Abstract
The COVID-19 pandemic disrupted mental health services delivery across the US, but the extent and implications of these disruptions are unclear. This retrospective observational analysis used the claims clearinghouse Office Ally to compare outpatient mental health services use from March to December 2016–18 against use during the same period in 2020. We identified encounters for people ages twelve and older with primary diagnosis codes corresponding to mental health conditions and categorized encounters as in-person or telehealth, using Current Procedural Terminology and place-of-service codes. In-person mental health encounters were reduced by half in the early months of the pandemic, with rapid recovery of service delivery attributable to telehealth uptake (accounting for 47.9 percent of average monthly encounters). We found variation in the degree to which telehealth use increased across groups: People with schizophrenia made up a lower proportion of telehealth encounters relative to in-person visits (1.7 percent versus 2.7 percent), whereas those with anxiety and fear-related disorders accounted for a higher proportion (27.5 percent versus 25.5 percent). These findings highlight the importance of broadening access to services through new modalities without supplanting necessary in-person care for certain groups.
The COVID-19 pandemic increased the need for mental health services while simultaneously disrupting the delivery of those services. There are growing reports that unmet demand for mental health services rose during the pandemic, going from one in ten adults reporting symptoms of anxiety or depression to four in ten adults, with differential impact across communities.1,2 These estimates correspond to recent studies suggesting that persistent psychological distress and anxiety are associated with surviving COVID-19 and with prolonged periods of quarantine, social isolation, and school and work disruptions among the population.3
In March 2020, early in the pandemic, many state and local governments also instituted stay-at-home orders and other restrictions to reduce viral spread. Evidence suggests that this lockdown was associated with increased emotional distress and risk for mental health disorders, signaling greater demand for mental health services.4,5 At the same time, emergency department encounters for mental health conditions6 and the number of new antidepressant and antipsychotic prescriptions decreased,7 raising concerns about the extent to which people with mental health conditions could obtain appropriately intensive services or maintain treatment continuity where needed.
The Coronavirus Aid, Relief, and Economic Security (CARES) Act was passed in March 2020, partly in response to these care delivery challenges.8 The CARES Act included provisions that expanded telehealth coverage, including reimbursement for telehealth services for Medicare enrollees at rates equivalent to those for in-person care. Many private insurers quickly followed suit. Within the Medicaid program, most states expanded access to telehealth, with all states eventually covering behavioral health services and forty-two states and Washington, D.C., specifying that some telehealth services be paid at the same rate as in-person services.9 These policy changes have contributed to increases in telehealth uptake across health care delivery settings and conditions.10
However, the extent to which these initial disruptions in mental health services affected care delivery in subsequent months and the degree to which telehealth adoption addressed these challenges are yet unknown. Despite extensive uptake of telehealth delivery for mental health care, it is also unclear whether uptake may have differed across mental health conditions. In this context, this descriptive study used a large claims database to compare mental health services use before and during the pandemic, including across different segments of the population with mental health conditions.
Study Data And Methods
We conducted a retrospective observational analysis using claims data from Office Ally, comparing 2016–18 prepandemic trends with trends during the pandemic, from March to December 2020. Office Ally is a claims clearinghouse that processes professional and institutional claims to Medicaid, Medicare, and commercial payers. Its billing providers typically send all claims within sixty days of the service date. Although Office Ally covers 3.4 billion claims on 100 million unique patients in all fifty states and Washington, D.C., it is used primarily among smaller and independent outpatient practices on the West Coast. Office Ally claims data were provided through the COVID-19 Research Database, a public-private consortium to facilitate pandemic-related research.11 We last accessed the data in November 2021.
DATA
We identified all encounters for people ages twelve and older whose primary diagnosis codes corresponded to mental health conditions; we excluded encounters with primary diagnosis codes related to substance use disorders because of differences in utilization patterns.12 We then categorized encounters by diagnosis, using the Healthcare Cost and Utilization Project’s Clinical Classifications Software for multilevel diagnoses into the following categories: depressive disorders, bipolar and other mood disorders, anxiety and fear-related disorders, schizophrenia and psychotic disorders, trauma and stress-related disorders, and other. We restricted our analytic sample to providers that were in the Office Ally claims clearinghouse in all study years (2016–18 and 2020).We excluded data from 2019 because large amounts of data were missing or unreliable in that year, an issue recognized by the COVID-19 Research Database. To ensure that our duringpandemic trends were directly comparable to prepandemic trends, we compared March–December 2020 data with data from the correlating months in prepandemic years.
