Abstract
Introduction
and Importance: Sirenomelia, which called sirenomelia sequences, is a very rare congenital malformation. It is characterized by complete or incomplete fused lower extremities, renal agenesis, oligohydramnios, absent urinary tract and external genitalia, single umbilical arteries, imperforate anus, etc.
We are reporting a case of mermaid syndrome, a twin pregnancy in which one was healthy and the other was identified to have characteristic features of sirenomelia at the time of examination.
Case presentation
We present a case of a preterm baby who was born at 34 weeks of gestational age by cesarean section for twin pregnancy due to oligohydramnios with fetal distress. He had abdominal distension, an imperforated anus, no pelvic bone, and a fused leg with two femur bones and two tibial bones that shared one skin and two separate feet. There was none of the two kidneys, ureter, or bladder. He had been diagnosed with an atrial septal defect.
Clinical discusion
Sirenomelia is virtually always a fatal congenital abnormality that affects the fetal body's caudal region. Although fusion of the lower limbs is its most obvious feature.
The reported percentage of elective termination of pregnancy for the fetal anomaly is about 49.5%.The anomaly is postulated to be due to a combination of genetic predisposition and an environmental trigger factor, while the precise etiology is undetermined and believed to be multifactorial.
In surviving sirenomelia cases, treatment can be provided with amultidisciplinary approach.
Conclusion
Mermaid Syndrome is a lethal congenital anomaly with a poor prognosis.
Ultrasonography can be used to diagnose sirenomelia. Oligo-hydramnios and fused lower limbs are crucial features that aid in the diagnosis during the first trimester of pregnancy, with possible termination of the pregnancy being suggested as an option if detected early.
Keywords: Sirenomalia, Imporfrate anus, Twin patient, Congenital malformation
Highlights
-
•
This is the first case of sirenomelia, a rare and lethal congenital abnormality, reported here.
-
•
Our case report is about twin sirenomelia cases. Although the incidence of sirenomelia in twin pregnancy is extremely low.
-
•
Half of the children with the condition are born alive, and the majority die within the first five days due to pulmonary hypoplasia and renal failure caused by renal agenesis.
1. İntroduction
Sirenomelia is a relatively unusual congenital abnormality also known as sirenomelia sequences, mermaid syndrome, or mermaid malformation. Complete or incomplete fusion of the lower extremities, renal agenesis, oligohydramnios, absence of the urinary tract and external genitalia, single umbilical artery, and imperforate anus are all symptoms,etc. [1].
In the perinatal phase, it is a fatal condition. Due to many congenital abnormalities, the survival and quality of life of sirenomelia live births are exceedingly low. Approximately 49.5% of pregnancies are terminated voluntarily due to fetal abnormality, according to reports [2]. The anomaly is postulated to be due to a combination of genetic predisposition and an environmental trigger factor, while the precise etiology is unknown and believed to be multifactorial [3].
In sirenomelia, the proportion of babies delivered alive, preterm, and weighing less than 2500g was 47%, 71.2%, and 88.2%, respectively [1]. Moreover, half of all cases of sirenomelia were stillbirths, and those that were born alive frequently died within 1 or 2 years of their birth due to aberrant kidney and bladder issues [4].
Only about 1% of babies survive the first week after birth [1]. The risk of sirenomelia is quite low in twin pregnancies. Sirenomelia is more than 100 times more common in monozygotic twins than in singleton pregnancy and dizygotic twins [5,6].
As a result, the diagnosis and treatment of sirenomelia in twin pregnancy is a topic worth discussing. The case at hand involves a twin pregnancy, one of which was healthy and the other of which was diagnosed with sirenomelia.
2. Case report
A preterm baby came to the emergency department, delivered by a 16-year-old female (G1+P2+A0+L2) who had an emergency cesarean section for twin pregnancy due to oligohydramnios with fetal distress at 34 weeks of gestational age. No antenatal care was done during this pregnancy with an unknown medical history. Two male neonates were delivered with good Apgar scores (8 at 1st minute, 10 at 5th minute). One of them had fused legs and an imperforated anus.
