Abstract
Study design
Exploratory clinical investigation.
Objectives
To assess the feasibility, acceptability, and preliminary efficacy of upper-body rowing exercise adapted to wheelchair users with spinal cord injury (SCI).
Setting
University exercise laboratory.
Methods
Eight individuals with SCI exercised on a rowing ergometer modified for wheelchair users (REMW), three times weekly, for up to 30 min per session. Participants completed feasibility and acceptability questionnaire (1–5 Likert scale), and the Wheelchair Users Shoulder Pain Index (WUSPI) before and after six weeks of exercise. Average power output (POAVG), distance rowed, percent peak heart rate (%HRpeak), and rating of perceived exertion (RPE) (6–20 scale) were monitored throughout the 18 exercise sessions and analyzed to evaluate preliminary efficacy of the exercise modality.
Results
All eight participants completed the study (97% adherence). Participants rated the exercise high on the feasibility and acceptability scale; median (interquartile range) = 5.0 (4.0–5.0), where higher numbers indicated greater feasibility. Shoulder pain was reduced by 21% yet not significantly different from baseline (p = 0.899). Physiological measures (%HRpeak = 80–83%; RPE = 15.0–16.0) indicated a high cardiovascular training load. From week 1 to week 6, POAVG and distance rowed increased by 37 and 36%, respectively (both p ≤ 0.001).
Conclusions
Data from six weeks of exercise on the REMW suggests that upper-body rowing is a feasible and acceptable exercise modality for wheelchair users with SCI. Session data on %HRpeak, RPE, and shoulder pain indicate that REMW evoked moderate to vigorous intensity exercise without exacerbation of shoulder pain. Future research is required to quantify potential training-induced changes in cardiorespiratory fitness.
Subject terms: Preventive medicine, Disability
Introduction
Recent exercise guidelines for improving cardiometabolic health in individuals with spinal cord injury (SCI) recommend at least three times of 30 min per week of moderate to vigorous intensity aerobic exercise [1]. In order to meet the recommended amount of aerobic exercise, individuals with SCI typically rely on exercise equipment that allows them to perform exercise using their upper-body due to either complete or partial loss of lower-body function. Upper-body aerobic exercise is typically restricted to a limited number of exercise modalities such as handcycling, wheelchair ergometry/propulsion or exercise using an arm crank ergometer (ACE) [2]. Unfortunately, adaptive equipment such as upper-body ergometers are not commonly available at community fitness centers [3]. Therefore, alternative exercise modalities and innovative ways to reach the recommended amount of aerobic exercise are needed.
Excessive demands placed on the musculoskeletal system of the upper-body result in high prevalence of shoulder pain in wheelchair users and their disengagement from physical activity [4, 5]. As wheelchair users rely on their upper limbs for daily function, shoulder pain must be prevented or limited to preserve function, physical independence and quality of life [6]. Repetitive motion, overuse, shoulder strength imbalances between anterior and posterior musculature and subsequent postural changes and impingement syndrome have been proposed to contribute to the development and exacerbation of shoulder pain [7, 8]. Traditional exercise modalities such as wheelchair propulsion/ergometry have shown to improve cardiorespiratory fitness [9] and some markers of cardiometabolic health [10]. However, wheelchair propulsion activities rely on repetitive, high force contractions of the anterior shoulder musculature, which increase the risk of developing pain and dysfunction of the shoulders [11]. Increasing evidence suggests that strength training of the posterior shoulder and scapular retractor musculature reduces or prevents shoulder pain [12].
Rowing is an exercise modality that involves both an aerobic and strength component for the posterior muscles [13]. For instance, muscle activation of the scapular retractors during traditional strength training is also evident during upper-body rowing [14]. Hybrid functional electrical stimulation (FES) rowing, where voluntary upper-body rowing is combined with FES of the lower limbs, are effective for improving cardiorespiratory fitness in individuals with SCI [15]. However, as FES is not readily available for individuals with SCI due to the costs and the specialized equipment required [16], it is relevant to examine if arms-only rowing can induce similar benefits, as this could more easily be incorporated into the individuals home or in community fitness centers. To our knowledge, only a few studies have explored the utility of isolated upper-body rowing (i.e. arms-only) in individuals with SCI. For instance, Solansky et al. [17] utilized arms-only rowing exercise where the seat on a standard rowing ergometer was fixed, necessitating the individual to transfer him or herself from the wheelchair to the ergometer. Other studies have modified existing cycle ergometers to rowing units [18–20]. Although innovative, none of these modified ergometers are commercially available and they have limited possibilities for adjusting resistance. Recently, Wong et al. [21] explored the usability of a custom made adaptive rowing machine and found that a single session of voluntary upper-body exercise performed on this ergometer was perceived as both enjoyable and effective aerobic exercise. However, this study did not assess exercise intensity by including measures such as heart rate or rating of perceived exertion (RPE) [21], rendering it difficult to quantify the actual training load of the adaptive rowing. With this explorative clinical investigation, we provide a detailed presentation of upper-body (i.e. arms-only) ergometer rowing exercise, and demonstrate how a commercially available rowing ergometer in combination with a single adaptive unit can be adapted to SCI wheelchair users with large variation in injury characteristics. Additionally, we present data on the feasibility and acceptability of the exercise modality, including the participants’ experiences of shoulder pain. Finally, as a secondary purpose, we present data demonstrating the preliminary efficacy in terms of the physiological (heart rate, power output) and psychophysiological (perceived exertion) training load elicited during six weeks (18 sessions) of exercise.
