ABSTRACT
Groin pain is a common symptom in hip and pelvic pathology and differentiating between the two remains a challenge. The purpose of this study was to examine whether a test combining resisted adduction with a sit-up (RASUT) differentiates between pelvic and hip pathology. The RASUT was performed on 160 patients with complaints of hip or groin pain who subsequently had their diagnosis confirmed by magnetic resonance imaging (MRI) or surgery. Patients were categorized as having pelvic pathology (athletic pubalgia or other) or hip pathology (intra-articular or other). Athletic pubalgia was defined as any condition involving the disruption of the pubic aponeurotic plate. Sensitivity, specificity, positive predictive accuracy, negative predictive accuracy and diagnostic odds ratios were computed. Seventy-one patients had pelvic pathology (40 athletic pubalgia), 81 had hip pathology and 8 had both. The RASUT was effective in differentiating pelvic from hip pathology; 50 of 77 patients with a positive RASUT had pelvic pathology versus 29 of 83 patients with a negative test (P < 0.001). RASUT was diagnostic for athletic pubalgia (diagnostic odds ratio 6.08, P < 0.001); 35 of 45 patients with athletic pubalgia had a positive RASUT (78% sensitivity) and 73 of 83 patients with a negative RASUT did not have athletic pubalgia (88% negative predictive accuracy). The RASUT can be used to differentiate pelvic from hip pathology and to identify patients without athletic pubalgia. This is a valuable screening tool in the armamentarium of the sports medicine clinician.
INTRODUCTION
There are many causes of groin pain in athletes with multiple terms used to describe the conditions, including Gilmore’s groin, sports hernia, athletic pubalgia, core muscle injury (CMI), hockey hip and, more recently, aponeurotic plate disruption [1, 2]. Groin pain has multiple possible etiologies including athletic pubalgia, osteitis pubis, nerve compression syndromes, hernias, genitourinary and gynecological disorders and femoroacetabular impingement (FAI) [3–7]. Groin pain often presents with overlapping conditions [8, 9], and it has been speculated that the motion limiting component of FAI may contribute to the development of athletic pubalgia [10].
Athletic pubalgia or CMI is commonly described as a strain or tear of soft tissue in the lower abdomen or groin [11, 12]. This has also been referred to as pubic-related groin pain [7]. The location frequently involved is the pubic aponeurotic complex. The pubic aponeurotic complex consists of the confluence of fibers superiorly from the rectus abdominis, conjoint tendon and the inguinal ligament, and inferiorly with the origin of adductor, pectineus and gracilis musculature (Fig. 1). The aponeurotic complex attaches to the pubis, allowing the structure to serve as an anchor point for the anterior pelvis [13]. One pathologic finding frequently identified by magnetic resonance imaging (MRI) and surgery is the detachment of the aponeurotic complex from the underlying pubic bone and symphysis, often referred to as a ‘cleft sign’ [14].
Fig. 1.
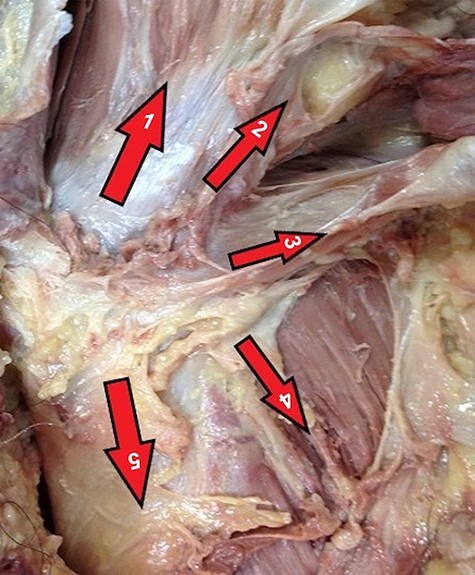
Muscular attachments at the pubic aponeurotic complex: rectus abdominus (1); transversalis fascia; (2); inguinal ligament (3); pectineus (4) and adductor longus (5).
