Abstract
Introduction
Gastrointestinal stromal tumor (GIST) is a term to describe the distant spread (metastasis) of primary tumors to the peritoneal cavity.
Case presentation
A 48-year-old woman complained of dilated stomach, stomachache, and nausea. Laboratory findings showed an increase in the tumor marker, CA-125147 U/mL and also LDH 350 U/L while quantitative total β HCG and CEA were normal. Ultrasonography showed dominantly a huge solid mass with the cystic component in pelvic cavity extended to the abdominal cavity, with vascularized on Doppler ultrasound, difficult to identify uterine or adnexa origin. Afterward, an abdominal CT scan with and without contrast was performed and showed a solid mass with cystic and necrotic component impression originating from GI tract with feeding branch of an artery mesenteric, attached to the mesenteric small bowel and peritoneal carcinomatosis. Core biopsy and immunohistochemical were also performed with the result suggesting GIST.
Discussion
The diagnosis of GIST was established based on laboratory findings, abdominal ultrasound, abdominal CT-scan, and confirmation of GIST.
Conclusion
The diagnosis of GIST can be distinguished from gynecological mass despite their similarities.
Keywords: Computed tomography, Histopathology, Microbiology, Peritoneal carcinomatosis
Highlights
-
•
A Gastrointestinal stromal tumor (GIST) can be distinguished from gynecological carcinoma using ROMA criteria.
-
•
The accuracy of carcinoma diagnosis can be confirmed by post-analysis of pathology anatomy.
-
•
ROMA Algorithm helps in differentiating tumors in the abdominal.
1. Introduction
Gastrointestinal stromal tumors (GIST) are the most common malignant subepithelial lesions of the gastrointestinal tract [1] and estimated 4500–6000 cases annually in the United States [2]. GIST to be 14.5 per million in south-west Sweden, 11 per million in Iceland, and 12.7 per million in the Netherlands [3], [4]. GIST is a rare tumor that can appear anywhere in the gastrointestinal tract. These tumors sometimes present as pelvic masses leading to misdiagnosis as gynecological masses. Confirmation from imaging and immunohistochemical plays a role in accurate preoperative diagnosis [5], [6]. We reported a case of a 48-year-old woman with GIST after being diagnosed with gynecological mass from immunohistochemical. We reported based on the surgical case report (SCARE) 2020 guideline [7].
2. Case presentation
A 48-year-old woman was referred to the Obstetrics and Gynecology Department with a chief complaint of dilated stomach, stomachache, and nausea. Menstrual history was normal. There was no history of malignancy in the family. On physical examination, a hard and stubby mass was found. Laboratory findings showed an increase in the tumor marker, CA-125147 U/mL (normal ≤35 U/mL post-menopausal, <90 U/mL in premenopausal woman) and also LDH 350 U/L (normal 120–250 U/L) while quantitative total β HCG and CEA were normal. She was diagnosed primarily as an ovarian malignancy due to the appearance of a large mass accompanied by ascites and increased CA-125 levels.
