Abstract
Introduction
and importance: Herein we present a rare case of multiple second to fifth carpometacarpal joint fracture-dislocations. It is important in such cases to be aware of a high-velocity impact etiology of the fractures, which will ensure proper imaging, diagnosis and treatment.
Case presentation
A 34-year-old male presented with severe pain in his left hand following a motorcycle accident. He was diagnosed as multiple second to fifth carpometacarpal joint fracture-dislocations. He was successfully treated with closed reduction with multiple Kirshner wires fixation under general anesthesia. A one-year follow up confirmed excellent clinical results.
Clinical discussion
There are various surgical options including casting, closed reduction and percutaneous pinning (CRPP), and open reduction internal fixation, however, the optimal treatment is still controversial. The closed reduction is recommended in all CMC joint dislocations. Adding a K-wire fixation can create a secure fixation and achieve an excellent outcome.
Conclusion
Multiple carpometacarpal joint fracture-dislocations is a very rare injury. Careful clinical examination is important for an accurate diagnosis and plain radiographic studies are necessary. Standard fracture dislocation treatment can be used. Simple closed reduction with the K-wires fixation technique is easy to perform and in our case achieved successful treatment in terms of clinical and radiographic outcomes.
Keywords: Carpometacarpal joint fracture dislocation, Operative treatment, Treatment outcomes
Highlights
-
•
Multiple carpometacarpal joint fracture-dislocations is a very rare injury.
-
•
Careful clinical examination is important for an accurate diagnosis and plain radiographic studies are necessary.
-
•
Simple closed reduction with the K-wires fixation technique is easy to perform and achieved successful treatment.
1. Introduction and importance
Carpometacarpal (CMC) joint fracture-dislocations are rare, occurring in less than 1% of hand injuries [1]. This condition is easily misdiagnosed, in up to 70% of cases [2], because the clinical presentation of generalized swelling can obscure the characteristic deformities. Fracture dislocations of the carpometacarpal joints are usually related to high-force injuries such as motor vehicle accidents, crush injuries, and heavy objects falling on the hand [3].
Herein, we report a case who presented with multiple carpometacarpal joint dislocations which were successfully managed operatively. The clinical presentation, mechanism of injury, radiographic description, treatment, and post-operative rehabilitation are discussed. This report has been written according to the SCARE 2020 guidelines [4].
2. Case presentation
The patient was a 34-year-old left hand-dominant male who presented to the emergency room with severe pain in his left hand 30 minutes following a motorcycle accident. He complained of pain, swelling, and deformity in his left hand. The physical examination showed prominent marked bony deformities at the dorsal aspect of his left hand with marked tenderness at the 2nd to 5th carpometacarpal joints (CMC joints). He could not move his left wrist due to severe pain. Posteroanterior, oblique, and radiographic views were taken (Fig. 1) and revealed dorsal dislocation of the 2nd to 5th CMC joints with a displaced avulsion fracture at the base of the 5th metacarpal bone. We discussed the positive findings with the patient and then we decided to manage the fracture dislocations operatively by closed reduction with multiple Kirshner wires fixation under general anesthesia. After general anesthesia was done, we performed closed reduction by longitudinal traction with direct pressure over the dorsal base of the CMC joints in the palmar aspect direction. We checked the alignment under fluoroscope and then applied multiple pins with K-wire number 1.5 mm in each metacarpal from the distal to the proximal direction (Fig. 2). Finally, we applied a volar slab with the hand in the safe position. The postoperative radiographs confirmed congruent joints of the left 2nd to 5th CMC joints. The patient's left hand was immobilized for 6 weeks, at which time the K-wires and slab were removed, and he began physical therapy for finger stiffness. Three months after the operation, he had regained complete and painless mobility of the wrist, with full hand grip (Fig. 3), and 6 months after the injury, he had returned to performing intense physical exercise using the affected hand without problems. A plain radiograph was done at 3 months and showed a minimally displaced small fragment at the base of the 5th metacarpal bone without any dislocation or subluxations of the other CMC joints (Fig. 4). He was very satisfied with the results of the treatment at the last follow-up at 1 year with a zero point score of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire, and equal grip strength and pinch strength on both sides.
Fig. 1.
Anteroposterior, oblique and lateral radiographs of the patient’s hand showing dislocation of the second to fifth CMCs with avulsion at the base of the fifth metacarpal bone.
Fig. 2.
Anteroposterior, oblique and lateral radiographs of the patient’s hand showing congruency of the second to fifth CMC joints following K-wire fixation.
