Abstract
Background
Pre-existing chronic pain has been associated with severe postoperative pain. In this study, we sought to prospectively analyse the association between the duration of chronic low back pain and the intensity of acute postoperative pain after lumbar fusion surgery.
Methods
A total of 330 patients who underwent lumbar fusion surgery were divided into three groups (chronic low back pain less than 1 year, one to 5 years, and more than 5 years) based on the duration of chronic pain. On the first postoperative day, the maximum pain scores of each patient were recorded during the day and at night. Bivariate correlation and logistic regression were performed to identify relationships between acute postoperative pain and related variables (age, sex, smoking history, body mass index, operation history, duration of surgery, level of preoperative pain, aetiology of back pain, Self-rating Anxiety Scale, Self-rating Depression Scale, FRAIL scale, and duration of chronic low back pain). If the postoperative pain score was > 3 when the patient reported was at rest, the patients were treated with postoperative intravenous self-controlled analgesia or rescue analgesics if necessary.
Results
There was an association between severe acute postoperative pain and the duration of chronic low back pain. In terms of VAS day, multivariable logistic regression showed the duration of chronic low back pain was not statistically significant (OR = 2.48, 95% CI: 0.900 to 6.828, p = 0.0789). The result is uncertain because the confidence interval included the null after controlling for SAS, SDS, BMI, and aetiology of back pain. In terms of VAS night, patients with a duration of chronic low back pain of more than 5 years were more likely having moderate to severe acute postoperative pain (VAS > 3) compared to patients with a duration of chronic low back pain less than 1 year (OR = 3.546, 95% CI: 1.405 to 8.95, p = 0.0074). Hospital stay, the pain score on the day of discharge and the pain score after 3 months displayed no significant difference among the three groups (P > 0.05). However, the need for postoperative rescue analgesics was different among the three groups (P < 0.05).
Conclusion
The longer the duration of chronic pain was, the higher the incidence of moderate to severe acute postoperative pain was and the greater the amount of analgesics required after surgery.
Trial registration
This study was registered at the Chinese Clinical Trial Registration Center (http://www.chictr.org.cn/index.aspx, clinical trial number: ChiECRCT20200165, date of registration: July 6, 2020).
Keywords: Duration of chronic low back pain, Acute postoperative pain, Lumbar fusion surgery
Background
Low back pain is one of the most frequent reasons people seek medical services [1]. It not only causes a high disability rate but also increases people’s medical burden [2]. Some people can recover naturally or through some form of intervention, and some people develop chronic low back pain [3]. Chronic low back pain is generally considered to be persistent if it lasts for more than 3 months [4]. The cause of chronic low back pain is uncertain (nonspecific). Some authors have suggested that lumbar spine stenosis, lumbar spondylolisthesis, disc herniation, and degenerative disc disease may play a role in the symptoms [5]. At the same time, these lumbar degenerative diseases are also the most common reasons for patients to choose fusion and internal fixation surgery [6].
In the past two decades, the number of patients choosing lumbar fusion surgery due to lumbar degenerative diseases has been increasing worldwide [7]. Clinical experience highlights that most patients choose fusion surgery to enable them to continue to work and to live an active life [8]. However, spine surgery patients are at high risk of postoperative pain [9]. Optimizing postoperative pain management can facilitate surgical recovery [10]. Risk factors for acute or persistent pain after lumbar fusion surgery can be targeted for perioperative treatment, including tailored postoperative pain treatment or individualized postoperative follow-up. At present, factors affecting the postoperative pain of patients can be broadly grouped into sex [11], obesity [12], preoperative opioid abuse [13], genetics [14], and many other factors. Preoperative chronic pain also affects postoperative pain and postoperative patient functional recovery [15, 16]. However, a careful review of the relevant literature did not yield any report about an association between the duration of chronic low back pain and acute postoperative pain while undergoing lumbar fusion surgery.
Therefore, in the present study, we investigated whether the duration of chronic low back pain influences the acute postoperative pain of patients undergoing lumbar fusion surgery. The visual analogue scale (VAS) is a tool used to assess postoperative pain. Our aim was to provide a reference for the pain management of patients with chronic low back pain.
Materials and methods
Ethics and patients
This study was approved by the ethics committee of the Chinese Ethics Committee of Registering Clinical Trials with approval number ChiECRCT20200165. The participating patients provided written informed consent. All methods were carried out in accordance with the Declaration of Helsinki and with the STROBE recommendations. This study was registered at the Chinese Clinical Trial Registration Center under the number ChiCTR2000029923 before patient enrolment. After obtaining written informed consent from all patients, we conducted this prospective observational study at The First Affiliated Hospital of USTC from July 8, 2020, to December 1, 2020. The inclusion criteria were as follows: patients with American Society of Anaesthesiologists (ASA) grades I to III, age range of 18 to 75 years, chronic low back pain supported by a focused history, physical examination and lumbar imaging by X-ray, magnetic resonance imaging, or computed tomography (showing spinal stenosis, spondylolisthesis or disc herniation). These preoperative examinations were conducted by clinicians. Patients with low back pain unresponsive to conservative treatment for more than 3 months and planned to undergo two-level open lumbar fusion surgery under general anaesthesia (all patients underwent the same type of surgery) were included. The exclusion criteria were as follows: patients who refused to participate or who had cognitive impairment (unable to provide informed consent); other chronic pain conditions (not related to surgical indications); took analgesic drugs before surgery (gabapentinoids and/or NSAIDS) or had a history of opioid abuse; chronic low back pain not due to spinal stenosis, spondylolisthesis; or disc herniation but manifested by one or more specific causes (for example, cancer, fractures, and infections); previously underwent lumbar spine surgery; chronic opioid or gabapentin treatment or a visual analogue scale score of > 3 over the past week (The preoperative pain score of the patients was assessed as a resting state. If the preoperative pain score was > 3, the patients were treated with additional analgesic measures, such as analgesic drugs in the hospital, we excluded patients in this category).