ANALYSIS
We categorized encounters as in-person or telehealth, using a combination of Current Procedural Terminology (CPT) and place-of-service codes. Telehealth appointment visits included both audio-only (CPT codes 99441–3) and audio-video (modifier codes GT, GQ, or 95) visits and also included encounters billed under a telehealth place-of-service code (02), capturing additional visits occurring before Medicare’s expanded telehealth coverage in March 2020 in response to the pandemic. Provider specialties were derived from the National Plan and Provider Enumeration System, with providers categorized as specialty mental health prescribers (psychiatrists, mental health nurse practitioners, and mental health physician assistants), nonprescribing mental health specialists (therapists and counselors, clinical nurse specialists, psychologists, and social workers), and all other providers.
We conducted descriptive analyses comparing outpatient services use before and during COVID-19.We compared the average proportion of monthly encounters by age, sex, and diagnosis group in both periods, using chi-square tests for independence, and we stratified changes in telehealth versus in-person encounters along a number of dimensions, including mental health condition and provider type. Finally, we estimated the correlation between pre- and duringpandemic changes in telehealth uptake and in-person services use at the state level. All analyses were conducted using SAS, version 9.4.
LIMITATIONS
This analysis had several limitations. First, external validity may be limited, as 43.0 percent of the providers in our analytic sample were located in California, Oregon, or Washington State (see online appendix exhibit A1).13 Second, we did not have access to patient or facility-level identifiers and thus were unable to evaluate whether utilization changes occurred at the patient or facility level, including whether patients were new or established. Third, we limited our data set to encounters with primary diagnosis codes related to mental health. This approach is commonly used in the literature for claims-based analyses.14–16 However, providers might not have coded a mental health diagnosis as “primary” even if they provided mental health care. Therefore, our analysis provides baseline estimates of utilization rates that excluded encounters where mental health conditions were addressed but were coded as secondary or tertiary diagnoses. Because we focused only on primary diagnoses, our approach could have included episodes with co-occurring mental health and substance use disorders. Finally, data from 2019 were excluded because of missing data in the Office Ally database, so we were unable to assess changes in utilization immediately before the start of the pandemic.
Study Results
Our data included 101.7 million outpatient mental health condition encounters; 76.4 million (75.1 percent) occurred in the pre-COVID-19 period, and 25.3 million (24.9 percent) occurred during COVID-19 (exhibit 1). In 2020, during the pandemic, a higher proportion of outpatient encounters occurred among those ages 18–24 and 25–34 (p < 0:001). Similarly, the distribution of encounters by mental health condition was significantly different between the pre-COVID-19 and COVID-19 periods, with the proportion of anxiety and fear-related disorders increasing slightly relative to 2016–18 (p < 0:001).
EXHIBIT 1.
