Abstract
Background
Glioblastoma (GBM) is the most frequent and lethal brain tumor, which possesses highly malignant characteristics and predominates in elder patients. Systemic inflammatory response index (SIRI) is a novel prognostic marker from peripheral blood, which is defined as neutrophil count × monocyte count/lymphocyte count. In the current research, we aim to explore the relationship between SIRI and newly diagnosed GBM underwent gross total resection (GTR).
Methods
A retrospective analysis was conducted on consecutive newly diagnosed GBM patients underwent operation at West China Hospital from March 2015 to January 2019. X-tile software was used to determine the optimal cut-off values of SIRI, and neutrophil to lymphocyte ratio (NLR). All statistical analyses were performed using SPSS software and R software. Propensity score matching (PSM) was conducted to adjust for imbalance of all potential confounding covariates.
Results
The current research included a total of 291 consecutive newly diagnosed GBM patients underwent gross total resection. Among them, 186 were male patients and 105 were female patients. In original cohort, only gender was evidently related to SIRI level. SIRI and NLR were independent prognostic indicators both in original cohort and PSM cohort. Prognostic models based on the independent prognostic factors were established, and prognostic capacity of Model SIRI was superior to Model NLR.
Conclusion
In the current research, SIRI was determined to be an independent prognostic indicator for GBM. And the prognostic predictive ability of SIRI was stronger than NLR.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12957-022-02588-0.
Keywords: Systemic inflammation response index (SIRI), Neutrophil to lymphocyte ratio (NLR), Glioblastoma (GBM), Gross total resection (GTR), Prognosis
Introduction
Glioblastoma (GBM) is the most common and lethal primary brain tumor, which is highly invasive but not metastatic, namely, it is confined to the central nervous system [1]. The median survival is 15 months in GBM patients who have though accepted aggressive combination of therapies including maximal safe resection, adjuvant radiotherapy, and adjuvant temozolomide (TMZ) treatment [2]. This incurable malignancy brings heavy financial burden on health care system all over the world. Surgery dominates various therapeutic schemes. Compared with subtotal resection (STR) and biopsy, gross total resection (GTR) is proved to effectively prolong overall survival (OS) and progression-free survival (PFS) [3, 4].
Inflammation is deemed as a hallmark of cancer development and progression, which is essential for tumor growth, invasion, angiogenesis, and metastasis [5, 6]. Systemic inflammation varies in development with tumor type and stage, and it remains unclear about the complicated mechanisms of systemic inflammatory response in in cancer patients [7]. Lots of peripheral blood-related inflammatory markers have been applied in clinical practice to determine and quantify the systemic inflammatory response. The representative markers include neutrophil to lymphocyte ratio (NLR), derived NLR (dNLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR), and Glasgow prognostic score (GPS). These markers are confirmed to have strong prognostic and predictive abilities in various tumors [7–13]. Compared with the above-mentioned markers, systemic inflammatory response index (SIRI) is a novel prognostic marker. And SIRI is reported to play a significant prognostic role in cancers like cervical cancer, head and neck squamous cell carcinoma, breast cancer, and gallbladder cancer [14–18].
Malignant progression of glioma is also connected with systemic inflammatory response. Preoperative hematological markers levels vary among glioma grades and have predictive ability [19]. Although the pathophysiological mechanisms of systemic inflammatory response of glioma also remains unknown, there is a hypothesis that it is generated when local inflammatory cells leak into the circulatory system from broken blood-brain barrier. As regard to GBM, it is reported that the markers including NLR, PLR, systemic immune-inflammation (SII), and prognostic nutrition index (PNI) have strong prognostic abilities in specific patient populations [20–23]. In the current research, we aim to explore the relationship between SIRI and newly diagnosed GBM with GTR. And with propensity score matching, we will further evaluate the prognostic value of SIRI in GBM patients.
Materials and methods
Patients
This was a retrospective analysis on consecutive newly diagnosed GBM patients who had underwent operation at West China Hospital from March 2015 to January 2019. All these patients underwent a craniotomy on GBM with GTR, and their baseline clinical data were retrieved from the electronic medical record system. The extent of resection was determined by surgical records and postoperative imaging including MRI and CT within 72 h after surgery. The pathological diagnosis criteria were followed the 2016 WHO classification of CNS tumors, and two independent pathologists verified the diagnoses of tumor specimens before 2017. These patients were followed up until January 2021.
The exclusion criteria were (1) younger than 18-year-old; (2) not GTR; (3) absence of definite pathological diagnosis; (4) incomplete baseline clinical data; (5) absence of preoperative magnetic resonance imaging (MRI); (6) receiving adjuvant therapy before operation; (7) receiving corticosteroids therapy before admission; (8) presence of history of infectious diseases or blood system diseases or in a low nutrition condition before surgery; (9) recurrent; (10) lost to follow-up at any stage of the disease.
Parameters assessment
The following clinical variables were retrieved from electronic medical record system: gender, age at diagnosis, preoperative Karnofsky performance status (KPS) score, presence of preoperative seizures, tumor locations, Ki-67 index, status of isocitrate dehydrogenase 1 (IDH-1), conditions of adjuvant therapy, and blood test results. Routine blood test was conducted within 1 week before operation. SIRI was defined as neutrophil count × monocyte count/lymphocyte count, and NLR was defined as neutrophil count/lymphocyte count.
After initial treatment, the patients were followed up every 3 months in the first year, and every 6 months thereafter. OS was defined as the duration from the date of operation to death or the end of the observation period.
Statistical analysis
X-tile software was used to determine the optimal cut-off values of SIRI and NLR [24].
