Abstract
Cancer-associated fibroblasts (CAFs) are critical components of the tumor microenvironment (TME) with diverse functions such as extracellular matrix (ECM) remodeling, modulation of metabolism and angiogenesis, and crosstalk with both cancer cells and infiltrating immune cells by production of growth factors, cytokines, and chemokines. Within the TME milieu, CAFs exhibit morphological and functional transitions with relatively specific markers and hold tremendous potential to facilitate tumorigenesis, development, and resistance towards multiple therapeutic strategies including chemotherapy, radiotherapy, targeted therapy, anti-angiogenesis therapy, immunotherapy, and endocrine therapy. Accordingly, CAFs themselves and the downstream effectors and/or signaling pathways are potential targets for optimizing the sensitivity of anti-cancer therapies. This review aims to provide a detailed landscape of the role that CAFs play in conferring therapeutic resistance in different cancers and the underlying mechanisms. The translational and therapeutic perspectives of CAFs in the individualized treatment of malignant tumors are also discussed.
Keywords: Cancer-associated fibroblast (CAF), Tumor microenvironment (TME), Resistance, Chemotherapy, Immunotherapy
Introduction
Cancer cells undergo uncontrolled proliferation and tendency of metastasis and therapeutic resistance owing to the support from complex tissue organizations in the tumor microenvironment (TME). The formation of these malignant phenotypes depends on both the genomic changes of cancer cells and the microenvironment suitable for their growth. The dynamic interactions between the tumor and TME profoundly influence the disease development and prognosis. In general, TME consists of cancer cells and heterogeneous nonmalignant constituents including fibroblasts, pericytes, immune cells, inflammatory cells, as well as soluble factors [1]. Activated fibroblasts, also known as cancer-associated fibroblasts (CAFs), are one of the well-recognized components of TME. Within the TME milieu, CAFs exhibit morphological and functional transitions and hold the tremendous potential to promote cancer progression as well as resistance to multiple therapeutics [2]. In this review, a thorough understanding of tumor and CAF crosstalk will be discussed. The functional role that CAFs play in conferring therapeutic resistance in different cancers and the underlying mechanisms have been exploited. The potential of novel markers for CAF-directed anticancer strategies will also be discussed.
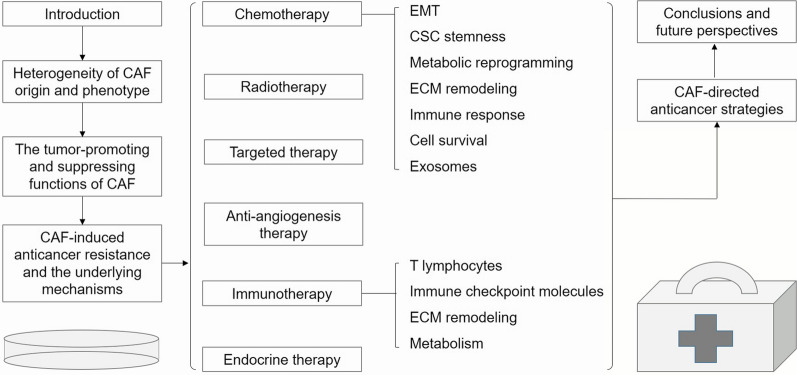
The outline of this review is shown in Fig. 1.
Fig. 1.
The outline of the manuscript. CAF cancer-associated fibroblast; CSC cancer stem cell; ECM extracellular matrix; EMT epithelial-mesenchymal transition
Heterogeneity of CAF origin and phenotype
Emerging evidence indicates that CAFs originate from structural and functional alternations of heterogeneous cell populations upon the influence of various intrinsic and extrinsic factors. Tissue-resident fibroblasts, bone marrow-derived mesenchymal stem cells (MSCs), epithelial, and endothelial cells might transform into CAFs through transforming growth factor-β (TGF-β), epithelial-mesenchymal transition (EMT), or endothelial-mesenchymal transition (EndMT) [3]. CAFs can also evolve from the transdifferentiation of adipocytes or pericytes which leads to the upregulation of mesenchymal lineage-committed genes, such as RUNX2 and PPARγ [4]. Moreover, vitamin deficiency in stromal cells might induce the upregulation of α-SMA and the differentiation into CAFs. In addition, CAFs can be derived from a variety of precursor cells recruited by cancer cells at both primary and metastatic sites including cancer stem cells (CSCs) [5].
Apart from the original heterogeneity, the diverse sources of CAF activation impact phenotypic heterogeneity. Histologically, the activated CAFs are spindled in shape with prominent nucleoli, rough endoplasmic reticulum, Golgi apparatus, gap junctions, and cytoplasmic myofilaments [6]. At this stage, the activated cells often show the expression of a broad range of distinct biological markers in a context-specific manner. Of note, although not exclusive to CAFs, the expression pattern of some surface markers such as alpha-smooth muscle actin (α-SMA), ferroptosis suppressor protein 1 (FSP1), secreted protein acidic and rich in cysteine (SPARC), platelet-derived growth factor β (PDGFβ), and integrin α 11, can be useful in the identification of CAFs [7].
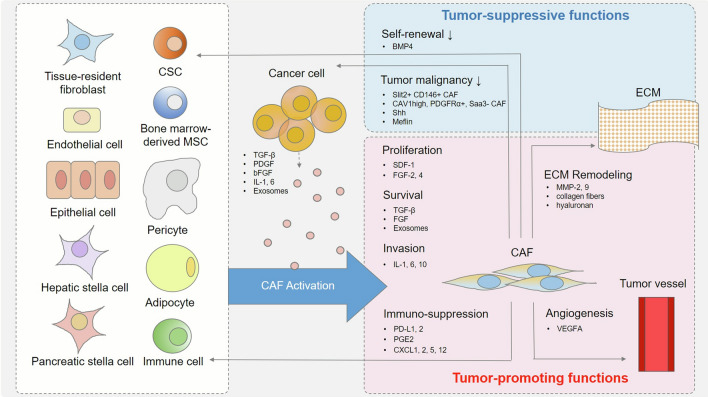
The tumor-promoting and suppressing functions of CAF
The primary role of CAFs is to remodel and regenerate the tissues in a highly-regulated, coordinating pattern. In the context of TME, CAFs facilitate tumorigenesis and cancer development by creating a pro-inflammatory, immuno-suppressive, and oxygen-rich microenvironment [8]. At the early stage of tumorigenesis, tumor-derived interleukin-1β induces CAF activation to orchestrate tumor-promoting inflammation in an NF-κB-dependent manner [9]. Furthermore, the immunosuppressive character of CAFs promotes tumor growth by facilitating immune evasion [10]. Some of the CAF subsets can deactivate the immune system directly by the expression of programmed death-ligand (PD-L)1/2 or the secretion of prostaglandin E2, an immunosuppressive factor that reduces the activation of T cells and NK cells [11]. Besides the direct effect on immune cells, CAFs take part in constructing extracellular matrix (ECM) protein networks that serve as a physical barrier for therapeutic drugs, as well as immune cells, from reaching the tumor [12]. Hypoxia is another well-known feature in the formation of the tumorigenic TME. In this context, CAFs often have upregulated expression of hypoxia-induced angiogenesis regulator (HIAR), which can increase CAF motility and secretion of vascular endothelial growth factor A (VEGFA) and further promote angiogenesis, thereby facilitating oxygenation and nutrient flow of the tumor [13].
In addition to their tumor-promoting role, CAFs are also involved in tumor suppression in some cases. For example, it is discovered that CAF ablation in genetically engineered mouse models of pancreatic ductal adenocarcinoma (PDAC) results in poorly differentiated tumors and shortened survival, indicating that sonic hedgehog (Shh)-driven CAFs can restrain tumor growth progression [14, 15]. Findings in bladder cancer and colon cancer also suggest that the Shh-Smo signaling-dependent CAFs are a source of urothelial differentiation factors [16, 17]. Further studies demonstrate that depletion of CAFs leads to invasive tumors and decreased survival in vivo with increased numbers of CSCs [18]. More recently, CD146 + CAFs, CAV1high CAFs, and PDGFRα + Saa3- CAFs have been identified as tumor-suppressive CAF subsets in breast cancer [19]. Slit2 + and CD146 + CAFs suppress tumorigenesis and increase chemosensitivity, while molecules such as BMP4 reduce the self-renewal of stem-like cancer cells [20]. Meflin, a marker of MSCs, is recently identified as a functional contributor to cancer-restraining CAFs that counteract cancer-promoting CAFs in PDAC [21].
The original and functional heterogeneity of CAFs in tumor progression is shown in Fig. 2.
Fig. 2.
The original and functional heterogeneity of CAFs in tumor progression. CAFs originate from structural and functional alternations of heterogeneous cell populations upon the influence of various intrinsic and extrinsic factors. CAFs can either promote (red section) or suppress (blue section) cancer progression through multiple mechanisms by secreting numerous cell growth factors, cytokines, and chemokines. BMP bone morphogenetic protein; CAF cancer-associated fibroblast; CSC cancer stem cell; CXCL C-X-C motif chemokine ligand; FGF fibroblast growth factor; IDO indoleamine 2,3-dioxygenase; IL interleukin; MMP matrix metallopeptidase; MSC mesenchymal stem cell; PDGF platelet-derived growth factor; PD-L1 programmed cell death ligand 1; PGE2 prostaglandin E2; TGF transforming growth factor; VEGF vascular endothelial growth factor
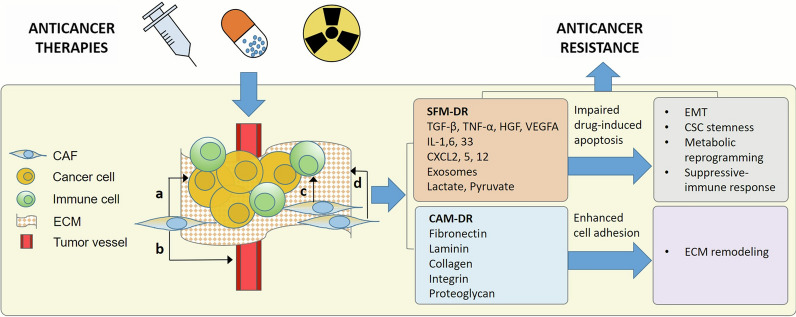
CAF-induced anticancer resistance and the underlying mechanisms
As mentioned above, CAFs are highly interrelated with sensitivity to anticancer therapies. According to the taxonomy raised by Meads et al., CAF-mediated drug resistance can be broadly divided into soluble and secretory factor-mediated drug resistance (SFM-DR) and cell adhesion-mediated drug resistance (CAM-DR) [22]. The SFM-DR is mediated by CAF-produced cytokines, chemokines, growth factors, exosomes, and desmoplastic reactions, which protect cancer cells against drug-induced apoptosis, while the CAM-DR is mediated by the adhesion of cancer cell integrins to stromal fibroblasts or to components of the ECM, such as fibronectin, collagen, and laminin. On the one hand, with the help of the paracrine regulatory factors including cytokines (TGF-β, TNF-α, IL-1, etc.), chemokines, and growth factors secreted by CAFs and cancer cells, CAFs facilitate in architecting a milieu feasible for tumor angiogenesis, metastasis, and therapeutic resistance, hence favoring tumor growth [23]. On the other hand, as the main component of the TME, CAFs act as a therapeutic barrier to prevent anticancer drugs as well as immune cell infiltration in solid cancer treatment [24].
