Abstract
BACKGROUND:
Incisional hernia develops in up to 20% of patients undergoing abdominal operations. We sought to identify characteristics associated with poor outcomes after acute incisional hernia incarceration.
STUDY DESIGN:
We performed a retrospective cohort study of adult patients with incisional hernias undergoing elective repair or with acute incarceration between 2010 and 2017. The primary end point was 30-day mortality. Logistic regression was used to determine adjusted odds associated with 30-day mortality. The American College of Surgeons Surgical Risk Calculator was used to estimate outcomes had these patients undergone elective repair.
RESULTS:
A total of 483 patients experienced acute incarceration; 30-day mortality was 9.52%. Increasing age (adjusted odds ratio 1.05; 95% CI, 1.02 to 1.08) and bowel resection (adjusted odds ratio 3.18; 95% CI, 1.45 to 6.95) were associated with mortality. Among those with acute incarceration, 231 patients (47.9%) had no documentation of an earlier surgical evaluation and 252 (52.2%) had been evaluated but had not undergone elective repair. Among patients 80 years and older, 30-day mortality after emergent repair was high (22.9%) compared with estimated 30-day mortality for elective repair (0.73%), based on the American College of Surgeons Surgical Risk Calculator. Estimated mortality was comparable with observed elective repair mortality (0.82%) in an age-matched cohort. Similar mortality trends were noted for patients younger than 60 years and aged 60 to 79 years.
CONCLUSIONS:
Comparison of predicted elective repair and observed emergent repair mortality in patients with acute incarceration suggests that acceptable outcomes could have been achieved with elective repair. Almost one-half of acute incarceration patients had no earlier surgical evaluation, therefore, targeted interventions to address surgical referral can potentially result in fewer incarceration-related deaths.
Incisional ventral hernias represent a considerable disease burden, as approximately 2 million abdominal operations are performed in the US each year, and up to 20% of those can be complicated by development of an incisional hernia.1 Definitive management consists of elective repair; however, a variety of patient- and provider-driven factors can lead to nonoperative management (NOM). NOM carries a risk of incarceration requiring emergent operation,2,3 although only a small proportion of patients (<3%) who undergo NOM ultimately require emergent operation.4 Aside from the risk of incisional hernia incarceration, it is also important to consider associated outcomes after acute incarceration, particularly given the established excess morbidity and mortality of emergent repair.1,5,6 Wide variability in acute incarceration outcomes, including some patients whose postoperative course might be similar to that for an elective repair, contributes to clinical equipoise surrounding incisional hernia management. Identification of the subset of patients who experience incarceration that results in a prolonged and complicated postoperative course and/or death might provide greater value in guiding patient selection for elective repair.
The elevated rates of adverse outcomes after an emergent operation for all types of ventral hernias are well established.1,5,6 Nevertheless, given their surgical history, patients with incisional hernias can theoretically be at higher risk for poor outcomes due to inherent difficulties in the operation associated with postoperative adhesions.2,7,8 There has been little directed inquiry focusing on outcomes after acute incisional hernia incarceration. The aim of this study was to investigate preoperative and perioperative characteristics among patients with an incisional hernia initially managed nonoperatively who experienced acute incarceration. We proposed that improved understanding of patient characteristics associated with poor outcomes after acute incarceration can identify variability in hernia management that is eligible for targeted quality improvement.
METHODS
Study design and patient selection
We performed a retrospective cohort study of all patients diagnosed with an incisional hernia who experienced an acute incarceration requiring emergent repair between January 1, 2010 and November 30, 2017 at 15 hospitals within the University of Pittsburgh Medical Center healthcare system. We excluded patients with primary, parastomal, inguinal, internal, or hiatal hernias. Full details of the entire population (n = 30,998) have been reported previously4 (Fig. 1). Briefly, we selected 17 ICD codes possessing face validity to maximize the sensitivity for identifying all patients with an incisional hernia. We defined an acute incarceration as a nonelective hernia repair (ie on presentation to the emergency department or after inter-facility transfer); patients who died as a result of acute incarceration without undergoing surgical intervention were also included. To identify acute incarceration events, we performed a thorough review of all nonelective incisional hernia repairs to confirm that the indication for operation was an acute incarceration, all nonelective exploratory laparotomies/laparoscopies to identify those cases in which an incarcerated hernia led to an operation but no hernia repair, and all inpatient deaths. We focused our investigation on patients who had a documented history of an incisional hernia during a separate earlier encounter, and could have theoretically undergone surgical evaluation before their incarceration event. As a result, we excluded all patients with a concurrent index incisional hernia diagnosis and emergent operation. Patients undergoing elective repair of an incisional hernia were identified by review of CPT codes. The IRB at the University of Pittsburgh approved this study.
Figure 1.