Methods
Study design and participants
In this study, data from six weeks of training from eight participants will be presented. Detailed description of participant characteristics can be seen in Table 1. The sample included both active and inactive participants at the time of enrollment. This study is a preliminary study of a larger randomized controlled trial (NCT04390087) [22]. Due to the national lockdown in relation to COVID19, we were forced to reduce the number of participants in the exercise group from the pre-specified n = 15 to n = 8, which resulted in a deviation from the trial registration. Briefly, participants were recruited through multiple channels related to disability- and SCI patient organizations. Men and woman aged 18–70 years, with a chronic SCI (≥1 year since injury), having sufficient sparing of arm flexor function to participate in upper-body rowing, and using a wheelchair for mobility were eligible for study participation.
Table 1.
Baseline demographic characteristics (N = 8).
| Participant | Sex | Age | Height (m) | Weight (kg) | BMI (kg/m2) | WC (cm) | TSI (yrs) | AIS grade | NLI | Etiology | V̇o2peak (ml/kg/min) | HRpeak (bpm) | RPEpeak | RERpeak |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | Male | 44 | 1.90 | 79.1 | 21.9 | 91.5 | 25 | B | C6 | Traumatic | 7.9 | 111 | 19 | 0.96 |
| P2 | Female | 57 | 1.50 | 89.5 | 39.8 | 129.5 | 47 | C | T12 | Unspecified | 12.2 | 144 | 15 | 1.02 |
| P3 | Male | 50 | 1.91 | 108.4 | 29.8 | 108.7 | 32 | A | T4 | Traumatic | 16.0 | 174 | 19 | 1.31 |
| P4 | Male | 51 | 1.89 | 89.8 | 25.1 | 103.8 | 34 | A | C7 | Traumatic | 10 | 95 | 14 | 0.97 |
| P5 | Female | 52 | 1.74 | 79.8 | 26.4 | 89.7 | 32 | C | L2 | Traumatic | 16.6 | 186 | 20 | 1.17 |
| P6 | Female | 51 | 1.64 | 65.3 | 24.3 | 83.7 | 51 | C | T12 | Spina bifida | 20.4 | 170 | 20 | 1.30 |
| P7 | Male | 48 | 1.76 | 88.4 | 28.5 | 124 | 19 | A | T10 | Traumatic | 14.7 | 140 | 19 | 1.44 |
| P8 | Male | 44 | 1.68 | 93.6 | 33.2 | 123.2 | 44 | C | L1 | Spina bifida | 22.9 | 149 | 19 | 1.13 |
| Mean (SD) | 49.6 (4.3) | 1.75 (0.14) | 86.7 (12.5) | 28.6 (5.7) | 106.7 (17.5) | 35.8 (11.4) | 15.1 (5.1) | 146 (31) | 18.1 (2.3) | 1.16 (0.18) |
BMI Body mass index, WC Waist circumference, TSI Time since injury, AIS grade American Spinal Injury Association Impairment Scale classification, NLI Neurological level of injury, V̇O2peak Peak oxygen consumption, HRpeak Heart rate peak, RPEpeak Peak rating of perceived exertion, RERpeak Peak respiratory exchange ratio.
Exercise prescription
Participants attended the laboratory for supervised exercise, three times per week, aiming for 30 min per session. Due to differences in functional capacity among the participants, we tailored the sessions to each participant’s physical capacity [23]. Thus, the target duration of 30 min could be met in several ways (e.g., shorter 5-min bouts, with 45 s–2.5 min of rest in between bouts, two to three 10–15 min bouts or 30 min continuous rowing). Some participants were not able to exercise for 30 min at the beginning of the training period. In those cases, the duration was progressively increased over time until attaining the targeted 30 min. As a general principle, the progression was made once weekly (i.e. every third session), by increasing the session duration with 5 min. When participants were able to row for 30 min, further progression was made by extending the duration of each bout (e.g., from 5 to 10 min), while reducing the number of bouts so that the total duration was maintained at 30 min. Exercise intensity was prescribed based on RPE. Participants were asked to exercise at an intensity ranging from 12 to 17 on the ‘Borg 6–20 RPE Scale’ [24]. To explore the cardiovascular load of upper-body rowing (by recording the highest heart rate attained), participants were encouraged to do minimum one session with maximal effort at the end of the session.
The exercise sessions were supervised by health professionals with knowledge about exercise considerations for SCI. Before each training session, participants were asked to empty their bladder, and a fan was positioned in front of the ergometer for comfortable cooling of the participants.