All statistical analyses were performed using SPSS software (Version 22.0, IBM Co., Armonk, NY, USA) and R software (Version 3.6.1). Continuous variables were presented as mean ± standard deviation (SD), and categorical variables were presented as frequency and percentage. Data that conformed to the normal distribution was compared using Student’s t test, otherwise Mann-Whitney U test was applied. Three or more independent groups were compared by using one-way analysis of variance (ANOVA) or Kruskal-Wallis test. Kaplan-Meier (K-M) curves were applied to calculate cumulative OS using the log-rank test. The Cox regression analysis were employed to determine the influences of risk factors for overall survival in GBM patients. Univariate Cox regression was firstly conducted to evaluate clinical variables, then variables with p value< 0.1 were included into backward stepwise multivariate Cox regression. Harrell’s concordance index (C-index) and Akaike information criterion (AIC) were calculated to evaluate different prognostic models. A higher C-index and a lower AIC indicated better predictive performance [25]. A two-sided p value < 0.05 referred as statistically significant difference.
Propensity score matching was conducted to adjust for imbalance of all potential confounding covariates: gender, age at diagnosis, KPS, presence of preoperative seizures, tumor locations, Ki-67 index, IDH-1 mutation status, and conditions of adjuvant therapy. These patients were matched 1:1 using the nearest-neighbor algorithm with a caliper width of 0.2 and without replacement.
Results
Baseline characteristics
After screening (Fig. 1), a total of 291 consecutive newly diagnosed GBM patients including 186 men and 105 women underwent gross total resection were included in the current research. (Table 1) The mean and median OS were 435.6 days and 355 days respectively, ranging from 31 to 1580 days. The mean and median age at diagnosis in the cohort was 53.7 and 54 years respectively. Among them, 40 patients had preoperative seizures, and 108 patients had better KPS score (> 80). The number of tumors in left and right hemispheres was roughly the same (144 vs 132), while 15 cases had tumors in midline area or involving both sides of the brain. As regard to tumor location, 98 foci were located at frontal lobes, 59 at temporal lobes, 26 at parietal lobes, 8 at occipital lobes, 12 at insular lobes, while 88 GBMs involved multiple lobes, structures, or cerebellum. A total of 230 patients received chemotherapy and radiotherapy, and most of the treatments were performed according to the Stupp’s regimen which contained 42–day concomitant radiochemotherapy and subsequent 6–12 consecutive cycles of temozolomide alone. The other 61 patients did not receive chemotherapy or radiotherapy or abandoned treatment at an early stage due to the deteriorative physical condition or severe side effects. Two pathological biomarkers were included in clinical variables. Ki-67 index greater than or equal to 30% was observed in 121 GBMS, and IDH-1 mutation was found in 42 patients.
Fig. 1.
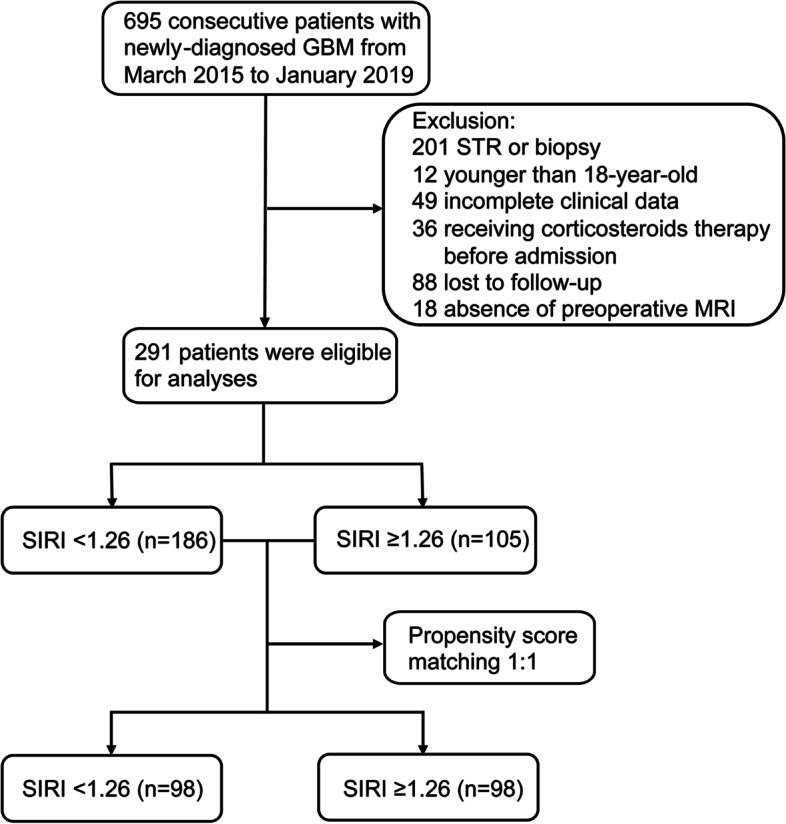
Flow chart of the current study. Abbreviations: GBM, glioblastoma; STR, subtotal resection; MRI, magnetic resonance imaging; SIRI, systemic inflammation response index
Table 1.
