Summary
Background
The objective of this study was to describe 12-month mortality following SARS-CoV-2 infection compared with a reference population with no history of SARS-CoV-2.
Methods
Nationwide cohort study using electronic health care data on SARS-CoV-2 RNA positive cases (n= 66,287) and reference group subjects (n=254,969) with linkage to SARS-CoV-2 testing and death records.
Findings
People infected with SARS-COV-2 had more than three times the risk of dying over the following year compared with those who remained uninfected (aHR 3·1, 95%CI 2·9-3·3). Short-term mortality (up to 5 weeks post-infection) was significantly higher among COVID-19 group (1623·0/10 000) than in the reference group (118/10 000). For COVID-19 cases aged 60 years or older, increased mortality persisted until the end of the first year after infection, and was related to increased risk for cardiovascular (aHR 2·1, 95%CI 1·8-2·3), cancer (aHR 1·5, 95%CI 1·2-1·9), respiratory system diseases (aHR 1·9, 95%CI 1·2-3·0), and other causes of death (aHR 1·8, 95%CI 1·4-2·2).
Interpretation
Increased risk of death from SARS-CoV-2 is not limited to the acute illness: SARS-CoV-2 infection carries a substantially increased mortality in the following 12 months. This excess death mainly occurs in older people and is driven by broad array of causes of death.
Funding
Research was carried out with the support of Estonian Research Council (grants PRG1197, PRG198), European Regional Development Fund (RITA 1/02-120) and European Social Fund via IT Academy program.
Keywords: COVID-19, Mortality, Estonia, Population-based, Cardiovascular death, SARS-CoV-2
Research in context.
Evidence before this study
As the COVID-19 pandemic continues, the need to understand and respond to long-term effects of the infection is increasingly pressing. The full range of long-term health consequences of COVID-19 is yet to be described. Most evidence about long-term effects COVID-19 has been limited and based on small cohorts (mostly of hospitalised COVID-19 cases) with short follow-up.
Added value of this study
The added value of our study is three-fold—first, we directly measured previously unmeasured 1-year mortality among SARS-CoV-2 cases; second, we showed that those who had SARS-CoV-2 have more than three times the risk of dying over the following year compared with those who remain uninfected (aHR 3·1, 95%CI 2·9-3·3), and third, this, increased risk of death was not limited to acute-SARS-CoV-2 infection period. Post-acute COVID-19 excess death is mainly affecting older people.
Implications of all evidence available
Increased risk of death from COVID-19 is not limited to the acute episode of SARS-CoV-2 infection, and having had SARS-CoV-2 carries with it a substantially increased mortality in the following 12 months. Within 1-year follow up, 60·6% of all deaths among SARS-CoV-2 cases occurred in individuals with severe or critical acute COVID-19. Continuing post-acute SARS-CoV-2 increased mortality by broad array of causes among older individuals calls for multi-disciplinary and targeted interventions to prevent these deaths.
Alt-text: Unlabelled box
Introduction
Infection with the SARS-CoV-2 virus (termed COVID-19) has had an enormous impact on public health and socioeconomic conditions globally. The COVID-19 pandemic has triggered life expectancy losses not seen since World War II in Western Europe and exceeded those observed around the dissolution of the Soviet Union in central and Eastern European countries.1 Evidence of the factors related to, and the total mortality impact of, COVID-19 is needed to inform preventive measures and the clinical management of COVID-19 patients. The clinical manifestations and mortality2,3 of acute COVID-19 in hospitalised patients have been well characterised, but evidence on the post-acute sequelae of this disease is still accumulating. Emerging reports suggest that excess mortality attributable to COVID-19 persists beyond the acute disease.2,4 However, most of the evidence on post-acute COVID-19 sequelae is limited to hospitalised cases2,5 over a relatively short period after the acute disease. In most settings, information on causes of death and the contribution of pre-existing health conditions to post-COVID-19 mortality is scarce.
The objective of this study was to compare post-acute COVID-19 mortality with a reference population with no history of COVID-19 over the first year of the COVID-19 epidemic in Estonia.
Methods
This nationwide, population-based cohort study used electronic health care data linked with SARS-CoV-2 testing and death records.
Data sources
National communicable disease case notification data
The Estonian Health Board (EHB) is a state agency that collects and analyses notification data on communicable diseases (which now includes all SARS-CoV-2 testing). Confirmed SARS-CoV-2 infection cases are based on real-time polymerase chain reaction (PCR) testing on nasopharyngeal specimens by a certified molecular diagnostics laboratory using certified methods.
The Estonian Health Insurance Fund (HIF)
By the end of 2020, universal public health insurance covered 95.2% of the Estonian population (1,328,889 people).6 Since its inception in the early 2000s, the HIF has maintained a complete record of health care services. Diagnoses are defined according to International Classification of Diseases, tenth revision (ICD-10). The HIF database records personal details (sex, age) and health care utilisation (date of service, primary and other diagnoses, and treatment type: in- or out-patient).
Estonian Causes of Death Registry (CDR)
The CDR collects data on all deaths registered among the residents of Estonia. Deaths are reported to the registry using a standard death certificate including the causes and date of death. The underlying cause of death is coded and processed in accordance with WHO standards using ICD-10. The registry conforms to the quality assurance criteria of the EUROSTAT.
The Population Register is a unified database of Estonian citizens and foreign nationals living in Estonia on the basis of right of residence or residence permit and is administered and developed by the Ministry of the Interior. The Population Register data was used identify study subject's residence location (incl emigration status).
In Estonia, unique 11-digit personal identification codes (PIC-s) are assigned to all residents at birth or at the time of immigration. PIC as single unique identifier is recorded accurately in all three data sources used in this study, enabling a straightforward and complete linkage between sources for cohort formation.
Population and setting
We included data on all people who tested positive for SARS-CoV-2 during the first year of the COVID-19 epidemic (26 February 2020 to 28 February 2021). SARS-CoV-2 infection cases entered the cohort on the index date (the 1st positive SARS-CoV-2 test date), with reference group subjects added from the same date. By the end of February 2021, only 6.0% of the population had received at least one dose of vaccine, and 2.6% had completed the initial vaccination protocol. In the people infected before 28 February 2021 (included in the present study), the respective vaccination rates were 4.1% and 1.8% by that date.
Cohort
The SARS-CoV-2 group (n= 66,287) comprised cases identified from the EHB database. Details of the personal identification code and date of SARS-CoV-2 positive specimen collection were abstracted.
The reference group (n=254,969) comprised an index date time-matched7 random subset of individuals insured by the HIF who were alive at the SARS-CoV-2 infection case index date but had no evidence of SARS-CoV-2. We used a SARS-CoV-2 infection case-to-reference group subject ratio of 1:4 (without replacement).8
For both SARS-CoV-2 cases and reference group subjects, health care data were abstracted from the HIF database for the period of 12 months before (for co-morbidity assessment) and for SARS-CoV-2 cases up to 30 days after the index date (for the early period disease severity assessment; including an acute COVID-19 severity assessment). All-cause and cause specific mortality was identified using the cause and date of death in the primary CDR record.