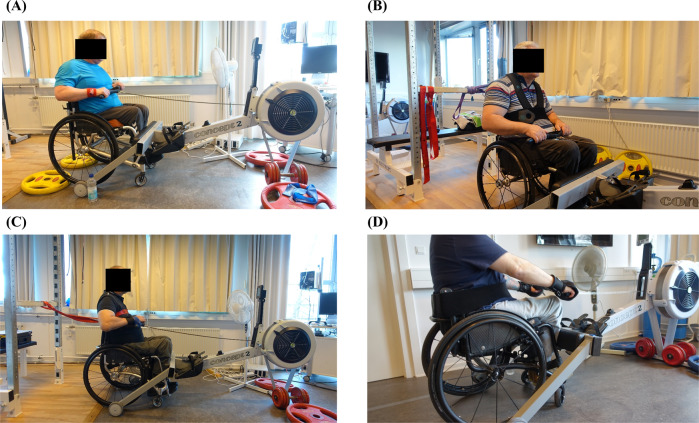
Ergometer rowing exercise
The exercise was performed on a commercially available rowing ergometer (Concept 2, Morrisville, Vermont, USA) modified for wheelchair users (REMW). We utilized an Adapt2row unit and adapted the ergometer to be used by wheelchair dependent individuals. The modification of the ergometer was made within seconds by separating it into two parts. Specifically, the seat and track of the ergometer (Concept 2, Model D or E) was detached and an Adapt2row unit was attached, allowing it to be used while sitting in a wheelchair (Fig. 1A). Some participants (P1, P3, P4, P7) in this study did not have sufficient trunk stability to resist the pull-back force of the handle required for maintaining seated during rowing. For these participants, we individually adapted the rowing exercise using supportive equipment for the trunk (see Supplementary Appendix 1 for detailed description). Three of the participants (P1, P4, P7) lacked sufficient grip strength (P1, P4 = SCI related, P7 = non-SCI related) to independently pull the handle of the ergometer. Consequently, these participants were equipped with either adaptive gloves (tetra gloves) or wrist straps with a hook (Supplementary Appendix 2).
Fig. 1. Ergometer rowing exercise adapted to wheelchair users with SCI.
A Participant performing upper-body rowing while sitting in his own wheelchair. B Participants with a lack of trunk stability performs upper-body rowing using a supportive vest and neoprene Velcro strap around the trunk and the wheelchair (C) or non-elastic chest belt. D Participant who lack some trunk stability and grip strength row with a neoprene Velcro strap and supportive gloves.
When seated in their own wheelchair, participants performed upper-body rowing exercise by repeatedly pulling the handle of the ergometer towards the ribcage. During the first sessions, careful attention was given to practice proper rowing technique [25]. For the recovery phase, participants were encouraged (if possible) to lean the upper-body slightly forward with the shoulders flexed and elbows extended. For the drive phase, emphasis was devoted to pulling the handle towards the lower ribs while maintaining the elbows close to the body and (if possible) extending the back slightly. During both phases, participants were instructed to keep the chest high, and specifically for the drive phase, to pull the shoulder blades together and keep the shoulders down.
The pulling resistance (air brake) and the stroke rate were individually adapted in order to reach the intended RPE for the session. Notably, although being considered primarily aerobic exercise, this modality also includes strengthening for the back, elbow flexors, and posterior shoulders [13]. For some participants with excessive pull strength, we fixated the chair with weight plates behind the rear wheels to avoid it from rolling backwards (Fig. 1A). During each session, participants received verbal encouragement, and power output, duration and distance were displayed on the ergometer thereby providing continuous feedback to the participants.
Data collection and analysis
Before the first exercise session, all participants arrived at the laboratory for baseline testing [22]. As a part of this visit, participants, while sitting in their own wheelchair, underwent a graded exercise test to exhaustion on an ACE (Monark 881E, Vansbro, Sweden) for determination of peak oxygen consumption (V̇O2peak). Breath-by-breath V̇O2, carbon dioxide production (V̇CO2), and heart rate was measured continuously using an open-circuit metabolic cart (JAEGER, Vyntus CPX, Carefusion) and a heart rate chest belt (Suunto, iQniter, Aalborg, Denmark), respectively. For offline analysis, V̇O2 and the respiratory exchange ratio (RER) were then averaged for every 15 s, with the highest two consecutive 15 s intervals (i.e. 30 s) reported as V̇O2peak and RERpeak, respectively, with the highest heart rate reported as HRpeak (for protocol details, see [22]). RPE was noted at the end of each minute, with the highest value reported as RPEpeak.
To obtain information about the usability and satisfaction with the REMW, participants completed the Feasibility and Acceptability Questionnaire [26]. Specifically, during week 1, 3 and 6, participants were asked to rate (Likert Scale) feasibility and acceptability of the rowing exercise. The scale was scored as: 1 (strongly disagree), 2 (disagree), 3 (moderately agree), 4 (agree), 5 (strongly agree). A median score of ≥3.0 was used as a criterion to indicate that the rowing exercise is perceived as acceptable [26]. The questionnaire consisted of six questions: how fun the exercise was perceived; the difficulty level of the exercise; whether the exercise was worth their time; if the exercise was easy to perform; whether the instructions for the exercise were clear; and whether they felt they received appropriate guidance in how to perform the exercise. Adherence to the training period (number of sessions completed) was recorded and presented as adherence rate (% participation). To evaluate the safety of the rowing exercise, any adverse events were noted.
Shoulder pain was assessed at baseline and at the end of week 6 using the Wheelchair Users Shoulder Pain Index (WUSPI) [27]. The index utilizes 15 visual analog scales (VAS) ranging from “no pain” to “worst pain ever experienced”, and provides a measure of the prevalence and severity of shoulder pain during different activities of daily living [27]. To account for missing activities, a performance-corrected shoulder pain score (PC-WUSPI) was calculated by dividing the raw total score by the number of executed activities multiplied by 15.
