Abstract
Fourteen of 22 (68%) Mycobacterium bovis strains isolated from cattle in Sardinia were found to be resistant to rifampin and isoniazid. Analysis of the rpoB and the katG, oxyR-ahpC, and inhA gene regions of these strains was performed in order to investigate the molecular basis of rifampin and isoniazid resistance, respectively. The most frequent mutation, encountered in 6 of 10 strains (60%), was in the rpoB gene; it occurred, at codon position 521 and resulted in leucine changed to proline. This suggests that codon 521 may be important for the development of rifampin resistance in M. bovis. Resistance to isoniazid is associated in Mycobacterium tuberculosis with a variety of mutations affecting one or more genes. Our results confirm the difficulty of interpreting the sequence variations observed in clinical strains of M. bovis. M. bovis strains isolated from the same geographic area showed similar mutations within the genes responsible for rifampin and isoniazid resistance. Our results represent the first study to elucidate the molecular genetic basis of drug resistance in M. bovis isolated from cattle.
Mycobacterium bovis is the major cause of tuberculosis in domestic animals and can produce human disease which is indistinguishable from that caused by Mycobacterium tuberculosis (6, 8). In many industrialized countries, M. bovis has been eradicated from cattle or reduced to very low levels through the implementation of control programs based on test-and-slaughter principles. Bovine tuberculosis continues to be a major problem in countries which cannot afford such programs or where these programs have been only partially effective due to wildlife reservoirs of infection (6). These include the badger in the United Kingdom and the brush-tailed opossum in New Zealand (4, 5). In Sardinia, as a result of an eradication program, bovine tuberculosis was considered eradicated in 1964. Recently various M. bovis strains have been isolated from different herds (17); one of these strains was isolated from an animal imported from Cremona (northern Italy) in 1996. Moreover various wild animals present in Sardinia, such as the mouflon and the wild boar (Sus scrofa), could be reservoirs for M. bovis (2).
The molecular basis of multidrug-resistant (MDR) tuberculosis has been well documented (3, 13, 14). The most common mechanisms of resistance to the primary antimycobacterial agents such as rifampin, isoniazid, and streptomycin in M. tuberculosis are mutations in the target genes. Consequently, virtually all isolates resistant to rifampin and related rifamycins carry mutations affecting a 27-amino-acid region of the coding sequence of the RNA polymerase beta subunit (15). The majority of isoniazid-resistant isolates carry mutations in the katG and inhA genes (13). Limited data are available regarding the genetic assessment of drug-resistant M. bovis strains (1), in particular M. bovis strains isolated from animals. Bovine tuberculosis remains a major infectious disease among cattle worldwide, making control of outbreaks and prevention of transmission to humans of MDR M. bovis mandatory. In this paper, we report a molecular analysis of the isoniazid and rifampin genes for 14 resistant M. bovis strains, isolated from cattle of different herds in Sardinia, in order to detect genetic alterations and evaluate their correlation to resistance phenotypes.
MATERIALS AND METHODS
M. bovis strains.
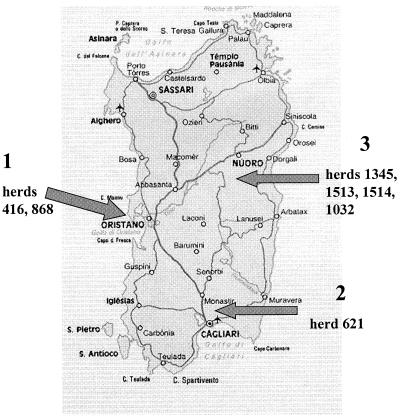
Among 22 M. bovis strains isolated from cattle of different herds in Sardinia (17) we found 14 isolates resistant to isoniazid and rifampin (a drug resistance prevalence rate of 63.6%), which were included in this study. Two strains (416/0 and 868/30) were isolated from two different herds in Oristano (100% resistant strains), six strains (621/2, 621/4, 621/6, 621/10, 621/16, and 621/17) were isolated in Cagliari (42.8% resistant strains) and six strains (1345/92, 1345/94, 1345/95, 1513/97, 1514/98, and 1032/164) were isolated from three different herds in Nuoro (100% resistant strains). The regions where the strains were isolated are shown in Fig. 1.
FIG. 1.
