Abstract
The novel coronavirus of 2019 (COVID-19) has resulted in a global pandemic; COVID-19 has resulted in significant challenges in the delivery of healthcare, including emergency management of multiple diagnoses, such as stroke and ST-segment myocardial infarction (STEMI). The aim of this study was to identify the impacts of the COVID-19 pandemic on emergency department care of stroke and STEMI patients. In this study a review of the available literature was performed using pre-defined search terms, inclusion criteria, and exclusion criteria. Our analysis, using a narrative review format, indicates that there was not a significant change in time required for key interventions for stroke and STEMI emergent management, including imaging (door-to-CT), tPA administration (door-to-needle), angiographic reperfusion (door-to-puncture), and percutaneous coronary intervention (door-to-balloon). Potential future areas of investigation include how emergency department (ED) stroke and STEMI care has adapted in response to different COVID-19 variants and stages of the pandemic, as well as identifying strategies used by EDs that were successful in providing effective emergency care in the face of the pandemic.
Keywords: Covid-19 pandemic, Stroke, CVA, ST-segment elevation myocardial infarction, STEMI, Emergency department
1. Introduction
Coronavirus disease of 2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2), has resulted in a global pandemic; the initial outbreak occurred in late 2019 in Wuhan, Hubei Province, China. The virus spread rapidly around the world and was initially declared a pandemic on March 11, 2020. Recent variants, including the Delta and Omicron variants, have resulted in significant increases in cases and a related massive impact on the delivery of healthcare, including emergency management of multiple diagnoses, syndromes, and presentations.
It has become evident that the COVID-19 pandemic has had both direct and indirect impacts on the ability of emergency systems to deliver high quality care in acute settings. With over 69 million COVID-19 cases to date in the United States, it is unsurprising that being forced to isolate, diagnose, and treat these patients while still managing the millions of other emergent cases is taxing on both the healthcare system and healthcare professionals [1]. Resources and staffing have subsequently become a growing concern nationwide as shortage of vital resources such of PPE has greatly increased burden on emergency medicine physicians [[2], [3], [4]]. In addition to the direct impacts of the COVID-19 pandemic discussed above, to date in the United States there have been over 79 million reported cases of coronavirus infection and nearly 1 million deaths due to the virus [5].
The indirect impacts of the COVID-19 pandemic may not be as evidently clear. Emergency medicine has long been at notoriously high risk of developing burnout before the pandemic due to their long hours, shift work, and high emotional burden [6,7]. The COVID-19 pandemic has been directly shown to increase the amount of healthcare workers suffering from exhaustion and subsequent burnout symptoms in several previous studies [8,9]. It has been theorized that this increased fatigue and burnout could lead to a decreased quality of care delivered in emergency departments including care to patients with acute life threatening conditons [10]. Additionally, the need for dawning personal protective equipment and general precautions around contracting COVID may delay emergency medical service response time. It is also probable that the acuity of the patients that are seen in the emergency room is higher than ever. Patients with acute, medical events such as stroke and ST-segment elevation myocardial infarction (STEMI) have been shown in several studies to be more reluctant to present to hospitals given the fear of contracting COVID-19 infection from these institutions [[11], [12], [13], [14], [15]].
When observing the quality of care that an emergency medicine program provides, there are several quality metrics that are usually assessed. For instance, the door to balloon time has become a performance measure of regional and national quality improvement initiatives by measuring the time it takes an emergency room to triage, diagnose and treat an occluded coronary artery causing a STEMI [16,17]. Similar metrics such as the time to administer tissue plasminogen activator (tPA) in patients with acute ischemic stroke (door-to-needle time) or time to angiographic reperfusion of the ischemic brain (door-to-puncture time) are also used [[17], [18], [19]].
While it is assumed that the strain of the pandemic has negatively impacted the care of all patients as outlined above, the exact impact of the COVID-19 pandemic on these quality metrics is not yet clear. This review aims to directly quantify the impact of the COVID-19 pandemic on the care of stroke and STEMI patients in emergency departments (ED) by assessing quality metrics door-to-balloon time and door-to-needle time, and door-to-puncture time.
