Abstract
Background
The start of the COVID-19 vaccination campaign among French healthcare and welfare sector workers in January 2021 offered an opportunity to study psychological antecedents of vaccination in this group.
Aim
We explored whether knowledge and attitude items related to social conformism and confidence in systems contributed to explaining intention for COVID-19 vaccination.
Methods
We developed a knowledge and attitude questionnaire with 30 items related to five established and two hypothetical psychological antecedents of vaccination (KA-7C). The online questionnaire was distributed from 18 December 2020 to 1 February 2021 through chain-referral via professional networks, yielding a convenience sample. We used multivariable logistic regression to explore the associations of individual and grouped KA-7C items with COVID-19 vaccine intention.
Results
Among 5,234 participants, the vaccine intention model fit (pseudo R-squared values) increased slightly but significantly from 0.62 to 0.65 when adding social conformism and confidence in systems items. Intention to vaccinate was associated with the majority opinion among family and friends (OR: 11.57; 95% confidence interval (CI): 4.51–29.67) and a positive perception of employer’s encouragement to get vaccinated (vs negative; OR: 6.41; 95% CI: 3.36–12.22). The strongest association of a knowledge item was identifying the statement ‘Some stages of vaccine development (testing) have been skipped because of the epidemic emergency.’ as false (OR: 2.36; 95% CI: 1.73–3.22).
Conclusion
The results suggest that social conformism and confidence in systems are distinct antecedents of vaccination among healthcare and welfare workers, which should be taken into account in vaccine promotion.
Keywords: COVID-19 vaccination, healthcare workers, vaccine hesitancy, vaccine acceptance
Introduction
Vaccination is one of the main tools to respond to the current coronavirus disease (COVID-19) pandemic. Healthcare workers (HCWs) are among the priority groups in most countries who aim to provide them with protection given their continuous exposure, protect the healthcare system from absenteeism and prevent nosocomial transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. In France, COVID-19 vaccination of HCWs has been recommended from early January 2021 on, initially limited to those aged 50 years or older or with underlying conditions, and without any limitations from early February 2021 on.
In July 2021, the COVID-19 vaccination coverage for at least one dose among HCWs in France was estimated at 60.5% and 80.5% in nursing homes and in private practices, respectively [2]. At the same time, a strong gradient of the vaccination rates from medical professions to nurses and nurse assistants was described in hospitals, similar to the expressed intentions in surveys performed France in 2020 [3,4]. A COVID-19 vaccine mandate for healthcare and welfare sector workers entered into force in France on 15 September 2021 and includes since 30 January 2022 a booster dose. To prepare a long term strategy of COVID-19 vaccine promotion, it will be important to understand and follow up antecedents of COVID-19 vaccine acceptance.
The term vaccine hesitancy was coined to describe the attitude of delay in acceptance or refusal towards vaccination despite availability [5]. To better understand the source of vaccine hesitancy and to evaluate interventions to mitigate, it is important to consider the psychological aspects of human behaviour and choice. The original 3C psychological antecedents model [5] included (i) confidence i.e. trust in vaccines, the system that delivers them and motivations of policy makers who decide on needed vaccines; (ii) complacency i.e. need of the vaccine given its effectiveness and severity of the disease; and (iii) convenience i.e. accessibility [5]. Betsch et al. proposed an expanded 5C-scale including two additional antecedents: (i) calculation (deliberation on risks and benefits); and (ii) collective responsibility (sense of altruism towards getting vaccinated) [6]. In our study we explore whether items related to two additional antecedents can improve the explanation of vaccine intention. First, we propose adding social conformism as a psychological antecedent. Taking decisions by imitating peers is known to be an important heuristic that helps to reduce mental load in daily life [7]. In several discrete choice experiments higher theoretical vaccination acceptance was found in scenarios presenting higher coverage in the community [8-10]. Furthermore, we examine whether the confidence psychological antecedent should discriminate between confidence in the vaccine and vaccine-related system and confidence in the wider circle of systems, including authorities and employer. In a study looking at French-speaking general practitioners in late 2020, the distrust in the Ministry of Health and in vaccine safety appeared to lead to lower COVID-19 vaccination acceptance [11]. Additionally, as pointed out by Larson et al., confidence can be separated into product trust, provider trust and political or system trust [12].
The roll-out of COVID-19 vaccination among HCWs in France provided an opportunity to study whether knowledge and attitude items related to social conformism and confidence in systems (authorities and employer) contributed to explaining the intention for COVID-19 vaccination among healthcare and welfare sector workers.
Methods
Participant recruitment
From 18 December 2020 to 1 February 2021, the Research Group for the Prevention of Occupational Infections in Healthcare Workers published an online survey via the Sphinx online survey platform. This was disseminated by email chain-referral throughout France, including overseas departments. Several formal and informal networks of hospital-based and private practice HCWs and of nursing home directors contributed to its dissemination. Since each participant could forward the survey across their own network, we did not estimate a response rate; nor were visits to the survey website counted.
Data collection
The questionnaire consisted of three parts. The first and third part collected socio-demographic, professional and health-related characteristics of the participants, and information on the intention to accept and recommend COVID-19 vaccination. The second part of the survey directed participants, by choosing a shape (square or triangle), to either a discrete choice experiment [13] or to the present questionnaire on knowledge and attitudes. Effective survey completion time was ca 8 min.