The mechanisms by which CAFs are involved in anticancer resistance are shown in Fig. 3.
Fig. 3.
CAF-induced anticancer resistance. CAFs interact with cancer cells, immune cells, ECM, and tumor vessels in the TME, mediating drug resistance through either secretory factors or direct cell adhesion. a alternative pathways activating; b revascularization; c immunosuppression; d ECM remodeling. CAF cancer-associated fibroblast; CAM-DR cell adhesion-mediated drug resistance; CSC cancer stem cell; CXCL C–X–C motif chemokine ligand; EMT epithelial-mesenchymal transition; HGF hepatocyte growth factor; SFM-DR soluble and secretory factor-mediated drug resistance; TGF transforming growth factor; TNF tumor necrosis factor; VEGF vascular endothelial growth factor
TGF-β is an extensively-studied, ubiquitously-expressed cytokine that plays a crucial role in tumor-stroma crosstalk. During the process of cancer progression, the dichotomous effect of CAFs is mainly manifested as an inhibitory factor in the early stage and a promoter in the advanced stage via the induction of diverse changes in CAFs, as well as the consequent secretion of diverse growth factors and cytokine including TGF-β [25]. CAF-induced drug resistance aided by TGF-β signaling will be described further in the corresponding sections underneath.
Chemotherapy
Chemoresistance, both acquired and primary, is proven to be associated with complex multifactorial processes such as increased drug efflux, reduced drug uptake, activation of pro-survival signaling and defective apoptosis, acquisition of EMT and CSC-like properties, epigenetic modulation, as well as the interaction with the TME, especially CAFs [26].
CAF and EMT
EMT is a reversible process regulated by several EMT-related transcription factors (EMT-TFs) including ZEB, Snail, Slug, and Twist. Existing data suggest that the expression of EMT-TFs by CAFs is required for the paracrine stimulus on the adjacent cancer cells and is one of the critical factors involved in the development of chemoresistance [27]. For instance, in colon cancer, the expression of EMT-TF Snail1 in tumor stroma is correlated with similar expression levels in cancer cells, thereby promoting chemoresistance in cancer cells through EMT [28]. In PDAC, the EMT driver protein ZEB1 expression in CAFs is closely associated with prognosis as the only independent factor of survival after resection [29]. In breast cancer, TGF-β-induced CAFs upregulate the expression of EMT-TF Twist1 in the adjacent ER-positive cancer cells, influencing the aggressiveness and outcome of ER-positive breast cancers [30]. In another instance, CAF-secreted TGF-β1 increases the aggressiveness of breast cancer cells by activating the TGF-β/Smad signaling pathway, accompanied by enhanced migratory potential, invasiveness, as well as increased expression of mesenchymal markers such as MMP 2 and 9, vimentin, and fibronectin [31]. In ovarian cancer, TGF-β-induced CAFs instigate VCAN gene expression and EMT process, facilitating cancer cell motility, invasion, and drug resistance [32]. TGF-β can also regulate the expression of matrix metalloproteinases (MMPs), which are the key factors involved in EMT-related chemoresistance [33]. After being proteolytically activated by MMPs, TGF-β activates CAFs and further promotes fibrosis perpetuation as well as MMP expression and secretion [34]. In bladder cancer, CAF-derived TGF-β1 induces the expression of EMT-specific markers, such as ZEB2 proteins, in cancer cells and increases cancer invasiveness through ZEB2NAT transcript [35].
CAF and CSC stemness
CSCs are cancer cells with the capabilities of self-renewal, differentiation, clonal-tumor induction, and tumor immortalization [36]. The most important functions of CSCs are their role in resistance to multiple anticancer therapies and the repopulation of cancer cells after the treatment. Accumulating evidence indicates that with the stimulation of chemotherapy drugs, a variety of cytokines and chemokines derived from CAFs will participate in CSC maintenance, further promoting drug resistance. It has been reported that human CAFs treated with chemotherapeutic drugs induce CSC self-renewal and tumor growth in vivo with the concurrent release of cytokine IL-17 A in colorectal cancer [37]. In response to the chemotherapeutic treatment, the upregulated TGF-β signaling in the CAFs supports the tumor-initiating potential of CSCs, while TGF-β suppression blocks tumor-stroma crosstalk and leads to the attenuation of cancer progression [38]. In gastric cancer, CAFs increase the self-renewal of CSCs by secretion of neuregulin1 (NRG1) and activation of the downstream NF-κB signaling pathway, giving rise to enhanced proliferation and drug resistance to doxorubicin [39, 40]. Interestingly, it is demonstrated that EMT induction is often accompanied by the generation and amplification of CSCs. In prostate cancer, the switch from non-CSCs to CSCs, as well as chemoresistance, can be triggered by a hypomethylating event at CpG islands that induces the activation of genes involved in the main pathways of cell stemness, such as Hedgehog, Wnt, and NOTCH. CAF-induced hypomethylation of CGIs is correlated with the induction of EMT and stemness [41].
CAF and metabolic reprogramming
Cancer metabolism is identified as one of the hallmarks of cancer [8]. Current findings indicate that CAFs facilitate cancer therapeutic resistance via the exchange of several metabolites and accelerations of specific programs on differentiation or metabolic switches [42]. For instance, the breast cancer cells could induce multidrug resistance mediator GPER translocation in CAFs, stimulating a novel estrogen/GPER/PKA/CREB signaling activation, thereby contributing to glycolytic CAFs for the production of energy-enriched pyruvate and lactate. The energy metabolic coupling between catabolic CAFs and anabolic cancer cells confers the breast cancer cells with multi-drug resistance by increasing mitochondrial activity [43]. Particularly, the lactate released by CAFs confers lower extracellular pH in the TME, which is associated with doxorubicin and paclitaxel resistance as well as the higher migratory potential of cancer cells [44]. In the case of prostate cancer, docetaxel-resistant cancer cells demonstrate a more efficient intake of glucose and lactate from the stromal cells than the sensitive cells and induce mitochondrial oxidative phosphorylation (OXPHOS) as a novel pattern of glycolysis [45]. Further studies demonstrate that upregulation of Ras signaling in CAFs is correlated with increased glutamine synthesis and subsequent macropinocytosis of extracellular fluid. The glutamine secreted from CAFs will then promote mitochondrial metabolism of cancer cells and lead to lethal tumor growth as well as therapeutic resistance against androgen signaling deprivation drugs [46]. It is recently reported that in non-small cell lung cancer (NSCLC), hypoxia-induced exosomes by the cisplatin-resistant cancer cells can deliver pyruvate kinase M2 (PKM2), a key mediator in the process of cancer cells converting glucose into lactic acid [47], to CAFs, leading to the release of pyruvate and lactate and subsequent chemoresistance [48]. Interestingly, it is demonstrated that oxidative stress promotes the TGF-β signaling in CAFs and increases the synthesis of glycolytic byproducts such as pyruvate, ketone bodies, and L-lactate. These metabolites fuel cancer cell growth and ultimately lead to increased tumorigenesis and therapeutic resistance [49].
CAF and ECM remodeling
Cancer ECM is generally denser and stiffer than the normal tissues [50], which could increase solid stress and interstitial fluid pressure in tumors to creating hypoxia and metabolic-stressed milieu with increased expression of anti-apoptotic proteins and drug-resistant signaling pathways, hence facilitating tumor growth, CSC phenotype, and therapeutic resistance [51]. Recent studies have revealed a strong correlation between CAF-derived ECM remodeling and cancer chemoresistance [52]. First of all, CAFs produce ECM proteins and generate desmoplasia and fibrosis in the tumor stroma to create a physical barrier between cancer cells and therapeutic drugs as well as immune cells. In addition, CAFs secrete metabolites to fuel cancer cell growth under hypoxic and undernourished conditions [53].
CAF and immune response
As the most important stromal component, CAFs are closely correlated with immune cells as a mechanism of therapeutic escape of cancer cells and the development of chemoresistance. It is demonstrated that the interaction between tumor-associated macrophages and CAFs could facilitate cancer cells to gain gemcitabine and paclitaxel resistance in pancreatic and breast cancer in an IGF-1/2-dependent manner [54, 55]. Natural killer (NK) cells are potent cancer cell killers, but exposure to TGF-β which is secreted by CAFs abrogates their cytotoxic activity via miR-183 mediated DAP12 transcription interruption, hence promoting cell survival and chemoresistance [56]. By secreting soluble factors such as CXCLs, CAFs also take part in the recruitment of tumor-associated neutrophils which aid in shaping TME and enhancing cancer cell proliferation, migration, and chemoresistance [57]. Additionally, CAF could secrete diverse cytokines and induce cancer chemoresistance in a paracrine manner. For instance, IL-6 is one of the typical cytokines secreted by CAFs that render chemoresistance in NSCLC cells. In an in vitro model, IL-6 family cytokine oncostatin-M (OSM) induces cancer cell EMT and escape from the targeted drug-induced apoptosis in an OSM receptor (OSMR)/JAK1/STAT3-dependent manner [58]. The role of CAF-derived IL-6 in inducing chemoresistance is also confirmed associated with the JAK2/STAT3 signaling pathway in patient samples of ovarian cancer [59]. Similarly, in gastric cancer, CAF-derived IL-11 is capable of inducing chemoresistance and CSC maintenance via the JAK/STAT3/Bcl2 signaling pathway [60].
CAF and cell survival
Considering the mechanism of chemotherapeutic drugs, it is obvious that apoptosis blockade could facilitate cancer cell survival and therapeutic resistance. It is suggested by a recent study that tumor necrosis factor superfamily member 4 (TNFSF4) is significantly up-regulated in lung CAFs under stress environments including chemotherapy, irradiation, and hypoxia. TNFSF4 not only inhibits the apoptosis of lung adenocarcinoma cells but also promotes cisplatin resistance mainly through enhanced activity of the NF-κB/BCL-XL signaling pathway [61].
Autophagy is also reported to be involved in the induction of chemoresistance of cancer cells [62]. In breast cancer, autophagy induced high-mobility group box 1 (HMGB1) secretion from CAFs further mediates CAF-CSC interaction and promotes tumorigenesis and therapeutic resistance in a Toll-like receptor 4 (TLR4)-dependent pattern [63]. CAF-mediated cisplatin resistance is also reported in tongue cancer via autophagy activation in the CAFs [64]. In the hypoxic TME, reactive oxygen species (ROS)-induced autophagy displays a negative feedback regulation by eliminating the source of ROS and thus protecting CAFs from oxidative damage. Blockage of autophagy resensitizes these CAFs to cisplatin [65]. In colorectal cancer, CAFs positively influence the metabolism of cancer cells through their autophagy and oxidative stress pathway which are initially induced by the neighboring cancer cells [66]. In cholangiocarcinoma, both in vitro and in vivo experiments show that CAF-derived IL-6 impairs the autophagy-associated apoptotic response to 5-FU in cancer cells. Cholangiocarcinoma patients with low stromal IL-6 levels and active autophagy flux in the cancer cells have a better prognosis and more effective response to postoperative chemotherapy [67].