Baseline clinical characteristics of glioblastoma patients in original and PSM cohort
| Clinical characteristic | Original cohort | PSM cohort | |
|---|---|---|---|
| Sample size | 291 (100) | 196 (100) | |
| Overall survival | Mean ± SD (day) | 435.6 ± 314.0 | 389.2 ± 282.8 |
| Median (range) | 355 (31–1580) | 304 (31–1580) | |
| Age at diagnosis | Mean ± SD (year) | 53.7 ± 14.2 | 54.2 ± 13.8 |
| Median (range) | 54 (18–85) | 55 (19–85) | |
| Gender | Male | 186 (63.9) | 147 (75.0) |
| Female | 105 (36.1) | 49 (25.0) | |
| Preoperative seizures | Yes | 40 (13.7) | 28 (14.3) |
| No | 251 (86.3) | 168 (85.7) | |
| Karnofsky performance status | ≤ 80 | 183 (62.9) | 123 (62.8) |
| > 80 | 108 (37.1) | 73 (37.2) | |
| Hemisphere | Right | 132 (45.4) | 89 (45.4) |
| Left | 144 (49.5) | 98 (50.0) | |
| Midline or bilateral | 15 (5.1) | 9 (4.6) | |
| Location | Frontal lobe | 98 (33.7) | 60 (30.6) |
| Temporal lobe | 59 (20.3) | 43 (21.9) | |
| Parietal lobe | 26 (8.9) | 18 (9.2) | |
| Occipital lobe | 8 (2.7) | 3 (1.5) | |
| Insular lobe | 12 (4.1) | 10 (5.1) | |
| Other locations | 88 (30.2) | 62 (31.6) | |
| Adjuvant therapy | Yes | 230 (79.0) | 156 (79.6) |
| No or undone | 61 (23.0) | 40 (20.4) | |
| Ki-67 | < 30% | 170 (58.4) | 119 (60.7) |
| ≥ 30% | 121 (41.6) | 77 (39.3) | |
| IDH-1 | Mutant | 42 (14.4) | 27 (13.8) |
| Wildtype | 249 (85.6) | 169 (86.2) | |
| SIRI | < 1.26 | 177 (60.8) | 98 (50.0) |
| ≥ 1.26 | 114 (39.2) | 98 (50.0) | |
| NLR | < 4.86 | 237 (81.4) | – |
| ≥ 4.86 | 54 (18.6) | – | |
| < 4.63 | – | 146 (74.5) | |
| ≥ 4.63 | – | 50 (25.5) | |
Data are presented as n (%)
Abbreviations: IDH-1 isocitrate dehydrogenase-1, SIRI systemic inflammation response index, NLR neutrophil to lymphocyte ratio, PSM propensity score matching
The optimal cut-off points of SIRI and NLR were 1.26 and 4.86 respectively (Supplementary Figure 1). In the original cohort, 177 patients showed SIRI < 1.26 while 114 with SIRI ≥ 1.26, and 237 patients had NLR < 4.86 while NLR≥4.86 was found in 54 patients.
To reveal the potential confounding bias between patients with SIRI level < 1.26 and ≥ 1.26, PSM was performed and a new cohort including 196 patients was available for further analyses. Clinical characteristics of patients in PSM cohort were listed in Table 1. Of note, after PSM, the optimal cut-off value of NLR was changed to 4.63 (Supplementary Figure 1). NLR < 4.63 and NLR ≥ 4.63 were found in 146 and 50 patients respectively.
Association between SIRI and clinical variables
As shown in Table 2, in original cohort, only gender was evidently related to SIRI level (p < 0.001), which indicated that male patients tended to have higher SIRI. In PSM cohort, there was not any clinical variable significantly associated with SIRI.
Table 2.
Relationship between SIRI and clinical variables
| Clinical variables | Original cohort | PSM cohort | |||||
|---|---|---|---|---|---|---|---|
| SIRI < 1.26 (n = 177) | SIRI ≥ 1.26 (n = 114) | p value | SIRI < 1.26 (n = 98) | SIRI ≥ 1.26 (n = 98) | p value | ||
| Age at diagnosis | < 55 | 94 | 55 | 0.933 | 50 | 46 | 0.988 |
| ≥ 55 | 83 | 59 | – | 48 | 52 | – | |
| Gender | Male | 96 | 90 | < 0.001 | 73 | 74 | 0.177 |
| Female | 81 | 24 | – | 25 | 24 | – | |
| Preoperative seizure | Yes | 25 | 15 | 0.83 | 15 | 13 | 0.974 |
| No | 152 | 99 | – | 83 | 85 | – | |
| KPS | ≤ 80 | 103 | 80 | 0.396 | 59 | 64 | 0.959 |
| > 80 | 74 | 34 | – | 39 | 34 | – | |
| Hemisphere | Right | 74 | 58 | 0.11 | 43 | 46 | 0.465 |
| Left | 94 | 50 | 51 | 47 | – | ||
| Midline or bilateral | 9 | 6 | – | 4 | 5 | – | |
| Tumor location | Frontal lobe | 70 | 28 | 0.088 | 32 | 28 | 0.136 |
| Temporal lobe | 29 | 30 | – | 16 | 27 | – | |
| Parietal lobe | 20 | 6 | – | 12 | 6 | – | |
| Occipital lobe | 6 | 2 | – | 1 | 2 | – | |
| Insular lobe | 7 | 5 | – | 5 | 5 | – | |
| Other regions | 45 | 43 | – | 32 | 30 | – | |
| Ki-67 index | < 30% | 105 | 65 | 0.636 | 63 | 56 | 0.217 |
| ≥ 30% | 72 | 49 | – | 35 | 42 | – | |
