Abstract
This study challenges two well-established associations in medical sociology: the beneficial effect of marriage on health and the predictive power of self-rated health on mortality. Using data from The National Health Interview Survey 1986–2004 with 1986–2006 mortality follow-up (789,096 respondents with 24,095 deaths) and Cox Proportional Hazards Models, we find the protective effect of marriage against mortality decreases with deteriorating health so that the married and unmarried in poor health are at similar risk for death. We also find the power of self-rated health to predict mortality is higher for the married than for any unmarried group. By using ordered logistic regression models, we find thresholds shift such that, compared to the unmarried, the married may not report poorer health until developing more severe health problems. These findings suggest the married tend to overestimate their health status. These two phenomena (diminishing protection and overestimation) contribute to but do not completely explain each other.
Keywords: marriage, mortality, predictive power, protective effect, self-rated health
The beneficial effect of marriage on health is one of the most established findings in medical sociology, demography, and social epidemiology (e.g., Waite 1995). An enormous literature has reported the protective effect of marriage on a variety of health outcomes, including self-rated health (SRH) (e.g., Rohrer et al. 2008) and mortality (e.g., Hu and Goldman 1990; Johnson et al. 2000; Waite 1995).
Similarly, the link between SRH and mortality is a persistent and well-established finding (Benyamini and Idler 1999; Idler and Benyamini 1997). SRH is an important and widely used measure of health (Goebeler, Jylha, and Hervonen 2007; Kawada et al. 2006; Rohrer et al. 2009) and a remarkably good predictor of objective health measures (Kennedy, Kasl, and Vaccarino 2001; Walker et al. 2004; Wilcox, Kasl, and Idler 1996).
Despite the persistent relationships between marital status and health and between SRH and mortality, research has neglected to delve more deeply into the intricacies of these relationships and how they may intersect. In this study, we use the National Health Interview Survey (NHIS) 1986–2004 with mortality follow-up data from 1986–2006, Cox Proportional Hazards Models, and ordered logistic regression to examine two related but distinct questions: (1) Do married people experience a protective effect against mortality across all levels of health, or is that protective effect stronger at mild or severe levels of health? We examine this question in terms of both SRH and more objective measures of health (e.g., activity limitations). (2) Do the married overestimate, underestimate, or accurately assess their health?
Marriage is often viewed as an important source of benefits for health; however, if the benefits of marriage diminish for certain levels of health status, this will have important implications for health promotion, disease prevention, and recovery. Furthermore, given the central role that measures of SRH play in the study of population health, marital status variation in reports of SRH will have important implications for the validity of SRH as an indicator of objective health and as a measurement to study health differentials by marital status.
BACKGROUND
Marital Status and Health
Most studies find that those who are married have better SRH than those who are single, divorced, widowed, or otherwise not married (e.g., Rohrer et al. 2008), and this trend of marital advantage has persisted across time (Liu and Umberson 2008). This relationship has held in various countries from Sweden (Lindstrom 2009) to Vietnam (Minh, Byass, and Wall 2010). Being married is also associated with lower risk of mortality than each non-married status (e.g., Johnson et al. 2000; Liu 2009). This lower relative risk of mortality for married people compared with non-married groups was also found in a meta-analysis of older adults, and this finding was robust to various statistical and sensitivity analyses and did not vary by gender, geographic location of the sample (North America or Europe), or the methodological quality of the study (Manzoli et al. 2007).
Very little research has addressed whether the protective effect of marriage on mortality is equally protective at different levels of health. It is possible that marriage may be most beneficial when health is not at its most harmful levels. Marriage may influence health through several pathways, such as buffering stress (Schwerdtfeger and Friedrich-Mai 2009), enhancing the flow of health-related information (Cohen 2004), shaping resources available, providing a sense of purpose, and increasing motivation and social pressure to behave in ways that promote health (Berkman and Glass 2000; Umberson 1992). These pathways may be especially useful to maintain good levels of health and reduce the likelihood of health’s deteriorating more so than influencing recovery once the level of health is more severe. Being married did not significantly influence one-year recovery from a state of exhaustion among older adults (Whitson et al. 2011) or the recovery or recurrence of depression over three years among older adults (Green et al. 1994). Married people had lower proportions of improvements in severity of disability over five years (Grundy and Glaser 2000), and marriage was not significantly associated with improvement in activities of daily living (ADL) in Israel or Italy (Gindin et al. 2007). Similarly, marital status was not related to changes in physical function or pain after hip replacement (MacWilliam et al. 1996). Goodwin et al. (1987) found the beneficial effect of being married on overall cancer survival was represented more in the stage of diagnosis, choice of treatment, and response to treatment than in final survival from cancer. This suggests a potentially diminished effect of marital status on health at more severe levels of health.
Another possibility if we find that marriage is not equally protective at all levels of health is that married people may overestimate their health. If married people do not report poor SRH until they reach more severe levels of health, then those who rate their health as poor are likely to be especially poor in health and likely to die sooner, which then may contribute to the diminishing protection effect of marriage. To address this possibility, we will examine whether married people overestimate their health and whether we find the same pattern of diminishing protection with more objective measures of health than self-ratings of health.
Ratings of Health and Potential Overestimation
SRH involves a relatively simple question asking respondents to rate their health on a scale with four or five categories including poor, fair, good, (very good), and excellent. It has been consistently linked with mortality in both the short- and the long-term, including more than 5 years (Hays et al. 1996), 12 years (Idler and Angel 1990), and 28 years (Strawbridge and Wallhagen 1999). This relationship persists after adjusting for a wide variety of control variables, including sociodemographic variables, mobility impairment, chronic conditions, health risk factors (Strawbridge and Wallhagen 1999), health behaviors, use of health services, cognitive function, affective mood, negative life events (Hays et al. 1996), demographic and clinical confounders (Thong et al. 2008), performance-based measures of functioning, anthropometric measures (Lyyra et al. 2006), and biomarkers (Jylha, Volpato, and Guralnik 2006).
There is evidence, however, suggesting that the relationship between SRH and mortality may vary across some groups. For instance, there are mixed findings with respect to the strength of the relationship between SRH and mortality by gender. Most of these studies suggest that the impact of SRH on mortality is stronger among men (Deeg and Kriegsman 2003; Okamoto et al. 2008; Spiers et al. 2003); however, there is some evidence of a stronger relationship among women (Lyyra et al. 2009). Some studies also suggest differences in this relationship by race, with a stronger impact of SRH on mortality among whites than African Americans (Franks, Gold, and Fiscella 2003; Lee et al. 2007). Some studies find the impact of SRH on mortality was stronger among those with higher socioeconomic status (SES) than their counterparts (Franks et al. 2003; Regidor et al. 2010).
