Abstract
Background
Research is a key component of medical practice, with involvement of medical students crucial for the future of healthcare. A major limitation for medical students is the lack of exposure to research education and projects. The purpose of this study was to analyse the exposure of medical students worldwide to research education and opportunities and their satisfaction with research in their curriculum and compare results between regions.
Methods
The International Federation of Medical Students Associations (IFMSA), through its Research Standing Committee, developed a questionnaire to understand the current situation worldwide regarding medical students’ access to research and research education in the medical curriculum. Students from all years from across the five regions of the IFMSA were eligible.
Results
A total of 619 responses representing 290 universities and 88 countries were received. Although 97.6% of medical students believed that research should be approached in their education, only 19.6% considered it was sufficiently addressed. Regarding education, only 36% of all respondents reported having specific mandatory research courses, with higher percentages in the Asia–Pacific and European countries. Even though an association between research opportunities and research participation was found, only 30% of students reported having specific places in research teams. Lastly, 39.3% had never participated in a research project.
Conclusion
Research education is a vital component of medical education, and medical students consider its inclusion as essential for their education. However, not enough emphasis on research education is placed across the globe, with most students seeking research opportunities to train themselves outside the formal curriculum.
Keywords: Medical students, Research, Curriculum, Education
Introduction
In the past decades, the medical curricula have evolved from traditional lectures to problem-based learning and use of a competency-based approach [1]. According to the CanMEDS 2015 Physician Competency Framework, physicians have a role as scholars, in which they should have the competency to contribute to the creation and dissemination of knowledge and practices applicable to health [2]. This includes understanding the scientific principles of research, applying research ethics, contributing to research, formulating research questions and selecting appropriate research methods as well as communicating research outcomes to professionals and patients.
The importance of research competencies for physicians has been shown through studies demonstrating that research-active healthcare institutions and providers appear to provide better care and achieve better patient outcomes [3–6]. Clinicians should demonstrate the ability to evaluate their own practices thoroughly, with the use of research tools. For example, all clinical guidelines are based on research studies such as systematic reviews and meta-analysis, therefore impacting clinicians’ decisions when diagnosing and treating patients [7].
In order to ensure physician participation in research, education and training in medical research should be included in medical education [8]. In fact, research experience is not only beneficial for physicians, but also appears to benefit medical students [9]. As medical graduates must show the ability to apply evidence-based medicine in their clinical practice, research for medical students improves their skills to critically analyse literature, ask the right questions and analyse data [10, 11]. This may help students to become physicians with a deeper appreciation, understanding and use of diagnostic techniques, as well as an evidence-based approach to medical problems. Furthermore, conducting research educates medical students to keep a record of their work in a complete, accurate and ethical way. These skills are transferable and applicable to clinical practice [12].
Research in medical school promotes professional development of a medical graduate. A study conducted in six countries found that 87% of medical students had been involved in some form of research, but only 34% had articles accepted or published in journals while in medical school [13]. Another study amongst international medical students only found that half were involved in research during medical school [14]. In contrast, several US-based studies found that up to 79% of their medical students had completed or were currently writing a manuscript of their research [15, 16]. Professional development through research was seen through a longitudinal study demonstrating that the percentage of students with publications is higher in the top 25% of funded residency programmes in the USA [17]. Not only publications and research presentations but university credits for undertaking research can enhance the competitiveness of a medical student to get their desired residency [12].
In medical school, research can be approached through theoretical research education or through research activities and experience, either mandatory, elective or extracurricular. However, there are still many barriers for medical student involvement in research. Several studies have found that the main factors limiting research work include insufficient supervision, lack of time and lack of institutional incentive [18, 19]. These barriers are reflected in the inclination of medical students to pursue a career in research. A multi-country study failed to find an increase in inclination towards a research career over the course of medical school, possibly due to the medical curricula, current methods of research education and absence of good research role models [13]. However, several medical student research programmes and initiatives have shown promising results with an increasing number of students interested in pursuing a research career after involvement in research projects [10, 20, 21]. Furthermore, an Irish study found that students with research competencies showed more motivation to continue in research [22]. Another key factor to consider is the perception of medical students, where 91 to 94% of medical students would include research in their curriculum [15, 19, 21].