To examine the cardiovascular demand of the exercise, participants were equipped with a chest belt for beat-to-beat recordings of heart rate. Average heart rate was recorded based on the entire session and expressed relative to the maximum heart rate obtained during the graded arm-cranking test (%HRpeak). Because heart rate may be a poor indicator of exercise intensity in those with high (≥T6) SCI, participants were also asked to rate their RPE every 5th minute to verify the intended exercise intensity. Finally, total exercise duration (min), average power output (POAVG) and distance rowed (km) were recorded to monitor progress in exercise capacity and performance.
Within each week, we reported median (interquartile range, Q1–Q3) for exercise data (%HRpeak, RPE, POAVG, distance rowed, and exercise duration) of all 24 sessions (three sessions for each of the eight participants). Wilcoxon signed-rank tests were used to test for differences in shoulder pain before and after the 6 weeks of training, and for comparison of exercise data between week 1 and 6. Standardised effect sizes (Cohen d) were calculated to describe the magnitude of change and reported as small (>0.2), moderate (>0.5), and large (>0.8). Statistical significance was accepted at p ≤ 0.05.
Results
Feasibility and acceptability of the exercise
Feasibility and acceptability scores of the upper-body rowing exercise are presented in Table 2. Overall, median (Q1–Q3) on the feasibility and acceptability scale was 5.0 (4.0–5.0). For both week 1, 3 and 6, all six questions reached a median score of ≥4.0, and therefore met the minimum acceptable criterion score, indicating that the rowing exercise was perceived as feasible.
Table 2.
Feasibility and acceptability of the rowing exercise.
| Week items | 1 | 3 | 6 |
|---|---|---|---|
| I found the exercise fun to perform | 5.0 (4.0–5.0) | 4.5 (4.0–5.0) | 5.0 (4.0–5.0) |
| I was able to perform the exercise without difficulty | 4.5 (4.0–5.0) | 4.5 (4.0–5.0) | 4.5 (4.0–5.0) |
| The exercise was worth my time | 5.0 (5.0–5.0) | 5.0 (5.0–5.0) | 5.0 (5.0–5.0) |
| The exercise was easy to perform | 4.0 (4.0–4.8) | 4.0 (4.0–4.0) | 4.0 (4.0–4.0) |
| The instructions on how to perform the exercise were clear | 5.0 (5.0–5.0) | 5.0 (5.0–5.0) | 5.0 (5.0–5.0) |
| I received the guidance I needed from the exercise responsible | 5.0 (5.0–5.0) | 5.0 (5.0–5.0) | 5.0 (5.0–5.0) |
Data presented as median (Q1–Q3).
Out of the total 144 sessions (18 sessions per participant), 139 were completed (five participants completed all sessions), corresponding to an adherence rate of 97%. Reasons for not completing the sessions included sickness; lack of time due to work; and, for P1, recovery from tenodesis grasp issues. Six participants reported some muscle soreness at the back of the shoulders and lower arm after week 1, but this muscle soreness dissipated as the training period progressed. One participant (P1) reported an adverse event. Specifically, due to insufficient grip strength, P1 used a wrist strap with a hook to pull the ergometer handle, and at the end of week 4, P1 reported concerns that his tenodesis grasp would be compromised due to repetitive pulls on his finger ligaments from the wrist strap. However, we developed a solution (see Discussion) that allowed P1 to continue and complete the training period.
Physiological and performance data
Physiological and performance data are presented in Table 3. Exercise duration increased from week 1 to week 6 (z = −3.438, p = 0.001, d = 0.97). There was an average increase of 36% (z = −4.042, p < 0.001, d = 1.35) in distance rowed from week 1 to 6. Similarly, average power output increased by 37% (z = −3.36, p = 0.001, d = 0.97) from week 1 to week 6. Heart rate was relatively stable during the first three weeks and then increased steadily through week 3–6, with a significant increase from week 1 to 6 (z = −2.942, p = 0.003, d = 0.82) (Table 3). In six out of seven participants, heart rate during the six weeks of training, reached or exceeded HRpeak obtained with the ACE (103 (100–110) %HRpeak). Heart rate was not recorded in P1 as exercise demand was poorly reflected in heart rate for this participant. Examples of representative heart rate profiles from two participants are shown in Fig. 2. The pronounced cardiovascular load was also reflected by the RPE increasing from 15.0 (14.3–15.6) in week 1 to 16.0 (15.5–16.7) in week 6 (z = −3.529, p < 0.001, d = 0.85).
Table 3.
Physiological and performance data from 6 weeks (18 sessions) of training.
| Week | 1 | 2 | 3 | 4 | 5 | 6 | P valueb |
|---|---|---|---|---|---|---|---|
| %HRpeaka | 80.0 (72.8–84.8) | 77.5 (72.0–81.0) | 80.0 (77.3–84.8) | 81.0 (78.5–83.5) | 82.0 (80–90.3) | 83.0 (81.0–91.5) | 0.003 |
| RPE, Borg6–20 | 15.0 (14.3–15.6) | 15.2 (14.1–15.8) | 15.1 (14.3–16.3) | 15.3 (14.7–16.2) | 15.5 (15.0–16.4) | 16.0 (15.5–16.7) | 0.001 |
| POAVG (W) | 34.6 (20.1–47.4) | 41.5 (20.0–52.4) | 44.2 (17.6–54.3) | 47.4 (18.3–62.0) | 45.9 (15.5–61.6) | 49.8 (20.2–66.5) | 0.001 |
| Distance rowed (km) | 3.50 (2.17–4.42) | 4.12 (2.87–4.79) | 4.49 (3.13–4.94) | 4.68 (3.49–5.14) | 4.62 (3.20–5.12) | 4.75 (3.53–5.21) | <0.001 |
| Exercise duration (min) | 25 (20–30) | 30 (25–30) | 30 (30–30) | 30 (30–30) | 30 (30–30) | 30 (30–30) | 0.001 |
Data presented as median (Q1–Q3).