Patient and visit characteristics of mental health encounters with clinicians before and during the COVID-19 pandemic, 2016–18 and 2020
| Before COVID-19 |
During COVID-19 |
|||
|---|---|---|---|---|
| 2016 (N = 23,367,181) |
2017 (N = 25,803,093) |
2018 (N = 27,224,568) |
2020 (N = 25,274,298) |
|
| Age (years)**** | ||||
| 12–17 | 10.8% | 11.0% | 11.2% | 10.3% |
| 18–24 | 10.6 | 11.0 | 11.5 | 12.2 |
| 25–34 | 19.2 | 19.8 | 19.9 | 21.1 |
| 35–44 | 19.2 | 19.0 | 18.9 | 19.3 |
| 45–54 | 17.9 | 17.3 | 16.6 | 15.3 |
| 55–64 | 13.5 | 13.2 | 13.1 | 12.5 |
| 65+ | 8.7 | 8.6 | 8.9 | 9.2 |
| Sex | ||||
| Female | 66.1 | 66.4 | 66.3 | 67.5 |
| Mental health conditions**** | ||||
| Depressive disorders | 33.1 | 32.0 | 31.1 | 29.6 |
| Bipolar and other mood disorders | 6.8 | 6.5 | 6.2 | 5.9 |
| Anxiety and fear-related disorders | 22.3 | 23.2 | 24.1 | 26.3 |
| Schizophrenia and other psychotic disorders | 2.5 | 2.5 | 2.5 | 2.3 |
| Trauma and stress-related disorders | 30.4 | 31.1 | 31.5 | 31.5 |
| Other | 4.8 | 4.6 | 4.6 | 4.5 |
| Encounter setting**** | ||||
| Telehealth | 0.0 | 0.1 | 0.3 | 39.6 |
| Provider type | ||||
| Specialty MH prescribera | 10.9 | 10.5 | 10.2 | 11.2 |
| Nonprescribing MH specialistb | 72.9 | 72.5 | 72.4 | 70.7 |
| Other provider or unspecified | 13.7 | 13.4 | 13.1 | 14.1 |
source Authors’ analysis of Office Ally administrative claims data. notes Selected characteristics of mental health (MH) encounters occurring in March–December before and during the pandemic. Sample sizes are numbers of encounters. Calculated column percentages are displayed. p value levels based on chi-square tests between proportions of average monthly encounters by age, sex, diagnosis group (mental health conditions), and encounter setting before and during COVID-19. A full version of this exhibit including counts of encounters is in appendix exhibit A2 (see note 13 in text).
Psychiatrists, mental health nurse practitioners, and mental health physician assistants.
Therapists and counselors, clinical nurse specialists, psychologists, and social workers.
p < 0.001
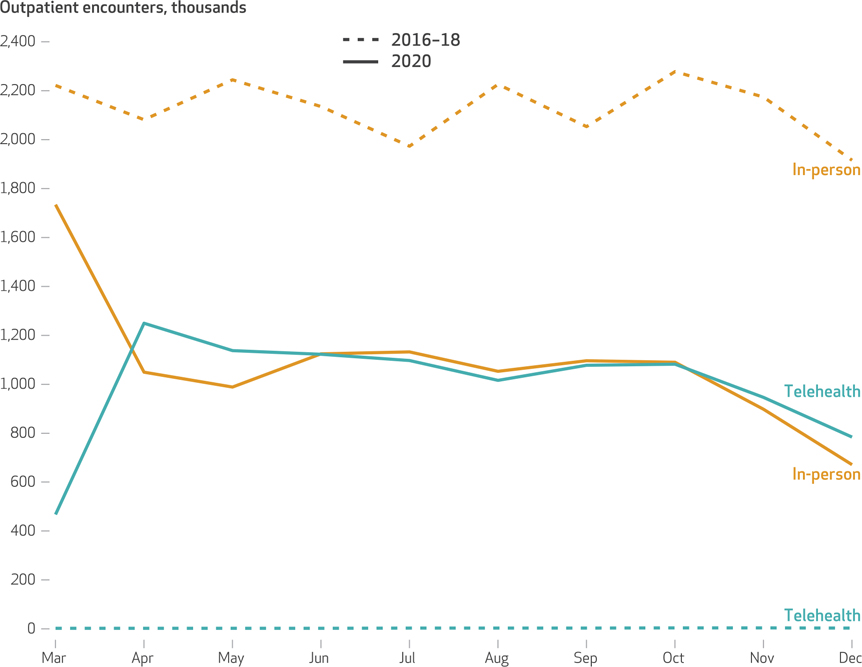
There was a 21.9 percent reduction in in-person visits in March 2020 compared with the same month in prior years, and reductions of 49.6 percent and 55.9 percent, respectively, in April and May 2020 compared with those months in prior years (exhibit 2). In subsequent months of the pandemic, there was a substantial recovery in outpatient mental health services use. As early as April 2020, for example, encounter volume (combination of in-person and telehealth encounters) exceeded prepandemic levels, at 2.3 million encounters, or 10.4 percent more than average monthly prepandemic levels in April 2016–18. Although in-person visits remained low, a growing share of telehealth encounters accounted for these increases in total volume ofoutpatient mental health services use after March 2020. During the pandemic 47.9 percent of monthly average encounters were telehealth compared with negligible telehealth volumes in preceding study years (ranging from 2,000 to 4,000 unique encounters). This rise in telehealth services use occurred within one month of the initial lockdown period.