2. Materials and methods
A structured literature search was conducted via PubMed, the National Library of Medicine with date parameters of 3/11/2020 to 1/1/2022. The earliest date used in the literature search parameters was selected as the day the World Health Organization (WHO) declared the COVID-19 outbreak to be a pandemic, 3/11/2020. Two separate searches were conducted, one pertaining to stroke and one pertaining to STEMI. No distinction was made between stroke subtype (hemorrhagic vs ischemic stroke), or stroke location. Each search used a combination of key words with free text and Medical Subject Headings (MeSH) terms. The final search regarding stroke was ((((“emergency services” OR “Emergency Room*” OR “Emergency Department*”) OR (“Emergency Service, Hospital”[Mesh])) AND (covid 19)) AND (((((“Mortality”[Mesh]) OR (“Treatment Outcome”[Mesh])) OR ((“Time-to-Treatment”[Mesh]) OR (“time to treatment”)))) OR (“treatment outcome*” OR “Morbidity” OR “Mortality” OR “Clinical Effectiveness” OR “Outcome assessment” OR “Outcome*”))) AND (((“stroke” OR “CVA”) OR (“Stroke”[Mesh]))). The final search regarding STEMI was (((((“emergency services” OR “Emergency Room*” OR “Emergency Department*”) OR (“Emergency Service, Hospital”[Mesh])) AND (covid 19)) AND (((((“Mortality”[Mesh]) OR (“Treatment Outcome”[Mesh])) OR ((“Time-to-Treatment”[Mesh]) OR (“time to treatment”)))) OR (“treatment outcome*” OR “Morbidity” OR “Mortality” OR “Clinical Effectiveness” OR “Outcome assessment” OR “Outcome*”))) AND (covid 19)) AND ((“ST Elevation Myocardial Infarction”[Mesh]) OR (“ST elevation myocardial infarction”)).
Articles were excluded if they did not contain primary data in emergency department settings, did not make distinctions between pre- and pandemic periods, did not reported quality measures such as time to intervention, had no mortality metrics, and were not written in English. Case reports, review articles, meta-analyses, and letters were also excluded. Data from the included articles was summarized by disease type. Details about each study included are included in the following sections (Table 1 ).
Table 1.
Studies included after screening based on inclusion and exclusion criteria with demographic information. NR indicated that a value was not reported or was not reported as raw data that could be used for further analysis.
| Paper | Stroke/STEMI/Both | Pre-pandemic study period (days) | Pandemic study period (days) | Total number of patients | Number of men | Number of women | Mean age (yr) |
|---|---|---|---|---|---|---|---|
| Velez et al. [20] | Stroke | 20 | 50 | 212 | 97 | 115 | 64.5 |
| Velilla-Alonso et al. [21] | Stroke | 61 | 61 | 195 | 105 | 90 | 72 |
| Saban et al. [22] | Stroke | 177 | 60 | 14,626 | NR | NR | NR |
| Uchino et al. [23] | Stroke | 67 | 24 | 902 | NR | NR | NR |
| Rinkel et al. [24] | Stroke | 48 | 48 | 716 | 373 | 343 | 69.5 |
| Paliwal et al. [25] | Stroke | 99 | 99 | 867 | 446 | 421 | 70.75 |
| Teo et al. [26] | Stroke | 60 | 61 | 162 | 77 | 85 | 71.85 |
| Pero et al. [27] | Stroke | 365 | 364 | 594 | 305 | 289 | 71 |
| Paolucci et al. [28] | Stroke | 62 | 31 | 316 | NR | NR | NR |
| Aboul et al. [29] | Stroke | 61 | 61 | 385 | 202 | 183 | 64 |
| Walker et al. [30] | Both | 36 | 73 | 53,683 | 25,017 | 28,666 | 50 |
| Ben-Haim et al. [31] | Both | 88 | 88 | 447 | 221 | 226 | 74.2 |
| Lee et al. [32] | Both | 135 | 139 | NR | NR | NR | NR |
| Mitra et al. [33] | Both | 29 | 29 | 109 | 83 | 26 | 72.9 |
| Su et al. [34] | STEMI | 249 | 63 | 158 | 102 | 24 | 60.1 |
| Scholz et al. [35] | STEMI | 93 | 31 | 15,800 | 11,558 | 4242 | 69.1 |
| Choudhary et al. [36] | STEMI | 31 | 31 | 1777 | 1314 | 463 | 61.4 |
| Rangé et al. [37] | STEMI | 424 | 31 | 2064 | 1563 | 501 | NR |
| Matsubara et al. [38] | STEMI | 338 | 337 | 295 | 167 | 128 | 72.7 |
| Sum | 2443.0 | 1681.0 | 93,308.0 | 41,630.0 | 35,802.0 | 943.5 | |
| Mean | 128.6 | 88.5 | 5183.8 | 2775.3 | 2386.8 | 67.4 | |
| Median | 67.0 | 61.0 | 520.5 | 221.0 | 226.0 | 70.1 |
Primary data extracted for strokes were the number of strokes presenting to EDs, door-to-needle time, and door-to-puncture-time in the pre-pandemic and pandemic periods. Door-to-needle time was defined as time from initial presentation to time of thrombolytic administration. Door-to-puncture time was defined as time from presentation to start of thrombectomy procedure. Secondary outcomes included onset-to-door time, door-to-CT time, and mortality for stroke patients presenting to emergency departments in the pre-pandemic and pandemic periods. Onset-to-door time was denied as time from when a patient first became symptomatic to presentation, while door-to-CT time was defined as time from a patient's initial presentation to obtaining a non-contrast CT head.
