Abstract
Objective
Frailty is a common geriatric syndrome defined as multiple deficits, impairing the capacity to figure out insult. Previous studies have reported a significant association between frailty and mortality in stroke patients. This study aimed to explore the association between frailty and mortality among older Chinese stroke patients.
Methods
This study was a secondary analysis of a multicenter prospective cohort study conducted in older Chinese inpatients from October 2018 to February 2020, and patients with a primary diagnosis of stroke including hemorrhage and ischemia, were included in our study. Frailty of older inpatients with stroke from six hospitals was measured by the FRAIL scale, and a one-year follow-up was performed by well-trained nurses of these hospitals via telephone. Multivariable logistic regression was used to detect the association between frailty and one-year mortality.
Results
A total of 530 stroke patients with an average age of 72.94 (SD = 5.79) years were included in the present study. There were 37 (7.0%) hemorrhagic strokes and 493 (93.0%) ischemic strokes, with 228 (43.0%) females in this population. The prevalence of frailty was 22.5%. In the logistic regression model with adjustment for age, sex, instrumental activities of daily living (IADL), basic activities of daily living (ADL), education, history of falls, BMI, smoking, alcohol consumption, low handgrip strength, type of stroke and polypharmacy, stroke patients with frailty had an increased risk of one-year mortality compared to those without frailty (OR = 3.38, 95% CI: 1.22–9.37, P = 0.019).
Conclusion
Our study indicated that frailty was an independent risk factor for one-year all-cause mortality among older stroke patients in China. Frailty may be an essential factor for clinicians to consider before making a comprehensive treatment, and corresponding mixed interventions, including exercise training and nutritional programs, need to be conducted among older stroke patients.
Keywords: Activities of daily living, Aged, China, Frailty, Stroke
What is known?
-
•
Several clinical factors, such as age, stroke severity, ischemic heart disease, and comorbidities, were associated with a higher risk of mortality but studies exploring prestroke characteristics and mortality are scarce.
-
•
Clinical frailty was an independent risk factor for 28-day mortality among patients with ischemic stroke.
What is new?
-
•
Frailty was an independent risk factor for one-year all-cause mortality among older stroke patients in China.
-
•
A 3.38-fold incremental risk of one-year all-cause mortality for stroke patients with frail compared with those without frail emphasizes the need for early frailty screening and comprehensive stroke prevention to improve the clinical outcomes for stroke survival.
1. Introduction
Stroke is one of the most common diseases worldwide and has become the second leading cause of death and the third leading cause of disability [1]. In a study of global disease burden in 2019, the authors reported that one in four individuals would experience a stroke during their lifetime. An estimated 9.6 million ischemic strokes and 4.1 million hemorrhagic strokes occur globally each year [2]. As societies age, the burden of stroke will become a massive challenge for the healthcare and social service system. In addition, a previous study indicated that the rate of mortality was higher among older stroke survivors [3]. Therefore, identifying and managing the risk of mortality among older patients with stroke is very important. Several clinical factors, such as age, stroke severity, ischemic heart disease, and comorbidities, are associated with a higher risk of mortality [[4], [5], [6]]. However, studies exploring prestroke characteristics and mortality are scarce.
Frailty is a common geriatric syndrome defined by decreased reserve and lower functional ability due to cumulative multisystem decline, leading to increased adverse outcomes when suffering from stressors [7,8]. Frailty has been reported to be associated with the risk of falls, fractures, disability, and even mortality among community-dwelling older adults or nursing home residents [[9], [10], [11]]. As stroke is a severe stressor, it is rational to explore the association between frailty and mortality among stroke survivors. Winovich et al. examined the risk factors associated with ischemic stroke survival and found that frailty was an independent risk factor for shorter survival [12]. Recently, several studies have investigated the association between frailty and mortality among patients with stroke [[13], [14], [15]].
In a study in 2020 [15], the authors reported that clinical frailty was an independent risk factor for 28-day mortality among patients with ischemic stroke (for a one-point increase in the Clinical Frailty Scale, OR = 1.03, 95% CI: 1.01–1.05, P < 0.01). Another study [14] from the USA focusing on 240 patients with intracerebral hemorrhage found that frailty, measured by the frailty index, was not associated with a high risk of mortality (P = 0.12). However, these studies usually had a relatively short-term follow-up, and the results were inconsistent; therefore, it is imperative to conduct studies with long-term follow-up to investigate the association between frailty and mortality. Our study aimed to examine the association between frailty, measured by the frailty scale, and all-cause mortality among Chinese patients with stroke using a one-year follow-up cohort study. We hypothesize that stroke patients with frailty have an increased risk of mortality compared to those without frailty.