| IDH-1 status | Mutant | 29 | 13 | 0.531 | 15 | 12 | 0.491 |
| Wildtype | 148 | 101 | – | 83 | 86 | – | |
Significant findings are expressed in bold and italic
Abbreviations: KPS Karnofsky performance status, IDH-1 isocitrate dehydrogenase-1, SIRI systemic inflammation response index, NLR neutrophil to lymphocyte ratio, PSM propensity score matching
Prognostic value of SIRI
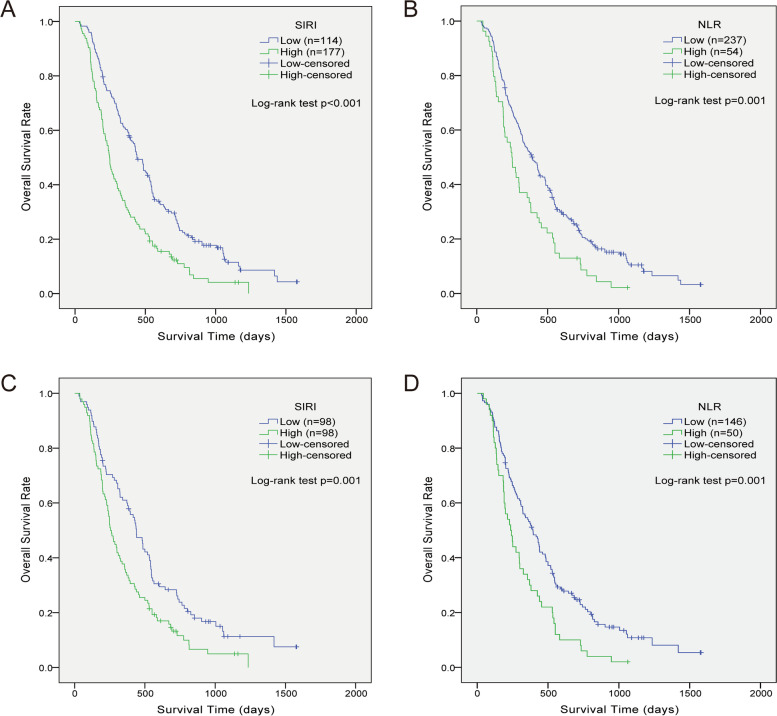
K-M curves indicated the reliability of optimal cut-off points (Fig. 2). In univariate Cox regression, age at diagnosis, gender, KPS, adjuvant therapy, IDH-1 status, NLR, and SIRI were considered to affect OS (p < 0.05) in original cohort (Table 3). After multivariate analysis, age (HR1.314, 95% CI 1.011–1.707, p = 0.041), gender (HR 0.699, 95% CI 0.528-0.925, p = 0.012), adjuvant therapy (HR 2.151, 95%CI 1.587–2.916, p < 0.001), Ki-67 index (HR 1.316, 95%CI 1.019–1.699, p = 0.036), IDH-1 status (HR 2.384, 95% CI 1.560–3.643, p < 0.001), SIRI (HR 1.646, 95%CI 1.253–2.163, p < 0.001), and NLR (HR 1.392, 95% CI 1.013–1.912, p = 0.041) were confirmed as independent predictors for OS.
Fig. 2.
Kaplan-Meier curves showing overall survival of GBM patients stratified by value of SIRI (A, C) and NLR (B, D) in original and PSM cohort respectively. Abbreviations: SIRI, systemic inflammation response index; NLR, neutrophil to lymphocyte ratio; PSM, propensity score matching
Table 3.
Univariate and multivariate Cox regression for risk factors predictive of GBM in original cohort
| Clinical variables | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | ||
| Age at diagnosis | < 55 | Reference | – | – | Reference | – | – |
| ≥ 55 | 1.699 | 1.325–2.180 | < 0.001 | 1.314 | 1.011–1.707 | 0.041 | |
| Gender | Male | Reference | – | – | Reference | – | – |
| Female | 0.626 | 0.482–0.814 | < 0.001 | 0.699 | 0.528–0.925 | 0.012 | |
| KPS | ≤ 80 | Reference | – | – | Reference | – | – |
| > 80 | 0.741 | 0.573–0.958 | 0.022 | 0.874 | 0.670–1.141 | 0.322 | |
| Hemisphere | Right | Reference | – | – | – | – | – |
| Left | 0.826 | 0.641–1.064 | 0.139 | – | – | – | |
| Midline or bilateral | 1.478 | 0.848–2.575 | 0.168 | – | – | – | |
| Frontal lobe | Reference | – | – | – | – | – | |
| Temporal lobe | 1.314 | 0.935–1.847 | 0.115 | – | – | – | |
| Location | Parietal lobe | 0.893 | 0.553–1.443 | 0.645 | – | – | – |
| Occipital lobe | 0.923 | 0.426–2.002 | 0.84 | – | – | – | |
| Insular lobe | 0.929 | 0.466–1.850 | 0.834 | – | – | – | |
| Other regions | 1.632 | 1.198–2.222 | 0.002 | – | – | – | |
| Preoperative seizures | No | Reference | – | – | – | – | – |
| Yes | 1.231 | 0.868–1.747 | 0.244 | – | – | – | |
| Adjuvant therapy | Yes | Reference | – | – | Reference | – | – |
| No or undone | 2.059 | 1.533–2.764 | < 0.001 | 2.151 | 1.587–2.916 | < 0.001 | |
| Ki67 | < 30% | Reference | – | – | Reference | – | – |
| ≥30% | 1.261 | 0.983–1.618 | 0.068 | 1.316 | 1.019–1.699 | 0.036 | |
| IDH-1 | Mutant | Reference | – | – | Reference | – | – |
| Wildtype | 2.867 | 1.917–4.288 | < 0.001 | 2.384 | 1.560–3.643 | < 0.001 | |
| SIRI | Low | Reference | – | – | Reference | – | – |
| High | 1.843 | 1.431-2.373 | < 0.001 | 1.646 | 1.253–2.163 | < 0.001 | |
| NLR | Low | Reference | – | – | Reference | – | – |
| High | 1.67 | 1.228-2.270 | 0.001 | 1.392 | 1.013–1.912 | 0.041 | |
Significant findings are expressed in bold and italic
Abbreviations: HR hazard ratio, CI confidence interval, KPS Karnofsky performance status, IDH-1 isocitrate dehydrogenase-1, SIRI systemic inflammation response index, NLR neutrophil to lymphocyte ratio, PSM propensity score matching
As shown in Table 4, in PSM cohort, similarly, SIRI (HR 1.641, 95% CI 1.206–2.234, p = 0.002) and NLR (HR 1.570, 95% CI 1.108–2.226, p = 0.011) were independent prognostic indicators based on the results of multivariate Cox regression. Other independent indicators included age at diagnosis, condition of adjuvant therapy, and IDH-1 status.
Table 4.
