Abstract
Trajectory studies of the COVID-19 pandemic have described patterns of symptoms over time. Yet, few have examined whether social determinants of health predict the progression of depression and anxiety symptoms during COVID-19 or identified which social determinants worsen symptom trajectories. Using a racially, ethnically, and linguistically diverse sample of adults participating in a randomized clinical trial with pre-existing moderate to severe depression and/or anxiety symptoms, we compare symptom patterns before and during COVID-19; characterize symptom trajectories over a 20-week follow-up period; and evaluate whether social determinants are associated with within- and between- person differences in symptom trajectories. Data were collected before and during COVID-19 in Massachusetts and North Carolina. On average, depression and anxiety symptoms did not seem to worsen during the pandemic compared to pre-pandemic. During COVID-19, anxiety scores at follow-up were higher for participants with baseline food insecurity (vs no food insecurity). Depression scores at follow-up were higher for participants with food insecurity and for those with utilities insecurity (vs no insecurity). Participants with child or family care responsibilities at baseline had depression symptoms decreasing at a slower rate than those without these responsibilities. We discuss the important implications of these findings.
Keywords: COVID-19, Depression, Anxiety, Trajectories, Social determinants of health, Racial/ethnic minorities
1. Introduction
In many countries, including the United States, the 2020 prevalence rates for anxiety and depression symptoms during the start of the COVID-19 pandemic doubled or more than doubled compared to previous years (OECD, 2021). Banks et al. (2021) hypothesize how the pandemic directly and indirectly contributes to increases in depression and anxiety through four potential mechanisms: 1) health-related anxiety and grief directly arising from the COVID-19 virus; 2) the direct mental health effects of the loss or restriction of fulfilling activities and positive social connections; 3) the mental health consequences of the pandemic's effect on an individual's financial situation; and 4) stressors related to domestic arrangements and family relations (Banks et al., 2021). However, mechanisms through which the pandemic has augmented anxiety and depression symptoms appear to differ across and within individuals over time. Studies consistently show higher overall prevalence and severity of depression and anxiety symptoms among people who are younger, female, of lower-socio-economic status, and with pre-existing mental health needs (Kwong et al., 2021; Vindegaard & Benros, 2020). Drawing on literature from systemic models of human development and family functioning, Prime et al. (2020) illustrate how families and individuals with greater exposure to vulnerabilities prior to COVID-19 (e.g., economic hardship, racism and marginalization, past traumatic events) are at greater risk for depression and anxiety symptoms from social disruption due to the COVID-19 pandemic (e.g., job loss, social isolation) (Prime et al., 2020). Likewise, certain protective factors prior to COVID-19 (e.g., economic security, family social support) put families and individuals in a better position to adapt to social disruption during the pandemic and maintain mental health (Prime et al., 2020). These patterns of greater risk and protection are consistent with research findings from previous pandemics and disasters (Goldmann & Galea, 2014; Quinn & Kumar, 2014).
Yet, whether those at greater risk recover or not, and how social determinants of health (SDH) might influence mental health symptom recovery are remaining questions. Study samples in this literature have been predominantly White (Batterham et al., 2021), inclusive of the general population with low mental health symptoms (Saunders et al., 2021), at low risk of COVID-19 infection and low risk of economic insecurity (Thomas et al., 2021). Studies of people with pre-existing anxiety or depression prior to the pandemic often have small samples and/or rely on mostly convenience sampling (Banks et al., 2021). Many of the studies with larger samples have cross-sectional designs, or include only two-three points of observation, and have not assessed social determinants needs during the pandemic.
In the present study, we used data from participants enrolled in the ongoing Strong Minds-Strong Communities randomized clinical trial (RCT), a predominantly racially/ethnically and linguistically diverse and low-income sample with pre-existing depression and/or anxiety from North Carolina and Massachusetts. The goals of the current study are threefold: (1) to test the hypothesis that participants enrolled in the RCT before the COVID-19 pandemic would have on average lower depression and anxiety symptoms compared to participants enrolled during the pandemic (Goal 1), (2) to examine whether depression and anxiety symptoms were stable, increasing, or decreasing during the pandemic within and between individuals (Goal 2); and (3) to test the hypothesis that participants negatively impacted by SDH, minority stress (i.e. discrimination), COVID stress (e.g., personal/family exposure or conflict due to COVID) and with certain sociodemographic and clinical characteristics (e.g., non-married, higher symptoms) would have worse trajectories of depression and anxiety symptoms during the pandemic (Goal 3). Together, these findings could inform our understanding of the clinical and social service needs during a pandemic among a raciallly/ethnically and linguistically diverse population with pre-existing moderate to severe depression and anxiety symptoms.
A unique contribution of our study is to examine the independent contribution of unmet basic needs to depression and anxiety trajectories in a racially and ethnically diverse population of adults with pre-existing mental health diagnoses. The participants included in both the Saunders and Batterham studies were mostly White, and most did not have mental health diagnoses pre-pandemic. Both of these studies demonstrated that the few participants who did have pre-existing mental health diagnoses had worse depression and anxiety trajectories than participants without mental health diagnoses, as would be expected. In our study, all participants met diagnostic-level criteria for depression or anxiety at baseline, and therefore we were able to examine the role of unmet basic needs in depression and anxiety symptom trajectories in a high-risk population.
1.1. What do we know about symptoms of depression and anxiety during the pandemic in the general population and in samples with pre-existing symptoms?
Recent studies in nationally representative samples across the world (Batterham et al., 2021; Fancourt et al., 2021; Saunders et al., 2021) report that the levels of symptoms of anxiety and depression peaked in March 2020 when lockdown was initiated, with a slow decline in the following months (Banks et al., 2021). In a longitudinal study (Shuster et al., 2021), people with previous mental health diagnoses experienced higher and increasing levels of symptoms during the pandemic. Nevertheless, different sources of mental health concerns during the pandemic are likely to have different time horizons (i.e., different shaped curves).
1.2. Trajectories of anxiety and depression symptoms during the pandemic
Researchers have identified distinct trajectories of symptoms for anxiety and depression during the COVID-19 pandemic. Banks et al. (2021) illustrated this with four different curves: a curve of those with immediate fear and response to lockdown (sharp spike and quick recovery); a curve for those having a response to pandemic adversities (starts later and ends later); insufficient mental health support (starts later and takes longer to recover); and mental health impacts of long-term consequences of the pandemic like recession, unrest, and poverty (delayed and large curve with no indication of decline). In Australia, Batterham et al. (2021) identified three trajectory classes for depression (stable low, stable moderate, or severe and declining) and four for anxiety (stable low, mild increasing, moderate increasing, and moderate declining) (Batterham et al., 2021). In the United Kingdom, Saunders et al. (2021) found that the most common pattern for depression and anxiety symptoms was low symptom severity throughout, while others had severe increasing; moderate throughout; worsening associated with lockdown; or severe initial anxiety that decreased quickly after lockdown (Saunders et al., 2021). It remains unanswered how the pandemic influenced trajectories for those who had significant mental health symptoms and were participating in a psychosocial program, and whether social and economic difficulties (either specific issues like housing or greater total number of difficulties) predict the progression of an individual's anxiety and depression symptoms over time.
1.3. Role of social determinants of health in symptom trajectories
Social determinants of health (SDH) can contribute to increased rates of depression and anxiety symptoms during the COVID-19 pandemic by loss of employment or income (Solomou & Constantinidou, 2020; Zhang et al., 2020); housing instability (Bushman & Mehdipanah, 2021); concerns about accessing basic needs such as paying for food, medications, and utilities (Wright et al., 2020); responsibilities of caring for children or other family members (Adams-Prassl et al., 2020); and decreased social interactions (Etheridge & Spantig, 2020). Longitudinal research from the United Kingdom indicates that in the first month of the pandemic, people with lower socioeconomic position experienced a greater number of these adverse events (Wright et al., 2020), and that these experiences had a greater impact on mental health among people from lower-income households compared to higher-income households (Banks & Xu, 2020); a finding consistent with data from the U.S. (Soria & Horgos, 2020). However there have been few longitudinal studies of this nature in the U.S.