2. Methods
2.1. Study design and participants
Our study was a secondary analysis derived from a large-scale cohort study on the prevalence of frailty and related factors among older Chinese inpatients from six tertiary hospitals. The original inclusion criteria were as follows: 1) older adults aged 65 years or older and 2) voluntary participation in this study and provided informed consent. Participants who were unconscious and their companions could not provide useful information about the survey were excluded. The detailed study design and sample methods were published [16], and it was registered in the Chinese Clinical Trial Registry (ChiCTR1800017682). Briefly, the designer adopted a two-stage cluster sample method with random sampling. First, we randomly selected six provinces or municipalities from each region according to China’s administrative region from October 2018 to February 2019. Then, six tertiary hospitals were confirmed by using the same random sampling from those regions. A total of 633 stroke patients were enrolled in the baseline survey. The stroke diagnosis was based on the guidelines for Diagnosis and Treatment of Stroke in China 2014 with history, physical examination, and computed tomography (CT) scans. The inclusion criteria were 1) abrupt onset of focal neurologic deficits with clinical symptoms; 2) head CT scans showing hemorrhage or early signs of infarction. The causes of stroke included ischemic stroke, transient ischemic attack, intracerebral hemorrhage, and subarachnoid hemorrhage in our study. We combined ischemic stroke and transient ischemic attack as ischemic stroke; intracerebral hemorrhage and subarachnoid hemorrhage were considered hemorrhagic stroke. The patients were followed up by well-trained nurses via telephone, and 103 patients were lost to follow-up one year after the beginning of enrollment.
2.2. Frailty assessment
Well-trained registered nurses from six selected hospital wards evaluated frailty of the stoke patients with the FRAIL scale within 48 h after hospital admission. The FRAIL scale examined five aspects of patients (illness, loss of weight, fatigue, resistance, and ambulation). The total score ranged from 0 to 5, classifying frailty (3–5), prefrail (1–2), and robust (0). This FRAIL scale has been validated in older Chinese adults [17]. In our study, prefrailty and robustness were considered non-frailty, and those with 3 points and more indicated frailty.
2.3. Study outcomes
The nurses contacted the patients via telephone for follow-up one year after enrollment, from October 2019 to February 2020. Data about one-year all-cause mortality was collected.
2.4. Covariates
Nurses collected data on demographic characteristics, including age, sex, level of education (illiterate, primary school, middle school, and university), and lifestyle factors (smoking, alcohol consumption), via a questionnaire. Investigators also used a calibrated instrument following standard procedures to measure weight, height, and handgrip strength. The handgrip strength was tested for the dominant hand, and the maximum value was recorded during two measurements. Low handgrip strength was defined by a cutoff value of <28 kg for males or <18 kg for females [18]. Additionally, we collected the number of medications at hospital admission and defined polypharmacy as patients who took five or more drugs daily [19]. History of falls and nutritional status were assessed. Nutritional status was evaluated by the Mini-Nutritional Assessment-Short Form and classified into three groups (12–14 indicating normal nutritional status; 8–11 indicating at risk of malnutrition; 0–7 indicating malnourished) [20]. Basic activities of daily living (ADL) and instrumental activities of daily living (IADL) were assessed for the functional ability of patients [21,22]. All covariates were collected within 48 h after hospital admission.
2.5. Statistical analysis
Descriptive data analysis was used to display continuous variables with Mean ± SD and categorical variables with frequency (%). Chi-square test and Student’s t-test were used to compare the difference between two groups (frail versus nonfrail; survivors versus deceased). In addition, we used multivariate logistic regression to identify the independent effect of frailty on one-year mortality of older stroke patients. Finally, we performed stratified analysis based on age group, sex, polypharmacy, low handgrip strength and diagnosis. We used SAS (version 9.4) for all the statistical analyses. A two-sided P-value of <0.05 was considered to indicate a statistically significant difference.
3. Results
3.1. Baseline characteristics of all participants
A total of 37 (7.0%) hemorrhagic strokes and 493 (93.0%) ischemic strokes were included in our study. The patients’ average age was 72.94 (SD = 5.79) years, with 228 (43.0%) females and 302 (57.0%) males. Among the total patients, the one-year all-cause mortality rate was 5.1%, with 119 (22.5%) categorized as frail and 411 (77.5%) as nonfrail. Baseline characteristics of all participants are shown in Table 1.
Table 1.