Most studies have focused on research activities, such as special programmes, and have not assessed research education within medical curricula. Moreover, studies have been limited to select universities and have not compared regional education systems. The purpose of the present exploratory study is to describe the exposure of medical students worldwide to research education and research opportunities and their satisfaction with research in their medical curriculum and to compare results between regions.
Materials and Methods
Study Design and Target Group
A quantitative descriptive, cross-sectional study was conducted to assess medical students’ opinions and experience with research education in their institutions. The target group included medical students and recently graduated medical students off all years from across the five regions of the International Federation of Medical Students’ Associations (IFMSA) (Africa, Americas, Asia–Pacific, Eastern Mediterranean Region and Europe). Pre-medical students were not included. Within this study, universities were not contacted directly.
Questionnaire Development
An online questionnaire consisting of 16 questions was developed, available in English. Questions included basic demographic questions, dichotomous (‘yes/no’) questions regarding research education and opportunities in their university as well as multiple choice questions with predefined answers. The questions were organised in 3 thematic blocks: the first block explored the demographics of the participants, the second one focused on research education in their medical faculty, and the third block covered their personal experience with research. The block investigating specific research competencies was designed by compiling competencies found in relevant studies [23–25], without inclusion of soft skills. All questions were of closed type and mandatory to fill out. The questionnaire took an average of 5 to 10 min to complete. The questionnaire was developed by an international working committee of IFMSA focusing on research education and piloted by medical students prior to distribution.
Sampling and Questionnaire Distribution
The questionnaire was distributed through formal and informal IFMSA channels, namely, mailing lists, international IFMSA events and social media, targeting medical students worldwide. Participants were also recruited through their national student representatives who disseminated the questionnaire to the target population in the medical faculties of their home country. Participation was completely voluntary, and full confidentiality was maintained as no personal identifiable information was collected through the questionnaire. The questionnaire was available for a total period of 2 weeks, in January 2019.
Data Analysis
Data was entered into an Excel database (Microsoft Inc., Richmond, WA), which was used to generate descriptive results. Descriptive statistics were used to describe demographic characteristics, research education, participation and opportunities using frequencies and percentages for categorical variables. Results were presented to compare regions. The Chi-square test was used to compare categorical variables. All statistical analyses were performed in SPSS v. 26, and p values of ≤ 0.05 were considered statistically significant.
Ethics
This study obtained approval from the International Federation of Medical Students’ Associations Executive Board in January 2019. All procedures used in this study comply with the Declaration of Helsinki 1975, as revised in 2008. Study participation was voluntary, and informed written consent was obtained from each student.
Results
A total of 619 responses were received. One response was excluded due to incoherent personal information given regarding region, country and university. Therefore, 618 were taken into further consideration for analysis. The overall response rate between regions was 50 from Africa (8.1%), 323 from Americas (52.3%), 71 from the Asia–Pacific (11.5%), 46 from the Eastern Mediterranean region (7.4%) and 128 from Europe (20.7%). In total, participation from 290 universities representing 88 countries was recorded. The demographics of the students who responded to the questionnaire are described in Table 1.
Table 1.
Characteristics of the study population according to region and year of studies
| Current year of studies | Africa | Americas | Asia–Pacific | Eastern Mediterranean | Europe | Total |
|---|---|---|---|---|---|---|
| 1st | 3 | 13 | 3 | 5 | 2 | 26 (4.2%) |
| 2nd | 5 | 47 | 23 | 4 | 15 | 94 (15.2%) |
| 3rd | 6 | 88 | 18 | 12 | 28 | 152 (24.6%) |
| 4th | 13 | 61 | 17 | 11 | 37 | 139 (22.5%) |
| 5th | 19 | 55 | 6 | 8 | 25 | 113 (18.3%) |
| 6th | 1 | 43 | 1 | 1 | 17 | 63 (10.2%) |
| 7th | 0 | 4 | 1 | 2 | 0 | 7 (1.1%) |
| 8th | 2 | 7 | 0 | 1 | 0 | 10 (1.6%) |
| Recently graduated | 1 | 5 | 2 | 2 | 4 | 14 (2.3%) |
| Total | 50 (8.1%) | 323 (52.3%) | 71 (11.5%) | 46 (7.4%) | 128 (20.7%) | 618 |
The survey found that 97.6% of participants believed that research should be approached in medical education. This was seen across all years of studies and regions. When being asked if research is sufficiently included in their medical curriculum, 31.4% of respondents stated it is not, 49% answered that it is only partially included, and 19.6% agreed that research is sufficiently addressed in their curriculum. Regional analysis of the responses can be found in Table 2. The Asia–Pacific (35.2%) had the highest percentage of answers mentioning sufficiently included research education in their curriculum, while a high percentage of respondents from Africa (48%), Eastern Mediterranean (45.7%) and Europe (39.8%) expressed that research is not sufficiently addressed in their curriculum.