Prior research both before and during the pandemic has demonstrated that unmet basic needs, particularly food insecurity, can worsen depression and anxiety independent of income (Jones, 2017; Liu et al., 2014; McAuliffe et al., 2021; Nagata et al., 2021). Yet none of the basic needs factors alone is enough to explain the negative impact of the COVID-19 pandemic on mental health for any subgroup. For example, Adams-Prassl and colleages (2020) found that the increased financial worries and childcare responsibilities only accounted for part of the effect of lockdown on women's mental health.
Several studies have examined whether certain demographic factors can help predict which symptom trajectory class an individual would most likely experience during the COVID-19 pandemic. Shuster et al. (2021) found that age, gender, ethnicity, income, prior diagnoses, living situation, personality factors and sociability predicted different trajectories. Batterham (2021) identified that prior mental health diagnoses, Covid-19 related financial distress, and social and work impairment were all associated with having a high symptom trajectory. Shuster et al. (2021) reported that Covid-19-related economic impact and increase in projected duration of the pandemic exacerbated depression and anxiety symptoms over time, increasing Covid-19 severity (7-day change in cases).
These studies provide some understanding of social determinants as predictors of mental health trajectories. Fewer studies have identified relationships between social needs and trajectories of depression and anxiety during the pandemic. Saunders et al. (2021) found that income and living situation were associated with different trajectories – individuals with lower incomes experienced higher levels of depression and anxiety symptoms that increased at a faster rate than people with higher incomes. Fancourt et al. (2021) found that educational attainment was associated with different trajectories – individuals with lower educational attainment started with higher levels of depressive symptoms and they declined at a different pace than those with higher levels of educational attainment. Additionally, some studies have identified relationships between social needs measured during the pandemic and trajectories of depression and anxiety during the pandemic. One longitudinal study from New York found that adolescents and young adults with greater concerns about basic needs (not having enough food or supplies) reported greater anxiety symptoms (Hawes et al., 2021). They suggested that basic SDH might have a greater impact on the mental health of adults who have more responsibilities.
The current study focuses on the role of SDH (e.g., housing instability, food insecurity, transportation difficulties, utility assistance needs) included in standardized screening tools for clinical settings (Billioux et al., 2017). We evaluate how SDH might impact the trajectories of depression and anxiety symptoms in a mostly racially/ethnically minoritized group of people already identified to have elevated depression and anxiety symptoms. In addition to these social determinants, we also examined the effect of perceived changes in family social needs specifically due to the pandemic (e.g., loss of household income or responsibilities in childcare) as past studies have found associations between COVID-19 family stressors and mental health symptoms (Brown et al., 2020). Another important social need is living in settings that feel welcoming and supportive (Ahrens et al., 2021; Pedrosa et al., 2020), so we examined the role of neighborhood minority stress as contributing to mental health trajectories. Examining which social needs lead to greater vulnerability in depression and anxiety symptoms among low-income minoritized populations can help identify what needs should be prioritized to reduce mental health challenges and preventively provide support for these services.
2. Methods
2.1. Participants
The ongoing Strong Minds-Strong Communities study is an RCT of an evidence-based psychosocial intervention offered to adults in North Carolina and Massachusetts (Alegría et al., 2019). The intervention is transdiagnostic, addressing moderate to severe depression, anxiety, and trauma-related symptoms through a manualized program of 10 sessions within 6 months. It is delivered virtually by mostly multilingual community health workers (CHWs), and offered in English, Spanish, Mandarin, and Cantonese. A care manager also provides linkages for SDH. Eligible participants were adults ages 18 years or older with demonstrated capacity to consent, and who had elevated symptom levels of depression or anxiety on the CAT-MH, a suite of validated computer adaptive tests for assessing mental health (Gibbons et al., 2018). The CAT-MH was calibrated by the developer for the current and future studies, to ensure accuracy across the study languages and congruence with commonly used measures such as the PHQ-9 (Kroenke et al., 2001). Moderate to severe symptoms were defined by a cut-off score of 50 for depression and 51 for anxiety in English-speakers, and of 42 for depression and 41 for anxiety in Spanish, Mandarin, or Cantonese speaking participants. Participants were excluded if they received psychotherapy or counseling in the three months prior to enrollment or had an appointment upcoming in the next month. We did not exclude participants for use of pharmacological treatments and related appointments with a psychiatrist. We also excluded participants with a history of psychosis, mania, psychotic symptoms (using the IMPACT screener)(Callahan et al., 2005), or severe alcohol or substance dependance as defined by the CAT-MH (Gibbons et al., 2018). Participants reporting a suicidal plan or attempt on the Paykel Suicide Risk Questionnaire (Paykel et al., 1974) took part in an emergency protocol and were rescreened 30-days after for potential eligibility.
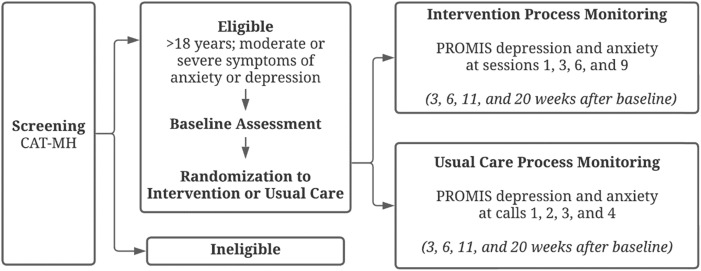
Most participants were economically disadvantaged, from racially or ethnically minoritized groups, and non-English speakers. After screening, participants completed a baseline assessment prior to randomization into either the intervention or enhanced usual care (EUC) condition. We additionally monitored anxiety and depression symptoms as part of intervention activities in both arms of the trial, which are the data utilized for the current analysis. These were monitored at approximately 3-, 6-, 11-, and 20-weeks post-baseline. The RCT monitoring process is presented in Fig. 1 . Follow-up questionnaires were administered at 3-, 6-, and 12-months post-baseline but were not used in the current analyses, as the trial is ongoing and data collection is not yet complete. All measures were administered by staff trained in data collection procedures. The study was approved by the appropriate Institutional Review Boards.
Fig. 1.
Study process monitoring flowchart.
2.2. Measures
2.2.1. Hypothesized baseline characteristics associated with symptom trajectories
Sociodemographic factors. Sociodemographic variables included gender (female vs male), age, marital status (married or cohabitating vs separated, widowed, divorced, or never married), and education (above high school vs at or below high school).
Social Determinants of Health (SDH). This self-report measure is an adaptation of the Accountable Health Communities Screening Tool for Health-Related Social Needs (Billioux et al., 2017) specific to populations served by Medicaid Accountable Care Organizations in Massachusetts and North Carolina. It was further customized to incorporate concerns of RCT participants and the services available in their communities. We used this measure to create 8 indicator variables for past 12-month difficulties with Lack of Transportation (1-item: transportation kept you from medical appointments or getting medication), Food Insecurity (2-items: worrying sometimes or often about food running out or not having enough money to buy more food), Housing Instability (3-items: lack of housing, moving two or more times in the past-year, or worrying about not having housing in the next two months), Utilities Insecurity (1-item: trouble paying heat or electric bill), Trouble Paying for Medications (1-item), Unemployment (1-item: currently unemployed and looking for work), Interest in More Education (1-item: “Are you interested in more education?“), and Childcare/Family Care Insecurity (1-item: trouble with childcare or the care of a family member). Each domain was analyzed separately and by a count variable for Total Number of Social Determinants of Health (range: 0–8). The full measure is presented in the Appendix.