Baseline characteristics of 530 older patients with stroke.
| Variables | Mean ± SD/n (%) |
|---|---|
| Age (years) | 72.94 ± 5.79 |
| 65–74 | 358 (67.5) |
| >74 | 172 (32.4) |
| Sex | |
| Female | 228 (43.0) |
| Male | 302 (57.0) |
| Education | |
| Illiterate | 120 (22.6) |
| Primary school | 152 (28.7) |
| Middle school | 194 (36.6) |
| University | 64 (12.1) |
| Drinking | |
| Never | 388 (73.2) |
| Current | 89 (16.8) |
| Quit | 53 (10.0) |
| Smoking | |
| Never smoking | 333 (62.8) |
| Current smoking | 95 (17.9) |
| Former smoker | 102 (19.2) |
| ADL independence score | 77.84 ± 26.19 |
| BMI (kg/m2) | 23.96 ± 3.27 |
| IADL independence score | 5.99 ± 2.51 |
| Diagnose | |
| Hemorrhagic stroke | 37 (7.0) |
| Ischemic stroke | 493 (93.0) |
| Frailty | |
| No | 411 (77.5) |
| Yes | 119 (22.5) |
| History of falls | |
| No | 400 (75.5) |
| Yes | 130 (24.5) |
| Polypharmacy | |
| No | 312 (58.9) |
| Yes | 218 (41.1) |
| Low handgrip strength | |
| Yes | 366 (69.0) |
| No | 164 (31.0) |
| MNA-SF | |
| Normal | 260 (49.0) |
| At risk of malnutrition | 221 (41.8) |
| Malnutrition | 49 (9.2) |
| One-year mortality | |
| No | 503 (94.9) |
| Yes | 27 (5.1) |
Note: ADL = basic activities of daily living. IADL = instrumental activities of daily living. MNA-SF = Mini-Nutritional Assessment-Short Form.
3.2. Baseline characteristics of frail and nonfrail patients
The average ages and gender of frail and nonfrail patients were similar, see Table 2. Stroke patients with frail had lower average ADL and IADL scores, and a higher rate of one-year all-cause mortality than nonfrail patients (all P < 0.05). There was no significant difference between frail and nonfrail patients in terms of BMI, education, diagnosis, smoking, drinking, or history of falls and polypharmacy, as shown in Table 2.
Table 2.
Comparison of baseline characteristics between stroke patients with and without frailty.
| Characteristics | Frail |
t/χ2 | P | |
|---|---|---|---|---|
| No (n = 411) | Yes (n = 119) | |||
| Age (years) | 72.73 ± 5.67 | 73.69 ± 6.14 | −1.607 | 0.109 |
| Sex | 0.062 | 0.802 | ||
| Female | 178 (43.3) | 50 (42.0) | ||
| Male | 233 (56.7) | 69 (58.0) | ||
| Age | 2.693 | 0.101 | ||
| 65–74 | 285 (69.3) | 73 (61.3) | ||
| >74 | 126 (30.7) | 46 (38.7) | ||
| Education | 17.888 | <0.001 | ||
| Illiterate | 80 (19.5) | 40 (33.6) | ||
| Primary school | 114 (27.7) | 38 (31.9) | ||
| Middle school | 168 (40.9) | 26 (21.9) | ||
| University | 49 (11.9) | 15 (12.6) | ||
| Drinking | 0.109 | 0.110 | ||
| Never | 301 (73.2) | 87 (73.1) | ||
| Current | 74 (18.0) | 15 (12.6) | ||
| Quit | 36 (8.8) | 17 (14.3) | ||
| Smoking | 0.944 | 0.624 | ||
| Never smoking | 257 (62.6) | 76 (63.9) | ||
| Current smoking | 77 (18.7) | 18 (15.1) | ||
| Former smoker | 77 (18.7) | 25 (21.0) | ||
| BMI (kg/m2) | 24.09 ± 3.15 | 23.53 ± 3.64 | 1.602 | 0.110 |
| ADL independence score | 82.46 ± 23.31 | 61.89 ± 29.24 | 7.979 | <0.001 |
| IADL independence score | 6.55 ± 2.09 | 4.05 ± 2.85 | 10.536 | <0.001 |
| Diagnose | 0.478 | 0.489 | ||
| Hemorrhagic stroke | 27 (6.6) | 10 (8.4) | ||
| Ischemic stroke | 384 (93.4) | 109 (91.6) | ||
| History of falls | 0.850 | 0.356 | ||
| No | 314 (76.4) | 86 (72.3) | ||
| Yes | 97 (23.6) | 33 (27.7) | ||
| Polypharmacy | 0.049 | 0.824 | ||
| No | 243 (59.1) | 69 (58.0) | ||
| Yes | 168 (40.9) | 50 (42.0) | ||
| Low handgrip strength | 9.689 | 0.002 | ||
| Yes | 270 (65.7) | 96 (80.7) | ||
| No | 141 (34.3) | 23 (19.3) | ||
| MNA-SF | 62.334 | <0.001 | ||
| Normal | 232 (56.4) | 28 (23.5) | ||
| At risk of malnutrition | 159 (38.7) | 62 (52.1) | ||
| Malnutrition | 20 (4.9) | 29 (24.4) | ||
| One-year mortality | 6.604 | <0.001 | ||
| No | 398 (96.8) | 105 (88.2) | ||
| Yes | 13 (3.2) | 14 (11.8) | ||
Note: Data are Mean ± SD or n (%). ADL = basic activities of daily living. IADL = instrumental activities of daily living. MNA-SF = Mini-Nutritional Assessment-Short Form.