Group differences in the predictive power of SRH on mortality may stem from groups’ estimating their health differently. Different groups may attribute different meanings or different frames of reference when rating their health (Franks et al. 2003). Krause and Jay (1994) found people often incorporated specific health problems, physical functioning, or health behaviors into their ratings of health, but the referents used varied across groups. One of the interpretations for gender differences is that men may incorporate more life-threatening conditions whereas women may incorporate more disabling but non-fatal conditions in their ratings of health (Deeg and Kriegsman 2003). One interpretation of SES differences is that less advantaged individuals may be more pessimistic in their health ratings due to their lack of social and financial resources, which may dilute the strength of the effect of SRH on mortality (Dowd and Zajacova 2007).
One of the implications of the differential predictive power of SRH on mortality by group is the potential overestimation or underestimation of self-ratings of health by group members. For example, Melzer and colleagues (2004) found that those with higher income had different thresholds for mobility disability, such that they reported difficulties only when they reached more severe levels, suggesting overestimates of good health. Idler, Hudson, and Leventhal (1999) suggest that those who overestimate their health have the most inclusive definitions of health that may incorporate things like social relationships and social activities as well as health risk behaviors and diagnoses.
Research has neglected to examine whether other groups beyond race, gender, and SES may rate their health differently. There is reason to suspect that married people may overestimate their health, and given the important and well-established relationship between marital status and better health (Dupre, Beck, and Meadows 2009), the married are an important group to examine with respect to whether they overestimate, underestimate, or accurately report their health, with important implications for research estimating SRH differentials by marriage. Since those who overestimate their health are more likely to incorporate things like social relationships into their health ratings (Idler et al. 1999), we might suspect that married people, who are embedded in a particularly important social relationship, would be prime candidates for including social relationships and activities into more inclusive definitions of health and possibly leading to overestimation of their health. In addition, similar to Dowd and Zajacova’s (2007) interpretation of differences by SES, if a disadvantaged group is more pessimistic about its health, it suggests that married people, as an advantaged group, may be more optimistic about their health than their non-married counterparts. Married people may have different thresholds for what they consider to be better or worse health, similar to differences in thresholds for those advantaged with greater income (Melzer et al. 2004). Although there is a dearth of research on marital status differences in how people rate their health, the evidence available suggests that married people may be more likely to overestimate their health than their non-married counterparts.
Hypotheses
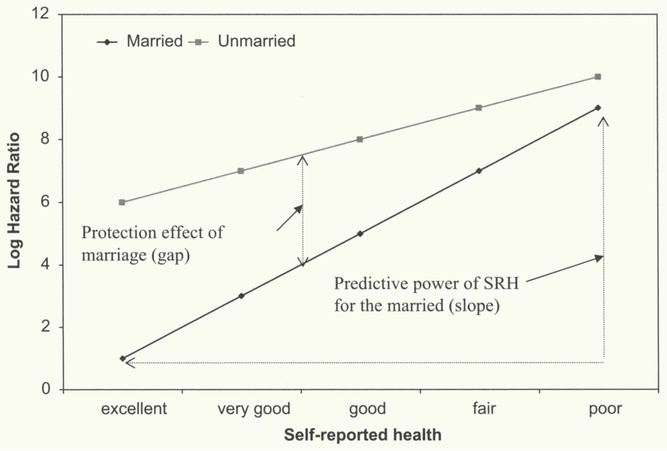
Based on the available evidence, we hypothesize (1) married people will experience diminished protection at the most severe levels of health compared to those belonging to the other marital statuses and (2) married people will overestimate their health. We test these hypotheses by comparing relative and absolute mortality rates of married and unmarried individuals at different levels of health. We use both SRH and objective health measures (activity limitations, activities of daily living [ADL], and instrumental activities of daily living [IADL]) in the first hypothesis. The diminishing protection hypothesis and the overestimation hypothesis are not mutually exclusive, as they refer to different phenomena. Graphically, as depicted in Figure 1, the diminishing protection hypothesis refers to the gap in log hazard ratios of mortality on marital status by different levels of SRH or objective health (SRH in this illustration). If this gap shrinks with increasingly worse health, then the protective effect of marriage decreases. If marriage were equally protective at each level of health, then the lines for the married and unmarried would be parallel. The overestimation hypothesis, however, refers to the slope of the log hazard ratio of mortality on SRH for each marital status group. If a group has a steeper slope, the predictive power of SRH is higher for this group (the married in this graphic illustration).1
Figure 1.
A Graphic Illustration of the Difference between Predictive Power of Self-Rated Health and the Protective Effect of Marriage.
It deserves clarification here that the overestimation hypothesis implies that the predictive power of SRH on mortality (i.e., the association between SRH and mortality) is stronger among the married than the unmarried as overestimation of health suggests the married may not report poor health until it reaches a more severe level, which then increases the responsiveness of mortality to poor health among the married, that is, a steeper slope. In this sense, higher predictive power of SRH on mortality is a necessary condition for the overestimation hypothesis to be valid. In other words, if the predictive power of SRH on mortality is lower among the married, then the overestimation hypothesis must be false. But this is not a sufficient condition, as higher predictive power of SRH on mortality could mean either overestimation or more accurate estimation of health status. Therefore, we will also test SRH reporting heterogeneity as described in the Method and Results sections to further investigate the overestimation hypothesis.
DATA AND METHOD
Data
Data are from the NHIS 1986–2004, with mortality follow-up data from 1986–2006. The NHIS is a multistage probability sample survey of the civilian non-institutionalized U.S. population conducted annually by the National Center for Health Statistics. Respondents interviewed between 1986 and 2004 are linked to the death records in the National Death Index 1986–2006 through a probabilistic record-matching method based on 12 criteria to ascertain the vital status of each respondent. We limit our analysis to respondents age 25 and older as a high proportion of young adults have not completed education prior to age 25. Only non-Hispanic whites and non-Hispanic blacks are included in the analysis. In the final sample, we have 789,096 respondents with 24,095 deaths during the three-year follow-up.
Outcome Variable
Mortality.
We constrain the mortality follow-up to a three-year (i.e., 12-quarter-year) period because the NHIS does not follow up the respondent’s marital status from the year of survey. A three-year period reduces the potential bias resulting from changes in marital status. We also truncate the mortality follow-up to different time periods, which do not substantially change the results as reported in Appendix I in the online supplement (available at http://jhsb.sagepub.com/supplemental).
Main Explanatory Variables
Marital status.
This variable includes five categories: married, never married, separated, divorced, and widowed. In our data, 542,781 respondents are married, 88,783 never married, 18,479 separated, 76,506 divorced, and 62,547 widowed. The corresponding numbers of deaths for these five marital statuses are 12,732, 1,700, 512, 2,143, and 7,008.
SRH.
This variable has remained largely unchanged across periodic revisions of the NHIS questionnaires. It has five response categories: poor, fair, good, very good, and excellent. We treat SRH as both a continuous variable (where excellent = 0, very good = 1, good = 2, fair = 3, poor = 4) and a set of dummies (where excellent is the reference group) to ascertain that the findings are not affected by the coding of SRH.