Outcome and covariates
Our primary outcome was all-cause mortality during the follow up. We measured time-to-event from the index date until either death, the study observational period end (November 14, 2021) or when the participant was censored (reference group subjects only - at the date of the first positive SARS-CoV-2 test). We assumed that patients not listed in the national mortality registry were alive as of November 14, 2021.
We constructed three mutually exclusive follow-up periods to better account for potentially time-varying risks after SARS-CoV-2 infection. These were (i) the first 5 weeks after a positive test (0-35 days; short-term mortality); (ii) the subsequent 7 weeks (36-84 days; mid-term mortality); and (iii) the remainder of the observation period (starting from week 8; long-term mortality).
Covariates were pre-selected based on literature and expert opinion to be relevant and routinely available rather than based on statistical significance.
Acute disease (COVID-19) severity
The ‘acute COVID-19 (SARS-CoV-2 infection)’ episode was classified as being (i) non-severe (patients who required no medical care or ambulatory medical care only); (ii) severe (patients who required hospitalisation but no intensive care); or (iii) critical (patients who received intensive care).9 For reference group, we created analogous disease severity variables – (i) non-severe (requiring no medical care or ambulatory medical care only); (ii) severe (requiring hospitalisation but no intensive care); or, (iii) critical (receiving intensive care) based on health care utilisation within the five weeks from the respective index dates.
Pre-COVID-19 comorbidity
Comorbidities were captured for the 365-day period prior to the index date for SARS-CoV-2 cases and reference group subjects. The comorbidity status for both groups was computed using the Charlson comorbidity index (CCI).10 Cohort members were divided into three groups comprising those with no (CCI score of 0), one (CCI score of 1) or at least two (CCI scores ≥2) comorbid conditions.
We also constructed a variable to assess an individual's contacts with the health care system by counting the number of out-patient visits and hospitalisations within the three years preceding the index date (ranging from 0 – no contacts with health care to 5 – hospitalised for over than 7 days). In addition, we had data on study subject's residence (at the county level).
Causes of death
Cause of death statements were classified following WHO guidelines into immediate causes of death, conditions leading to cause of death, underlying causes and further relevant conditions that may have contributed to the fatal outcome.11 Cause of death was assigned using the underlying cause of death field (main/primary cause of death coded in ICD-10) in the death registration certificate. A COVID-19 death was defined as any death with the underlying cause coded as U07.1 (“COVID-19, virus identified”) or U07.2 (“COVID-19, virus not identified”). Non-COVID deaths comprised all other deaths; these were also further sub-divided into categories covering the most common causes of death, namely cancer (ICD-10 chapter C00-D48), cardiovascular disease (chapter I00-I99), respiratory conditions (chapter J00-J99) and other (all other ICD-10 codes).
Statistical analysis
Demographic and health status data are reported as frequencies and proportions for categorical variables and as means with standard deviations (SD) and range for continuous variables. Crude mortality rates and confidence intervals for mortality rates were obtained using Poisson regression. Using age groups 0-29, 30-34, 35-39, …, 80-84, 85+ years, also the age-standardized mortality ratio was obtained with 95%CI (from Poisson regression).
An important factor in coherent mortality models is the reference population or group of populations that are modelled together.12 We conducted sensitivity analysis to test the robustness of estimates for SARS-CoV-2 infection related mortality based on a reference group sampled from the list of individuals covered by the Estonian HIF. For this analysis, an alternative reference population data (pre-COVID pandemic, year 2019 in Estonia13 on total population yearly mortality by age group) was used for standardised mortality ratio (SMR) calculations.
We used Kaplan-Meier curves to represent cumulative probabilities of dying during each of the three follow-up periods. For the 2nd and 3rd (mid- and long term) periods, only individuals under follow-up by the beginning of the corresponding period were included (the number of persons at risk for Kaplan Meier plots are presented in Supplement Table 3S). To estimate hazard ratios, we used Cox's proportional hazards model fitting two models: the base model (adjusted for sex and age) and an adjusted model. The adjusted model included all baseline covariates (age, sex, period, pre-index date Charlson comorbidity index, health care utilization intensity, and the county of Estonia). We tested the proportional hazards assumption for the survival model using a test based on Schoenfeld residuals. In case the assumption of proportional hazards was not valid (either for the overall follow-up period or separately in the three follow-up periods), a time-varying model was used to allow the SARS-CoV-2 case- reference group subject hazard ratio to change over different periods of follow up. The final model allowed the COVID-19 case- reference group subject hazard ratio to differ across six intervals: the early acute period was divided into three intervals (1-10, 11-20 and 21-35 days), mid-term mortality period into two intervals (36-50 and 51-84 days), and the long-term mortality (85-365 days). There was no indication of non-proportionality of hazards within any of these intervals. We saw a significant interaction of the SARS-CoV-2 case- reference group subject status and age in their effects on mortality. Therefore, data on individuals aged below 60 and 60 or older were modelled separately14 (using the same covariates in multivariable models).
For cause-specific mortality, Kaplan-Meier graphs for cumulative mortality are presented, using the multi-state modelling approach to account for competing risks. To estimate cause-specific hazard ratios, Cox models were used separately for each cause, while treating deaths due to other causes as censoring. Further, we used the attributable mortality percentage (AM%) to quantify the proportion of deaths attributable to SARS-CoV-2 infection as a risk factor. The AM% was calculated by dividing the difference in cause-specific mortality between SARS-CoV-2 and reference groups by the cause-specific mortality in the SARS-CoV-2 group and then multiplying the product by 100 to obtain a percentage.15
Missing data were uncommon. Only region of residence (county) had a substantial number of missing values (5.9%). No attempt was made to impute missing values.
Statistical analyses were completed in R version 4.1.0.
The study was approved by the Research Ethics Committee of the University of Tartu.
The funding agencies had role in study design, data collection, data analysis, interpretation, writing of the report.
Results
Cohort description
The cohort comprised 66,287 people who tested positive for SARS-CoV-2 RNA between 26 February 2020 and 28 February 2021, and 254,969 randomly selected individuals from the reference population (Table 1). People with SARS-CoV-2 infection were slightly older in average, with a mean age of 44·0 (SD 20·6) years versus 42·4 (SD 22·9) years for reference group subjects (a difference of 1·7 years, 95%CI 1·5-1·9 years, p<0·001); 35,806 (54·0%) and 130,620 (51·2%) subjects were female (p<0·001) in the SARS-CoV-2 and reference groups, respectively. The age difference is mainly explained by the fact that children aged 0-9 are underrepresented among SARS-CoV-2 cases (3·5%) compared to reference group (9·6%), whereas the proportion of individuals aged 60 or above is even slightly lower in SARS-CoV-2 cases (23·5%) than in reference group subjects (24·9%, p<0·001). Both cohorts were relatively healthy: 89·8% of SARS-CoV-2 cases and 92·7% of reference group individuals scored 0 on the CCI score (p< 0·0001) (Table 1).