Primary data extracted in regards to STEMIs were number of cases presenting to EDs and door-to-balloon time in the pre-pandemic and pandemic periods. Secondary outcomes were onset-to-door time and mortality in both periods. Door-to-balloon time was defined as the time form presentation to percutaneous coronary intervention. Onset-to-door time was defined as the time from first reported symptom to prestation.
Statistical analysis was performed using XLSTAT software. Student two-tailed t-test was used to evaluate for statistically significant differences between means. Statistical significance was set at alpha <0.05.
3. Results
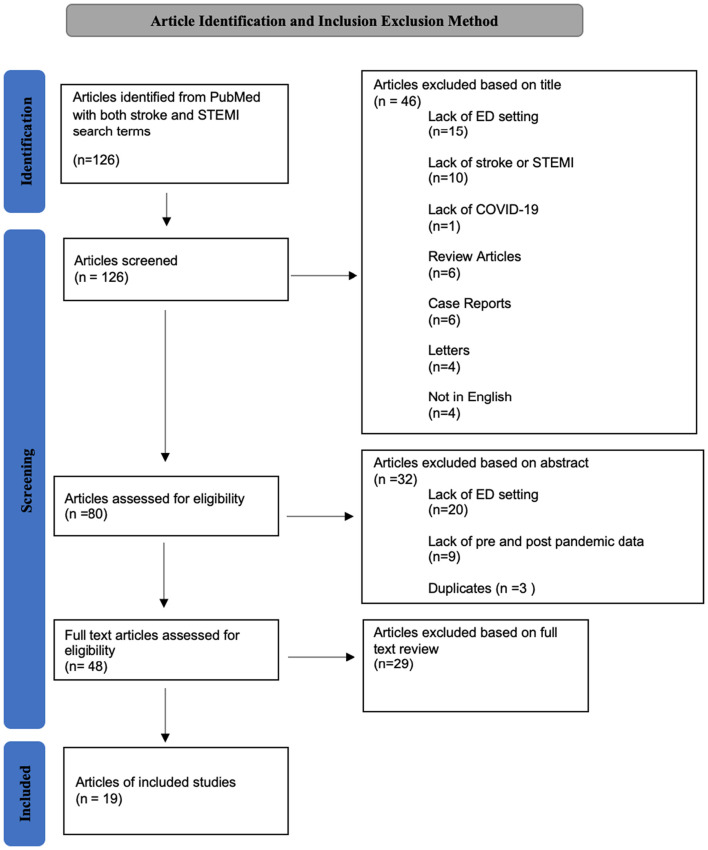
The initial literature search identified 126 articles, of which 19 met inclusion criteria (Fig. 1 ). Of the 19 articles included in this study 10 pertained to stroke only, 5 pertained to STEMI only, and 4 pertained to both stroke and STEMI. The average number of emergency department patients included in each article was 5075.72 (range 109 to 53,683) with a median of 416. The average number of total patients including those in in-patient and designated stroked center settings was 5183.7 (range 109 to 53,683) with median of 520.5 patients. Men made up an average of 221 (42.5%) of included article's study populations and the mean age was 70.1 years. Pre-pandemic study periods ranged from 20 to 424 days, with mean pre-pandemic study period length being 128.58 days. Pandemic study periods ranged from 24 to 364 days, with a mean pandemic study period length of 88.47 days (See Fig. 2, Fig. 3).
Fig. 1.
Number of articles reviewed and reason for exclusion.