Methods and data acquisition
Patients were evaluated from hospital admission until 3 months after discharge by the same investigator who was blinded to the design of the trial. The evaluator introduced the questionnaire and scoring rules to each patient in detail. The online questionnaire was used to record the clinical information via a tablet. Before surgery, the age, sex, smoking history, body mass index (BMI), operation history, duration of surgery, level of preoperative pain (VAS, the preoperative pain score of the patients was assessed as a resting state), aetiology of back pain (spinal stenosis, spondylolisthesis, or disc herniation), Self-rating Anxiety Scale (SAS), Self-rating Depression Scale (SDS), FRAIL scale, and duration of chronic low back pain were recorded online by an anaesthetis. According to their chronic low back pain duration, the patients could be classified into three groups: duration of pain less than 1 year, one to 5 years, and more than 5 years. We conducted a unified general anaesthesia program. The VAS (ranging from 0 to 10) was used to evaluate the acute postoperative pain (maximum intensity) during the day (VAS day) and night (VAS night) on the first postoperative day after surgery. All patients were treated with postoperative intravenous self-controlled analgesia (PCIA). The PCIA contained 100 μg of sufentanil and 98 mL of saline. The analgesic pump was set as follows: background infusion of sufentanil 2 μg/h, bolus dose of sufentanil 2 μg, and lockout interval 10 min. Patients pressed the PCIA when they experienced pain at rest > 3. If patients still reported pain or greater than 4 on a 0–10 scale on the VAS, supplemental rescue boluses of intravenous flurbiprofen axetil injection of 50 mg were administered. The patient’s analgesic dosage (analgesics for remedy), pain scores on the day of discharge, pain scores after 3 months, and hospital stay were recorded.
Sample size calculation
To achieve a sufficient sample size, we used PASS software to calculate the power. We first conducted a preliminary experiment, and the means of the maximum pain score (VAS) of the three groups (duration of pain less than 1 year, one to 5 years, and more than 5 years) during the day were 2.60, 2.90, and 3.20, respectively. The SDs of the maximum pain score of the three groups during the day were 0.88, 0.85, and 0.83, respectively. The significance level (α) was set at 0.05 and power (1-β) = 0.98. In the one-way ANOVA in PASS software, the sample size required for each group was 79. The mean maximum pain scores (VAS) of the three groups during the night were 3.55, 3.85, and 4.10, respectively. The SDs of the maximum pain score of the three groups during the day were 0.95, 0.88, and 0.85, respectively. The sample size was calculated in the same way, and the number of patients required for each group was 101. Considering a certain loss to follow-up, the sample size of each group was set to 110.
Questionnaire and scores
The preoperative mental state was evaluated on the day before surgery using the Chinese-language versions of the SAS and SDS. The SAS and SDS are self-report questionnaires that provide a comprehensive assessment of the anxiety and depression status of patients [17]. The SAS and the SDS comprise 20 items. Each item is scored on a 4-point scale (1– not at all; 2 –somewhat; 3– moderately so; and 4 – very much so); the total score for each questionnaire is multiplied by 1.25 to convert it into a standardized score (range, 25–100; higher scores indicate higher levels of anxiety and depression) [18].
The VAS (Visual Analogue Score) is a tool used to assess pain levels [19]. It is on a scale ranging from 0 (no pain) to 10 (unimaginable pain), mild (0–3), moderate (4–6) and severe pain (7–10), in which higher scores indicate more pain [20].
The FRAIL scale [21, 22] is a simple tool to evaluate the physical condition and includes five items. It measures fatigue, resistance (ability to climb one flight of stairs), ambulation (ability to walk one block), illness (more than five past or current diagnoses), and weight loss (more than 5%). Each positive response within a domain scored 1 point, yielding a maximum score of 5. Higher scores indicate increased frailty [23].
Statistical analysis
Statistical calculations were performed using IBM SPSS Statistics Version 22. Descriptive analysis was performed to identify the number and percentage of demographic characteristics. Data are shown as the mean ± standard deviation (SD) or number (%). One-way ANOVA and the chi-square test were used to identify the differences among the three groups in the baseline demographic variables (age, sex, BMI, operation history, smoking, level of preoperative pain (VAS), SAS scale, SDS scale, FRAIL scale, duration of surgery, aetiology of back pain). Bivariate correlation analysis [24] (Spearman’s correlation and Pearson’s correlation) was used to estimate the interrelation between some preoperative variables (age, sex, BMI, operation history, smoking, level of preoperative pain (VAS), SAS scale, SDS scale, FRAIL scale, duration of surgery, aetiology of back pain) and the VAS day or VAS night. The independent variables (SAS scale, SDS scale, duration of surgery, aetiology of back pain) with P < 0.1 in the bivariate correlation analysis were included in the binary logistic regression for further analysis. Logistic regression models were used to examine the effect of some independent variables on acute postoperative pain (VAS day and VAS night). According to the degree of postoperative pain scores, we converted the measurement data into dichotomous data [25]. Two separated multivariable logistic regression models were built with VAS day and VAS night as outcome respectively. All possible risk factors were tested in univariate logistic regression and then candidates (with p < 0.20 in univariate logistic regression) put into the multivariable logistic regression model. After the stepwise model selection, only risk factors with p < 0.10 were kept in the final logistic regression model. Odds ratios with 95% confidence intervals were reported based on the regression models. A significant difference between different groups and a significant correlation of variables were set at P < 0.05.