Table 1.
Cohort characteristics and mortality rates, SARS-CoV-2 cases and the reference group, Estonia 2020-2021.
| SARS-CoV-2 group |
Reference group |
||||||
|---|---|---|---|---|---|---|---|
| N |
% |
Crude mortality rate per 10 000 py |
N |
% |
Crude mortality rate per 10 000 py |
||
| Number | 66287 | 342·1 | 254969 | 106·3 | |||
| Sociodemographic characteristics | |||||||
| Sex | |||||||
| Female | 35806 | 54·0 | 355·3 | 130620 | 51·2 | 109·8 | |
| Male | 30481 | 46·0 | 326·7 | 124349 | 48·8 | 102·6 | |
| Age (mean, SD, range) | 44·1 | 20·6 | 0-103·7 | 42·4 | 22·9 | 103·7 | |
| Age groups | |||||||
| 0-9 | 2288 | 3·5 | 0·0 | 24584 | 9·6 | 4·3 | |
| 10-19 | 7219 | 10·9 | 4·9 | 25962 | 10·2 | 5·1 | |
| 20-29 | 8226 | 12·4 | 4·2 | 28286 | 11·1 | 4·7 | |
| 30-39 | 11704 | 17·7 | 14·8 | 42522 | 16·7 | 9·6 | |
| 40-49 | 11188 | 16·9 | 33·9 | 37472 | 14·7 | 25·3 | |
| 50-59 | 10095 | 15·2 | 88·0 | 32575 | 12·8 | 55·2 | |
| 60-69 | 8253 | 12·5 | 372·9 | 29466 | 11·6 | 140·5 | |
| 70-79 | 3814 | 5·8 | 1470·1 | 20044 | 7·9 | 313·2 | |
| 80+ | 3500 | 5·3 | 4592·8 | 14058 | 5·5 | 959·0 | |
| Region | |||||||
| Harju | 35409 | 53·4 | 295·3 | 106815 | 41·9 | 90·7 | |
| Ida-Viru | 11346 | 17·1 | 376·7 | 24023 | 9·4 | 149·2 | |
| Other | 18901 | 28·5 | 416·8 | 105585 | 41·4 | 129·0 | |
| Missing | 631 | 1·0 | 105·5 | 18546 | 7·3 | 12·4 | |
| Pre-index date comorbidity | |||||||
| Charlson comorbidity index (mean, SD, range) | 0·2 | 0·5 | 0-9 | 0·1 | 0·4 | 0-9 | |
| Charlson comorbidity index groups | |||||||
| 0 | 59528 | 89·8 | 162·8 | 236306 | 92·7 | 66·1 | |
| 1 | 4246 | 6·4 | 1693·7 | 12224 | 4·8 | 46·8 | |
| 2+ | 2513 | 3·8 | 2868·5 | 6439 | 2·5 | 933·5 | |
| Acute period disease severity | |||||||
| Out-patient care only | 61063 | 92·1 | 128·8 | 250823 | 98·4 | 92·8 | |
| Hospital care | 3557 | 5·4 | 2354·9 | 2106 | 0·8 | 1188·1 | |
| Intensive care | 1467 | 2·2 | 5423·2 | 666 | 0·3 | 2006·9 | |
| Unknown | 200 | 0·3 | 7249·6 | 1374 | 0·5 | 221·0 | |
Among the 66,287 individuals in the SARS-CoV-2 group, the overwhelming majority (92·1%, n=61,063) had a non-severe course of COVID-19; 5·4% (n=3,557) had severe disease (requiring hospitalisation) and 2·2% (n=1,467) had critical disease (needing intensive care). In the reference group, within the acute period (up to five weeks after the index date), 0·8% had a health condition requiring hospitalization (n=2,106), and 0·3% (n=666) needed intensive care.
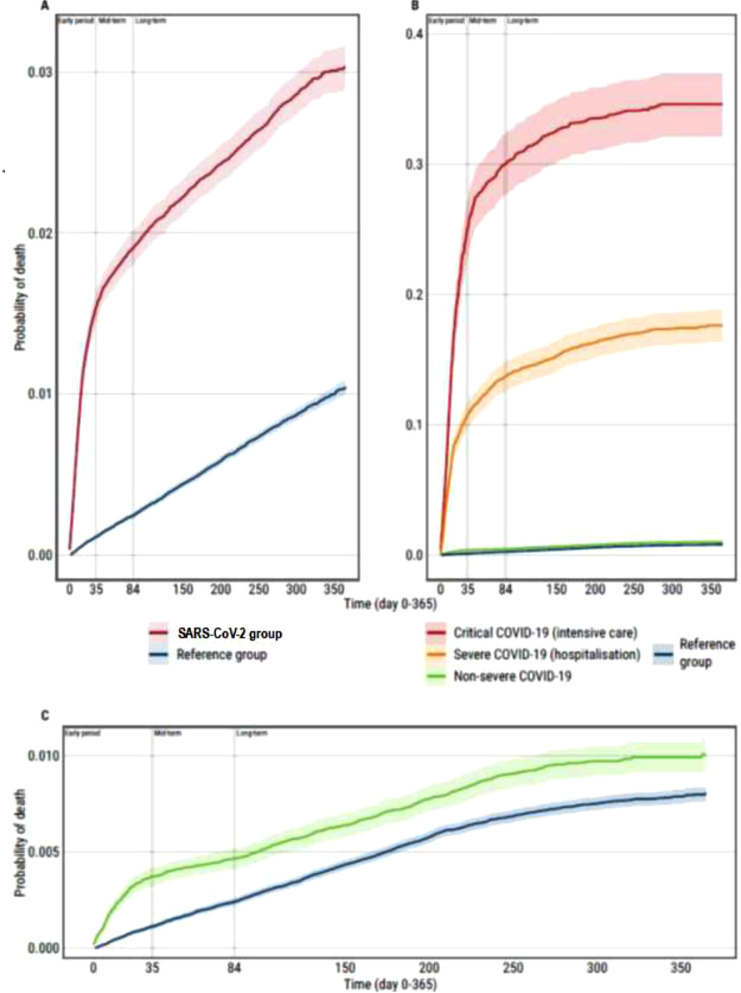
Overall mortality rates
The overall mortality rate was 342·1/10,000 person years (95%CI 327·2-357·7) (1,933 deaths) in the SARS-CoV-2 group and 106·3/10,000 person years (95%CI 102·0-110·7) (2,262 deaths) in the reference group (the crude mortality ratio in cases versus reference group subjects 3·2, 95%CI 3·0-3·4) (Table 1, Figure 1). The age-standardized mortality ratio between SARS-CoV-2 cases and reference group subjects was 3·8 (95%CI 3·6-3·9), which leads to the estimate of SARS-CoV-2 infection related attributable mortality (AM) fraction of 73·3% (95%CI 72·2-74·5%).