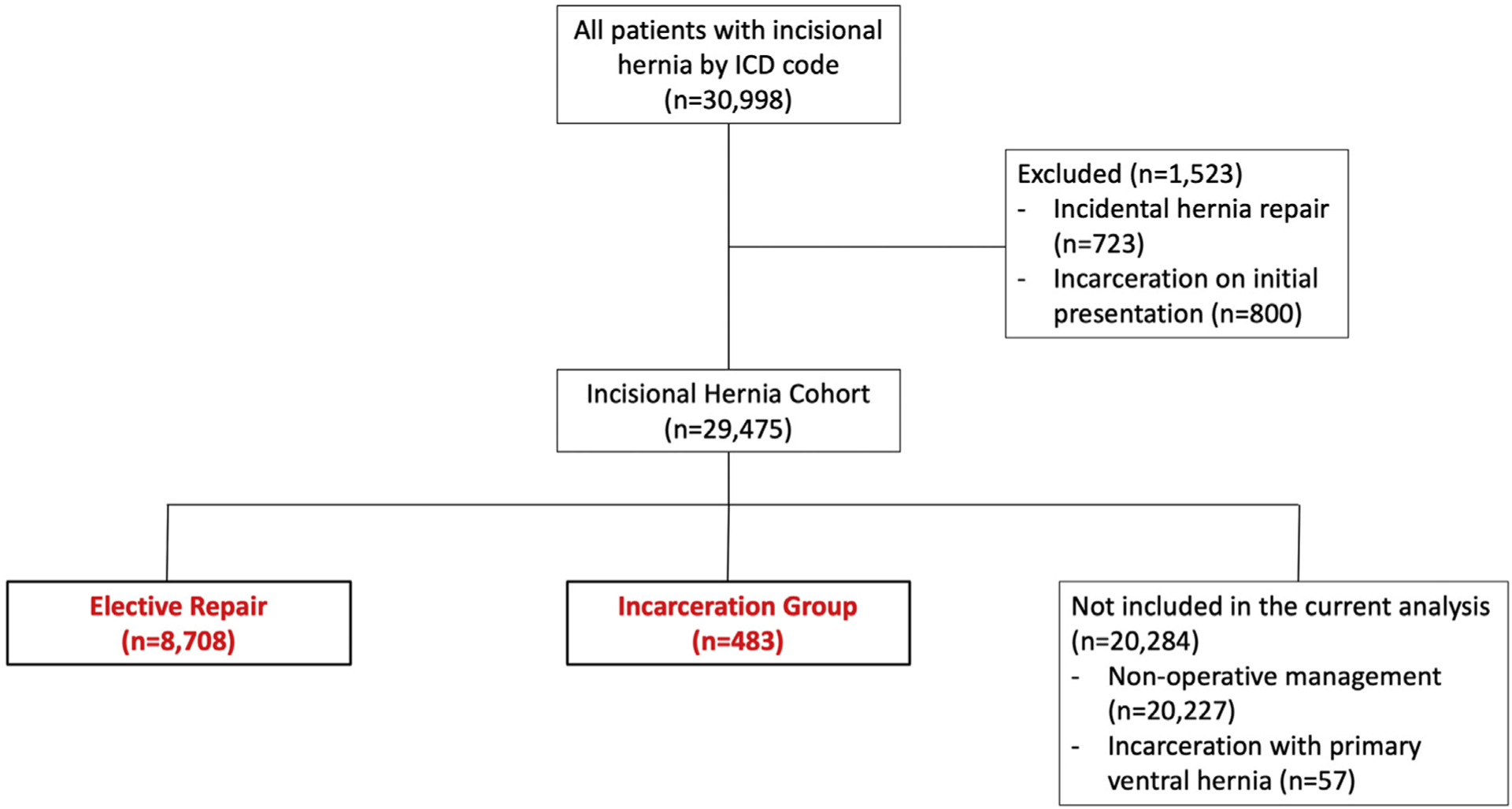
Flowchart of the study cohort. The populations analyzed in this study (ie elective repair and incarceration group) are shown in red font.
Characteristics among patients with acute incarceration
Patient variables were extracted by manual review of the electronic health record (EHR). Baseline variables were obtained from review of records at the index date of diagnosis (defined as the first documentation of the incisional hernia). Perioperative variables were obtained from the encounter that included the emergency operation. Our primary end point was 30-day mortality, which we obtained from review of inpatient records and from the Social Security Death Index.9 In a secondary analysis, patients were stratified based on the need for a bowel resection for compromised bowel, as specified in the operative report. Patients who required bowel resection that was deemed inherent to the complexity of the case were analyzed along with those patients who did not undergo bowel resection.
Categorization of incisional hernia management
Our payor-provider, multihospital healthcare system insures more than 43% of individuals in Western Pennsylvania and all in-network encounters are captured in our EHR. Patients with an initial encounter and incisional hernia diagnosis are likely to have subsequent records within our EHR. Patients were categorized based on whether they had any documented surgical evaluation of their hernia after their index date of diagnosis. All outpatient surgical visits were reviewed for documentation of assessment and decision-making for management of the incisional hernia.
Patients without documented surgical evaluation were classified based on provider documentation as one of the following: hernia noted by radiologist, hernia noted by nonsurgeon and no surgical referral documented, or surgical referral recommended but no record of surgical evaluation. Patients who underwent surgical evaluation were categorized based on whether repair was not offered (ie documentation included assessment of the hernia but no mention of offering repair), repair was recommended but the patient declined, or incarceration occurred before a scheduled elective repair date. For patients who were not offered repair, reasons were categorized as one of the following: excess weight (including any documentation in which the surgeon recommended weight loss before reconsidering repair), comorbidities, or lack of symptoms such that the benefits of the procedure were deemed minimal.
To compare perioperative mortality in elective and emergent repair cases, we examined 30-day postoperative mortality rates based on age (ie younger than 60 years, 60 to 79 years, or 80 years and older) in both the incarceration cohort and a cohort of patients who underwent elective incisional hernia repair. We used baseline variables to estimate elective repair mortality for those patients with incarceration using the American College of Surgeons Surgical Risk Calculator.10
Statistical analysis
Continuous data are reported as mean (SD) or median (interquartile range) and categorical data are reported as number (%). We performed pairwise comparison of continuous data using Student’s t-test or Mann-Whitney U test for continuous variables and chi-square analysis for categorical variables. Missingness was < 10% for all variables. All hypothesis testing was 2-sided and p < 0.05was considered significant. We performed multivariable logistic regression of relevant demographic and clinical variables to calculate adjusted odds ratios (aOR) with 95% CIs of 30-day mortality and need for bowel resection. Both age and sex were also included in the perioperative model. The aORs were obtained using stepwise logistic regression with backward elimination and included all variables with p < 0.05 in the final multivariable regression model. We performed a propensity score-matched analysis of patients undergoing elective repair and emergent repair for comparison of 30-day mortality rates. Propensity matching with 1:1 pairing was performed using age, sex, race, smoking, and the presence of comorbidities (eg heart disease, COPD, diabetes, end-stage renal disease, and cirrhosis). Elective and emergent repair patients were matched using nearest neighbor matching with a caliper distance of 0.20 the SD of the logit of the propensity score. Appropriateness of matching was confirmed by an absolute standardized mean difference of < 0.10. Kaplan-Meier curves were constructed for overall survival as well as survival stratified by age groups (younger than 60 years, 60 to 79 years, and 80 years and older) and by bowel resection. Statistical analyses were performed using STATA Software, release 16 (StataCorp).