Results
Patient demographics
Age, sex, BMI, level of preoperative pain (VAS), operation history, smoking history, duration of surgery, SAS, SDS, aetiology of back pain, and FRAIL scale were all recorded as the baseline before surgery. Initially, 332 patients consented to participate in this prospective trial but. 1 patient was lost to follow-up and, 1 patient changed to a different surgical procedure. Data from the remaining 330 patients were included in this analysis. The number and percentage of these items were used to describe and measure the patient demographics in the three groups, as shown in Table 1. Except for the level of preoperative pain, SAS, and SDS, the three groups displayed no significant difference in demographic characteristics or clinical information.
Table 1.
Summary statistics of the baseline characteristics
| Variable | Chronic pain duration classification | P value | ||
|---|---|---|---|---|
| < 1 year | 1 ~ 5 years | > 5 years | ||
| (N = 110) | (N = 110) | (N = 110) | ||
| Age, yr (mean ± SD) | 54.48 ± 9.94 | 55.06 ± 10.30 | 56.36 ± 8.68 | 0.320 |
| Female (%) | 67 (60.91) | 64 (58.18) | 69 (62.73) | 0.482 |
| BMI (mean ± SD) | 24.48 ± 3.11 | 24.12 ± 3.77 | 24.03 ± 3.67 | 0.619 |
| Operation history (%) | 0.788 | |||
| 0 | 30 (27.27) | 33 (30.00) | 31 (28.18) | |
| 1 | 47 (42.73) | 41 (37.27) | 46 (41.82) | |
| ≥ 2 | 33 (30.00) | 36 (32.73) | 33 (30.00) | |
| Smoking (%) | 40 (36.36) | 43 (39.09) | 39 (35.45) | 0.359 |
| Level of preoperative pain (VAS) (mean ± SD) | 1.71 ± 0.65 | 1.88 ± 0.69 | 2.07 ± 0.71 | < 0.05* |
| SAS (mean ± SD) | 36.91 ± 6.72 | 40.03 ± 6.59 | 43.25 ± 6.36 | < 0.05* |
| SDS (mean ± SD) | 39.31 ± 7.21 | 42.35 ± 6.83 | 46.25 ± 7.28 | < 0.05* |
| FRAIL (mean ± SD) | 1.71 ± 0.70 | 1.66 ± 0.76 | 1.74 ± 0.75 | 0.760 |
| Duration of surgery, min (mean ± SD) | 121.01 ± 8.69 | 122.99 ± 9.40 | 123.75 ± 10.69 | 0.088 |
| Etiology of back pain(%) | 0.817 | |||
| spinal stenosis | 57 (51.82) | 51 (46.36) | 49 (44.55) | |
| spondylolisthesis | 34 (30.91) | 37 (33.67) | 41 (37.27) | |
| disc herniation | 19 (17.27) | 22 (19.97) | 20 (18.18) | |
One-way ANOVA and chi-square tests were used to identify the differences among the three groups for some variables
BMI Body mass index, VAS Visual analogue scale for pain, SAS Self-rating Anxiety Scale, SDS Self-rating Depression Scale, FRAIL FRAIL scale, SD Standard deviation, yr Year
*P < 0.05; significant difference among the three groups
Bivariate correlation analysis of factors correlated with acute postoperative pain (VAS scores)
Bivariate correlation analysis was employed to assess the relationship between acute postoperative VAS scores (VAS day and VAS night) and the duration of chronic low back pain or other variables. In the bivariate correlation analysis, age, sex, BMI, level of preoperative pain (VAS), operation history, smoking history, duration of surgery, SAS, SDS, FRAIL scale, aetiology of back pain, and duration of chronic low back pain (three groups) were included. Ultimately, the independent variables with P < 0.1 were level of preoperative pain (correlation coefficient: 0.386, P < 0.001), SAS (correlation coefficient: 0.735, P < 0.001), SDS (correlation coefficient: 0.734, P < 0.001), and duration of chronic low back pain (correlation coefficient: 0.460, P < 0.001), which were correlated with VAS day. The independent variables with P < 0.1 were level of preoperative pain (correlation coefficient: 0.391, P < 0.001), SAS (correlation coefficient: 0.766, P < 0.001), SDS (correlation coefficient: 0.799, P < 0.001), and duration of chronic low back pain (correlation coefficient: 0.397, P < 0.001), which were correlated with VAS night (Table 2).
Table 2.