Figure 1.
Cumulative probability of dying by group status: SARS-CoV-2 cases (all (A) and by disease severity (B)) and reference group, one year post- SARS-CoV-2 infection period, Estonia 2020-2021.
Among SARS-CoV-2 cases, 60·6% of all deaths were attributed to individuals with severe (n=657) or critical (n=515) COVID-19.
The overall standardized mortality ratio (SMR) in cases, compared to population data in 2019, was 3·7 (95%CI 3·5-3·9). When reference group was compared with the 2019 population, the SMR was found to be 1·0 (95%CI 0·9-1·1), indicating no significant mortality difference in reference group and the overall population in the pre-COVID year, 2019.
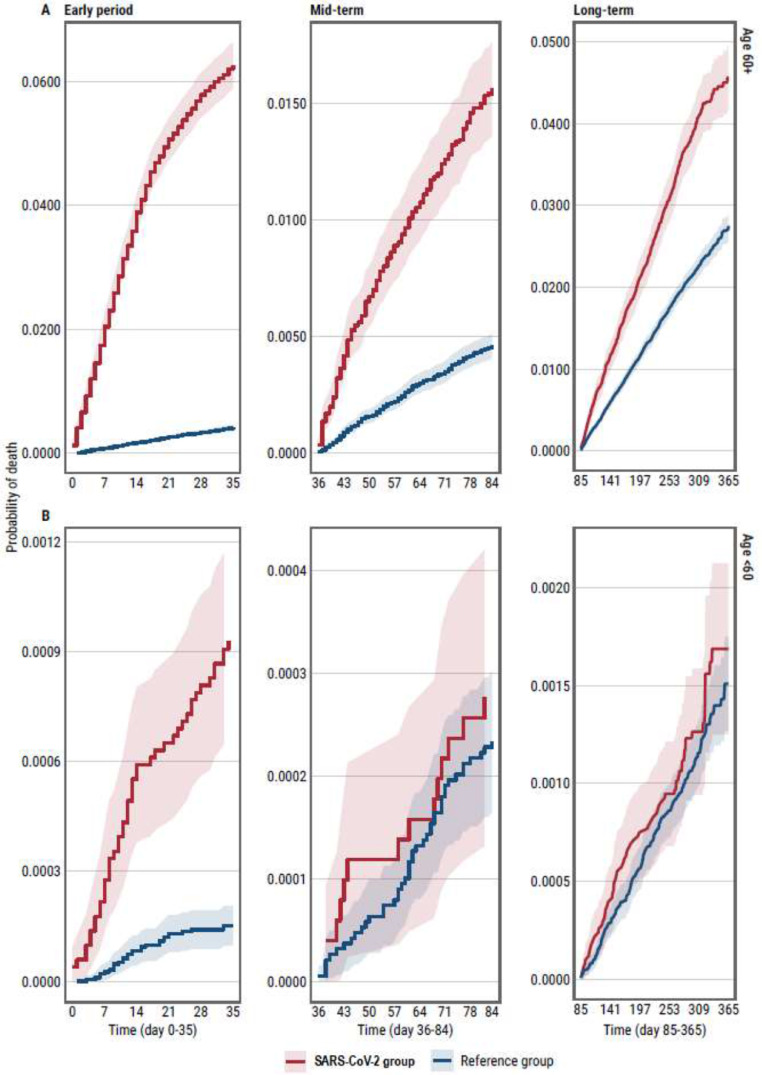
Follow-up period specific mortality
Mortality (per 10,000 person years with 95%CI) during the first five weeks after the index date was 1623·0 (95%CI 1526·4-1725·7) among SARS-CoV-2 cases and 117·8 (95%CI 105·0-132·3) among reference group subjects (crude mortality ratio 13·8, 95%CI 12·1-15·7). For those who survived for 5 weeks, mid-term mortality (up to 12-weeks post index date) was 276·5 (95%CI 243·7-313·6) for SARS-CoV-2 cases and 97·9 (95%CI 87·9-109·0) for reference group (crude mortality ratio 2·8, 95%CI 2·4-3·3). Among those surviving over 12 weeks, long-term mortality (to the end of the observation period) was 118·7 (95%CI 110·1-128·1) for SARS-CoV-2 cases and 77·5 (95%CI 73·8-81·3) for reference group (crude mortality ratio 1·5, 95%CI 1·4-1·7). Cumulative all-cause mortality curves by age and observation period are shown in Figure 2.
Figure 2.
Cumulative probability of dying by age group among SARS-CoV-2 cases and reference group by the period of observation (early, mid- and long-term post-acute SARS-CoV-2 infection), Estonia 2020-2021. (A) SARS-CoV-2 cases compared to reference group (among those 60 years and older); (B) SARS-CoV-2 cases compared to reference group (among those less than 60 years old).
Data on deaths occurring in those aged 18 years or less (n=22) were excluded from this analysis· While SARS-CoV-2 case status was associated with increased all-cause mortality across the whole study period, there was considerable variation over the periods of follow up and by age (see Table 2, and Supplement Table S1).
Table 2.
Adjusted time-dependent hazard ratios comparing overall and cause-specific mortality in SARS-CoV-2 cases and reference group in two age groups across different stages of follow-up, Estonia 2020-2021.