RESULTS
Clinical characteristics and perioperative mortality
A total of 483 patients (mean [SD] age 62.3 [14.7] years, 73.1% were female) experienced acute incarceration (Table 1). The majority of patients (n = 473 [97.9%]) underwent emergent operation and the remaining 10 patients did not undergo operation due to futility or patient preferences. Of the 483 patients, 46 (9.52%) died within 30 days of presentation. We first analyzed patient characteristics available at the time of hernia diagnosis to determine which characteristics were predictive of mortality after incarceration. After adjusting for baseline characteristics, age 80 years and older (aOR 5.92; 95% CI, 2.51 to 13.96; p < 0.001), male sex (aOR 2.14; 95% CI, 1.11 to 4.13; p = 0.024), and presence of symptoms (aOR 2.12; 95% CI, 1.01 to 4.43; p = 0.046) were significantly associated with mortality (Table 2). Next, we analyzed characteristics at the time of acute presentation. Among perioperative variables, age 80 years and older (aOR 3.69; 95% CI, 1.42 to 9.58; p = 0.007), WBC count (aOR 1.08; 95% CI, 1.02 to 1.13; p = 0.004), creatinine level (aOR 1.35; 95% CI, 1.11 to 1.63; p = 0.003), mean arterial pressure (aOR 0.97; 95% CI, 0.95 to 0.99; p = 0.020), and bowel resection (aOR 3.54; 95% CI, 1.61 to 7.79; p = 0.002) were independently associated with 30-day mortality. Kaplan-Meier analysis was performed for all patients (eFig. 1A) and in patients stratified by age (eFig. 1B).
Table 1.
Baseline and Perioperative Characteristics of Patients with Incisional Hernia Incarceration, Stratified by Death at 30 Days
| Characteristic | Overall (n = 483) | Alive (n = 437) | Deceased (n = 46) | p Value |
|---|---|---|---|---|
| Baseline | ||||
| Patient | ||||
| Age, y, mean (SD) | 62.3 (14.7) | 61.5 (14.5) | 70.4 (14.4) | < 0.001 |
| Sex, n (%) | 0.050 | |||
| Male | 130 (26.9) | 112 (25.6) | 18 (39.1) | |
| Female | 353 (73.1) | 325 (74.4) | 28 (60.9) | |
| Race/ethnicity, n (%) | 0.79 | |||
| Caucasian | 412 (85.3) | 372 (85.1) | 40 (87.0) | |
| Black | 67 (13.9) | 61 (14.0) | 6 (13.0) | |
| Hispanic | 4 (0.8) | 4 (0.9) | 0 | |
| BMI, kg/m2, mean (SD) | 37.45 (10.4) | 37.6 (10.3) | 36.4 (11.3) | 0.47 |
| Smoking status, n (%) | 0.18 | |||
| Never | 173 (35.8) | 158 (36.2) | 15 (32.6) | |
| Current | 144 (29.8) | 130 (29.8) | 14 (30.4) | |
| Former | 144 (29.8) | 132 (30.2) | 12 (26.1) | |
| Unspecified | 22 (4.6) | 17 (3.9) | 5 (10.9) | |
| Hernia, n (%) | ||||
| Symptoms | 278 (57.6) | 246 (56.3) | 32 (69.6) | 0.083 |
| Incision type | 0.43 | |||
| Midline | 335 (69.4) | 298 (68.2) | 37 (80.4) | |
| Pfannenstiel | 26 (5.4) | 23 (5.3) | 3 (6.5) | |
| Laparoscopic | 80 (16.6) | 76 (17.4) | 4 (8.7) | |
| Old stoma | 24 (4.97) | 22 (5.0) | 2 (4.4) | |
| Bilateral subcostal | 4 (0.8) | 4 (0.9) | 0 | |
| Other | 14 (2.9) | 14 (3.2) | 0 | |
| Earlier hernia repair | 159 (33.0) | 138 (31.7) | 21 (45.7) | 0.055 |
| Earlier mesh placement | 82 (17) | 75 (17.2) | 7 (15.2) | 0.73 |
| Comorbidity, n (%) | ||||
| COPD | 88 (18.2) | 77 (17.6) | 11 (23.9) | 0.29 |
| ESRD | 21 (4.4) | 18 (4.1) | 3 (6.5) | 0.45 |
| Cirrhosis | 28 (5.8) | 25 (5.7) | 3 (6.5) | 0.83 |
| Diabetes | 178 (36.9) | 156 (35.7) | 22 (47.8) | 0.11 |
| Active cancer | 42 (8.7) | 35 (8.0) | 7 (15.2) | 0.099 |
| Immunosuppression | 44 (9.1) | 40 (9.2) | 4 (8.7) | 0.92 |
| Perioperative | ||||
| Vital sign, mean (SD) | ||||
| Maximum temperature, °C | 36.7 (0.6) | 36.7 (0.4) | 36.8 (0.5) | 0.85 |
| Heart rate, beats/min | 86.6 (17.9) | 85.5 (17.0) | 97.3 (22.5) | < 0.001 |
| Mean arterial pressure, mmHg | 96.1 (20.4) | 97.2 (19.5) | 86.5 (27.11) | 0.003 |
| Laboratory values at presentation, mean (SD) | ||||
| WBC count, × 103 cells/mL | 10.9 (5.6) | 10.5 (4.9) | 14.3 (9.7) | < 0.001 |
| Neutrophil to lymphocyte ratio | 12.7 (67.5) | 11.9 (70.1) | 21.6 (23.2) | 0.42 |