%HRpeak Average percent of peak heart rate, RPE Rating of perceived exertion, POAVG Average power output.
aN = 7
bChange from week 1 to week 6.
Fig. 2. Heart rate profiles from two representative participants.
A The participant (HRpeak of 186 bpm) rowed 6 x 5 min. B The participant (HRpeak of 170 bpm) rowed 2 x 15 min. Note that irrespectively of different durations and numbers of bouts, both participants reached the target duration of 30 min of effective exercise.
Shoulder pain
From baseline (23.0 (1.9–45.8)) to the end of week 6 (7.8 (1.5–47.9)), there was a non-significant (z = −0.14, p = 0.889, d = −0.22) reduction of 21% in shoulder pain, as measured with the PC-WUSPI. Individual and median (Q1–Q3) PC-WUSPI scores are presented in Table 4.
Table 4.
Wheelchair Users Shoulder Pain Index (WUSPI) at baseline and after six weeks.
| Participant | Activities completed | Raw WUSPI score | PC-WUSPI score | |||
|---|---|---|---|---|---|---|
| BL | 6 W | BL | 6 W | BL | 6 W | |
| P1 | 15 | 11 | 43.5 | 35.5 | 43.5 | 48.4 |
| P2 | 14 | 14 | 3.9 | 6.2 | 4.2 | 6.6 |
| P3 | 14 | 13 | 1.1 | 2.0 | 1.2 | 2.3 |
| P4 | 14 | 14 | 43.5 | 43.4 | 46.6 | 46.4 |
| P5 | 15 | 15 | 0.5 | 0.2 | 0.5 | 0.2 |
| P6 | 15 | 15 | 14.5 | 1.3 | 14.5 | 1.3 |
| P7 | 15 | 14 | 73.8 | 8.4 | 73.8 | 8.9 |
| P8 | 15 | 15 | 31.5 | 56.4 | 31.5 | 56.4 |
| Median (Q1–Q3) | 23.0 (1.8–43.5) | 7.3 (1.4–41.4) | 23.0 (1.9–45.8) | 7.8 (1.5–47.9) | ||
WUSPI Wheelchair Users Shoulder Pain Index, PC-WUSPI Performance-corrected Wheelchair Users Shoulder Pain Index, BL Baseline, 6W Six week follow up.
Discussion
The purpose of this study was to evaluate the feasibility, acceptability, and preliminary efficacy of wheelchair-modified rowing exercise and demonstrate how a commercially available rowing ergometer can be adapted to wheelchair users using an adaptive unit. Our main findings were that (1) exercise performed on the REMW were rated high on the feasibility and acceptability scale, with high adherence rates, (2) rowing exercise evoked moderate to vigorous intensity, as reflected in the high %HRpeak and RPE obtained during the sessions, and 3) rowing exercise did not exacerbate shoulder pain.
In this study, we addressed some of the reported challenges and barriers for exercise participation in individuals with SCI [3–5]. The REMW modality is easy to implement, as it only requires a commercially available Concept 2 ergometer and an Adapt2row (http://www.adapt2row.com/) unit for those with low SCI, whereas those with higher lesion, may require additional adaptive equipment such as trunk stability vest and supportive gloves. At the end of week 1, 3 and 6, participants rated the exercise to be feasible and acceptable. Notably, participants strongly agreed that the exercise was worth their time, and adherence rate was 97% with complete participant retention, which is considerable compared to adherence rates and dropout rates reported in previous interventions performed in this population [28]. While based on only six weeks of training, these findings indicate that REMW is a pragmatic and useful exercise option for individuals with SCI.
During each session, we carefully monitored the workload performed by the participants. As presented in Table 3, participants increased the distance rowed from week 1 to 6. The longer distance rowed aligned well with an increase in exercise duration. Despite this increase in total distance and duration, POAVG increased from week 1 to 6 suggesting that the participants improved their exercise capacity within this relatively short training period. The large effect sizes for the change in %HRpeak and RPE from week 1 to 6 suggest that the participants pushed themselves to a greater extent as the training period progressed. In fact, throughout the six weeks, median RPE was in the higher end of the prescribed intensity domain (12–17), suggesting that the participants were capable of maintaining vigorous intensity during the training sessions, and thus complying with recent exercise guidelines [1]. Among the three participants with SCI above T6, both P3 and P4 were able to increase heart rate to above 150 bpm during the rowing exercise. However, for P1, heart rate peaked at 100–115 bpm during both the ACE test and the first rowing sessions, suggesting disruption to the sympathetic nerves innervating the heart. Hence, heart rate did not adequately reflect exercise demand for this individual.