| OVERALL MORTALITY | ||||||
|---|---|---|---|---|---|---|
| Age <60 |
Age 60+ |
|||||
| Adjusted hazard ratio * (95% CI) | p-value | Deaths in SARS-CoV-2 cases/reference group | Adjusted hazard ratio (95% CI) | p-value | Deaths in SARS-CoV-2 cases/reference group | |
| Early, acute period | 4·7 (3·0-7·5) | <0·0001 | 47/28 | |||
| 1-10 days | 20·1 (15·5-26·1) | <0·0001 | 402/67 | |||
| 11-20 days | 15·5 (12·1-19·7) | <0·0001 | 344/80 | |||
| 21-35 days | 7·9 (6·2-9·9) | <0·0001 | 219/105 | |||
| Mid- and long-term | 0·9 (0·7-1·2) | 0·5360 | 81/244 | |||
| 36-50 days | 3·9 (2·9-5·1) | <0·0001 | 104/104 | |||
| 51-84 days | 2·8 (2·2-3·5) | <0·0001 | 130/184 | |||
| 85-365 days | 1·7 (1·5-1·8) | <0·0001 | 581/1376 | |||
|
CAUSE-SPECIFIC MORTALITY I00-I99: DISEASES OF THE CIRCULATORY SYSTEM | ||||||
| Early, acute period | 1·5 (0·5-5·0) | 0·5038 | 4/8 | 5·4 (4·4-6·6) | <0·0001 | 221/144 |
| Mid- and long-term | 1·1 (0·6-2·2) | 0·6730 | 12/33 | 2·1 (1·8-2·3) | <0·0001 | 401/748 |
| C00-D48: NEOPLASMS | ||||||
| Early, acute period | 4·8 (1·4-15·8) | 0·0109 | 8/4 | 4·3 (3·0-6·3) | <0·0001 | 68/47 |
| Mid- and long-term | 1·0 (0·6-1·7) | 0·9104 | 18/46 | 1·5 (1·2-1·9) | <0·0001 | 135/297 |
| J00-J99: DISEASES OF THE RESPIRATORY SYSTEM | ||||||
| Early, acute period | (0-Inf) | 0·9906 | 2/0 | 29·2 (12·5-68·3) | <0·0001 | 49/6 |
| Mid- and long-term | 2·0 (0·4-8·9) | 0·3684 | 3/4 | 1·9 (1·2-3·0) | 0·0111 | 23/51 |
| OTHER CAUSES | ||||||
| Early, acute period | 1·2 (0·5-3·2) | 0·6731 | 6/14 | 5·0 (3·4-7·6) | <0·0001 | 55/41 |
| Mid- and long-term | 0·8 (0·5-1·3) | 0·3827 | 27/93 | 1·8 (1·4-2·2) | <0·0001 | 117/264 |
*All models are adjusted for age, sex, Charlson comorbidity index and pre-index date health care utilization intensity. The models for overall mortality are additionally adjusted for the county of Estonia. (HR-s corresponding to all adjustment variables as well as sex- and age-adjusted case-control hazard ratios are provided in Online Supplement).
One year all-cause mortality (expressed as adjusted hazard ratio, aHR with 95%CI) was higher among SARS-CoV-2 cases than reference group subjects (aHR 3·1, 95%CI 2·9-3·3).
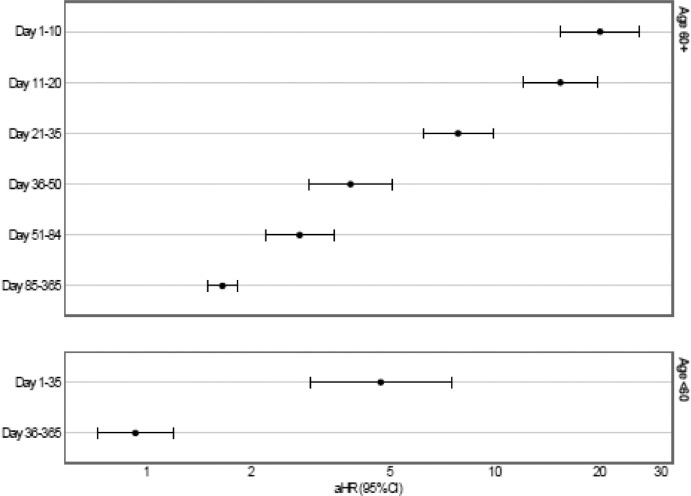
A time-dependent analysis showed that among individuals aged under 60, all-cause mortality was higher among SARS-CoV-2 cases than reference group up to 35-days post positive SARS-CoV-2 test (aHR 4·7, 95%CI 3·0-7·5), but not later in the follow up (mid-and long-term aHR 0·9, 95%CI 0·7-1·2).
Among subjects aged 60 and above, mortality in the SARS-CoV-2 group remained higher than in the reference group for the entire follow-up period (Figures 2, 3), ranging from extremely high risk of death within 10 days of a positive SARS-CoV-2 test (aHR 20·1, 95%CI 15·5-26·1), and being over three times higher during mid-term (weeks 36-84: aHR 3·9, 95%CI 2·9-5·1) and close to two times higher in the long-term period (aHR 1·7, 95%CI 1·5-1·8) (Figure 3).
Figure 3.
Time-varying hazard ratios for death from any cause among SARS-CoV-2 cases compared to reference group (early, mid- and long-term post-acute SARS-CoV-2 infection), Estonia 2020-2021. (A) SARS-CoV-2 cases compared to reference group (among those 60 years and older); (B) SARS-CoV-2 cases compared to reference group (among those less than 60 years old).
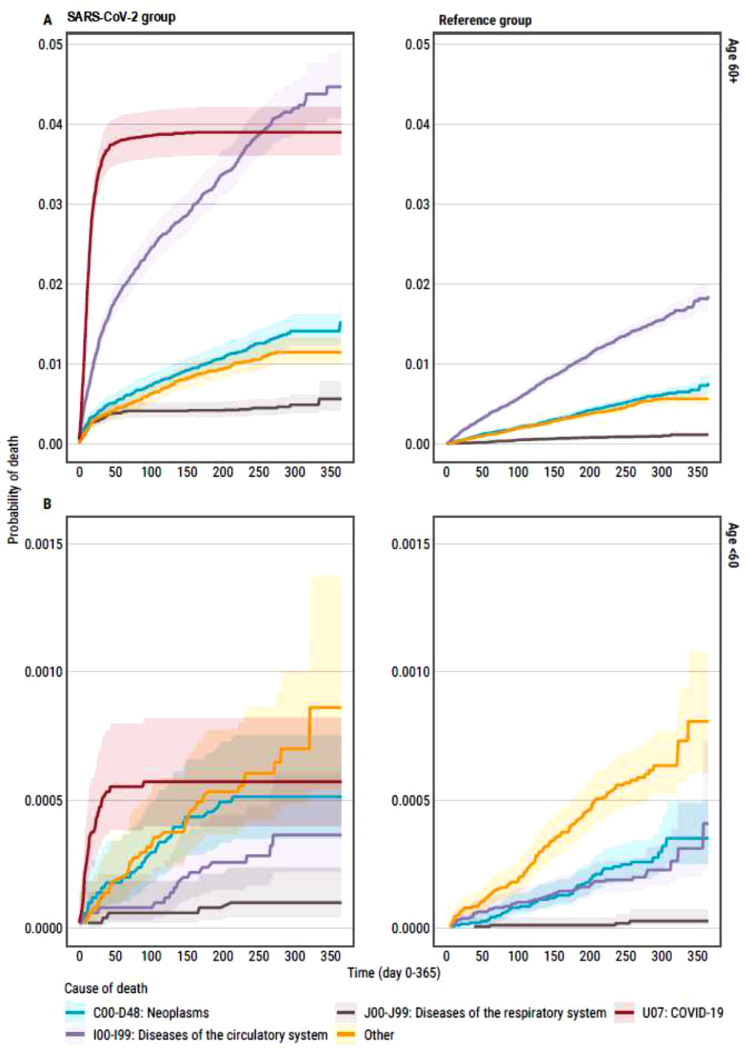
Cause-specific mortality
Cause-specific mortality analysis was limited to 3708 deaths (88·4% of all observed deaths) for which a cause was known at the time of data abstraction. In the SARS-CoV-2 group, there were 636 deaths caused by SARS-CoV-2 infection (35·1% of deaths). Diseases of the cardiovascular system represented 35·9% (n=649) and 50% (n=949) of deaths among COVID-19 cases and reference group (p<0·0001) respectively. One tenth of SARS-CoV-2 cases (n=233, 12·9%) and one fifth of reference group subjects (n=399, 21·0%, p<0·0001) died from a malignant neoplasm. Apart from COVID-19 deaths, hypertensive heart disease (ICD-10 I11) was the most frequent specific cause of death both among SARS-CoV-2 cases (10·8%) and reference group (15·0%); followed by chronic ischaemic heart disease (ICD-10 I25) 6·9% and 8·6%; hypertensive heart and renal disease (ICD-10 I13) 3·9% and 3·8%; and cerebral infarction (ICD-10 I63) 2·3% and 3·2%. The cumulative mortality curves presented in Figure 4 show the cause-specific probabilities of death among SARS-CoV-2 cases and reference group subjects over the follow-up period. (Details of the most frequent causes of death by follow-up period and study group are presented in the Supplement Table S2).
