A middle-aged patient presented with mild facial dysmorphisms, small teeth with enamel hypoplasia, progressive gait disturbances, memory problems, and history of syndactyly, corrected in early childhood. MRI showed a hypomyelination pattern compatible with oculodentaldigital dysplasia (ODDD)1,2 (Figure 1). Ophthalmic findings revealed severe bilateral myopia. Exome sequencing revealed a heterozygous GJA1 missense variant (p.Gly138Asp). The patient's mother (deceased) had developed slowly progressive neurodegeneration, ataxia, and seizures. MRI (age 80) revealed extensive leukodystrophic changes (Figure 2). ODDD diagnosis is often missed, highlighting the importance of clinical suspicion, MRI, and molecular testing in adult patients with facial, dental, and neurologic clinical features.
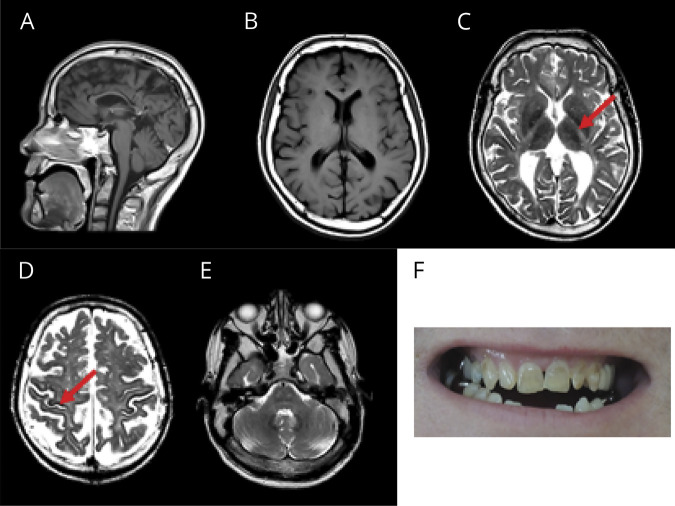
Figure 1. Patient’s MRI and Teeth.
(A) MRI reveals thin corpus callosum and mild vermian atrophy. Axial T1 and T2 images show diffuse hypomyelination (B, C) with typical involvement of the posterior limb of the internal capsule (C, arrow), pons (corticospinal tracts, medial lemniscus, raphe pontis), and cerebellar peduncles (E) with hypointensity of the rolandic cortex (D, arrow) and dentate nucleus. (F) Dental abnormalities.
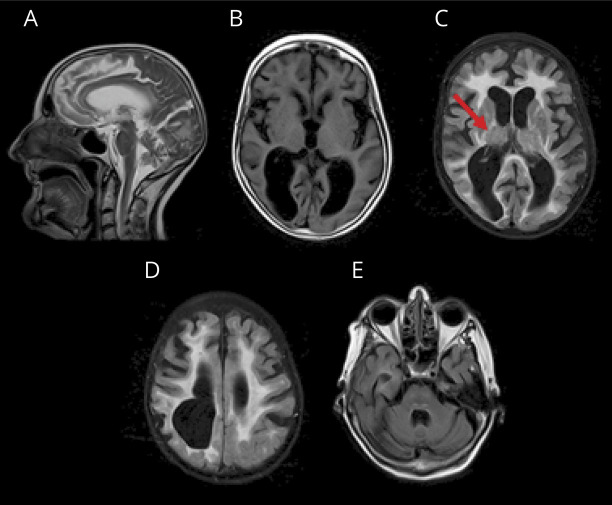
Figure 2. Mother's MRI.
(A) Thin corpus callosum, ventriculomegaly (atrophy), and cerebellar vermis atrophy on sagittal T2 image. (B) Axial T1 image shows ventriculomegaly and significant posterior white matter atrophy. Fluid-attenuated inversion recovery images reveal diffuse white matter hyperintensity (C, D) involving the posterior limb of the internal capsule (C, arrow) and corticospinal tracts and medial lemniscus in the pons (E).
This study was approved by the Montreal Children's Hospital and McGill University Health Center research ethics boards (11-105-PED; 2019-4972).
Acknowledgment
The authors thank the patient and his family for participation; McGill University and Genome Quebec Innovation Center; and Compute Canada (computecanada.ca) for support.
Appendix. Authors
Study Funding
Canadian Institutes for Health Research (project grant 426534 and 201610PJT-377869).
Disclosure
G. Bernard was a consultant for Passage Bio Inc. and Ionis; serves on the scientific advisory board of the Pelizaeus Merzbacher Foundation; is the Chair of the Medical Advisory Board of the United Leukodystrophy Foundation; is on the editorial board of Neurology Genetics, Frontiers in Neurology Neurogenetics, and Journal of Medical Genetics; is a site investigator for the GM1 gangliosidosis and Krabbe gene therapy trials of Passage Bio, Alexander disease trial of Ionis, metachromatic leukodystrophy trial of Shire/Takeda, and adrenoleukodystrophy/hematopoietic stem cell transplantation natural history study of Bluebird Bio; and is a sub-I for the Hunter syndrome gene therapy trial of REGENXBIO. W. Koehler receives research support from Alexion, Bluebird Bio, and MedDay; is consultant and coinvestigator for the AMN disease trial of Minoryx; and serves on scientific advisory boards of the United Leukodystrophy Foundation, the European Leukodystrophy Association, and the Myelin Project Germany. G. Bernard has received the Clinical Research Scholar Junior 1 award from the Fonds de Recherche du Quebec–Santé (FRQS) (2012–2016), the New Investigator Salary Award from the Canadian Institutes of Health Research (2017–2022), and the Clinical Research Scholar Senior from the FRQS (2022–2025). S. Perrier is supported by the FRQS Doctoral Scholarship, the Fondation du Grand défi Pierre Lavoie Doctoral Scholarship, the McGill Faculty of Medicine F.S.B. Miller Fellowship, and the Research Institute of the McGill University Health Centre Desjardins Studentship in Child Health Research. M. Michell-Robinson is supported by the Vanier Canada Graduate Scholarship and the McGill University Faculty of Medicine. The other authors have no disclosures to report. Go to Neurology.org/N for full disclosures.
References
- 1.Harting I, Karch S, Moog U, Seitz A, Pouwels PJW, Wolf NI. Oculodentodigital dysplasia: a hypomyelinating leukodystrophy with a characteristic MRI pattern of brain stem involvement. Am J Neuroradiol. 2019;40:903-907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paznekas WA, Boyadjiev SA, Shapiro RE, et al. Connexin 43 (GJA1) mutations cause the pleiotropic phenotype of oculodentodigital dysplasia. Am J Hum Genet. 2003;72:408-418. [DOI] [PMC free article] [PubMed] [Google Scholar]