Activity limitation.
The NHIS asked respondents if they were limited in activities such as work, school, personal care, physical health, and any other activities. The coding of this synthetic variable is a little different across surveys. For example, the 1986 survey has four categories: (1) unable to perform major activity, (2) limited in kind/amount of major activity, (3) limited in other activities, and (4) not limited (includes unknowns). The 2002 survey has three categories: (1) limited in any way, (2) not limited in any way, and (3) unknown if limited. We recoded respondents who were limited in any activities as 1, otherwise, 0, to make the coding consistent across surveys.
ADL and IADL.
The question about the need for help with routine tasks asks respondents if they are able to perform IADL, including everyday household chores, necessary business, shopping, and getting around for other purposes. The question about personal care needs asks respondents if they are able to perform ADL, including eating, bathing, dressing, using the toilet, and getting around inside their homes. Before 1997, the question about routine needs was combined with a question about personal care needs. Since 1997, the routine needs question has been separated from the personal care question. Because it is difficult to separate routine needs from personal care for data before 1997, we combined IADL and ADL information into one variable for data after 1997. Respondents who need help for any personal care or routine need were coded 1, otherwise, 0, which makes this variable comparable across all waves of data. Another complication is the different age ranges to which these questions were posed. Prior to 1997, these questions were asked of sample members aged 70 and younger; after 1997, they were asked of all respondents. Due to this problem, we did sensitivity analyses separately by these two time periods, and the findings are very similar.
Control Variables
We also control for several variables that are established correlates of health: survey year, family income adjusted for inflation, years of fonnal education, work status (1 =full-/part-time job, 0 = not employed), sex (1 = male, 0 = female), race (1 = white, 0 = black), age (in years), and age squared.
Method
We use Cox Proportional Hazards Models to estimate the effect of SRH/activity limitation/ADL and IADL, marital status, and their interactions on the subsequent three-year (i.e., 12-quarter-year) mortality risk after controlling for individual covariates (e.g., age, gender, race, and SES). This model can be specified as:
where i indexes individuals and t represents time. h0(t) is the baseline hazard function when X = 0, representing the baseline death hazard at time t. To make h0(t) meaningful, we grand mean centered all the continuous variables; thus, h0(t) represents the death hazard with all continuous variables at grand mean level and categorical variables at reference group. hi(t) is the death hazard at time t when X = x, a set of covariates. Each unit increase in x increases the log hazard by β unit or the hazard by (eβ-l)*100%.
In this model specification, we treated SRH as a continuous variable with excellent health equal to 0 for simplicity. As the diminishing protection hypothesis tests the gaps in the absolute mortality risk among five marital statuses across the spectrum of SRH, we need to include the main effects of marital status in this calculation. That is, 0, α, 2α, 3α, and 4α represent the log hazard ratios of marriage on mortality risk from excellent health to poor health. λ1, λ1 + κ1 + α, λ1+α, λ1+2κ1+2α, λ1+3κ1+3α and λ1+4κ1+4α represent the log hazard ratios of never married on mortality risk from excellent health to poor health. The same rationale applies to the other marital statuses.
As the overestimation hypothesis concerns the slope of mortality on SRH for each marital status (i.e., relative mortality risk at other levels of SRH compared to excellent health for each marital status), we do not need to include the main effects of marital status (λ1, λ2, λ3, λ4) in the calculation of predictive power of SRH. Then α represents the slope of the log hazard ratio of mortality on SRH for the married (the reference group), and α+k1, α+k2, α+k3, α+k4, for the never married, separated, divorced, and widowed, respectively. Although the above calculations use SRH as a continuous variable for simplicity, we also treated SRH as an ordered variable and calculated the relative and absolute mortality risk in the same way.
Cox Proportional Hazards Models, however, cannot tell whether the married are likely to overestimate their health as the higher predictive power of SRH on mortality is a necessary but not sufficient condition for overestimation, as discussed in the Hypotheses section. Therefore, we further examine the latent structure of SRH or reporting heterogeneity among the married and the unmarried to test the overestimation hypothesis. The ordered logit regression model posits an underlying latent continuous variable corresponding to an ordered categorical response variable along which sample responses can be arrayed (Fox 2008:363–68). The continuous variable is conceived of as dissected into m regions by m − 1 thresholds or boundaries of varying width. The ordered logit model permits estimation of the thresholds, which then can be used to assess whether the latent thresholds deviate from the ordered categorical responses. If the latent threshold above which the married start reporting poor health is much higher than the response value of fair health (which is equal to 3 in this study), then the married are more likely to overestimate their health. We use SAS Proc Glimmix with multinomial distribution and clogit link function to obtain the latent thresholds for each marital status by estimating ordered logistic regression for each marital status with SRH as an outcome variable and individual sociodemographic covariates controlled.
RESULTS
Does the Protective Effect of Marriage Decline with Deteriorating Health?
Table 1 shows the hazard ratios for the Cox Proportional Hazards Model of mortality within three years on individual SRH, marital status, and other covariates. Due to the large number of interactions between marital status (married as reference) and dummy variables for each category of the five-point SRH scale (excellent as reference), we present the models estimated by treating SRH as a continuous variable where excellent health is coded 0 and higher scores reflect worse health. Findings are very similar when SRH is treated as a categorical variable.
Table I.
Hazard Ratios for Cox Proportional Hazards Model of Mortality within Three Years on Individual Self-Rated Health (SRH), Marital Status, and Other Covariates.
| All-cause Mortality | |
|---|---|
|
| |
| SRH | 1.856** |
| Never married | 2.033** |
| Separated | 2.188** |
| Divorced | 1.876** |
| Widowed | 2.153** |
| SRH × Never Married | .883** |
| SRH × Separated | .851** |
| SRH × Divorced | .896** |
| SRH × Widowed | .815** |
Note: The model controls for survey year, age, age squared, gender, race, education, family income, and employment status. Higher scores on self-rated health indicate worse health.
p < .01.
p < .001.
Being unmarried (i.e., never married, separated, divorced, and widowed) significantly increases the mortality risk. For example, the mortality risk for the never married is two times that for the married at the level of excellent health. The interaction effects can be interpreted as the higher risk of being unmarried compared with being married for mortality declines for worse self-ratings of health. For example, every unit increase in worse SRH decreases the risk of being unmarried on subsequent mortality by 12 percent (100 * [1 – .883]) for the never married, 15 percent for the separated, 10 percent for the divorced, and 18 percent for the widowed.
Part I in Table 2 presents the differences in the absolute mortality risk among the five marital status groups where SRH is treated as a set of dummies and excellent is the reference. The main effects of marital status are included in the calculation of log hazard ratios as we are interested here in how the absolute mortality risk among different marital statuses may vary by different levels of SRH. At the level of excellent health, the log hazards of dying in the subsequent three years for the never married, the separated, the divorced, and the widowed are .56, .46, .48, and .66 units higher, respectively, than that for the married.2 But at the level of poor health, the log hazards of dying in the subsequent three years for the never married and divorced are .18 and .15 units higher, respectively, and the separated and widowed are .01 and .09 units lower, respectively, than that for the married. Therefore, the advantage of being married with regard to mortality risk declines when self-reported health deteriorates.