Map of Sardinia. Arrows indicate regions where M. bovis strains were isolated: 1, Oristano; 2, Cagliari; 3, Nuoro.
The BACTEC 460 TB radiometric method (7) was used to test the rifampin (breakpoint, 0.5 μg/ml) and isoniazid (breakpoint, 0.5 μg/ml) susceptibilities of the M. bovis isolates. Four of the fourteen isolates were found resistant to isoniazid, five were resistant to rifampin, and five were resistant to both drugs. Susceptibility to other antibiotic drugs was not tested. M. bovis strains were identified by biochemical tests (niacin production; growth in the presence of thiophene-2-carboxylic acid hydrazide, nitrate reductase, and pyrazinamidase); identification was confirmed by a species-specific assay described by Rodriguez et al.(16).
Epidemiological characterization of the M. bovis strains.
Molecular typing of these isolates was performed by using several methods such as IS6110 fingerprinting, PCR ribotyping, enterobacterial repetitive intergenic consensus (ERIC)-PCR, and PCR-(GTG)5, as previously described (17).
Sample preparation for PCR.
A loopful of each M. bovis strain grown on Löwenstein-Jensen medium was suspended in 500 μl of distilled water and heat inactivated at 80°C for 30 min. Then each sample was centrifuged at 12,000 × g for 5 min, and the pellet was suspended in 100 μl of distilled water and subjected to three cycles of boiling and freezing (5 min at 100°C and 5 min at −20°C) (9). Then an equal volume of chloroform was added, and the samples were vortexed and centrifuged at 12,000 × g for 10 min. The aqueous phase containing the extracted DNA was used for amplification or transferred to a clean microcentrifuge tube and stored at −20°C until use.
Detection of mutations.
Specific regions of the katG, oxyR-ahpC, and inhA genes that are related to isoniazid resistance and the region of the rpoB gene involved in rifampin resistance were PCR amplified by using primer pairs as previously described (3). The PCR products were cloned in the T/A cloning vector (Invitrogen), and the DNA sequence was determined by the dideoxy-chain termination method with the ABI PRISM Dye Terminator Cycle Sequencing kit (Perkin-Elmer) and the ABI PRISM 310 automatic sequencer (Applied Biosystems). To verify the existence of specific mutations, products from three independent PCR amplifications were cloned and sequenced. Sequence data were analyzed with DNASIS software, version 2.1 (Hitachi Software Engineering Co.), and the mutations were detected by nucleotide alignment with M. bovis genomic sequences deposited in GenBank (accession numbers X83277, U41388, U43947, and AF057451).
RESULTS
Molecular characterization of M. bovis isolates.
Various molecular biology-based methods, such as IS6110 DNA fingerprinting, PCR ribotyping, and PCR fingerprinting with (GTG)5 and ERIC sequences, were used as independent molecular markers to characterize the 14 M. bovis strains, as described previously (17). By using these molecular approaches, we found that the isolates were genetically related as previously described (17) (Table 1). For instance, the strain (621/4) isolated in 1996 from a cow imported from Cremona (northern Italy) has, the same IS6110 fingerprinting pattern (1.9-kb hybridizing band) as strain 621/6 from the same herd (Table 1). Three other strains belonging to the same herd and isolated in 1998 (strains 621/10, 621/16, and 621/17) did not show any IS6110-hybridizing band and generated different patterns with the other techniques. The same pattern (1.9-kb hybridizing band) was found in strains isolated in Nuoro (1513/97, 1514/98, and 1032/64) from three different herds. However, other strains from different herds in Nuoro (strains 1345/92, 1345/95, and 1345/94) showed a completely different fingerprinting pattern, with 6 and 5 bands at the same molecular size (confirmed by the other fingerprinting methods [Table 1]). Finally, strain 621/2 produced a different IS6110 pattern (a single band at 5.5 kb [Table 1]), which was found 13 months later in strain 416/10 isolated in Oristano; these strains generated the same (GTG)5 fingerprinting pattern, pattern A (Table 1).
TABLE 1.