Groin pain is a common symptom in both hip and pelvic pathology and differentiating between the two remains a challenge. It is imperative to have physical exam findings in combination with history and imaging to make an accurate diagnosis and provide the most appropriate treatment [12]. Patient history typically includes activity-related lower abdominal, groin or adductor pain. Symptoms might resolve with rest but return with activity. Common activities associated with pain include running, kicking, cutting or twisting, as well as positions of trunk hyperextension or hip abduction. Sports often associated with this pathology include hockey, soccer and football. Symptoms can be unilateral or bilateral depending on whether the injury crosses the midline. There are several physical exam findings consistent with athletic pubalgia. Patients can have pain with palpation at the pubic tubercle, pubic symphysis or the adductor insertion [3]. A resisted sit-up maneuver with palpation at the rectus abdominis insertion has previously been described [15]. Patients may also have pain with resisted adduction or pain with palpation of the proximal adductor origin [5, 16–18]. The resisted adduction sit-up test (RASUT) combines isometric adduction with a sit-up [19]. The potential advantage of the RASUT is that it allows the clinician to stress the pubic aponeurotic complex from both the superior and inferior vector forces at the same time. However, the clinical utility of the RASUT has not been examined. Therefore, the purpose of this study was to examine whether the RASUT differentiates between pelvic and hip pathology. It was hypothesized that a positive RASUT would be indicative of pelvic pathology.
MATERIALS AND METHODS
The RASUT was performed on first encounter with the patient as a screening tool in 204 patients with complaints of hip and/or groin pain. Exams were performed between 2018 and 2020 by either a fellowship-trained hip arthroscopist or an athletic pubalgia general surgeon specialist. Patients lay supine with knees flexed to 90° and feet flat on the exam table (Fig. 2). The examiner placed his forearm between the patient’s knees and the patient was instructed to squeeze the knees together while executing a sit up.
Fig. 2.

Resisted Adduction Sit-up Test.
Patients were asked to report discomfort during the test on a scale of 0 (no discomfort) to 10 (excruciating pain). Patients were also asked to identify the location of the pain relative to the inguinal fold (above the fold, on the fold or below the fold). Any test eliciting pain was categorized as positive. The patients then underwent further evaluation and treatment by their physician. Diagnosis was made by MRI using the protocol described previously [14]. Diagnoses were subsequently confirmed by surgical findings in those patients who went on to surgery. Forty-four patients did not have an MRI and did not have subsequent surgery; therefore, they were excluded from the study, leaving 160 patients (89 men, 71 women, age 38 ± 12 years). These patients comprised the study sample. Patients were categorized based on sporting participation as elite (n = 13), competitive (n = 31), recreational (n = 95) and not involved in sport (n = 21). The study was approved by the institutional review board where the study was performed.
Patients were categorized as having pelvic pathology (n = 71), hip pathology (n = 81) or a combination of both (n = 8) (Fig. 3). The hip arthroscopist saw 84 of the patients in the study (79 had hip pathology and 5 had pelvic pathology) and the athletic pubalgia specialist saw 76 of the patients (2 had hip pathology, 66 had pelvic pathology 8 had a combination of both).
Fig. 3.
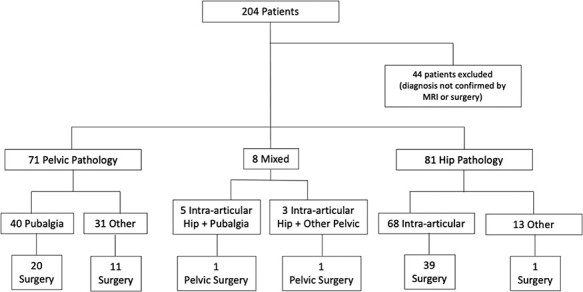
Diagnostic flow chart of MRI and surgical findings. ‘Mixed’ refers to combined pelvic and hip pathology.
Pelvic pathology was subdivided into athletic pubalgia (n = 40) and other pathologies (n = 31). Athletic pubalgia was defined as any condition involving the disruption of the pubic aponeurotic complex. Other pelvic conditions included 24 hernias, 3 adductor longus injuries and 4 other conditions (abdominal mass, pelvic venous occlusion, pubic ramus fracture and urachal duct remnant). Hip pathology was subdivided into intra-articular pathology (n = 68) and other hip or thigh pathology (n = 13). These other conditions included three trochanteric bursitis, three hamstring injuries, two gluteus medius injuries, two tensor fascia lata tendinopathies and three other conditions (femoral neck stress fracture, lumbar spine disease and myositis ossificans). Of the eight patients with a combination of pelvic and hip pathology five had an intra-articular hip injury with athletic pubalgia and three had an intra-articular hip injury with a hernia. Patients with other hip and thigh conditions were included in this study because their initial complaint included groin pain. In assessing the clinical utility of the RASUT for identifying pelvic pathology it was important to include all conditions with associated groin pain regardless of subsequent diagnosis. This provided a comprehensive assessment of test specificity [percentage of patients without pelvic pathology who had a negative RASUT test (% true negative)]. Patients with other hip and thigh conditions were differentiated from those with intra-articular hip conditions because the latter is commonly associated with athletic pubalgia [8, 9].