Questionnaire development
The knowledge and attitude (KA) questionnaire was based on the 5C-scale for evaluation of psychological antecedents presented by Betsch et al. [5]. Since the 5C-scale relates to vaccination in general, we adapted questions to apply specifically to COVID-19 vaccination of healthcare and welfare sector workers in the epidemic context in France. Item groups related to the two additional antecedents were included in the KA-7C questionnaire: social conformism and confidence in systems (authorities and employer). One author developed a draft of the KA-7C questionnaire which was reviewed by other co-authors for coherence with the 5C-scale. Each item group consisted of at least one attitude and knowledge question. In total, the KA-7C questionnaire had 30 questions: nine questions were associated with the attitude towards the vaccine and systems; 19 questions were associated with the knowledge about the vaccines, their development and COVID-19. A 5-point Likert scale was used to simplify questionnaire administration. Two items were general attitude questions on confidence in the authorities for managing the public health and economic crisis caused by COVID-19 and concern about the COVID-19 epidemic, both on an 11-point scale (Supplementary Table S1). Knowledge items were either presented as a statement to which participants could answer ‘Right’, ‘Do not know’ or ‘Wrong’, or requested a single choice answer to a question from several options which included ‘Do not know’ (Supplementary Table S1).
Prior to finalisation, the questionnaire was reviewed by occupational health specialists in hospitals who are in charge of vaccine promotion towards HCWs, and pilot-tested in think-aloud sessions with HCWs including physicians, pharmacists and nurses.
Data analysis
Knowledge variables were coded as incorrect answer, ‘Do not know’ and correct answer. We kept ‘Do not know’ as a distinct modality of the knowledge variables, to distinguish the specific situation of participants recognising their lack of knowledge. Answers to the general attitude questions (i.e on confidence in crisis management and concern about the COVID-19 epidemic) were transformed into three categories: (i) low: 0–3; (ii) medium: 4–6; and (iii) high: 7–10. Other attitude items were maintained on a 5-point scale.
We used bivariate logistic regression models to explore the association of participant characteristics and individual KA-7C items with vaccine intention. Initial analyses explored vaccine intention as ‘Yes’ with and without the ’Do not know’ modality. No major differences were detected between these analyses, therefore the final analyses were carried out on the variable ’Yes’ vs ’No/Do not know’ to clearly focus on vaccine intention. We created a variable for the different periods of survey participation: (i) period 1 from 18 December 2020 to 4 January 2021, which was the early phase of the COVID-19 vaccination campaign targeting nursing home residents; (ii) period 2 from 5 January to 14 January 2021, when vaccination was expanded to HCWs aged 50 years or older; and (iii) period 3 from 15 January to 1 February 2021, when the COVID-19 vaccination campaign was expanded to the general population aged 75 years or older or to people having specific high-risk comorbidities such as rare immune disorders.
We evaluated collinearity between the KA-7C items using the collin command in Stata version 16.1 (StataCorp, College Station, Texas, United States (US)). For variables with variance inflation factor > 2, we conducted pairwise Spearman correlation testing and considered any correlation with rho < 0.70 as not critical. To identify socio-demographic and health-related determinants of vaccine intention, we included variables with p value < 0.20 in bivariate regression into a multivariable logistic regression model using a stepwise forward procedure (basic model). In France, most professional categories in the healthcare and welfare sector are well-defined and correlate with educational trajectories [14,15]. We therefore did not include educational level in the models.
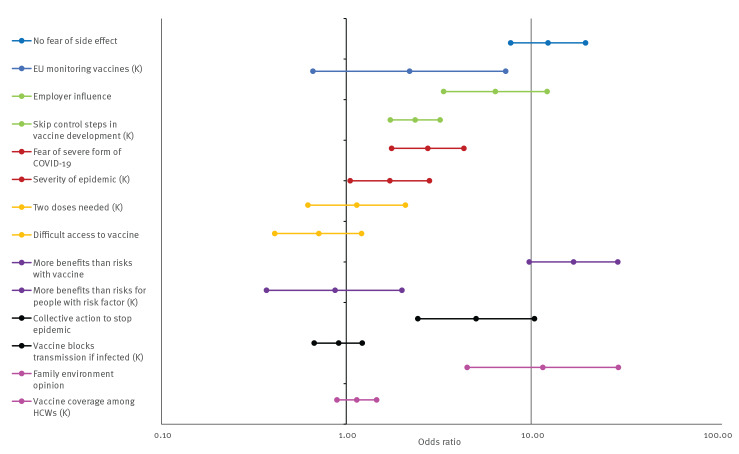
We examined the contribution of items and item groups to the explanation of vaccine intention variation based on MacFadden pseudo R-squared values (R2) where values above 0.20–0.40 indicate excellent fit. The significance of the contribution of the hypothetical antecedent item groups was assessed based on the nested log likelihood ratio test. Figure 1 presents: a basic model adjusting only for socio-demographic variables; a model with all 30 KA-7C items compared with a model limited to five antecedents (5C); models including only knowledge compared with only attitude items and models with individual C-item groups.
Figure 1.
Flowchart of model examination to explore the fit of regression models with KA-7C items explaining vaccine intention at the start of the COVID-19 vaccination campaign, France, 18 December 2020–1 February 2021
A: attitude item; COVID-19: coronavirus disease; K: knowledge item; R2: pseudo R-squared value.
5C and 7C refer to the five established (5C) and additional two hypothetical antecedents (7C) of vaccination respresented by item group.
Finally, for presentation of effect estimates, we defined a shortlist of 14 KA-7C items, selecting for each 7C item group the attitude and the knowledge item with the highest pseudo R-squared value. We estimated the association of each KA-7C item and item group with vaccine intention in multivariable models reporting odds ratios (OR) and 95% confidence intervals (CI). All models controlled for age group, sex, professional category, work in a nursing home and period of study participation.