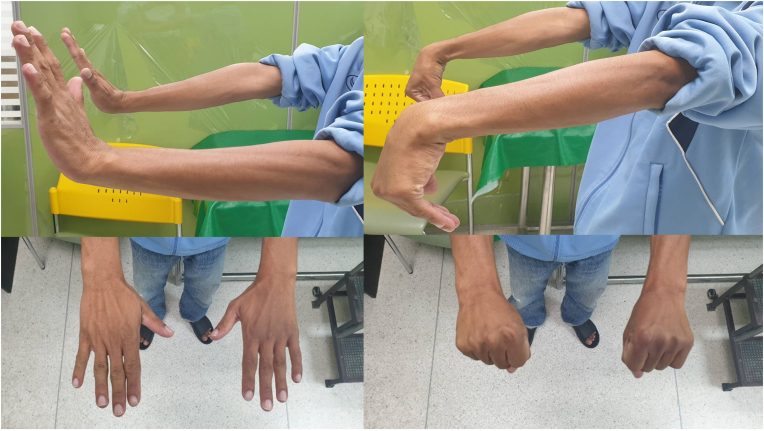
Fig. 3.
Pictures showing full hand grip and range of motion of the patient’s hand six months post-operatively.
Fig. 4.
Anteroposterior, oblique and lateral radiographs of the patient’s hand showing well-congruent second to fifth CMC joints with a minimal non-union at the base of the fifth metacarpal bone.
3. Clinical discussion
Multiple carpometacarpal joint dislocations are very rare. One study [5] investigated the incidence of hand fractures and found that CMC joint fracture-dislocations in merely three of 1621 reviewed hand fractures, an incidence of less than 0.2%. Regarding the anatomy of the CMC joints, the fifth CMC joint is a saddle joint similar to the thumb CMC joint that leads to the fifth CMC joint having more mobility than the central three CMC joints. Moreover, the fifth metacarpal configuration slopes toward the ulnar side while the fourth CMC is transverse and the base of the 5th CMC joint is the point of insertion of the flexor carpi ulnaris tendon, which are the two factors creating instability in the 5th CMC [3], while dislocation of the central three CMC joints is not commonly seen.
The mechanism of this type of injury is usually a high-velocity impact [6,7] as in our patient who had a motorcycle accident. These fracture dislocations are classified into dorsal and volar dislocations, depending on the direction of the force. The dorsal fracture dislocation is more common than the volar fracture dislocation. Although simultaneous divergence of the CMC joint dislocation in different digits has been reported [8], our case was the common type of CMC dorsal direction displacement.
In this type of injury, at least two plain radiographs with anteroposterior and lateral views should be obtained to aid an accurate diagnosis. Parallel “M lines” are used for evaluation of the CMC joint(s) on the anteroposterior view [9]. The direction of displaced CMC joint fracture dislocation(s) can be evaluated using the lateral view [2]. Our patient could be diagnosed using plain radiographs. Advanced imaging such as computer tomography can have a role in cases of occult fracture.
Open fracture dislocations, joint instability after failed closed reduction, intra-articular damage, concomitant fractures to the carpal or metacarpal bones, or displaced avulsion fractures involving the extensor carpi ulnaris such as in our case are the indications for surgical treatment [10]. There are various surgical options including casting, closed reduction and percutaneous pinning (CRPP), and open reduction internal fixation, however, the optimal treatment is still controversial [11]. The closed reduction method is suitable in cases of uninjured intra-articular involvement or successful joint relocation and is also recommended in all CMC joint dislocations [12]. The disadvantage of this method is usually secondary instability or re-displacement when treating alone [13]. Adding a K-wire fixation can mitigate these problems by creating a secure fixation. In cases of failed reduction or open fracture, an open reduction approach is recommended. Although our case had a small avulsion fracture at the base of the fifth metacarpal bone, we used the closed reduction method because we tried closed reduction first and found that the joints could be relocated congruently successfully with K-wires, which is an easy fixation technique to prevent further subluxation.
There is to date no consensus concerning the ideal length of time for K-wire fixation of these joints [14]. One study recommended removal no earlier than 6 weeks in adults with a report of two good outcomes and one fair outcome following K-wire fixation for 6 weeks [15]. Our patient's hand was immobilized using a volar slab in the safe position for 6 weeks, at which time the K-wires and slab were removed and physiotherapy started to prevent joint stiffness. Our case achieved a DASH score of 0 with excellent results at the one-year follow-up, which was in contrast with a previous report on patient who was suffering disability and loss of function at the same interval [15].
4. Conclusion
Multiple carpometacarpal joint fracture-dislocations is a very rare injury. Careful clinical examination is important and plain radiographic studies are necessary. Standard fracture dislocation treatment can be used. Simple closed reduction with the K-wires fixation technique is easy to perform and in our case achieved successful treatment in terms of clinical and radiographic outcomes.
Ethical approval
The present study was approved by the Prince of Songkla University Institutional Review Board, Faculty of Medicine, Songklanagarind Hospital, Prince of Songkla University (IRB number REC 64-160-11-1).
Sources of funding
No funding was involved regarding this review.
Author contribution
Sitthiphong Suwannaphisit —Preparation of case report, Literature review, Writing the paper. Porames Suwanno — Literature review. Warangkana Fongsri - Literature review. Sunton Wongsiri – Writing the paper.