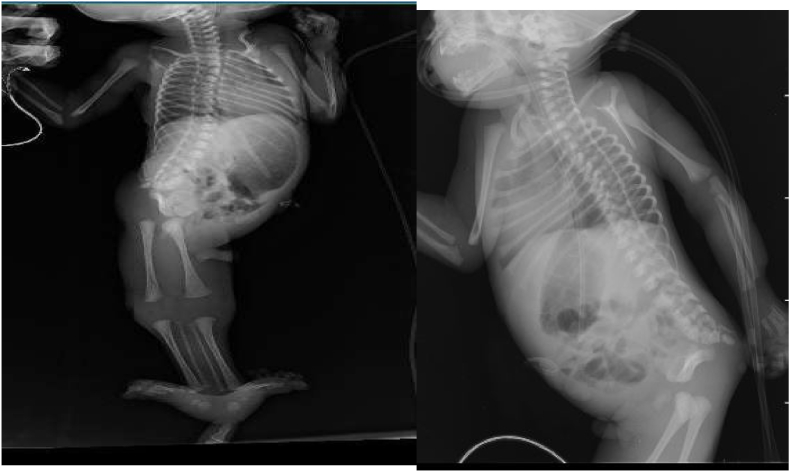
After delivery, the affected twin was transferred to the tertiary referral center, Recep Tayyip Erdogan Training, and Research Hospital, and admitted into the neonatal intensive care unit. We did an examination and found that he had abdominal distension, an imperforated anus, and a fused leg with two femur bones and two tibial bones that shared one skin and two separate feet, no cleft lip or palate, good sucking, no hydrocephaly, or spinal Bifida. We did an abdominal ultrasound, distended bowel, and renal agenesis. No bladder was seen on ultrasound. We did an x-ray with two femurs, two tibias, and two fibulae with no pelvic bone. Spinal bone deformity with scoliosis (Fig. 1, Fig. 2).
Fig. 1.
Sirenomelic baby on admission before emergency colostomy.
Fig. 2.
x-ray of chest and lower limbs.
We did echocardiography with congenital heart disease and ASD. An emergency colostomy was performed on the first day of admission. After surgery, maintenance of intravenous fluid and antibiotics (Ampicillin and Cefotaxime) was started (Fig. 3). He had no meconium or urine excretion for 48 hours. Urea and creatinine start to increase gradually. Then, after intestinal movement (peristalsis) was regained and a small amount of meconium was observed in the colostomy tube, the oral.
Fig. 3.
Sirenomelic baby after emergency colostomy.
Feeding was started gradually with a decrease in maintenance IV fluid until it stopped. Despite the treatment, the patient's situation continued to deteriorate. Urea and creatinine continued to rise, bloody vomiting, poor sucking, and severe anemia developed. After 17 days, the baby died.
This work has been reported in line with the scare 2020 criteria [28].
3. Discussion
Sirenomelia is virtually always a fatal congenital abnormality that affects the fetal body's caudal region. Although fusion of the lower limbs is its most obvious feature, it is invariably linked with less visible anomalies such as lumbosacral and pelvic bone deformities, blinding colon, nonexistent external genitalia, and renal agenesis [7].
According to the findings of mouse studies aimed at discovering how this defect develops (the genetic basis), this defect develops as a result of excessive retinoic acid (RA) secretion (disruption of the Cyp26a1 enzyme causes RA function to resume) and a lack of bone morphogenetic protein (Bmp) signalization to the lower part of the body in humans. When Bmp signaling is reduced in the ventral caudal embryonic mesoderm, many caudal abnormalities, severe cardiac deformities, and the absence of major arteries occur. As a result, RA and BMP play a role in each other's regulation. Balanced translocation, involving chromosome 16, and triploid mosaic are among the genetic explanations. 8. In our instance, no genetic testing was done.