DNA damage response is a network of cellular pathways that sense, signal, and repair DNA damage [68]. ROS produced in tumor stroma under oxidative stress is commonly observed during carcinogenesis, triggering DNA damage and genomic instability of adjacent cells including CAFs [69]. In turn, the soluble factors secreted by these ROS-induced CAFs promote cell survival and therapeutic resistance of cancer cells in a paracrine manner. For example, serine protease inhibitor Kazal type I (SPINK1), a senescence-associated secretory phenotype (SASP) factor produced in human stromal cells after genotoxic treatment, primes the aggressiveness and chemoresistance of cancer cells [70]. In multiple myeloma, the DNA-damaging drug doxorubicin could trigger an ataxia-telangiectasia-mutated (ATM) kinase-dependent DDR in bone marrow stromal cells, leading to increased IL-6 secretion by CAFs and resistance of myeloma cells to doxorubicin-induced apoptosis [71]. In prostate cancer, DNA damage increases the expression of the Wnt family member WNT16B in CAFs mediated by NF-κB, which further attenuates the cytotoxic effects of chemotherapeutic drugs mitoxantrone and docetaxel, thereby promoting the aggressiveness of the cancer cells in vivo [72].
Exosomes in CAF-mediated drug resistance
As nano-sized membrane-bound vesicles, exosomes provide new means of intercellular communication by delivering various bioactive molecules, including proteins, lipids, and nucleic acids, as well as participating in tumor initiation and progression [73]. Cancer-derived exosomes can change the behavior of surrounding stromal cells and vice versa, ultimately creating a suitable microenvironment for tumor growth [74]. It is suggested that in colorectal cancer, CAF-derived exosomes prime the drug-resistant character of CSCs by mediating the activation of the Wnt signaling pathway [75]. Further study indicates that CAFs contribute to cancer stemness, EMT, metastasis, and 5-FU/L-OHP resistance by directly transferring exosomes to cancer cells, which leads to a significant increase of miR-92a-3p and activation of Wnt/β-catenin pathway, hence inhibiting mitochondrial apoptosis by directly inhibiting F-box and WD repeat domain-containing 7 (FBXW7) and modulator of apoptosis 1 (MOAP1) [76]. In gastric cancer, CAF-secreted exosomal miR-522 could facilitate acquired drug resistance by induction of ferroptosis via arachidonate lipoxygenase 15 (ALOX15) regulation [77]. In PDAC, CAFs exhibit intrinsic resistance to gemcitabine. CAF-exosomes contribute to gemcitabine resistance by transferring miR-106b to neighboring cancer cells and directly targeting tumor protein 53-induced nuclear protein 1 (TP53INP1) [78]. In the context of ovarian cancer, it is revealed that CAF-derived exosomes carrying overexpressed miR-98-5p could promote cisplatin resistance of cancer cells by downregulating cyclin-dependent kinase inhibitor 1 A (CDKN1A) [79].
Radiotherapy
Both in vitro and in vivo studies have confirmed the inhibitory effect of CAFs on cancer radiation response by either direct or paracrine interaction. For instance, radiotherapy treatment upon CAFs leads to increased secretion of HGF and elevated phosphorylation of c-Met, the HGF receptor, facilitating the proliferation and metastasis of pancreatic cancer cells [80]. An elevation of CXCL12 secretion is also confirmed in irradiated CAFs, with a stimulating effect on pancreatic cancer cell migration, invasion, and EMT-related drug resistance [81]. As previously described [30–35, 38], both EMT and CSC stemness can be modulated by stromal TGF-β. It is demonstrated that TGF-β produced by radiation-treated CAFs not only promotes cancer cell migration and potential metastatic escape but also augments resistance to radiotherapy, hence contributing to the poor survival outcomes of patients [82, 83].
Similar to the development of chemoresistance, desmoplasia is also involved in radioresistance via integrin β1 and the downstream FAK and MAPK-AKT signaling pathways in cancer cells [84]. The hypoxic TME created by the desmoplastic reaction will further exacerbate the radioresistant feature of cancer cells [85]. In lung cancer, it is reported that CAFs produce IGF1/2, CXCL12, and β-hydroxybutyrate post-radiation, which are capable of increasing ROS expression and protein phosphatase 2 A (PP2A) activity, thereby inducing autophagy in cancer cells and promoting cell recovery from radiation-induced damage both in vitro and in vivo [86].
Targeted therapy
An increasing number of evidence supports the idea that EMT is involved in the development of resistance against tyrosine kinase inhibitors (TKIs) such as erlotinib and gefitinib in NSCLC [87, 88]. TKI-resistant cancer cells have mesenchymal cell characteristics based on cell morphology and upregulation of EMT-related proteins such as Vimentin and N-cadherin. In the nucleus, upregulation of p120-catenin and its binding to the Kaiso factor initiate transcription by activating EMT transcription factors including ZEB1, Snail, Slug, and Twist. The silencing of p120-catenin not only reverses the EMT process but also resensitizes cancer cells to erlotinib [89].
CAFs also play an active metabolic role in adaptive resistance to TKIs. It is proposed that under prolonged treatment with TKIs, EGFR- or MET-addicted NSCLC cells display an increase in producing glycolysis and lactate. Secreted lactate is the key molecule instructing CAFs to produce HGF in a nuclear factor kB-dependent manner, activating MET-dependent signaling in cancer cells, and finally sustaining resistance to TKIs [90]. Another study demonstrates that CAFs significantly increase the expression and phosphorylation of Annexin A2 (ANXA2) by secretion of HGF and IGF-1 as well as activation of the corresponding receptors c-met and IGF-1R, hence regulating EMT and gefitinib resistance in a paracrine manner [87].
Anti-angiogenesis therapy
CAFs take part in the resistance of anti-angiogenesis including sorafenib, sunitinib, and bevacizumab mainly through secreting different angiogenic factors such as VEGF in the hypoxic TME [91]. For instance, CAFs from anti-VEGF-resistant murine lymphoma could down-regulate drug response of the sensitive cancer cells through revascularization in a PDGF-C-dependent manner both in vitro and in vivo [92]. In PDAC, CAFs stimulate the invasion activity of cancer cells via paracrine IGF1/IGF1R signaling, especially under hypoxia [93]. A recent study utilizing mass spectrometry-based proteomic analysis of CAFs indicates that hypoxic human mammary CAFs promote angiogenesis in CAF endothelial cell co-cultures in vitro by altering their secretion of various pro-and anti-angiogenic factors. Being the most increased protein in an abundance of hypoxic CAFs, HIAR exercises its pro-angiogenic and pro-migratory functions by inducing secretion of VEGFA and consequently enhancing VEGF/VEGFR downstream signaling in the endothelial cells [13].
Immunotherapy
In recent years, the successful application of immune checkpoint inhibitors (ICIs) of cytotoxic T-lymphocyte antigen-4 (CTLA-4), programmed cell death-1 (PD-1), and programmed cell death ligand 1 (PD-L1) in various advanced cancers has attracted widespread attention in the field of immuno-oncology [94]. In this process, CAFs exert their immunomodulatory functions via modulation of both the cancer cells and the infiltrated immune cells, as well as the crosstalk among the complex components of the ECM [95, 96].
CAF and T lymphocytes
CAF abundancy is commonly correlated with aggressive clinical phenotype and poor responses to anticancer immunotherapy. The direct effect of CAFs on immunomodulatory is the attenuation of the CD8 + T lymphocyte function as well as the increase of the content in FOXP3 + regulatory T cells (Tregs), which are critical in maintaining immune tolerance and homeostasis of the immune system [97]. CAF subset heterogeneity analysis further refines the correlation between CAFs and immune infiltration. For example, fibroblast activation protein-α (FAP-α) + CAFs can increase the survival of CD4 + CD25 + T lymphocytes by secreting CXCL-12 and further induce these T cells differentiation into CD4 + CD25 + FOXP3 + Tregs and increase their ability to inhibit CD4 + effector T cell proliferation, thereby contributing to a tumor-promoting microenvironment in breast cancer and ovarian cancer [98]. FAP + CAFs also express high levels of TGF-β [99], which reduces T lymphocyte cytotoxicity by specifically inhibiting the expression of cytolytic gene products including perforin, granzyme A and B, Fas ligand, and interferon γ (IFN γ) [100]. TGFβ1 also reduces the responsiveness of memory T cells by blocking CD28-TCR signaling [101]. Interestingly, TGFβ secreted by CAFs can induce T cell apoptosis and enhance CTLA-4 + Tregs polarization [102]. Another subtype named PDPN + CAFs can suppress the proliferation of effector T lymphocytes in a nitric oxide-dependent manner, while PDPN- FAP + CAFs are not immunosuppressive [103]. Moreover, a recent study suggests that CD8 + T cells fail to infiltrate CAF-rich tumors, instead of accumulating at the tumor margin, and upregulating the expression of CTLA-4, leading to the resistance to multiple immunotherapies such as therapeutic vaccination and αPD1 [104]. In addition, CAF-derived IL-33 facilitates breast cancer metastasis in vivo by instigating type-2 inflammation in the metastatic microenvironment and mediates the recruitment of eosinophils, neutrophils, and inflammatory monocytes to the metastases [105]. Another study reveals that in melanoma and breast and colon cancers, TLR and Nod2 signaling could increase MCP-1 and RANTES expression in both cancer cells and CAFs. These secreted proteins promote the recruitment, generation, and expansion of Th17 cells [106], an independent lineage of Th cells that further promote tumor growth through the IL-17/IL-6/STAT3 functional axis [107].
CAF and immune checkpoint molecules
Given that CAFs could strongly inhibit T-cell proliferation in a contact-independent manner, it is further demonstrated that in pancreatic cancer, CAFs express higher levels of the PD-1 ligands PD-L1 and PD-L2 in comparison with normal tissues [108]. Immunotherapy based on PD-L1 blockade could not prevent the interaction of PD-L2 and PD-1, thus high expression of PD-L2 in CAFs could be a new mechanism of immunoresistance. Interestingly, the non-metastatic NSCLC patients with PD-L1 + CAFs exhibit significantly prolonged relapse-free survival than those with PD-L1- CAFs, and the expression of PD-L1 in CAFs is reversibly regulated by environmental stimuli including IFN γ from activated lymphocytes [109]. Mechanically, CAFs induce the expression of immune checkpoints such as T cell immunoglobulin mucin-domain-containing-3 (Tim-3), PD-1, CTLA-4, and lymphocyte activation gene (LAG)-3 on CD4 + and CD8 + T-cells, leading to fewer IFN γ, TNF-α, and CD107a production and a diminished immune function [108]. Subsequent studies indicate that CAFs promote PD-L1 expression in cancer cells through CXCL5 or CXCL2 secretion [110, 111]. Besides, CAF-derived exosomal miR-92 could downregulate large tumor suppressor kinase 2 (LATS2), an important component of the Hippo signaling pathway, leading to increased Yes-associated protein 1 (YAP1) nuclear translocation, thereby enhancing PD-L1 transcription and impairing T cell proliferation in breast cancer [112]. Moreover, CAFs themselves can function as antigen-presenting cells and induce CD8 + T cell death in an antigen-specific manner via PD-L2 and FASL [113].