Figure 4.
Competing risk analysis for cause-specific mortality of SARS-CoV-2 cases and in the reference group, Estonia 2020-2021. (A) SARS-CoV-2 cases compared to reference group (among those 60 years and older); (B) SARS-CoV-2 cases compared to reference group (among those less than 60 years old).
Cardiovascular deaths
The overall (age-standardized) SARS-CoV-2 infection attributable mortality fraction of cardiovascular deaths was 68·5% (95%CI 66·1-70·6%).
The mortality risk from cardiovascular diseases among those aged less than 60 years did not differ significantly by follow-up period or from that in the reference group (early period aHR 1·5, 95%CI 0·5-5·0; mid- and long-term aHR 1·1, 95%CI 0·6-2·2) (see Table 2, Figure 4).
Among the population aged 60 years and older, the risk of cardiovascular death in the SARS-CoV-2 cases differed that of in the reference group and over time: it was higher in the early period (aHR 5·4, 95%CI 4·4-6·6) than later in the course of follow up (mid- and long-term mortality aHR 2·1, 95%CI 1·8-2·3). In the first 5 weeks of observation, for SARS-CoV-2 cases, attributable mortality fraction of cardiovascular deaths was 84·8% (95%CI 81·2-87·7%), driven by deaths due to hypertensive heart disease, chronic ischaemic heart disease, hypertensive heart and renal disease, cerebral infarction, and acute myocardial infarction (see Figure 4, Supplement Table S2). Later in the course of the post-covid period (mid- and long-term), attributable mortality of cardiovascular deaths was 55·1% (95%CI 49·2-60·3%) and related to health failure, complications and ill-defined descriptions of heart disease, and hypertensive heart disease hypertensive heart and renal disease, atrial fibrillation, chronic ischaemic heart disease, sequelae of cerebrovascular disease (ICD-10 I69).
Cancer deaths
The overall (age-standardized) SARS-CoV-2 infection attributable mortality fraction of cancer deaths was 61·0% (95%CI 56·1-66·4%).
Mortality related to cancer among the younger SARS-CoV-2 group (<60 years) was higher than in the reference group during the early, acute period (mortality aHR 4·8, 95%CI 1·4-15·8), but not later in the follow-up. In this, younger age group and early period after SARS-CoV-2 infection, SARS-CoV-2 infection attributable mortality fraction of cancer deaths was 86·7% (95%CI 50·4-97·1%).
Among those aged 60 years and older, cancer mortality in the early phase of follow up was higher than among reference group subjects (aHR 4·3, 95%CI 3·0-6·3). Yielding attributable mortality of cancer deaths of 83·6% (95%CI 76·1-88·8%) (increased numbers of lung, bladder, pancreatic liver and colon cancers) among SARS-CoV-2 cases. Mid- and long-term cancer mortality was also higher in the SARS-CoV-2 cases than in the reference group in the older age catergory (aHR 1·5, 95%CI 1·2-1·9), with the attributable mortality fraction of cancer death of 47·3% (95%CI 34·9-57·1%) (increased risk of colon, pancreatic, and of ovarian cancers).
Deaths due to respiratory diseases
The overall (age-standardized) SARS-CoV-2 infection attributable mortality fraction of deaths due to respiratory disease was 82·3% (95%CI 78·8-86·4%).
During the early period, mortality related to respiratory conditions did not differ between SARS-CoV-2 and reference groups for those under 60 years old, but was significantly higher among COVID-19 cases than in the reference group in the older age category (aHR 29·2, 95%CI 12·5-68·3), with SARS-CoV-2 infection attributable fraction of 96·8% (95%CI 93·0-98·8%) in relation to significantly more deaths from pneumonias and chronic obstructive pulmonary disease among older SARS-CoV-2 cases. Mortality due to respiratory diseases in the older age group was also higher among SARS-CoV-2 cases than reference group subjects in the mid- and long-phase of follow-up (aHR 1·9, 95%CI 1·2-3·0) (AM% 44·0%, 95%CI 3·1-66·6%).
Other causes of death
For other causes of death, the risk of death did not differ between reference group subjects and COVID-19 cases aged less than 60 years, but among those aged 60 years and older, the risk in both the early phase and mid- and long-phase of follow-up was higher than that in reference group (aHR 5·0, 95%CI 3·4-7·6, and aHR 1·8, 95%CI 1·4-2·2, accordingly). During the early period SARS-CoV-2 infection cases had 81% (95%CI 72·5-88·1%) excess other deaths of (driven by non-insulin-dependent diabetes mellitus, other disorders of urinary system (ICD-10 N39), and Alzheimer's disease deaths). In the mid-to long-term period, in the SARS-CoV-2 group the excess of other deaths was 45·5% (95%CI 31·7-56·3) (related to non-insulin-dependent diabetes mellitus, and septicaemia). For both age groups, the risk of death from other causes increased with increasing age.
Discussion
There is a sizeable body of evidence on short-term sequelae of COVID-19 including mortality,16,17 but it is unclear whether COVID-19 is associated with increased long-term mortality.
In Estonia, over the first two years of the COVID-19 epidemic, the population level excess mortality has been relatively modest, with the decrease in life expectancy below the average of developed countries.18,19
In this study, we show that those who had SARS-CoV-2 infection have more than three times the risk of dying over the following year compared with those who remain uninfected. To the best of our knowledge, this is the first study investigating the risk of dying over a year after the initial episode of SARS-CoV-2 infection and comparing mortality to that among uninfected individuals in a population-based setting. In addition to showing differences in risk of death for SARS-CoV-2 cases and reference group subjects, we were also able to explore the causes of death.