Results
Participants
The survey reached all French regions, including the overseas departments, although participation in the latter was sporadic. A total of 9,580 participants from diverse health-related careers and sectors participated. The KA-7C questionnaire was completed by 5,234 participants, with similar distribution across the periods defined by roll-out of the vaccination campaign: 38.7%, 30.9% and 30.4%. Women represented 78.4% of participants and 23.2%, 40.0% and 36.8%, respectively, were aged 18–34 years, 35–49 years and 50 years or older (Table). Nurses represented 22.9%, nurse assistants 9.4%, biomedical professionals (including physicians, midwives, pharmacists and biologists) 27.7%, other paramedical staff 15.7% and administration staff 24.4% (Table). Among physicians in our sample, 59% were female and median age group was 35–49 years (cf.d with 50% and 49.3 years mean age according to official estimates in 2021 [16]). Among nurses, 85% were female and median age group was 35–49 years (cf.d with 88% and 40.2 years mean age in 2011 [17]).
Table. Survey responses by healthcare and welfare sector workers at the start of the COVID-19 vaccination campaign, France, 18 December 2020–1 February 2021 (n = 5,234).
| Characteristics and shortlist of KA-7C items | n | % | Intention to get COVID-19 vaccination | Full multivariable modela | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No/DNK | Yes | Yes vs No/DNK | ||||||||
| n | % | n | % | OR | 95% CI | |||||
| Socio-demographic characteristics | ||||||||||
| Age (years) | 18–34 | 1,215 | 23.2 | 681 | 56.1 | 534 | 44.0 | Ref | ||
| 35–49 | 2,092 | 40.0 | 932 | 44.6 | 1,160 | 55.5 | 1.04 | 0.80–1.35 | ||
| ≥ 50 | 1,927 | 36.8 | 578 | 30.0 | 1,349 | 70.0 | 1.47 | 1.11–1.96 | ||
| Sex |
Female | 4,103 | 78.4 | 1,889 | 46.0 | 2,214 | 54.0 | Ref | ||
| Male | 1,131 | 21.6 | 302 | 26.7 | 829 | 73.3 | 1.22 | 0.94–1.60 | ||
| Profession |
Nurses | 1,197 | 22.9 | 603 | 50.4 | 594 | 49.6 | Ref | ||
| Nurse assistants | 491 | 9.4 | 341 | 69.5 | 150 | 30.6 | 0.78 | 0.51–1.19 | ||
| Other paramedical staffb | 819 | 15.7 | 407 | 49.7 | 412 | 50.3 | 0.73 | 0.53–1.01 | ||
| Biomedical professionalsc | 1,449 | 27.7 | 287 | 19.8 | 1,162 | 80.2 | 1.25 | 0.92–1.70 | ||
| Admin/technical staff | 1,278 | 24.4 | 553 | 43.3 | 725 | 56.7 | 1.03 | 0.77–1.37 | ||
| Work in a nursing home | No | 4,429 | 84.6 | 1,766 | 39.9 | 2,663 | 60.1 | Ref | ||
| Yes | 805 | 15.4 | 425 | 52.8 | 380 | 47.2 | 0.97 | 0.72–1.31 | ||
| Study period | 1 | 2,026 | 38.7 | 1,113 | 54.9 | 913 | 45.1 | Ref | ||
| 2 | 1,618 | 30.9 | 574 | 35.5 | 1,044 | 64.5 | 1.73 | 1.34–2.23 | ||
| 3 | 1,590 | 30.4 | 504 | 31.7 | 1,086 | 68.3 | 2.20 | 1.68–2.88 | ||
| Confidence in COVID-19 vaccine | ||||||||||
| ’I am afraid of having a severe side effect of vaccination.’ | Strongly disagree | 1,203 | 23.0 | 127 | 10.6 | 1,076 | 89.4 | 12.36 | 7.76–19.70 | |
| Disagree | 1,341 | 25.6 | 245 | 18.3 | 1,096 | 81.7 | 10.52 | 7.02–15.79 | ||
| Undecided | 959 | 18.3 | 418 | 43.6 | 541 | 56.4 | 4.87 | 3.30–7.17 | ||
| Agree | 891 | 17.0 | 652 | 73.2 | 239 | 26.8 | 2.19 | 1.48–3.24 | ||
| Strongly agree | 840 | 16.1 | 749 | 89.2 | 91 | 10.8 | Ref | |||
| ’The security of vaccines is monitored not only at the national level, but also in collaboration between European countries.’ | False (i) | 92 | 1.76 | 79 | 85.9 | 13 | 14.1 | Ref | ||
| DNK | 855 | 16.3 | 596 | 69.7 | 259 | 30.3 | 1.43 | 0.42–4.84 | ||
| True (c) | 4,287 | 81.9 | 1,516 | 35.4 | 2,771 | 64.6 | 2.20 | 0.66–7.29 | ||
| Confidence in systems | ||||||||||
| ’If my employer encourages me to get vaccinated, this…’ | Dissuades me | 274 | 5.2 | 247 | 90.2 | 27 | 9.9 | Ref | ||
| Has no effect | 3,409 | 65.1 | 1,695 | 49.7 | 1,714 | 50.3 | 2.71 | 1.45–5.06 | ||
| Motivates me | 1,551 | 29.6 | 249 | 16.1 | 1,302 | 84.0 | 6.41 | 3.36–12.22 | ||
| ’Some stages of vaccine development (testing) have been skipped because of the epidemic emergency.’ | False (c) | 2,252 | 43.0 | 399 | 17.7 | 1,853 | 82.3 | 2.36 | 1.73–3.22 | |
| DNK | 2,023 | 38.7 | 1,071 | 52.9 | 952 | 47.1 | 2.02 | 1.50–2.71 | ||