3.3. Univariate analysis
Stroke patients with frailty had a higher rate of one-year mortality than those without frailty (P<0.001). Generally, patients who died were more likely to have lower IADL and ADL scores than stroke survivors. In addition, stroke patients with malnutrition had a higher risk of one-year mortality than those with normal nutrition. The rate of one-year all-cause mortality in patients with hemorrhagic stroke was higher than that in patients with ischemic stroke. Other variables, such as education, sex, smoking, alcohol consumption, history of falls, polypharmacy, and low handgrip strength, were not different between these two groups (survivors and deceased), as shown in Table 3.
Table 3.
Comparison of baseline characteristics between stroke patients with different outcomes.
| Characteristics | Survivors (n = 503) | Deceased (n = 27) | t/χ2 | P |
|---|---|---|---|---|
| Age (years) | 72.81 ± 5.72 | 75.38 ± 6.50 | −2.251 | 0.032 |
| Sex | 0.062 | 0.806 | ||
| Female | 217 (43.1) | 11 (40.7) | ||
| Male | 286 (56.9) | 16 (59.3) | ||
| Drinking | 5.797 | 0.055 | ||
| Never | 363 (72.2) | 25 (92.6) | ||
| Current | 87 (17.3) | 2 (7.4) | ||
| Quit | 53 (10.5) | 0 (0.0) | ||
| Smoking | 3.210 | 0.201 | ||
| Never smoking | 317 (63.0) | 16 (59.3) | ||
| Current smoking | 87 (17.3) | 8 (29.6) | ||
| Former smoker | 99 (19.7) | 3 (11.1) | ||
| ADL independence score | 86.29 ± 20.50 | 77.38 ± 26.3 | 3.403 | 0.004 |
| BMI (kg/m2) | 24.03 ± 3.26 | 22.57 ± 3.22 | 2.148 | 0.028 |
| IADL independence score | 6.08 ± 2.47 | 4.26 ± 2.65 | 3.728 | <0.001 |
| Diagnose | 5.831 | 0.016 | ||
| Hemorrhagic stroke | 32 (6.4) | 5 (18.5) | ||
| Ischemic stroke | 471 (93.6) | 22 (81.5) | ||
| History of falls | 1.191 | 0.275 | ||
| No | 382 (75.9) | 18 (66.7) | ||
| Yes | 121 (24.1) | 9 (33.3) | ||
| Education | 2.275 | 0.517 | ||
| Illiterate | 112 (22.3) | 8 (29.6) | ||
| Primary school | 144 (28.6) | 8 (29.6) | ||
| Middle school | 184 (36.6) | 10 (37.0) | ||
| University | 63 (12.5) | 1 (3.7) | ||
| Polypharmacy | 2.716 | 0.099 | ||
| No | 292 (58.0) | 20 (74.1) | ||
| Yes | 211 (42.0) | 7 (25.9) | ||
| Low handgrip strength | 3.463 | 0.063 | ||
| Yes | 343 (68.2) | 23 (85.2) | ||
| No | 160 (31.8) | 4 (14.8) | ||
| MNA-SF | 10.616 | 0.005 | ||
| Normal | 255 (50.7) | 5 (18.5) | ||
| At risk of malnutrition | 203 (40.4) | 18 (66.7) | ||
| Malnutrition | 45 (8.9) | 4 (14.8) | ||
| Frailty | 14.122 | <0.001 | ||
| No | 398 (79.1) | 13 (48.1) | ||
| Yes | 105 (20.9) | 14 (51.9) |
Note: Data are Mean ± SD or n (%). ADL = basic activities of daily living. IADL = instrumental activities of daily living. MNA-SF = Mini-Nutritional Assessment-Short Form.