Results of different DNA fingerprinting methods after analysis of the 14 M. bovis strains
| Herd/strain | Mo/yr of isolation | IS6110 fragment size or no. of bands | PCR resulta obtained with:
|
Resulta of PCR ribotyping and digestion with:
|
||
|---|---|---|---|---|---|---|
| ERIC | (GTG)5 | HaeIII | PvuII | |||
| 416/0 | 12/1997 | 5.5 kb | A | A | A | A |
| 868/30 | 6/1997 | 0 bands | B | B | A | B |
| 621/2 | 11/1996 | 5.5 kb | D | A | B | A |
| 621/4 | 12/1996 | 1.9 kb | E | C | C | C |
| 621/6 | 1/1998 | 1.9 kb | E | C | D | D |
| 621/10 | 1/1998 | 0 bands | F | B | A | A |
| 621/16 | 9/1998 | 0 bands | A | E | A | A |
| 621/17 | 9/1998 | 0 bands | B | A | A | B |
| 1345/92 | 3/1997 | 6 bands | E | C | C | G |
| 1345/94 | 6/1997 | 5 bands | E | C | C | C |
| 1345/95 | 6/1997 | 6 bands | E | C | C | C |
| 1513/97 | 12/1997 | 1.9 kb | E | C | C | G |
| 1514/98 | 4/1998 | 1.9 kb | E | G | C | C |
| 1032/164 | 4/1998 | 1.9 kb | E | C | C | C |
Expressed as a pattern.
Phenotypic resistance to rifampin and isoniazid.
Table 2 shows the results of drug susceptibility testing for rifampin and isoniazid. Only five isolates were resistant to both drugs, indicating an MDR phenotype.
TABLE 2.
Susceptibilities to isoniazid and rifampinaof the 14 M. bovis isolates analyzed in this study and mutations in genes involved in isoniazid and rifampin resistanceb
| Strain | Susceptibilityc to isoniazid (0.1 μg/ml) | Isoniazid resistance-related mutation
|
Susceptibilityc to rifampin (0.5 μg/ml) | Rifampin resistance-related mutation
|
||||
|---|---|---|---|---|---|---|---|---|
| katGd | inhAe | oxyR-ahpC | Nucleotide substitution | Codon | Amino acid mutation | |||
| 416/0 | R | E506K (GAG→AAG) | 209T | WT | R | CAC→GAC | 526 | H→Y |
| 868/30 | R | E506K (GAG→AAG) | 209T | WT | R | CAC→GAC | 526 | H→Y |
| 621/2 | R | L463R (CTG→CGG) | WT | WT | S | |||
| 621/4 | R | L463R (CTG→CGG) | WT | WT | S | |||
| 621/6 | R | L463R (CTG→CGG) | WT | WT | S | |||
| 621/10 | R | S315T (AGC→ACC) | WT | WT | S | |||
| 621/16 | R | WT | WT | WT | R | CAA→AAA | 513 | Q→K |
| 621/17 | R | WT | WT | WT | R | CAA→AAA | 513 | Q→K |
| 1345/92 | S | R | CTG→CCG | 521 | L→P | |||
| 1345/94 | S | R | CTG→CTT | 521 | L→P | |||
| 1345/95 | S | R | CTG→CCG | 521 | L→P | |||
| 1513/97 | R | S315T (AGC→ACC) | 209T | WT | R | CTG→CCG | 521 | L→P |
| 1514/98 | S | R | CTG→CTT | 521 | L→P | |||
| 1032/164 | S | R | CTG→CCG | 521 | L→P | |||
Determined by the BACTEC 460 TB radiometric method.
Detected in 9 and 10 resistant M. bovis strains, respectively.
R, resistant, S, susceptible.
Amino acid mutation (nucleotide substitution). WT, wild type.
Nucleotide substitution.
Analysis of the rpoB gene region responsible for the rifampin resistance phenotype.
In order to look for mutations associated with rifampin resistance, a 157-bp region of the rpoB gene was amplified from the 10 rifampin-resistant M. bovis isolates using the primers described previously (3). The PCR products were cloned and sequenced. We identified three nucleotide substitution mutations involving codons 513, 521, and 526, designated Q513K, L521P, and H526Y, respectively (Table 2). Mutation L521P, which changes leucine to proline, was detected in 6 of the 10 rifampin-resistant M. bovis isolates, suggesting the putative role of this amino acid substitution in determining the resistance phenotype. All mutations found are summarized in Table 2.