Maternal diabetes, retinoic acid, heavy metals, and teratogen exposure, genetic variables, monozygotic twins, male gender, and the mother's age of 20 years or >40 years are all risk factors for sirenomelia malformation[[9], [10], [11], [12], [13]]. [[9], [10], [11], [12], [13]] [[9], [10], [11], [12], [13]].
The relative risk ratio for sirenomelia and maternal diabetes is 1:200–250, and it has been shown that this ratio is 22% in fetuses with abnormalities [8,[13], [14], [15], [16]].The male/female ratio is 2.7–3 [8,13,17,18]. Two factors were relevant in this case: the mother's age of 20 years and the male gender. After a thorough search of relevant literature in many databases, a study conducted a search and analyzed the whole literature referring to cases of sirenomelia in twin pregnancy.This is a common misunderstanding [20].In English and Chinese, 23 articles documented cases of sirenomelia in twin pregnancy while 1 article reported cases of sirenomelia in a triplet pregnancy. In our situation, the placental status was not noted. Stocker and Heifetz report a more accurate classification of sirenomelia: I, all thigh and leg bones are present; II, single fibula; III, absent fibulae; IV, partially fused femurs, fused fibulae; V, partially fused femurs, absent fibulae; VI, partially fused femurs, fused fibulae; VII, partially fused femurs, absent fibulae; VIII, partially fused femurs, absent fibulae fibulae; VI, single femur, single tibia; VII, single femur, absent tibiae (Table 1).
Table 1.
Classification of sirenomelia.
| Type 1 | all thigh and leg bones are present |
|---|---|
| Type 2 | single fibula |
| Type 3 | absent fibulae |
| Type 4 | partially fused femurs, fusedfibulae |
| Type 5 | partially fused femurs, absent fibulae |
| Type 6 | single femur, single tibia |
| Type 7 | single femur, absent tibiae |
According to clinical examination, leg x-ray and ultrasonography, fused lower extremities, and all thigh and leg bones present, sirenomelia twin was categorized as type I in this case. [19].
Bilateral renal agenesis, kidney malformations, single umbilical artery, megacystis, VACTERL/VATER (vertebral defects, anal atresia, cardiac defects, tracheoesophageal fistula, renal anomalies, and limb abnormalities) connection, and caudal regression syndrome are among the differential diagnoses (CRS). Despite the fact that sirenomelia is a severe version of the latter, the two entities are separate nosologic disorders that require specific genetic counseling [21].
Caudal dysplasia, sacral dysgenesis or regression, congenital sacralagenesis, sacral defect with anterior meningocele, sacro-coccygeal dysgenesis, and caudal dysplasia sequence are all terms used to describe CRS or CDS [[22], [23], [24], [25]].
It encompasses a wide range of congenital defects that affect the caudal spine and spinal cord, the hindgut, the urogenital system, and the lower limbs, with a wide range of severity. In the general population, 1–3 newborn infants per 100,000 live births are said to be affected by CRS. In diabetes moms' children, the prevalence rate is substantially higher.
A multidisciplinary approach is required, and many patients will require a phased surgical procedure. We discuss a patient with CRS in this paper [26].
In fact, While CRS is thought to be caused by a fundamental abnormality in the caudal mesoderm that prevents the creation of the thenotochord, sirenomelia is caused by blood flow being diverted away from the caudal region of the embryo through a single vitelline artery [21].
Caudal regression fetuses have two umbilical arteries, two hypoplastic lower extremities, and non-fatal kidney findings with imperforate or normal anus, whereas sirenomelic babies have renal agenesis or dysgenesis, a single aberrant umbilical artery, fused sub-extremities, and imperforate anus [21,27].We diagnosed our patient with sirenomelia due to the presence of single umbilical artery, no testis, imperforate anus, fused lower extremities, no pelvic bone, total renal agenesis, and absence of the bladder, ureter, urethra.
In surviving sirenomelia cases, treatment can be provided with amultidisciplinary approach. The conjoined legs can be surgically separated. During the preparation for surgery, subcutaneous tissue expanders such as balloons can be placed and the skin stretched and prepared for enlargement by filling the balloons with saltwater. The enlarged skin is used during surgical separation [14,16,18].