COVID-19 Family Stress. The COVID-19 Family Stress Screener (Huth-Bocks, 2020) is a 10-item measure assessing increased stress from COVID-19 related events (1 = strongly disagree to 5 = strongly agree) within different domains of daily living such as “physical health concerns for me or a family member” or “loss of social connections and social isolation”. Although five items overlapped with social needs domains from the SDH measure (e.g., losing job or decrease in income) they were not excluded since they were reported in relation to COVID-19 related events. Total scores were calculated summing all items (range: 10–50), with greater scores indicating higher levels of stress (α = 0.81 overall, and 0.75, 0.84, 0.78, and 0.83 in English, Spanish, Mandarin, and Cantonese, respectively).
Minority Stress. We used a 4-item adaptation (Duarte et al., 2021) of the Minority Status Stress Scale (Smedley et al., 1993). Participants are instructed to think about their current neighborhood, and select a response from a 4-point scale (0 = strongly disagree to 3 = strongly agree) to each of the following four statements: “You can perceive/notice negative attitudes/treatment of people like you by your neighbors”; “The neighborhood is an unfriendly place for people like you”; “In this neighborhood people like you are not treated nicely”; and “People like you do not feel at home in this neighborhood”. All items were summed to create a total score (range: 0–12) with higher scores reflecting higher levels of minority stress (α = 0.81 overall, and 0.75, 0.84, 0.78, and 0.83 in English, Spanish, Mandarin, and Cantonese, respectively).
2.2.2. Outcomes: anxiety and depression symptoms
Approximately 3-, 6-, 9-, and 20-weeks post-baseline, anxiety and depression symptoms were measured using the short-forms of the Patient Reported Outcomes Measurement Information System (PROMIS) (Cella et al., 2010). The PROMIS anxiety module measures past seven days self-reported emotional distress caused by fear, anxious misery, hyperarousal, and somatic symptoms related to arousal (Pilkonis et al., 2011). The short-form assesses how often the respondent has been bothered by each of the following seven symptoms: “I felt fearful”, “I felt anxious”, “I felt worried”, “I found it hard to focus on anything other than my anxiety”, “I felt nervous”, “I felt uneasy” and “I felt tense”; r = 0.96 with the full 29-item PROMIS anxiety bank (Cella et al., 2010). Each item is rated on a 5-point scale (1 = never and 5 = always), which add up to a total score ranging from 7 to 35; α = 0.88 total, and 0.87, 0.89, 0.89, and 0.90 in English, Spanish, Mandarin, and Cantonese, respectively.
The PROMIS depression module measures past seven days self-reported affective and cognitive manifestations of depression rather than somatic symptoms such as appetite, fatigue, and sleep (Pilkonis et al., 2011). The short-form assesses how often the respondent has been bothered by each the following eight symptoms: “I felt worthless”, “I felt that I had nothing to look forward to”, “I felt helpless,” “I felt sad,” “I felt like a failure,” “I felt depressed,” “I felt unhappy,” and “I felt hopeless”; r = 0.96 with the full 28-item PROMIS depression bank (Cella et al., 2010). Each item is rated on a 5-point scale (1 = never and 5 = always), which add up to a total score ranging from 8 to 40; with an α = 0.89 for the total sample, and 0.86, 0.90, 0.89, and 0.90 in English, Spanish, Mandarin, and Cantonese, respectively.
PROMIS scores were measured among intervention participants during their intervention sessions with CHWs, and among EUC participants during calls with a Care Manager that were scheduled at similar time periods. Analyses for Goal 1 used PROMIS scores at first measurement (i.e., 3-weeks post-baseline) as the outcome, while analyses for Goals 2 and 3 used PROMIS scores at all time points (3-, 6-, 11-, and 20-weeks post-baseline) as the outcome.
2.2.3. Additional descriptive characteristics
Descriptive baseline information included state of recruitment (Massachusetts or North Carolina), race/ethnicity (non-Latinx White, non-Latinx Black, Asian, Latinx, American Indian, and multiracial), and anxiety and depression symptoms. Consistent with required reporting for NIH and general census guidelines, there were two separate questions for participants to self-report race and ethnicity. Pre-existing anxiety and depression symptoms were assessed during screening for trial eligibility through the CAT-MH (Gibbons et al., 2018).
2.3. Analytical samples
Between September 25, 2019 (date when the first participant was enrolled) and November 3, 2021, a total of 804 participants were enrolled in the RCT. For Goal 1, the analytic sample included all current 804 enrolled participants, 94 of whom completed their first PROMIS measures (i.e., 3-weeks post-baseline) before the COVID-19 pandemic (March 15, 2020), and 710 of whom completed their first PROMIS measures during the pandemic (on or after March 15, 2020). For Goals 2 and 3, participants who enrolled in the trial before the pandemic (N = 151) or who enrolled in the trial less than 6 months before November 3, 2021 (N = 147) were excluded, resulting in a final analytic sample of 504 participants for Goals 2 and 3. Although 151 participants enrolled before the pandemic, the first exclusion criteria were applied because only 5 of them had completed all of their PROMIS measures pre-pandemic, which did not allow us to compare trajectories of anxiety and depression pre- and during the pandemic. The second exclusion criteria were applied because participants can complete all their PROMIS measures only when enrolled in the trial for about six months.
2.4. Statistical analyses
For Goal 1, we examined the average differences in the first PROMIS anxiety and depression scores (i.e., 3-weeks post-baseline) before and during the pandemic using a local linear function and we plotted anxiety and depression scores against the date the scores were completed. For Goals 2 and 3, we compared the distribution of baseline characteristics between participants included in the trajectory analyses (N = 504) and participants excluded from these analyses (N = 298) because they either enrolled in the trial before the pandemic or had not reached the six-month period of observation in the trial. We then used multilevel growth models to assess how anxiety and depression symptoms changed over time (Goal 2) and how that change was related to baseline sociodemographic factors, social determinants of health, COVID-19 family stress, and minority stress (Goal 3). These models fitted the symptoms scores at each time point (3-, 6-, 11-, and 20-weeks post-baseline) as a function of linear and quadratic time, with assessment time centered at 3-weeks.
For Goal 2, we started with a model that included an intercept as a fixed- and random-effect and linear time as a fixed-effect (Model 1). The intercept fixed-effect captured average symptoms at the first measurement (i.e., 3-weeks post-baseline), the linear time fixed-effect captured average linear rate of change over time, and the intercept random-effect captured individual variability in symptoms at the first measurement. We then added random-effects for the linear time to capture individual variability in the linear rate of change over time (Model 2). Finally, we added a quadratic term for time to test for deviations from linearity (Model 3), but we could not include a random-effect for this quadratic term because it was not empirically identified in our data. We used a likelihood ratio test to select the best-fitting model.
Using the best-fitting model from Goal 2, we then added baseline characteristics and their two-way interaction with linear time as fixed-effects (Goal 3). The fixed-effect for baseline characteristics represented the average difference in symptoms at first measurement between participants with and without a specific baseline characteristic (e.g., with and without food insecurity). The fixed-effect for the two-way interactions represented the average difference in the linear rate of change over time as a function of baseline characteristics. To focus on the overall effect of each characteristic, we included each separately without adjusting for other characteristics. All models adjusted for intervention condition and state of recruitment (North Carolina or Massachusetts), but the intervention was not analyzed since the RCT is still ongoing. All analyses were conducted in Stata Version 15 (StataCorp, 2021).