Exhibit 2. Trends in monthly in-person and telehealth outpatient mental health encounters in the US before and during the COVID-19 pandemic, 2016–18 and 2020.
source Authors’ analysis of Office Ally administrative claims data. notes The dashed lines show the average monthly in-person and telehealth encounters in the prepandemic period (March–December 2016–18). The solid lines show average monthly in-person and telehealth encounters during the pandemic (March–December 2020). Pre-2020 monthly telehealth encounter volumes ranged stably from 2,000 to 4,000 unique visits. Data for 2019 were not available from the Office Ally database, as explained in the text.
Exhibit 3 compares outpatient mental health services use before and during the COVID-19 pandemic, stratified by patient characteristics and mental health conditions. The average number of monthly mental health encounters was 2.12 million in the prepandemic period versus 2.11 million during the pandemic period—a relative decrease in volume of only 0.7 percent. However, during the pandemic the number of average monthly encounters declined by 7.2 percent for those ages 12–17, by 11.9 percent for those ages 45–54, and by 6.7 percent for those ages 55–64, while increasing for other age groups. Likewise, the number of average monthly encounters declined by 10.6 percent for bipolar disorders, 8.5 percent for schizophrenia and psychotic disorders, and 8.2 percent for depressive disorders. Average monthly encounters for anxiety and fear-related disorders rose by 12.1 percent, from 494,000 to 554,000 encounters, during this period (appendix exhibit A3).13
Exhibit 3.
Changes in mental health services use (monthly mental health encounters) before and during the COVID-19 pandemic In the US, by population characteristics and mental health conditions, 2016–18 and 2020
| 2016–18 (N = 2,122,079) |
2020 (N = 2,106,192) |
||||
|---|---|---|---|---|---|
| % of visits | % of visits | % change from 2016–18 | % in person | % telehealth | |
| Unique encounters | —a | —a | −0.7 | 60.4 | 39.6 |
| Age (years)**** | |||||
| 12–17 | 11.0 | 10.3 | −7.2 | 10.4 | 10.1 |
| 18–24 | 11.1 | 12.2 | 9.8 | 11.5 | 13.3 |
| 25–34 | 19.7 | 21.1 | 6.7 | 19.5 | 23.6 |
| 35–44 | 19.0 | 19.3 | 0.7 | 18.7 | 20.2 |
| 45–54 | 17.3 | 15.3 | −11.9 | 15.6 | 14.9 |
| 55–64 | 13.3 | 12.5 | −6.7 | 13.1 | 11.6 |
| 65+ | 8.7 | 9.2 | 5.1 | 11.2 | 6.2 |
| Sex**** | |||||
| Female | 66.3 | 67.5 | 1.1 | 66.1 | 69.7 |
| Mental health condition**** | |||||
| Depressive disorders | 32.0 | 29.6 | −8.2 | 30.4 | 28.4 |
| Bipolar and other mood-related disorders | 6.5 | 5.9 | −10.6 | 9.0 | 5.7 |
| Anxiety and fear-related disorders | 23.3 | 26.3 | 12.1 | 25.5 | 27.5 |
| Schizophrenia and other psychotic disorders | 2.5 | 2.3 | −8.5 | 2.7 | 1.7 |
| Trauma and stress-related disorders | 31.0 | 31.5 | 0.6 | 31.1 | 32.0 |
| Other | 4.7 | 4.5 | −5.0 | 4.4 | 4.6 |
| Provider type**** | |||||
| Specialty MH prescriberb | 10.5 | 11.2 | 5.9 | 11.9 | 10.2 |
| Nonprescribing MH specialistc | 72.6 | 70.7 | −3.3 | 68.5 | 74.0 |
| Other provider or unspecified | 16.9 | 18.1 | 6.2 | 15.7 | 14.4 |
source Authors’ analysis of Office Ally administrative claims data. notes Monthly average outpatient mental health (MH) encounters before (March–December 2016–18) and during (March–December 2020) the COVID-19 pandemic among specific population and condition groups, along with the relative proportion of total encounters made up by in-person versus telehealth modalities in 2020. Data for 2019 were not available from the Office Ally database, as explained in the text. Relative proportions of in-person versus telehealth visits are not shown for 2016–18 because of the stable small numbers of telehealth encounters (accounting for approximately 0.1% of average monthly visits). Changes in the absolute number of encounters between the two periods are also displayed. The number of unique average monthly encounters is shown in the column headings in parentheses; these are the numbers on which the percentages are based. “Percent change, 201 6–18” values are calculated from the number of visits, which are not shown in this exhibit but can be found in appendix exhibit A3, which is the full version of the exhibit (see note 13 in text). p value levels based on chi-square test for significant differences in average percent of visits in person versus telehealth for each group during March–December 2020.