| Hematocrit, % | 39.0 (6.5) | 39.1 (6.4) | 38.3 (7.4) | 0.47 |
| Creatinine, mg/dL | 1.3 (1.4) | 1.2 (1.2) | 2.1 (2.4) | < 0.001 |
| Bicarbonate, mEq/L | 26.6 (5.1) | 26.7 (3.5) | 25.4 (12.8) | 0.099 |
| Operative detail | ||||
| ASA classification, mean (SD) | 3.2 (0.6) | 3.1 (0.6) | 3.69 (0.59) | < 0.001 |
| Case duration, min, median (IQR) | 159 (113.5–220) | 158.5 (113–219.5) | 174.5 (125–221.5) | 0.35 |
| Procedure detail, n (%) | ||||
| Bowel resection | 112 (23.2) | 90 (20.6) | 22 (47.8) | < 0.001 |
| Hernia repair with mesh | 212 (44.4) | 206 (47.6) | 6 (13.3) | < 0.001 |
| Length of stay, d, median (IQR) | ||||
| Total | 7 (4–11) | 7 (4–11) | 6.5 (1–13) | 0.076 |
| ICU | 0 (0–2) | 0 (0–2) | 2 (0–8) | < 0.001 |
| Disposition, n (%) | < 0.001 | |||
| Home | 341 (70.6) | 326 (74.6) | 15 (32.6) | |
| Facility | 113 (23.4) | 109 (24.9) | 4 (8.7) | |
| Inpatient death | 29 (6) | 2 (0.5) | 27 (58.7) |
ASA, American Society of Anesthesiologists; ESRD, end-stage renal disease; IQR, interquartile range.
Table 2.
Multivariable Analysis of 30-Day Mortality after Incisional Hernia Incarceration
| Characteristic | Odds ratio | 95% CI | p Value |
|---|---|---|---|
| Baseline | |||
| Age | |||
| Younger than 60 y | Reference | Reference | Reference |
| 60 to 79 y | 1.84 | 0.87–3.91 | 0.110 |
| 80 y and older | 5.92 | 2.51713.96 | < 0.001 |
| Male sex | 2.14 | 1.1174.13 | 0.024 |
| Symptoms | 2.12 | 1.0174.43 | 0.046 |
| Perioperative | |||
| Age | |||
| Younger than 60 y | Reference | Reference | Reference |
| 60 to 79 y | 1.84 | 0.7974.30 | 0.156 |
| 80 y and older | 3.69 | 1.4279.58 | 0.007 |
| WBC count | 1.08 | 1.0271.13 | 0.004 |
| Creatinine | 1.35 | 1.1171.63 | 0.003 |
| Mean arterial pressure | 0.97 | 0.9570.99 | 0.020 |
Bowel resection
We compared characteristics of patients undergoing bowel resection (eTable 1). Patients with a earlier hernia repair (aOR 1.68; 95% CI, 1.07 to 2.65; p = 0.025) and those with a lower BMI (aOR 0.97; 95% CI, 0.95 to 0.99; p = 0.007) at baseline had an increased odds of bowel resection (Table 3). Perioperative temperature (aOR 2.46; 95% CI, 1.41 to 4.29; p = 0.001), bicarbonate level (OR 0.91; 95% CI, 0.85 to 0.98; p = 0 .011), and neutrophil to lymphocyte ratio (NLR) (aOR 1.05; 95% CI, 1.03 to 1.07; p < 0.001) emerged as independent predictors of bowel resection. Kaplan-Meier analysis demonstrates reduced survival after bowel resection (log-rank p < 0.001) (eFig. 2). Also shown are additional hernia-related outcomes (eTable 2).
Table 3.
Multivariable Analysis of the Need for Bowel Resection among Patients Undergoing Emergency Operation for an Incisional Hernia
| Characteristic | Odds ratio | 95% CI | p Value |
|---|---|---|---|
| Baseline | |||
| BMI | 0.97 | 0.95–0.99 | 0.007 |
| Earlier repair | 1.68 | 1.07–2.65 | 0.025 |
| Perioperative | |||
| Maximum temperature | 2.46 | 1.41–4.29 | 0.001 |
| Bicarbonate level | 0.91 | 0.85–0.98 | 0.011 |
| Neutrophil to lymphocyte ratio | 1.05 | 1.03–1.07 | < 0.001 |
Documentation of nonoperative management
We explored medical decision-making, as documented in the EHR, to improve understanding of the rationale for NOM (Tables 4 and 5). Overall, 231 patients (47.8%) had no documentation of an earlier surgical consultation. The remaining patients underwent surgical evaluation, which resulted in 175 patients (36.2%) not being offered repair, 39 (8.1%) declining repair, and 38 (7.9%) having a repair scheduled; however, acute incarceration occurred before the repair date. Among patients who died, only half (n = 23) had undergone an earlier surgical evaluation. Patients 80 years and older were less likely to have been referred to a surgeon (20 of 61 [32.8%]) compared with patients younger than 60 years (120 of 214 [56.1%]) and 60 to 79 years (112 of 208 [53.8%]).
Table 4.