3. Results
3.1. Goal 1: Differences in initial anxiety and depression symptoms pre- and during the pandemic
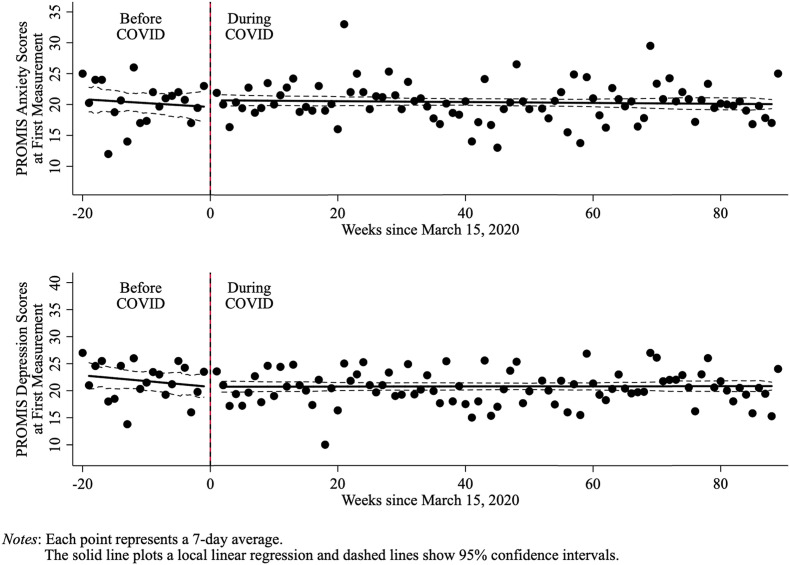
In Fig. 2 , we plotted PROMIS anxiety and depression scores at first measurement (i.e., 3-weeks post-baseline) against the date when the scores were taken and used a local linear function that distinguished pre- and during pandemic periods. The dashed lines represent 95% confidence intervals (95% CIs). The figure shows that neither anxiety nor depression scores increased after the first monitoring period (3-weeks post-baseline) when the pandemic started (March 15, 2020). That is, the pandemic did not seem to worsen anxiety and depression symptoms among RCT participants who were already moderately to severely anxious or depressed at baseline.
Fig. 2.
Mean anxiety and depression PROMIS scores at first measurement (3-weeks post-baseline) before and during the COVID-19 pandemic.
3.2. Goal 2: Anxiety and depression symptom change over time, adjusting for treatment condition
Descriptive information of participants included in our trajectory analyses are displayed in Table 1 . Participants were on average 45 years old, with the sample being mostly female and Latinx. No differences were observed between participants included and excluded from the trajectory analyses. Results from our multilevel growth models of anxiety and depression symptom change over time are presented in Table 2 . As shown in this table, for both outcomes Model 2 had better fit than Model 1, and Model 3 had better fit than Model 2. That is, the best-fitting model for both anxiety and depression was Model 3, which included fixed effects for the intercept, linear time, and quadratic time, as well as random effects for the intercept and linear time. Thus, we focused our interpretation on the effects estimated in Model 3.
Table 1.
Baseline characteristics of overall study participants (Goal 1), participants excluded from goals 2 and 3, and analytical sample for goals 2 and 3.
| Baseline characteristic | Overall: Goal 1 |
Excluded from Goals 2 and 3 |
Analytical Sample for Goals 2 and 3 |
P Value |
|---|---|---|---|---|
| (N = 804) | (N = 298) | (N = 506) | ||
| Age, years, mean (SD) | 44.4 (13.4) | 44.0 (13.7) | 44.6 (13.2) | 0.55 |
| Gender, N (%) | ||||
| Male | 126 (15.7) | 47 (15.8) | 79 (15.6) | 0.86 |
| Female | 674 (83.8) | 249 (83.6) | 425 (84.0) | |
| Other | 4 (0.5) | 2 (0.7) | 2 (0.4) | |
| Race/ethnicity, N (%) | ||||
| White | 67 (8.3) | 16 (5.4) | 51 (10.1) | <0.001 |
| Black | 100 (12.4) | 59 (19.8) | 41 (8.1) | |
| Asian | 110 (13.7) | 40 (13.4) | 70 (13.8) | |
| Latinx | 511 (63.6) | 174 (58.4) | 337 (66.6) | |
| Other | 16 (2.0) | 9 (3.0) | 7 (1.4) | |
| Education, N (%) | ||||
| Less than high school | 556 (69.2) | 204 (68.5) | 352 (69.6) | 0.89 |
| High school and above | 246 (30.6) | 93 (31.2) | 153 (30.2) | |
| Missing | 2 (0.2) | 1 (0.3) | 1 (0.2) | |
| Marital Status, N (%) | ||||
| Married or cohabitating | 366 (45.5) | 150 (50.3) | 216 (42.7) | 0.07 |
| Separated, divorced, widowed, or never married | 436 (54.2) | 148 (49.7) | 288 (56.9) | |
| Missing | 2 (0.2) | 0 (0.0) | 2 (0.4) | |
| State, N (%) | ||||
| North Carolina | 348 (43.3) | 129 (43.3) | 219 (43.3) | 1.00 |
| Massachusetts | 456 (56.7) | 169 (56.7) | 287 (56.7) | |
| Condition, N (%) | ||||
| Control | 397 (49.4) | 145 (48.7) | 252 (49.8) | 0.75 |
| Intervention | 407 (50.6) | 153 (51.3) | 254 (50.2) | |
| CAT-MH Anxiety, mean (SD) | 51.7 (17.8) | 50.8 (17.4) | 52.2 (18.1) | 0.25 |
| CAT-MH Depression, mean (SD) | 57.2 (12.7) | 58.0 (12.5) | 56.8 (12.8) | 0.22 |
| Total Number of Social Determinants of Health, mean (SD) | 3.0 (1.9) | 3.0 (1.9) | 3.0 (1.9) | 0.67 |
| COVID-19 Family Stress Screener, mean (SD)a | 34.2 (8.8) | 33.2 (8.4) | 34.5 (8.9) | 0.13 |
| Minority stress | 5.7 (1.4) | 5.7 (1.4) | 5.6 (1.4) | 0.22 |
Measure was collected for the first time on April 6th, 2020, and thus missing for 192 participants (152 enrolled pre-pandemic, and 40 enrolled between March 15th, 2020, and April 5th, 2020).
Table 2.
Multilevel models of PROMIS anxiety and depression scores change during the COVID-19 pandemic.
| Random Effects Model | Fixed-part Estimates, Coeff. [95% CI] |
Random Effects Variances, Coeff. [95% CI] |
Model Comparison, χ2(1) [p-value] | |||
|---|---|---|---|---|---|---|
| Intercept | Slope (Time) | Slope Squared | Intercept | Slope (Time) | ||
| PROMIS Anxiety | ||||||
| 1. Intercept | 19.99 [19.39, 20.58] | −0.23 [-0.27, −0.20] | 23.62 [19.82, 28.14] | 1 vs. linear model, 455.63 [<0.001] | ||
| 2. Intercept and slope | 19.89 [19.31, 20.47] | −0.23 [-0.27, −0.19] | 22.98 [19.19, 27.51] | 0.04 [0.02, 0.07] | 2 vs. 1, 15.43 [<0.001] | |
| 3. Intercept and slope (Fixed slope squared) | 20.42 [19.81, 21.03] | −0.56 [-0.68, −0.43] | 0.02 [0.01, 0.03] | 23.23 [19.43, 27.76] | 0.04 [0.02, 0.07] | 3 vs. 2, 27.20 [<0.001] |
| PROMIS Depression | ||||||
| 1. Intercept | 20.38 [19.71, 21.04] | −0.25 [-0.29, −0.21] | 30.92 [26.05, 36.71] | 1 vs. linear model, 497.29 [<0.001] | ||
| 2. Intercept and slope | 20.32 [19.66, 20.98] | −0.25 [-0.29, −0.20] | 30.42 [25.54, 36.22] | 0.02 [0.01, 0.06] | 2 vs. 1, 4.41 [0.04] | |
| 3. Intercept (Fixed slope squared) | 20.76 [20.07, 21.46] | −0.51 [-0.66, −0.37] | 0.02 [0.01, 0.02] | 30.54 [25.66, 36.34] | 0.02 [0.01, 0.06] | 3 vs. 2, 14.60 [<0.001] |
On average, PROMIS anxiety scores 3-weeks post-baseline (intercept fixed-effect) were 20.42 (95% CI, 19.81 to 21.03). Anxiety decreased 0.56 points the week following the first measurement (slope fixed-effect, −0.56; 95% CI, −0.68 to −0.43), but the decrease decelerated every week after (quadratic slope fixed-effect, 0.02; 95% CI, 0.01 to 0.03). Coefficient estimates for PROMIS depression were of similar magnitude. On average, PROMIS depression scores 3-weeks post-baseline were 20.76 (95% CI, 20.07 to 21.46). Depression decreased 0.51 points the week following the first measurement (slope fixed-effect, −0.51; 95% CI, −0.66 to −0.37), but this decrease decelerated every week after (quadratic slope, 0.02; 95% CI, 0.01 to 0.02).