CAF and ECM remodeling
As mentioned above, CAFs primarily prevent the infiltration and migration of immune cells by remodeling the ECM to serve as a contact barrier between the immune cells and cancer cells [114]. The dense ECM could also prevent T cells from therapeutic PD-1 inhibitors, thereby promoting the resistance of cancer cells to immune checkpoint inhibitors. Integrin α11 is a stromal collagen receptor that could promote tumor growth and metastasis and is associated with the regulation of collagen stiffness in the ECM. In a xenograft model of NSCLC, integrin α11 is reported to regulate the expression of CAF-derived lysyl oxidase like-1 (LOXL1), a matrix cross-linking enzyme, hence supporting tumor growth and immunoresistance through collagen matrix remodeling and collagen fiber alignment both in vitro and in vivo [115].
Metabolism in CAF-mediated immunosuppression
In addition to direct interaction with T cells and indirect influence via ECM remodeling, CAFs also take advantage of metabolic reprogramming to regulate T cell immunosuppression. On the one hand, glucose consumption by glycolytic CAF decreases environmental glucose levels of the TME, thereby impairing effector T cell activity without affecting cancer cell survival, as cancer cells could use lactate and pyruvate released by CAF [116]. On the other hand, the release of lactate by glycolytic CAFs acts on CD4 + T cells and shapes T cell polarization by decreasing Th1 and increasing Treg content [117]. Moreover, CAFs impair T cell function through increased activity of amino acid degrading enzymes involved in the regulation of immune tolerance of tumors [118]. For example, upon stimulation with IFN γ, CAFs express IDO protein and exhibit functional IDO activity, resulting in tryptophan depletion and kynurenine production as a novel T-cell inhibitory effector mechanism [119]. CAFs also inhibit anti-tumor effector T cell responses through arginase II (ARG2), which converts arginine to ornithine, leading to a lack of arginine, as well as reduced lymphocyte infiltration and attenuated function. The presence of ARG2-expressing CAFs is proposed to be an indicator of poor prognosis and hypoxia in cancer tissue [120]. In addition, it is detected in cervical cancer that CAFs express higher levels of CD39 and CD73 ectonucleotidases in cell membranes compared with normal tissues, and this feature is associated with the capability of decreasing the proliferation, activation and effector functions of cytotoxic T-cells through the generation of high amounts of adenosine from the hydrolysis of ATP, ADP and AMP nucleotides [121]. In melanoma, CAFs impair cytotoxic T lymphocyte (CTL) activity and reveal a pivotal role played by arginase in this phenomenon. CAF-derived soluble factors not only reduce CD69 on the surface of activated CTLs, but also increase l-arginase activity and CXCL12 release. The high amounts of CXCL12 by CAFs can act as a chemorepellent, explaining at least partially the exclusion of CD8 + T cells from solid tumors [122].
Endocrine therapy
Endocrine therapy has become the cornerstone of hormone-sensitive tumors such as hormone-receptor-positive breast cancer and prostate cancer, while resistance is also widely observed. In breast cancer, tamoxifen induces the upregulation of TP53-induced glycolysis and apoptosis regulator (TIGAR), a p53 regulated gene that protects cancer cells against the onset of stress-induced mitochondrial dysfunction and aerobic glycolysis. In a CAF co-culturing model of breast cancer, it was demonstrated that mitochondrial activity in epithelial cancer cells drives tamoxifen resistance [123]. Further studies confirm that soluble stromal factors and extracellular matrix components are also involved in protection against tamoxifen-induced cell death. In detail, CAF-derived soluble factors protect the epithelial cancer cells from tamoxifen-induced cell death via EGFR and MMPs upstream of PI3K/AKT. Exogenous fibronectin confers endocrine resistance through interaction with integrin β1 and activation of PI3K/AKT and MAPK/ERK1/2 pathways. Treatment with both CAF co-culturing and fibronectin leads to the phosphorylation of the estrogen receptor at serine-118, suggesting stromal factors as modulators of ER activity [124]. In prostate cancer, the tumor stroma is enriched in CAFs that secrete androgen receptor (AR)-activating factors, which modulate AR signaling in cancer cells after androgen deprivation therapy. Loss of CAF-dependent AR activation may be responsible for castration-resistant prostate cancer progression [125]. The glutamine secreted from the CAFs also promotes resistance against androgen signaling deprivation therapy in the prostate cancer cells [49].
CAF-directed anticancer strategies
The tumor-promoting functions that CAFs exert during cancer development make them promising targets in anticancer therapies. CAF-directed anticancer strategies can be generally divided into targeting the tumor-promoting function of CAFs, the downstream effectors, and the normalization of CAF-activated phenotype.
Anti-CAF therapies have been primarily focused on CAF depletion by targeting specific surface markers. For example, FAP causes rapid hypoxic necrosis of both cancer and stromal cells in dependence on IFN γ and TNFα to facilitate anti-tumor T cell infiltration and function, bringing benefits in transplantable models of NSCLC and PDAC [10, 126]. Targeting of FAP + CAFs by oral DNA vaccine increases the intratumoral infiltration of both CD8 + T cells and chemotherapeutic drugs in multi-drug-resistant breast and colon cancer [127, 128]. Further strategies such as FAP-CAR-T cell therapy and FAP-targeted oncolytic adenovirus promote a specific immune attack against FAP + CAFs, upregulate pro-inflammatory cytokines, and increase antigen presentation, T cell function, as well as trafficking, leading to enhanced anti-tumor efficacy [129–131]. FAP5-DM1, a monoclonal antibody targeting FAP + CAFs, induces long-lasting suppression of tumor growth and complete regression in xenograft models of a series of cancers with no obvious toxicity [132]. More recently, it is demonstrated in breast cancer and lung cancer that targeting the CD10 + GPR77 + CAFs correlated with chemoresistance and poor survival by using a neutralizing monoclonal antibody against GPR77 could induce tumor formation and improves chemotherapy efficacy in vivo [133]. Considering the complexity of cancer development, anticancer therapies are designed as combinatorial strategies that target crucial mediators in the TME and achieve promising and inspiring results. For example, Simlukafusp alfa (FAP-IL2v, RO6874281/RG7461) is an immunocytokine comprising an antibody against fibroblast activation protein α (FAP) and an IL-2 variant with a retained affinity for IL-2Rβγ > IL-2 Rβγ and abolished binding to IL-2 Rα. It is proven to be a potent immunocytokine that potentiates the efficacy of different T- and NK-cell-based cancer immunotherapies both in vitro and in vivo [134]. Another CAF-targeting strategy is to revert the activated state of the pro-tumorigenic CAFs into a relatively quiescent state or a tumor-suppressive phenotype. Treatment with vitamin D induces stromal reprogramming that normalizes the activated phenotype of CAFs and inhibits inflammation and fibrosis, improving the uptake of chemotherapeutic drugs and survival of pancreatic stellate cells [135].
Novel agents have been proposed to target downstream effectors and/or signaling pathways of CAFs including CAF-derived cytokines and chemokines. For instance, agents targeting IL-6, IL-6R, and JAK/STAT3 signaling pathways downstream of IL-6 have been approved by the US Food and Drug Administration (FDA) in myeloproliferative diseases and autoimmune disorders in order to suppress the FAP + CAF-induced proinflammatory cytokines and pro-angiogenic factors, which increase cancer cell proliferation and metastasis and negatively regulate T cell and NK cytotoxic activity [136]. In addition to IL-6, therapeutic agents targeting TGF-β signaling could interfere with the CAF activation or reduce the CAF numbers, leading to inhibited tumor growth and an anti-tumor effect. It is recently reported that small molecule kinase inhibitor LY2109761 blocks TGF-βRI and TGF-βRII receptors, suppresses the synthesis of CTGF, and reduces the stromal component of the tumors, leading to a significant reduction in the hepatocellular carcinoma growth, intravasation, and metastatic dissemination [137]. Galunisertib (LY2157299 monohydrate) is another TGF-βRI kinase inhibitor that specifically downregulates the phosphorylation of SMAD2, abrogating activation of the canonical pathway. It has been investigated in patients with glioblastoma, hepatocellular carcinoma, and pancreatic cancer [138]. Interestingly, co-administration of anti-TGF-β agents along with anti-PD-L1 immunotherapeutic drugs successfully suppresses TGF-β signaling of CAFs, facilitating T cell infiltration in TME and enhancing anti-tumor immunity [139]. Similarly, the AMD3100 compound, which targets the CXCL12-CXCR4 axis and reverses FAP + CAFs, impels immunosuppression and anti-PD-L1 immunotherapy in pancreatic cancer [140]. In addition, targeting CAF-induced fibrosis with the anti-fibrotic agent tranilast leads to enhanced tumor growth and invasiveness, as well as the immunosuppressive role of CAFs, via the decreased presence of Tregs and enhanced cytotoxic T cell response. This effect can be amplified in combination with effector-stimulatory immunotherapy such as dendritic cell-based vaccines [141].
Other anti-stromal therapies target ECM components in order to block cancer-driving signaling pathways and to facilitate the penetrance of therapeutic drugs as well as anti-tumor immune cells. MMPs and a disintegrin and metalloproteases (ADAMs) are the main metalloproteinase families participating in the remodeling of the ECM. Clinical trials have been undertaken with selective MMP and ADAM inhibitors, which are developed based on antibodies/antibody fragments or small molecules designed to take advantage of protease secondary binding sites or allosteric sites [142]. Moreover, it is demonstrated that the angiotensin inhibitor losartan could reduce stromal collagen and hyaluronan production and facilitate increased vascular perfusion, associated with decreased expression of profibrotic signals TGF-β1. Through this mechanism, losartan improves drug and oxygen delivery to TME in breast and pancreatic cancer models [143]. Additionally, remodeling the stroma of hyaluronan-rich tumors by depletion of hyaluronan, a PEGylated recombinant hyaluronidase, improves the antitumor activity of paclitaxel in the SKOV3/HAS3 tumor model [144].
Active clinical trials targeting CAFs in cancers are summarized in Table 1. Details for trials with NCT numbers can be accessed on https://clinicaltrials.gov (accessed on 1 December 2021).
Table 1.