Analysis of the katG, oxyR-ahpC, and inhA gene regions involved in the isoniazid resistance phenotype.
To detect mutations involving the isoniazid resistance of M. bovis, DNA from all of the nine isoniazid-resistant isolates was subjected to PCRs using specific primers which amplify the oxyR-ahpC intergenic region of 455 bp (3). After all the PCR-amplified products were cloned and sequenced, we failed to detect sequence variations, although several mutations in the same genomic region have been described (14). Moreover, sequence analysis of the oxyR region revealed the presence of a polymorphic adenine residue at nucleotide position 285 in all of the strains. This polymorphism has been used to differentiate M. bovis from other members of the M. tuberculosis complex, thus confirming that all of our isolates were M. bovis (18). Unlike the findings for the oxyR-ahpC region, inhA gene analysis showed a C→T substitution involving nucleotide 209 in the inhA regulatory region for three strains, whereas a wild-type sequence was detected in the remaining isolates (Table 2). In contrast, as shown in Table 2, we detected one of three mutations in the katG gene for all but two of the isolates examined. Three strains had a CTG→CGG change in codon 463 (L463R), two strains had an AGC→ACC change in codon 315 (S315T), and two strains had a GAG→AAG alteration in codon 506 (E506K).
DISCUSSION
We report the presence of mutations in all of the M. bovis strains, isolated from cattle, that exhibited rifampin resistance. One of the mutations detected resulted in the common substitution at codon 526, which, along with a mutation at codon 531, occurs most frequently in M. tuberculosis strains (14). However, the most frequent mutation, encountered in 6 of 10 strains (60%), occurred at codon position 521 and resulted in leucine being changed to proline. The high frequency of this mutation and the occurrence of different nonsynonymous substitutions (Table 2) demonstrated that codon 521 may be important for the development of rifampin resistance in M. bovis. In contrast, Blasquez et al. (1) reported, in a study carried out on 19 MDR M. bovis strains isolated in a nosocomial outbreak, that the rifampin resistance of these isolates was associated with the S531L mutation, found mostly in rifampin-resistant M. tuberculosis strains. In contrast, resistance to isoniazid is associated in M. tuberculosis with a variety of mutations affecting one or more genes: katG, encoding catalase-peroxidase; inhA, encoding enoyl-acyl carrier protein reductase; and ahpC, encoding alkyl-hydroperoxide reductase. With regard to the inhA gene, we detected a mutation (nucleotide substitution 209C→T) only in the regulatory region and not in the structural gene, in full agreement with the data reported by Telenti et al. (19) for M. tuberculosis. Our results confirm the difficult nature of the interpretation of the sequence variations observed in clinical strains.
With regard to the katG gene, the role of the transversion mutation at codon 463 that converts an arginine (CGG) into a leucine (CTG) in the resistance of M. tuberculosis, to isoniazid is still unclear (9, 11; A. S. G. Lee, L. L.-H. Tang, I. H.-K. Lim, M.-L. Ling, L. Tay, and S.-Y. Wong, Letter, J. Infect. Dis. 177:1125–1126, 1997). However, several studies (11, 12) report that Leu463 is normally found in M. bovis and Mycobacterium microti, suggesting that this amino acid is linked to wild-type genome sequences in these microorganisms. In our study, three of our M. bovis isolates presented the arginine at the 463 codon that normally occurs in M. tuberculosis. For this reason, we think that the Leu→Arg change at codon 463, found in the three isoniazid-resistant strains, can be considered a polymorphic variant. In contrast, the Ser→Thr mutation affecting codon 315, found in two of our isolates, can be considered significant for isoniazid resistance in M. bovis, because this mutation has been associated with resistance in M. tuberculosis (9, 19). Finally, mutation at codon 506 has not been previously reported either in M. tuberculosis or in M. bovis; thus, the role of this mutation in determining isoniazid resistance should be investigated.
It is interesting that M. bovis strains isolated from the same geographic area show similar mutations within the genes responsible for rifampin and isoniazid resistance. For instance, strains 416/0 and 868/30, both isolated from cattle in Oristano, presented the same mutation in the rpoB gene at codon 526. The same situation was found for katG and inhA genes. The fingerprinting patterns of these strains obtained by various techniques were different except for those generated by PCR ribotyping followed by HaeIII digestion.