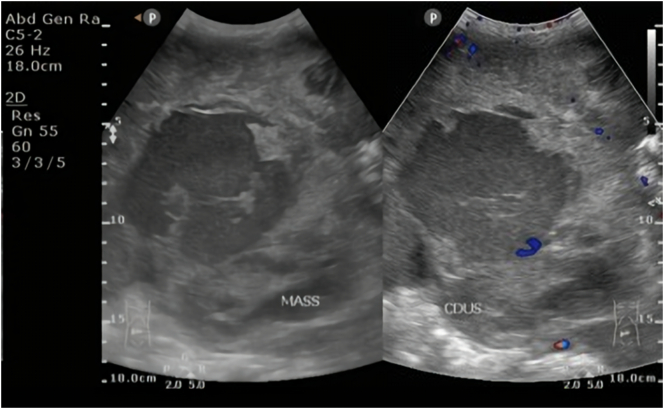
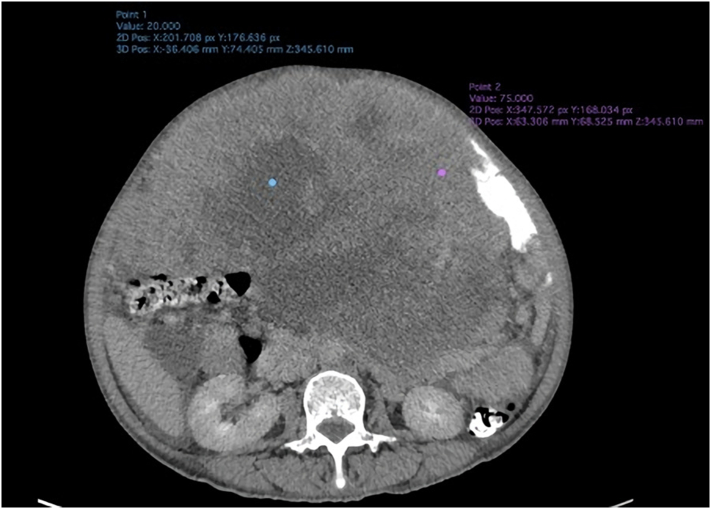
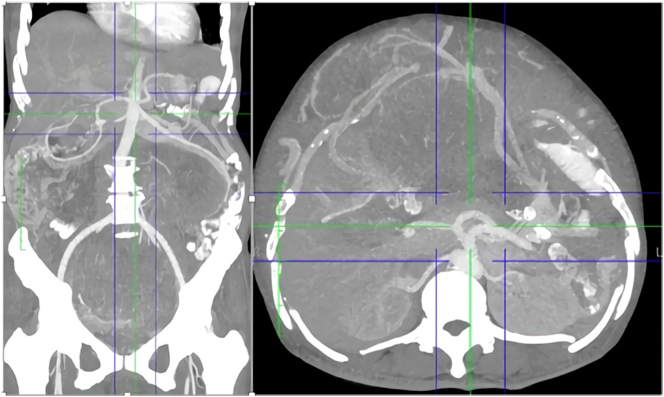
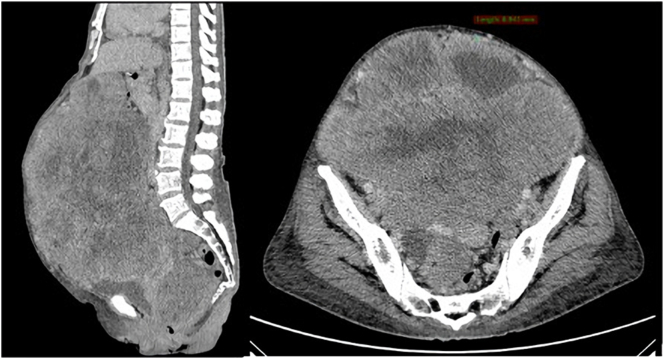
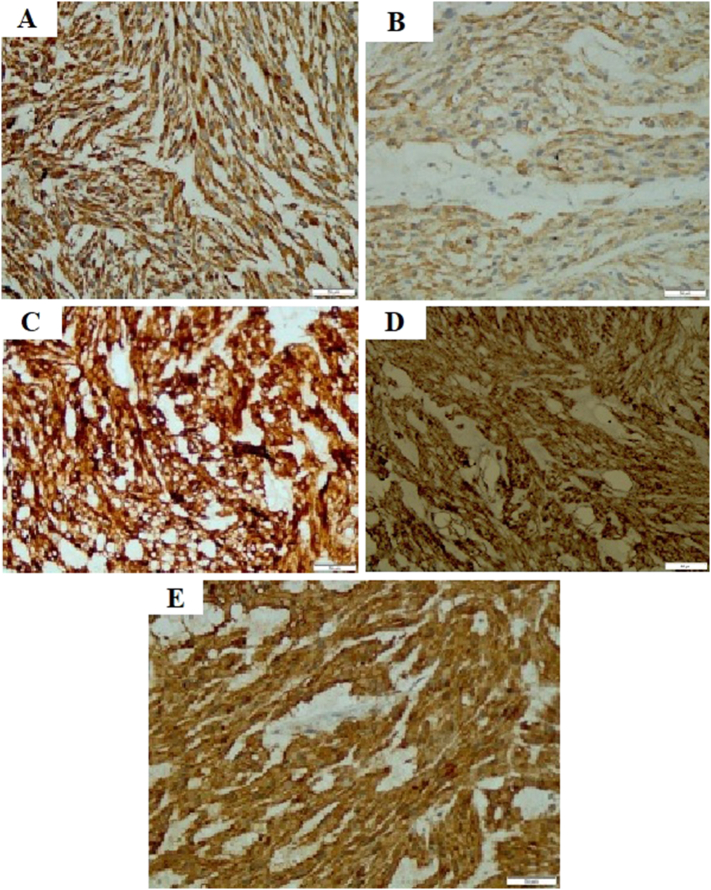
Ultrasonography showed dominantly a huge solid mass with the cystic component in pelvic cavity extended to the abdominal cavity, with vascularized on Doppler ultrasound, difficult to identify uterine or adnexa origin (Fig. 1). Afterward, an abdominal CT scan with and without contrast was performed and showed a solid mass with cystic and necrotic component impression originating from GI tract (Fig. 2) with feeding branch of an artery mesenteric (Fig. 3), attached to the mesenteric small bowel and peritoneal carcinomatosis (Fig. 4). Core biopsy and immunohistochemical were also performed with the result suggesting GIST (Fig. 5).
