Short abstract
Content available: Author Interview and Author Audio Recording
Abbreviations
- HU
Hounsfield unit
- COVID‐19
coronavirus disease 2019
- ESLD
end‐stage liver disease
- LT
liver transplant
- LTE
liver transplant evaluation
- MD
medical doctor
Watch the interview with the author.
Listen to an audio presentation of this article.
Telemedicine refers to the remote delivery of patient care using information technologies. It has previously been applied in diverse ways in hepatology, including treatment of chronic hepatitis C in rural areas 1 and virtual tumor boards, 2 but it is only now beginning to penetrate the space of the liver transplant (LT) evaluation (LTE). The successful use of such “tele‐evaluations” in patients with end‐stage liver disease (ESLD) requires not only an understanding of the logistics and benefits of implementation but also an anticipation of the potential pitfalls and obstacles that may lie ahead.
LT “Tele‐Evaluations”: What, Why, and How?
What modalities can be used to conduct transplant “tele‐evaluations”? Providers may gather and review electronic records asynchronously to triage patients prior to in‐person evaluations. In a recent study at the Richmond Veterans Affairs medical center, investigators conducted initial tele‐reviews of data from patients referred for LTE to determine eligibility. The process led to significant reductions in future in‐person evaluations that resulted in denial, as well as 85% and 74% reductions in time from referral to initial evaluation and time to listing, respectively. 3 , 4 Tele‐evaluations can also occur directly with the patient through phone or video visits. In a recent pilot study conducted at the University of Pennsylvania, hepatologists connected with a community‐based gastroenterology practice to perform video‐based tele‐visits with patients referred for management of ESLD. 5 Patients were located in a clinic room at the community practice for the tele‐visit. Of 57 total visits, 18% of patients were referred for LTE, and two ultimately were placed on the wait list. Importantly, patient and provider satisfaction were high.
Why might patients benefit from access to tele‐evaluations? According to the Scientific Registry of Transplant Recipients, 13 states in the United States do not have an LT center. Increasing distance from an LT center is associated with lower access to wait‐list placement and receipt of LT and increased mortality. 6 Of wait‐listed patients, almost one‐fourth live more than 100 miles from the closest LT center. 7 Imagine the stress experienced by patients and families—already burdened by encephalopathy, polypharmacy, hospitalizations, and readmissions—when traveling long distances for an in‐person LTE that may simply result in more appointments and tests or, worse, in denial for LT. Tele‐evaluations offer the tremendous opportunities of increasing access, identifying in advance major barriers to transplant, and streamlining necessary testing—all with the hopes of improving care delivery and reducing patient stress.
How can tele‐evaluations be implemented successfully? The ongoing coronavirus disease 2019 (COVID‐19) pandemic has been instructive regarding the uptake of telemedicine in all disciplines, including hepatology. A survey of liver and intestinal transplant programs showed that telemedicine use increased from 16% at baseline to 98% one month into the pandemic, with 65% of the programs conducting tele‐evaluations. 8 The earlier‐referenced University of Pennsylvania study illustrates the importance of a well‐designed workflow with stakeholder involvement, using Health Insurance Portability and Accountability Act–compliant technology and ensuring full access to necessary records. A sample workflow is demonstrated in Fig. 1. Patient and provider satisfaction are also paramount. A single‐center survey of gastroenterology practices during the COVID‐19 pandemic showed overall patient and provider satisfaction (78% of patients were somewhat/very satisfied with the overall quality of their telemedicine experience, and 80% reported probable/definite future use). 9 However, older patients were less likely to have high ratings, and Black patients were less likely to report anticipated future telemedicine use.
FIG 1.
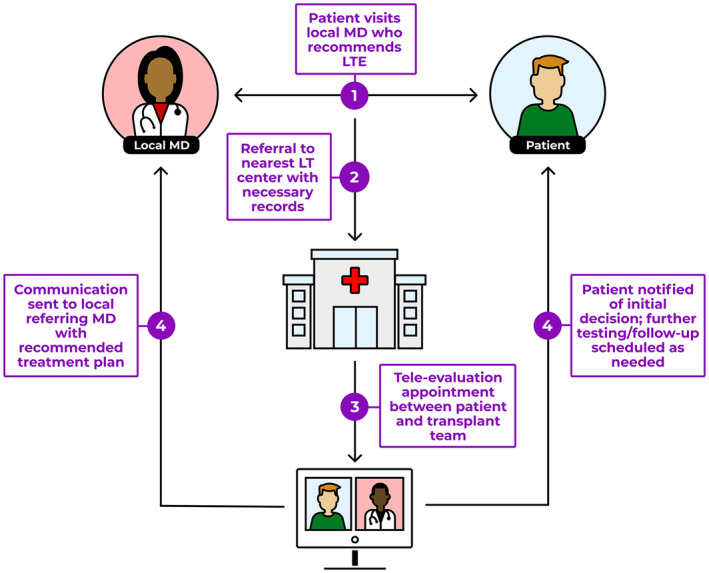
Theoretical workflow for telemedicine LTE.
Pitfalls and Anticipated Obstacles
The benefits notwithstanding, any new process and technology will have barriers and unforeseen consequences. A comprehensive LTE requires a vast multidisciplinary team with multiple different assessments of patient health. A tele‐evaluation can reasonably assess many crucial components of the evaluation, including medical comorbidities (cardiac disease, malignancy, etc.), surgical anatomy, or substance abuse issues, many of which are common reasons for denial. 10 However, other crucial components may prove more difficult.