| True (i) | 959 | 18.3 | 721 | 75.2 | 238 | 24.8 | Ref | |||
| Complacency | ||||||||||
| ’I am afraid of getting a severe form of COVID-19.’ | Strongly disagree | 1,109 | 21.2 | 528 | 47.6 | 581 | 52.4 | Ref | ||
| Disagree | 1,524 | 29.1 | 673 | 44.2 | 851 | 55.8 | 1.28 | 0.94–1.73 | ||
| Undecided | 1,222 | 23.4 | 488 | 39.9 | 734 | 60.1 | 1.38 | 0.96–1.93 | ||
| Agree | 796 | 15.2 | 284 | 35.7 | 512 | 64.3 | 1.88 | 1.30–2.71 | ||
| Strongly agree | 583 | 11.1 | 218 | 37.4 | 365 | 62.6 | 2.76 | 1.76–4.33 | ||
| ’The gravity of the epidemic requires making vaccines quickly available.’ | False (i) | 411 | 7.9 | 331 | 80.5 | 80 | 19.5 | Ref | ||
| DNK | 513 | 9.8 | 387 | 75.4 | 126 | 24.6 | 1.73 | 0.97–3.12 | ||
| True (c) | 4,310 | 82.4 | 1,473 | 34.2 | 2,837 | 65.8 | 1.72 | 1.05–2.82 | ||
| Convenience | ||||||||||
| ’In practice, it will be difficult for me to get vaccinated.’ | Strongly disagree | 2,429 | 46.4 | 772 | 31.8 | 1,657 | 68.2 | Ref | ||
| Disagree | 1,386 | 26.5 | 610 | 44.0 | 776 | 56.0 | 0.93 | 0.72–1.20 | ||
| Undecided | 765 | 14.6 | 436 | 57.0 | 329 | 43.0 | 0.60 | 0.44–0.81 | ||
| Agree | 361 | 6.9 | 182 | 50.4 | 179 | 49.6 | 1.08 | 0.71–1.65 | ||
| Strongly agree | 293 | 5.6 | 191 | 65.2 | 102 | 34.8 | 0.71 | 0.41–1.22 | ||
| ‘It is necessary to have two injections to be immunised.’ d | False (i) | 159 | 3.0 | 98 | 61.6 | 61 | 38.4 | Ref | ||
| DNK | 524 | 10.0 | 372 | 71.0 | 152 | 29.0 | 0.76 | 0.38–1.51 | ||
| True (c) | 4,551 | 87.0 | 1,721 | 37.8 | 2,830 | 62.2 | 1.14 | 0.62–2.09 | ||
| Calculation | ||||||||||
| ’I think that vaccination against COVID-19 will have more benefits than risks for me.’ | Strongly disagree | 496 | 9.5 | 437 | 88.1 | 59 | 11.9 | Ref | ||
| Disagree | 670 | 12.8 | 603 | 99.0 | 67 | 10.0 | 0.74 | 0.42–1.31 | ||
| Undecided | 1,136 | 21.7 | 841 | 74.0 | 295 | 26.0 | 1.33 | 0.80–2.20 | ||
| Agree | 1,205 | 23.0 | 242 | 20.1 | 963 | 79.9 | 6.39 | 3.82–10.67 | ||
| Strongly agree | 1,727 | 33.0 | 68 | 3.9 | 1,659 | 96.1 | 16.97 | 9.78–29.47 | ||
| ‘For a person with risk factors, these vaccines have more benefits than risks in the current epidemic situation.’ d | False (i) | 148 | 2.8 | 124 | 83.8 | 24 | 16.2 | Ref | ||
| DNK | 875 | 16.7 | 700 | 80.0 | 175 | 20.0 | 0.76 | 0.32–1.81 | ||
| True (c) | 4,211 | 80.5 | 1,367 | 32.5 | 2,844 | 67.5 | 0.87 | 0.37–2.00 | ||
| Collective responsibility | ||||||||||
| ’Getting vaccinated will also be a collective action to stop the crisis caused by the epidemic.’ | Strongly disagree | 253 | 4.8 | 231 | 91.3 | 22 | 8.7 | Ref | ||
| Disagree | 318 | 6.1 | 297 | 93.4 | 21 | 6.6 | 0.70 | 0.28–1.73 | ||
| Undecided | 686 | 13.1 | 620 | 90.4 | 66 | 9.6 | 0.71 | 0.33–1.55 | ||
| Agree | 1,222 | 23.4 | 612 | 50.1 | 610 | 49.9 | 2.35 | 1.12–4.93 | ||
| Strongly agree | 2,755 | 52.6 | 431 | 15.6 | 2,324 | 84.4 | 5.04 | 2.44–10.43 | ||
| ‘The vaccine blocks transmission of the virus to those around you in case of infection.’ d | False (c) | 781 | 14.9 | 1095 | 41.7 | 1,531 | 58.3 | 0.91 | 0.67–1.22 | |
| DNK | 1,827 | 34.9 | 820 | 44.9 | 1,007 | 55.1 | 0.95 | 0.69–1.30 | ||
| True (i) | 2,626 | 50.2 | 276 | 35.3 | 505 | 64.7 | Ref | |||
| Social conformism | ||||||||||
| ‘Among your family and friends, how would you describe the majority opinion towards COVID-19 vaccination?’ | Very favourable | 390 | 7.5 | 8 | 2.1 | 382 | 98.0 | 11.57 | 4.51–29.67 | |
| Favourable | 1,418 | 27.1 | 199 | 14.0 | 1,219 | 86.0 | 4.42 | 2.70–7.22 | ||
| Both skeptical and favourable | 1,653 | 31.6 | 701 | 42.4 | 952 | 57.6 | 2.28 | 1.43–3.63 | ||
| Skeptical | 1,319 | 25.2 | 897 | 68.0 | 422 | 32.0 | 1.59 | 0.99–2.56 | ||
| Very skeptical | 454 | 8.7 | 386 | 85.0 | 68 | 15.0 | Ref | |||
| ‘Do you know the approximate percentage of healthcare workers who intend to get the COVID-19 vaccine?’ | 30% (i) | 1,743 | 33.3 | 906 | 52.0 | 837 | 48.0 | Ref | ||
| DNK | 2,064 | 39.4 | 937 | 45.4 | 1,127 | 54.6 | 1.14 | 0.89–1.46 | ||
| 60% and 90% (c) | 1,427 | 27.3 | 348 | 24.4 | 1,079 | 75.6 | 1.41 | 1.07–1.86 | ||
COVID-19: coronavirus disease; DNK: Do not know; OR: odds ratio; 95% CI: 95% confidence intervals.