Table 2.
Comparison of research education and research opportunities according to region
| Total (n = 618) | Africa (n = 50) | Americas (n = 323) | Asia–Pacific (n = 71) | Eastern Mediterranean (n = 46) | Europe (n = 128) | |
|---|---|---|---|---|---|---|
| Is research education addressed sufficiently in your medical curriculum? | ||||||
| Yes | 121 (20%) | 6 (12%) | 65 (20%) | 25 (35%) | 8 (17%) | 17 (13%) |
| No | 194 (31%) | 24 (48%) | 82 (25%) | 16 (23%) | 21 (46%) | 51 (40%) |
| Partially | 303 (49%) | 20 (40%) | 176 (54%) | 30 (42%) | 17 (37%) | 60 (47%) |
| How is research education approached in your medical school? | ||||||
| Specific mandatory courses | 222 (36%) | 5 (10%) | 102 (32%) | 37 (52%) | 12 (26%) | 66 (52%) |
| Part of some courses | 143 (23%) | 13 (26%) | 89 (28%) | 15 (21%) | 6 (13%) | 20 (16%) |
| Specific elective courses | 56 (9%) | 0 | 24 (7%) | 8 (11%) | 9 (20%) | 15 (12%) |
| Extracurricular opportunities | 154 (25%) | 25 (50%) | 85 (26%) | 9 (13%) | 17 (37%) | 18 (14%) |
| Not approached at all | 43 (7%) | 7 (14%) | 23 (7%) | 2 (3%) | 2 (4%) | 9 (7%) |
| Does your school provide research opportunities for medical students? | ||||||
| Yes, there are specific places for students | 184 (30%) | 10 (20%) | 100 (31%) | 30 (42%) | 11 (24%) | 33 (26%) |
| Yes, if I personally reach out to investigators | 321 (52%) | 15 (30%) | 167 (52%) | 31 (44%) | 23 (50%) | 85 (67%) |
| No | 113 (18%) | 25 (50%) | 56 (17%) | 10 (14%) | 12 (26%) | 10 (8%) |
| Have you ever taken part in any kind of research project? | ||||||
| Yes, as lead investigator | 52 (8%) | 2 (4%) | 31 (10%) | 8 (11%) | 3 (6.5%) | 8 (6%) |
| Yes, as part of a research team | 213 (34%) | 21 (42%) | 111 (34%) | 22 (31%) | 24 (52%) | 35 (27%) |
| Yes, during a short-term placement (exchange, internship) | 110 (18%) | 8 (16%) | 50 (15%) | 9 (13%) | 3 (6.5%) | 40 (31%) |
| No | 243 (39%) | 19 (38%) | 131 (41%) | 32 (45%) | 16 (35%) | 45 (35%) |
Within the survey, medical students were asked about the way research education is approached in their medical curriculum (Table 2). Overall, only 36% of all respondents reported having specific mandatory courses tackling research. Responses showed clear regional differences. Students from the Asia–Pacific (52%) and Europe (52%) reported having more mandatory courses compared to students from other regions (Americas 32%, Eastern Mediterranean 26% and Africa 10%).
Answers regarding research opportunities provided by their universities were collected (Table 2), with the majority (51.9%) of respondents stating they have research opportunities provided by the university only if they personally reach out to the investigators. Only 30% of respondents had access to specific places in research teams. The highest percentage of research opportunities was found amongst students from the Asia–Pacific with 42% of respondents having specific places in research teams, while 50% of African respondents answered that their school did not provide any research opportunities. Regarding participation in research projects (Table 2), 39.3% of respondents had never participated in a research study, while only 8.4% had led an investigation. Out of the 375 respondents having taken part in a research opportunity, only 27.4% (n = 103) took part in the research project because it was mandatory by the university. Furthermore, there is an association between research opportunities provided by medical schools and participation in research projects (as lead investigator or as part of a research team) (p = 0.001). Similarly, a significant association between increasing year of studies and participation in research projects was found (p = 0.003).