Statistical analyses
Fisher’s exact tests were used to assess whether the RASUT was effective at (i) differentiating pelvic pathology from hip pathology, (ii) identifying patients with pubalgia and (iii) identifying patients requiring surgery for pelvic pathology. Given the hypothesis that a positive RASUT test would differentiate pelvic from hip pathology, it was estimated that with a sample size of 160 patients equally split between those with pelvic versus hip pathology there would be 95% power to detect twice as many positive tests in patients with pelvic versus hip pathology at an alpha level of 0.05. Sensitivity, specificity, positive predictive accuracy, negative predictive accuracy and diagnostic odds ratios were computed where there was a statistically significant Fisher’s exact test (P < 0.05). Sensitivity refers to the percentage of patients with a given condition (e.g. pelvic pathology) who test positive for the test of interest (e.g. positive RASUT). Specificity refers to the percentage of patients without a given condition who test negative for the test of interest. Positive predictive accuracy refers to the percentage of positive tests that have the condition of interest. Negative predictive accuracy refers to the percentage of negative tests that do not have the condition of interest. The diagnostic odds ratio refers to the ratio of positive to negative tests in the patients with the condition of interest versus that ratio in the patients without the condition of interest.
RESULTS
The RASUT was positive in 77 of 160 patients (48%) (Fig. 4). Sixty-five percent (50 of 77) of patients with a positive RASUT had pelvic pathology (positive predictive accuracy) compared with 35% (29 of 83) of patients with a negative RASUT (65% negative predictive accuracy; P < 0.001). Specifically, the RASUT was diagnostic for athletic pubalgia (diagnostic odds ratio 6.08, Table I); 78% of patients with athletic pubalgia had a positive RASUT (sensitivity) and 88% of patients with a negative RASUT did not have athletic pubalgia (negative predictive accuracy). Of the 79 patients with pelvic pathology (8 with a combination of hip and pelvic pathology) 33 required surgical treatment; 79% of those requiring surgery had a positive RASUT (sensitivity) compared with 52% of patients not requiring surgery (48% specificity) (Table I).
Fig. 4.
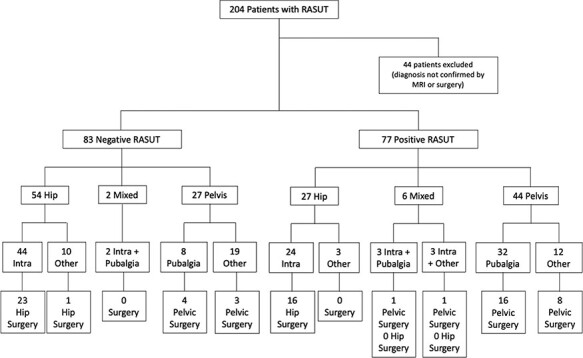
Diagnostic flow chart for RASUT results. ‘Mixed’ refers to combined pelvic and hip pathology.
Table I.
Ability of the RASUT to differentiate pelvic pathology from hip pathology
| Pelvic pathology (with or without hip pathology) | Hip pathology (only) | Athletic pubalgia | Other pelvic or hip pathology | Pelvic pathology requiring surgery | Pelvic pathology not requiring surgery | ||
|---|---|---|---|---|---|---|---|
| RASUT | Positive | 50 | 27 | 35 | 42 | 26 | 24 |
| Negative | 29 | 54 | 10 | 73 | 7 | 22 | |
| P value Fisher’s exact test | P < 0.001 | P < 0.001 | P = 0.019 | ||||
| Sensitivity (95% CI) | 63% (52–74%) | 78% (63–89%) | 79% (61–91%) | ||||
| Specificity (95% CI) | 67% (55–77%) | 63% (54–72%) | 48% (33–63%) | ||||
| Positive predictive accuracy | 65% (57–72%) | 45% (38–53%) | 52% (44–60%) | ||||
| Negative predictive accuracy | 65% (57–72%) | 88% (81–93%) | 76% (60–87%) | ||||
| Diagnostic odds ratio | 3.45 (1.80–6.61) | 6.08 (2.74–13.52) | 3.41 (1.23–9.40) | ||||
The intensity of the pain elicited during the RASUT was not different between the patients with pelvic versus hip pathology (3.7 ± 1.6 versus 4.0 ± 2.0, P = 0.440), athletic pubalgia versus other pelvic or hip pathology (3.8 ± 1.6 versus 3.8 ± 1.9, P = 0.99) or pelvic pathology requiring surgery versus pathology not requiring surgery and other pelvic and hip pathology (3.4 ± 1.7 versus 4.0 ± 1.8, P = 0.175).