3.3. Goal 3: Anxiety and depression symptom change related to baseline characteristics
Table 3 presents coefficient estimates of anxiety and depression symptom change as a function of baseline characteristics. Each row of the table shows how a specific predictor was related to the level (intercept) and slope of symptoms within persons. The column titled Intercept contains the predictor main effect; it reveals if the predictor was associated with a difference in symptoms at the first measurement. The column titled Slope contains the estimate of the interaction between the predictor and time and indicated whether those characteristics were associated with differences in the rate of change over time. For comparison purposes we present at the bottom of Table 3 the intercept and slope value in the comparison group. Because these values varied slightly across predictors, we present the median in the table.
Table 3.
Predictors of intercept and slope in multilevel models of PROMIS anxiety and depression scores change during the COVID-19 pandemic.
| Predictor | PROMIS Anxiety, Coeff. [95% CI]a |
PROMIS Depression, Coeff. [95% CI]a |
||
|---|---|---|---|---|
| Intercept | Slope | Intercept | Slope | |
| Female (vs Male) | 1.42 [-0.15, 2.98] | −0.02 [-0.13, 0.09] | 0.37 [-1.42, 2.17] | 0.02 [-0.09, 0.14] |
| Age | −0.02 [-0.06, 0.02] | 0.00 [0.00, 0.00] | 0.00 [-0.05, 0.05] | 0.00 [0.00, 0.00] |
| Married/cohabitating (vs separated, divorced, widowed, or never married) | −1.16 [-2.29, −0.02]* | −0.03 [-0.11, 0.05] | −2.22 [-3.51, −0.94]* | −0.07 [-0.15, 0.02] |
| Above high school (vs at or below high school) | 0.61 [-0.60, 1.81] | 0.03 [-0.06, 0.12] | −0.03 [-1.41, 1.35] | 0.02 [-0.07, 0.11] |
| Social Determinants of Health | ||||
| Lack of Transportation | 0.62 [-0.73, 1.98] | 0.08 [-0.02, 0.18] | 1.39 [-0.15, 2.94] | 0.09 [-0.01, 0.19] |
| Food Insecurity | 1.30 [0.17, 2.43]* | 0.03 [-0.05, 0.11] | 1.81 [0.52, 3.09]* | 0.01 [-0.08, 0.09] |
| Housing Instability | 0.81 [-0.41, 2.03] | −0.02 [-0.11, 0.07] | 1.15 [-0.24, 2.54] | −0.04 [-0.13, 0.06] |
| Utilities Insecurity | 1.03 [-0.15, 2.21] | 0.03 [-0.05, 0.12] | 1.90 [0.56, 3.23]* | −0.03 [-0.12, 0.07] |
| Trouble Paying for Medications | 0.39 [-1.03, 1.81] | 0.04 [-0.06, 0.15] | 0.99 [-0.62, 2.60] | 0.06 [-0.05, 0.17] |
| Unemployment | 0.51 [-0.71, 1.72] | 0.07 [-0.02, 0.16] | 0.22 [-1.16, 1.61] | 0.09 [-0.005, 0.18] |
| Interest in More Education | −0.24 [-1.58, 1.10] | −0.04 [-0.14, 0.06] | −0.81 [-2.34, 0.72] | −0.01 [-0.11, 0.09] |
| Child or Family Care Insecurity | 0.14 [-1.31, 1.59] | 0.05 [-0.06, 0.15] | −0.86 [-2.52, 0.80] | 0.11 [0.004, 0.22]* |
| Total number of SDH | 0.26 [-0.03, 0.55] | 0.01 [-0.01, 0.04] | 0.32 [-0.01, 0.66] | 0.01 [-0.01, 0.04] |
| COVID-19 Family Stress Screener | 0.10 [0.04, 0.17]* | 0.00 [0.00, 0.01] | 0.04 [-0.04, 0.11] | 0.00 [0.00, 0.01] |
| Minority Stress | 0.27 [-0.14, 0.69] | 0.00 [-0.03, 0.03] | 0.18 [-0.29, 0.65] | 0.01 [-0.02, 0.05] |
|
| ||||
| Median intercept and slopeb | 20.21 | −0.56 | 20.45 | −0.52 |
All models included intercept and linear time (slope) fixed- and random-effects, and fixed-effects for quadratic time, baseline characteristic, intervention condition, state of recruitment, and a two-way interaction between baseline characteristic and linear time.
Each predictor was examined in a separate analysis, and so the reference intercept and slope varied slightly across analyses. The median of these values are shown here for use in interpreting the differences.
Levels of PROMIS anxiety scores at the first measurement were 1.16 points lower (5.7% below median) for participants who were married or cohabitating at baseline (vs separated, widowed, divorced, or never married), 1.30 points higher (6.4% above median) for participants with baseline food insecurity (vs no food insecurity), while a one-point increase in COVID-19 family stress scores increased anxiety at the first measurement in 0.10 points (0.5% above median). We did not find evidence that baseline characteristics were associated with the rate of change over time in anxiety symptoms.
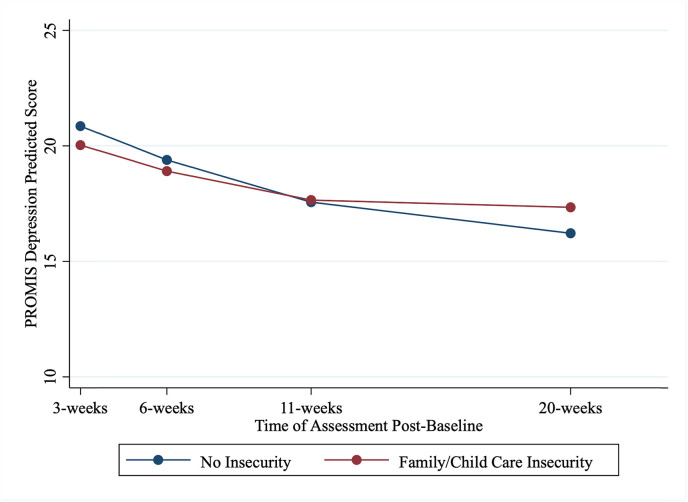
PROMIS depression scores at the first measurement were 2.22 points lower (10.9% below median) for participants who were married or cohabitating at baseline (vs separated, widowed, divorced, or never married), 1.81 points higher (8.9% above median) for participants with baseline food insecurity (vs no food insecurity), and 1.90 points higher (9.3% above median) for participants with baseline utilities insecurity (vs no utilities insecurity). Only childcare or family care responsability was associated with the linear rate of change over time in depression symptoms. Compared to those with no childcare or family care responsability, participants who were affected by this type of responsibility had depression symptoms that decreased at a 21.2% slower linear rate over time compared to the median rate (Fig. 3 ).
Fig. 3.
PROMIS depression scores trajectories by family or child care insecurity.
4. Discussion
During the COVID-19 pandemic, the general population samples evidenced an increase in the global prevalence of depression and anxiety symptoms (Salari et al., 2020; Santomauro et al., 2021), with accompanying increases in social determinants of health potentially compounding the mental health impact. With a cohort study, our first objective was to investigate whether there was a difference in anxiety and depression before and after the start of COVID-19 for those already with elevated symptoms. Although we had a smaller sample pre-pandemic as compared to during the ongoing pandemic, our findings are consistent with other longitudinal studies of samples with moderate to severe mental health symptoms prior to the COVID-19 pandemic (Robinson et al., 2022), showing that symptom severity remained stable across time. The pattern, as shown in Fig. 1, is one of consistency probably because conditions of the COVID-19 pandemic remained, and effects of the intervention were not considered in the current analyses. Our findings diverge from the results of the general population (Banks & Xu, 2020), where most people tend to have no symptoms or mild symptoms prior to March 2020, which could account for the overall rising trends in symptoms associated with the pandemic found in other studies.