The rpoB genes of strains 621/16 and 621/17, both isolated in Cagliari, were found mutated at codon 513, whereas no mutation was detected in the katG, inhA, and oxyR-ahpc genes. These strains generated similar patterns by PCR ribotyping following digestion with HaeIII endonuclease and showed no IS6110 insertion when hybridized with the probe. Furthermore, we detected the same mutation at codon 521 in the rpoB genes of M. bovis strains isolated in Nuoro (1345/92, 1345/94, 1345/95, 1345/97, and 1032/92). These isolates were grouped into two IS6110 clusters, whereas ERIC-PCR and PCR ribotyping followed by HaeIII digestion generated only one group. The strains isolated showed multiple fingerprinting patterns with different techniques, and although we can attempt to monitor the dissemination of particular strains in Sardinia, it is clear that there are different sources of infection. This study shows that similar mutations within the genes responsible for rifampin and isoniazid resistance arose independently among different strains isolated in the same geographic area, suggesting the presence of selective pressure in those environments (20). We do not know what the selective pressure that led to the mutations in the genes responsible for antibiotic resistance was, since rifampin and isoniazid are not allowed for the prevention of bovine tuberculosis or for treatment of infected animals. This study raises questions which will need further investigation in order to be answered.
ACKNOWLEDGMENTS
This work was supported by the Third National Project “Tubercolosi” of the Istituto Superiore di Sanità, Rome, Italy, and by MURST ex 40%.
We thank E. Manca for technical assistance.
REFERENCES
- 1.Blasquez J, Espinosa de los Monteros L E, Camper S, Martin C, Guerriero A, Cobo J, van Embden J, Vaquero F, Gomez-Mampaso E. Genetic characterization of multidrug-resistant Mycobacterium bovis strains from a hospital outbreak involving human immunodeficiency virus-positive patients. J Clin Microbiol. 1997;35:1390–1393. doi: 10.1128/jcm.35.6.1390-1393.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bollo E, Ferroglio E, Dini V, Mignone W, Biolatti B, Rossi L. Detection of Mycobacterium tuberculosis complex in lymph nodes of wild boar (Sus scrofa) by a target-amplified test system. J Vet Med B. 2000;47:337–342. doi: 10.1046/j.1439-0450.2000.00354.x. [DOI] [PubMed] [Google Scholar]
- 3.Cingolani A, Antinori A, Sanguinetti M, Gillini L, De Luca A, Posteraro B, Ardito F, Fadda G, Ortona L. Application of molecular methods for detection and transmission analysis of Mycobacterium tuberculosis drug resistance in patients attending a reference hospital in Italy. J Infect Dis. 1999;179:1025–1029. doi: 10.1086/314677. [DOI] [PubMed] [Google Scholar]
- 4.Clifton-Hadley R S, Wilesmith J W, Richards M S, Upton P, Johnston S. The occurrence of Mycobacterium bovis infection in cattle in and around an area subject to extensive badger (Meles meles) control. Epidemiol Infect. 1995;114:179–193. doi: 10.1017/s0950268800052031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins D M, De Lisle G W, Gabric D M. Geographic distribution of restriction types of Mycobacterium bovis isolates from brush-tailed possums (Trichosurus vulpecula) in New Zealand. J Hyg (London) 1986;96:431–438. doi: 10.1017/s0022172400066201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cosivi O, Grange J M, Daborn C J, Raviglione M C, Fujikura T, Cousins D, Robinson R A, Huchzermeyer H F A K, de Kantor I, Meslin F-X. Zoonotic tuberculosis due to Mycobacterium bovis in developing countries. Emerg Infect Dis. 1998;4:1–15. doi: 10.3201/eid0401.980108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fadda G, Roe S L. Recovery and susceptibility testing of Mycobacterium tuberculosis from extrapulmonary specimens by the BACTEC radiometric method. J Clin Microbiol. 1984;19:720–721. doi: 10.1128/jcm.19.5.720-721.