Frailty is a strong predictor of post‐LT outcomes and has increasingly become a cornerstone of LTE through objective measurements, such as the Liver Frailty Index. Patients typically undergo an initial assessment followed by serial measurements over time to assess for decline or improvement. Out of necessity, a tele‐evaluation may prioritize other aspects of the evaluation and postpone the frailty test for a later in‐person visit. Will such a delay waste precious time for frail patients who may have benefited from an earlier assessment and referral for physical therapy? Here, we can learn from the kidney transplant literature, where attempts are being made to validate tools for remote frailty assessments (e.g., the self‐reported physical functioning subscale score [Short Form 36 (SF‐36)]). 11
How will the transplant team reliably evaluate and verify social support? On the one hand, an at‐home video visit may afford the transplant team the opportunity to “meet” more family members and even to gain a glimpse into the patient’s home environment. On the other hand, whether the “video presence” of a caregiver will translate to an ability to travel with patients for tests or emergencies is yet unknown. Observations of physical and emotional interactions between patients and their caregivers are crucial to the assessment of support and can be diminished or lost completely through video or phone visits.
Finally, what will be the lasting impact of remote tele‐evaluations on patients and families, especially when the result is a denial for transplant? The discussion surrounding liver transplantation is already wrought with ethical and emotional complexity. Will a digital video experience detract from our ability to hold difficult conversations in a respectful and empathic manner? It is encouraging that qualitative literature in palliative care, where difficult conversations are the norm, suggests that patients report positive perceptions of telemedicine as it pertains to the doctor–patient relationship, user experience, and comfort and safety. 12
There are other obstacles to consider, including payor reimbursement strategies and regulatory barriers. Further, telehealth can have significant impacts, both positive and negative, on existing disparities within liver transplantation. On the surface, tele‐evaluations should reduce inequity to access, but the story is much more complex and requires a more granular analysis that is outside the scope of this discussion.
Conclusion
There are clear benefits of a process for tele‐evaluations in liver transplantation (Table 1). We can improve overall access to LT, create more geographical parity, reduce costs and stress for patients, and increase awareness and education among nontransplant clinicians. Certainly, all new systems and technologies have downsides. However, rather than being a deterrent, the potential for such consequences should motivate the transplant community to engage in both careful planning and meticulous ongoing reassessment to maximize the benefits while minimizing the risks.
TABLE 1.
Benefits and Pitfalls of Tele‐evaluations
| Benefits | Pitfalls |
|---|---|
| Reduced costs to patients (travel, time lost from work, parking, etc.) | Lack of validated remote assessments of physical frailty |
| Ease of access to LT for patients with geographic barriers | Difficulty in evaluating reliability of social support network for travel to appointments |
| Reduction in time between initial referral and subsequent evaluation | Alienating patients with low health and digital literacy or rural populations with limited Internet access |
| Enhanced relationship between transplant centers and community physicians | Harder to establish rapport and hold difficult conversations via video |
| Unique glimpse into patient’s home situation may uncover social issues (or strengths) |
Potential conflict of interest: L.K. is on the speaker’s bureau of Gilead, Target Hcc, and PeerView CME. She is on the speakers’ bureau of and advises Eisai. She advises and consults for Exelixis. She consults for Bayer and Merck.
References
- 1. Arora S, Kalishman S, Thornton K, et al. Expanding access to HCV treatment – Extension for Community Health Outcomes (ECHO) Project: disruptive innovation in specialty care. Hepatology 2010;52:1124‐1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Salami AC, Barden GM, Castillo DL, et al. Establishment of a regional virtual tumor board program to improve the process of care for patients with hepatocellular carcinoma. J Oncol Pract 2015;11:e66‐e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Konjeti VR, Heuman D, Bajaj JS, et al. Telehealth‐based evaluation identifies patients who are not candidates for liver transplantation. Clin Gastroenterol Hepatol 2019;17:207‐209. [DOI] [PubMed] [Google Scholar]
- 4. John BV, Love E, Dahman B, et al. Use of telehealth expedites evaluation and listing of patients referred for liver transplantation. Clin Gastroenterol Hepatol 2020;18:1822‐1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Serper M, Cubell AW, Deleener ME, et al. Telemedicine in liver disease and beyond: can the COVID‐19 crisis lead to action? Hepatology 2020;72:723‐728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goldberg DS, French B, Forde KA, et al. Association of distance from a transplant center with access to waitlist placement, receipt of liver transplantation, and survival among US veterans. JAMA 2014;311:1234‐1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ross K, Patzer RE, Goldberg DS, et al. Sociodemographic determinants of waitlist and posttransplant survival among end‐stage liver disease patients. Am J Transplant 2017;17:2879‐2889. [DOI] [PubMed] [Google Scholar]
- 8. Sherman CB, Said A, Kriss M, et al. In‐person outreach and telemedicine in liver and intestinal transplant: a survey of national practices, impact of COVID‐19 and areas of opportunity. Liver Transpl 2020;26:1354‐1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Serper M, Nunes F, Ahmad N, et al. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID‐19 pandemic. Gastroenterology 2020;159:1589‐1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Poonja Z, Brisebois A, van Zanten SV, et al. Patients with cirrhosis and denied liver transplants rarely receive adequate palliative care or appropriate management. Clin Gastroenterol Hepatol 2014;12:692‐698. [DOI] [PubMed] [Google Scholar]
- 11. Watford DJ, Cheng XS, Han J, et al. Toward telemedicine‐compatible physical functioning assessments in kidney transplant candidates. Clin Transplant 2020;35:e14173 [online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tasneem S, Kim A, Bagheri A, et al. Telemedicine video visits for patients receiving palliative care: a qualitative study. Am J Hosp Palliat Care 2019;36:789‐794. [DOI] [PubMed] [Google Scholar]