Active clinical trials targeting CAFs in cancers
| NCT number | Cancer type | Drug | Compatibe drug | Target/mechanism | Clinical phase | Refs. | |
|---|---|---|---|---|---|---|---|
| NCT02699606 | NSCLC, urothelial cancer, gastric cancer, esophageal cancer or cholangiocarcinoma | Erdafitinib | / | A pan- FGFR tyrosine kinase inhibitor | Phase 2 | [145] | |
| NCT03762122 | Squamous-cell NSCLC | Rogaratinib | / | A pan-FGFR inhibitor | Phase 2 | [146] | |
| NCT03386721 | Head and neck, oesophageal or cervical cancer | RO6874281 | Atezolizumab (MPDL3280A), or Gemcitabine and Vinorelbine | An immunocytokine consisting of IL-2v targeting FAP-α | Phase 2 | [147] | |
| NCT02627274 | Breast cancer or head and neck cancer | RO6874281 | Trastuzumab or Cetuximab | An immunocytokine consisting of IL-2v targeting FAP-α | Phase 1 | [148] | |
| NCT03875079 | Melanoma | RO6874281 | Pembrolizumab | An immunocytokine consisting of IL-2v targeting FAP-α | Phase 1 | [149] | |
| NCT03834220 | Solid tumors | Debio 1347 | / | A pan-FGFR inhibitor | Phase 2 | [150] | |
| NCT03822117 | Solid tumors | Pemigatinib | / | Targeting activating FGFR mutations or translocations (FIGHT-207) | Phase 2 | [151] | |
| NCT02872714 | Urothelial cancer | Pemigatinib | / | Tarageting FGF/FGFR alterations (FIGHT-201) | Phase 2 | [152] | |
| NCT02924376 | Cholangiocarcinoma | Pemigatinib | / | Targeting FGFR2 | Phase 2 | [153] | |
| NCT02399215 | Carcinoid tumor, metastatic carcinoid tumor, or neuroendocrine neoplasm | Nintedanib | / | Blocking VEGFR from attaching to its target | Phase 2 | [154] | |
| NCT02834780 | Hepatocellular carcinoma | H3B-6527 | / | Targeting FGFR4 and FGF19 | Phase 1 | [155] | |
| NCT03343301 | Gastrointestinal cancer | FPA144 | mFOLFOX6 | Targeting FGFR2 | Phase 1 | [156] | |
| NCT02432274 | Solid malignant tumors or osteosarcoma | Lenvatinib | Ifosfamide, and Etoposide | An inhibitor of VEGFR2 tyrosine kinase with potential antineoplastic activity | Phase 1/2 | [157] | |
| NCT02508467 | Hepatocellular Carcinoma | Fisogatinib (BLU-554) | / | Targeting FGF19 | Phase 1 | [158] | |
FAP fibroblast activation protein; FGF fibroblast growth factor; FGFR fibroblast growth factor receptor; IL-2v interleukin-2 variant; NSCLC non-small-cell lung cancer; VEGFR vascular endothelial growth factor receptor
Conclusions and future perspectives
In recent years, increasing evidence has demonstrated the participation and importance of CAFs in tumorigenesis, development, immunosuppression, and drug resistance in a variety of cancers. As a key component of TME, CAFs exercise phenotypical and functional heterogeneity in a context-dependent manner in close relationship with TME as well as the host as a whole. Current research hotspots of CAFs in tumorigenesis and therapeutic resistance are mainly focused on subgroup analysis and functional research relying on CAF-specific markers and secretions such as IFN γ and TGF-β, which are expressed at different levels at different cancer stages in a context-specific manner. Existing results show that some targeting markers used in CAF-directed anticancer strategies are actually non-specific and also found on cancer cells as well. Moreover, hypoxia, acidic microenvironment, and tumor vascular abnormality remain the hurdles to be overcome concurrently in practice. To this end, more reasonable in vitro and in vivo research models are being called for. From the strategic point of view, the development of combinatorial strategies which not only target the interplay between CAFs and the TME but also promote conventional therapeutic effectiveness is still the mainstream direction in clinical trial design. Furthermore, attention should be paid to the dose of combinatorial agents and the potential occurrences, in order to truly realize the individualized anticancer therapies in the future.
Acknowledgements
Not applicable.
Abbreviations
- BMP
Bone morphogenetic protein
- CAF
Cancer-associated fibroblast
- CAM-DR
Cell adhesion mediated drug resistance
- CSC
Cancer stem cell
- CTL
Cytotoxic T lymphocyte
- ECM
Extracellular matrix
- EMT
Epithelial-mesenchymal transition
- FAP
Fibroblast activation protein
- FGF
Fibroblast growth factor
- ICI
Immune checkpoint inhibitors
- IFN
Interferon
- IL
Interleukin
- MSC
Mesenchymal stem cell
- NK
Natural killer
- NSCLC
Non-small cell lung cancer
- PD-1
Programmed cell death-1
- PD-L1
Programmed cell death ligand 1
- PDAC
Pancreatic ductal adenocarcinoma
- ROS
Reactive oxygen species
- SFM-DR
Secretory factor-mediated drug resistance
- Shh
Sonic hedgehog
- TGF
Transforming growth factor
- TKI
Tyrosine kinase inhibitors
- TLR
Toll-like receptor
- TME
Tumor microenvironment
- Treg
Regulatory T cell
- VEGFA
Vascular endothelial growth factor A
Author contributions
BF conceived the idea for the work and performed the literature search and data analysis. All authors participated in writing. JF, FJ, BS, and JW critically revised the work. All authors read and approved the final manuscript.
Funding
This work receives support from key projects for social development of Jiangsu Provincial Department of Science and Technology (BE2021745), provided by the people’s government of Jiangsu province. The funding bodies had no influence on the design of the study, the collection, analysis, and interpretation of data, and the writing of the manuscript.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Feng Jiang, Email: jiangfengnjykdx@126.com.
Jifeng Feng, Email: fjif@jszlyy.com.cn.
References
- 1.Lorusso G, Rüegg C. The tumor microenvironment and its contribution to tumor evolution toward metastasis. Histochem Cell Biol. 2008;130(6):1091–103. doi: 10.1007/s00418-008-0530-8. [DOI] [PubMed] [Google Scholar]
- 2.Cirri P, Chiarugi P. Cancer-associated-fibroblasts and tumour cells: a diabolic liaison driving cancer progression. Cancer Metastasis Rev. 2012;31(1–2):195–208. doi: 10.1007/s10555-011-9340-x. [DOI] [PubMed] [Google Scholar]
- 3.Aoto K, Ito K, Aoki S. Complex formation between platelet-derived growth factor receptor β and transforming growth factor β receptor regulates the differentiation of mesenchymal stem cells into cancer-associated fibroblasts. Oncotarget. 2018;9(75):34090–102. doi: 10.18632/oncotarget.26124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strong AL, Pei DT, Hurst CG, et al. Obesity Enhances the conversion of adipose-derived stromal/stem cells into carcinoma-associated fibroblast leading to cancer cell proliferation and progression to an invasive phenotype. Stem Cells Int. 2017;2017:9216502. doi: 10.1155/2017/9216502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nair N, Calle AS, Zahra MH, et al. A cancer stem cell model as the point of origin of cancer-associated fibroblasts in tumor microenvironment. Sci Rep. 2017;7(1):6838. doi: 10.1038/s41598-017-07144-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Worthley DL, Giraud AS, Wang TC. Stromal fibroblasts in digestive cancer. Cancer Microenviron. 2010;3(1):117–25. doi: 10.1007/s12307-009-0033-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kadel D, Zhang Y, Sun HR, et al. Current perspectives of cancer-associated fibroblast in therapeutic resistance: potential mechanism and future strategy. Cell Biol Toxicol. 2019;35(5):407–21. doi: 10.1007/s10565-019-09461-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 9.Erez N, Truitt M, Olson P, et al. Cancer-associated fibroblasts are activated in incipient neoplasia to orchestrate tumor-promoting inflammation in an NF-kappaB-dependent manner. Cancer Cell. 2010;17(2):135–47. doi: 10.1016/j.ccr.2009.12.041. [DOI] [PubMed] [Google Scholar]
- 10.Kraman M, Bambrough PJ, Arnold JN, et al. Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-alpha. Science. 2010;330(6005):827–30. doi: 10.1126/science.1195300. [DOI] [PubMed] [Google Scholar]
- 11.Li T, Yang Y, Hua X, et al. Hepatocellular carcinoma-associated fibroblasts trigger NK cell dysfunction via PGE2 and IDO. Cancer Lett. 2012;318(2):154–61. doi: 10.1016/j.canlet.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 12.Glentis A, Oertle P, Mariani P, et al. Cancer-associated fibroblasts induce metalloprotease-independent cancer cell invasion of the basement membrane. Nat Commun. 2017;8(1):924. doi: 10.1038/s41467-017-00985-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kugeratski FG, Atkinson SJ, Neilson LJ, et al. Hypoxic cancer-associated fibroblasts increase NCBP2-AS2/HIAR to promote endothelial sprouting through enhanced VEGF signaling. Sci Signal. 2019;12(567):eaan8247. doi: 10.1126/scisignal.aan8247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rhim AD, Oberstein PE, Thomas DH, et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014;25(6):735–47. doi: 10.1016/j.ccr.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JJ, Perera RM, Wang H, et al. Stromal response to Hedgehog signaling restrains pancreatic cancer progression. Proc Natl Acad Sci USA. 2014;111(30):E3091-100. doi: 10.1073/pnas.1411679111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin K, Lim A, Zhao C, et al. Hedgehog signaling restrains bladder cancer progression by eliciting stromal production of urothelial differentiation factors. Cancer Cell. 2014;26(4):521–33. doi: 10.1016/j.ccell.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerling M, Büller NV, Kirn LM, et al. Stromal Hedgehog signalling is downregulated in colon cancer and its restoration restrains tumour growth. Nat Commun. 2016;7:12321. doi: 10.1038/ncomms12321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Özdemir BC, Pentcheva-Hoang T, Carstens JL, et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25(6):719–34. doi: 10.1016/j.ccr.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brechbuhl HM, Finlay-Schultz J, Yamamoto TM, et al. Fibroblast subtypes regulate responsiveness of luminal breast cancer to estrogen. Clin Cancer Res. 2017;23(7):1710–21. doi: 10.1158/1078-0432.CCR-15-2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mhaidly R, Mechta-Grigoriou F. Role of cancer-associated fibroblast subpopulations in immune infiltration, as a new means of treatment in cancer. Immunol Rev. 2021;302(1):259–72. doi: 10.1111/imr.12978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miyai Y, Esaki N, Takahashi M, et al. Cancer-associated fibroblasts that restrain cancer progression: Hypotheses and perspectives. Cancer Sci. 2020;111(4):1047–57. doi: 10.1111/cas.14346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meads MB, Gatenby RA, Dalton WS. Environment-mediated drug resistance: a major contributor to minimal residual disease. Nat Rev Cancer. 2009;9(9):665–74. doi: 10.1038/nrc2714. [DOI] [PubMed] [Google Scholar]
- 23.Jena BC, Das CK, Bharadwaj D, et al. Cancer associated fibroblast mediated chemoresistance: a paradigm shift in understanding the mechanism of tumor progression. Biochim Biophys Acta Rev Cancer. 2020;1874(2):188416. doi: 10.1016/j.bbcan.2020.188416. [DOI] [PubMed] [Google Scholar]