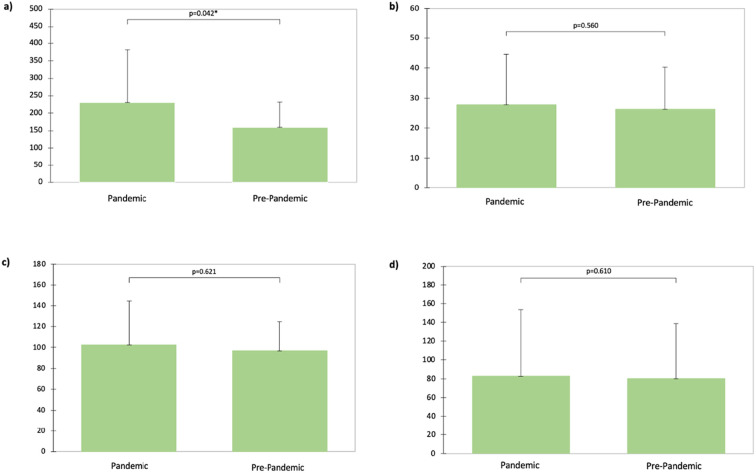
Fig. 2.
Stroke mean quality measures for the pandemic and pre-pandemic periods. All times are measured in minutes and are: a) onset-to-door time, b) door-to-CT time, c) door-to-puncture time, d) door-to-needle time.
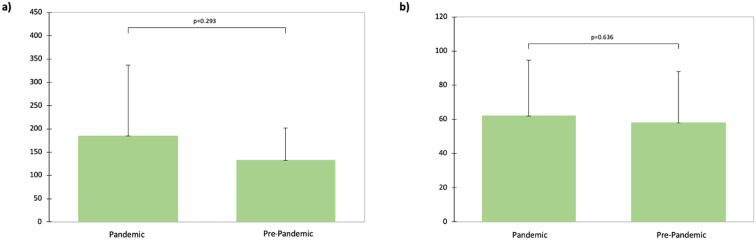
Fig. 3.
STEMI mean quality measures for the pandemic and pre-pandemic periods. All times are measured in minutes and are: a) onset-to-door time, b) door-to-balloon time.
3.1. Stroke
Across included articles with data pertaining to ED stroke presentations there were a total of 2596 confirmed stroke presentations in the pre-pandemic period with mean of 185.43 (range 17 to 536). In the pandemic period a total of 1863 were reported with a mean of 133.1 (range 18 to 298). This constitutes a negative 28.24% change between the pre-pandemic and pandemic study periods. The difference between the means was 52.36 (95% CI −103.66 to −1.05). There was a statically significant difference in the mean number of stroke presentations between the two periods with t = −2.21 (p-value = 0.046).
Of the 14 papers with stroke data 11 reported door-to-needle time. The mean pre-pandemic door-to-needle time was 80.19 min (min) (range 28 to 202.2), and the mean pandemic study period door-to-needle time was 82.76 (range 31 to 232.8) min. The percent change of these values is a positive 3.21%, representing an increase in door-to-needle time between the pre-pandemic and pandemic study periods. There was no significant between door-to-needle time in the pre-pandemic and pandemic periods with a difference between the means of 2.57 (95% CI −8.33 to 13.57) and t = 0.53 (p-value = 0.061).
Eleven papers with stroke data reported door-to-puncture times for the pre-pandemic and pandemic periods. The mean pre-pandemic door-to-puncture time was 96.75 min (range 55 to 145); and the pandemic period mean door-to-puncture time was 102.18 min (range 58 to 207). Difference between the means was 5.43 (95% CI -18.3 to 29.15) with two-tailed test = 2.23 (p-value = 0.062). The percent change between the means was 5.61% indicating an increase in the door-to-puncture time between the pre-pandemic and pandemic periods.
Onset of symptoms from the time a patient presented to an ED (onset-to-door time) was investigated as a secondary outcome. Nine of the 14 articles reporting stroke data also reported onset-to-door time. Mean onset-to-door time in the pre-pandemic period was 159.61 min (range 77 to 288), compared to 230.89 min (range 83 to 564) in the pandemic period. There was a significant difference in onset-to-door time between the two periods with a difference between means of 71.28 (95% CI 3.38, 139.18) and; two-tailed t-test = 0.51 (p- value = 0.042). There was also a percent 44.66% change in onset-to-door time between the pre-pandemic and pandemic study periods. Additionally, 8 of the 14 stroke papers reported door-to-CT time. Based on this data the mean pre-pandemic and pandemic period door-to-CT time was 21.19 min (range 8 to 52) and 27.69 min (range 13 to 65) respectively. The percent change between the means was 5.73. There was no significant difference between the means (1.5 min 95% CI −4.29 to 7.29) with t = 0.61 (p-value = 0.56). However there was a considerable difference between the minimum door-to-CT time between the two study periods (8 vs 13 min).