Due to the different exercise protocols (constant vs incremental), direct comparison between exercise performed on the REMW and ACE is difficult. However, it is noteworthy that six out of seven participants reached comparable or higher HRpeak values during rowing compared with graded exercise test on the ACE. Together with the high average %HRpeak observed during the training sessions, these results suggest that upper-body rowing is an effective aerobic exercise modality challenging the cardiorespiratory system. In fact, the average %HRpeak levels were comparable to levels previously reported for whole-body exercise (upper-body + lower extremity FES) [17]. Considering the rhythmic contractions and engagement of numerous arm, back and shoulder muscles [19], it may not be surprising that rowing represents a cardiorespiratory challenge, even though the activity is limited to the upper-body. Therefore, it is possible that a larger amount of active muscle mass may explain the higher heart rates attained during rowing, compared to ACE. Future studies are required to systematically compare the HRpeak and V̇O2peak obtained during rowing with that of more traditional exercise for individuals with SCI, as has previously been done for e.g., ACE and wheelchair ergometry [29]. Furthermore, the long term effects of this exercise modality on cardiorespiratory fitness level (V̇O2peak) and reduction in morbidity risk should be investigated, especially considering that individuals with SCI have an exaggerated risk of cardiovascular disease [30].
No exacerbation of shoulder pain was evident even though participants underwent six weeks of vigorous intensity upper-body exercise training. In fact, we observed an average reduction in shoulder pain of 21%, which is substantial considering the short training period. In comparison, Curtis et al. [12] observed an average reduction in PC-WUSPI score of ~40% after six months of strength and stretch training for the posterior and anterior shoulder musculature. Previously, Wilbanks et al. [31] demonstrated that six weeks of three weekly sessions of vigorous intensity FES-assisted rowing significantly reduced WUSPI score in individuals with SCI. In contrast, the reduction in shoulder pain in our study did not reach statistical significance. However, as the power to detect significant differences are influenced by small sample sizes, we also calculated Cohen d to determine the magnitude of effect. Nevertheless, as indicated by the small standardised effect size (d = 0.22), the clinical relevance of the reduction in shoulder pain at group level is questionable and thus remain to be demonstrated. Therefore, the conservative interpretation of our data is that six weeks of exercise on the REMW does not exacerbate shoulder pain. It should be noted, however, that several of the participants had minimal to no shoulder pain at baseline, which makes it difficult to show a reduction. Notably, the individual data (Table 4), reveal that the reduction in PC-WUSPI score for two participants (P6 and P7; both demonstrating shoulder pain at baseline) exceeded the estimated minimum detectable change of 5.10 points on the WUSPI scale [32], indicating a clinically important change in shoulder pain for these two participants. Studies including a longer training period are needed to adequately evaluate the effects of REMW on shoulder pain. Moreover, future studies are needed to investigate potential shoulder health benefits obtained from other upper-body exercise modalities that may preferentially active posterior muscle groups, such as ski polling ergometers [33].
One participant (P1) reported an adverse event related to the rowing exercise. Due to insufficient grip strength, P1 (AIS: B, NLI: C6) used a wrist strap with a hook to pull the ergometer handle, and at the end of week 4, P1 reported concerns that his tenodesis grasp would be compromised due to repetitive pulls on his finger ligaments from the wrist strap. We therefore developed a solution where the ergometer handle was tied to the participant’s elbow using a rope, thereby allowing him to pull without involvement of any musculature distal to the elbow (Supplementary Appendix 3). This solution allowed P1 to continue and complete the training period. Even though the other participant with tenodesis grasp (P4) did not experience similar issues, this undesirable event for P1 should be noted and warrants further attention. There were no other adverse events associated with the upper-body rowing. Together with our finding of complete participant retention and high adherence rate, these results suggest that exercise performed on a REMW is safe as long as current exercise recommendations and considerations are followed [34].
The small and heterogeneous sample, in terms of SCI characteristics (e.g., AIS score and etiology), is a limitation. Despite the large variation in injury characteristics, we were able to adapt the REMW to a large range of participants, including one with a motor complete injury as high as C6, leading to high adherence rate and overall satisfaction with the exercise training. Whereas four of the participants were able to perform the rowing exercise without any additional equipment, the other four participants required adaptive equipment to support the trunk or grip function. Although it worked as intended, rowing with the trunk support is a limitation, as the vest or chest belt cannot easily be secured to a frame (Fig. 1B, C), or other rigid material, independently by the user. Future investigations are needed to explore alternative ways to counteract this gravity challenge for individuals with a high lesion, for example by testing the feasibility of recumbent rowing, or by use of a chest pad mounted on the ergometer as recently explored [21].
Conclusion
In this feasibility study we demonstrated how rowing exercise can be adapted to wheelchair dependent individuals with SCI using a commercially available rowing ergometer and an adaptive unit. The modification of the rowing ergometer allowed these individuals to sit in their own wheelchair while performing upper-body rowing. Our preliminary data suggest that exercise performed on a REMW is a feasible and acceptable exercise modality and should be considered as an alternative or supplementary exercise modality for wheelchair dependent individuals. Finally, that the rowing exercise evoked moderate to vigorous intensity with no exacerbation of shoulder pain indicates that this modality may constitute a pragmatic and useful tool in terms of offering effective and safe aerobic exercise, with the potential to improve cardiorespiratory fitness level in this population.
Supplementary information
Acknowledgements
We would like to thank the participants who participated in the study. We would also like to acknowledge suppliers of training equipment (Wolturnus A/S for assistive equipment (Bodypoint vests and belt) and arm crank ergometer; Aalborg Rowing Club for lending of a Concept 2 ergometer; Modest Sport for sponsoring Adapt2row units; and iQniter for sponsoring heart rate belts). No financial assistance was received in support of this study.