Table 2.
Relative and Absolute Mortality Risk among the Married and the Unmarried.
| Part I.Absolute Mortality Risk Differences among Five Marital Status Groups (Log Hazard Ratio in the Cell) | |||||
|
| |||||
| Married | Never Married | Separated | Divorced | Widowed | |
|
| |||||
| Excellent | 0 | .559 | .462 | .483 | .660 |
| Very good | .267 | .844 | .860 | .767 | .847 |
| Good | .788 | 1.295 | 1.404 | 1.268 | 1.138 |
| Fair | 1.380 | 1.786 | 1.777 | 1.693 | 1.582 |
| Poor | 2.295 | 2.479 | 2.287 | 2.441 | 2.210 |
|
| |||||
| Part II. Relative Mortality Risk Compared to Excellent Health for Each Marital Status Group (Hazard Ratio in the Cell) | |||||
|
| |||||
| Married | Never Married | Separated | Divorced | Widowed | |
|
| |||||
| Very good | 1.305 | 1.329 | 1.489 | 1.327 | 1.205 |
| Good | 2.198 | 2.086 | 2.565 | 2.191 | 1.613 |
| Fair | 3.975 | 3.411 | 3.723 | 3.353 | 2.513 |
| Poor | 9.927 | 6.821 | 6.201 | 7.086 | 4.710 |
Note: All models control for survey year, age, age squared, gender, race, education, family income, and employment status. Excellent and Married are the reference groups.
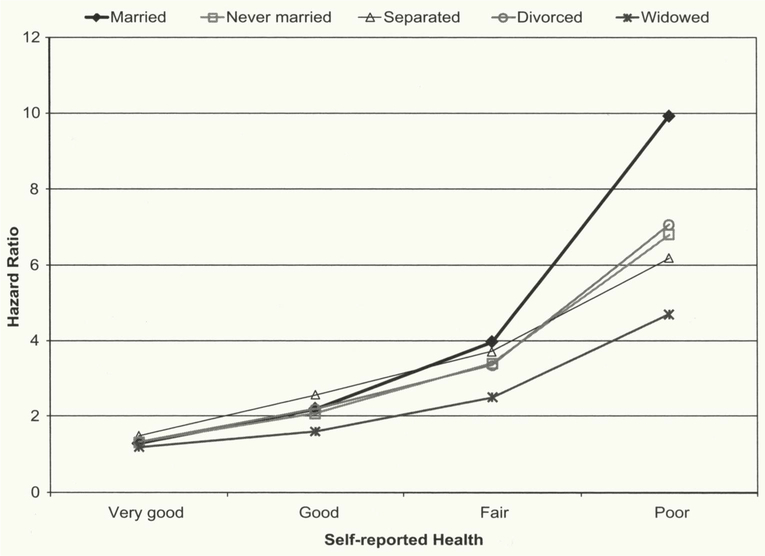
Figure 2 plots the log hazard ratios of mortality on marital status by levels of SRH based on Part I in Table 2. It deserves reiterating the essential idea delivered in Figure 1 that the diminishing protection hypothesis concerns the gap in mortality risk at each level of SRH between the married and unmarried. As can be seen from this figure, the absolute mortality risk is significantly lower for the married at excellent health, but the gap in log hazard ratios between the married and unmarried decreases as health declines. At poor levels of health, married people have a slightly higher risk of dying than the widowed and separated, although this difference is not significant. These findings show that the advantage of being married shrinks with declining SRH and disappears at poor health. In other words, the protective effect of marriage from death decreases with deteriorating health.
Figure 2.
Log Hazard Ratios of Mortality on Marital Status by Levels of Self-Rated Health, Based on Part I of Table 2.
Do Married People Overestimate Their Health?
As shown in the All-cause Mortality column in Table 1, every unit increase in worse SRH increases the death hazard by 86 percent ([1.856 − 1] * 100) for the married. All the interaction terms suggest that being unmarried decreases the predictive power of SRH on the death hazard. For example, every unit increase in worse SRH increases the death hazard by 64 percent (100 * [1.856 * 0.883 − 1]) for the never married, 58 percent for the separated, 66 percent for the divorced, and 51 percent for the widowed. These numbers are all lower than 86 percent (the increased hazard for the married), which suggests the predictive power of SRH on mortality is higher for the married than for the unmarried.
Part II in Table 2 presents the relative mortality risk at other levels of SRH compared to excellent health for each marital status group. The main effects of marital status are excluded in the calculation of hazard ratios as we are interested here in how the predictive power of SRH varies by marital status rather than how the absolute mortality risk differences among different marital statuses may vary by different levels of SRH. Married people who report poor health have 10 times the risk of dying compared to married people who report excellent health, while the never married, the separated, the divorced, and the widowed who report poor health have 7, 6, 7, and 5 times the risk of dying relative to those in each respective status who report excellent health.
Figure 3 plots the predictive power of SRH on mortality by marital status based on Part II in Table 2. It deserves reiterating the essential idea delivered in Figure 1 that the predictive power is only concerned with the slope of mortality on SRH within each marital status and has nothing to do with the gap in mortality hazard at each level of SRH between the married and the unmarried. As seen in Figure 3, the effect of reporting poor health compared to excellent health on subsequent mortality risk is significantly higher for the married than for the unmarried. The slope for the married curve is steeper than that for other groups, which indicates subsequent mortality is more responsive to SRH for the married. In other words, the predictive power of SRH on mortality is higher for the married than for the unmarried.
Figure 3.
Predictive Power of Self-Rated Health on Mortality by Marital Status, Based on Part II of Table 2.
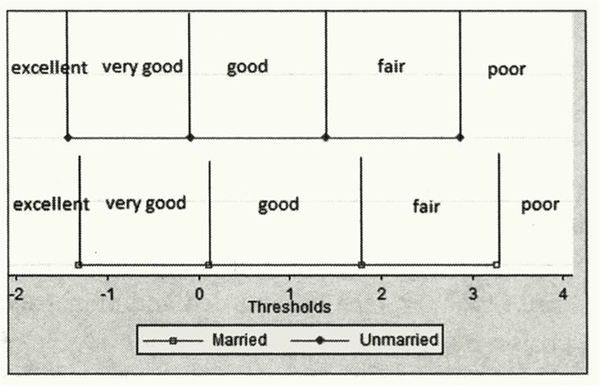
Does this mean that the married more accurately estimate their health than the unmarried or that the married are more likely to overestimate their health, which results in higher relative mortality risk when they report poor health? As discussed in the Hypotheses and Method sections, higher predictive power of SRH on mortality among the married is a necessary but not sufficient condition for supporting the overestimation hypothesis; therefore, we further test SRH reporting heterogeneity among the married and the unmarried as illustrated in Figure 4.3 The thresholds are retrieved from ordered logistic regression on SRH separately by marital status. This model assumes that SRH has a latent continuous structure, where higher values indicate worse health, and the thresholds indicate the cut-points in the values of this latent variable.