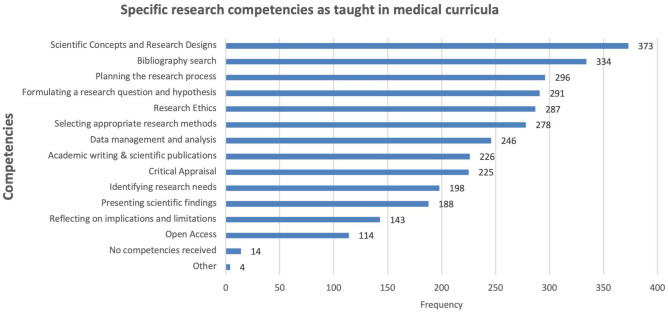
To better understand the specific research competencies taught in medical curricula worldwide, students were also asked which competencies they received from their universities, either through mandatory or elective courses. The specific research competencies can be found in Fig. 1. Lastly, students were asked whether they had published an article or presented their research at a conference. Only 10.3% (n = 64) respondents had published a research article.
Fig. 1.
Frequency of research competencies taught in medical school
Discussion
Our exploratory study has shown that a strong majority of medical students (97.6%) believe that research should be approached in medical education. However, only 19.6% of participants agreed that it is sufficiently addressed in their medical curriculum. These results clearly demonstrate a global lack of proper research education in medical schools as part of the official curriculum and show that there is a big demand for curricular change.
Within our survey, we found that only 35.9% of participants’ curriculum requires mandatory research courses, highlighting that majority of participants are not educated about medical research. While a previous study amongst international students compared high-income versus low-income countries [14], the present study aimed at comparing regions. A major limitation is the limited number of responses from several regions, such as Africa, the Asia–Pacific and the Eastern Mediterranean Region, making it difficult to draw well-based conclusions, also due to the heterogeneity of medical curricula. However, the limited data does show some trends. Surprisingly, considerable differences could be seen between regions with more than half of Asia–Pacific and European students reporting mandatory research courses, while the percentage in other regions was much lower. Only 7% of students reported that research was not approached at all in their education. However, 25% of students could only find research education through extracurricular education, further highlighting the need for proper implementation of research education and incentives. It is important to note that students might not recognise some research training or opportunities as ‘formal research training’ or ‘mandatory research courses’. However, as most medical students believe research is necessary within medical curricula, this underlines the necessity for formal curricular implementation or at least for a more systematic and structured way of organising research courses. Several studies have already suggested benefits from mandatory research courses and electives [10–12]. De Oliveira et al. suggested it is not only important to make research courses mandatory, it is also crucial to ensure that all aspects, ranging from technical aspects to hypothesis writing and presentation of results, are adequately taught [19]. This was also suggested in a longitudinal study where no change in inclination towards research or a research career was seen throughout medical studies [13].
Our results suggest that less than one third of students have access to formal research opportunities and that formal research education and opportunities might be the bottleneck to the conduction of evidence-based medicine. It is possible that the reports regarding research opportunities are underrepresented as responders from first years of medical school might not be aware of all opportunities. 51.9% of respondents reported that research opportunities exist only when personally reaching out to investigators, and 18.3% of students even reported that no research opportunities and placements are available at all for them. Yet, these results have a very broad variance depending on regions. While in Europe 65.9% reported having research spots when personally reaching out to investigators, 50% of African medical students reported not having any research opportunities at all. A review reported elective research projects as the most common research opportunities [9]. However, most studies are US-based or have focused on specific research programmes of universities. The literature reports variable percentages of involvement in research projects by medical students. A study amongst Canadian students showed that 43% of students had no involvement in research projects during medical school [26], and a Brazilian study only had 47% of students involved in research [19], while other studies reported up to 87% involvement in research [13]. Although this study suggests regional differences in research opportunities, especially for African medical students, further studies are needed to confirm these differences and investigate underlying determinants. While it is still unclear whether research activity in medical school should be mandatory or elective, it is concerning to see that regional or national location can have an impact on availability of research opportunities [9]. Therefore, an initial step should be taken by medical schools and research centres to provide elective research opportunities for students without opportunities.