Post-COVID-19 one-year all-cause mortality
In our study, 8% of SARS-CoV-2 infected people required hospitalisation, and close to two thirds of deaths during the year after the positive SARS-CoV-2 test occurred in this subgroup of SARS-CoV-2 cases. Mortality among SARS-CoV-2 cases varied substantially over time. The short-term mortality (up to 5 weeks post index date) was significantly higher in the SARS-CoV-2 group than in the reference group (1623 vs 118 per 10 000 respectively). However, an increased mortality persisted after the acute SARS-CoV-2 infection period until the end of the first year among SARS-CoV-2 cases aged 60 or older. For those under 60 years old, SARS-CoV-2 cases, the mortality over the mid- and long-term follow up periods was similar to that in the reference group.
Acute SARS-CoV-2 infection period mortality
In the COVID-19 group, 35.1% of deaths were caused by COVID-19. But in addition to this, individuals with SARS-CoV-2 were at higher risk of cancer death over the 5 weeks after having positive SARS-CoV-2 test. This, higher risk of cancer death affected all SARS-CoV-2 infected individual irrespective of age. Having a cancer (hepatic, colon, breast, bladder kidney, brain, stomach, pancreatic cancers and leukaemia in our data) combined with higher healthcare utilization suggest that these individuals might have underlying malignancy/active cancer care and/or more advance stage cancers. This finding is in close agreement with evidence on higher death rate among SARS-CoV-2 infected cancer patients compared to non-cancer COVID-19 patients from other studies.20 In the older age group of SARS-CoV-2 cases, there was a higher risk of death from cardiovascular diseases, respiratory diseases and due to other causes during the early follow-up period. This is in agreement with other studies assessing acute SARS-CoV-2 infection related mortality.21,22
Post-acute SARS-CoV-2 infection period cause-specific mortality
Importantly, as per our results, increased mortality among those infected with SARS-CoV-2 extends beyond early (acute COVID) period. We observed an excess of cardiovascular, cancer, respiratory and other diseases related mortality extending over a year among the older SARS-CoV-2 cases. We believe this to be a significant finding. After the acute disease period, the older SARS-CoV-2 cases were at increased risk for respiratory diseases, malignant neoplasms, and cardiovascular deaths.
Increasing age has repeatedly been reported to unfavourably affecting COVID-19 outcomes.23 Our findings also indicate an independent effect of age on COVID-19 mortality. Observation of higher mortality after acute SARS-CoV-2 infection, across several cause-of-death categories suggests that in old age the increased risk of death is dominated by ageing processes that eventually raise the vulnerability of almost all individuals to multiple pathologies.24 Since influenza and COVID-19 have similar risk factors and modes of transmission leading to severe respiratory illness, there is significant interest in comparing both epidemics. Seasonal all-cause excess mortality for influenza A and B, especially among elderly has been reported.25,26 While several studies have documented long term (persisting for over a year) lung disability and psychological impairment among hospital treated influenza patients, data on long-term mortality after influenza are scars.27,28
Via an array of potential mechanisms,29 acute SARS-CoV-2 infection can lead to new clinical sequelae (new diseases, conditions) or exacerbate/lead to more serious course of pre-existing (chronic) conditions that the individual had prior SARS-CoV-2 infection.5,30 Sato et al., have proposed that the SARS-CoV-2 infection can trigger acute and chronic cardiovascular disease.31 The mechanisms that account for raised cardiovascular risk in the COVID-19 acute phase have been explored,32,33 long-term cardiac complications associated with COVID-19 are incompletely characterised.34 The lungs are the primary target of SARS-CoV-2 infection. While data characterizing long terms effects of COVID-19 on lungs is still limited, there is evidence on chronic lung fibrosis and possibly chronic pulmonary hypertension being sequelae of the SARS-CoV-2 infection.35 Saini and Aneja36 have speculated that long COVID-19 may predispose recovered patients to cancer development and accelerate cancer progression (based on growing evidence of the ability of SARS-CoV-2 to modulate oncogenic pathways, promote chronic low-grade inflammation, and cause tissue damage).
SARS-CoV-2 infected individuals may be at higher risk of mortality through biological effects in combination with other determinants, such as belonging to racial/ethnic minority groups, low socioeconomic status, and limited health care access. COVID-19 health disparities, especially in terms of morbidity and mortality warrant further research also in Estonia.
Strengths and limitations
Our findings should be put into the context of the study's limitations. We used routinely collected data, which limits the set of variables available for analysis. We were not able to control for some potential confounders (i.e. health behaviour and socio-economic status). This is a weakness of our analysis. However, we were able to control for most significant known confounding factors such as age, sex and comorbidity. The mortality patterns we observed persisted even after adjustment for comorbidities. This suggests that the excess mortality observed during the acute period and beyond is related to SARS-CoV-2 infection. We are aware of the potential misclassification of reference group (due to people having undiagnosed SARS-CoV-2 infection) which could lead to an underestimation of the true effect of death risk factors (producing more conservative estimates). However, this misclassification is probably limited (owing to the very low prevalence of undiagnosed SARS-CoV-2 infection in the population). Finally, we did not account for the potential effect of COVID-19 vaccination which started in January 2021 in Estonia. At the time of data collection for this study, only incomplete data on COVID-19 vaccination status of study subjects was available (∼ 60% of those vaccinated). However, based on this incomplete data, the proportion of those vaccinated was equal among cases and reference group (data not shown; data from HIF).
A major strength of this study is the large, nation-wide non-selected population (including all people who tested SARS-CoV-2 positive across all age groups). The results of sensitivity analysis run (yielding very similar SMR for the reference group and 2019 general population mortality) increase our confidence in the validity of the reference group used in this analysis. Previously published studies have been conducted mainly on hospitalised COVID-19 patients, have not compared them with reference group subjects, and have used short follow-up periods. Our study, benefited from substantial sample size and long follow-up to address the questions it posed.
Conclusions
This nationally representative cohort study indicates that the increased mortality from SARS-CoV-2 infection is not limited to the initial infection episode. We found that having SARS-CoV-2 carries with it a substantially increased mortality in the following 12 months, driven by deaths in older people (60+ years). The observed increased mortality among older individuals following SARS-CoV-2 infection calls for multi-disciplinary and targeted interventions to prevent such deaths. Our data provides an important contribution to the evidence on individual and population-based effects of SARS-CoV-2.
Contributors
AU: Conceptualization, Methodology, Funding acquisition, Writing original draft; TJ Data curation, Formal analysis, Visualization; HP Data curation, Formal analysis; RK Visualization, Writing - Review and Editing; TM, AT, KS, RK, and MP Investigation, Writing - Review and Editing; KF Conceptualization, Methodology, Writing - Review and Editing. All authors discussed the results and approved the final version.
Data availability
The data that support the findings of this study are available on request from the corresponding author, [AU]. The data are not publicly available due to restrictions.
Declaration of interests
The authors report no conflicts of interest.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2022.100394.