3.4. The association between frailty and one-year all-cause mortality
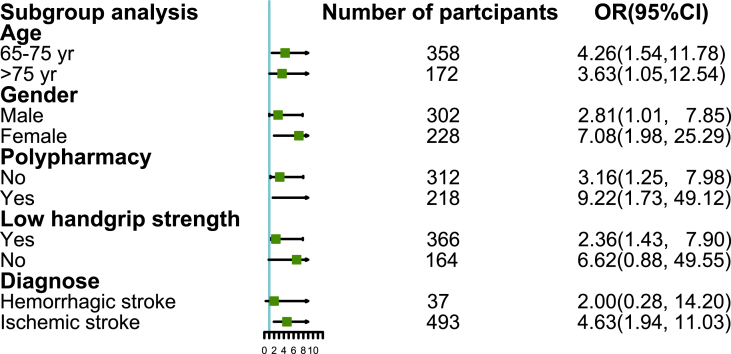
Table 4 displays three logistic regression models. In Model 1 without any adjustment for covariates, the OR of frailty for one-year all-cause mortality among stroke patients was 4.08 (95% CI: 1.86–8.95, P <0.001). Finally, after fully adjustment for variables such as age, sex, IADL, ADL, education, history of falls, BMI, smoking, alcohol consumption, low handgrip strength, polypharmacy and type of stroke, the association between frailty and one-year all-cause mortality still existed among patients with stroke, with an OR of 3.38 (95% CI: 1.22–9.37, P = 0.019). Subgroup analysis in terms of age, sex, low handgrip strength, diagnosis, and polypharmacy showed that these associations between frailty and one-year all-cause mortality were unchanged (Fig. 1).
Table 4.
Association of older stroke patients’ frailty during hospitalization with their one-year mortality in unadjusted and adjusted logistic regression analysis.
| Model | OR (95%CI) | P |
|---|---|---|
| Model 1 | 4.08 (1.86, 8.95) | <0.001 |
| Model 2 | 3.57 (1.04, 12.28) | 0.043 |
| Model 3 | 3.38 (1.22, 9.37) | 0.019 |
Note:Model 1: none adjusted. Model 2: age, sex, education adjusted. Model 3: age, sex, ADL, IADL, education, history of falls, BMI, smoking, alcohol consumption, low handgrip strength, polypharmacy, and type of stroke adjusted. ADL = basic activities of daily living. IADL = instrumental activities of daily living.
Fig. 1.
Subgroup analysis for the association between frailty and one-year all-cause mortality among stroke patients.
4. Discussion
Our study found that stroke patients with preexisting frailty defined by the FRAIL scale had an increased risk of one-year mortality compared to those without frailty. This risk was independent of confounding variables such as ADL, IADL, low handgrip strength and polypharmacy. Our study suggests that frailty can be an independent risk factor for one-year mortality, indicating that clinicians or nurses should screen frailty early and conduct corresponding interventions, including physical activity and appropriate nutritional programs for stroke patients.
4.1. Comparison with other previous studies
The prevalence of frailty among stroke patients was 22.5%, which was lower than the earlier study by Evans et al. [15] that reported the prevalence of frailty among patients with ischemic stroke was 54.04%. The main reason for this divergence may be the age, and the average age of 72.73 years in our study was younger than that in an earlier study (median age of 83 years in nonfrail patients and 87 years in frail patients). The older the patient is, the higher the risk of frailty. A previous study found that the prevalence of frailty was 12% (95% CI: 11%–14%) among the 60–69 age group but 31% (95% CI: 29%–34%) in the 80–89 age group [23]. Apart from age, other factors, such as measurement tools for frailty [24] and severity of illness, can also influence prevalence reports.
Several studies have explored the impact of frailty on mortality. In a study in 2017 including 717 individuals with incident ischemic stroke, the authors found that frailty was associated with shorter survival, which was consistent with our results [12]. Our finding extends a recent study that also found that frailty was an independent risk factor for 28-day mortality compared to stroke patients without frailty [15]. Although our study obtained similar results, there were some differences. Our study included two types of stroke (hemorrhagic stroke and ischemic stroke), whereas both of these studies focused only on ischemic stroke. A previous study found that the rate of hemorrhagic stroke was higher than that of ischemic stroke [25]. In addition, our study had a long-term follow-up with further evidence. In contrast, Kim et al. found that patients of spontaneous intracerebral hemorrhage with frailty, as measured by the modified Frailty Index, did not have an increased risk of mortality than those without frailty [14]. The main reason suspected by the authors was that physicians were more likely to choose more severe patients for frailty assessment, leading to a selective patient bias. However, Imaoka et al. conducted a study including 156 patients with spontaneous intracerebral hemorrhage and found that each one-point increase in the modified Frailty Index led to an approximately 2-fold risk of mortality (OR = 1.97, 95% CI: 1.34–2.90) in multivariate analysis models [13]. Although our study reported a statistically significant association between frailty and one-year mortality among stroke patients, more research with a large sample size covering different types of stroke investigating the impact of frailty on adverse outcomes, such as mortality, will be warranted in the future.