Not applicable.
Psychiatrists, mental health nurse practitioners, and mental health physician assistants.
Therapists and counselors, clinical nurse specialists, psychologists, and social workers.
p < 0.001
There was also variation in the degree to which telehealth services use increased within groups. For example, telehealth encounters for schizophrenia made up a lower proportion of total outpatient encounters relative to in-person visits (1.7 percent versus 2.7 percent) in 2020 (exhibit 3). In comparison, for people with anxiety and fear-related disorders, telehealth visits made up a higher proportion of total outpatient encounters in 2020 than did in-person visits (27.5 percent versus 25.5 percent). In addition, in 2020 telehealth uptake was higher, relative to in-person encounters, among nonprescribing mental health specialists (74.0 percent versus 68.5 percent) than among specialty mental health prescribers (10.2 percent versus 11.9 percent) and other providers (14.4 percent versus 15.7 percent). These differences in the distribution of telehealth and in-person encounters, relative to average total monthly outpatient volume, were significant (p < 0:001 for all).
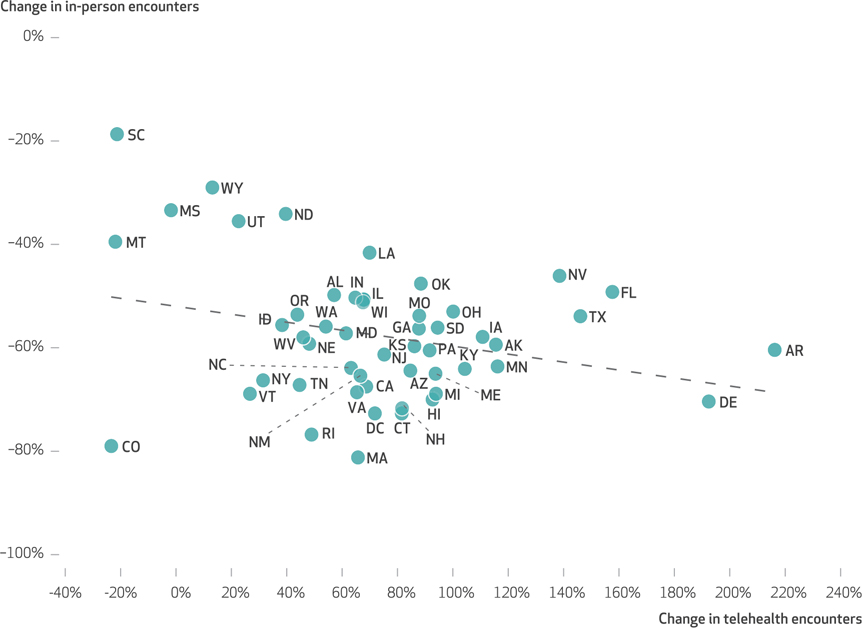
Exhibit 4 displays the association between changes in telehealth uptake versus in-person services use at the state level before and during the pandemic. At the state level, as the volume of in-person encounters decreased from March to December 2020, the volume of telehealth encounters increased, suggesting that to some extent, telehealth uptake may have served as a substitute for in-person care.