Bivariate analysis of factors correlated with VAS day and VAS night
| Independent variables | Dependent variables | |||
|---|---|---|---|---|
| VAS day | VAS night | |||
| Correlation coefficient | P value | Correlation coefficient | P value | |
| Age | 0.056 | 0.309 | 0.041 | 0.456 |
| Sex | 0.048 | 0.381 | −0.037 | 0.502 |
| BMI | −0.080 | 0.145 | −0.009 | 0.874 |
| Operation history | −0.004 | 0.939 | −0.056 | 0.313 |
| Smoking | −0.0077 | 0.162 | 0.035 | 0.525 |
| Level of preoperative pain (VAS) | 0.386 | < 0.001* | 0.391 | < 0.001* |
| SAS | 0.735 | < 0.001* | 0.766 | < 0.001* |
| SDS | 0.734 | < 0.001* | 0.799 | < 0.001* |
| FRAIL | 0.012 | 0.822 | 0.05 | 0.365 |
| Duration of surgery | 0.064 | 0.245 | 0.102 | 0.064 |
| Chronic pain duration | 0.460 | < 0.001* | 0.397 | < 0.001* |
| Aetiology of back pain | −0.55 | 0.319 | 0.023 | 0.672 |
Spearman’s correlation analysis and Pearson’s correlation analysis were used in the bivariate analyses. There was a significant difference between the independent variables and the dependent variables
*P < 0.1 (n = 330)
BMI Body mass index, VAS Visual analogue scale for pain, SAS Self-rating Anxiety Scale, SDS Self-rating Depression Scale, FRAIL FRAIL scale
Logistic regression model to examine the effect of the variables on acute postoperative pain
In the regression model with VAS day had moderate or severe pain score as outcome, only SAS, SDS, duration of chronic low back pain, BMI and aetiology of back pain are included in the multivariable logistic regression. Although the level of preoperative pain (VAS) showed statistical significance in univariate analysis, but it was not included in the final multivariable model, it could be due to the interactions or correlations among variables. SAS and SDS showed statistical significance in both univariate logistic regression and multivariable logistic regression. After controlling SAS, SDS, BMI, and aetiology of back pain, the duration of chronic low back pain did not show statistical significance. The result is uncertain because the confidence interval included the null after controlling for SAS SDS, BMI, and aetiology of back pain (OR = 2.48, 95% CI: 0.900 to 6.828, p = 0.0789) (Table 3).
Table 3.
Univariate and multivariable logistic regression results with VAS day as outcome
| Risk factors | Univariate logistic regression | Multivariable logistic regression | ||
|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | |
| SAS | 1.581 (1.420, 1.761) | <.0001 | 1.335 (1.149, 1.551) | 0.0002 |
| SDS | 1.487 (1.353, 1.634) | <.0001 | 1.214 (1.070, 1.377) | 0.0026 |
| Chronic pain duration | ||||
| < 1 year (reference) | 1 | NA | 1 | NA |
| 1–5 years | 1.863 (0.921, 3.765) | 0.0833 | 1.053 (0.367, 3.020) | 0.924 |
| > 5 years | 6.333 (3.272, 12.259) | <.0001 | 2.48 (0.900, 6.828) | 0.0789 |
| BMI | 0.951 (0.888, 1.019) | 0.1548 | 0.865 (0.766, 0.977) | 0.0199 |
| Aetiology of back pain | ||||
| Spinal stenosis | 2.453 (1.152, 5.222) | 0.02 | 4.252 (1.314, 13.762) | 0.0157 |
| Spondylolisthesis | 2.364 (1.077, 5.187) | 0.0319 | 5.149 (1.514, 17.512) | 0.0087 |
| Disc herniation (reference) | 1 | NA | 1 | NA |
| Preoperative pain score (VAS) | 2.574 (1.774, 3.734) | <.0001 | ||
| Age | 1.019 (0.994, 1.046) | 0.1379 | ||
| Gender (male) | 0.860 (0.526, 1.405) | 0.5465 | ||
| Duration of surgery | 1.019 (0.995, 1.045) | 0.1274 | ||
| Smoking | 1.166 (0.709, 1.918) | 0.5449 | ||
| Frail | 1.063 (0.768, 1.471) | 0.7134 | ||
| Operation history | 1.025 (0.752, 1.398) | 0.8762 | ||
Variables for the multivariable logistic regression included SAS, SDS, duration of chronic low back pain, BMI and aetiology of back pain
BMI Body mass index, VAS Visual analogue scale for pain, SAS Self-rating Anxiety Scale, SDS Self-rating Depression Scale, FRAIL FRAIL scale, CI Confidence interval, OR Odds ratio, NA Not available
The model for VAS night is a little bit different. Only SAS, SDS, and duration of chronic low back pain are included in the multivariable logistic regression. Again, the level of preoperative pain (VAS) showed statistical significance in univariate analysis, but it was not included in the final multivariable model. SAS and SDS still showed statistical significance in both univariate logistic regression and multivariable logistic regression. After controlling SAS and SDS, the duration of chronic low back pain is showed statistically significant. Patients with a duration of chronic low back pain of more than 5 years were more likely having moderate to severe acute postoperative pain (VAS > 3) compared to patients with a duration of chronic low back pain less than 1 year (OR = 3.546, 95% CI: 1.405 to 8.95, p = 0.0074) (Table 4).
Table 4.