Given the exposure to economic and social disadvantage observed in this population as shown in Table 1, it is surprising that the symptoms of anxiety or depression did not change. Several explanations are possible for these findings. One possibility is that the manifestation of the mental health impact of the COVID-19 pandemic could be showing in other behaviors like use of alcohol or drugs or self-harming behaviors. A second possibility is that people with elevated symptomatology might have greater resiliency dealing with isolation and the direct mental health effects of the loss or restriction of fulfilling activities and positive social connections (Hamm et al., 2020). A third possibility is that some of the changes that took place during the pandemic were either protective or served to reduce risk factors for some people. For example, some participants may have experienced increased family support and time with family during the pandemic, which can buffer against feelings of loneliness and isolation (Li & Xu, 2022; Szkody et al., 2021). As another example, social distancing may have reduced anxiety for some participants by decreasing expectations for out-of-home social events and providing greater freedom with one's time; a similar explanation was hypothesized in a study finding reduced incidence of migraine corresponding to lockdown in the Netherlands (Verhagen et al., 2021).
Our second objective evaluates whether the trajectory within and between people with elevated symptoms varied during the pandemic. Like findings from Banks and colleagues (2021), the trajectory of recovery is encouraging, showing that for the most part, symptoms of depression and anxiety during the pandemic diminish even within those with elevated symptomatology at baseline (Table 2). These findings support that people appear to adapt to COVID circumstances and for the most part show a decrease in symptoms over time.
Our third question examined the role of social determinants in the trajectories of depression and anxiety symptoms during COVID. We found that anxiety and depression scores for those with food insecurity were generally higher across the follow-up period compared to people without food insecurity; however, there was no evidence that the rate of symptom change was different over time for those with food insecurity. The difference in levels is consistent with literature showing that food insecurity increases anxiety and depression symptoms (McLaughlin et al., 2012). We also expected the trajectory of depression and anxiety symptoms (or slope) to differ between those who had enough food and those who were food insecure, especially since the pandemic exacerbated food insecurity in April 2020 among families already enrolled in school-based nutrition programs in 2019 (Sharma et al., 2020). But this pattern was not evident in our data. Perhaps increases in nutrition community resources, safety net programs (e.g., SNAP or Pandemic EBT), and meals provided to families through schools later in the pandemic (Schanzenbach, Ruffini & Whitmore, 2021) buffered the effect of food insecurity on the progression of mental health symptoms. It will be important to follow-up with our sample and other vulnerable populations to characterize their symptoms during and after the phasing out of social safety net policies provided during COVID-19 emergency policies, including employment benefits, stimulus checks, and eviction bans.
Several other social determinants of health expected to be related to mental health trajectories were not statistically significant in Table 3. It would be premature to conclude that a number of these factors are definitively not important, because 95% confidence intervals often include effects that are clinically meaningful. For example, the data are consistent with housing instability intercept effects of 2.03 and 2.54, but the intervals also include zero. Any non-significant findings should be considered in the context of accumulating evidence.
The only social determinant predictive of change in trajectories was need for childcare or care of a family member. We found that people with childcare or family care needs have slower improvement in depression symptoms than the median improvement we noticed for the full sample (bottom row in Table 3). Problems with childcare and family care seem to affect systematically the symptom trajectories of the people who are enrolled. This finding is not likely to be due to type I error given all the literature on the relationship between child and family care and mental health and the cross-sectional evidence from the COVID-19 pandemic about the harm to caregivers. It could give caregivers less time to attend to their own mental health needs, with fears for the wellbeing of people they are taking care of and limited opportunities to obtain support for themselves (Prime et al., 2020). Etheridge and Spantig (2020) suggest that changes in women's social networks could explain part of the negative impact. Ensuring access to quality childcare is one of Surgeon General Murthy's (2021) priorities for addressing economic and social barriers that contribute to poor mental health for families and caregivers.
Similar to Shuster et al. (2021), we found that being married or cohabitating with a partner correlated with lower overall levels of depression but not anxiety during the pandemic, and like Shuster we found that marital or cohabitating status did not predict the trajectory of respondents' symptoms. Some literature indicates people living with others had increases in anxiety during the pandemic (Solomou & Constantinidou, 2020), which the authors hypothesized was due to higher stress about contracting or spreading the virus and less ability to social distance. In a trajectories study of the UK general population (Bu et al., 2020), living with others was protective against loneliness, with 75% lower odds of being in the highest loneliness class. Living with others may be a better indicator of mental health trajectories than marital status (Bu et al., 2020), since it more clearly indicates an individual's opportunities for social interactions in the home.
Even though inconclusive (no statistically significant difference), the effects of other social determinants were in the direction that we would expect. For instance, the confidence intervals for medical transportation needs indicate that lack of transportation is still an exacerbating problem in the trajectory. Our study is a secondary analysis of an ongoing study. Further work will be needed to help understand the mechanisms of the relation between social determinants and mental health trajectories among people with prior moderate and severe depression and anxiety symptoms; for instance, whether the lack of correlation in our sample is due to government support buffering the effects of these social determinants.
4.1. Limitations
Alongside the strengths of this study – longitudinal design, a sample of Black, Asian, and Latinx adults who are mostly low-income and non-English speakers, use of a standardized screening tool for social determinants of health – there are several limitations. The broadest limitation, which the others stem from, is that this sample comes from a clinical trial and thus is not representative of the general population. The trial recruited people with moderate to severe depression or anxiety symptoms at baseline, and the literature shows that on average, they will improve over time. The trajectories we observed may also reflect other aspects of the recruitment strategy (e.g., recruitment from community-based organizations and primary care referrals) rather than wider population trends. Second, our study was not designed to evaluate differences in anxiety and depression symptoms pre- and during-COVID. Thus, time of entry into the study might be subject to selection bias since participants were not recruited at random times. For example, the pandemic could have made symptoms more salient for some people and increased their motivation to participate, or it could have raised barriers to participation for others. So, any observed differences between the pre- and during-COVID subsamples may be attributable to unobserved systematic differences between these subsamples rather than the effect of the pandemic itself. However, our analyses for Goal 1 indicated that there were no differences in anxiety and depression symptoms between study participants recruited before and during the pandemic (Fig. 1), which makes this limitation less concerning. Third, because the trial enrolled participants continuously throughout 2020 and 2021, participants began their baseline assessments and subsequent symptom assessments at different times. This prevents us from characterizing group trajectories aligned with the exact events of the pandemic. Whether changes can be totally attributed to COVID is difficult to establish since there is limited causal inference to quantify the unique contribution of the pandemic versus other factors. Fourth, since the RCT is still ongoing, we were unable to report on the effect of the intervention on the trajectory of PROMIS anxiety and depression scores. Prior studies have reported that PROMIS anxiety and depression are highly correlated with two of the RCT's primary outcomes (r = 0.86 between PROMIS anxiety and GAD-7 and r = 0.84 between PROMIS depression and PHQ-9 (Choi et al., 2014; Schalet et al., 2014). Thus, the intervention could have been associated with the overall trajectory of symptoms and could have also moderated the association between social determinants and trajectory of symptoms. Although we could not report on the overall effect of the intervention, in sensitivity tests (e.g., running models that included intervention condition, linear time, and each explanatory variable, together with their three-way interactions to assess whether there were significant differences in either intercept or slope of symptoms as a function of both the intervention and baseline characteristics) we did not find evidence that the association between social determinants and trajectory of symptoms was moderated by the intervention (analyses available from the authors). Finally, there was also sample attrition. When controlling for these factors through sensitivity analyses, the results did not change substantively, but there could be selection bias due to other unmeasured differences between samples over time.