(c): correct knowledge item response; (i): incorrect knowledge item response.
a Full multivariable model with shortlist KA-7C items adjusting for age group, sex, professional category, work in a nursing home and period of study participation.
b Includes workers in direct contact with patients, except biomedical professions (see below), nurses and nurse-assistants: e.g., physiotherapists, dieticians, psychologists and educators.
c Includes physicians, midwives, dentists, pharmacists and biologists.
d These questions were introduced as follows: ‘For the most advanced COVID-19 vaccines (close to licensure), the scientific data show that …’.
Working at least part-time in a nursing home was reported by 805 (15.4%) participants (Table). Three-thousand and thirty-four participants (58.1%) indicated vaccine intention against COVID-19, 1,153 (22.0%) indicated no intention, while 1,038 (19.8%) did not know yet. Among participants, 2,779 (53.1%) reported vaccination against influenza during the 2019/20 winter season. The variable on receiving the previous influenza vaccine in 2019/20 was highly associated with COVID-19 vaccine intention but not included in models to avoid overfitting (data not shown).
Exploration of model fit
Compared with a model including the initial 5C item groups, the addition of confidence in systems and social conformism increased the model fit slightly but significantly, from R2 = 0.62 to 0.65 (p < 0.001) (Figure 1). The model with attitude 7C-items only had a substantially higher R2 when compared with the model with knowledge 7C-items only (0.64 vs 0.38).
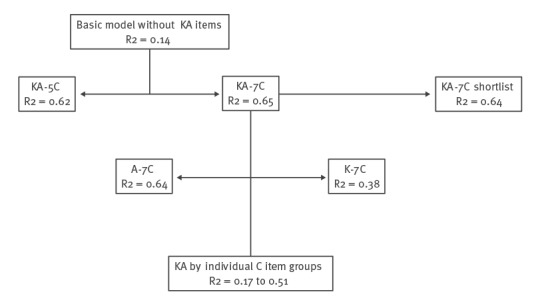
Model fits (R2), corresponding to the percentage of variation in vaccine intention that can be explained, ranged from 0.17 to 0.51 for individual item groups (Figure 2). Confidence in systems and social conformism showed an R2 of 0.37 and 0.30, respectively.
Figure 2.
Fit of regression models explaining vaccination intention among healthcare and welfare sector workers at the start of the COVID-19 vaccination campaign, contribution by each 7C-item group, France, 18 December 2020–1 February, 2021 (n = 5,234)
Pseudo R-squared (R2) values obtained from multivariable regression models including vaccine intention and items from a given C item group, adjusting for age group, sex, professional category, work in a nursing home and period of study participation.
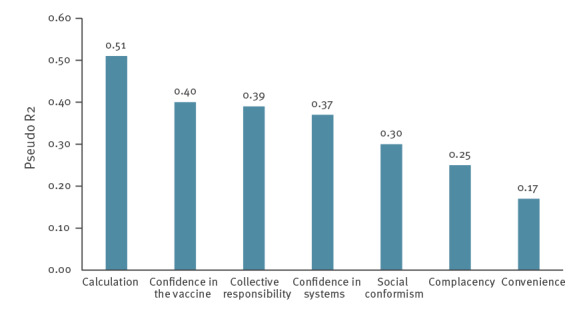
In a full model that included the shortlist KA-7C items and adjusted for socio-demographic characteristics (Supplementary Table S2 showing results of all KA-7C items), the strongest associations were observed for a positive attitude regarding the vaccine’s benefit-risk balance (strongly agree vs strongly disagree, OR: 16.81; 95% CI: 9.66–29.25), fear of a severe side effect (strongly agree vs strongly disagree, OR: 12.47; 95% CI: 7.80–19.92) and a very favourable majority opinion among family and friends (vs very skeptical, OR: 11.02; 95% CI: 4.19–29.01) (Table, Figure 3). The strongest association with a knowledge item was identifying the statement ’Some stages of vaccine development (testing) have been skipped because of the epidemic emergency.’ as being false (OR: 2.36; 95% CI: 1.73–3.22).
Figure 3.
Associations with COVID-19 vaccination intention among healthcare and welfare sector workers, France, 18 December 2020–1 February 2021 (n = 5,234) at the start of the COVID-19 vaccination campaign
COVID-19: coronavisus disease; EU: European Union; HCWs: healthcare workers; K: knowledge variable.
a Points and bars represent odds ratios and 95% confidence intervals estimated in a multivariable model adjusting age group, sex, professional category, work in a nursing home and study phase and including all KA-7C items of the questionnaire shortlist.
b Only highest vs reference categories are shown.
Discussion
In this cross-sectional study of a convenience sample of French healthcare and welfare sector workers exploring the psychological antecedents of COVID-19 vaccination, we found that items referring to social conformism and confidence in systems contributed to the explanation of vaccine intention, in addition to the 5C-model previously presented by Betsch et al. [5]. While the additional explanatory effect of including the two additional item groups was significant but relatively small, the effect sizes of corresponding items (opinion in private environment and perception of employer’s encouragement) were among the strongest in multivariable analysis.