Decision-Making for Initial Nonoperative Management among Patients Who Ultimately Experienced Acute Incisional Hernia Incarceration, Stratified by Mortality
| Category | Overall (n = 483) | Alive (n = 437) | Deceased (n = 46) | p Value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Hernia only noted by radiologist | 99 | 20.5 | 94 | 21.5 | 5 | 10.9 | 0.005 |
| Note of hernia by nonsurgeon, no surgical referral | 107 | 22.2 | 89 | 20.4 | 18 | 39.1 | |
| Referred to surgeon, no documentation of surgical visit | 25 | 5.2 | 25 | 5.7 | 0 | 0 | |
| Evaluated by surgeon, repair not offered | 175 | 36.2 | 154 | 35.2 | 21 | 45.7 | |
| Evaluated by surgeon, offered repair, patient refused | 39 | 8.1 | 38 | 8.7 | 1 | 2.2 | |
| Evaluated by surgeon, offered repair, incarceration occurred before repair date | 38 | 7.9 | 37 | 8.5 | 1 | 2.2 | |
| Decision-making for nonoperative management among patients evaluated by a surgeon | 0.089 | ||||||
| Repair not offered due to patient weight | 67 | 38.3 | 59 | 38.3 | 8 | 38.1 | |
| Repair not offered due to comorbidity | 44 | 25.1 | 35 | 22.7 | 9 | 42.9 | |
| Repair not offered due to lack of symptoms | 64 | 36.6 | 60 | 39.0 | 4 | 19.1 | |
Table 5.
Decision-Making for Initial Nonoperative Management among Patients Who Ultimately Experienced Acute Incisional Hernia Incarceration, Stratified by Age
| Category | Age group | |||||
|---|---|---|---|---|---|---|
| Younger than 60 y (n = 214) | 60 to 79 y (n = 208) | 80 y and older (n = 61) | ||||
| n | % | n | % | n | % | |
| Hernia only noted by radiologist | 41 | 19.2 | 43 | 20.1 | 15 | 24.6 |
| Note of hernia by nonsurgeon, no surgical referral | 43 | 20.1 | 41 | 19.7 | 23 | 37.7 |
| Referred to surgeon, no documentation of surgical visit | 10 | 4.7 | 12 | 5.8 | 3 | 4.9 |
| Evaluated by surgeon, repair not offered | 92 | 43.0 | 71 | 34.1 | 12 | 19.7 |
| Evaluated by surgeon, offered repair, patient refused | 16 | 7.5 | 20 | 9.6 | 3 | 4.9 |
| Evaluated by surgeon, offered repair, incarceration occurred before repair date | 12 | 5.6 | 21 | 10.1 | 5 | 8.2 |
| Decision-making for nonoperative management among patients evaluated by a surgeon | ||||||
| Repair not offered due to patient weight | 52 | 56.5 | 15 | 21.1 | 0 | 0 |
| Repair not offered due to comorbidity | 9 | 9.8 | 28 | 39.4 | 7 | 58.3 |
| Repair not offered due to lack of symptoms | 31 | 33.7 | 28 | 39.4 | 5 | 41.7 |
Estimated and observed perioperative mortality for elective repair
In a cohort of 8,708 patients who underwent elective incisional hernia repair, 30-day postoperative mortality rates in patients younger than 60 years, 60 to 79 years, and 80 years and older were 0.12%, 0.47%, and 0.82%, respectively (Fig. 2). In comparison, 30-day mortality rates among our 483 patients with acute incarceration, stratified by these age groups, were 5.61%, 9.62%, and 22.91%, respectively. Estimated mortality rates had these patients undergone elective repair (from the American College of Surgeons Surgical Risk Calculator) were 0.14%, 0.51%, and 0.73% in patients younger than 60 years, 60 to 79 years, and 80 years and older, respectively. Overall, estimated elective repair mortality (0.37%) in patients who ultimately experienced acute incarceration was not significantly different from observed elective repair mortality (0.28%; p = 0.399). After propensity score matching using demographic characteristics and comorbidities (eTable 3), observed 30-day mortality rates for patients undergoing emergent repair (9.15%) remained significantly higher than mortality rates among those patients undergoing elective repair (0.64%; p < 0.001).
Figure 2.
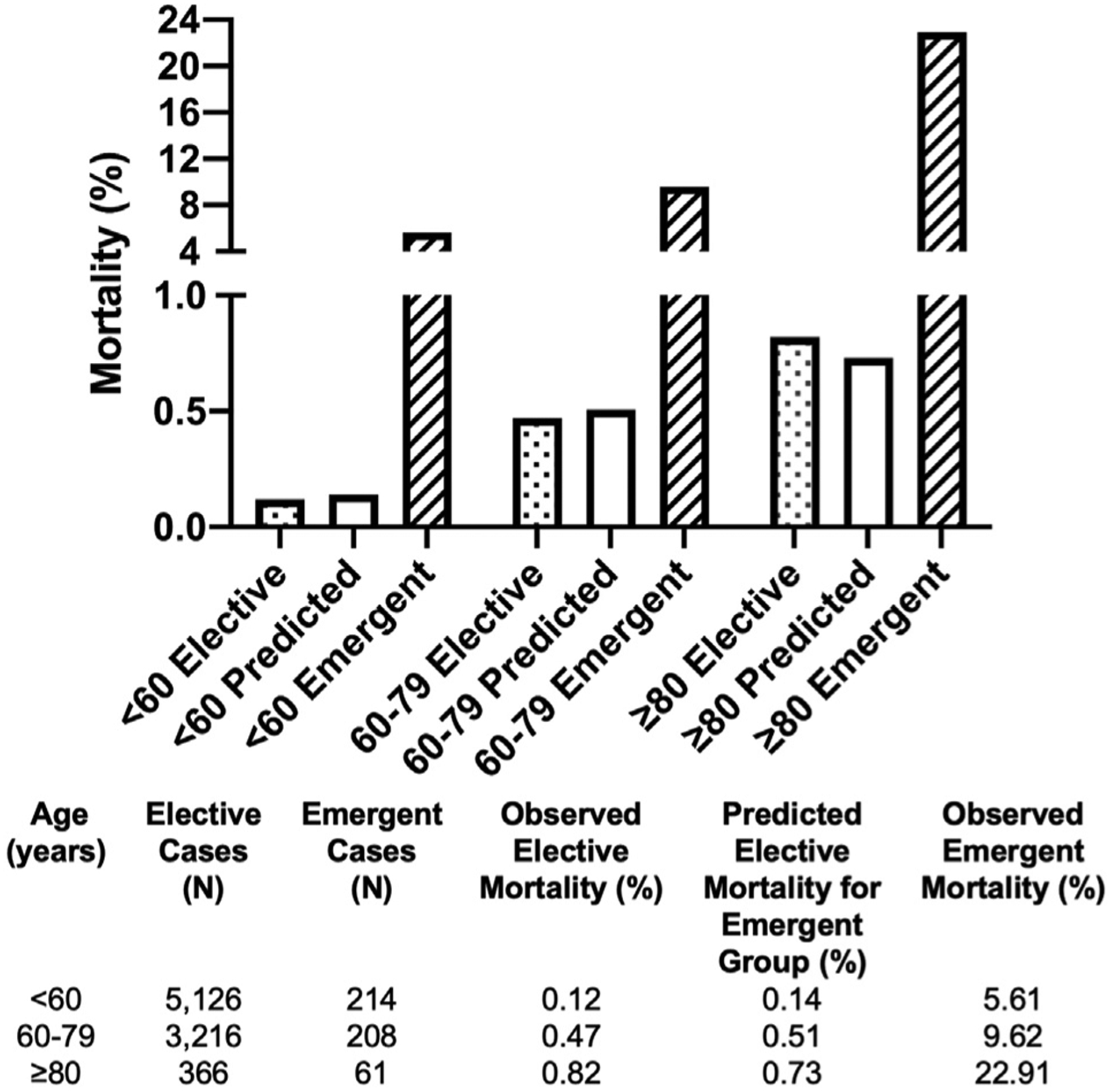
Thirty-day postoperative mortality in patients with acute incisional hernia incarceration, stratified by age. Observed mortality rates for patients undergoing elective repair and emergent repair are shown. We used the American College of Surgeons Surgical Risk Calculator to predict elective repair mortality from baseline characteristics for the 483 patients with acute incarceration
DISCUSSION