Regarding participation in research, almost 40% of our respondents stated that they never participated in a research project, without considerable differences between regions. 34.5% had been part of a research team and only 8.4% had led an investigation themselves. Another interesting finding is that 17.8% of students participated in a short-term placement such as research exchange or an internship, which indicates that there is a role of extracurricular research opportunities and placements. These results also confirm the different degrees of involvement in research. With unclear literature about this topic, this underlines the necessity to investigate to which degree medical students should be involved in research. Our findings also confirm that there is a direct correlation between research opportunities offered by the university and research participation of the students which further emphasises the importance of providing proper research opportunities in formal medical curricula. Some universities have already shown that implementation of research training programmes is effective both in increasing knowledge and competency in research but also in motivating students towards a career in research [10, 27]. For example, Norway has implemented the Student Research Programme to recruit medical students to research, which has led to an increase in recruitment of physicians with interest to pursue research [20]. However, despite local initiatives found in the literature and student motivation to be involved in research, our results clearly demonstrate the lack of research opportunities and involvement across all regions.
The survey also investigated which research competencies are currently taught in medical curricula worldwide either as a part of elective or mandatory courses. Our results have shown that there is a big gap between different aspects of research that are officially taught in medical schools (Fig. 1). Some topics such as basic technical aspects, hypothesis formation, bibliography search and research ethics are regularly being addressed as part of the curriculum globally. On the other hand, some important topics that might be crucial for future physicians are not included in the curriculum systematically — for example, critical appraisal, reflection on implications and limitations of research and Open Science as well as presentation of scientific findings and academic writing. Although there are existing competency-based frameworks for physicians [28–31] and clinical research professionals [32], research competencies and frameworks for medical students and graduates are scarce in the literature. Further work is needed to define which research competencies and skills should be included in medical curriculum and to what degree. Furthermore, the implementation of structured programmes for scientific training accessible to all students should be explored [19]. One such example of a programme in the UK uses a curriculum designed at teaching research skills incrementally to complete a research project at the end. However, this requires proper theoretical research training and experiential learning through research opportunities and supervision [24].
It is somehow surprising that only 10.3% of respondents published a research article. A possible explanation is the inclusion of students from all years of education, while studies have shown that research productivity and output increase throughout medical training [26]. However, a multi-country study reported variable percentages of students who had published an article while in medical school, from 9% to as high as 76% depending on the school [13]. It is unclear why these differences in student publications between countries and schools exist, possibly due to variable research opportunities or research publications as an important factor for residency applications. Another possible explanation for low scientific output of medical students could be the lack of formal training in academic writing and dissemination of research as shown in this study.
There are several limitations to this study. Firstly, results are based on self-reported questionnaires by medical students. Although these measures are often used in cross-sectional studies, responses can be subject-dependent and are subject to recall bias and cultural differences in observation and reporting, especially in responses regarding research education and competencies received. Further studies are required to target universities formally and objectively. Secondly, there are differences in medical education systems worldwide, imposing significant limitations on comparisons of research in the medical curriculum between countries and regions. Several countries require previous degrees (sometimes research-oriented), while others do not. Therefore, more thorough investigations exploring specific requirements for medical schools as well as the background of medical students are necessary to be able to compare countries more objectively. Thirdly, although there are participants from 88 countries, the number of responses per university is considerably low. There is also an unequal distribution between regions, with an overrepresentation of students from the Americas region. Given the large geographic distribution, the sample size of individual countries is low. Lastly, due to the dissemination of the questionnaire amongst members of a non-governmental organisation advocating for research education, there is a selection bias towards students who might have more access to extracurricular research education and opportunities.