- 24.Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016;16(9):582–98. doi: 10.1038/nrc.2016.73. [DOI] [PubMed] [Google Scholar]
- 25.Chandra Jena B, Sarkar S, Rout L, et al. The transformation of cancer-associated fibroblasts: current perspectives on the role of TGF-β in CAF mediated tumor progression and therapeutic resistance. Cancer Lett. 2021;520:222–32. doi: 10.1016/j.canlet.2021.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Maji S, Panda S, Samal SK, et al. Bcl-2 antiapoptotic family proteins and chemoresistance in cancer. Adv Cancer Res. 2018;137:37–75. doi: 10.1016/bs.acr.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Baulida J. Epithelial-to-mesenchymal transition transcription factors in cancer-associated fibroblasts. Mol Oncol. 2017;11(7):847–59. doi: 10.1002/1878-0261.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Francí C, Gallén M, Alameda F, et al. Snail1 protein in the stroma as a new putative prognosis marker for colon tumours. PLoS ONE. 2009;4(5):e5595. doi: 10.1371/journal.pone.0005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bronsert P, Kohler I, Timme S, et al. Prognostic significance of Zinc finger E-box binding homeobox 1 (ZEB1) expression in cancer cells and cancer-associated fibroblasts in pancreatic head cancer. Surgery. 2014;156(1):97–108. doi: 10.1016/j.surg.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 30.Román-Pérez E, Casbas-Hernández P, Pirone JR, et al. Gene expression in extratumoral microenvironment predicts clinical outcome in breast cancer patients. Breast Cancer Res. 2012;14(2):R51. doi: 10.1186/bcr3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu Y, Xiao CH, Tan LD, et al. Cancer-associated fibroblasts induce epithelial-mesenchymal transition of breast cancer cells through paracrine TGF-β signalling. Br J Cancer. 2014;110(3):724–32. doi: 10.1038/bjc.2013.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yeung TL, Leung CS, Wong KK, et al. TGF-β modulates ovarian cancer invasion by upregulating CAF-derived versican in the tumor microenvironment. Cancer Res. 2013;73(16):5016–28. doi: 10.1158/0008-5472.CAN-13-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heerboth S, Housman G, Leary M, et al. EMT and tumor metastasis. Clin Transl Med. 2015;4:6. doi: 10.1186/s40169-015-0048-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yeldag G, Rice A, Del Río Hernández A. Chemoresistance and the self-maintaining tumor microenvironment. Cancers. 2018;10(12):471. doi: 10.3390/cancers10120471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhuang J, Lu Q, Shen B, et al. TGFβ1 secreted by cancer-associated fibroblasts induces epithelial-mesenchymal transition of bladder cancer cells through lncRNA-ZEB2NAT. Sci Rep. 2015;5:11924. doi: 10.1038/srep11924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nguyen LV, Vanner R, Dirks P, et al. Cancer stem cells: an evolving concept. Nat Rev Cancer. 2012;12(2):133–43. doi: 10.1038/nrc3184. [DOI] [PubMed] [Google Scholar]
- 37.Lotti F, Jarrar AM, Pai RK, et al. Chemotherapy activates cancer-associated fibroblasts to maintain colorectal cancer-initiating cells by IL-17A. J Exp Med. 2013;210(13):2851–72. doi: 10.1084/jem.20131195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Calon A, Lonardo E, Berenguer-Llergo A, et al. Stromal gene expression defines poor-prognosis subtypes in colorectal cancer. Nat Genet. 2015;47(4):320–9. doi: 10.1038/ng.3225. [DOI] [PubMed] [Google Scholar]
- 39.Cho SJ, Park JW, Kang JS, et al. Nuclear factor-kappaB dependency of doxorubicin sensitivity in gastric cancer cells is determined by manganese superoxide dismutase expression. Cancer Sci. 2008;99(6):1117–24. doi: 10.1111/j.1349-7006.2008.00789.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han ME, Kim HJ, Shin DH, et al. Overexpression of NRG1 promotes progression of gastric cancer by regulating the self-renewal of cancer stem cells. J Gastroenterol. 2015;50(6):645–56. doi: 10.1007/s00535-014-1008-1. [DOI] [PubMed] [Google Scholar]
- 41.Pistore C, Giannoni E, Colangelo T, et al. DNA methylation variations are required for epithelial-to-mesenchymal transition induced by cancer-associated fibroblasts in prostate cancer cells. Oncogene. 2017;36(40):5551–66. doi: 10.1038/onc.2017.159. [DOI] [PubMed] [Google Scholar]
- 42.Sebens S, Schafer H. The tumor stroma as mediator of drug resistance—a potential target to improve cancer therapy? Curr Pharm Biotechnol. 2012;13(11):2259–72. doi: 10.2174/138920112802501999. [DOI] [PubMed] [Google Scholar]
- 43.Yu T, Yang G, Hou Y. Cytoplasmic GPER translocation in cancer-associated fibroblasts mediates cAMP/PKA/CREB/glycolytic axis to confer tumor cells with multidrug resistance. Oncogene. 2017;36(15):2131–45. doi: 10.1038/onc.2016.370. [DOI] [PubMed] [Google Scholar]
- 44.Tavares-Valente D, Baltazar F, Moreira R, et al. Cancer cell bioenergetics and pH regulation influence breast cancer cell resistance to paclitaxel and doxorubicin. J Bioenerg Biomembr. 2013;45(5):467–75. doi: 10.1007/s10863-013-9519-7. [DOI] [PubMed] [Google Scholar]
- 45.Rong G, Kang H, Wang Y, et al. Candidate markers that associate with chemotherapy resistance in breast cancer through the study on Taxotere-induced damage to tumor microenvironment and gene expression profiling of carcinoma-associated fibroblasts (CAFs) PLoS ONE. 2013;8(8):e70960. doi: 10.1371/journal.pone.0070960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mishra R, Haldar S, Placencio V, et al. Stromal epigenetic alterations drive metabolic and neuroendocrine prostate cancer reprogramming. J Clin Invest. 2018;128(10):4472–84. doi: 10.1172/JCI99397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Suzuki A, Puri S, Leland P, et al. Subcellular compartmentalization of PKM2 identifies anti-PKM2 therapy response in vitro and in vivo mouse model of human non-small-cell lung cancer. PLoS ONE. 2019;14(5):e0217131. doi: 10.1371/journal.pone.0217131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang D, Zhao C, Xu F, et al. Cisplatin-resistant NSCLC cells induced by hypoxia transmit resistance to sensitive cells through exosomal PKM2. Theranostics. 2021;11(6):2860–75. doi: 10.7150/thno.51797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhao X, He Y, Chen H. Autophagic tumor stroma: mechanisms and roles in tumor growth and progression. Int J Cancer. 2013;132(1):1–8. doi: 10.1002/ijc.27664. [DOI] [PubMed] [Google Scholar]
- 50.Senthebane DA, Rowe A, Thomford NE, et al. The role of tumor microenvironment in chemoresistance: to survive, keep your enemies closer. Int J Mol Sci. 2017;18(7):1586. doi: 10.3390/ijms18071586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Henke E, Nandigama R, Ergün S. Extracellular Matrix in the Tumor Microenvironment and Its Impact on Cancer Therapy. Front Mol Biosci. 2020;6:160. doi: 10.3389/fmolb.2019.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bergamaschi A, Tagliabue E, Sørlie T, et al. Extracellular matrix signature identifies breast cancer subgroups with different clinical outcome. J Pathol. 2008;214(3):357–67. doi: 10.1002/path.2278. [DOI] [PubMed] [Google Scholar]
- 53.Helms E, Onate MK, Sherman MH. Fibroblast heterogeneity in the pancreatic tumor microenvironment. Cancer Discov. 2020;10(5):648–56. doi: 10.1158/2159-8290.CD-19-1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ireland L, Santos A, Ahmed MS, et al. Chemoresistance in pancreatic cancer is driven by stroma-derived insulin-like growth factors. Cancer Res. 2016;76(23):6851–63. doi: 10.1158/0008-5472.CAN-16-1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ireland L, Santos A, Campbell F, et al. Blockade of insulin-like growth factors increases efficacy of paclitaxel in metastatic breast cancer. Oncogene. 2018;37(15):2022–36. doi: 10.1038/s41388-017-0115-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Donatelli SS, Zhou JM, Gilvary DL, et al. TGF-β-inducible microRNA-183 silences tumor-associated natural killer cells. Proc Natl Acad Sci USA. 2014;111(11):4203–8. doi: 10.1073/pnas.1319269111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Powell DR, Huttenlocher A. Neutrophils in the tumor microenvironment. Trends Immunol. 2016;37(1):41–52. doi: 10.1016/j.it.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shien K, Papadimitrakopoulou VA, Ruder D, et al. JAK1/STAT3 activation through a proinflammatory cytokine pathway leads to resistance to molecularly targeted therapy in non-small cell lung cancer. Mol Cancer Ther. 2017;16(10):2234–45. doi: 10.1158/1535-7163.MCT-17-0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang L, Zhang F, Cui JY, et al. CAFs enhance paclitaxel resistance by inducing EMT through the IL–6/JAK2/STAT3 pathway. Oncol Rep. 2018;39(5):2081–90. doi: 10.3892/or.2018.6311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ma J, Song X, Xu X, et al. Cancer-associated fibroblasts promote the chemo-resistance in gastric cancer through secreting IL-11 targeting JAK/STAT3/Bcl2 pathway. Cancer Res Treat. 2019;51(1):194–210. doi: 10.4143/crt.2018.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li Y, Chen Y, Miao L, et al. Stress-induced upregulation of TNFSF4 in cancer-associated fibroblast facilitates chemoresistance of lung adenocarcinoma through inhibiting apoptosis of tumor cells. Cancer Lett. 2021;497:212–20. doi: 10.1016/j.canlet.2020.10.032. [DOI] [PubMed] [Google Scholar]
- 62.Sui X, Chen R, Wang Z, et al. Autophagy and chemotherapy resistance: a promising therapeutic target for cancer treatment. Cell Death Dis. 2013;4(10):e838. doi: 10.1038/cddis.2013.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhao XL, Lin Y, Jiang J, et al. High-mobility group box 1 released by autophagic cancer-associated fibroblasts maintains the stemness of luminal breast cancer cells. J Pathol. 2017;243(3):376–89. doi: 10.1002/path.4958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liao JK, Zhou B, Zhuang XM, et al. Cancer-associated fibroblasts confer cisplatin resistance of tongue cancer via autophagy activation. Biomed Pharmacother. 2018;97:1341–8. doi: 10.1016/j.biopha.2017.11.024. [DOI] [PubMed] [Google Scholar]