Fig. 1.
Abdominal ultrasound shows a huge solid mass with the cystic component at pelvic cavity extended to the abdominal cavity, confirmatory from color doppler that vascularized intralesional.
Fig. 2.
Axial CT (venous phase) shows a huge solid mass with cystic and necrotic components almost fulfilling pelvic cavity extended to abdominal cavity impressed origin from the gastrointestinal tract.
Fig. 3.
Axial and coronal CT scan demonstrates that mass get feeding on the branch of the mesenteric artery and dominantly attached to small bowel mesentery.
Fig. 4.
Coronal view demonstrates this huge mass attached to the bladder with irregularity of bladder wall and ill-defined border to rectum and rectosigmoid. Axial view shows peritoneal carcinomatosis which is peritoneal thickening, lymphadenopathy, mesenteric nodule (blue head arrow), and ascites (black arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Fig. 5.
Immunohistochemistry examination received from core biopsy at target solid lesion shows conformity of the gastrointestinal stromal tumor (GIST).
3. Discussion
Gastrointestinal stromal tumors are rare tumors and may present a diagnostic dilemma in women with abdominopelvic mass [3], [8]. GIST is typically present in adults over 40 years (median ages 55–60 years) and only exceptional cases are found in children. The clinical sign and symptoms are the presence of mass or bleeding. These tumors occasionally present a pelvic mass and lead to misdiagnosis of gynecologic abnormality. The age and clinical presentation of this case report were consistent with another report that mimicked the symptom of ovarian mass [8], [9], [10].
The preferred imaging modality is enhanced computed tomography. The predominant pattern is heterogeneously enhancing exophytic mass. Distal small bowel tumors and those arising from the sigmoid colon and rectum may be erroneously identified as gynecologic cancer. The detection of immunohistochemistry CD 117 and DOG-1 are positive markers of GIST with high sensitivity (94.4%) [9], [10], [11], [12]. GIST of the small bowel and recto-sigmoid region presents as a heterogeneous complex pelvic tumor. The clinical and imaging features mimic the ovarian mass due to the absence of specific symptoms and/or imaging characters of GIST. In addition, to distinguish between GITS and gynecological mass, the ROMA criteria and ROMA Algorisms can be used, which if these criteria are not met then GITS can be enforced [13], [14].
4. Conclusion
We report the case of a 48-year-old female with clinical and laboratory signs of gynecological mass. An ultrasound cannot give information about the origin of the mass, as the huge mass almost fulfills the pelvic cavity to the abdominal cavity. A CT scan remains an imaging modality that demonstrates solid mass with necrotic and cystic impression originating from the GI tract and feeding by the branch of the mesenteric artery. GIST should be considered as the differential diagnosis of the patient presented with abdominal or pelvic mass or pelvic pain in the Gynecology oncology department, with the unmatched symptoms and laboratory result to the gynecology disease, the possibility of disease other than gynecologic disease has to be considered.
Sources of funding
Nothing.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Not applicable.
Author contribution
All authors contributed toward data analysis, drafting and revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Registration of research studies
Not applicable.