Figure 4. Self-Rated Health Reporting Heterogeneity among the Married and the Unmarried.
Note: The differences in all the thresholds between the married and the unmarried are statistically significant.
For example, the married report poor health when the value of the latent variable is greater than 3.26, while the unmarried start reporting poor health when the latent variable value is greater than 2.88. As can be seen from this figure, the married have consistently stricter standards for what is considered worse health as all the thresholds shift to the right, which is called an “index shift” (Dowd and Zajacova 2007; Lindeboom and van Doorslaer 2004). The threshold above which to report poor health for the married, which is 3.26 (3.24, 3.28), is significantly higher than the response value of fair health (which is equal to 3) and the threshold for the unmarried, which is 2.88 (2.85, 2.90). These findings suggest the married may not report poor health until their health is in a severe condition. The threshold below which to report excellent health is further shifted to the left for the unmarried than for the married, which suggests the unmarried have a stricter standard for reporting excellent health and may potentially underestimate their health.
It merits clarification here that the unmarried have a stricter standard for reporting excellent health not because there are fewer of them in this status. The unmarried are less likely to report excellent health and more likely to report poor health than the married, but this observed SRH distribution has nothing to do with the SRH reporting heterogeneity test. We did not compare the distribution of observed categorical responses or the position of latent thresholds between the married and the unmarried but instead compared the position of ordered categorical responses and the position of latent thresholds within the married and within the unmarried, respectively.
Diminishing Protection Tested with More Objective Measures of Health
It is possible that we see the diminishing protection of marriage at the poorer levels of health because married people inflate their self-ratings of health. Thus, we tested whether this pattern is replicable with more objective health measures than SRH. We examine the changes in the log hazard ratios of mortality on marital status by activity limitation and ADL/IADL as shown in Table 3. Consistent with the results using SRH, the smaller-than-1 hazard ratios for all the interaction effects suggest the detrimental effects of being unmarried (i.e., never married, separated, divorced, and widowed) relative to the married on subsequent three-year mortality risk decline when people have worse health measured by activity limitations or difficulties with ADL/IADL. These findings show that the diminishing protection of marriage on mortality is not an artifact of the use of SRH.
Table 3.
Hazard Ratios for Cox Proportional Hazards Model of Mortality within Three Years on Individual Activity Limitation (AL), Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL), Marital Status, and Other Covariates.
| Model 1 | Model 2 | |
|---|---|---|
|
| ||
| AL | 3.003** | |
| ADL/IADL | 4.357** | |
| Never married | 1.544** | 1.671** |
| Separated | 1.657** | 1.616** |
| Divorced | 1.389** | 1.517** |
| Widowed | 1.346** | 1.328** |
| AL × Never Married | .814** | |
| AL × Separated | .738* | |
| AL × Divorced | .913 | |
| AL × Widowed | .779** | |
| ADL/IADL × Never Married | .566** | |
| ADL/IADL × Separated | .519** | |
| ADL/IADL × Divorced | .648** | |
| ADL/IADL × Widowed | .677** | |
Note: All models control for survey year, age, age squared, gender, race, education, family income, and employment status.
p < .01.
p < .001.
Gender-specific Analysis
Appendices II and III in the online supplement (available at http://jhsb.sagepub.com/supplemental) show the stratified gender-specific analysis. Appendix II suggests for both men and women, the predictive power of SRH on mortality is higher for the married than for the unmarried as the coefficients for the interaction terms SRH and each marital dummy are smaller than 1, which is consistent with Table 1; however, we found significantly greater predictive power of SRH on mortality only for never married women compared to never married men and for widowed women compared to widowed men. These significant differences hold when SRH is treated as a continuous variable but disappear when SRH is treated as a categorical variable.
Appendix III supports that in general the married have a stricter standard for what is considered worse health as all the thresholds shift to the right for both men and women. In other words, married men and women may not report poor health until their health is in a severe condition. The differences among thresholds for unmarried men and unmarried women are not significant. Married men have a less strict standard for what is considered excellent and very good health but the same strict standard for what is considered poor health as do married women.
As the coefficients for the interaction terms between SRH and each marital status dummy are smaller than 1 for both men and women, the protective effect of marriage declines with deteriorating health for both genders. The protection effect of marriage relative to never married and widowed declines with deteriorating health at a slightly faster rate for women than for men, but these significant differences hold only when SRH is treated as a continuous variable and disappear when SRH is treated as a categorical variable.
DISCUSSION
Two well-established and important findings in medical sociology are (1) the beneficial effect of marriage on health and (2) the predictive power of SRH on mortality. But questions remain in these two relationships: First, does marriage have equally protective effects on the continuous spectrum from health to illness? Second, is SRH an equally valid indicator of objective health across marital groups?
We probe these questions using the NHIS 1986–2004 with mortality follow-up data from 1986–2006, Cox Proportional Hazards Models, and ordered logistic regression. We find that the protective effect of marriage on mortality decreases with deteriorating health and finally diminishes at poor health. This finding holds for SRH as well as more objective health measures (e.g., activity limitations, ADL/IADL); that is, marriage does not have significant protective effects against mortality when the married are in worse health due to activity limitations or difficulty with ADL/IADL. Current research suggesting that marriage is not related to or less important for recovery from more severe health issues (Goodwin et al. 1987; Grundy and Glaser 2000; Whitson et al. 2011) supports the idea that the protective effect of marriage may not be as strong at worse levels of health. Since married people often engage in healthier behaviors, this may reduce the likelihood of some health problems, but even those with generally healthy behaviors may experience debilitating disease. Thus, marriage may be more important for disease prevention, but it may be more limited in recovery from illness or severe health problems.
We also find that the predictive power of SRH on subsequent three-year mortality risk is higher for the married than for the four unmarried groups; that is, every unit increase in worse SRH increases the relative mortality risk to a larger extent for the married than for the unmarried. By using ordered logistic regression models, we find the thresholds for reporting fair and poor health are significantly higher for the married than for the unmarried compared to the ordered categorical responses, which means the married may not report bad health until their health reaches an especially severe level. Indeed, there is an index shift in the thresholds, which suggests married people uniformly have a stricter standard for what is considered worse health than the unmarried. These findings suggest the married are more likely to overestimate their health, which leads to a higher predictive power of SRH on mortality among the married than the unmarried.
