The 2008 Ryan Haight Act generally requires an in-person medical evaluation before the prescribing of medications such as buprenorphine for opioid use disorder (MOUD).1,2 Early in the COVID-19 pandemic (March 2020), the requirement was temporarily waived3 and there was a sharp increase in MOUD inductions via telemedicine.4
To inform debate about whether this waiver should be permanent, we identified characteristics of patients and clinicians associated with receiving a telemedicine (vs. in-person) induction during the pandemic.
METHODS
Using 2020 Medicare fee-for-service claims, we used methods describe elsewhere4 to identify buprenorphine inductions from January 2020 through May 2021. Patients could have multiple inductions if there was a >90-day gap between buprenorphine treatment.
We used multivariable logistic regression to identify patient and clinician characteristics associated with telemedicine buprenorphine inductions during the pandemic (March 13, 2020, through May 2021), adjusting for clustering (i.e., same clinician inducting different patients; and same patient with multiple inductions during the pandemic).
We characterized patients by race/ethnicity, sex, age, reason for Medicare enrollment, Census region, dual enrollment in Medicaid, and rural/urban designation. Using the Physician Compare National File, we characterized clinicians based on specialty, years of experience, sex, and number of clinicians in the practice. Specialty was grouped based on specialty taxonomy codes: primary care physician, psychiatrist, anesthesiologist, primary care nurse practitioner, physician assistants and non-primary care nurse practitioner, other non-physician clinician, and other physician.
Statistical analyses were performed in SAS, version 9.4. The Harvard Medical School Institutional Review Board exempted this study from review.
RESULTS
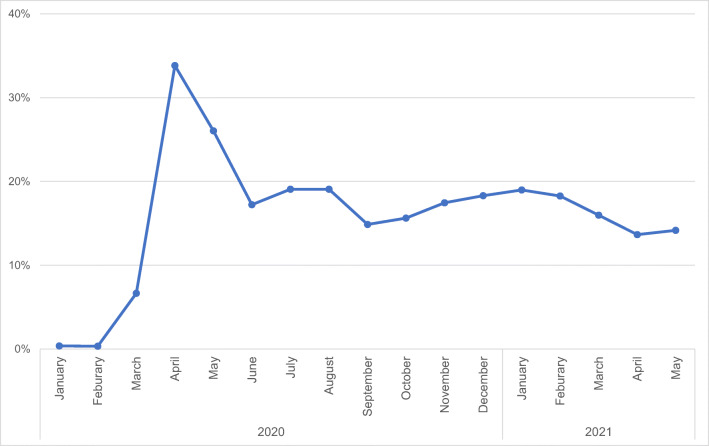
Among the 22,569 inductions between March 13, 2020, and May 30, 2021, 3,212 (14.7%) were via telemedicine. The monthly rate of telemedicine inductions peaked at 33.8% in April 2020 before dropping to 14.2% by May 2021 (Fig. 1).
Figure 1.
Trends in the proportion of buprenorphine inductions conducted via telemedicine among Medicare fee-for-service beneficiaries (January 2020 through May 2021). The denominator is the total number of buprenorphine inductions in a given month. Numerator is the number of buprenorphine inductions delivered via telemedicine. During the COVID-19 pandemic (March 13, 2020, through May 2021), we identified 22,569 inductions, 3,212 (14.7%) of which occurred via telemedicine.
Compared to White, urban, and higher-income beneficiaries, Black (aOR 0.83; 95% CI, 0.72, 0.96), rural (aOR 0.79; 95% CI, 0.72, 0.86), and dual eligible (aOR 0.86; 95% CI, 0.79, 0.94) beneficiaries were less likely to receive a buprenorphine induction via telemedicine (Table 1).
Table 1.