Univariate and multivariate Cox regression for risk factors predictive of GBM in PSM cohort
| Clinical variables | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | – | ||
| Age at diagnosis | < 55 | Reference | – | – | Reference | – | – |
| ≥ 55 | 1.976 | 1.447–2.697 | < 0.001 | 1.441 | 1.042–1.993 | 0.027 | |
| Gender | Male | Reference | – | – | Reference | – | – |
| Female | 0.613 | 0.429–0.875 | 0.007 | 0.758 | 0.521–1.101 | 0.146 | |
| KPS | ≤ 80 | Reference | – | – | Reference | – | – |
| > 80 | 0.745 | 0.543–1.022 | 0.068 | 0.83 | 0.598-1.153 | 0.267 | |
| Hemisphere | Right | Reference | – | – | – | – | – |
| Left | 0.982 | 0.724–1.332 | 0.906 | – | – | – | |
| Midline or bilateral | 1.772 | 0.817–3.846 | 0.148 | – | – | – | |
| Frontal lobe | Reference | – | – | – | – | – | |
| Temporal lobe | 1.407 | 0.930–2.130 | 0.106 | – | – | – | |
| Location | Parietal lobe | 0.892 | 0.502–1.586 | 0.698 | – | – | – |
| Occipital lobe | 0.870 | 0.314–2.416 | 0.790 | – | – | – | |
| Insular lobe | 0.734 | 0.333–1.620 | 0.444 | – | – | – | |
| Other regions | 1.353 | 0.924–1.980 | 0.121 | – | – | – | |
| Preoperative seizures | No | Reference | – | – | – | – | – |
| Yes | 1.136 | 0.725–1.780 | 0.578 | – | – | – | |
| Adjuvant therapy | Yes | Reference | – | – | Reference | – | – |
| No or undone | 1.751 | 1.211–2.533 | 0.003 | 1.685 | 1.158-2.451 | 0.006 | |
| Ki67 | < 30% | Reference | – | – | – | – | – |
| ≥ 30% | 1.206 | 0.890–1.635 | 0.227 | – | – | – | |
| IDH-1 | Mutant | Reference | – | – | Reference | – | – |
| Wildtype | 3.327 | 1.989–5.566 | < 0.001 | 2.958 | – | < 0.001 | |
| SIRI | Low | Reference | – | – | Reference | – | – |
| High | 1.637 | 1.209–2.217 | 0.001 | 1.641 | – | 0.002 | |
| NLR | Low | Reference | – | – | Reference | – | – |
| High | 1.751 | 1.253–2.447 | 0.001 | 1.57 | 1.108–2.226 | 0.011 | |
Significant findings are expressed in bold and italic
Abbreviations: HR hazard ratio, CI confidence interval, KPS Karnofsky performance status, IDH-1 isocitrate dehydrogenase-1, SIRI systemic inflammation response index, NLR neutrophil to lymphocyte ratio, PSM propensity score matching
Prognostic model based on SIRI and NLR
To compare the prognostic ability of SIRI and NLR in the current two cohorts, prognostic models were established based on the independent prognostic factors (Table 5). In original cohort, in addition to SIRI and NLR, other 5 variables including age at diagnosis, gender, adjuvant therapy, Ki-67 index, and IDH-1 status were involved in the composition of the models. Model SIRI had higher C-index and lower AIC compared with Model NLR (C-index 0.672 VS 0.659, AIC 2410.09 VS 2418.68). In PSM cohort, each model had 4 variables. As the same, prognostic ability of Model SIRI was superior to that of Model NLR (C-index 0.656 VS 0.650, AIC 1516.63 VS 1518.11).
Table 5.
Prognostic model based on SIRI and NLR for GBM patients
| Clinical variables | Prognostic models | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Original cohort (model SIRI) | Original cohort (model NLR) | PSM cohort (model SIRI) | PSM cohort (model NLR) | ||||||||||
| HR | 95% CI | p value | HR | 95% CI | p value | HR | 95% CI | p value | HR | 95% CI | p value | ||
| Age at diagnosis | < 55 | Reference | – | – | Reference | – | – | Reference | – | – | Reference | – | – |
| ≥ 55 | 1.314 | 1.011–1.707 | 0.041 | 1.340 | 1.032–1.740 | 0.028 | 1.441 | 1.042–1.993 | 0.027 | 1.516 | 1.099–2.090 | 0.011 | |
| Gender | Male | Reference | – | – | Reference | – | – | – | – | – | – | – | – |
| Female | 0.699 | 0.528–0.925 | 0.012 | 0.618 | 0.473–0.807 | < 0.001 | – | – | – | – | – | – | |
| Adjuvant therapy | Yes | Reference | – | – | Reference | – | – | Reference | – | – | Reference | – | – |
| No or undone | 2.151 | 1.587–2.916 | < 0.001 | 2.139 | 1.569–2.914 | < 0.001 | 1.685 | 1.158–2.451 | 0.006 | 1.511 | 1.030–2.216 | 0.035 | |
| Ki67 | < 30% | Reference | – | – | Reference | – | – | – | – | – | – | – | – |
| ≥ 30% | 1.316 | 1.019–1.699 | 0.036 | 1.274 | 0.988–1.644 | 0.062 | – | – | – | – | – | – | |
| IDH-1 | Mutant | Reference | – | – | Reference | – | – | Reference | – | – | Reference | – | – |
| Wildtype | 2.384 | 1.560–3.643 | < 0.001 | 2.404 | 1.575–3.668 | < 0.001 | 2.958 | 1.729–5.063 | < 0.001 | 2.837 | 1.658–4.855 | < 0.001 | |
| SIRI | Low | Reference | – | – | – | – | – | Reference | – | – | – | – | – |
| High | 1.646 | 1.253-2.163 | < 0.001 | – | – | – | 1.641 | 1.206–2.234 | 0.002 | – | – | – | |
| NLR | Low | – | – | – | Reference | – | – | – | – | – | Reference | – | – |
| High | – | – | – | 1.392 | 1.013–1.912 | 0.041 | – | – | – | 1.601 | 1.132–2.265 | 0.008 | |
| C-index | 0.672 | 0.659 | 0.656 | 0.650 | |||||||||
| AIC | 2410.09 | 2418.68 | 1516.63 | 1518.11 | |||||||||
Significant findings are expressed in bold and italic
Abbreviations: HR hazard ratio, CI confidence interval, IDH-1 isocitrate dehydrogenase-1, SIRI systemic inflammation response index, NLR neutrophil to lymphocyte ratio, PSM propensity score matching, C-index Harrell’s concordance index, AIC Akaike information criterion
Discussion
As grade 4 glioma, GBM possesses highly malignant characteristics and predominates in patients over 55 years of age [26]. Through the years, oncology researchers have stressed on less invasive and convenient methods to detect and monitor tumor growth, progression, and even real-time treatment response. Peripheral blood markers and liquid biopsy markers including circulating tumor cells, circulating tumor DNA, extracellular vesicles, and exosomes certainly have the potential to change the dynamics of cancer management and treatment [27, 28]. In the current research, we attempted to explore the relationship between pretreatment peripheral blood SIRI and newly diagnosed GBM with GTR. We found SIRI can serve as an independent prognosis indicator for newly diagnosed GBM after GTR. Though NLR had similar independent prognostic ability in same cohort, SIRI seemed to have better predictive ability on prognosis.