Decision-making for incisional hernia management is complex and requires assessment of both the risk of elective repair and the potential for acute incarceration. This is particularly true because patients who experience acute incarceration and require emergent operations tend to have worse outcomes.11–13 We identified contributors to increased risk of mortality and bowel resection to inform incisional hernia management. Among 483 patients with acute incarceration, age, leukocytosis, elevated creatinine, and the need for bowel resection were independently associated with 30-day mortality. Interestingly, almost half of these patients had no documentation of an earlier surgical evaluation, and estimation of elective mortality rates suggests that mortality rates comparable with those for patients who underwent elective repair could have been achieved. Taken together, these data suggest 3 potential strategies to mitigate the excess mortality of acute incisional hernia incarceration, including education of nonsurgical providers to increase surgical referral among patients with incisional hernias; expanded use of elective repair, especially in elderly patients; and immediate operation in patients presenting acutely with the potential for bowel compromise.
Elevated mortality rates after emergency operations for many procedure types have been extensively detailed, yet the inherent complexity associated with reoperation in incisional hernia cases distinguishes these cases from primary ventral hernias. As a point of reference, postoperative mortality rates after emergency groin hernia operation have been reported as 1% to 3%.14–16 In contrast, published studies on a heterogeneous mix of patients undergoing emergent operations for ventral hernias have quoted mortality rates between 4.5% and 14.3%.12,17,18 In this large cohort study of patients with known incisional hernias undergoing emergent operations, we found a 30-day mortality rate of 9.52%. Notably, age, male sex, and symptoms at diagnosis were predictive of 30-day mortality after subsequent incarceration. The association between older age and worse surgical outcomes has been well established. Studies have attributed this correlation to higher rates of complications19,20 and failure to rescue21–23 in older patients, but not necessarily the number of comorbidities.19,24 This was corroborated by our finding that age, but not the presence of kidney disease, cirrhosis, or diabetes, was associated with death after emergent hernia repair. Our earlier work also established age as a risk factor for incarceration.4 With these findings, we believe that the informed consent for older incisional hernias patients should include discussion of the combined increased risks of both acute incarceration and death after emergent repair. In addition, stronger consideration should be given to elective repair in a controlled setting.
Review of surgical decision-making revealed a population of patients who were evaluated and not offered repair due to comorbidity burden. We speculate that this is due to a perception of an elevated perioperative risk.25 However, our finding of comparable estimated elective repair mortality calls for reconsideration of the risks and benefits of elective repair. In particular, although age was associated with perioperative death, both estimated and observed elective repair mortality rates were < 1% for patients 80 years and older compared with the 22.9% mortality rate with emergent repair. This suggests that age alone should not preclude elective repair, particularly because older age is a risk factor for incarceration.4 One major limitation in studies comparing patients undergoing elective vs emergent operations is the potential for selection bias. Many elderly patients undergoing elective repair might be deemed as “highly selected,” and would be expected to have favorable outcomes in contrast to patients undergoing NOM, who perhaps were deemed too high risk for elective repair. On the contrary, we found that half of incarceration patients had no earlier documentation of a surgical evaluation and were not necessarily undergoing NOM because of a perceived high risk. It is also important to consider that risk modification and prehabilitation strategies can represent feasible approaches to further improve elective repair mortality in patients with borderline perioperative risk, particularly elderly patients.26–28 Increased surgical and nonsurgical provider awareness about the risks associated with incisional hernias in elderly patients can improve overall outcomes through individualized, patient-centered management approaches.