While the KA-7C questionnaire explained 65% of the variation in vaccine intention, most explanatory power came from attitude items, contrasting with limited contribution from knowledge items. Regarding social conformism, the response to the question about majority opinion on COVID-19 vaccination among colleagues or family and friends was strongly associated with vaccine intention of the individual healthcare and welfare sector worker. Vaccination is a socially influenced process, and given the tendency towards homophily (self-selected association with similar people) [18], those who intend to vaccinate are likely to be in a social network with people who share the same sentiments and vice versa [19]. Our results are in concordance with results of previous discrete choice experiments, where the presentation of higher levels of vaccine coverage in the community was associated with greater theoretical vaccine acceptance among HCWs (seasonal influenza and pertussis vaccines) [9], adolescents (human papilloma virus vaccine) [20] and university students (measles and meningococcal vaccines) [8]. The heuristic concept of imitating-your-peers [7] should be further explored in promotion of COVID-19 and other vaccines towards healthcare and welfare sector workers. Taking into account local cultures and group norms, creating chain effects within social networks should help normalise vaccination. Research on vaccine acceptance should therefore increasingly target specific milieus, professional categories and social networks. Any interventions will require a good understanding of the positive or negative social influences acting within the target group.
During the COVID-19 epidemic, confidence in national authorities has become an important polarising characteristic [19] that affects adherence to epidemic control measures and vaccine intention in populations. We addressed this aspect in two ways, by asking questions about participants’ confidence in authorities with regard to COVID-19 crisis management and their perception of a vaccine recommendation from the employer. In France, having previously voted for political parties on the far-left or far-right spectrum, was negatively associated with early COVID-19 vaccine intention in spring 2020 [19]; and a negative perception of healthcare working conditions has been found to be inversely related to influenza vaccine uptake [21]. HCWs play a crucial role at the interface between public health officials and the general population. However, many HCWs are not vaccinology experts and are well aware of how little they know of various vaccines and their inability to answer some of their patients’ questions [22]. As stated by Ward et al., the relationship between public health authorities and HCWs in France has deteriorated over the past 30 years along with depleted funding for public hospitals and the restructuring of the health system [23]. Neither change has helped to induce a positive perception of the vaccine-related or wider systems.
In France, only authorities can issue mandates and often mandates are expected from authorities, which explains why vaccination is highly politicised. Vaccine mandates for HCWs, often supported by hospital managers and doctors, can be seen as either the solution or as an aggravating factor to the problem of suboptimal vaccine coverage among HCWs. Primary and booster vaccination against COVID-19 has become mandatory for healthcare and welfare sector workers in France, and contract terminations for non-compliance with the mandate have been reported since October 2021. Further research is needed to evaluate in how far general, not vaccine-related, societal trust should be taken into account as a separate psychological antecedent of acceptance of other recommended vaccines and for the general population.
Knowledge items played a small role in explaining COVID-19 vaccine intention. The healthcare and welfare sector workers in our sample were a heterogeneous group with education ranging from vocational training to over 6 years of medical training. The frequently observed difference in influenza vaccine uptake between professional categories has led to the conclusion that professionals with shorter educational duration need more or better information on vaccines. Previous vaccine promotion campaigns among French HCWs have focused on organising meetings to deliver scientific messages and answer any questions as decision makers tend to think that lack of knowledge might be conducive to vaccine hesitancy [24], However, attitudes may be more important, albeit more challenging to influence. In a previous study looking at the general US population, better knowledge about the vaccine and less acceptance of conspiracy theories were associated with higher COVID-19 vaccine acceptance [25], while education level was not consistently associated with believing vaccine misinformation across different countries [26]. Research in social psychology has provided strong evidence that better knowledge alone does not lead to greater motivation for behavioural change, but that changing attitudes may impact behaviour [27,28]. From a social marketing perspective, information should be presented in a way that positively influences attitudes, for example by informing about high vaccine coverage among the target group in other countries, rather than mentioning local insufficient coverage.
There is a considerable body of evidence on factors that influence COVID-19 vaccine acceptance and uptake among HCWs [29]. Other studies on COVID-19 vaccine acceptance by HCWs in Europe underpin the importance of trust and confidence [30-32]. We found a high overall capacity of this KA-7C questionnaire to explain variation in COVID-19 vaccine intention among healthcare and welfare sector workers. In comparison, socio-demographic differences explained a smaller proportion of variation (14%), which is surprising given the observation that vaccine coverage against influenza and against COVID-19 consistently differs substantially between socio-demographic and professional groups. A separate analysis will address the capacity of the KA-7C questionnaire to explain these variations between professional categories. Further psychometric analysis is required to validate the questionnaire and model structure with social conformism and confidence in systems as psychological antecedents.
Our study has some limitations. First, the study evaluates COVID-19 vaccine intention, but not eventual uptake. A considerable gap between vaccine intention and uptake exists [33], but looking at the factors that influence intention can at least contribute to explaining the thought processes that inform health decision-making as suggested in the Health Belief Model [33], the COM-B model [34] and the Theory of Planned Behaviour [35]. Second, for some knowledge questions we used relatively unspecific words, such as easily and frequently, which may not allow for the exact knowledge to be measured. However, more detailed estimates would probably have been difficult to expect apart from scientist HCWs and for some items (e.g. risk of long COVID-19) no precise estimate was available at the time of the survey. Third, data collection took place at the start of the COVID-19 vaccine campaign in France, during a period of constant communication of new information regarding vaccine efficacy and safety. However, our final model adjusted for the periods of survey participation such that the identified psychological antecedents should be independent of such trends. Finally, our results are limited to healthcare and welfare sector workers in France willing to participate in an online survey, while the relative importance of 7C item groups for COVID-19 vaccine intention may be different among non-participating healthcare and welfare sector workers, other population groups and other countries. Also, while the importance of social conformism and confidence in systems have been described for other vaccinations including influenza and childhood vaccinations, it likely has been exacerbated by the epidemic situation and may be lower in other contexts and with other vaccinations.