Exhibit 4. US state-level association between change in telehealth outpatient mental health encounters and change in in-person encounters, March–December 2020.
source Authors’ analysis of Office Ally administrative claims data. notes State-level plots of relative changes in the volume of telehealth outpatient mental health encounters during March–December 2020 against relative changes in in-person encounters during this period. Overall, the declining number of in-person encounters was associated with an increase in telehealth encounters (correlation coefficient, −0.28; p = 0.046).
Discussion
Using administrative claims data, we found substantial declines in in-person mental health services use in the initial lockdown phase of the COVID-19 pandemic, followed by a rapid rebound in utilization volume driven chiefly by uptake of telehealth appointments. These findings are consistent with early reports of declining outpatient and non-COVID-19-related health care use across a number of conditions.17,18 Temporary regulatory waivers and expanded reimbursement for telehealth coverage across payers likely facilitated this care delivery shift.19 We also found relative reductions in encounter volume for certain groups of mental health conditions, specifically for serious mental illnesses such as bipolar and mood disorders and schizophrenia and psychotic disorders, whereas encounters for anxiety and fear-related disorders rose slightly. In 2020 people with schizophrenia also had lower composition of telehealth encounters as a proportion of total outpatient encounters compared to people with other conditions.
Our data suggest that although telehealth uptake helped bridge access during the pandemic, the volume of encounters dropped for certain conditions, such as bipolar disorder and schizophrenia, in part because of relatively lower telehealth uptake among these groups. There are several reasons why we may have observed these utilization patterns, including differences in how telehealth modalities are used across populations. For example, older adults, Black and Hispanic people, people living alone,20 and people with lower incomes and poorer self-reported health status are less likely to access telehealth.21,22 A growing body of literature suggests inequitable uptake across communities in universal broadband and other critical technology infrastructure.20,22 Similarly, it is also possible that although telehealth is acceptable to many people with serious mental illness,23 some may experience discomfort or challenges engaging with this modality.
It is also unclear whether our observed trends in mental health services use were limited to people already connected to care. Some observers have expressed concerns that telehealth is more likely to supplement and complement in-person care among those who already receive mental health services instead of expanding access to those who otherwise are unable to obtain in-person care.24 One study from a single large health system found that the number of established mental health patient visits was stable between 2019 and 2020 but that the number of new patient visits dropped significantly.25 It remains to be seen whether certain groups have been more likely to delay or forgo mental health care altogether and, if so, how the associated downstream effects will manifest. As telehealth care delivery continues to grow, strategies will need to be developed and studied to improve the accessibility and acceptability of services among people with more serious mental health comorbidities. Given the rise in mental health care demand resulting from the pandemic and the need for increased access among a broad swath of patients, understanding how telehealth can expand services while maintaining access for those already engaged with the health care system will be equally important.
On the whole, our findings on telehealth uptake for mental health conditions are consistent with recent estimates that suggest rapid and substantial adoption in mental health services delivery, particularly when compared with medical and surgical care.14 Telehealth may be uniquely suited to mental health services delivery for a number of reasons. First, prepandemic, there was already a robust evidence base supporting the mental health telehealth expansion, especially to improve access to care for the 119 million Americans who live in a Mental Health Care Health Professional Shortage Area.24,26 A recent study by Michael Barnett and coauthors, for instance, showed slow but sustained growth in telehealth use among rural Medicare enrollees, particularly for mental health care.16 Second, therapy and counseling for mental health conditions do not typically require a detailed physical exam or laboratory testing. Third, studies also have demonstrated high acceptance of and satisfaction with telehealth for mental health services delivery among providers and patients for outcomes such as remote medication and symptom telemonitoring.27 Finally, additional barriers relevant to other conditions (for example, opioid use disorder), including federal and state regulatory requirements, patient and clinician acceptance, and perceived differences in quality of care, may contribute to slower uptake in other clinical scenarios.
Our findings support the expectation that telehealth for mental health services delivery will be sustained even after the COVID-19 pandemic subsides. The pandemic accelerated the need for targeted policies that expand access to and improve delivery of mental health services, and there are growing calls by large US health systems to formally establish telehealth regulatory policies in this context.28 Furthermore, as clinicians have voiced a desire for payment parity between in-person and telehealth visits, supporting continued telehealth use will require greater scrutiny on how the postpandemic regulatory and payment landscape ought to be structured.29 Although reducing regulatory and payment barriers may improve access to care, increased reliance on telehealth could exacerbate existing health care disparities or worsen care outcomes for other populations, particularly if access to broadband internet is limited in some regions or unavailable to lower-income or clinically vulnerable populations. Future research is needed to understand how telehealth modalities can best improve equitable access to mental health care in the face of increased overall demand.