4.2. Potential mechanism for the association between frailty and mortality
The mechanism between frailty and mortality among stroke patients is unclear. Several reasons could explain these associations. First, frailty was a syndrome indicating poor functional ability and accumulated deficits of multiple systems, which was confirmed to increase the risk of mortality by a great body of different populations and settings [10,26]. Older adults experienced stroke accidents, and either hemorrhagic stroke or ischemic stroke was a huge stressor, aggravating the negative impact of frailty on patients and eventually likely increasing the risk of mortality. Second, for frail patients, due to the decreased physiological reserve, stroke patients who experience frailty might be insufficient to endure invasive medical procedures such as surgery, mechanical ventilation and medication in the acute disease stage, leading to a higher risk of mortality. Third, at the chronic and rehabilitation stages, stroke patients usually have disability [27] and dysphagia [28], resulting in long-term inactivity and a risk of malnutrition [29] and therefore exacerbating the situation of frailty. Stroke patients with frailty might develop a vicious circle of frailty coexisting with inactivity and malnutrition and eventually contribute to unfavorable outcomes such as mortality and severe disability. Given the complexity between frailty and mortality, more studies related to the pathomechanism of this vital issue need to be conducted.
4.3. Implication for clinical nursing
This finding indicated that clinicians could assess the risk of mortality for patients with stroke and identify stroke patients who need more special clinical attention. In addition, early frailty screening could help clinicians implement comprehensive treatment by considering the benefit and risk in the clinical decision process with the family. Moreover, for surviving patients after the acute disease stage of stroke, screening frailty could help clinicians and family members make an appropriate rehabilitation program and intervention program for exercise and nutrition. A previous study suggested that a combination of exercise training and nutritional intervention with branched-chain amino acid improvements can effectively improve leg press strength and the Berg balance scale score among poststroke patients [30].
4.4. Strengths and limitations
Our study possesses some strengths and limitations. First, the sample size in our study was not large, especially for the number of hemorrhagic strokes (n = 37), failing to make a conclusive result based on subgroup analysis of diagnosis. Second, our study did not calculate comorbidity and stroke severity associated with mortality, which might underestimate or overestimate the impact of frailty on one-year all-cause mortality. Third, the well-trained nurses in charge of telephone follow-up of one-year mortality did not collect the reason for death; therefore, we cannot perform a subgroup analysis based on the type of reason for mortality. Fourth, we did not collect the treatment for stroke patients, such as thrombolysis and surgery operations, which may lead to overestimated or underestimated results. However, our study possesses some merits. First, our study was a prospective multicenter cohort study with long-term follow-up (one-year mortality) and a larger sample size than previous studies, which helped to better explore the association between frailty and mortality. Second, compared to prior studies, our study controlled for several potential confounding factors (age, ADL, IADL, low handgrip strength and polypharmacy), which were closely related to adverse outcomes. Third, to the best of our knowledge, this was the first study focusing on ischemic and hemorrhagic stroke in China to explore the association between frailty and one-year mortality. We believe that our findings add new evidence for this field.
5. Conclusion
Our findings clearly suggest that frailty is an independent risk factor for one-year mortality among older patients with stroke. Early screening frailty among stroke patients at hospital admission is very important, and corresponding interventions should also be implemented to reduce the rate of mortality among older stroke patients.
Ethical statement
The Ethics Committee of Peking Union Medical College Hospital approved the present study (Approval No. S-K540). In addition, participants agreed to sign written informed consent before participating in this project. The authors confirm that this study was conducted in accordance with the Declaration of Helsinki.
Funding
This study was funded by Fundamental Research Funds for Central Universities of Peking Union Medical College (No. 3332020007).
Author statement
Xiao-Ming Zhang: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, Writing - original draft, Writing - review & editing, Project administration. Jing Jiao: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Data curation, Writing - review & editing, Supervision, Project administration, Funding acquisition. Tao Xu: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Data curation, Writing - review & editing, Supervision. Xin-Juan Wu: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Writing - review & editing, Supervision.