Logistic Regression of Association Between Buprenorphine Inductions Delivered via Telemedicine and Patient/Clinician Characteristics (March 13, 2020, Through May 2021). Analysis adjusts for patient- and provider-level clustering
| No. of inductions (%) | Adjusted odds ratio of having a telemedicine induction (95% CI) | ||||
|---|---|---|---|---|---|
| Telemedicine (n=3,312) |
In-person (n=19,257) |
||||
| Patient characteristics | Race/ethnicity | White | 2676 (81) | 15445 (80) | Reference |
| Black | 262 (8) | 1885 (10) | 0.83 (0.72, 0.96) | ||
| Other | 286 (9) | 1576 (8) | 0.99 (0.86, 1.14) | ||
| Unknown | 88 (3) | 351 (2) | 1.34 (1.04, 1.71) | ||
| Patient sex | Male | 1669 (50) | 9808 (51) | Reference | |
| Female | 1643 (50) | 9449 (49) | 1.03 (0.95, 1.11) | ||
| Reason for Medicare enrollment | Old age | 721 (22) | 4042 (21) | Reference | |
| Disabled, ESRD, or both | 2591 (78) | 15215 (79) | 1.04 (0.91, 1.20) | ||
| Age | <65 | 2208 (67) | 13050 (68) | Reference | |
| 65–74 | 888 (27) | 4944 (26) | 1.06 (0.94, 1.21) | ||
| 75+ | 216 (7) | 1263 (7) | 1.02 (0.83, 1.24) | ||
| Rurality^ | Urban | 2460 (74) | 13078 (68) | Reference | |
| Rural | 852 (26) | 6179 (32) | 0.79 (0.72, 0.86) | ||
| Dual | No | 1226 (37) | 6635 (34) | Reference | |
| Yes | 2086 (63) | 12622 (66) | 0.86 (0.79, 0.94) | ||
| Region | Northeast | 923 (28) | 4102 (21) | Reference | |
| Midwest | 584 (18) | 3680 (19) | 0.74 (0.66, 0.84) | ||
| West | 858 (26) | 4219 (22) | 0.96 (0.87, 1.07) | ||
| South Atlantic | 947 (29) | 7255 (38) | 0.64 (0.57, 0.71) | ||
| Clinician characteristics | Clinician sex | Male | 1988 (60) | 12217 (64) | Reference |
| Female | 1322 (39) | 6998 (36) | 1.17 (1.07, 1.29) | ||
| Specialty | Primary care physician** | 1024 (31) | 7407 (39) | Reference | |
| Psychiatrist | 490 (15) | 1573 (8) | 2.01 (1.77, 2.29) | ||
| Anesthesiologist | 308 (9) | 1995 (10) | 0.93 (0.80, 1.08) | ||
| NP (primary care specialty***) | 518 (16) | 2992 (16) | 1.08 (0.95, 1.23) | ||
| Non-physician clinician (other) | 301 (9) | 1713 (9) | 1.11 (0.95, 1.30) | ||
| Physician (other) | 347 (11) | 1997 (10) | 1.20 (1.05, 1.38) | ||
| PA/NP (non-primary care specialty) | 322 (10) | 1578 (8) | 1.18 (1.02, 1.36) | ||
| Years of experience | 0–19 | 1467 (47) | 8471 (46) | Reference | |
| 20–30 | 689 (22) | 4415 (24) | 1.02 (0.92, 1.15) | ||
| 31–40 | 628 (20) | 3778 (20) | 1.09 (0.97, 1.23) | ||
| ≥ 41 | 369 (12) | 1895 (10) | 1.19 (1.01, 1.35) | ||
| Practice size | Solo practitioner | 582 (18) | 4118 (22) | Reference | |
| Small (2–9) | 882 (28) | 5089 (27) | 1.36 (1.20, 1.55) | ||
| Medium (10–49) | 1282 (41) | 6618 (36) | 1.38 (1.22, 1.56) | ||
| Large (>50) | 410 (13) | 2742 (15) | 1.19 (1.02, 1.37) | ||
Abbreviations: NP, nurse practitioner; PA, physician assistant; ESRD, end stage renal disease
**Includes family medicine, internal medicine, and pediatrics
***Includes NPs with a specialty of family medicine, adult health, gerontology, and pediatrics
^Rural-urban communing area under the 4-category U.S. Census designation
Compared to solo practitioners, clinicians in larger practices were more likely to use telemedicine for induction (e.g., 10–49 physician practices vs. solo practitioners, aOR 1.38; 95% CI, 1.22, 1.56). Psychiatrists were more likely to use telemedicine for inductions than primary care physicians (aOR 2.01; 95% CI, 1.77, 2.29).