- 65.Wang Q, Xue L, Zhang X, et al. Autophagy protects ovarian cancer-associated fibroblasts against oxidative stress. Cell Cycle. 2016;15(10):1376–85. doi: 10.1080/15384101.2016.1170269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhou W, Xu G, Wang Y, et al. Oxidative stress induced autophagy in cancer associated fibroblast enhances proliferation and metabolism of colorectal cancer cells. Cell Cycle. 2017;16(1):73–81. doi: 10.1080/15384101.2016.1252882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Thongchot S, Vidoni C, Ferraresi A, et al. Cancer-associated fibroblast-derived IL-6 determines unfavorable prognosis in cholangiocarcinoma by affecting autophagy-associated chemoresponse. Cancers. 2021;13(9):2134. doi: 10.3390/cancers13092134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Polo SE, Jackson SP. Dynamics of DNA damage response proteins at DNA breaks: a focus on protein modifications. Genes Dev. 2011;25(5):409–33. doi: 10.1101/gad.2021311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Martinez-Outschoorn UE, Balliet RM, Rivadeneira DB, et al. Oxidative stress in cancer associated fibroblasts drives tumor-stroma co-evolution: A new paradigm for understanding tumor metabolism, the field effect and genomic instability in cancer cells. Cell Cycle. 2010;9(16):3256–76. doi: 10.4161/cc.9.16.12553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen F, Long Q, Fu D, et al. Targeting SPINK1 in the damaged tumour microenvironment alleviates therapeutic resistance. Nat Commun. 2018;9(1):4315. doi: 10.1038/s41467-018-06860-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tang H, Shu M, Dai B, et al. DNA damage response-initiated cytokine secretion in bone marrow stromal cells promotes chemoresistance of myeloma cells. Leuk Lymphoma. 2018;59(9):2220–6. doi: 10.1080/10428194.2017.1413188. [DOI] [PubMed] [Google Scholar]
- 72.Sun Y, Campisi J, Higano C, et al. Treatment-induced damage to the tumor microenvironment promotes prostate cancer therapy resistance through WNT16B. Nat Med. 2012;18(9):1359–68. doi: 10.1038/nm.2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Das CK, Jena BC, Banerjee I, et al. Exosome as a novel shuttle for delivery of therapeutics across biological barriers. Mol Pharm. 2019;16(1):24–40. doi: 10.1021/acs.molpharmaceut.8b00901. [DOI] [PubMed] [Google Scholar]
- 74.Cheng L, Sharples RA, Scicluna BJ, et al. Exosomes provide a protective and enriched source of miRNA for biomarker profiling compared to intracellular and cell-free blood. J Extracell Vesicles. 2014 doi: 10.1002/pmic.201600389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hu Y, Yan C, Mu L, et al. Fibroblast-derived exosomes contribute to chemoresistance through priming cancer stem cells in colorectal cancer. PLoS ONE. 2015;10(5):e0125625. doi: 10.1371/journal.pone.0125625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hu JL, Wang W, Lan XL, et al. CAFs secreted exosomes promote metastasis and chemotherapy resistance by enhancing cell stemness and epithelial-mesenchymal transition in colorectal cancer. Mol Cancer. 2019;18(1):91. doi: 10.1186/s12943-019-1019-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang H, Deng T, Liu R, et al. CAF secreted miR-522 suppresses ferroptosis and promotes acquired chemo-resistance in gastric cancer. Mol Cancer. 2020;19(1):43. doi: 10.1186/s12943-020-01168-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fang Y, Zhou W, Rong Y, et al. Exosomal miRNA-106b from cancer-associated fibroblast promotes gemcitabine resistance in pancreatic cancer. Exp Cell Res. 2019;383(1):111543. doi: 10.1016/j.yexcr.2019.111543. [DOI] [PubMed] [Google Scholar]
- 79.Guo H, Ha C, Dong H, et al. Cancer-associated fibroblast-derived exosomal microRNA-98-5p promotes cisplatin resistance in ovarian cancer by targeting CDKN1A. Cancer Cell Int. 2019;19:347. doi: 10.1186/s12935-019-1051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ohuchida K, Mizumoto K, Murakami M, et al. Radiation to stromal fibroblasts increases invasiveness of pancreatic cancer cells through tumor-stromal interactions. Cancer Res. 2004;64(9):3215–22. doi: 10.1158/0008-5472.can-03-2464. [DOI] [PubMed] [Google Scholar]
- 81.Li D, Qu C, Ning Z, et al. Radiation promotes epithelial-to-mesenchymal transition and invasion of pancreatic cancer cell by activating carcinoma-associated fibroblasts. Am J Cancer Res. 2016;6(10):2192–206. [PMC free article] [PubMed] [Google Scholar]
- 82.Papadopoulou A, Kletsas D. Human lung fibroblasts prematurely senescent after exposure to ionizing radiation enhance the growth of malignant lung epithelial cells in vitro and in vivo. Int J Oncol. 2011;39(4):989–99. doi: 10.3892/ijo.2011.1132. [DOI] [PubMed] [Google Scholar]
- 83.Zhang H, Xie C, Yue J, et al. Cancer-associated fibroblasts mediated chemoresistance by a FOXO1/TGFβ1 signaling loop in esophageal squamous cell carcinoma. Mol Carcinog. 2017;56(3):1150–63. doi: 10.1002/mc.22581. [DOI] [PubMed] [Google Scholar]
- 84.Mantoni TS, Lunardi S, Al-Assar O, et al. Pancreatic stellate cells radioprotect pancreatic cancer cells through β1-integrin signaling. Cancer Res. 2011;71(10):3453–8. doi: 10.1158/0008-5472.CAN-10-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Horsman MR, Overgaard J. The impact of hypoxia and its modification of the outcome of radiotherapy. J Radiat Res. 2016;57(Suppl 1):i90–8. doi: 10.1093/jrr/rrw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wang Y, Gan G, Wang B, et al. Cancer-associated fibroblasts promote irradiated cancer cell recovery through autophagy. EBioMedicine. 2017;17:45–56. doi: 10.1016/j.ebiom.2017.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yi Y, Zeng S, Wang Z, et al. Cancer-associated fibroblasts promote epithelial-mesenchymal transition and EGFR-TKI resistance of non-small cell lung cancers via HGF/IGF-1/ANXA2 signaling. Biochim Biophys Acta Mol Basis Dis. 2018;1864(3):793–803. doi: 10.1016/j.bbadis.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 88.Choe C, Shin YS, Kim C, et al. Crosstalk with cancer-associated fibroblasts induces resistance of non-small cell lung cancer cells to epidermal growth factor receptor tyrosine kinase inhibition. Onco Targets Ther. 2015;8:3665–78. doi: 10.2147/OTT.S89659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Iderzorig T, Kellen J, Osude C, et al. Comparison of EMT mediated tyrosine kinase inhibitor resistance in NSCLC. Biochem Biophys Res Commun. 2018;496(2):770–7. doi: 10.1016/j.bbrc.2018.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Apicella M, Giannoni E, Fiore S, et al. Increased lactate secretion by cancer cells sustains non-cell-autonomous adaptive resistance to MET and EGFR targeted therapies. Cell Metab. 2018;28(6):848–65.e6. doi: 10.1016/j.cmet.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 91.Beckermann BM, Kallifatidis G, Groth A, et al. VEGF expression by mesenchymal stem cells contributes to angiogenesis in pancreatic carcinoma. Br J Cancer. 2008;99(4):622–31. doi: 10.1038/sj.bjc.6604508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Crawford Y, Kasman I, Yu L, et al. PDGF-C mediates the angiogenic and tumorigenic properties of fibroblasts associated with tumors refractory to anti-VEGF treatment. Cancer Cell. 2009;15(1):21–34. doi: 10.1016/j.ccr.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 93.Hirakawa T, Yashiro M, Doi Y, et al. Pancreatic fibroblasts stimulate the motility of pancreatic cancer cells through IGF1/IGF1R signaling under hypoxia. PLoS ONE. 2016;11(8):e0159912. doi: 10.1371/journal.pone.0159912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chae YK, Arya A, Iams W, et al. Immune checkpoint pathways in non-small cell lung cancer. Ann Transl Med. 2018;6(5):88. doi: 10.21037/atm.2017.09.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Monteran L, Erez N. The dark side of fibroblasts: cancer-associated fibroblasts as mediators of immunosuppression in the tumor microenvironment. Front Immunol. 2019;10:1835. doi: 10.3389/fimmu.2019.01835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nagarsheth N, Wicha MS, Zou W. Chemokines in the cancer microenvironment and their relevance in cancer immunotherapy. Nat Rev Immunol. 2017;17(9):559–72. doi: 10.1038/nri.2017.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dominguez CX, Müller S, Keerthivasan S, et al. Single-cell RNA sequencing reveals stromal evolution into LRRC15 + myofibroblasts as a determinant of patient response to cancer immunotherapy. Cancer Discov. 2020;10(2):232–53. doi: 10.1158/2159-8290.CD-19-0644. [DOI] [PubMed] [Google Scholar]
- 98.Costa A, Kieffer Y, Scholer-Dahirel A, et al. Fibroblast heterogeneity and immunosuppressive environment in human breast cancer. Cancer Cell. 2018;33(3):463–79.e10. doi: 10.1016/j.ccell.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 99.Kieffer Y, Hocine HR, Gentric G, et al. Single-cell analysis reveals fibroblast clusters linked to immunotherapy resistance in cancer. Cancer Discov. 2020;10(9):1330–51. doi: 10.1158/2159-8290.CD-19-1384. [DOI] [PubMed] [Google Scholar]
- 100.Thomas DA, Massagué J. TGF-beta directly targets cytotoxic T cell functions during tumor evasion of immune surveillance. Cancer Cell. 2005;8(5):369–80. doi: 10.1016/j.ccr.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 101.Broderick L, Bankert RB. Membrane-associated TGF-beta1 inhibits human memory T cell signaling in malignant and nonmalignant inflammatory microenvironments. J Immunol. 2006;177(5):3082–8. doi: 10.4049/jimmunol.177.5.3082. [DOI] [PubMed] [Google Scholar]
- 102.Takahashi H, Sakakura K, Kawabata-Iwakawa R, et al. Immunosuppressive activity of cancer-associated fibroblasts in head and neck squamous cell carcinoma. Cancer Immunol Immunother. 2015;64(11):1407–17. doi: 10.1007/s00262-015-1742-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cremasco V, Astarita JL, Grauel AL, et al. FAP delineates heterogeneous and functionally divergent stromal cells in immune-excluded breast tumors. Cancer Immunol Res. 2018;6(12):1472–85. doi: 10.1158/2326-6066.CIR-18-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hanley CJ, Thomas GJ. T-cell tumour exclusion and immunotherapy resistance: a role for CAF targeting. Br J Cancer. 2020;123(9):1353–5. doi: 10.1038/s41416-020-1020-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shani O, Vorobyov T, Monteran L, et al. Fibroblast-derived IL33 facilitates breast cancer metastasis by modifying the immune microenvironment and driving type 2 immunity. Cancer Res. 2020;80(23):5317–29. doi: 10.1158/0008-5472.CAN-20-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Su X, Ye J, Hsueh EC, et al. Tumor microenvironments direct the recruitment and expansion of human Th17 cells. J Immunol. 2010;184(3):1630–41. doi: 10.4049/jimmunol.0902813. [DOI] [PubMed] [Google Scholar]
- 107.Li Q, Han Y, Fei G, et al. IL-17 promoted metastasis of non-small-cell lung cancer cells. Immunol Lett. 2012;148(2):144–50. doi: 10.1016/j.imlet.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 108.Gorchs L, Fernández Moro C, Bankhead P, et al. Human pancreatic carcinoma-associated fibroblasts promote expression of co-inhibitory markers on CD4 + and CD8 + T-cells. Front Immunol. 2019;10:847. doi: 10.3389/fimmu.2019.00847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Teramoto K, Igarashi T, Kataoka Y, et al. Clinical significance of PD-L1-positive cancer-associated fibroblasts in pN0M0 non-small cell lung cancer. Lung Cancer. 2019;137:56–63. doi: 10.1016/j.lungcan.2019.09.013. [DOI] [PubMed] [Google Scholar]