For patients with a positive RASUT the location of the pain further differentiated pelvic from hip pathology (Fig. 5); 78% of patients with pain at or above the inguinal fold had pelvic pathology (43 of 55) compared with 32% of patients with pain only below the inguinal fold (7 of 22; P < 0.001).
Fig. 5.
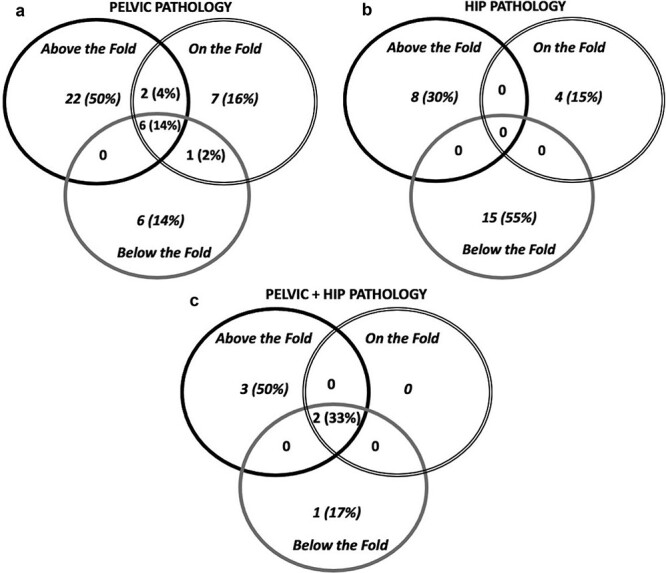
Location of pain relative to the inguinal fold in patients with positive RASUT: (a) patients with pelvic pathology, (b) patients with hip pathology and (c) patients with a combination of pelvic and hip pathology.
Hip pathology was more prevalent in female patients, while pelvic pathology was more prevalent in male patients: of the 71 female patients 52 had hip pathology, 18 had pelvic pathology and 1 had both; of the 89 male patients 53 had pelvic pathology, 29 had hip pathology and 7 had both (sex difference in prevalence P < 0.001). Only 2 of the 45 patients with pubalgia were women.
DISCUSSION
The purpose of this study was to determine if a test combining a sit-up with an adductor squeeze would be useful in differentiating pelvic pathology from hip pathology. The results indicated that the RASUT was effective at differentiating pelvic and hip pathology but was most useful for ruling out athletic pubalgia; of the 83 patients with a negative RASUT only 10 had athletic pubalgia (88% negative predictive accuracy).
Previously it was reported that 88% of patients with athletic pubalgia had pain with resisted adduction (88% sensitivity) and that 46% had pain with a resisted sit-up (46% sensitivity) [11]. However, the study only included patients with athletic pubalgia; therefore, specificity, positive predictive accuracy and negative predictive accuracy of the tests could not be assessed. In the present study, 78% of patients with athletic pubalgia had pain with the RASUT (sensitivity), which is comparable to that reported by Meyers et al. [11]. The present study extends those previous findings by showing that the RASUT has good specificity (67% of patients without athletic pubalgia had a negative RASUT test), low positive predictive accuracy (45% of patients with a positive RASUT had athletic pubalgia) and excellent negative predictive accuracy (88% of patients with a negative RASUT did not have athletic pubalgia).
A resisted cross-body sit-up test was previously shown to have excellent sensitivity (100%) and negative predictive accuracy (100%) for identifying athletic pubalgia, but had poor specificity (3%) and low positive predictive accuracy (52%) [20]. The study sample comprised patients with suspected athletic pubalgia but did not include any patients with isolated hip pathology. Thus, there was limited ability to assess test specificity. The present study had a more diverse patient population and therefore the RASUT had a higher specificity for athletic pubalgia (65%) than the resisted cross-body sit-up (3%). Kurowicki et al. [20] also showed that the Stinchfield test had a specificity of 60% but only 15% sensitivity, 26% positive predictive accuracy and 43% negative predictive accuracy (all four values lower than for the RASUT).