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gutierrez M C, Gala J C, Blasquez J, Bouvet E, Vincent V. Molecular markers demonstrate that the first described multidrug-resistant Mycobacterium bovis outbreak was due to Mycobacterium tuberculosis. J Clin Microbiol. 1999;37:971–975. doi: 10.1128/jcm.37.4.971-975.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heym B, Alzari P M, Honoré N, Cole S T. Missense mutations in the catalase-peroxidase gene, katG, are associated with isoniazid resistance in Mycobacterium tuberculosis. Mol Microbiol. 1995;15:235–245. doi: 10.1111/j.1365-2958.1995.tb02238.x. [DOI] [PubMed] [Google Scholar]
- 10.Heym B, Honore N, Truffot-Pernot C, Banerjee A, Schurra C, Jacobs W R, Jr, van Embden J D A, Grosset J H, Cole S T. Implications of multidrug resistance for the future of short course chemotherapy of tuberculosis: a molecular study. Lancet. 1994;344:293–298. doi: 10.1016/s0140-6736(94)91338-2. [DOI] [PubMed] [Google Scholar]
- 11.Marttila H J, Soini H, Eerola E, Vyshnevskaya E, Vyshnevskiv B I, Otten T F, Vasilyef A V, Vijanen M K. A Ser315Thr substitution in KatG is predominant in genetically heterogeneous multidrug-resistant Mycobacterium tuberculosis isolates originating from the St. Petersburg area in Russia. Antimicrob Agents Chemother. 1998;42:2443–2445. doi: 10.1128/aac.42.9.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morris S, Bai G H, Suffys P, Portillo-Gomez L, Fairchok M, Rouse D. Molecular mechanisms of multiple drug resistance in clinical isolates of Mycobacterium tuberculosis. J Infect Dis. 1995;171:954–960. doi: 10.1093/infdis/171.4.954. [DOI] [PubMed] [Google Scholar]
- 13.Musser J M, Kapur V, Williams D L, Kreiswirth B N, van Soolingen D, van Embden J D A. Characterization of the catalase-peroxidase gene (katG) and inhA locus in isoniazid-resistant and -susceptible strains of Mycobacterium tuberculosis by automated DNA sequencing: restricted array of mutations associated with drug resistance. J Infect Dis. 1996;173:196–202. doi: 10.1093/infdis/173.1.196. [DOI] [PubMed] [Google Scholar]
- 14.Musser J M. Antimicrobial agent resistance in mycobacteria: molecular genetic insights. Clin Microbiol Rev. 1995;8:496–514. doi: 10.1128/cmr.8.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramaswamy S, Musser J M. Molecular genetic basis of antimicrobial resistance in Mycobacterium tuberculosis: 1998 update. Tuber Lung Dis. 1998;79:3–29. doi: 10.1054/tuld.1998.0002. [DOI] [PubMed] [Google Scholar]
- 16.Rodriguez J G, Mejia G A, Del Portillo P, Patarroyo M E, Murillo L A. Species-specific identification of Mycobacterium bovis by PCR. Microbiology. 1995;141:2131–2138. doi: 10.1099/13500872-141-9-2131. [DOI] [PubMed] [Google Scholar]
- 17.Sechi L A, Leori G, Lollai S A, Dupré I, Molicotti P, Fadda G, Zanetti S. Different strategies for molecular differentiation of Mycobacterium bovis strains isolated in Sardinia, Italy. Appl Environ Microbiol. 1999;65:1781–1785. doi: 10.1128/aem.65.4.1781-1785.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sreevatsan S, Escalante P, Pan X, Gillies II D A, Siddiqui S, Khalaf C N, Kreiswirth B N, Bifani P, Adams L G, Ficht T, Perumaalla V S, Cave M D, van Embden J D, Musser J M. Identification of a polymorphic nucleotide in oxyR specific for Mycobacterium bovis. J Clin Microbiol. 1996;34:2007–2010. doi: 10.1128/jcm.34.8.2007-2010.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Telenti A, Honoré N, Bernasconi C, March J, Ortega A, Heym B, Takiff H E, Cole S T. Genotypic assessment of isoniazid and rifampin resistance in Mycobacterium tuberculosis: a blind study at reference laboratory level. J Clin Microbiol. 1997;35:719–723. doi: 10.1128/jcm.35.3.719-723.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Witte W. Ecological impact of antibiotic use in animals on different complex microflora: environment. Int J Antimicrob Agents. 2000;14:321–325. doi: 10.1016/s0924-8579(00)00144-8. [DOI] [PubMed] [Google Scholar]