There are several possible reasons that married people may overestimate their health. One potential reason is that people who have definitions of health that include social activities and relationships are more likely to overestimate their health (Idler et al. 1999), so married people who are embedded in a particularly important social relationship could be more likely to include social relationships in their definitions of health and thus be more likely to overestimate it. Second, studies of SES differences suggest that advantaged groups may be especially optimistic about their health (Dowd and Zajacova 2007) and may have higher thresholds for what they consider worse health (Melzer et al. 2004), which supports the idea that married people, as another advantaged group, may be likely to overestimate their health. Married people may be more optimistic about their health because of the resources gained through marriage and thus rate it as better than it is. Related to this, the social support embedded within many marital relationships may influence spouses with health problems to not rate their health as poorly as it objectively is because their spouse is helping them cope with their issues. In other words, their health problems may not affect their lives as much because of that support from marriage, so they may not perceive themselves to be in poor health. Another possibility is that because married people often engage in better health behaviors than non-married people, they perceive themselves as healthier regardless of whether they objectively are or not.
The overestimation and diminishing protection hypotheses are not contradictory to each other but rather may contribute to each other. On the one hand, because married people are more likely to overestimate their health, their objective health may be quite bad and possibly worse than the unmarried when they report their health as fair or poor. This likely contributes to the diminishing protective effect of marriage in poor health to some extent. In other words, if the married did not overestimate their health, the protective power of marriage may diminish to a lesser extent. On the other hand, because of the diminishing protective effect of marriage at poor health, the relative mortality risk at poor health compared to excellent health is particularly larger for the married than for the unmarried, which likely contributes to married people’s overestimation of health to some extent. In other words, if the protective effect of marriage did not decline, married people’s overestimation of health may be reduced to some extent.
Married people’s overestimation of health and the diminishing protective effect of marriage do not completely explain each other, however. The diminishing protective effect of marriage does not only result from the overestimation propensity among the married, as replacing SRH with other objective health measures does not change the pattern. The overestimation propensity among the married does not only result from the diminishing protective effect of marriage as the thresholds analysis suggests married people uniformly have a stricter standard for what is considered bad health. Graphically, these two phenomena do not necessarily coincide. For example, hypothetically, if we moved the “married” line above the “unmarried” line in Figure 1, we would still support the overestimation hypothesis but not the diminishing protection hypothesis. In this sense, these two phenomena contribute to each other but do not completely explain each other.
This study takes a unique approach to evaluate the overestimation hypothesis through testing SRH reporting heterogeneity derived from ordered logistic regression models; many extant studies, however, test the predictive power of SRH by comparing it to objective health measures. In line with these studies, we also tested the relationship between SRH and activity limitation, ADL/IADL, and morbidity conditions (e.g., cancer and heart diseases). All these results support a stronger correlation between SRH and these objective health measures among the married than the unmarried (table available on request), which is consistent with the higher predictive power of SRH on mortality (which probably is the most solid measure of objective health) among the married.
Extant literature suggests men benefit more from marriage than do women (Berkman and Breslow 1983). Enlightened by this line of research, we explored the possible gender difference in the diminishing protection effect of marriage and in the overestimation of health among the married. Gender-specific analysis replicated the major findings in this article; that is, for both men and women, (1) the protective effect of marriage declines with deteriorating health, (2) the predictive power of SRH on mortality is higher for the married than for the unmarried, and (3) the married tend to overestimate their health. We found very few gender differences. The protection effect of marriage relative to never married and widowed declines with deteriorating health at a slightly faster rate for women than for men. We found significantly greater predictive power of SRH on mortality for never married women than for never married men, and for widowed women than for widowed men, but these significant differences hold only when SRH is treated as a continuous variable and disappear when SRH is treated as a categorical variable. Although married men have a less strict standard for what is considered excellent and very good health than do married women, we did not find significant gender differences in the SRH reporting heterogeneity among the married and unmarried. Although extant literature has found that men benefit more from marriage than do women, this does not necessarily provide a clear theoretical rationale for a gender difference in the overestimation of health among the married or the diminishing protection effect of marriage. Indeed, there has been mixed evidence about gender differences in the strength of the relationship between SRH and mortality (Lyyra et al. 2009; Okamoto et al. 2008), so it is not clear that there would be a gender difference among the married or unmarried. Future research, however, should continue investigating these research questions by using different datasets and possibly different research designs.
One of the limitations of this study is that NHIS data do not follow up respondents’ marital status from the year of survey; therefore, we have to constrain the mortality follow-up to a 12-quarter-year period to reduce the potential bias resulting from changes in marital status (e.g., Liu 2009). For sensitivity analysis, we also truncate the mortality follow-up to different time periods, which do not substantially change the results as reported in Appendix I in the online supplement. This indicates the findings are relatively solid. Future research could replicate the analyses in this study with other datasets. Another limitation is that we are not able to capture a specific and complete profile of physical functioning (e.g., acute or chronic condition) and test whether the married are more likely to underreport physical problems even if they have the same problems as the unmarried. Although we did test the association between SRH and activity limitation, ADL/IADL, and morbidity conditions (e.g., cancer and heart diseases), due to data limitations we could not test the discrepancy between true problem and reporting problem. Future research may further explore this direction by using a dataset with better measures of physical functioning.
Despite limitations, this study provides compelling evidence that married people may overestimate their health and that the protective effect that marriage accords may diminish at the most severe levels of health. Although different marital groups may evaluate their health differently, this does not distort much the validity of SRH as a proxy for objective health when it is used as an explanatory variable because more objective measures of health, such as ADL/IADL and activity limitations, also show marriage’s diminishing protection from mortality at worse levels of health. However, the overestimation of health by married people suggests the use of caution when SRH is used to measure health differentials by marital status. Because of married people’s overestimates of their health, the difference between the married and the unmarried (especially the widowed) in SRH may be larger than their real difference in objective health status. Therefore, when SRH is used to measure health differentials, there is the possibility that the health benefits of marriage may be inflated. Although marriage is certainly related to health as reported in much prior research, the diminishing protective effect at poorer levels of health found in our study suggests that marriage may not be equally protective at all levels of health. Marriage is also less beneficial for people in worse health due to activity limitations or ADL/IADL difficulties. This may have important implications for the role of marriage in health promotion versus recovery from serious illness.
Supplementary Material
ACKNOWLEDGMENTS
We thank the anonymous reviewers for their helpful comments.
FUNDING
Patricia A. Thomas has received support from the grant 5 T32 HD007081, Training Program in Population Studies, awarded to the Population Research Center at the University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Health and Child Development.
Biography
Hui Zheng is an assistant professor of sociology at The Ohio State University. His scholarship applies advanced statistical and demographic methods and interdisciplinary perspectives to study the causes and consequences of health, obesity, aging, and mortality. His scholarship has appeared in American Sociological Review, Demography, Social Science & Medicine, and Criminology.
Patricia A. Thomas is a postdoctoral fellow at the Population Research Center at the University of Texas at Austin. Her research examines the impact of social relationships and social position on health across the life course. Her scholarship has appeared in Journal of Gerontology, Social Science & Medicine, American Journal of Public Health, and Journal of Aging & Health.