Hematological markers are of intense interest in current clinical cancer research [29, 30]. These markers are accessible and the tests are mostly harmless so that large-scale prospective and retrospective studies have been conducted. Tumor microenvironment is associated to cascades of inflammation such as platelet activation, stimulation of coagulation, and subsequent release of inflammatory cytokines [6]. Transcription factors, cytokines, chemokines, and infiltrating leukocytes are key orchestrators of the inflammation-mediated tumor progression [31]. Local immune response leads to changes of systemic inflammation, therefore peripheral blood markers are theoretically indirectly connected to tumor progression. In fact, large trials also verify that cancer-related inflammatory markers have prognostic relevance and even interact with adjuvant therapy [32–34].
It is still unclear about the underline mechanism of the relationship between systemic inflammation and tumor prognosis. And it also remains unknown about the specific role of immune cells that are adjacent to or infiltrate into the tumor due to the heterogeneous functions of inflammatory cells that may promote tumor progression, and alternatively may lead to tumor cell destruction [35]. At the same time, tumor-related systemic and local inflammatory responses are considered to be crucial therapeutic targets for cancer treatment. Targeting inflammatory mediators like immune cells, stromal cells, fibroblasts, and endothelial cells might be effective in controlling the inflammatory response in cancer patients [36]. It is an issue about how to tip the balance between cancer-promoting inflammatory responses and cancer-inhibiting inflammatory responses [37].
NLR, the ratio of systemic neutrophils to lymphocytes, has prognostic value in various tumors. In the field of glioma, a meta-analysis included 16 studies from Lei et al. indicated that high NLR was considered a high-risk prognostic factor in gliomas [38]. SIRI, a modified version of NLR, is highly similar to NLR in structure. In previous studies, the optimal cut-off values of pretreatment SIRI ranged from 0.54 to 2.3. In our study, the optimal cut-off value calculated by X-tile software was 1.26, which was within an acceptable range. Several cancer-related studies compared the prognostic ability between SIRI and NLR in the same cohort by using receiver operating characteristic (ROC) curves, and SIRI was found to have stronger predictive capacity than NLR [39–41]. In the current study, we compared the prognostic ability between SIRI and NLR by building prognosis predictive models, which were more precise and reasonable. After adjusting potential confounders by PSM, we got the same results in the new cohort.
There were still some limitations in the current research. Firstly, other important tumor-related biomarkers like O6-methylguanine-DNA methyltransferase (MGMT) and telomerase reverse transcriptase (TERT) status that were related to prognosis were not included in the study due to insufficient pathological data. Secondly, there was not enough participants to divide the original cohort into training group and validation group, which can make results more convincing. Thirdly, there lacked of effective and practical methods to monitor the progression of GBMs after surgery due to the rapid recurrence and high early mortality. Therefore, we did not acquire precise clinical data to calculate progression-free survival, and OS was the only outcome. Fourthly, it is hard for us to regularly collect and analyze the blood from GBM patients at follow-up period, so we cannot proceed further analyses for the relationship between postoperative SIRI and GBM.
Conclusion
To our knowledge, this is the first study focusing on prognostic significance of preoperative SIRI in newly diagnosed GBM patients underwent GTR. In the current research, SIRI was determined to be an independent prognostic marker for overall survival in GBM. And the prognostic predictive capacity of SIRI was stronger than NLR. In the future, systemic inflammation-based prognostic markers could possibly not only identify cancer patients at risk but may also potentially provide precise therapeutic targets for clinical treatment.
Supplementary Information
Additional file 1: Supplementary Figure 1. X-tile software was used to calculate the optimal cut-off values of SIRI in original cohort (A) and NLR in both original (B) and PSM cohort (C). Abbreviations: SIRI, systemic inflammation response index; NLR, neutrophil to lymphocyte ratio; PSM, propensity score matching.
Acknowledgements
We would like to express our gratitude to all the colleagues who have assisted clinical data collection. And we would like to thank to all the glioma patients who were admitted in our hospital who have contributed to the development of medicine.
