension in rural Maharashtra:A cross-sectional study. Indian J Community Med. 2009;34:183–7. doi: 10.4103/0970-0218.55269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. ICMR–INDIAB Collaborative Study Group. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India:Phase I results of the Indian Council of Medical Research-India DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 25.Oommen AM, Abraham VJ, George K, Jose VJ. Prevalence of risk factors for non-communicable diseases in rural and urban Tamil Nadu. Indian J Med Res. 2016;144:460–71. doi: 10.4103/0971-5916.198668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramakrishnan S, Zachariah G, Gupta K, Shivkumar Rao J, Mohanan PP, Venugopal K, et al. Prevalence of hypertension among Indian adults:Results from the great India blood pressure survey. Indian Heart J. 2019;71:309–13. doi: 10.1016/j.ihj.2019.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thankappan KR, Shah B, Mathur P, Sarma PS, Srinivas G, Mini GK, et al. Risk factor profile for chronic non-communicable diseases:Results of a community-based study in Kerala, India. Indian J Med Res. 2010;131:53–63. [PubMed] [Google Scholar]
- 28.Singh MK, Singamsetty B, Kandati J. An epidemiological study of prevalence of hypertension and its risk factors in a rural community of Nellore, Andhra Pradesh, India. Int J Community Med Public Health. 2016;3:3408–14. [Google Scholar]
- 29.Swaminathan K, Veerasekar G, Kuppusamy S, Sundaresan M, Velmurugan G, Palaniswami NG. Noncommunicable disease in rural India:Are we seriously underestimating the risk?The Nallampatti noncommunicable disease study. Indian J Endocrinol Metab. 2017;21:90–5. doi: 10.4103/2230-8210.196001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tushi A, Rao SR, Pattabi K, Kaur P. Prevalence of risk factors for non-communicable diseases in a rural tribal population of Mokokchung, Nagaland, India. Natl Med J India. 2018;31:11–4. doi: 10.4103/0970-258X.243405. [DOI] [PubMed] [Google Scholar]
- 31.Mohanraj S, Swaminathan K, Velmurugan G, Alexander T, Palaniswami NG. Prevalence of hypertension and associated risk factors in Suburban Tamil Nadu. Apollo Med. 2019;16:216–9. [Google Scholar]
- 32.Indian Institute for Population Sciences (IIPS) and MoHFW, National Family Health Survey-4, National Fact sheet India. 2017 [Google Scholar]
- 33.Indian Institute for Population Sciences (IIPS) and MoHFW. National Family Health Survey-4. District Fact sheet. Varanasi Uttar Pradesh: 2017. [Google Scholar]
- 34.Ghosh S, Kumar M. Prevalence and associated risk factors of hypertension among persons aged 15–49 in India:A cross-sectional study. BMJ Open. 2019;9:e029714. doi: 10.1136/bmjopen-2019-029714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kumar K, Misra S. Sex differences in prevalence and risk factors of hypertension in India:Evidence from the National Family Health Survey-4. PLoS One. 2021;16:e0247956. doi: 10.1371/journal.pone.0247956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhansali A, Dhandania VK, Deepa M, Anjana RM, Joshi SR, Joshi PP, et al. Prevalence of and risk factors for hypertension in urban and rural India:The ICMR-INDIAB study. J Hum Hypertens. 2015;29:204–9. doi: 10.1038/jhh.2014.57. [DOI] [PubMed] [Google Scholar]
- 37.Rao CR, Kamath VG, Shetty A, Kamath A. High blood pressure prevalence and significant correlates:a quantitative analysis from coastal karnataka, India. ISRN Prev Med. 2012;2013:574973. doi: 10.5402/2013/574973. doi:10.5402/2013/574973. PMID:24967139;PMCID:PMC4062860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parthaje PM, Unnikrishnan B, Thankappan KR, Thapar R, Fatt QK, Oldenburg B. Prevalence and correlates of prehypertension among adults in urban South India. Asia Pac J Public Health. 2016;28(1 Suppl):93S–101S. doi: 10.1177/1010539515616453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhise MD, Patra S. Prevalence and correlates of hypertension in Maharashtra, India:A multilevel analysis. PLoS One. 2018;13:e0191948. doi: 10.1371/journal.pone.0191948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corsi DJ, Subramanian SV. Socioeconomic gradients and distribution of diabetes, hypertension, and obesity in India. JAMA Netw Open. 2019;2:e190411. doi: 10.1001/jamanetworkopen.2019.0411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prenissl J, Manne-Goehler J, Jaacks LM, Prabhakaran D, Awasthi A, Bischops AC, et al. Hypertension screening, awareness, treatment, and control in India:A nationally representative cross-sectional study among individuals aged 15 to 49 years. PLoS Med. 2019;16:e1002801. doi: 10.1371/journal.pmed.1002801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patel SA, Ali MK, Alam D, Yan LL, Levitt NS, Bernabe-Ortiz A, et al. Obesity and its relation with diabetes and hypertension:A cross-sectional study across 4 geographical regions. Glob Heart. 2016;11:71–9. doi: 10.1016/j.gheart.2016.01.003. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.World Health Organization. News More than 700 million people with untreated hypertension. [Last accessed on 2021 Sep 30]. Available from:https://www.who.int/news/item/25-08-2021-more-than-700-million-people-with-untreated-hypertension .