5. Conclusion
Our findings may be useful to primary care and community-based organizations screening for social determinants of health need and connecting people with social services. Our adaptation of the Centers for Medicare and Medicaid Services Accountable Health Communities standardized screening tool for SDH (Billioux et al., 2017) used in clinics had slight variations but included four (housing instability, food insecurity, utility needs, and transportation needs) of the five primary domains. Screening and referral for health-related social needs is a stated priority for Centers for Medicare and Medicaid Services (CMS) (Centers for Medicare and Medicaid Services, 2021); however CMS covers costs of screening, but not care coordination (Ewald et al., 2021). Nurses, clinical social workers, and care managers can and do provide care coordination, but Medicare does not currently accept billing codes for them to provide these needed services without the presence of a physician, preventing the implementation of care coordination (Ewald et al., 2021). Further, CMS also pays for select social needs services, but these are largely limited to people with disabilities and older adults. Yet states with higher ratios of spending on social services and public health to spending on healthcare have better health outcomes, including fewer “mentally unhealthy days” (Bradley et al., 2016). The current study can provide an example of how to link health-related social needs data with changes in depression and anxiety symptoms over time.
Our findings demonstrate the potential importance of considering social needs and coordination as part of the overall health care plan during COVID-19. These results emphasize the value of screening for social determinants as a way to tailor the priorities of those in economic disadvantage for which attention to health needs might be a secondary priority given their resource constraints. The opportunity to ensure timely supports for food and utilities highlights how there needs to be a whole person approach so that mental health symptoms do not worsen during the pandemic. The role of supports to caregivers during the pandemic cannot be overstated due to the central role that they play for families and children. Mechanisms for family leave and family supports appear vital.
Funding
This study was supported by the National Institute of Mental Health, Grants R01MH117246 and R01MH117247. The funders had no role in study design, data collection and analysis, decision to publish, or manuscript preparation. The content of this paper is solely the responsibility of the authors and does not necessarily represent the views of the funders.
Data statement
The data is confidential and unavailable to share online.
CRediT authorship contribution statement
Margarita Alegría: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing. Mario Cruz-Gonzalez: Methodology, Formal analysis, Visualization. Isabel Shaheen O'Malley: Conceptualization, Writing – original draft, Writing – review & editing. Kiara Alvarez: Conceptualization, Critical review. Gabriela Livas Stein: Supervision, Investigation. Larimar Fuentes: Project administration, Data curation. Kari Eddington: Project administration, Data curation. Claire Poindexter: Project administration, Data curation. Sheri Lapatin Markle: Funding acquisition, Project administration. Anne N. Thorndike: Critical review. Lulu Zhang: Formal analysis. Patrick E. Shrout: Supervision, Methodology.
Declaration of competing interest
The authors declare no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.brat.2022.104102.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- Adams-Prassl A., Boneva T., Golin M., Rauh C. Working papers (No. 2020–030; working papers) Human Capital and Economic Opportunity Working Group; 2020. The impact of the coronavirus lockdown on mental health: Evidence from the US.https://ideas.repec.org/p/hka/wpaper/2020-030.html [Google Scholar]
- Ahrens K.F., Neumann R.J., Kollmann B., Brokelmann J., von Werthern N.M., Malyshau A., Weichert D., Lutz B., Fiebach C.J., Wessa M., Kalisch R., Plichta M.M., Lieb K., Tüscher O., Reif A. Impact of COVID-19 lockdown on mental health in Germany: Longitudinal observation of different mental health trajectories and protective factors. Translational Psychiatry. 2021;11(1):1–10. doi: 10.1038/s41398-021-01508-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M., Frontera W., Cruz-Gonzalez M., Markle S.L., Trinh-Shevrin C., Wang Y., Herrera L., Ishikawa R.Z., Velazquez E., Fuentes L. Effectiveness of a disability preventive intervention for minority and immigrant elders: The positive minds-strong bodies randomized clinical trial. American Journal of Geriatric Psychiatry. 2019;27(12):1299–1313. doi: 10.1016/j.jagp.2019.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks J., Fancourt D., Xu X. World Happiness Report. 2021. Mental health and the COVID-19 pandemic; p. 24.https://worldhappiness.report/ed/2021/mental-health-and-the-covid-19-pandemic/ 2021. [Google Scholar]
- Banks J., Xu X. The mental health effects of the first two months of lockdown during the COVID-19 pandemic in the UK*. Fiscal Studies. 2020;41(3):685–708. doi: 10.1111/1475-5890.12239. [DOI] [Google Scholar]
- Batterham P.J., Calear A.L., McCallum S.M., Morse A.R., Banfield M., Farrer L.M., Gulliver A., Cherbuin N., Harris R.M.R., Shou Y., Dawel A. Trajectories of depression and anxiety symptoms during the COVID‐19 pandemic in a representative Australian adult cohort. Medical Journal of Australia. 2021;214(10) doi: 10.5694/mja2.51043. https://www.mja.com.au/journal/2021/214/10/trajectories-depression-and-anxiety-symptoms-during-covid-19-pandemic [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billioux A., Verlander K., Anthony S., Alley D. Standardized screening for health-related social needs in clinical settings: The accountable health Communities screening tool. NAM perspectives. 2017 doi: 10.31478/201705b. [DOI] [Google Scholar]
- Bradley E.H., Canavan M., Rogan E., Talbert-Slagle K., Ndumele C., Taylor L., Curry L.A. Variation in health outcomes: The role of spending on social services, public health, and health care, 2000–09. Health Affairs. 2016;35(5):760–768. doi: 10.1377/hlthaff.2015.0814. [DOI] [PubMed] [Google Scholar]
- Brown S.M., Doom J.R., Lechuga-Peña S., Watamura S.E., Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect. 2020;110 doi: 10.1016/j.chiabu.2020.104699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bushman G., Mehdipanah R. Housing and health inequities during COVID-19: Findings from the national household pulse survey. Journal of Epidemiology & Community Health. 2021 doi: 10.1136/jech-2021-216764. [DOI] [PubMed] [Google Scholar]
- Bu F., Steptoe A., Fancourt D. Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Social Science & Medicine. 2020;265 doi: 10.1016/j.socscimed.2020.113521. 1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan C.M., Kroenke K., Counsell S.R., Hendrie H.C., Perkins A.J., Katon W., Noel P.H., Harpole L., Hunkeler E.M., Unützer J., IMPACT Investigators Treatment of depression improves physical functioning in older adults. Journal of the American Geriatrics Society. 2005;53(3):367–373. doi: 10.1111/j.1532-5415.2005.53151.x. [DOI] [PubMed] [Google Scholar]
- Cella D., Riley W., Stone A., Rothrock N., Reeve B., Yount S., Amtmann D., Bode R., Buysse D., Choi S., Cook K., Devellis R., DeWalt D., Fries J.F., Gershon R., Hahn E.A., Lai J.-S., Pilkonis P., Revicki D.…PROMIS Cooperative Group The patient-reported outcomes measurement information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. Journal of Clinical Epidemiology. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services . Vol. 57. 2021. (A guide to using the accountable health Communities health-related social needs screening tool: Promising practices and key insights). [Google Scholar]
- Choi S.W., Schalet B., Cook K.F., Cella D. Establishing a common metric for depressive symptoms: Linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychological Assessment. 2014;26(2):513–527. doi: 10.1037/a0035768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte C.S., Canino G.J., Alegria M., Ramos-Olazagasti M.A., Vila D., Miranda P., Ramjattan V., Alvarez K., Musa G.J., Elkington K., Wall M., Lapatin S., Bird H. Developmental psychopathology and ethnicity I: The young adulthood assessment of the Boricua youth study. Journal of the American Academy of Child & Adolescent Psychiatry. 2021;60(3):398–409. doi: 10.1016/j.jaac.2020.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etheridge B., Spantig L. ISER working paper series (No. 2020–08; ISER working paper series) Institute for Social and Economic Research; 2020. The gender gap in mental well-being during the Covid-19 outbreak: Evidence from the UK.https://ideas.repec.org/p/ese/iserwp/2020-08.html [Google Scholar]