Based on the current results in a patient sample with pelvic and/or hip pathology a positive RASUT increases the possibility that a patient has pelvic pathology (65% positive predictive accuracy) and a negative RASUT increases the possibility that the patient does not have athletic pubalgia (88% negative predictive accuracy). A negative RASUT in a patient with pelvic pathology was more likely to be treated non-operatively. The positive predictive accuracy for identifying athletic pubalgia (45%) was lower than for differentiating pelvic from hip pathology (65%) because a lot of the patients with other pelvic pathologies also had a positive RASUT (15 of 34). The location of pain in the positive RASUT study also helped differentiate pelvis from hip pathology, with pain only below the inguinal fold being more common in patients with hip pathology with no pelvic involvement. As the data tend to support better results with operative intervention, it is important for clinicians to be able to make an accurate diagnosis quickly and help form an adequate treatment algorithm.
One possible limitation of this study is using MRI to confirm the diagnosis in patients who did not have surgery. The utility of MRI in these conditions has increased dramatically over the last two decades. Zoga et al. [21] report that MRI is 68% sensitive and 100% specific for rectus abdominus pathology and 86% sensitive and 89% specific for adductor pathology. The use of dedicated MRI protocols has been helpful in our practice for increased detection of common athletic pubalgia pathology [13, 14]. The inclusion of non-operative patients is beneficial in terms of getting an accurate assessment of the diagnostic utility of the RASUT. In fact, in patients with pelvic pathology the RASUT was predictive of those not requiring surgery (negative predictive accuracy 76%). Additionally, the patient sample in this study was diverse in terms of sports participation, with 28% being in elite or competitive sports, 59% involved in recreational sports and 13% not involved in sports. Thus, these results may be more generalizable to the majority of clinical practices.
An important limitation of this study is that inter-observer reliability was not evaluated for the RASUT. The test was performed by two physicians with independent practices geared toward athletic groin versus hip pain. It will be important to ensure that there is good inter-observer agreement to maximize the clinical utility of the RASUT. We have anecdotally found the RASUT easy, quick and reproducible when taught to our residents and fellows.
The exclusion of 44 patients who did not have an MRI to confirm their diagnosis may be a limitation. However, the investigators did not want to bias their diagnosis based on the results of the RASUT and invalidate a study based on a diagnostic screening tool. Thus, their exclusion increased the objectivity of the results.
CONCLUSION
In conclusion, based on the sensitivity, specificity, positive predictive accuracy, negative predictive accuracy and diagnostic odds ratio, the RASUT maneuver is a good screening tool for the diagnosis of athletic pubalgia. Patients with a negative RASUT are unlikely to have athletic pubalgia.
ACKNOWLEDGEMENTS
This study was presented at the International Society for Hip Arthroscopy Annual Meeting, Madrid, Spain, 17–19 October 2019, and won The Hip Preservation Society Physiotherapy Research Award for Original Research.
Contributor Information
Gregory J Galano, New York Orthopedics, 159 East 74 Street, New York, NY 10021, USA.
Timothy F Tyler, Nicholas Institute of Sports Medicine and Athletic Trauma, MEETH, Lenox Hill Hospital, 210 East 64 Street, New York, NY 10075, USA; Professional Physical Therapy, 2 Overhill Road, Scarsdale, NY 10583, USA.
Trevor Stubbs, Nicholas Institute of Sports Medicine and Athletic Trauma, MEETH, Lenox Hill Hospital, 210 East 64 Street, New York, NY 10075, USA.
Ali Ashraf, Nicholas Institute of Sports Medicine and Athletic Trauma, MEETH, Lenox Hill Hospital, 210 East 64 Street, New York, NY 10075, USA.
Michael Roberts, Nicholas Institute of Sports Medicine and Athletic Trauma, MEETH, Lenox Hill Hospital, 210 East 64 Street, New York, NY 10075, USA.
Malachy P McHugh, Nicholas Institute of Sports Medicine and Athletic Trauma, MEETH, Lenox Hill Hospital, 210 East 64 Street, New York, NY 10075, USA.
Mark P Zoland, Department of Surgery, Lenox Hill Hospital, 130 East 77 Street, New York, NY 10075, USA.