In addition to guiding patient-provider decision-making in an elective setting, we sought to explore perioperative characteristics that might aid in prognostication at the time of emergent repair. Aside from its association with death, bowel resection has been associated with loss of intestinal length, surgical site infection, and potential need for ostomy placement, all of which increase long-term morbidity, therefore, the need for bowel resection was explored as a secondary outcome.29,30 The predictive and prognostic value of the NLR has been described in strangulated inguinal hernias and in emergency general surgery cases in the elderly.31–33 In 1 study, an elevated NLR was associated with the need for bowel resection after incarceration, although 96% of patients in that series had either primary umbilical or groin hernias.34 The NLR, a readily available laboratory value, might be particularly valuable not only in discussing the potential for bowel resection at the time of acute incarceration, but also in triaging patients to ensure that those patients with an elevated NLR do not experience any delays before operative intervention. Additional studies will be necessary to clarify the role of NLR as a prognostic tool.
Our study cohort was unique in that it consisted of patients diagnosed with an incisional hernia in a variety of practice settings. The lack of formal guidelines renders it difficult to direct optimal management, however, it is important to consider whether nonsurgical providers should be encouraged to refer these patients for surgical evaluation, including any incidentally noted incisional hernias. We have previously described risk factors for incisional hernia incarceration, including age, female sex, and obesity, and we believe that patients with any of these risk factors, even with an incidental finding, should be referred to a surgeon.4 In addition, the natural history of incisional hernias is not well defined, and an earlier surgical evaluation should not preclude re-evaluation. We do acknowledge, however, that not all patients with incisional hernias should undergo elective repair based on the presence of the hernia alone.35 At minimum, patients should undergo surgical evaluation to generate an individualized plan based on patient-specific risk, which would benefit from future studies to refine relevant risk factors. Efforts to encourage referral for surgical consultation by nonsurgical providers, including emergency department providers and primary care providers, might ultimately improve outcomes for this common surgical disease.
This study has several limitations. Due to the retrospective study design, we were unable to fully account for all contributors to decision-making, and factors such as symptom details, quality of life, and frailty were not included. We acknowledge that the clinical documentation in the health record that we used to understand surgical decision-making or reasons for absence of surgical referral might not completely or accurately reflect the argumentation for operative or nonoperative management in some patients. Likewise, clinical documentation did not consistently provide the character and severity of symptoms, and we limited the classification of hernia-related symptoms to either “present” or “absent.” It is possible that patients had undergone surgical evaluation before our study period; however, given the potential for progression of incisional hernias, we think that an earlier evaluation does not preclude a reassessment of risks and perhaps a recent evaluation is more relevant. We were limited to available data and were not able to incorporate all potentially relevant biochemical assessments, including preoperative albumin and create-nine levels, as well as perioperative lactate levels, due to the lack of available data. Finally, we acknowledge that hernia features (eg shape, size, and location) are likely important factors in both the propensity for incarceration, as well as incarceration outcomes. These were not included in this analysis but are the subject of an ongoing investigation by our group.
CONCLUSIONS
As incisional hernias are inherently surgical sequelae, management and care of these patients should be of paramount importance to surgical providers. The observed postoperative mortality rate approaching 10% for acute incisional hernia incarceration calls for reconsideration of current multidisciplinary practices for referral and management of incisional hernias, including incidentally diagnosed incisional hernias. Specifically, our findings of an increased risk of death with increasing age with a high mortality rate compared with elective repair underscore the call for more assertive surgical management among elderly patients. Additional work is needed to fully enumerate the risk of incarceration based on patient-specific characteristics that will ultimately result in an individualized risk calculator, estimating combined risks of morbidity and mortality of elective repair, likelihood of incarceration, and morbidity and mortality risk of emergent repair for each patient.
Supplementary Material
Abbreviations and Acronyms
- aOR
adjusted odds ratio
- EHR
electronic health record
- NLR
neutrophil to lymphocyte ratio
- NOM
nonoperative management
Footnotes
Presented at the Academic Surgical Congress in Orlando, FL, February 2020.
Disclosure Information: Nothing to disclose.
REFERENCES
- 1.Beadles CA, Meagher AD, Charles AG. Trends in emergent hernia repair in the United States. JAMA Surg 2015;150: 194–200. [DOI] [PubMed] [Google Scholar]
- 2.Verhelst J, Timmermans L, Van De Velde M, et al. Watchful waiting in incisional hernia: is it safe? Surgery 2015;157: 297–303. [DOI] [PubMed] [Google Scholar]
- 3.Nieuwenhuizen J, Kleinrensink GJ, Hop WCJ, et al. Indications for incisional hernia repair: an international questionnaire among hernia surgeons. Hernia 2008;12:223–225. [DOI] [PubMed] [Google Scholar]
- 4.Dadashzadeh ER, Huckaby LV, Handzel R, et al. The risk of incarceration during non-operative management of incisional hernias: a population-based analysis of 30,998 patients. Ann Surg 2020. Jul 8 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T. Outcomes after emergency versus elective ventral hernia repair: a prospective nationwide study. World J Surg 2013;37:2273–2279. [DOI] [PubMed] [Google Scholar]
- 6.Wolf LL, Scott JW, Zogg CK, et al. Predictors of emergency ventral hernia repair: targets to improve patient access and guide patient selection for elective repair. Surgery 2016;160:1379–1391. [DOI] [PubMed] [Google Scholar]
- 7.Sneiders D, Yurtkap Y, Kroese LF, et al. Risk factors for incarceration in patients with primary abdominal wall and incisional hernias: a prospective study in 4472 patients. World J Surg 2019:1906–1913. [DOI] [PubMed] [Google Scholar]
- 8.Kokotovic D, Bisgaard T, Helgstrand F. Long-term recurrence and complications associated with elective incisional hernia repair. JAMA 2016;316:1575–1582. [DOI] [PubMed] [Google Scholar]
- 9.Quinn J, Kramer N, McDermott D. Validation of the Social Security Death Index (SSDI): an important readily-available outcomes database for researchers. West J Emerg Med 2008;9:6–8. [PMC free article] [PubMed] [Google Scholar]
- 10.American College of Surgeons. Welcome to the ACS NSQIP Surgical Risk Calculator. Available at: https://riskcalculator.facs.org/RiskCalculator/. Accessed February 12, 2020.