Data availability statement
Data can be accessed by contacting with corresponding authors with reasonable request.
Declaration of competing interest
The authors have declared no conflict of interest.
Acknowledgments
The authors sincerely thank all the participants for their voluntary participation and all the investigators for their work.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.02.001.
Contributor Information
Xiao-Ming Zhang, Email: zhangmuxi0310@163.com.
Jing Jiao, Email: jiaojing.2006@aliyun.com.
Tao Xu, Email: xutaosd@126.com.
Xin-Juan Wu, Email: wuxinjuan@sina.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.GBD 2016 Lifetime Risk of Stroke Collaborators. Feigin V.L., Nguyen G., Cercy K., Johnson C.O., Alam T., et al. Global,regional,and country-specific lifetime risks of stroke,1990 and 2016. N Engl J Med. 2018;379(25):2429–2437. doi: 10.1056/NEJMoa1804492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell B.C.V., Khatri P. Stroke Lancet. 2020;396(10244):129–142. doi: 10.1016/S0140-6736(20)31179-X. [DOI] [PubMed] [Google Scholar]
- 3.Denti L., Scoditti U., Tonelli C., Saccavini M., Caminiti C., Valcavi R., et al. The poor outcome of ischemic stroke in very old people:a cohort study of its determinants. J Am Geriatr Soc. 2010;58(1):12–17. doi: 10.1111/j.1532-5415.2009.02616.x. [DOI] [PubMed] [Google Scholar]
- 4.Rønning O.M., Stavem K. Predictors of mortality following acute stroke:a cohort study with 12 years of follow-up. J Stroke Cerebrovasc Dis. 2012;21(5):369–372. doi: 10.1016/j.jstrokecerebrovasdis.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Fekadu G., Chelkeba L., Melaku T., Tegene E., Kebede A. 30-day and 60-day rates and predictors of mortality among adult stroke patients: prospective cohort study. Ann Med Surg. 2020;53:1–11. doi: 10.1016/j.amsu.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Oliveira A.D.P., de Andrade-Valença L.P.A., Valença M.M. Factors associated with in-hospital mortality in very elderly patients with ischemic stroke:A cohort study. J Stroke Cerebrovasc Dis. 2019;28(10):104281. doi: 10.1016/j.jstrokecerebrovasdis.2019.06.039. [DOI] [PubMed] [Google Scholar]
- 7.Avers D. In: Guccione's geriatric physical therapy. fourth ed. Avers D., Wong R.A., editors. Mosby; St. Louis (MO): 2020. Chapter 13 - the older adult who is frail; pp. 283–308. [Google Scholar]
- 8.Clegg A., Young J., Iliffe S., Rikkert M.O., Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Vries O.J., Peeters G.M.E.E., Lips P., Deeg D.J.H. Does frailty predict increased risk of Falls and fractures? A prospective population-based study. Osteoporos Int. 2013;24(9):2397–2403. doi: 10.1007/s00198-013-2303-z. [DOI] [PubMed] [Google Scholar]
- 10.Zhang X.M., Dou Q.L., Zhang W.W., Wang C.H., Xie X.H., Yang Y.Z., et al. Frailty as a predictor of all-cause mortality among older nursing home residents:A systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(6):657–663. doi: 10.1016/j.jamda.2018.11.018. e4. [DOI] [PubMed] [Google Scholar]
- 11.Doi T., Tsutsumimoto K., Ishii H., Nakakubo S., Kurita S., Shimada H. Frailty and driving status associated with disability:a 24-month follow-up longitudinal study. BMJ Open. 2021;11(4) doi: 10.1136/bmjopen-2020-042468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winovich D.T., Longstreth W.T., Arnold A.M., Varadhan R., Zeki Al Hazzouri A., Cushman M., et al. Factors associated with ischemic stroke survival and recovery in older adults. Stroke. 2017;48(7):1818–1826. doi: 10.1161/strokeaha.117.016726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Imaoka Y., Kawano T., Hashiguchi A., Fujimoto K., Yamamoto K., Nishi T., et al. Modified frailty index predicts postoperative outcomes of spontaneous intracerebral hemorrhage. Clin Neurol Neurosurg. 2018;175:137–143. doi: 10.1016/j.clineuro.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Kim M.G., Gandhi C., Azizkhanian I., Epstein B., Mittal A., Lee N., et al. Frailty and spontaneous intracerebral hemorrhage:does the modified frailty index predict mortality? Clin Neurol Neurosurg. 2020;194:105816. doi: 10.1016/j.clineuro.2020.105816. [DOI] [PubMed] [Google Scholar]