Stephen J Nicholas, New York Orthopedics, 159 East 74 Street, New York, NY 10021, USA; Nicholas Institute of Sports Medicine and Athletic Trauma, MEETH, Lenox Hill Hospital, 210 East 64 Street, New York, NY 10075, USA.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
FUNDING
There was no external funding for this study.
REFERENCES
- 1. Dimitrakopoulou A, Schilders E. Sportsman’s hernia? An ambiguous term. J Hip Preserv Surg 2016; 24: 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kuhn AW, Noonan BC, Kelly BT et al. The hip in ice hockey: a current concepts review. Arthroscopy 2016; 32: 1928–38. [DOI] [PubMed] [Google Scholar]
- 3. Caudill P, Nyland J, Smith C et al. Sports hernias: a systematic literature review. Br J Sports Med 2008; 42: 954–64. [DOI] [PubMed] [Google Scholar]
- 4. Elattar O, Choi HR, Dills VD et al. Groin injuries (Athletic Pubalgia) and return to play. Sports Health 2016; 8: 313–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Larson CM. Sports hernia/athletic pubalgia: evaluation and management. Sports Health 2014; 6: 139–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Röling MA, Mathijssen NM, Bloem RM. Incidence of symptomatic femoroacetabular impingement in the general population: a prospective registration study. J Hip Preserv Surg 2016; 3: 203–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weir A, Brukner P, Delahunt E et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med 2015; 49: 768–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hammoud S, Bedi A, Magennis E et al. High incidence of athletic pubalgia symptoms in professional athletes with symptomatic femoroacetabular impingement. Arthroscopy 2012; 28: 1388–95. [DOI] [PubMed] [Google Scholar]
- 9. Varada S, Moy MP, Wu F et al. The prevalence of athletic pubalgia imaging findings on MRI in patients with femoroacetabular impingement. Skeletal Radiol 2020; 49: 1249–58. [DOI] [PubMed] [Google Scholar]
- 10. Birmingham PM, Kelly BT, Jacobs R et al. The effect of dynamic femoroacetabular impingement on pubic symphysis motion: a cadaveric study. Am J Sports Med 2012; 40: 1113–8. [DOI] [PubMed] [Google Scholar]
- 11. Meyers WC, Foley DP, Garrett WE et al. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med 2000; 28: 2–8. [DOI] [PubMed] [Google Scholar]
- 12. Paajanen H, Brinck T, Hermunen H et al. Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: a randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman’s hernia (athletic pubalgia). Surgery 2011; 150: 99–107. [DOI] [PubMed] [Google Scholar]
- 13. Zoland M. Deciphering Groin and Pelvic Pain: The Interplay between Sports Hernia, Athletic Pubalgia, and Pelvic Floor Dysfunction. 2020. Available at: https://www.blurb.com/b/10265226. Accessed: 1 August 2021.
- 14. Zoland MP, Maeder ME, Iraci JC et al. Referral patterns for chronic groin pain and athletic pubalgia/sports hernia: magnetic resonance imaging findings, treatment, and outcomes. Am J Orthop (Belle Mead NJ) 2017; 46: E251–6. [PubMed] [Google Scholar]
- 15. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg 2007; 15: 507–14. [DOI] [PubMed] [Google Scholar]
- 16. Thorborg K, Serner A, Petersen J et al. Hip adduction and abduction strength profiles in elite soccer players: implications for clinical evaluation of hip adductor muscle recovery after injury. Am J Sports Med 2011; 39: 121–6. [DOI] [PubMed] [Google Scholar]
- 17. Tyler TF, Campbell R, Nicholas SJ et al. The association of hip strength and flexibility on the incidence of groin strains in professional ice hockey players. Am J Sports Med 2001; 29: 124–8. [DOI] [PubMed] [Google Scholar]
- 18. Tyler TF, Nicholas SJ. Rehabilitation of extra-articular sources of hip pain in athletes. N Am J Sports Phys Ther 2007; 2: 207–16. [PMC free article] [PubMed] [Google Scholar]
- 19. Meyers WC. Introducing the Core: Demystifying the Body of an Athlete, Thorofare, NJ: SLACK Inc., 2019. [Google Scholar]
- 20. Kurowicki J, Kraeutler MJ, Dávila Castrodad IM et al. Diagnostic accuracy of physical examination tests in core muscle injury. Am J Sports Med 2020; 48: 1983–8. [DOI] [PubMed] [Google Scholar]
- 21. Zoga AC, Kavanagh EC, Omar IM et al. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology 2008; 247: 797–807. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