Abbreviations
- AIC
Akaike information criterion
- ANOVA
Analysis of variance
- C-index
Harrell’s concordance index
- CI
Confidence interval
- GBM
Glioblastoma
- GTR
Gross total resection
- HR
Hazard ratio
- IDH-1
Isocitrate dehydrogenase 1
- K-M
Kaplan-Meier
- KPS
Karnofsky performance status
- LMR
Lymphocyte to monocyte ratio
- MGMT
O6-methylguanine-DNA methyltransferase
- MRI
Magnetic resonance imaging
- NLR
Neutrophil to lymphocyte ratio
- OS
Overall survival
- PSM
Propensity score matching
- PFS
Progression-free survival
- PLR
Platelet to lymphocyte ratio
- PNI
Prognostic nutrition index
- ROC
Receiver operating characteristic
- SD
Standard deviation
- SII
Systemic immune-inflammation
- SIRI
Systemic inflammatory response index
- TMZ
Temozolomide
- TERT
Telomerase reverse transcriptase
Authors’ contributions
Study design: Yanhui Liu, Zhihao Wang. Data retrieval: Junhong Li, Yuanbo Yuan, Zhihao Wang, Mingrong Zuo. Statistical analysis: Junhong Li, Tengfei Li, Zhihao Wang. Result interpretation: Yanhui Liu, Zhihao Wang, Junhong Li. Manuscript preparation: All authors. Text correction: Yanhui Liu. All authors read and approved the final manuscript.
Funding
No funding.
Availability of data and materials
The datasets for this study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of Sichuan University (ethic number 2018NO569) and conducted following the principles of the Declaration of Helsinki. All patients and their authorized trustees were informed and provided signed informed consent to use their clinical data for research purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Omuro A, DeAngelis LM. Glioblastoma and other malignant gliomas: a clinical review. Jama. 2013;310(17):1842–1850. doi: 10.1001/jama.2013.280319. [DOI] [PubMed] [Google Scholar]
- 2.Aldape K, Zadeh G, Mansouri S, Reifenberger G, von Deimling A. Glioblastoma: pathology, molecular mechanisms and markers. Acta Neuropathol. 2015;129(6):829–848. doi: 10.1007/s00401-015-1432-1. [DOI] [PubMed] [Google Scholar]
- 3.Salvati M, Bruzzaniti P, Relucenti M, et al. Retrospective and randomized analysis of influence and correlation of clinical and molecular prognostic factors in a mono-operative series of 122 patients with glioblastoma treated with STR or GTR. Brain Sci. 2020;10(2). [DOI] [PMC free article] [PubMed]
- 4.Brown TJ, Brennan MC, Li M, et al. Association of the extent of resection with survival in glioblastoma: a systematic review and meta-analysis. JAMA Oncol. 2016;2(11):1460–1469. doi: 10.1001/jamaoncol.2016.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–e503. doi: 10.1016/S1470-2045(14)70263-3. [DOI] [PubMed] [Google Scholar]
- 6.Iyengar NM, Gucalp A, Dannenberg AJ, Hudis CA. Obesity and Cancer Mechanisms: Tumor Microenvironment and Inflammation. J Clin Oncol. 2016;34(35):4270–4276. doi: 10.1200/JCO.2016.67.4283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diem S, Schmid S, Krapf M, et al. Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer. 2017;111:176–181. doi: 10.1016/j.lungcan.2017.07.024. [DOI] [PubMed] [Google Scholar]
- 8.Templeton AJ, McNamara MG, Šeruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. doi: 10.1093/jnci/dju124. [DOI] [PubMed] [Google Scholar]
- 9.Li B, Zhou P, Liu Y, et al. Platelet-to-lymphocyte ratio in advanced Cancer: Review and meta-analysis. Clin Chim Acta. 2018;483:48–56. doi: 10.1016/j.cca.2018.04.023. [DOI] [PubMed] [Google Scholar]
- 10.Zhang S, Li M, Yuan F, et al. The predictive value of dynamic monitoring of peripheral blood lymphocyte to monocyte ratio in patients with extranodal NK/T cell lymphoma. Cancer Cell Int. 2019;19:272. doi: 10.1186/s12935-019-0993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan D, Fu Y, Tong W, Li F. Prognostic significance of lymphocyte to monocyte ratio in colorectal cancer: A meta-analysis. Int J Surg. 2018;55:128–138. doi: 10.1016/j.ijsu.2018.05.030. [DOI] [PubMed] [Google Scholar]
- 12.McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–540. doi: 10.1016/j.ctrv.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Jansson H, Cornillet M, Björkström NK, Sturesson C, Sparrelid E. Prognostic value of preoperative inflammatory markers in resectable biliary tract cancer - Validation and comparison of the Glasgow Prognostic Score and Modified Glasgow Prognostic Score in a Western cohort. Eur J Surg Oncol. 2020;46(5):804–810. doi: 10.1016/j.ejso.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Chao B, Ju X, Zhang L, Xu X, Zhao Y. A novel prognostic marker systemic inflammation response index (SIRI) for operable cervical cancer patients. Front Oncol. 2020;10:766. doi: 10.3389/fonc.2020.00766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valero C, Pardo L, Sansa A, et al. Prognostic capacity of systemic inflammation response index (SIRI) in patients with head and neck squamous cell carcinoma. 2020;42(2):336–43. [DOI] [PubMed]
- 16.Hua X, Long ZQ, Huang X, et al. The preoperative systemic inflammation response index (SIRI) independently predicts survival in postmenopausal women with breast cancer. Curr Probl Cancer. 2020;44(4):100560. doi: 10.1016/j.currproblcancer.2020.100560. [DOI] [PubMed] [Google Scholar]
- 17.Wang L, Zhou Y, Xia S, et al. Prognostic value of the systemic inflammation response index (SIRI) before and after surgery in operable breast cancer patients. Cancer Biomark. 2020;28(4):537–547. doi: 10.3233/CBM-201682. [DOI] [PubMed] [Google Scholar]
