We read with interest the manuscript entitled “BMPR2 mutations and response to inhaled or parenteral prostanoids: a case series” published in by Scelsi et al. 1 in a recent issue of Pulmonary Circulation. The authors reported a small series of 13 patients (6 with idiopathic or anorexigen‐induced PAH and 7 with heritable PAH due to BMPR2 mutation) in whom treatment escalation consisted in adding an inhaled or a parenteral prostacyclin. It was intriguing that BMPR2 negative patients achieved a greater hemodynamic improvement than BMPR2 positive patients (−10.1 vs. −2.4 WU), more than 1 year after initiation of prostacyclin.
On the basis of these findings, we analyzed from the French referral Pulmonary Hypertension center database the effects of treatment escalation with a parenteral prostacyclin in all idiopathic, heritable, and anorexigen‐induced PAH patients receiving a background oral combination therapy with an endothelin‐receptor antagonist and a phosphodiesterase type‐5 inhibitor. We identified 24 patients between 2007 and 2020. All were sequenced for BMPR2 mutations and other predisposing PAH genes. 2 There were 15 idiopathic PAH, 2 anorexigen‐induced PAH and 7 heritable PAH due to BMPR2 mutations. Intravenous epoprostenol was initiated in 7 BMPR2 positive and 6 BMPR2 negative patients, and subcutaneous treprostinil was initiated in the remaining 11 nonheritable PAH patients. The first hemodynamic reassessment was performed 6 ± 3 months after initiation of prostacyclin. Cardiopulmonary haemodynamics improved after prostacyclin initiation in almost all patients (Figure 1). Pulmonary vascular resistance decreased from 13.4 ± 5.5 to 8.9 ± 3.8 WU (p = 0.02), in the same proportion than previously described. 3 There was no significant difference according to BMPR2 status with a decrease by 5.9 WU (interquartile range: 4.5–9.0) and 3.1 WU (1.2–6.7) in BMPR2 positive and BMPR2 negative patients, respectively (p = 0.21). In addition, after prostacyclin initiation all patients carrying a BMPR2 mutation achieved a low‐risk status according to COMPERA methodology. 4
Figure 1.
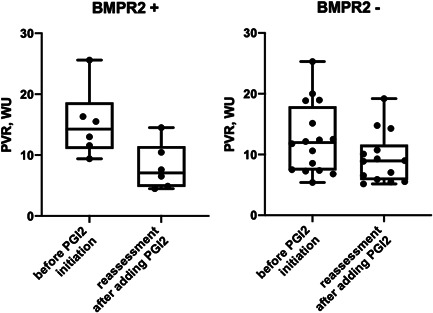
Plots of pulmonary vascular resistance before and after addition of parenteral prostacyclin (PGI2) in BMPR2 mutations carriers and non BMPR2 mutations carriers receiving background oral combination therapy
Our results in a larger series of idiopathic and heritable PAH do not validate the conclusions of a lower response to prostanoids in PAH patients carrying a BMPR2 mutation as suggested by Scelsi et al. 1 In an international meta‐analysis of 1550 PAH patients, Evans et al. reported that PAH patients carrying a BMPR2 mutation present at a younger age with more severe disease, and are at increased risk of death or transplantation, compared with those without BMPR2 mutations. 5 However, a recent study on long‐term outcomes of PAH according to initial treatment strategy has shown that patients initiated with triple combination therapy including parenteral prostacyclin had an excellent long‐term survival (86% at 10 years) despite their clinical and hemodynamic severity. 6 Among the 76 patients initiated with triple combination therapy, 48 had heritable PAH. 6 One can suggest that an ambitious therapeutic approach may counterbalance the natural history of heritable PAH and that these patients respond favorably to combination therapy including parenteral prostanoids.
In this cohort, BMPR2 mutations carriers, in whom a treatment escalation was performed by adding a parenteral prostacyclin, all achieved a low‐risk status and improved their hemodynamics. These results suggest that BMPR2 status should not be considered as a prognostic factor of poor response to prostanoids.
REFERENCES
- 1. Scelsi L, Greco A, Acquaro M, Olivieri C, Sobrero M, Turco A, Cappelletti D, Visconti LO, & Ghio S. BMPR2 mutations and response to inhaled or parenteral prostanoids: a case series. Pulm Circ. 2021;11:20458940211037276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Girerd B, Montani D, Jaïs X, Eyries M, Yaici A, Sztrymf B, Savale L, Parent F, Coulet F, Godinas L, Lau EM, Tamura Y, Sitbon O, Soubrier F, Simonneau G, & Humbert M. Genetic counselling in a national referral centre for pulmonary hypertension. Eur Respir J. 2016;47:541–52. [DOI] [PubMed] [Google Scholar]
- 3. Bergot E, Sitbon O, Cottin V, Prévot G, Canuet M, Bourdin A, de Groote P, Rottat L, Gressin V, Jaïs X, Humbert M, & Simonneau G. Current epoprostenol use in patients with severe idiopathic, heritable or anorexigen‐associated pulmonary arterial hypertension: data from the French pulmonary hypertension registry. Int J Cardiol. 2014;172:561–7. [DOI] [PubMed] [Google Scholar]
- 4. Hoeper MM, Kramer T, Pan Z, Eichstaedt CA, Spiesshoefer J, Benjamin N, Olsson KM, Meyer K, Vizza CD, Vonk‐Noordegraaf A, Distler O, Opitz C, Gibbs JSR, Delcroix M, Ghofrani HA, Huscher D, Pittrow D, Rosenkranz S, & Grünig E. Mortality in pulmonary arterial hypertension: prediction by the 2015 European pulmonary hypertension guidelines risk stratification model. Eur Respir J. 2017;50:1700740. [DOI] [PubMed] [Google Scholar]
- 5. Evans JDW, Girerd B, Montani D, Wang XJ, Galiè N, Austin ED, Elliott G, Asano K, Grünig E, Yan Y, Jing ZC, Manes A, Palazzini M, Wheeler LA, Nakayama I, Satoh T, Eichstaedt C, Hinderhofer K, Wolf M, Rosenzweig EB, Chung WK, Soubrier F, Simonneau G, Sitbon O, Gräf S, Kaptoge S, Angelantonio ED, Humbert M, & Morrell NW. BMPR2 mutations and survival in pulmonary arterial hypertension: an individual participant data meta‐analysis. Lancet Respir Med. 2016;4:129–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Boucly A, Savale L, Jaïs X, Bauer F, Bergot E, Bertoletti L, Beurnier A, Bourdin A, Bouvaist H, Bulifon S, Chabanne C, Chaouat A, Cottin V, Dauphin C, Degano B, Groote P, Favrolt N, Feng Y, Horeau‐Langlard D, Jevnikar M, Jutant EM, Liang Z, Magro P, Mauran P, Mornex JF, Palat S, Parent F, Picard F, Pichon J, Poubeau P, Prévot G, Renard S, Reynaud‐Gaubert M, Riou M, Roblot P, Sanchez O, Seferian A, Tromeur C, Weatherald J, Simonneau G, Montani D, Humbert M, & Sitbon O. Association between initial treatment strategy and long‐term survival in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2021;204:842–54. [DOI] [PubMed] [Google Scholar]