Guarantor
Muhammad Hidayat Surya Atmaja is the person in charge of the publication of our manuscript.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
Devy Yuspita Rahma and Muhammad Hidayat Surya Atmaja declare that they have no conflict of interest.
Acknowledgment
We thank our editor “Fis Citra Ariyanto”.
References
- 1.Akahoshi K., Oya M., Koga T., Shiratsuchi Y. Current clinical management of gastrointestinal stromal tumor. World J. Gastroenterol. 2018;24(26):2806–2817. doi: 10.3748/wjg.v24.i26.2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel N., Benipal B. Incidence of gastrointestinal stromal tumors in the United States from 2001–2015: a United States cancer statistics analysis of 50 states. Cureus. 2019;11(2) doi: 10.7759/cureus.4120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joensuu H. Gastrointestinal stromal tumor (GIST) Ann. Oncol. 2006;17(Suppl. 10) doi: 10.1093/annonc/mdl274. x280-6. [DOI] [PubMed] [Google Scholar]
- 4.Parab T.M., DeRogatis M.J., Boaz A.M., Grasso S.A., Issack P.S., Duarte D.A., et al. Gastrointestinal stromal tumors: a comprehensive review. J. Gastrointest. Oncol. 2019;10(1):144–154. doi: 10.21037/jgo.2018.08.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinto V., Ingravallo G., Cicinelli E., Pintucci A., Sambati G.S., Marinaccio M., et al. Gastrointestinal stromal tumors mimicking gynecological masses on ultrasound: a report of two cases. Ultrasound Obstet. Gynecol. 2007;30(3):359–361. doi: 10.1002/uog.4097. [DOI] [PubMed] [Google Scholar]
- 6.Yayci E., Guler O.T., Kuzey G.M., Comuoglu C., Atacag T., Cetin A., et al. Gastrointestinal stromal tumor mimicking gynecological mass: a case report. Gynecol. Oncol. Case. Rep. 2012;2(3):107–109. doi: 10.1016/j.gynor.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 8.Joensuu H., Hohenberger P., Corless C.L. Gastrointestinal stromal tumour. Lancet (London, England) 2013;382(9896):973–983. doi: 10.1016/s0140-6736(13)60106-3. [DOI] [PubMed] [Google Scholar]
- 9.Ijeri S.K., Rathod P.S., Kundargi R., Pallavi V.R., Shobha K., Shankaranand Gastrointestinal stromal tumor mimicking as ovarian tumor in gynaecologic oncology. Indian J. Surg. Oncol. 2016;7(1):56–61. doi: 10.1007/s13193-015-0479-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y.Y., Peng F.S., Lin H.H., Hsiao S.M. Gastrointestinal stromal tumor mimicking ovarian malignancy in a woman with type I neurofibromatosis. Taiwan. J. Obstet. Gynecol. 2015;54(3):330–331. doi: 10.1016/j.tjog.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Kim K.M., Kang D.W., Moon W.S., Park J.B., Park C.K., Sohn J.H., et al. Gastrointestinal stromal tumors in koreans: it's incidence and the clinical, pathologic and immunohistochemical findings. J. Korean Med. Sci. 2005;20(6):977–984. doi: 10.3346/jkms.2005.20.6.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tirumani S.H., Baheti A.D., Tirumani H., O'Neill A., Jagannathan J.P. Update on gastrointestinal stromal tumors for radiologists. Korean J. Radiol. 2017;18(1):84–93. doi: 10.3348/kjr.2017.18.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montagnana M., Danese E., Ruzzenente O., Bresciani V., Nuzzo T., Gelati M., et al. The ROMA (Risk of ovarian malignancy Algorithm) for estimating the risk of epithelial ovarian cancer in women presenting with pelvic mass: is it really useful? Clin. Chem. Lab. Med. 2011;49(3):521–525. doi: 10.1515/cclm.2011.075. [DOI] [PubMed] [Google Scholar]
- 14.Chudecka-Głaz A.M. ROMA, an algorithm for ovarian cancer. Clin. Chim. Acta. 2015;440:143–151. doi: 10.1016/j.cca.2014.11.015. [DOI] [PubMed] [Google Scholar]