Conclusions
Our study provides evidence that social conformism and confidence in systems are distinct psychological antecedents of vaccination and that attitude items play a larger role than knowledge in explaining vaccine intention. It may be worth considering social conformism and confidence in systems for more targeted vaccine promotion, although this would make the task more complex: a more detailed understanding of social influences and of opinions about working conditions and politics among subgroups is required. A first step could be insisting on the fact that vaccine decision among HCWs is a professional question to be addressed by occupational health, apart from private social environment on one side, and political claims on the other.
In January 2022, the COVID-19 vaccination mandate in France was extended to a booster dose. Our findings can help improve COVID-19 vaccine acceptance among French healthcare and welfare sector workers in the perspective of a long-term strategy beyond the mandate, but also in other population groups, for other vaccines and in other countries.
Acknowledgements
We thank the GERES network members, U.R.P.S. Auvergne Rhône-Alpes and Union Française pour la santé bucco dentaire for distribution of the study invitation.
Ethical statement
The planning, conduct and reporting of the study was in line with the Declaration of Helsinki, as revised in 2013. We obtained ethical approval for the study from the ethics committee of the Centre Hospitalier Universitaire de Saint-Étienne (reference number: IRBN1092021/CHUSTE) and the survey database was registered by the Ecole des hautes études en santé publique the French School of Public Health according to the European Union General Data Protection Regulation (GDPR). Study participation was anonymous without possibility of indirect identification. Data including on self-reported vaccination status and self-assessed presence of a risk factor for severe COVID-19 were thus not considered sensitive personal data and no written informed consent was required. Persons visiting the study website saw the study information and had to agree to participation before starting the questionnaire.
Funding
The funder (Santé Public France) as an institution did not have any role in the conduct of the study or decision to submit this article.
Supplementary Data
Conflict of interest: None declared.
Authors’ contributions: Study design: CO, AGB, GP, DA, IB, ER, EBN, JEM; funding acquisition: IB, GP, ER; data collection: CO, AGB, GP, DA, IB, ER, EBN; data analysis: SM, JEM; manuscript drafting: SM, AGN, JEM; manuscript review: all authors have reviewed the manuscript and validated the final version.
References
- 1. Labetoulle R, Detoc M, Gagnaire J, Berthelot P, Pelissier C, Fontana L, et al. COVID-19 in health-care workers: lessons from SARS and MERS epidemics and perspectives for chemoprophylaxis and vaccines. Expert Rev Vaccines. 2020;19(10):937-47. 10.1080/14760584.2020.1843432 [DOI] [PubMed] [Google Scholar]
- 2.Santé Publique France. COVID-19: point épidémiologique du 8 juillet 2021. [COVID-19: epidemiological update of 8 July 2021]. Saint-Maurice: Santé Publique France; 2021. French. Available from: https://www.santepubliquefrance.fr/recherche/#search=COVID%2019%20%20%20point%20epidemiologique&publications=donn%C3%A9es®ions=National&sort=date
- 3. Gagneux-Brunon A, Detoc M, Bruel S, Tardy B, Rozaire O, Frappe P, et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021;108:168-73. 10.1016/j.jhin.2020.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mueller JE, Olivier C, Diaz Luevano C, Bouvet E, Abiteboul D, Pellissier G, et al. Étude transversale des intentions de vaccination contre la grippe saisonnière et la Covid-19 des professionnels de santé: quels leviers pour la promotion vaccinale? [Cross-sectional study of seasonal flu and Covid-19 vaccination intentions of healthcare professionals: what are levers for vaccine promotion?]. Bull. Epidémiol Hebd. 2021;(Cov_2):2-9. French. Available from: https://beh.santepubliquefrance.fr/beh/2021/cov_2/2021_Cov_2_ 1.html
- 5. MacDonald NE, SAGE Working Group on Vaccine Hesitancy . Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161-4. 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 6. Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13(12):e0208601. 10.1371/journal.pone.0208601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gigerenzer G. Moral satisficing: rethinking moral behavior as bounded rationality. Top Cogn Sci. 2010;2(3):528-54. 10.1111/j.1756-8765.2010.01094.x [DOI] [PubMed] [Google Scholar]
- 8. Seanehia J, Treibich C, Holmberg C, Müller-Nordhorn J, Casin V, Raude J, et al. Quantifying population preferences around vaccination against severe but rare diseases: A conjoint analysis among French university students, 2016. Vaccine. 2017;35(20):2676-84. 10.1016/j.vaccine.2017.03.086 [DOI] [PubMed] [Google Scholar]
- 9. Godinot LD, Sicsic J, Lachatre M, Bouvet E, Abiteboul D, Rouveix E, et al. Quantifying preferences around vaccination against frequent, mild disease with risk for vulnerable persons: A discrete choice experiment among French hospital health care workers. Vaccine. 2021;39(5):805-14. 10.1016/j.vaccine.2020.12.057 [DOI] [PubMed] [Google Scholar]
- 10. Verelst F, Willem L, Kessels R, Beutels P. Individual decisions to vaccinate one’s child or oneself: A discrete choice experiment rejecting free-riding motives. Soc Sci Med. 2018;207:106-16. 10.1016/j.socscimed.2018.04.038 [DOI] [PubMed] [Google Scholar]