Footnotes
Predictive power of self-rated health (SRH) on mortality refers to the association between SRH and mortality. Predictive power is not equal to the degree of accuracy. A higher predictive power may imply higher accuracy of reporting health or overestimation of health. For simplicity and consistency with extant literature, we use “predictive power” rather than “association between SRH and mortality.”
The mortality risk for the married at excellent health is 0 because The Married is the reference group. It does not mean that the married have 0 mortality risk when they report excellent health. The married have smaller mortality risk at excellent or very good health than the unmarried not because the unmarried overestimate their health but because of the protection effect of marriage. When we do between-group comparisons, we need to take into account the main effect of group characteristics. Overestimation of health, however, is concerned with within-group comparison, that is, the effect of other levels of SRH compared to excellent health on mortality within each marital status.
We also did the analysis separately for each unmarried status, with similar findings. For the sake of simplicity and clarity in the figure, we group these unmarried statuses.
REFERENCES
- Benyamini Yael and Idler Ellen L.. 1999. “Community Studies Reporting Association between Self-rated Health and Mortality: Additional Studies, 1995 to 1998.” Research on Aging 21:392–401. [Google Scholar]
- Berkman Lisa F. and Breslow Lester. 1983. Health and Ways of Living: The Alameda County Study. New York: Oxford University Press. [Google Scholar]
- Berkman Lisa F. and Glass Thomas. 2000. “Social Integration, Social Networks, Social Support, and Health.” Pp. 137–73 in Social Epidemiology, edited by Berkman LF and Kawachi I. New York: Oxford University Press. [Google Scholar]
- Cohen Sheldon. 2004. “Social Relationships and Health.” American Psychologist 59:676–84. [DOI] [PubMed] [Google Scholar]
- Deeg Dorly J. H. and Kriegsman Didi M. W.. 2003. “Concepts of Self-rated Health: Specifying the Gender Difference in Mortality Risk.” Gerontologist 43:376–86. [DOI] [PubMed] [Google Scholar]
- Dowd Jennifer Beam and Zajacova Anna. 2007. “Does the Predictive Power of Self-rated Health for Subsequent Mortality Risk Vary by Socioeconomic Status in the US?” International Journal of Epidemiology 36:1214–21. [DOI] [PubMed] [Google Scholar]
- Dupre Matthew E., Beck Audrey N., and Meadows Sarah O.. 2009. “Marital Trajectories and Mortality among US Adults.” American Journal of Epidemiology 170:546–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox John. 2008. Applied Regression Analysis and Generalized Linear Models. Thousand Oaks, CA: Sage. [Google Scholar]
- Franks Peter, Gold Marthe E., and Fiscella Kevin. 2003. “Sociodemographics, Self-rated Health, and Mortality in the US.” Social Science & Medicine 56:2505–14. [DOI] [PubMed] [Google Scholar]
- Gindin Jacob, Walter-Ginzburg Adrian, Geitzen Moshe, Epstein Shulamit, Levi Shmuel, Landi Francisco, and Bernabei Roberto. 2007. “Predictors of Rehabilitation Outcomes: A Comparison of Israeli and Italian Geriatric Post-acute Care (PAC) Facilities Using the Minimum Data Set (MDS).” Journal of the American Medical Directors Association 8:233–42. [DOI] [PubMed] [Google Scholar]
- Goebeler Sirkka, Jylha Marja, and Hervonen Antti. 2007. “Self-reported Medical History and Self-rated Health at Age 90. Agreement with Medical Records.” Aging Clinical and Experimental Research 19:213–19. [DOI] [PubMed] [Google Scholar]
- Goodwin James S., Hunt William C., Key Charles R., and Samet Jonathan M.. 1987. “The Effect of Marital Status on Stage, Treatment, and Survival of Cancer Patients “ JAMA—Journal of the American Medical Association 258:3125–30. [PubMed] [Google Scholar]
- Green BH, Copeland JRM, Dewey ME, Sharma V, and Davidson IA. 1994. “Factors Associated with Recovery and Recurrence of Depression in Older People: A Prospective Study.” International Journal of Geriatric Psychiatry 9:789–95. [Google Scholar]
- Grundy Emily and Glaser Karen. 2000. “Sociodemographic Differences in the Onset and Progression of Disability in Early Old Age: A Longitudinal Study.” Age and Ageing 29:149–57. [DOI] [PubMed] [Google Scholar]
- Hays Judith C., Schoenfeld David, Blazer Dan G., and Gold Deborah T.. 1996. “Global Self-ratings of Health and Mortality: Hazard in the North Carolina Piedmont.” Journal of Clinical Epidemiology 49:969–79. [DOI] [PubMed] [Google Scholar]
- Hu Yuanreng and Goldman Noreen. 1990. “Mortality Differentials by Marital Status: An International Comparison.” Demography 27:233–50. [PubMed] [Google Scholar]
- Idler Ellen L. and Angel Ronald J.. 1990. “Self-rated Health and Mortality in the NHANES-I Epidemiologic Follow-up Study.” American Journal of Public Health 80:446–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler Ellen L. and Benyamini Yael. 1997. “Self-rated Health and Mortality: A Review of Twenty-seven Community Studies.” Journal of Health and Social Behavior 38:21–37. [PubMed] [Google Scholar]
- Idler Ellen L., Hudson Shawna V., and Leventhal Howard. 1999. “The Meanings of Self-ratings of Health.” Research on 21:458–76. [Google Scholar]
- Johnson Norman J., Backlund Eric, Sorlie Paul D., and Loveless Catherine A.. 2000. “Marital Status and Mortality: The National Longitudinal Mortality Study” Annals of Epidemiology 10:224–38. [DOI] [PubMed] [Google Scholar]
- Jylha Marja, Volpato Stefano, and Guralnik Jack M.. 2006. “Self-rated Health Showed a Graded Association with Frequently Used Biomarkers in a Large Population Sample.” Journal of Clinical Epidemiology 59:465–71. [DOI] [PubMed] [Google Scholar]
- Kawada Tomoyuki, Suzuki Shosuke, Tsukioka Tokio, and Iesaki Satoru. 2006. “Factors Associated with Perceived Health of Very Old Inhabitants of Japan.” Gerontology 52:258–63. [DOI] [PubMed] [Google Scholar]
- Kennedy Byron S., Kasl Stanislav V., and Vaccarino Viloa. 2001. “Repeated Hospitalizations and Self-rated Health among the Elderly: A Multivariate Failure Time Analysis.” American Journal of Epidemiology 153:232–41. [DOI] [PubMed] [Google Scholar]