Conclusion
The data presented in this exploratory study shows that research in the medical curriculum is insufficiently addressed throughout all regions. Although almost all participants recognise the importance of research education, most students did not receive mandatory research courses. Furthermore, this study is the first to make a global analysis, suggesting considerable regional differences in both research education and research opportunities. Consistent with the literature, these results suggest that not all students have access to research opportunities. However, regional analysis suggests that African students have less opportunities than students from other regions, while European students often need to reach out to investigators personally to pursue research. The literature presents several examples of successful research education without compromising other elements of the medical curriculum. Due to the limited data, it is difficult to draw specific conclusions. To enhance research education throughout all regions and countries, further studies are needed to understand how research education can be incorporated in a sustainable manner. Furthermore, understanding the research competencies medical students should master will help to incorporate research education equally throughout medical schools.
Availability of Data and Material
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics Approval
Ethics approval was described in the Methods section.
Consent to Participate
Study participation was voluntary and informed written consent obtained from all individuals.
Consent for Publication
Consent for publication was obtained from all individuals before study participation.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Boyd V, Whitehead C, Thille P, Ginsburg S, Brydges R, Kuper A. Competency-based medical education: the discourse of infallibility. Med Educ. 2018;52(1):45–57. doi: 10.1111/medu.13467. [DOI] [PubMed] [Google Scholar]
- 2.Frank J, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015. [Google Scholar]
- 3.Du Bois A, Rochon J, Lamparter C, Pfisterer J. Pattern of care and impact of participation in clinical studies on the outcome in ovarian cancer. Int J Gynecol Cancer. 2005;15(2):183–191. doi: 10.1111/j.1525-1438.2005.15202.x. [DOI] [PubMed] [Google Scholar]
- 4.Majumdar S, Roe M, Peterson E, Chen A, Gibler W, Armstrong P. Better outcomes for patients treated at hospitals that participate in clinical trials. Arch Intern Med. 2008;168(6):657–662. doi: 10.1001/archinternmed.2007.124. [DOI] [PubMed] [Google Scholar]
- 5.Selby P, Autier P. The impact of the process of clinical research on health service outcomes. Ann Oncol. 2011;22(Suppl 7):vii5–vii9. doi: 10.1093/annonc/mdr419. [DOI] [PubMed] [Google Scholar]
- 6.Clarke M, Loudon K. Effects on patients of their healthcare practitioner's or institution's participation in clinical trials: a systematic review. Trials. 2011;12:16. doi: 10.1186/1745-6215-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacob H. Why all doctors should be involved in research. BMJ. 2016;352:i164. doi: 10.1136/bmj.i164. [DOI] [Google Scholar]
- 8.Rahman S, Majumder M, Shaban S, Rahman N, Ahmed M, Abdulrahman K, et al. Physician participation in clinical research and trials: issues and approaches. Adv Med Educ Pract. 2011;2:85–93. doi: 10.2147/AMEP.S14103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carberry C, McCombe G, Tobin H, Stokes D, Last J, Bury G, et al. Curriculum initiatives to enhance research skills acquisition by medical students: a scoping review. BMC Med Educ. 2021;21(1):1–13. doi: 10.1186/s12909-021-02754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Houlden R, Raja J, Collier C, Clark A, Waugh J. Medical students' perceptions of an undergraduate research elective. Med Teach. 2004;26(7):659–661. doi: 10.1080/01421590400019542. [DOI] [PubMed] [Google Scholar]
- 11.Metcalfe D. Involving medical students in research. J R Soc Med. 2008;101(3):102–103. doi: 10.1258/jrsm.2008.070393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collier A. Medical school hotline: importance of research in medical education. Hawai'i J Med Public Health. 2012;71(2):53–56. [PMC free article] [PubMed] [Google Scholar]