Author contributions
RKH, AS, UL and RGL conceived and designed the protocol. RKH, JLJW and KF acquired data and RKH and JLJW analyzed data. RKH, AS, UL, RGL and KF interpreted the results. RKH and RGL drafted the manuscript and JLJW, AS, UL, KF revised the manuscript for important intellectual content. RKH, JLJW, AS, UL, KF and RGL all approved the final version of the manuscript, and all agreed to be accountable for all aspects of the work. As a corresponding author, RKH confirms that he has full access to the data in this study and final responsibility for the decision to submit for publication.
Data availability
The datasets of the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Committees on Health Research Ethics in The North Denmark Region (N-20190053) and registered at ClinicalTrials.gov (NCT04390087). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Informed consent
All participants received verbal as well as written information about the study before written consent was obtained.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
5/16/2022
A Correction to this paper has been published: 10.1038/s41394-022-00522-w
Supplementary information
The online version contains supplementary material available at 10.1038/s41394-022-00518-6.
References
- 1.Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–21. doi: 10.1038/s41393-017-0017-3. [DOI] [PubMed] [Google Scholar]
- 2.Eitivipart AC, de Oliveira CQ, Arora M, Middleton J, Davis GM. Overview of systematic reviews of aerobic fitness and muscle strength training after spinal cord injury. J Neurotrauma. 2019;36:2943–2963. doi: 10.1089/neu.2018.6310. [DOI] [PubMed] [Google Scholar]
- 3.Dolbow DR, Figoni SF. Accommodation of wheelchair-reliant individuals by community fitness facilities. Spinal Cord. 2015;53:515–519. doi: 10.1038/sc.2015.26. [DOI] [PubMed] [Google Scholar]
- 4.Gutierrez DD, Thompson L, Kemp B, Mulroy S. The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med. 2007;30:251–5. doi: 10.1080/10790268.2007.11753933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hansen RK, Larsen RG, Laessoe U, Samani A, Cowan RE. Physical activity barriers in danish manual wheelchair users: a cross-sectional study. Arch Phys Med Rehabil. 2021;102:687–93. doi: 10.1016/j.apmr.2020.09.384. [DOI] [PubMed] [Google Scholar]
- 6.Nash MS, van de Ven I, van Elk N, Johnson BM. Effects of circuit resistance training on fitness attributes and upper-extremity pain in middle-aged men with paraplegia. Arch Phys Med Rehabil. 2007;88:70–75. doi: 10.1016/j.apmr.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Ambrosio F, Boninger ML, Souza AK, Fitzgerald SG, Koontz AM, Cooper RA. Biomechanics and strength of manual wheelchair users. J Spinal Cord Med. 2005;28:407–14. doi: 10.1080/10790268.2005.11753840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burnham RS, May L, Nelson E, Steadward R, Reid DC. Shoulder pain in wheelchair athletes. The role of muscle imbalance. Am J Sports Med. 1993;21:238–42. doi: 10.1177/036354659302100213. [DOI] [PubMed] [Google Scholar]
- 9.van der Scheer JW, Martin Ginis KA, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury. A systematic review. Neurology. 2017;89:736–45. doi: 10.1212/WNL.0000000000004224. [DOI] [PubMed] [Google Scholar]
- 10.Farrow M, Nightingale TE, Maher J, McKay CD, Thompson D, Bilzon JLJ. Effect of exercise on cardiometabolic risk factors in adults with chronic spinal cord injury: a systematic review. Arch Phys Med Rehabil. 2020;101:2177–205. doi: 10.1016/j.apmr.2020.04.020. [DOI] [PubMed] [Google Scholar]
- 11.Arnet U, Van Drongelen S, Scheel-Sailer A, Van Der Woude LHV, Veeger DHEJ. Shoulder load during synchronous handcycling and handrim wheelchair propulsion in persons with paraplegia. J Rehabil Med. 2012;44:222–8. doi: 10.2340/16501977-0929. [DOI] [PubMed] [Google Scholar]
- 12.Curtis KA, Tyner TM, Zachary L, Lentell G, Brink D, Didyk T, et al. Effect of a standard exercise protocol on shoulder pain in long-term wheelchair users. Spinal Cord. 1999;37:421–9. doi: 10.1038/sj.sc.3100860. [DOI] [PubMed] [Google Scholar]
- 13.Volianitis S, Yoshiga CC, Secher NH. The physiology of rowing with perspective on training and health. Eur J Appl Physiol. 2020;120:1943–63. doi: 10.1007/s00421-020-04429-y. [DOI] [PubMed] [Google Scholar]
- 14.Olenik LM, Laskin JJ, Burnham R, Wheeler CD, Steadward RD. Efficacy of rowing, backward wheeling and isolated scapular retractor exercise as remedial strength activities for wheelchair users: application of electromyography. Paraplegia. 1995;33:148–52. doi: 10.1038/sc.1995.32. [DOI] [PubMed] [Google Scholar]
- 15.Ye G, Grabke EP, Pakosh M, Furlan JC, Masani K. Clinical benefits and system design of FES-rowing exercise for rehabilitation of individuals with spinal cord injury: a systematic review. Arch Phys Med Rehabil. 2021;102:1595–605. doi: 10.1016/j.apmr.2021.01.075. [DOI] [PubMed] [Google Scholar]