Univariate and multivariable logistic regression results with VAS night as outcome
| Risk factors | Univariate logistic regression | Multivariable logistic regression | ||
|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | |
| SAS | 1.579 (1.429, 1.746) | <.0001 | 1.273 (1.112, 1.457) | 0.0005 |
| SDS | 1.488 (1.372, 1.614) | <.0001 | 1.244 (1.109, 1.396) | 0.0002 |
| Chronic pain duration | ||||
| < 1 year (reference) | 1 | NA | 1 | NA |
| 1–5 years | 1.803 (1.055, 3.080) | 0.0311 | 1.069 (0.453, 2.522) | 0.8781 |
| > 5 years | 7.011 (3.781, 13.002) | <.0001 | 3.546 (1.405, 8.951) | 0.0074 |
| BMI | 1.004 (0.943, 1.068) | 0.908 | ||
| Aetiology of back pain | ||||
| Spinal stenosis | 0.924 (0.511, 1.671) | 0.7925 | ||
| Spondylolisthesis | 1.389 (0.737, 2.617) | 0.3099 | ||
| Disc herniation (reference) | 1 | NA | ||
| Preoperative pain score (VAS) | 2.962 (2.064, 4.253) | <.0001 | ||
| Age | 0.996 (0.973, 1.018) | 0.7013 | ||
| Gender (male) | 1.325 (0.844, 2.081) | 0.221 | ||
| surgery time | 1.018 (0.995, 1.041) | 0.1349 | ||
| smoking 0 | 0.707 (0.447, 1.118) | 0.1381 | ||
| Frail | 1.098 (0.814, 1.481) | 0.5404 | ||
| Operation history | 0.898 (0.676, 1.195) | 0.4615 | ||
Variables for the multivariable logistic regression included SAS, SDS, and duration of chronic low back pain
BMI Body mass index, VAS Visual analogue scale for pain, SAS Self-rating Anxiety Scale, SDS Self-rating Depression Scale, FRAIL FRAIL scale, CI Confidence interval, OR Odds ratio, NA Not available
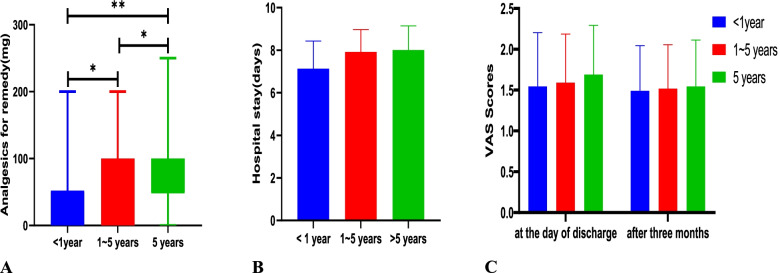
Except for the consumption of analgesics after surgery (Fig. 1A, P < 0.05), hospital stay (Fig. 1B), pain scores at the day of discharge and after 3 months displayed no significant difference (Fig. 1C) among the three groups.
Fig. 1.
Consumption of postoperative analgesics, hospital stay, pain scores at the day of discharge and after three months among the three groups. Comparisons among groups were performed using analysis of variance and the Kruskal–Wallis test. **indicates P < 0.001, * indicates P < 0.05
Discussion
The purpose of this study was to examine whether the duration of chronic low back pain before lumbar fusion surgery affected patients’ postoperative pain, consumption of analgesic drugs and hospital stay. The results of our study indicated that the duration of chronic low back pain affected patients’ acute postoperative pain and consumption of analgesic drugs. Postoperative pain is the main factor affecting the functional recovery of patients after surgery [26, 27]. At present, the focus is more on the prevention and treatment of postoperative acute pain [28], often neglecting the impact of preoperative chronic pain on postoperative pain and functional recovery. Chronic pain before surgery causes a series of problems for patients after surgery. Preoperative chronic pain was shown to distract people’s attention before surgery and reduced their recovery of attention and memory abilities during the follow-up period after surgery among nonelderly patients [29].
Doctors have begun to pay more attention to the impact of chronic pain before surgery on postoperative recovery. A prospective study of postoperative pain and functional recovery of patients undergoing hip replacement surgery found that patients with chronic pain other than hip-related pain had slower postoperative mobilization, worse physical function, and greater psychological distress after surgery [15]. Regarding pain sensitivity, researchers have pointed out that patients with chronic low back pain before surgery showed increased sensitivity to pain and decreased sensitivity to harmless stimuli [30], and patients with a history of low back pain had decreased pain tolerance [31]. In a study of the correlation between chronic pain and pain sensitivity, Joachim Erlenwein and his colleagues [32] found that patients with chronic pain had a higher intensity of zoster-related acute pain. However, there is no relevant research on whether the duration of chronic pain affects postoperative pain, consumption of analgesic drugs, or hospital stay. This observational study was the first to report the relationship between the duration of chronic low back pain and acute postoperative pain measured by VAS scores. This study found that the longer the duration of chronic low back pain was, the higher the incidence of moderate to severe acute postoperative pain and the more analgesic drugs were consumed.
Intervertebral disc degeneration is considered to be the main cause of chronic low back pain [33]. Degenerated intervertebral discs contain high levels of proinflammatory mediators and cytokines [34, 35]. Secondary osteoarthritis with or without synovial facets is the main source of chronic low back pain. Long-term inflammation can lead to chronic pain. At the same time, these inflammatory mediators can also reduce the pain threshold of patients [36]. We believe that the impact of chronic pain duration on the acute postoperative pain of lumbar fusion surgery may be related to the duration of chronic inflammation. In a trial [12] that studied obesity and postoperative pain sensitivity, it was found that obese patients had higher pain sensitivity, which may be related to macrophages. Macrophage accumulation is related to the release of inflammatory mediators. Obese patients have more macrophages than nonobese patients, which may help reduce the pain threshold of obese patients [37]. Chronic inflammation is a long-term accumulation process. The longer the duration of chronic pain is, the higher the pain sensitivity after lumbar fusion surgery, which may be related to the release of more inflammatory mediators in these patients.