- 11. Verger P, Scronias D, Dauby N, Adedzi KA, Gobert C, Bergeat M, et al. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill. 2021;26(3):2002047. 10.2807/1560-7917.ES.2021.26.3.2002047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, et al. Measuring trust in vaccination: A systematic review. Hum Vaccin Immunother. 2018;14(7):1599-609. 10.1080/21645515.2018.1459252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Díaz Luévano C, Sicsic J, Pellissier G, Chyderiotis S, Arwidson P, Olivier C, et al. Quantifying healthcare and welfare sector workers’ preferences around COVID-19 vaccination: a cross-sectional, single-profile discrete-choice experiment in France. BMJ Open. 2021;11(10):e055148. 10.1136/bmjopen-2021-055148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.French Ministry of Health and Solidarity. Les métiers de la santé. Les fiches-métiers. [Jobs in the healthcare system. Job descriptions]. Paris: Ministry of Health and Solidarity. [Accessed: Apr 2022]. French. Available from: https://solidarites-sante.gouv.fr/metiers-et-concours/les-metiers-de-la-sante/les-fiches-metiers/
- 15.French Ministry of Health and Solidarity. Les fiches-métiers du travail social. [Job descriptions for social work]. Paris: Ministry of Health and Solidarity. [Accessed: Apr 2022]. French. Available from: https://solidarites-sante.gouv.fr/metiers-et-concours/les-metiers-du-travail-social/les-fiches-metiers-du-travail-social/
- 16.French Ministry of Health and Solidarity. Quelle démographie récente et à venir pour les professions médicales et pharmaceutiques? [Recent and future demographics for professions in the medical and pharmaceutical fields]. Paris: Ministry of Health and Solidarity. Mar 2021. French. Available from: https://drees.solidarites-sante.gouv.fr/sites/default/files/2021-03/DD76_0.pdf
- 17.French Ministry of Health and Solidarity. La profession d’infirmière : situation démographique et trajectoires professionnelles? [Nurse profession: demographic situation and forward looking]. Paris: Ministry of Health and Solidarity. May 2011. French. Available from: https://drees.solidarites-sante.gouv.fr/sites/default/files/2020-10/er759.pdf
- 18. Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149-207. 10.1177/1529100618760521 [DOI] [PubMed] [Google Scholar]
- 19. Peretti-Watel P, Seror V, Cortaredona S, Launay O, Raude J, Verger P, et al. COCONEL Group . A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020;20(7):769-70. 10.1016/S1473-3099(20)30426-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chyderiotis S, Sicsic J, Raude J, Bonmarin I, Jeanleboeuf F, Le Duc Banaszuk AS, et al. Optimising HPV vaccination communication to adolescents: A discrete choice experiment. Vaccine. 2021;39(29):3916-25. 10.1016/j.vaccine.2021.05.061 [DOI] [PubMed] [Google Scholar]
- 21. Mignot A, Wilhelm M-C, Valette A, Gavard-Perret M-L, Abord-De-Chatillon E, Epaulard O. Behavior of nurses and nurse aides toward influenza vaccine: the impact of the perception of occupational working conditions. Hum Vaccin Immunother. 2020;16(5):1125-31. 10.1080/21645515.2019.1694328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Verger P, Collange F, Fressard L, Bocquier A, Gautier A, Pulcini C, et al. Prevalence and correlates of vaccine hesitancy among general practitioners: a cross-sectional telephone survey in France, April to July 2014. Euro Surveill. 2016;21(47):30406. 10.2807/1560-7917.ES.2016.21.47.30406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ward JK, Peretti-Watel P, Bocquier A, Seror V, Verger P. Vaccine hesitancy and coercion: all eyes on France. Nat Immunol. 2019;20(10):1257-9. 10.1038/s41590-019-0488-9 [DOI] [PubMed] [Google Scholar]
- 24. Chamoux A, Denis-Porret M, Rouffiac K, Baud O, Millot-Theis B, Souweine B. [Impact study of an active antiflu vaccination programme on the Clermont-Ferrand Teaching Hospital staff]. Med Mal Infect. 2006;36(3):144-50. 10.1016/j.medmal.2006.01.004 [DOI] [PubMed] [Google Scholar]
- 25. Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080-6. 10.1016/j.vaccine.2021.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32(19):2150-9. 10.1016/j.vaccine.2014.01.081 [DOI] [PubMed] [Google Scholar]
- 27. Fabrigar LR, Petty RE, Smith SM, Crites SL, Jr. Understanding knowledge effects on attitude-behavior consistency: the role of relevance, complexity, and amount of knowledge. J Pers Soc Psychol. 2006;90(4):556-77. 10.1037/0022-3514.90.4.556 [DOI] [PubMed] [Google Scholar]
- 28. Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, Dasch H, et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021;17(6):1612-21. 10.1080/21645515.2020.1846397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crawshaw J, Konnyu K, Castillo G, van Allen Z, Grimshaw J, Presseau J. Factors affecting COVID-19 vaccination acceptance and uptake among the general public: a living behavioural science evidence synthesis (v3, June 18th, 2021). Available from: https://www.researchgate.net/publication/353044590_HCW_Vaccination_Living_Behavioural_Science_Evidence_Synthesis_v3_Jun_18
- 30. Szmyd B, Karuga FF, Bartoszek A, Staniecka K, Siwecka N, Bartoszek A, et al. Attitude and behaviors towards SARS-CoV-2 Vaccination among healthcare workers: A cross-sectional study from Poland. Vaccines (Basel). 2021;9(3):218. 10.3390/vaccines9030218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Petravić L, Arh R, Gabrovec T, Jazbec L, Rupčić N, Starešinič N, et al. Factors affecting attitudes towards COVID-19 Vaccination: An online survey in Slovenia. Vaccines (Basel). 2021;9(3):247. 10.3390/vaccines9030247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lehmann BA, Ruiter RAC, Chapman G, Kok G. The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine. 2014;32(51):6986-91. 10.1016/j.vaccine.2014.10.034 [DOI] [PubMed] [Google Scholar]
- 33. Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):354-86. 10.1177/109019817400200405 [DOI] [PubMed] [Google Scholar]
- 34. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Paulussen TGW, Hoekstra F, Lanting CI, Buijs GB, Hirasing RA. Determinants of Dutch parents’ decisions to vaccinate their child. Vaccine. 2006;24(5):644-51. 10.1016/j.vaccine.2005.08.053 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.