DISCUSSION
During the pandemic, 14.7% of buprenorphine inductions among Medicare beneficiaries were conducted via telemedicine. We found that telemedicine was less likely to be used among dual eligible for Medicaid, Black, and rural patients for buprenorphine induction. Telemedicine was more likely to be used among clinicians in larger practices as well as psychiatrists. Our findings are consistent with prior research among those with commercial insurance where 13.9% of buprenorphine inductions during the pandemic insured were conducted via telemedicine.4
Some disadvantaged populations are less likely to have a telemedicine induction. This finding supports concerns that barriers to using technology, such as lack of reliable cell phones, laptops, or internet service, prevent telemedicine use for disadvantaged populations (i.e., the “digital divide”) and may further increase existing disparities in care among disadvantaged groups. Similarly, solo practitioners or primary care providers may lack the resources required to set up the infrastructure to deliver OUD care via telemedicine. Psychiatrists may be more likely to use telemedicine for buprenorphine inductions given behavioral health providers use telemedicine at higher rates than other specialties.5 Policy interventions to address differences in telemedicine use across patients and providers include expanding community broadband availability, making available community programs to teach patients how to have a telemedicine visit, and financial supporting practices with upfront costs of starting telemedicine.
The Ryan Haight Act was established to prevent indiscriminate prescribing of controlled substances, during a time when prescribing absent an in-person examination was considered “outside the usual practice.”3 Our results highlight that using telemedicine for buprenorphine induction appears to be both acceptable and feasible for many clinicians. While existing evidence suggests that telemedicine may be a safe option for buprenorphine induction,6 there is a need for more research comparing patient outcomes with telemedicine vs. in-person buprenorphine inductions.
A key limitation is our findings may not be generalizable to commercially insured and Medicaid beneficiaries. Further, in the claims data we cannot characterize many patient and clinician factors that may underlie variation in the use of telemedicine.
Acknowledgements
We thank Rebecca Shyu for manuscript preparation efforts.
Funding
This project was supported by the Commonwealth Fund, National Institute on Drug Abuse (R01 DA04853303, P30 DA035772), and the National Institute of Mental Health (T32MH019733).
Declarations
Conflict of Interest
Authors have no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang L, Weiss J, Ryan EB, Waldman J, Rubin S, Griffin JL. Telemedicine increases access to buprenorphine initiation during the COVID-19 pandemic. J Subst Abuse Treat. 2021;124:108272. doi: 10.1016/j.jsat.2020.108272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warner Pushes for Release of Long-Delayed Telehealth Guidance to Expand Access to Medical Treatment. Mark R. Warner. Published May 3, 2021. Accessed October 10, 2021. https://www.warner.senate.gov/public/index.cfm/2021/5/warner-pushes-for-release-of-long-delayed-telehealth-guidance-to-expand-access-to-medical-treatment
- 3.COVID-19 Information Page. U.S. Department of Justice Drug Enforcement Administration. Accessed October 10, 2021. https://www.deadiversion.usdoj.gov/coronavirus.html
- 4.Barsky BA, Busch AB, Patel SY, Mehrotra A, Huskamp HA. Use of telemedicine for buprenorphine inductions in patients with commercial insurance or Medicare advantage. JAMA Netw Open. 2022;5(1):e2142531. doi: 10.1001/jamanetworkopen.2021.42531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Affairs. 2021;40(2):349–358. doi: 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huskamp HA, Riedel L, Uscher-Pines L, et al. Initiating opioid use disorder medication via telemedicine during COVID-19: implications for proposed reforms to the Ryan Haight Act. J Gen Intern Med. 2022;37(1):162–167. doi: 10.1007/s11606-021-07174-w. [DOI] [PMC free article] [PubMed] [Google Scholar]