- 15.Evans N.R., Wall J., To B., Wallis S.J., Romero-Ortuno R., Warburton E.A. Clinical frailty independently predicts early mortality after ischaemic stroke. Age Ageing. 2020;49(4):588–591. doi: 10.1093/ageing/afaa004. [DOI] [PubMed] [Google Scholar]
- 16.Zhang X.M., Jiao J., Zhu C., Guo N., Liu Y., Lv D.M., et al. Cognitive frailty and 30-day mortality in a national cohort of older Chinese inpatients. Clin Interv Aging. 2021;16:389–401. doi: 10.2147/CIA.S294106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woo J., Yu R., Wong M., Yeung F., Wong M., Lum C. Frailty screening in the community using the FRAIL scale. J Am Med Dir Assoc. 2015;16(5):412–419. doi: 10.1016/j.jamda.2015.01.087. [DOI] [PubMed] [Google Scholar]
- 18.Chen L.K., Woo J., Assantachai P., Auyeung T.W., Chou M.Y., Iijima K., et al. Asian working group for sarcopenia:2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–307. doi: 10.1016/j.jamda.2019.12.012. e2. [DOI] [PubMed] [Google Scholar]
- 19.Masnoon N., Shakib S., Kalisch-Ellett L., Caughey G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. doi: 10.1186/s12877-017-0621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soysal P., Veronese N., Arik F., Kalan U., Smith L., Isik A.T. Mini Nutritional Assessment Scale-Short Form can be useful for frailty screening in older adults. Clin Interv Aging. 2019;14:693–699. doi: 10.2147/CIA.S196770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiao C.C., Hsu H.C., Chen I.L., Weng C.Y., Chuang J.C., Lin S.C., et al. Lower barthel index is associated with higher risk of hospitalization-requiring pneumonia in long-term care facilities. Tohoku J Exp Med. 2015;236(4):281–288. doi: 10.1620/tjem.236.281. [DOI] [PubMed] [Google Scholar]
- 22.Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. 2008;108(4):52–62. doi: 10.1097/01.NAJ.0000314810.46029.74. ;quiz62-3. [DOI] [PubMed] [Google Scholar]
- 23.O'Caoimh R., Sezgin D., O'Donovan M.R., Molloy D.W., Clegg A., Rockwood K., et al. Prevalence of frailty in 62 countries across the world:a systematic review and meta-analysis of population-level studies. Age Ageing. 2020;50(1):96–104. doi: 10.1093/ageing/afaa219. [DOI] [PubMed] [Google Scholar]
- 24.He B., Ma Y., Wang C., Jiang M., Geng C., Chang X., et al. Prevalence and risk factors for frailty among community-dwelling older people in China:a systematic review and meta-analysis. J Nutr Health Aging. 2019;23(5):442–450. doi: 10.1007/s12603-019-1179-9. [DOI] [PubMed] [Google Scholar]
- 25.Andersen K.K., Olsen T.S., Dehlendorff C., Kammersgaard L.P. Hemorrhagic and ischemic strokes compared:stroke severity,mortality,and risk factors. Stroke. 2009;40(6):2068–2072. doi: 10.1161/STROKEAHA.108.540112. [DOI] [PubMed] [Google Scholar]
- 26.Hu K.Y., Zhou Q., Jiang Y.B., Shang Z.Z., Mei F., Gao Q.Q., et al. Association between frailty and mortality,Falls,and hospitalization among patients with hypertension:a systematic review and meta-analysis. BioMed Res Int. 2021;2021:2690296. doi: 10.1155/2021/2690296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang Y., Shi Y.Z., Zhang N., Wang S., Ungvari G.S., Ng C.H., et al. The disability rate of 5-year post-stroke and its correlation factors:A national survey in China. PLoS One. 2016;11(11) doi: 10.1371/journal.pone.0165341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh S. Dysphagia in stroke patients. Postgrad Med. 2006;82(968):383–391. doi: 10.1136/pgmj.2005.043281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bouziana S.D., Tziomalos K. Malnutrition in patients with acute stroke. J Nutr Metab. 2011;2011:167898. doi: 10.1155/2011/167898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ikeda T., Morotomi N., Kamono A., Ishimoto S., Miyazawa R., Kometani S., et al. The effects of timing of a leucine-enriched amino acid supplement on body composition and physical function in stroke patients:a randomized controlled trial. Nutrients. 2020;12(7):1928. doi: 10.3390/nu12071928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data can be accessed by contacting with corresponding authors with reasonable request.