Supplementary Material
Acknowledgments
Jane Zhu received support from the National Institute of Mental Health (Grant No. 1K08MH123624). K. John McConnell also received support from the National Institute of Mental Health (Grant Nos. R01MH122199 and R01MH123416). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Jane M. Zhu, Oregon Health & Science University, Portland, Oregon.
Renae Myers, Oregon Health & Science University and Portland State University, Portland, Oregon..
K. John McConnell, Oregon Health & Science University..
Ximena Levander, Oregon Health & Science University..
Sunny C. Lin, Washington University in St. Louis, St. Louis, Missouri.
References
- 1.Panchal N, Kamal R, Cox C, Garfield R. The implications of COVID-19 for mental health and substance use [Internet]. San Francisco (CA): Henry. J. Kaiser Family Foundation; 2021. Feb 10 [cited 2022 Jan 28]. Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substanceuse/ [Google Scholar]
- 2.Bray MJC, Daneshvari NO, Radhakrishnan I, Cubbage J, Eagle M, Southall P, et al. Racial differences in statewide suicide mortality trends in Maryland during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Psychiatry. 2021; 78(4):444–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–2. [DOI] [PubMed] [Google Scholar]
- 5.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–8. [DOI] [PubMed] [Google Scholar]
- 6.Yu J, Hammond G, Waken RJ, Fox D, Joynt Maddox KE. Changes in non-COVID-19 emergency department visits by acuity and insurance status during the COVID-19 pandemic. Health Aff (Millwood). 2021;40(6): 896–903. [DOI] [PubMed] [Google Scholar]
- 7.Nason I, Stein DT, Frank RG, Stein MB. Decline in new starts of psychotropic medications during the COVID-19 pandemic. Health Aff (Millwood). 2021;40(6):904–9. [DOI] [PubMed] [Google Scholar]
- 8.Moss K, Wexler A, Dawson L, Long M, Kates J, Cubanski J, et al. The Coronavirus Aid, Relief, and Economic Security Act: summary of key health provisions [Internet]. San Francisco (CA): Henry J. Kaiser Family Foundation; 2020. Apr 9 [cited 2022 Jan 28]. Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/the-coronavirus-aid-relief-and-economic-security-act-summary-of-key-healthprovisions/ [Google Scholar]
- 9.Chu RC, Peters C, De Lew N, Sommers BD. State Medicaid telehealth policies before and during the COVID-19 public health emergency [Internet]. Washington (DC): Department of Health and Human Services, Office Of the Assistant Secretary for Planning and Evaluation, Office of Health Policy; 2021. Jul [cited 2022 Jan 28]. Available from: https://www.aspe.hhs.gov/sites/default/files/2021-07/medicaid-telehealth-brief.pdf [Google Scholar]
- 10.Demeke HB, Merali S, Marks S, Pao LZ, Romero L, Sandhu P, et al. Trends in use of telehealth among health centers during the COVID-19 pandemic—United States, June 26-November 6, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(7):240–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVID-19 Research Database [Internet]. [location unknown]: COVID-19 Research Database; [cited 2022 Jan 28]. Available from: https://covid19researchdatabase.org/ [Google Scholar]
- 12.Gryczynski J, Schwartz RP, O’Grady KE, Restivo L, Mitchell SG, Jaffe JH. Understanding patterns of high-cost health care use across different substance user groups. Health Aff (Millwood). 2016;35(1):12–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.To access the appendix, click on the Details tab of the article online.