- Krause Neal M. and Jay Gina M.. 1994. “What Do Global Self-rated Health Items Measure?” Medical Care 32:930–42. [DOI] [PubMed] [Google Scholar]
- Lee Sei J., Moody-Ayers Sandra Y., Landefeld C. Seth, Walter Louise C., Lindquist Karla, Segal Mark R., and Covinsky Kenneth E.. 2007. “The Relationship between Self-rated Health and Mortality in Older Black and White Americans.” Journal of the American Geriatrics Society 55:1624–29. [DOI] [PubMed] [Google Scholar]
- Lindeboom Maarten and van Doorslaer Eddy. 2004. “Cut-point Shift and Index Shift in Self-reported Health.” Journal of Health Economics 23:1083–99. [DOI] [PubMed] [Google Scholar]
- Lindstrom Martin. 2009. “Marital Status, Social Capital, Material Conditions and Self-rated Health: A Population-based Study.” Health Policy 93:172–79. [DOI] [PubMed] [Google Scholar]
- Liu Hui. 2009. “Till Death Do Us Part: Marital Status and US Mortality Trends, 1986–2000.” Journal of Marriage and the Family 71:1158–73. [Google Scholar]
- Liu Hui and Umberson Debra. 2008. “The Times They Are a Changin’: Marital Status and Health Differentials from 1972 to 2003.” Journal of Health and Social Behavior 49:239–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyyra Tiina-Mari, Heikkinen Eino, Lyyra Anna-Liisa, and Jylha Marja. 2006. “Self-rated Health and Mortality: Could Clinical and Performance-based Measures of Health and Functioning Explain the Association?” Archives of Gerontology and Geriatrics 42:277–88. [DOI] [PubMed] [Google Scholar]
- Lyyra Tiina-Mari, Leskinen Esko, Jylha Marja, and Heikkinen Eino. 2009. “Self-rated Health and Mortality in Older Men and Women: A Time-dependent Covariate Analysis.” Archives of Gerontology and Geriatrics 48:14–18. [DOI] [PubMed] [Google Scholar]
- MacWilliam Cynthia H., Yood Marianne U., Vemer James J., McCarthy Bruce D., and Ward Richard E.. 1996. “Patient-related Risk Factors That Predict Poor Outcome after Total Hip Replacement.” Health Services Research 31:623–3 8. [PMC free article] [PubMed] [Google Scholar]
- Manzoli Lamberto, Villari Paolo, Pirone Giovanni M., and Boccia Antonio. 2007. “Marital Status and Mortality in the Elderly: A Systematic Review and Meta-analysis.” Social Science & Medicine 64:77–94. [DOI] [PubMed] [Google Scholar]
- Melzer David, Lan Tzuo-Yun, Tom Brian D. M., Deeg Dorly J. H., and Guralnik Jack M.. 2004. “Variation in Thresholds for Reporting Mobility Disability between National Population Subgroups and Studies.” Journal of Gerontology: Medical Sciences 59:1295–1303. [DOI] [PubMed] [Google Scholar]
- Minh Hoang V., Byass Peter, and Wall Stig. 2010. “Multilevel Analysis of Effects of Individual Characteristics and Household Factors on Self-rated Health among Older Adults in Rural Vietnam.” Geriatrics & Gerontology International 10:209–15. [DOI] [PubMed] [Google Scholar]
- Okamoto Kazushi, Momose Yumiko, Fujino Ayumi, and Osawa Yukari. 2008. “Gender Differences in the Relationship between Self-rated Health (SRH) and 6-year Mortality Risks among the Elderly in Japan.” Archives of Gerontology and Geriatrics 47:311–17. [DOI] [PubMed] [Google Scholar]
- Regidor Enrique, Guallar-Castillon Pilar, Gutierrez-Fisac Juan L., Banegas José R., and Rodriguez-Artalejo Fernando. 2010. “Socioeconomic Variation in the Magnitude of the Association between Self-rated Health and Mortality.” Annals of Epidemiology 20:395–400. [DOI] [PubMed] [Google Scholar]
- Rohrer James E., Bernard Matthew E., Zhang Yan, Rasmussen Norman H., and Woroncow Halina. 2008. “Marital Status, Feeling Depressed and Self-rated Health in Rural Female Primary Care Patients.” Journal of Evaluation in Clinical Practice 14:214–17. [DOI] [PubMed] [Google Scholar]
- Rohrer James E., Herman David C., Merry Stephen P., Naessens James M., and Houston Margaret S.. 2009. “Validity of Overall Self-rated Health as an Outcome Measure in Small Samples: A Pilot Study Involving a Case Series.” Journal of Evaluation in Clinical Practice 15:366–69. [DOI] [PubMed] [Google Scholar]
- Schwerdtfeger Andreas and Friedrich-Mai Peter. 2009. “Social Interaction Moderates the Relationship between Depressive Mood and Heart Rate Variability: Evidence from an Ambulatory Monitoring Study.” Health Psychology 28:501–509. [DOI] [PubMed] [Google Scholar]
- Spiers Nicola, Jagger Carol, Clarke Michael, and Arthur Antony. 2003. “Are Gender Differences in the Relationship between Self-rated Health and Mortality Enduring? Results from Three Birth Cohorts in Melton Mowbray, United Kingdom.” Gerontologist 43:406–11. [DOI] [PubMed] [Google Scholar]
- Strawbridge William J. and Wallhagen Margaret I.. 1999. “Self-rated Health and Mortality over Three Decades: Results from a Time-dependent Covariate Analysis.” Research on Aging 21:402. [Google Scholar]
- Thong Melissa, S. Y., Kaptein Adrian A., Benyamini Yael, Krediet Raymond T., Boeschoten Elizabeth W., and Dekker Friedo W.. 2008. “Association between a Self-rated Health Question and Mortality in Young and Old Dialysis Patients: A Cohort Study.” American Journal of Kidney Diseases 52:111–17. [DOI] [PubMed] [Google Scholar]
- Umberson Debra. 1992. “Gender, Marital Status and the Social Control of Health Behavior.” Social Science & Medicine 34:907–17. [DOI] [PubMed] [Google Scholar]
- Waite Linda J. 1995. “Does Marriage Matter?” Demography 32:483–507. [PubMed] [Google Scholar]
- Walker Jennifer D., Maxwell Colleen J., Hogan David B., and Ebly Erika M.. 2004. “Does Self-rated Health Predict Survival in Older Persons with Cognitive Impairment?” Journal of the American Geriatrics Society 52:1895–1900. [DOI] [PubMed] [Google Scholar]
- Whitson Heather E., Thielke Stephen, Diehr Paula, O’Hare Ann M., Chaves Paulo H. M., Zakai Neil A., Arnold Alice, Chaudhry Sarwat, Ives Diane, and Newman Anne B.. 2011. “Patterns and Predictors of Recovery from Exhaustion in Older Adults: The Cardiovascular Health Study.” Journal of the American Geriatrics Society 59:207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox Victoria L., Kasl Stanislav V., and Idler Ellen L.. 1996. “Self-rated Health and Physical Disability in Elderly Survivors of a Major Medical Event.” Journals of Gerontology Series B: Psychological Sciences and Social Sciences 51:S96–S104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.