- 16.Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Gater DR. The effects of electrical stimulation on body composition and metabolic profile after spinal cord injury - Part II. J Spinal Cord Med. 2015;38:23–37. doi: 10.1179/2045772314Y.0000000244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Solinsky R, Draghici A, Hamner JW, Goldstein R, Taylor A. High-intensity, whole-body exercise improves blood pressure control in individuals with spinal cord injury: a prospective randomized controlled trial. PLoS One. 2021;16:1–13. doi: 10.1371/journal.pone.0247576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lamont LS. A simple ergometer modification can expand the exercise options for wheelchair clients. Disabil Rehabil Assist Technol. 2011;6:176–8. doi: 10.3109/17483107.2010.522681. [DOI] [PubMed] [Google Scholar]
- 19.Troy KL. Biomechanical validation of upper extremity exercise in wheelchair users: design considerations and improvements in a prototype device. Disabil Rehabil Assist Technol. 2011;6:22–28. doi: 10.3109/17483107.2010.509883. [DOI] [PubMed] [Google Scholar]
- 20.Troy KL, Munce TA, Longworth JA. An exercise trial targeting posterior shoulder strength in manual wheelchair users: Pilot results and lessons learned. Disabil Rehabil Assist Technol. 2015;10:415–20. doi: 10.3109/17483107.2014.905644. [DOI] [PubMed] [Google Scholar]
- 21.Wong RN, Stewart AL, Sawatzky B, Laskin JJ, Borisoff J, Mattie J et al. Exploring exercise participation and the usability of the adaptive rower and arm crank ergometer through wheelchair users’ perspectives. Disabil. Rehabil. (in press). [DOI] [PubMed]
- 22.Hansen RK, Samani A, Laessoe U, Handberg A, Larsen RG. Effect of wheelchair-modified rowing exercise on cardiometabolic risk factors in spinal cord injured wheelchair users: protocol for a randomised controlled trial. BMJ Open. 2020;10:e040727. doi: 10.1136/bmjopen-2020-040727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Powell KE, Paluch AE, Blair SN. Physical activity for health: what kind? how much? how intense? on top of what? Annu Rev Public Health. 2011;32:349–65. doi: 10.1146/annurev-publhealth-031210-101151. [DOI] [PubMed] [Google Scholar]
- 24.Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehab Med. 1970;2-3:92–98. [PubMed] [Google Scholar]
- 25.Soper C, Hume PA. Towards an ideal rowing technique for performance: the contributions from biomechanics. Sport Med. 2004;34:825–48. doi: 10.2165/00007256-200434120-00003. [DOI] [PubMed] [Google Scholar]
- 26.Visovsky C, Corripio J. Feasibility and acceptability of a resistance exercise intervention: for women undergoing chemotherapy for breast cancer. Nurs Heal. 2015;3:110–9. doi: 10.13189/nh.2015.030502. [DOI] [Google Scholar]
- 27.Curtis KA, Roach KE, Applegate EB, Amar T, Benbow CS, Genecco TD, et al. Development of the Wheelchair User’s Shoulder Pain Index (WUSPI) Paraplegia. 1995;33:290–3. doi: 10.1038/sc.1995.65. [DOI] [PubMed] [Google Scholar]
- 28.Martin Ginis KA, Hicks AL. Exercise research issues in the spinal cord injured population. Exerc Sport Sci Rev. 2005;33:49–53. [PubMed] [Google Scholar]
- 29.Baumgart JK, Brurok B, Sandbakk Ø. Comparison of peak oxygen uptake between upper-body exercise modes: a systematic literature review and meta-analysis. Front Physiol. 2020;11:1–12. doi: 10.3389/fphys.2020.00412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cragg JJ, Noonan VK, Krassioukov A, Borisoff J. Cardiovascular disease and spinal cord injury. Results a Natl Popul health Surv Neurol. 2013;81:723–8. doi: 10.1212/WNL.0b013e3182a1aa68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilbanks SR, Rogers R, Pool S, Bickel CS. Effects of functional electrical stimulation assisted rowing on aerobic fitness and shoulder pain in manual wheelchair users with spinal cord injury. J Spinal Cord Med. 2016;39:645–54. doi: 10.1179/2045772315Y.0000000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Curtis KA, Roach KE, Applegate EB, Amar T, Benbow CS, Genecco TD, et al. Reliability and validity of the Wheelchair User’s Shoulder Pain Index (WUSPI) Paraplegia. 1995;33:595–601. doi: 10.1038/sc.1995.126. [DOI] [PubMed] [Google Scholar]
- 33.Bjerkefors A, Tinmark F, Nilsson J, Arndt A. Seated double-poling ergometer performance of individuals with spinal cord injury - a new ergometer concept for standardized upper body exercise. Int J Sports Med. 2013;34:176–82. doi: 10.1055/s-0032-1311653. [DOI] [PubMed] [Google Scholar]
- 34.Evans N, Wingo B, Sasso E, Hicks A, Gorgey AS, Harness E. Exercise recommendations and considerations for persons with spinal cord injury. Arch Phys Med Rehabil. 2015;96:1749–50. doi: 10.1016/j.apmr.2015.02.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets of the current study are available from the corresponding author on reasonable request.