Another reason may be that the duration of chronic pain is related to different mental and psychological effects on patients. Chronic pain is often accompanied by psychosocial complications [38]. Preoperative anxiety levels were associated with the efficacy of pain management after knee surgery [14], and the more severe the preoperative anxiety was, the greater the need for analgesia was [39]. Our research also shows that the longer the duration of CLBP, the higher the degree of anxiety and depression in patients. Chronic pain can lead to the development and aggravation of anxiety disorders, whereas anxiety disorders can lead to increased pain duration and intensity [40]. This shows that chronic pain has a series of effects on the patient’s emotions and psychology. The longer the chronic pain lasts, the more likely it is that the patient will have symptoms, such as anxiety.
Research [41] has found changes in anxiety and depression was associated with pain severity undergoing lower-extremity total joint arthroplasty. This was consistent with our conclusion. However, for some previously reported factors associated with pain sensitivity such as female sex [42], history of tobacco use [43], our results did not suggest an association.
However, this study also has some limitations. First, as lumbar disc herniation is a naturally occurring disease related to the patient’s lifestyle, the duration of chronic low back pain, which is provided by patients, may not be accurate and thus this might undermine the results. Therefore, we also specifically divided the chronic pain time into three groups to reduce the impact of this potentially inaccurate information on the results. Second, there were other important factors (e.g., disability, education, living status, insurance claims) not reported in our study, and these factors may be associated with acute postoperative pain intensity. Third, this is a single-centre, relatively small population trial, and a multicentre trial is necessary to verify the results.
Conclusion
For patients with a history of chronic low back pain who underwent lumbar fusion surgery, the longer the preoperative pain lasted, the higher the incidence of moderate to severe acute postoperative pain and the more analgesic drugs required after surgery. Therefore, it is very important to pay attention to patients’ chronic pain before surgery, especially the duration of chronic pain. Patients with long-lasting chronic pain should undergo stricter analgesia treatment supervision after surgery to prevent them from suffering from more severe pain.
Author details
Department of Anaesthesiology, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, Anhui, 230,036, China.
All coauthors of this work are very grateful to the clinical staff at the Department of Anaesthesiology, The First Affiliated Hospital of USTC, Hefei, Anhui, China, for their support and kind help.
Abbreviations
- BMI
Body mass index
- VAS
Visual analogue scale for pain
- SAS
Self-rating Anxiety Scale
- SDS
Self-rating Depression Scale
- FRAIL
FRAIL scale
- SD
Standard deviation
Authors’ contributions
MPQ and MRD were responsible for designed this study and collected the data. MPQ was responsible for study execution and manuscript writing. JL and FK revised it critically. All authors have read and approved the final version of the manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request. The datasets will be available at www.chictr.org.cn 6 months after publication.
Declarations
Ethics approval and consent to participate
This study was registered at the Chinese Clinical Trial Registration Center (ChiCTR2000029923, date of registration: 2020-02-16). This study was conducted in accordance with the Declaration of Helsinki and was approved by the Chinese Ethics Committee of Registering Clinical Trials (ChiECRCT20200165, address: West China Hospital, Sichuan University, No. 37, Guo Xue Xiang, Chengdu, Sichuan, China). Written informed consent was obtained from all participating patients.
Consent for publication
Not applicable.
Competing interests
All authors have no conflicts of interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ko S, Chae S. Correlations between the SF-36, the Oswestry-disability index and Rolland-Morris disability questionnaire in patients undergoing lumbar decompression according to types of spine origin pain. Clin Spine Surg. 2017;30(6):E804–E808. doi: 10.1097/BSD.0000000000000438. [DOI] [PubMed] [Google Scholar]
- 2.Snidvongs S, Taylor RS, Ahmad A, Thomson S, Sharma M, Farr A, Fitzsimmons D, Poulton S, Mehta V, Langford R. Facet-joint injections for non-specific low back pain: a feasibility RCT. Health Technol Assess. 2017;21(74):1–+. doi: 10.3310/hta21740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costa LDM, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LOP. The prognosis of acute and persistent low-back pain: a meta-analysis. Can Med Assoc J. 2012;184(11):E613–E624. doi: 10.1503/cmaj.111271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.VanDenKerkhof EG, Peters ML, Bruce J. Chronic pain after surgery time for standardization? A framework to establish Core risk factor and outcome domains for epidemiological studies. Clin J Pain. 2013;29(1):2–8. doi: 10.1097/AJP.0b013e31824730c2. [DOI] [PubMed] [Google Scholar]