Appendix. Supplementary materials
References
- 1.Aburto JM, Schöley J, Kashnitsky I, et al. Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: a population-level study of 29 countries. Int J Epidemiol. 2022;51:63–74. doi: 10.1093/ije/dyab207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Donnelly JP, Wang XQ, Iwashyna TJ, et al. Readmission and Death After Initial Hospital Discharge Among Patients With COVID-19 in a Large Multihospital System. JAMA. 2021;325:304–306. doi: 10.1001/jama.2020.21465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williamson E, Walker AJ, Bhaskaran KJ, et al. OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594:259–264. doi: 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]
- 5.Ayoubkhani D, Khunti K, Nafilyan V, et al. Post-Covid syndrome in individuals admitted to hospital with Covid-19: retrospective cohort study. BMJ. 2021;372:n693. doi: 10.1136/bmj.n693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Estonian Health Insurance Fund. Health statistics. https://statistika.haigekassa.ee/PXWeb/pxweb/et/kindlustatu/kindlustatu__Kindlustus/KN05.px/table/tableViewLayout2/?rxid=670aaa19-7a8d-4b6d-801d-6861fd3b5fca. Accessed 18 March 2022
- 7.Borgan O, Samuelsen S. A review of cohort sampling designs. Norsk Epidemiologi. 2003;13:239–248. [Google Scholar]
- 8.Richardson DB. An incidence density sampling program for nested case-control analyses. Occup Environ Med. 2004;61:e59. doi: 10.1136/oem.2004.014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO 2021. COVID-19 Clinical management: living guidance, 25 January 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2. Accessed 19 March 2022
- 10.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 11.WHO 1979. Medical certification of cause of death: instructions for physicians on use of international form of medical certificate of cause of death, 4th ed. https://apps.who.int/iris/handle/10665/40557. Accessed 18 February 2021.
- 12.Kjærgaard S, Canudas-Romo V, Vaupel JW. The importance of the reference population for coherent mortality forecasting models. (2015) https://epc2016.princeton.edu/papers/160625. Accessed 18 March 2021
- 13.Statistics Estonia. https://andmed.stat.ee/en/stat. Accessed 18 November 2021
- 14.Bonanad C, García-Blas S, Tarazona-Santabalbina F, et al. The Effect of Age on Mortality in Patients With COVID-19: A Meta-Analysis With 611,583 Subjects. J Am Med Dir Assoc. 2020;21:915–918. doi: 10.1016/j.jamda.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.von Cube M, Timsit JF, Schumacher M, et al. Quantification and interpretation of attributable mortality in core clinical infectious disease journals. Lancet Infect Dis. 2020;20:e299–e306. doi: 10.1016/S1473-3099(20)30485-0. [DOI] [PubMed] [Google Scholar]
- 16.Groff D, Sun A, Ssentongo AE, et al. Short-term and Long-term Rates of Postacute Sequelae of SARS-CoV-2 Infection: A Systematic Review. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.28568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Günster C, Busse R, Spoden M, et al. 6-month mortality and readmissions of hospitalized COVID-19 patients: A nationwide cohort study of 8,679 patients in Germany. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Islam N, Jdanov DA, Shkolnikov VM, Khunti K, Kawachi I, White M, et al. Effects of covid-19 pandemic on life expectancy and premature mortality in 2020: time series analysis in 37 countries. BMJ. 2021;375 doi: 10.1136/bmj-2021-066768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.COVID-19 Excess Mortality Collaborators Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022 doi: 10.1016/S0140-6736(21)02796-3. S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bertuzzi AF, Ciccarelli M, Marrari A., et al. Impact of active cancer on COVID-19 survival: a matched-analysis on 557 consecutive patients at an Academic Hospital in Lombardy, Italy. Br J Cancer. 2021;125:358–365. doi: 10.1038/s41416-021-01396-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahmoud M, Carmisciano L, Tagliafico L, et al. Patterns of Comorbidity and In-Hospital Mortality in Older Patients With COVID-19 Infection. Front Med (Lausanne) 2021;8 doi: 10.3389/fmed.2021.726837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elezkurtaj S, Greuel S, Ihlow J, et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci Rep. 2021;11:4263. doi: 10.1038/s41598-021-82862-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tiruneh SA, Tesema ZT, Azanaw MM, et al. The effect of age on the incidence of COVID-19 complications: a systematic review and meta-analysis. Syst Rev. 2021;10:80. doi: 10.1186/s13643-021-01636-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horiuchi S, Finch CE, Meslé F, et al. Differential patterns of age-related mortality increase in middle age and old age. J Gerontol A Biol Sci Med Sci. 2003;58:495–507. doi: 10.1093/gerona/58.6.b495. [DOI] [PubMed] [Google Scholar]
- 25.Nielsen J, Vestergaard LS, Richter L, et al. European all-cause excess and influenza-attributable mortality in the 2017/18 season: should the burden of influenza B be reconsidered? Clin Microbiol Infect. 2019;25:1266–1276. doi: 10.1016/j.cmi.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Vestergaard LS, Nielsen J, Krause TG, et al. Excess all-cause and influenza-attributable mortality in Europe, December 2016 to February 2017. Euro Surveill. 2017;22:30506. doi: 10.2807/1560-7917.ES.2017.22.14.30506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luyt CE, Combes A, Becquemin MH, et al. Long-term outcomes of pandemic 2009 influenza A(H1N1)-associated severe ARDS. Chest. 2012;142:583–592. doi: 10.1378/chest.11-2196. [DOI] [PubMed] [Google Scholar]
- 28.Chen J, Wu J, Hao S, et al. Long term outcomes in survivors of epidemic Influenza A (H7N9) virus infection. Sci Rep. 2017;7:17275. doi: 10.1038/s41598-017-17497-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Proal AD, VanElzakker MB. Long COVID or Post-acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms. Front Microbiol. 2021;12 doi: 10.3389/fmicb.2021.698169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sato K, Sinclair JE, Sadeghirad H, et al. Cardiovascular disease in SARS-CoV-2 infection. Clin Transl Immunology. 2021;10:e1343. doi: 10.1002/cti2.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nishiga M, Wang DW, Han Y, et al. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17:543–558. doi: 10.1038/s41569-020-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gu SX, Tyagi T, Jain K, et al. Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat Rev Cardiol. 2021;18:194–209. doi: 10.1038/s41569-020-00469-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Satterfield BA, Bhatt DL, Gersh BJ. Cardiac involvement in the long-term implications of COVID-19. Nat Rev Cardiol. 2021 doi: 10.1038/s41569-021-00631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Halawa S, Pullamsetti SS, Bangham CRM, et al. Potential long-term effects of SARS-CoV-2 infection on the pulmonary vasculature: a global perspective. Nat Rev Cardiol. 2021 doi: 10.1038/s41569-021-00640-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saini G, Aneja R. Cancer as a prospective sequela of long COVID-19. Bioessays. 2021;43 doi: 10.1002/bies.202000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, [AU]. The data are not publicly available due to restrictions.