Finally, ultrasonography can be used to diagnose sirenomelia. Oligo-hydramnios and fused lower limbs are crucial features that aid in the diagnosis during the first trimester of pregnancy.
4. Conclusion
Mermaid Syndrome is a lethal congenital anomaly with a poor prognosis.
Ultrasonography can be used to diagnose sirenomelia. Oligo-hydramnios and fused lower limbs are crucial features that aid in the diagnosis during the first trimester of pregnancy, with possible termination of the pregnancy being suggested as an option if detected early.
Ethical approval
No need Ethical approval for case study at Mogadishu Somali Turkey, Recep Tayyip Erdogan Training and Research Hospital.
Sources of funding
No funding for this research.
Author contribution
MZY wrote the manuscript and corrected the manuscript for its scientific basis. FMH, AM and MA, collected the data for the study. AAY revised the manuscript for grammar and syntax mistakes.
Consent
The Patient's father was invited and written informed consent was obtained for his anonymized information to be published in this study.
Registration of research studies
1. Name of the registry:
2. Unique Identifying number or registration ID:
3. Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
MZY corrected the manuscript for its scientific basis.
Declaration of competing interest
The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript.
Contributor Information
Mehmet Zeki Yaşar, Email: mzekiyasar@gmail.com.
Abdisalam Abdullahi Yusuf, Email: taqi1434@gmail.com.
Fardowsa Mohamed Hassan, Email: Fureydeyse@gmail.com.
Amal Abdullahi Ali, Email: cafaaf199@gmail.com.
Miski Abdullahi Roble, Email: miskiroble10@gmail.com.
References
- 1.Orioli I.M., Amar E., Arteaga-Vazquez J., et al. Sirenomelia: an epidemiologic study in a large data set from the International Clearing house of Birth Defects Surveillance and Research, and literature review. Am J Med Genet C Semin Med Genet. 2011;157c:358–373. doi: 10.1002/ajmg.c.30324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu T., Wang X., Luo H., Yu H. Sirenomelia in twin pregnancy: a case report and literature review. Medicine. 2018;97(51) doi: 10.1097/MD.0000000000013672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen H., editor. Atlas of Genetic Diagnosis and Counseling. Humana Press; Totowa, NJ: 2006. pp. 905–906. [Google Scholar]
- 4.Ugwu R.O., Eneh A.U., Wonodi W. Sirenomelia in a Nigerian triplet: a case report. J. Med. Case Rep. 2011;5:426. doi: 10.1186/1752-1947-5-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen C.P., Shih S.L., Liu F.F., et al. Cebocephaly, alobarholoprosencephaly, spina bifida, and sirenomelia in a stillbirth. J. Med. Genet. 1997;34:252–255. doi: 10.1136/jmg.34.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davies J., Chazen E., Nance W.E. Symmelia in one of monozygotic twins. Teratology. 1971;4:367–378. doi: 10.1002/tera.1420040312. [DOI] [PubMed] [Google Scholar]
- 7.Stocker J.T., Heifetz S.A. Sirenomelia. A morphological study of 33 cases and review of the literature. Perspect. Pediatr. Pathol. 1987;10:7–50. [PubMed] [Google Scholar]
- 8.Kavunga E.K., Bunduki G.K., Mumbere M., Masumbuko C.K. Sirenomelia associated with an anterior abdominal wall defect: a case report. J. Med. Case Rep. 2019;13:213–218. doi: 10.1186/s13256-019-2162-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garrido-Allepuz C., Haro E., González-Lamuño D., MartínezFrías M.L., Bertocchini F., Ros M.A. A clinical and experimental overview of sirenomelia: insight into the mechanisms of congenital limb malformations. Dis Model Mech. 2011;4:289–299. doi: 10.1242/dmm.007732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kılınç N., Demir B., Yayla M. Sirenomelia: BirOtopsiOlgusu. PerinatalojiDergisi. 2003;11:56–58. [Google Scholar]