- 14.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood). 2021; 40(2):349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charlesworth CJ, Zhu JM, Horvitz-Lennon M, McConnell KJ. Use of behavioral health care in Medicaid managed care carve-out versus carve-in arrangements. Health Serv Res. 2021; 56(5):805–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnett ML, Huskamp HA, Busch AB, Uscher-Pines L, Chaiyachati KH, Mehrotra A. Trends in outpatient telemedicine utilization among rural Medicare beneficiaries, 2010 to 2019. JAMA Health Forum. 2021; 2(10):e213282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cox C, Amin K, Kamal R. How have health spending and utilization changed during the coronavirus pandemic? [Internet]. New York (NY): Peterson-KFF Health System Tracker; 2021. Mar 22 [cited 2022 Jan 28]. Available from: https://www.healthsystemtracker.org/chart-collection/how-have-healthcare-utilization-and-spending-changed-so-far-during-the-coronavirus-pandemic/ [Google Scholar]
- 18.Mehrotra A, Chernew ME, Linetsky D, Hatch H, Cutler DA. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges [Internet]. New York (NY): Commonwealth Fund; 2020. May 19 [cited 2022 Jan 28]. Available from: https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits [Google Scholar]
- 19.Centers for Medicare and Medicaid Services [Internet]. Baltimore (MD): CMS. Press release, Trump administration issues second round of sweeping changes to support U.S. healthcare system during COVID-19 pandemic; 2020. Apr 30 [cited 2022 Jan 28]. Available from: https://www.cms.gov/newsroom/pressreleases/trump-administrationissues-second-round-sweepingchanges-support-us-healthcare-system-during-covid [Google Scholar]
- 20.Lam K, Lu AD, Shi Y, Covinsky KE. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med. 2020; 180(10):1389–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tse J, LaStella D, Chow E, Kingman E, Pearlman S, Valeri L, et al. Telehealth acceptability and feasibility among people served in a community behavioral health system during the COVID-19 pandemic. Psychiatr Serv. 2021;72(6):654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel SY, Rose S, Barnett ML, Huskamp HA, Uscher-Pines L, Mehrotra A. Community factors associated with telemedicine use during the COVID-19 pandemic. JAMA Netw Open. 2021;4(5):e2110330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bashshur RL, Shannon GW, Bashshur N, Yellowlees PM. The empirical evidence for telemedicine interventions in mental disorders. Telemed J E Health. 2016;22(2): 87–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehrotra A, Huskamp HA, Souza J, Uscher-Pines L, Rose S, Landon BE, et al. Rapid growth in mental health telemedicine use among rural Medicare beneficiaries, wide variation across states. Health Aff (Millwood). 2017;36(5):909–17. [DOI] [PubMed] [Google Scholar]
- 25.Ridout KK, Alavi M, Ridout SJ, Koshy MT, Harris B, Dhillon I, et al. Changes in diagnostic and demographic characteristics of patients seeking mental health care during the early COVID-19 pandemic in a large, community-based health care system. J Clin Psychiatry. 2021; 82(2):20m13685. [DOI] [PubMed] [Google Scholar]
- 26.Henry J Kaiser Family Foundation. Mental Health Care Health Professional Shortage Areas (HPSAs) [Internet]. San Francisco (CA): KFF; 2021. Sep 30 [cited 2022 Jan 28]. Available from: https://kff.org/other/state-indicator/mental-health-care-health-professional-shortage-areas-hpsas/?currentTimeframe=0&selectedRows=%7B%22wrapups%22:%7B%22united-states%22:%7B%7D%7D%7D [Google Scholar]
- 27.Lawes-Wickwar S, McBain H, Mulligan K. Application and effectiveness of telehealth to support severe mental illness management: systematic review. JMIR Ment Health. 2018;5(4):e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lau J, Knudsen J, Jackson H, Wallach AB, Bouton M, Natsui S, et al. Staying connected in the COVID-19 pandemic: telehealth at the largest safety-net system in the United States. Health Aff (Millwood). 2020;39(8):1437–42. [DOI] [PubMed] [Google Scholar]
- 29.Mehotra A, Wang B, Snyder G. Telemedicine: what should the post-pandemic regulatory and payment landscape look like? [Internet]. New York (NY): Commonwealth Fund; 2020. Aug 5 [cited 2022 Jan 28]. Available from: https://www.commonwealthfund.org/publications/issue-briefs/2020/aug/telemedicine-post-pandemic-regulation [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.