Registration of research studies
None.
Guarantor
Sitthiphong Suwannaphisit, MD.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Declaration of competing interest
No conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103596.
Contributor Information
Sitthiphong Suwannaphisit, Email: aunsittipong@gmail.com.
Porames Suwanno, Email: ake23488@gmail.com.
Warangkana Fongsri, Email: fwarangk@gmail.com.
Sunton Wongsiri, Email: joesunton@gmail.com.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Sharma A.K., John J.T. Unusual case of carpometacarpal dislocation of all the four fingers of ulnar side of hand. Med. J. Armed Forces India. 2005;61(2):188–189. doi: 10.1016/S0377-1237(05)80024-3. Feb. Epub 2011 Jul 21. PMID: 27407748; PMCID: PMC4922986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henderson J.J., Arafa M.A. Carpometacarpal dislocation. An easily missed diagnosis. J. Bone Joint. Surg. Br. 1987;69(2):212–214. doi: 10.1302/0301-620X.69B2.3818751.PMID:3818751. Mar. [DOI] [PubMed] [Google Scholar]
- 3.Malshikare V.A. An ulnar-type dislocation of fifth carpometacarpal joint: case report and review of the literature. J. Hand Microsurg. 2020;12(Suppl 1):S61–S63. doi: 10.1055/s-0039-1680277. Oct. Epub 2019 Mar 1. PMID: 33335375; PMCID: PMC7735547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. Dec. Epub 2020 Nov 9. PMID: 33181358. [DOI] [PubMed] [Google Scholar]
- 5.Dobyns J.H., Linscheid R.L., Cooney W.P., 3rd Fractures and dislocations of the wrist and hand, then and now. J. Hand Surg. Am. 1983;8(5 Pt 2):687–690. doi: 10.1016/s0363-5023(83)80247-0. Sep. PMID: 6630950. [DOI] [PubMed] [Google Scholar]
- 6.Breiting V. Simultaneous dislocations of the bases of the four ulnar metacarpals upon the last row of carpals. Hand. 1983;15(3):287–289. Oct. PMID: 6642305. [PubMed] [Google Scholar]
- 7.Waugh R.L., Yancey A.G. Carpometacarpal dislocations with particular reference to simultaneous dislocation of the bases of the fourth and fifth metacarpals. J. Bone Joint. Surg. Am. 1948;30A(2):397–404. Apr. PMID: 18912301. [PubMed] [Google Scholar]
- 8.Kumar R., Malhotra R. Divergent fracture-dislocation of the second carpometacarpal joint and the three ulnar carpometacarpal joints. J. Hand Surg. Am. 2001;26(1):123–129. doi: 10.1053/jhsu.2001.20153.PMID:11172378. Jan. [DOI] [PubMed] [Google Scholar]
- 9.Gilula L.A. Carpal injuries: analytic approach and case exercises. AJR Am. J. Roentgenol. 1979;133(3):503–517. doi: 10.2214/ajr.133.3.503. Sep. PMID: 111512. [DOI] [PubMed] [Google Scholar]
- 10.Büren C., Gehrmann S., Kaufmann R., Windolf J., Lögters T. Management algorithm for index through small finger carpometacarpal fracture dislocations. Eur. J. Trauma Emerg. Surg. 2016;42(1):37–42. doi: 10.1007/s00068-015-0611-z. Feb. Epub 2015 Dec 11. PMID: 26660674. [DOI] [PubMed] [Google Scholar]
- 11.Lattanza L.L., Choi P.D. In: Hand Surgery. Berger R.A., Weiss A.-P.C., editors. Lippincott Williams & Wilkins; Philadelphia, PA: 2004. Intraarticular injuries of the metacarpophalangeal and carpometacarpal joints; pp. 176–179. [Google Scholar]
- 12.Cates R.A., Rhee P.C., Kakar S. Multiple volar carpometacarpal dislocations: case report/review of the literature. J. Wrist Surg. 2016;5(3):236–240. doi: 10.1055/s-0036-1580602. Aug. Epub 2016 Mar 9. PMID: 27468376; PMCID: PMC4959901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawlis J.F., III, Gunther S.F. Carpometacarpal dislocations. Long-term follow-up. J. Bone Joint. Surg. Am. 1991;73(1):52–59. PMID: 1985994. [PubMed] [Google Scholar]
- 14.Gunther S.F. The carpometacarpal joints. Orthop. Clin. N. Am. 1984;15(2):259–277. PMID: 6728445. [PubMed] [Google Scholar]
- 15.Kumar S., Arora A., Jain A.K., Agarwal A. Volar dislocation of multiple carpometacarpal joints: report of four cases. J. Orthop. Trauma. 1998;12(7):523–526. doi: 10.1097/00005131-199809000-00019. PMID: 9781780. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.