- 110.Li Z, Zhou J, Zhang J, et al. Cancer-associated fibroblasts promote PD-L1 expression in mice cancer cells via secreting CXCL5. Int J Cancer. 2019;145(7):1946–57. doi: 10.1002/ijc.32278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Inoue C, Miki Y, Saito R, et al. PD-L1 induction by cancer-associated fibroblast-derived factors in lung adenocarcinoma cells. Cancers. 2019;11(9):1257. doi: 10.3390/cancers11091257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Dou D, Ren X, Han M, et al. Cancer-associated fibroblasts-derived exosomes suppress immune cell function in breast cancer via the miR-92/PD-L1 pathway. Front Immunol. 2020;11:2026. doi: 10.3389/fimmu.2020.02026. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 113.Lakins MA, Ghorani E, Munir H, et al. Cancer-associated fibroblasts induce antigen-specific deletion of CD8 + T Cells to protect tumour cells. Nat Commun. 2018;9(1):948. doi: 10.1038/s41467-018-03347-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nicolas-Boluda A, Vaquero J, Vimeux L, et al. Tumor stiffening reversion through collagen crosslinking inhibition improves T cell migration and anti-PD-1 treatment. Elife. 2021;10:e58688. doi: 10.7554/eLife.58688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zeltz C, Pasko E, Cox TR, et al. LOXL1 Is regulated by integrin α11 and promotes non-small cell lung cancer tumorigenicity. Cancers. 2019;11(5):705. doi: 10.3390/cancers11050705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Becker LM, O’Connell JT, Vo AP, et al. Epigenetic reprogramming of cancer-associated fibroblasts deregulates glucose metabolism and facilitates progression of breast cancer. Cell Rep. 2020;31(9):107701. doi: 10.1016/j.celrep.2020.107701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Comito G, Iscaro A, Bacci M, et al. Lactate modulates CD4 + T-cell polarization and induces an immunosuppressive environment, which sustains prostate carcinoma progression via TLR8/miR21 axis. Oncogene. 2019;38(19):3681–95. doi: 10.1038/s41388-019-0688-7. [DOI] [PubMed] [Google Scholar]
- 118.Timosenko E, Hadjinicolaou AV, Cerundolo V. Modulation of cancer-specific immune responses by amino acid degrading enzymes. Immunotherapy. 2017;9(1):83–97. doi: 10.2217/imt-2016-0118. [DOI] [PubMed] [Google Scholar]
- 119.Meisel R, Zibert A, Laryea M, et al. Human bone marrow stromal cells inhibit allogeneic T-cell responses by indoleamine 2,3-dioxygenase-mediated tryptophan degradation. Blood. 2004;103(12):4619–21. doi: 10.1182/blood-2003-11-3909. [DOI] [PubMed] [Google Scholar]
- 120.Ino Y, Yamazaki-Itoh R, Oguro S, et al. Arginase II expressed in cancer-associated fibroblasts indicates tissue hypoxia and predicts poor outcome in patients with pancreatic cancer. PLoS One. 2013;8(2):e55146. doi: 10.1371/journal.pone.0055146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.de Lourdes Mora-García M, García-Rocha R, Morales-Ramírez O, et al. Mesenchymal stromal cells derived from cervical cancer produce high amounts of adenosine to suppress cytotoxic T lymphocyte functions. J Transl Med. 2016;14(1):302. doi: 10.1186/s12967-016-1057-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Érsek B, Silló P, Cakir U, et al. Melanoma-associated fibroblasts impair CD8 + T cell function and modify expression of immune checkpoint regulators via increased arginase activity. Cell Mol Life Sci. 2021;78(2):661–73. doi: 10.1007/s00018-020-03517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Martinez-Outschoorn UE, Goldberg A, Lin Z, et al. Anti-estrogen resistance in breast cancer is induced by the tumor microenvironment and can be overcome by inhibiting mitochondrial function in epithelial cancer cells. Cancer Biol Ther. 2011;12(10):924–38. doi: 10.4161/cbt.12.10.17780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Pontiggia O, Sampayo R, Raffo D, et al. The tumor microenvironment modulates tamoxifen resistance in breast cancer: a role for soluble stromal factors and fibronectin through β1 integrin. Breast Cancer Res Treat. 2012;133(2):459–71. doi: 10.1007/s10549-011-1766-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ishii K, Matsuoka I, Sasaki T, et al. Loss of fibroblast-dependent androgen receptor activation in prostate cancer cells is involved in the mechanism of acquired resistance to castration. J Clin Med. 2019;8(9):1379. doi: 10.3390/jcm8091379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gunderson AJ, Yamazaki T, McCarty K, et al. Blockade of fibroblast activation protein in combination with radiation treatment in murine models of pancreatic adenocarcinoma. PLoS ONE. 2019;14(2):e0211117. doi: 10.1371/journal.pone.0211117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Duperret EK, Trautz A, Ammons D, et al. Alteration of the tumor stroma using a consensus DNA vaccine targeting fibroblast activation protein (FAP) synergizes with antitumor vaccine therapy in mice. Clin Cancer Res. 2018;24(5):1190–201. doi: 10.1158/1078-0432.CCR-17-2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Loeffler M, Krüger JA, Niethammer AG, et al. Targeting tumor-associated fibroblasts improves cancer chemotherapy by increasing intratumoral drug uptake. J Clin Invest. 2006;116(7):1955–62. doi: 10.1172/JCI26532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lo A, Wang LS, Scholler J, et al. Tumor-promoting desmoplasia is disrupted by depleting FAP-expressing stromal cells. Cancer Res. 2015;75(14):2800–10. doi: 10.1158/0008-5472.CAN-14-3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Freedman JD, Duffy MR, Lei-Rossmann J, et al. An oncolytic virus expressing a T-cell engager simultaneously targets cancer and immunosuppressive stromal cells. Cancer Res. 2018;78(24):6852–65. doi: 10.1158/0008-5472.CAN-18-1750. [DOI] [PubMed] [Google Scholar]
- 131.de Sostoa J, Fajardo CA, Moreno R, et al. Targeting the tumor stroma with an oncolytic adenovirus secreting a fibroblast activation protein-targeted bispecific T-cell engager. J Immunother Cancer. 2019;7(1):19. doi: 10.1186/s40425-019-0505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ostermann E, Garin-Chesa P, Heider KH, et al. Effective immunoconjugate therapy in cancer models targeting a serine protease of tumor fibroblasts. Clin Cancer Res. 2008;14(14):4584–92. doi: 10.1158/1078-0432.CCR-07-5211. [DOI] [PubMed] [Google Scholar]
- 133.Su S, Chen J, Yao H, et al. CD10 + GPR77 + cancer-associated fibroblasts promote cancer formation and chemoresistance by sustaining cancer stemness. Cell. 2018;172(4):841–56.e16. doi: 10.1016/j.cell.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 134.Waldhauer I, Gonzalez-Nicolini V, Freimoser-Grundschober A, et al. Simlukafusp alfa (FAP-IL2v) immunocytokine is a versatile combination partner for cancer immunotherapy. MAbs. 2021;13(1):1913791. doi: 10.1080/19420862.2021.1913791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sherman MH, Yu RT, Engle DD, et al. Vitamin D receptor-mediated stromal reprogramming suppresses pancreatitis and enhances pancreatic cancer therapy. Cell. 2014;159(1):80–93. doi: 10.1016/j.cell.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Johnson DE, O’Keefe RA, Grandis JR. Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat Rev Clin Oncol. 2018;15(4):234–48. doi: 10.1038/nrclinonc.2018.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mazzocca A, Fransvea E, Dituri F, et al. Down-regulation of connective tissue growth factor by inhibition of transforming growth factor beta blocks the tumor-stroma cross-talk and tumor progression in hepatocellular carcinoma. Hepatology. 2010;51(2):523–34. doi: 10.1002/hep.23285. [DOI] [PubMed] [Google Scholar]
- 138.Herbertz S, Sawyer JS, Stauber AJ, et al. Clinical development of galunisertib (LY2157299 monohydrate), a small molecule inhibitor of transforming growth factor-beta signaling pathway. Drug Des Devel Ther. 2015;9:4479–99. doi: 10.2147/DDDT.S86621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Batlle E, Massagué J. Transforming growth factor-β signaling in immunity and cancer. Immunity. 2019;50(4):924–40. doi: 10.1016/j.immuni.2019.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Biasci D, Smoragiewicz M, Connell CM, et al. CXCR4 inhibition in human pancreatic and colorectal cancers induces an integrated immune response. Proc Natl Acad Sci U S A. 2020;117(46):28960–70. doi: 10.1073/pnas.2013644117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ohshio Y, Teramoto K, Hanaoka J, et al. Cancer-associated fibroblast-targeted strategy enhances antitumor immune responses in dendritic cell-based vaccine. Cancer Sci. 2015;106(2):134–42. doi: 10.1111/cas.12584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Amar S, Minond D, Fields GB. Clinical implications of compounds designed to inhibit ECM-modifying metalloproteinases. Proteomics. 2017 doi: 10.1002/pmic.201600389. [DOI] [PubMed] [Google Scholar]
- 143.Chauhan VP, Martin JD, Liu H, et al. Angiotensin inhibition enhances drug delivery and potentiates chemotherapy by decompressing tumour blood vessels. Nat Commun. 2013;4:2516. doi: 10.1038/ncomms3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Morosi L, Meroni M, Ubezio P, et al. PEGylated recombinant human hyaluronidase (PEGPH20) pre-treatment improves intra-tumour distribution and efficacy of paclitaxel in preclinical models. J Exp Clin Cancer Res. 2021;40(1):286. doi: 10.1186/s13046-021-02070-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT02699606. Accessed 1 Dec 2021.
- 146.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT03762122. Accessed 1 Dec 2021.
- 147.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT03386721. Accessed 1 Dec 2021.
- 148.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT02627274. Accessed 1 Dec 2021.
- 149.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT03875079. Accessed 1 Dec 2021.
- 150.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT03834220. Accessed 1 Dec 2021.
- 151.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT03822117. Accessed 1 Dec 2021.
- 152.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT02872714. Accessed 1 Dec 2021.
- 153.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT02924376. Accessed 1 Dec 2021.
- 154.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT02399215. Accessed 1 Dec 2021.
- 155.US National Library of Medicine. ClinicalTrials.gov. 2020. https://clinicaltrials.gov/ct2/show/NCT02834780. Accessed 1 Dec 2021.
- 156.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT03343301. Accessed 1 Dec 2021.
- 157.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT02432274. Accessed 1 Dec 2021.
- 158.US National Library of Medicine. ClinicalTrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT02508467. Accessed 1 Dec 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.