- 13.Ha T, Ng S, Chen C, Yong S, Koh G, Tan S, et al. Inclination towards research and the pursuit of a research career among medical students: an international cohort study. BMC Med Educ. 2018;18(1):86. doi: 10.1186/s12909-018-1202-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salloum RH, Nazha B, Zgheib NK. Interest and involvement in research during medical school: a global comparison of students at high- and low-income universities. Med Sci Educ. 2014;24(1):65–73. doi: 10.1007/s40670-014-0019-0. [DOI] [Google Scholar]
- 15.Jacobs C, Cross P. The value of medical student research: the experience at Stanford University School of Medicine. Med Educ. 1995;29(5):342–346. doi: 10.1111/j.1365-2923.1995.tb00023.x. [DOI] [PubMed] [Google Scholar]
- 16.Karani R, Ognibene F, Fallar R, Gliatto P. Medical students' experiences with authorship in biomedical research: a national survey. Acad Med. 2013;88(3):364–368. doi: 10.1097/ACM.0b013e31827fc6ae. [DOI] [PubMed] [Google Scholar]
- 17.Conroy M, Shaffiey S, Jones S, Hackam D, Sowa G, Winger D, et al. Scholarly research projects benefit medical students' research productivity and residency choice: outcomes from the University of Pittsburgh School of Medicine. Acad Med. 2018;93(11):1727–1731. doi: 10.1097/ACM.0000000000002328. [DOI] [PubMed] [Google Scholar]
- 18.Ville R, Ilkka H, Ilkka S. Research and medical students. Med Teach. 2000;22(2):164–167. doi: 10.1080/01421590078599. [DOI] [Google Scholar]
- 19.de Oliveira N, Luz M, Saraiva R, Alves L. Student views of research training programmes in medical schools. Med Educ. 2011;45(7):748–755. doi: 10.1111/j.1365-2923.2011.03986.x. [DOI] [PubMed] [Google Scholar]
- 20.Hunskaar S, Breivik J, Siebke M, Tømmerås K, Figenschau K, Hansen J. Evaluation of the medical student research programme in Norwegian medical schools. A survey of students and supervisors. BMC Medical Educ. 2009;9:43. doi: 10.1186/1472-6920-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oliveira C, de Souza R, Abe E, Silva Móz L, de Carvalho L, Domingues M. Undergraduate research in medical education: a descriptive study of students' views. BMC Med Educ. 2014;14:51. doi: 10.1186/1472-6920-14-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burgoyne L, O'Flynn S, Boylan G. Undergraduate medical research: the student perspective. Med Educ Online. 2010;15. [DOI] [PMC free article] [PubMed]
- 23.Ianni P, Samuels E, Eakin B, Perorazio T, Ellingrod V. Assessments of research competencies for clinical investigators: a systematic review. Eval Health Prof. 2021;44(3). [DOI] [PMC free article] [PubMed]
- 24.Riley S, Morton J, Ray D, Swann D, Davidson D. An integrated model for developing research skills in an undergraduate medical curriculum: appraisal of an approach using student selected components. Perspect Med Educ. 2013;2(4). [DOI] [PMC free article] [PubMed]
- 25.Laidlaw A, Aiton J, Struthers J, Guild S. Developing research skills in medical students: AMEE Guide No. 69. Med Teach. 2012;34(9). [DOI] [PubMed]
- 26.Siemens D, Punnen S, Wong J, Kanji N. A survey on the attitudes towards research in medical school. BMC Med Educ. 2010;10:4. doi: 10.1186/1472-6920-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dicianno B, Glick R, Sowa G, Boninger M. Processes and outcomes from a medical student research training program in integrative, complementary, and alternative medicine. Am J Phys Med Rehabil. 2016;95(10):779–786. doi: 10.1097/PHM.0000000000000508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bland C, Center B, Finstad D, Risbey K, Staples J. A theoretical, practical, predictive model of faculty and department research productivity. Acad Med. 2005;80(3):225–237. doi: 10.1097/00001888-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Löwe B, Hartmann M, Wild B, Nikendei C, Kroenke K, Niehoff D, et al. Effectiveness of a 1-year resident training program in clinical research: a controlled before-and-after study. J Gen Intern Med. 2008;23(2):122–128. doi: 10.1007/s11606-007-0397-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dilmore T, Moore D, Bjork Z. Developing a competency-based educational structure within clinical and translational science. Clin Transl Sci. 2013;6(2):98–102. doi: 10.1111/cts.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel M, Tomich D, Kent T, Chaikof E, Rodrigue J. A program for promoting clinical scholarship in general surgery. J Surg Educ. 2018;75(4):854–860. doi: 10.1016/j.jsurg.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 32.Sonstein S, Silva H, Seltzer J, Li R, Jones C, Daemen E. Moving from compliance to competency: a harmonized core competency framework for the clinical research professional. J Clin Res Best Pract. 2014;10:1–11. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.