- 5.Dai F, Belfer I, Schwartz CE, Banco R, Martha JF, Tighioughart H, Tromanhauser SG, Jenis LG, Kim DH. Association of catechol-O-methyltransferase genetic variants with outcome in patients undergoing surgical treatment for lumbar degenerative disc disease. Spine J. 2010;10(11):949–957. doi: 10.1016/j.spinee.2010.07.387. [DOI] [PubMed] [Google Scholar]
- 6.Forsth P, Olafsson G, Carlsson T, Frost A, Borgstrom F, Fritzell P, Ohagen P, Michaelsson K, Sanden B. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med. 2016;374(15):1413–1423. doi: 10.1056/NEJMoa1513721. [DOI] [PubMed] [Google Scholar]
- 7.Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine. 2019;44(5):369–376. doi: 10.1097/BRS.0000000000002822. [DOI] [PubMed] [Google Scholar]
- 8.Lotzke H, Jakobsson M, Brisby H, Gutke A, Hägg O, Smeets R, den Hollander M, Olsson LE, Lundberg M. Use of the PREPARE (PREhabilitation, Physical Activity and exeRcisE) program to improve outcomes after lumbar fusion surgery for severe low back pain: a study protocol of a person-centred randomised controlled trial. BMC musculoskeletal disorders. 2016;17(1):349. [DOI] [PMC free article] [PubMed]
- 9.Maheshwari K, Avitsian R, Sessler DI, Makarova N, Tanios M, Raza S, Traul D, Rajan S, Manlapaz M, Machado S, et al. Multimodal analgesic regimen for spine surgery a randomized placebo-controlled trial. Anesthesiology. 2020;132(5):992–1002. doi: 10.1097/ALN.0000000000003143. [DOI] [PubMed] [Google Scholar]
- 10.Tan M, Law LS-C, Gan TJ. Optimizing pain management to facilitate enhanced recovery after surgery pathways. Can J Anesth. 2015;62(2):203–218. doi: 10.1007/s12630-014-0275-x. [DOI] [PubMed] [Google Scholar]
- 11.Wise EA, Price DD, Myers CD, Heft MW, Robinson ME. Gender role expectations of pain: relationship to experimental pain perception. Pain. 2002;96(3):335–342. doi: 10.1016/S0304-3959(01)00473-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Majchrzak M, Brzecka A, Daroszewski C, Błasiak P, Rzechonek A, Tarasov VV, Chubarev VN, Kurinnaya AS, Melnikova TI, Makhmutova A et al: Increased Pain Sensitivity in Obese Patients After Lung Cancer Surgery. Front Pharmacol. 2019;10:626. [DOI] [PMC free article] [PubMed]
- 13.Jain N, Phillips FM, Weaver T, Khan SN. Preoperative chronic opioid therapy a risk factor for complications, readmission, continued opioid use and increased costs after one- and two-level posterior lumbar fusion. Spine. 2018;43(19):1331–1338. doi: 10.1097/BRS.0000000000002609. [DOI] [PubMed] [Google Scholar]
- 14.Thomazeau J, Rouquette A, Martinez V, Rabuel C, Prince N, Laplanche J-L, Nizard R, Bergmann J-F, Perrot S, Lloret-Linares C. Predictive factors of chronic post-surgical pain at 6 months following knee replacement: influence of postoperative pain trajectory and genetics. Pain Physician. 2016;19(5):E729–E741. [PubMed] [Google Scholar]
- 15.Erlenwein J, Przemeck M, Degenhart A, Budde S, Falla D, Quintel M, Pfingsten M, Petzke F. The influence of chronic pain on postoperative pain and function after hip surgery: a prospective observational cohort study. J Pain. 2016;17(2):236–247. doi: 10.1016/j.jpain.2015.10.013. [DOI] [PubMed] [Google Scholar]
- 16.Boyle JK, Anthony IC, Jones BG, Wheelwright EF, Blyth MJG. Influence of low back pain on total knee arthroplasty outcome. Knee. 2014;21(2):410–414. doi: 10.1016/j.knee.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 17.Zung WWK, Richards CB, Short MJ. Self-rating depression scale in an outpatient clinic - further validation of SDS. Arch Gen Psychiatry. 1965;13(6):508. doi: 10.1001/archpsyc.1965.01730060026004. [DOI] [PubMed] [Google Scholar]
- 18.Yin W, Pang L, Cao X, McGoogan JM, Liu M, Zhang C, Li Z, Li J, Rou K. Factors associated with depression and anxiety among patients attending community-based methadone maintenance treatment in China. Addiction. 2015;110:51–60. doi: 10.1111/add.12780. [DOI] [PubMed] [Google Scholar]
- 19.Hirschfeld G, Zernikow B. Cut points for mild, moderate, and severe pain on the VAS for children and adolescents: what can be learned from 10 million ANOVAs? Pain. 2013;154(12):2626–2632. doi: 10.1016/j.pain.2013.05.048. [DOI] [PubMed] [Google Scholar]
- 20.Ferster APOC, Hu A. Perceptions of pain of laryngeal electromyography. Laryngoscope. 2018;128(4):896–900. doi: 10.1002/lary.26860. [DOI] [PubMed] [Google Scholar]
- 21.Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi: 10.1007/s12603-012-0084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gleason LJ, Benton EA, Alvarez-Nebreda ML, Weaver MJ, Harris MB, Javedan H. FRAIL questionnaire screening tool and Short-term outcomes in geriatric fracture patients. J Am Med Dir Assoc. 2017;18(12):1082–1086. doi: 10.1016/j.jamda.2017.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Susano MJ, Grasfield RH, Friese M, Rosner B, Crosby G, Bader AM, Kang JD, Smith TR, Lu Y, Groff MW, et al. Brief preoperative screening for frailty and cognitive impairment predicts delirium after spine surgery. Anesthesiology. 2020;133(6):1184–1191. doi: 10.1097/ALN.0000000000003523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126(5):1763–1768. doi: 10.1213/ANE.0000000000002864. [DOI] [PubMed] [Google Scholar]
- 25.Slater H, Paananen M, Smith AJ, O'Sullivan P, Briggs AM, Hickey M, Mountain J, Karppinen J, Beales D. Heightened cold pain and pressure pain sensitivity in young female adults with moderate-to-severe menstrual pain. Pain. 2015;156(12):2468–2478. doi: 10.1097/j.pain.0000000000000317. [DOI] [PubMed] [Google Scholar]