- Ewald B., Golden R., Mason D.J. Promoting health Equity by paying for social care. JAMA Health Forum. 2021;2(12) doi: 10.1001/jamahealthforum.2021.5023. [DOI] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons R.D., Alegría M., Cai L., Herrera L., Markle S.L., Collazos F., Baca-García E. Successful validation of the CAT-MH Scales in a sample of Latin American migrants in the United States and Spain. Psychological Assessment. 2018;30(10):1267–1276. doi: 10.1037/pas0000569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annual Review of Public Health. 2014;35(1):169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Hamm M.E., Brown P.J., Karp J.F., Lenard E., Cameron F., Dawdani A., Lavretsky H., Miller J.P., Mulsant B.H., Pham V.T., Reynolds C.F., Roose S.P., Lenze E.J. Experiences of American older adults with pre-existing depression during the beginnings of the COVID-19 pandemic: A multicity, mixed-methods study. American Journal of Geriatric Psychiatry. 2020;28(9):924–932. doi: 10.1016/j.jagp.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes M.T., Szenczy A.K., Olino T.M., Nelson B.D., Klein D.N. Trajectories of depression, anxiety and pandemic experiences; A longitudinal study of youth in New York during the Spring-Summer of 2020. Psychiatry Research. 2021;298:113778. doi: 10.1016/j.psychres.2021.113778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huth-Bocks A. 2020. COVID-19 family stress screener v.4.1.20.https://docs.google.com/document/d/1xBFEOxn40EGF0og1JuBIOI7LLGlbLhtifPKbBc1ImZY/edit [Google Scholar]
- Jones A.D. Food insecurity and mental health status: A global analysis of 149 countries. American Journal of Preventive Medicine. 2017;53(2):264–273. doi: 10.1016/j.amepre.2017.04.008. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwong A.S.F., Pearson R.M., Adams M.J., et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. The British Journal of Psychiatry. 2021;218(6):334–343. doi: 10.1192/bjp.2020.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Njai R.S., Greenlund K.J., Chapman D.P., Croft J.B. Relationships between housing and food insecurity, frequent mental distress, and insufficient sleep among adults in 12 US States, 2009. Preventing Chronic Disease. 2014;11:E37. doi: 10.5888/pcd11.130334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Xu Q. Family support as a protective factor for attitudes toward social distancing and in preserving positive mental health during the COVID-19 pandemic. Journal of Health Psychology. 2022;27(4):858–867. doi: 10.1177/1359105320971697. [DOI] [PubMed] [Google Scholar]
- McAuliffe C., Daly Z., Black J., Pumarino J., Gadermann A., Slemon A., Thomson K.C., Richardson C., Jenkins E.K. Examining the associations between food worry and mental health during the early months of the COVID-19 pandemic in Canada. Canadian Journal of Public Health = Revue Canadienne De Sante Publique. 2021;112(5):843–852. doi: 10.17269/s41997-021-00557-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin K.A., Green J.G., Alegría M., Jane Costello E., Gruber M.J., Sampson N.A., Kessler R.C. Food insecurity and mental disorders in a national sample of U.S. adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(12):1293–1303. doi: 10.1016/j.jaac.2012.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy V. Office of the Surgeon General; 2021. Protecting youth mental health: The US Surgeon General's advisory.https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf [Google Scholar]
- Nagata J.M., Ganson K.T., Whittle H.J., Chu J., Harris O.O., Tsai A.C., Weiser S.D. Food insufficiency and mental health in the U.S. During the COVID-19 pandemic. American Journal of Preventive Medicine. 2021;60(4):453–461. doi: 10.1016/j.amepre.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD . 2021. Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response—OECD.https://read.oecd-ilibrary.org/view/?ref=1094_1094455-bukuf1f0cm&title=Tackling-the-mental-health-impact-of-the-COVID-19-crisis-An-integrated-whole-of-society-response [Google Scholar]
- Paykel E.S., Myers J.K., Lindenthal J.J., Tanner J. Suicidal feelings in the general population: A prevalence study. The British Journal of Psychiatry. 1974;124:460–469. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- Pedrosa A.L., Bitencourt L., Fróes A.C.F., Cazumbá M.L.B., Campos R.G.B., de Brito S.B.C.S., Simões e Silva A.C. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Frontiers in Psychology. 2020;11:2635. doi: 10.3389/fpsyg.2020.566212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis P.A., Choi S.W., Reise S.P., Stover A.M., Riley W.T., Cella D., PROMIS Cooperative Group. Item banks for measuring emotional distress from the patient-reported outcomes measurement information System (PROMIS®): Depression, anxiety, and anger. Assessment. 2011;18(3):263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Quinn S.C., Kumar S. Health inequalities and infectious disease Epidemics: A challenge for global health security. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2014;12(5):263–273. doi: 10.1089/bsp.2014.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health. 2020;16(1):57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santomauro D.F., Herrera A.M.M., Shadid J.…Murray C.J.L. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders R., Buckman J.E.J., Fonagy P., Fancourt D. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychological Medicine. 2021;1–9 doi: 10.1017/S0033291721000957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schalet B.D., Cook K.F., Choi S.W., Cella D. Establishing a common metric for self-reported anxiety: Linking the MASQ, PANAS, and GAD-7 to PROMIS anxiety. Journal of Anxiety Disorders. 2014;28(1):88–96. doi: 10.1016/j.janxdis.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schanzenbach L.B., Ruffini K., Whitmore D. Brookings; 2021. An update on the effect of Pandemic EBT on measures of food hardship.https://www.brookings.edu/research/an-update-on-the-effect-of-pandemic-ebt-on-measures-of-food-hardship/ [Google Scholar]
- Sharma S.V., Chuang R.-J., Rushing M., Naylor B., Ranjit N., Pomeroy M., Markham C. Social determinants of health–related needs during COVID-19 among low-income households with children. Preventing Chronic Disease. 2020;17:E119. doi: 10.5888/pcd17.200322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuster A., O'Brien M., Luo Y., Berner L.A., Perl O., Heflin M., Kulkarni K., Chung D., Na S., Fiore V.G., Gu X. Emotional adaptation during a crisis: Decline in anxiety and depression after the initial weeks of COVID-19 in the United States. Translational Psychiatry. 2021;11(1):1–7. doi: 10.1038/s41398-021-01552-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley B.D., Myers H.F., Harrell S.P. Minority-status stresses and the college adjustment of ethnic minority freshmen. Journal of Higher Education. 1993;64(4):434–452. doi: 10.2307/2960051. [DOI] [Google Scholar]
- Solomou I., Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: Age and sex matter. International Journal of Environmental Research and Public Health. 2020;17(14):4924. doi: 10.3390/ijerph17144924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soria K.M., Horgos B. SERU Consortium, University of California - Berkeley and University of Minnesota; 2020. Social class Differences in students' Experiences during the COVID-19 pandemic [report]http://conservancy.umn.edu/handle/11299/216229 [Google Scholar]
- StataCorp . StataCorp LLC; 2021. Stata statistical software (Release 17) [computer software] [Google Scholar]
- Szkody E., Stearns M., Stanhope L., McKinney C. Stress-buffering role of social support during COVID-19. Family Process. 2021;60(3):1002–1015. doi: 10.1111/famp.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas D., Lawton R., Brown T., Kranton R. Prevalence, severity and distribution of depression and anxiety symptoms using observational data collected before and nine months into the COVID-19 pandemic. The Lancet Regional Health – Americas. 2021;1 doi: 10.1016/j.lana.2021.100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhagen I.E., van Casteren D.S., de Vries Lentsch S., Terwindt G.M. Effect of lockdown during COVID-19 on migraine: A longitudinal cohort study. Cephalalgia: An International Journal of Headache. 2021;41(7):865–870. doi: 10.1177/0333102420981739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright L., Steptoe A., Fancourt D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. Journal of Epidemiology & Community Health. 2020;74(9):683–688. doi: 10.1136/jech-2020-214475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S.X., Wang Y., Rauch A., Wei F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.