- 18.Sun L, Hu W, Liu M, et al. High systemic inflammation response index (SIRI) indicates poor outcome in gallbladder cancer patients with surgical resection: a single institution experience in China. Cancer Res Treat. 2020;52(4):1199–1210. doi: 10.4143/crt.2020.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang PF, Meng Z, Song HW, et al. Preoperative changes in hematological markers and predictors of glioma grade and survival. Front Pharmacol. 2018;9:886. doi: 10.3389/fphar.2018.00886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Topkan E, Besen AA, Ozdemir Y, et al. Prognostic value of pretreatment systemic immune-inflammation index in glioblastoma multiforme patients undergoing postneurosurgical radiotherapy plus concurrent and adjuvant temozolomide. 2020;2020:4392189. [DOI] [PMC free article] [PubMed]
- 21.Yang C, Wen HB, Zhao YH, Huang WH, Wang ZF, Li ZQ. Systemic inflammatory indicators as prognosticators in glioblastoma patients: a comprehensive meta-analysis. Front Neurol. 2020;11:580101. doi: 10.3389/fneur.2020.580101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lopes M, Carvalho B, Vaz R, Linhares P. Influence of neutrophil-lymphocyte ratio in prognosis of glioblastoma multiforme. J Neuro-Oncol. 2018;136(1):173–180. doi: 10.1007/s11060-017-2641-3. [DOI] [PubMed] [Google Scholar]
- 23.Liang R, Li J, Tang X, Liu Y. The prognostic role of preoperative systemic immune-inflammation index and albumin/globulin ratio in patients with newly diagnosed high-grade glioma. Clin Neurol Neurosurg. 2019;184:105397. doi: 10.1016/j.clineuro.2019.105397. [DOI] [PubMed] [Google Scholar]
- 24.Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004;10(21):7252–7259. doi: 10.1158/1078-0432.CCR-04-0713. [DOI] [PubMed] [Google Scholar]
- 25.Vrieze SI. Model selection and psychological theory: a discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC) Psychol Methods. 2012;17(2):228–243. doi: 10.1037/a0027127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 27.Shankar GM, Balaj L, Stott SL, Nahed B, Carter BS. Liquid biopsy for brain tumors. Expert Rev Mol Diagn. 2017;17(10):943–947. doi: 10.1080/14737159.2017.1374854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vaidyanathan R, Soon RH, Zhang P, Jiang K, Lim CT. Cancer diagnosis: from tumor to liquid biopsy and beyond. Lab Chip. 2018;19(1):11–34. doi: 10.1039/c8lc00684a. [DOI] [PubMed] [Google Scholar]
- 29.Ocana A, Nieto-Jiménez C, Pandiella A, Templeton AJ. Neutrophils in cancer: prognostic role and therapeutic strategies. Mol Cancer. 2017;16(1):137. doi: 10.1186/s12943-017-0707-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coffelt SB, Wellenstein MD, de Visser KE. Neutrophils in cancer: neutral no more. Nat Rev Cancer. 2016;16(7):431–446. doi: 10.1038/nrc.2016.52. [DOI] [PubMed] [Google Scholar]
- 31.Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30(7):1073–1081. doi: 10.1093/carcin/bgp127. [DOI] [PubMed] [Google Scholar]
- 32.Yao D, Dong M, Dai C, Wu S. Inflammation and inflammatory cytokine contribute to the initiation and development of ulcerative colitis and its associated cancer. Inflamm Bowel Dis. 2019;25(10):1595–1602. doi: 10.1093/ibd/izz149. [DOI] [PubMed] [Google Scholar]
- 33.Alfaro C, Sanmamed MF, Rodríguez-Ruiz ME, et al. Interleukin-8 in cancer pathogenesis, treatment and follow-up. Cancer Treat Rev. 2017;60:24–31. doi: 10.1016/j.ctrv.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 34.Masson-Lecomte A, Rava M, Real FX, Hartmann A, Allory Y, Malats N. Inflammatory biomarkers and bladder cancer prognosis: a systematic review. Eur Urol. 2014;66(6):1078–1091. doi: 10.1016/j.eururo.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 35.Deans C, Wigmore SJ. Systemic inflammation, cachexia and prognosis in patients with cancer. Curr Opin Clin Nutr Metab Care. 2005;8(3):265–269. doi: 10.1097/01.mco.0000165004.93707.88. [DOI] [PubMed] [Google Scholar]
- 36.Shinko D, Diakos CI, Clarke SJ, Charles KA. Cancer-related systemic inflammation: the challenges and therapeutic opportunities for personalized medicine. Clin Pharmacol Ther. 2017;102(4):599–610. doi: 10.1002/cpt.789. [DOI] [PubMed] [Google Scholar]
- 37.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 38.Lei YY, Li YT, Hu QL, Wang J, Sui AX. Prognostic impact of neutrophil-to-lymphocyte ratio in gliomas: a systematic review and meta-analysis. World J Surg Oncol. 2019;17(1):152. doi: 10.1186/s12957-019-1686-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Z, Ge H, Miao Z, Shao S, Shi H, Dong C. Dynamic changes in the systemic inflammation response index predict the outcome of resectable gastric cancer patients. Front Oncol. 2021;11:577043. doi: 10.3389/fonc.2021.577043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen Z, Wang K, Lu H, et al. Systemic inflammation response index predicts prognosis in patients with clear cell renal cell carcinoma: a propensity score-matched analysis. Cancer Manag Res. 2019;11:909–919. doi: 10.2147/CMAR.S186976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen Y, Jin M, Shao Y, Xu G. Prognostic value of the systemic inflammation response index in patients with adenocarcinoma of the oesophagogastric junction: a propensity score-matched analysis. 2019;2019:4659048. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Figure 1. X-tile software was used to calculate the optimal cut-off values of SIRI in original cohort (A) and NLR in both original (B) and PSM cohort (C). Abbreviations: SIRI, systemic inflammation response index; NLR, neutrophil to lymphocyte ratio; PSM, propensity score matching.
Data Availability Statement
The datasets for this study are available from the corresponding author on reasonable request.