- 26.Kehlet H. Postoperative pain, analgesia, and recovery-bedfellows that cannot be ignored. Pain. 2018;159(9):S11–S16. doi: 10.1097/j.pain.0000000000001243. [DOI] [PubMed] [Google Scholar]
- 27.Andersen LO, Gaarn-Larsen L, Kristensen BB, Husted H, Otte KS, Kehlet H. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia. 2009;64(5):508–513. doi: 10.1111/j.1365-2044.2008.05831.x. [DOI] [PubMed] [Google Scholar]
- 28.Azim S, Nicholson J, Rebecchi MJ, Galbavy W, Feng T, Reinsel R, Volkow ND, Benveniste H, Kaczoche M. Endocannabinoids and acute pain after total knee arthroplasty. Pain. 2015;156(2):341–347. doi: 10.1097/01.j.pain.0000460315.80981.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gu H, Deng X, Lv Y, Chen Q, Yu W. Preoperational chronic pain impairs the attention ability before surgery and recovery of attention and memory abilities after surgery in non-elderly patients. J Pain Res. 2019;12:151–158. doi: 10.2147/JPR.S178118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meints SM, Mawla I, Napadow V, Kong J, Gerber J, Chan S-T, Wasan AD, Kaptchuk TJ, McDonnell C, Carriere J, et al. The relationship between catastrophizing and altered pain sensitivity in patients with chronic low-back pain. Pain. 2019;160(4):833–843. doi: 10.1097/j.pain.0000000000001461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alfieri FM, Souto Lima AR, Battistella LR, de Oliveira Vargas e Silva NC. Superficial temperature and pain tolerance in patients with chronic low back pain. J Bodyw Mov Ther. 2019;23(3):583–587. doi: 10.1016/j.jbmt.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Erlenwein J, Thoms K-M, Brandebusemeyer F, Pfingsten M, Mansur A, Quintel M, Schoen MP, Petzke F. Pre-existing chronic pain influences the severity of acute herpes zoster pain-a prospective observational cohort study. Pain Med. 2016;17(7):1317–1328. doi: 10.1093/pm/pnv116. [DOI] [PubMed] [Google Scholar]
- 33.Willems PC. Provocative diskography: safety and predictive value in the outcome of spinal fusion or pain intervention for chronic low-back pain. J Pain Res. 2014;7:699–705. doi: 10.2147/JPR.S45615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kang JD, StefanovicRacic M, McIntyre LA, Georgescu HI, Evans CH. Toward a biochemical understanding of human intervertebral disc degeneration and herniation - contributions of nitric oxide, interleukins, prostaglandin E-2, and matrix metalloproteinases. Spine. 1997;22(10):1065–1073. doi: 10.1097/00007632-199705150-00003. [DOI] [PubMed] [Google Scholar]
- 35.Kang JD, Georgescu HI, McIntyreLarkin L, StefanovicRacic M, Donaldson WF, Evans CH. Herniated lumbar intervertebral discs spontaneously produce matrix metalloproteinases, nitric oxide, interleukin-6, and prostaglandin E (2) Spine. 1996;21(3):271–277. doi: 10.1097/00007632-199602010-00003. [DOI] [PubMed] [Google Scholar]
- 36.Jensen KB, Loitoile R, Kosek E, Petzke F, Carville S, Fransson P, Marcus H, Williams SC, Choy E, Mainguy Y, et al. Patients with fibromyalgia display less functional connectivity in the brain's pain inhibitory network. Mol Pain. 2012;8:32. [DOI] [PMC free article] [PubMed]
- 37.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Investig. 2003;112(12):1796–1808. doi: 10.1172/JCI200319246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Skeppholm M, Fransson R, Hammar M, Olerud C. The association between preoperative mental distress and patient-reported outcome measures in patients treated surgically for cervical radiculopathy. Spine J. 2017;17(6):790–798. doi: 10.1016/j.spinee.2016.02.037. [DOI] [PubMed] [Google Scholar]
- 39.Stamenkovic DM, Rancic NK, Latas MB, Neskovic V, Rondovic GM, Wu JD, Cattano D. Preoperative anxiety and implications on postoperative recovery: what can we do to change our history. Minerva Anestesiol. 2018;84(11):1307–1317. doi: 10.23736/S0375-9393.18.12520-X. [DOI] [PubMed] [Google Scholar]
- 40.Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K. Association of Depression and Anxiety Alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 2008;70(8):890–897. doi: 10.1097/PSY.0b013e318185c510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hassett AL, Marshall E, Bailey AM, Moser S, Clauw DJ, Hooten WM, Urquhart A, Brummett CM. Changes in anxiety and depression are mediated by changes in pain severity in patients undergoing lower-extremity Total joint arthroplasty. Reg Anesth Pain Med. 2018;43(1):14–18. doi: 10.1097/AAP.0000000000000682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yoon S, Hong WP, Joo H, Kim H, Park S, Bahk JH, Lee HJ. Long-term incidence of chronic postsurgical pain after thoracic surgery for lung cancer: a 10-year single-center retrospective study. Reg Anesth Pain Med. 2020;45(5):331–336. doi: 10.1136/rapm-2020-101292. [DOI] [PubMed] [Google Scholar]
- 43.Khan JS, Sessler DI, Chan MTV, Wang CY, Garutti I, Szczeklik W, Turan A, Busse JW, Buckley DN, Paul J, et al. Persistent incisional pain after noncardiac surgery: an international prospective cohort study. Anesthesiology. 2021;135(4):711–723. doi: 10.1097/ALN.0000000000003951. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request. The datasets will be available at www.chictr.org.cn 6 months after publication.