- 11.Kılınç N., Demir B., Yayla M. Sirenomelia: BirOtopsiOlgusu. PerinatalojiDergisi. 2003;11:56–58. [Google Scholar]
- 12.Saxena R., Puri A. Sirenomelia or mermaid syndrome. Indian J. Med. Res. 2015;141:495. doi: 10.4103/0971-5916.159323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joshi R., Duomai V.K., Sangma B. Sirenomelia, the mermaid baby: a case report. Int J ReprodContraceptObstet Gynecol. 2019;8:4609–4611. [Google Scholar]
- 14.Samal S.K., Rathod S. Sirenomelia: the mermaid syndrome: report of two cases. J Nat ScBiol Med. 2015;6:264–266. doi: 10.4103/0976-9668.149227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kshirsagar V.Y., Ahmed M., Colaco S.M. Sirenomeliaapus: a rare deformity. J ClinNeonatol. 2012;1:146–148. doi: 10.4103/2249-4847.101699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reddy K.R., Srinivas S., Kumar S., Reddy S., Prasad H., Irfan G.M. Sirenomelia: a rare presentation. J. Neonatal Surg. 2012;1:7. [PMC free article] [PubMed] [Google Scholar]
- 17.Dursun A., Akyol G., Eren L., Erdem M. Birsirenomeliavakası. Anatolian J Gynecol. 1993;3:283–285. [Google Scholar]
- 18.Browne M., Fitchev P., Adley B., Crawford S.E. Sirenomelia with an angiomatous lumbosacral myelocystocele in a full-term infant. J. Perinatol. 2004;24:329–331. doi: 10.1038/sj.jp.7211085. [DOI] [PubMed] [Google Scholar]
- 19.Stocker J.T., Heifetz S.A. Sirenomelia: a morphological study of 33 cases and review of the literature. Perspect. Pediatr. Pathol. 1987;10:7–50. [PubMed] [Google Scholar]
- 20.Xu T., Wang X., Luo H., Yu H. Sirenomelia in twin pregnancy: a case report and literature review. Medicine (Baltim.) 2018 Dec;97(51) doi: 10.1097/MD.0000000000013672. PMID: 30572488; PMCID: PMC6320003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roselló J.M., Loscalzo G., Buongiorno S., Jakaitė V., Perales-Marín A. Sirenomelia, case report and review of the literature. J. Matern. Fetal Neonatal Med. 2020;26:1–4. doi: 10.1080/14767058.2020.1742693. [DOI] [PubMed] [Google Scholar]
- 22.Duhamel B. From the mermaid to anal imperforation: the syndrome of caudal regression. Arch. Dis. Child. 1961;36:152–155. doi: 10.1136/adc.36.186.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferrer-Vaquer A., Hadjantonakis A.-K. Birth defects associated with perturbations in preimplantation, gastrulation, and axis extension: from conjoined twinning to caudal dysgenesis. Wiley Interdiscip Rev. Dev. Biol. 2012;2:427–442. doi: 10.1002/wdev.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh S.K., Singh R.D., Sharma A. Caudal regression syndrome—case report and review of literature. Pediatr. Surg. Int. 2005;21:578–581. doi: 10.1007/s00383-005-1451-4. [DOI] [PubMed] [Google Scholar]
- 25.Thottungal A.D., Charles A.K., Dickinson J.E., Bower C. Caudal dysgenesis and sirenomelia-single centre experience suggests common pathogenic basis. Am. J. Med. Genet. 2010;152:2578–2587. doi: 10.1002/ajmg.a.33599. [DOI] [PubMed] [Google Scholar]
- 26.Kylat R.I., Bader M. Caudal regression syndrome. Children. 2020;7(11):211. doi: 10.3390/children7110211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uyanıkoğlu H., Gengeç K., Sak S., Sak M.E. A rare seen case report: sirenomelia in a term pregnant woman. J. Harran Univ. Med. Fac. 2016;13:176–179. [Google Scholar]
- 28.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020 Dec 1;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]