- 11.Mrdutt MM, Munoz-Maldonado Y, Regner JL. Impact of obesity on postoperative 30-day outcomes in emergent open ventral hernia repairs. Am J Surg 2016;212:1068–1075. [DOI] [PubMed] [Google Scholar]
- 12.Martínez-Serrano MÁ, Pereira JA, Sancho JJ, et al. Risk of death after emergency repair of abdominal wall hernias. Still waiting for improvement. Langenbecks Arch Surg 2010;395:551–556. [DOI] [PubMed] [Google Scholar]
- 13.Davies M, Davies C, Morris-Stiff G, Shute K. Emergency presentation of abdominal hernias: outcome and reasons for delay in treatment—a prospective study. Ann R Coll Surg Engl 2007;89:47–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tiernan JP, Katsarelis H, Garner JP, Skinner PP. Excellent outcomes after emergency groin hernia repair. Hernia 2010; 14:485–488. [DOI] [PubMed] [Google Scholar]
- 15.Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 1996;25:835–839. [DOI] [PubMed] [Google Scholar]
- 16.Alani A, Page B, O’Dwyer PJ. Prospective study on the presentation and outcome of patients with an acute hernia. Hernia 2006;10:62–65. [DOI] [PubMed] [Google Scholar]
- 17.Gul M, Aliosmanoglu I, Kapan M, et al. Factors affecting morbidity and mortality in patients who underwent emergency operation for incarcerated abdominal wall hernia. Int Surg 2012;97:305–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altom LK, Snyder CW, Gray SH, et al. Outcomes of emergent incisional hernia repair. Am Surg 2011;77:971–976. [PubMed] [Google Scholar]
- 19.Merani S, Payne J, Padwal RS, et al. Predictors of in-hospital mortality and complications in very elderly patients undergoing emergency surgery. World J Emerg Surg 2014;9:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lees MC, Merani S, Tauh K, Khadaroo RG. Perioperative factors predicting poor outcome in elderly patients following emergency general surgery: a multivariate regression analysis. Can J Surg 2015;58:312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheetz KH, Waits SA, Krell RW, et al. Improving mortality following emergent surgery in older patients requires focus on complication rescue. Ann Surg 2013;258:614–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scarborough JE, Pappas TN, Bennett KM, Lagoo-Deenadayalan S. Failure-to-pursue rescue: explaining excess mortality in elderly emergency general surgical patients with preexisting do-not-resuscitate orders. Ann Surg 2012;256:453–461. [DOI] [PubMed] [Google Scholar]
- 23.Sheetz KH, Krell RW, Englesbe MJ, et al. The importance of the first complication: understanding failure to rescue after emergent surgery in the elderly. J Am Coll Surg 2014;219:365–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Havens JM, Peetz AB, Do WS, et al. The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg 2015;78:306–311. [DOI] [PubMed] [Google Scholar]
- 25.Helgstrand F, Rosenberg J, Kehlet H, et al. Nationwide prospective study of outcomes after elective incisional hernia repair. J Am Coll 2013;216:217–228. [DOI] [PubMed] [Google Scholar]
- 26.Liang MK, Bernardi K, Holihan JL, et al. Modifying risks in ventral hernia patients with prehabilitation. Ann Surg 2018; 268:674–680. [DOI] [PubMed] [Google Scholar]
- 27.Hall DE, Arya S, Schmid KK, et al. Development and initial validation of the Risk Analysis Index for measuring frailty in surgical populations. JAMA Surg 2017;152:175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McIsaac DI, Jen T, Mookerji N, et al. Interventions to improve the outcomes of frail people having surgery: a systematic review. PLoS One 2017;12:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xourafas D, Lipsitz SR, Negro P, et al. Impact of mesh use on morbidity following ventral hernia repair with a simultaneous bowel resection. Arch Surg 2010;145:739–744. [DOI] [PubMed] [Google Scholar]
- 30.Gray SH, Vick CC, Graham LA, et al. Risk of complications from enterotomy or unplanned bowel resection during elective hernia repair. Arch Surg 2008;143:582–586. [DOI] [PubMed] [Google Scholar]
- 31.Zhou H, Ruan X, Shao X, et al. Clinical value of the neutrophil/lymphocyte ratio in diagnosing adult strangulated inguinal hernia. Int J Surg 2016;36:76–80. [DOI] [PubMed] [Google Scholar]
- 32.Vaughan-Shaw PG, Rees JRE, King AT. Neutrophil lymphocyte ratio in outcome prediction after emergency abdominal surgery in the elderly. Int J Surg 2012;10:157–162. [DOI] [PubMed] [Google Scholar]
- 33.Xie X, Feng S, Tang Z, et al. Neutrophil-to-lymphocyte ratio predicts the severity of incarcerated groin hernia. Med Sci Monit 2017;23:5558–5563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Köksal H, Ateş D, Nazik EE, et al. Predictive value of preoperative neutrophil-to-lymphocyte ratio while detecting bowel resection in hernia with intestinal incarceration. Ulus Travma ve Acil Cerrahi Derg 2018;24:207–210. [DOI] [PubMed] [Google Scholar]
- 35.Krpata DM, Schmotzer BJ, Flocke S, et al. Design and Initial Implementation of HerQLes: a hernia- related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 2012;215:635–642. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