Mortality due to stroke was reported in 7 articles. The average mortality was similar between the two periods of interest with a mean pre-pandemic and pandemic period mortality of 13.19 (range 1 to 34) and 13.57 (range 3 to 40). The difference between the means was 0.39 (95% CI −3.47 to 4.24). The difference between the means was not significant with t = 0.25 (p-value = 0.82).
3.2. STEMI
A total of 2819 and 201 STEMI patients were reported across all included articles in the pre-pandemic and pandemic periods respectively. The mean number of pre-pandemic STEMI cases presenting to EDs was 313.22 while the mean number of pandemic period STEMI cases was 100.11. This constitutes a percent change of −68.04, with a difference between the means of −213.11 (95% CI −466.7 to 40.48). Two-tailed test between the means showed no significant difference (t = −1.94, p-value = 0.089).
Door-to-balloon time was reported in 7 of the 9 articles included pertaining to ED STEMI presentations. The mean door-to-balloon time in the pre-pandemic period was 57.97 min (range 29.0 to 119.0), compared to 61.94 min (range 22.7 to 122.0) in the pandemic period. Percent change between the means was calculated to be 6.85. Difference between the means was found to be 3.87 (95% CI −15.54 to 23.48). There was no significant difference between the mean door-to-balloon times in the two study periods (two-tailed test = 0.49, p-value = 0.64).
Onset-to-door time was reported in 5 of the articles pertaining to STEMI included in this study. The mean onset-to-door time was 132.22 (range 69 to 238) minutes in the pre-pandemic period compared to 184.68 min (range 78 to 450) in the pandemic period. The percent change between the means was 33.44, and the difference between the means was 52.46 (95% CI −67.9 to 172.82). However, the difference between the means was not significantly different with two-tailed test = 1.21 and p-value = 0.29.
Mortality was reported in 8 included articles. The mean pre-pandemic and pandemic period mortality reported due to STEMI was 51.38 (range 3 to 169) and 34 (range 1 to 205) respectively. The percent change between the two means was −33.82. The difference between the means was −17.38 (95% CI −49.22 to 14.49). Two-tailed t-test showed no significant difference with t = −1.29 (p-value = 0.24).
4. Discussion
While direct clinical outcomes related to COVID-19, such as case incidence rate, mortality, and morbidity, have been closely tracked; the indirect effects of the pandemic are multifactorial and less clearly established. Various reports and previous studies have demonstrated that the public fear regarding contracting the virus, especially in early stages of the pandemic, resulting in decreased utilization of emergency medical services [12,37,38]. Other studies have reported significant delays in acute care for a variety of emergent medical conditions, such as stroke and STEMI [[41], [42], [43], [44], [45]]. Finally, it has been well established that the COVID-19 pandemic has led to increased burnout for healthcare workers due to emotional exhaustion and decreased staff availability [44]. In this narrative review we set out to quantify the extent to which the pandemic affected the acute management of stroke and STEMI in the ED setting using commonly used quality measures.
Multiple previous studies have reported decreased numbers of stroke and STEMI cases presenting to EDs since the start of the pandemic [39,40]. While we did not find a statically significant decrease in the number of STEMI cases, there was an absolute decrease in the number of both STEMI and stroke cases seen between the pre-pandemic and pandemic periods. However, we did find a statistically significant decrease in the number of stroke cases presenting to EDs. While the national incidence of stroke had been reported to be decreasing in the years leading up to the COVID-19 pandemic, the sharp decrease seen between the pre-pandemic and pandemic periods seen in this study makes it unlikely to be an organic decrease in the incidence of stroke. It is more likely a reflection of public hesitancy to present to the ED settings due to concerns of contracting covid which has been previously reported [5,45].
A statistically significant increase in onset-to-door time was found among stroke patients with a mean of 160 min in the pre-pandemic period to 231 min during the pandemic. This further supports previous literature that had found patients took longer to present to the ED after developing symptoms during the pandemic period. This change suggests public fear of potential nosocomial infection and hesitancy to increase contact with healthcare faculties during the COVID-19 pandemic has had a negative impact on the care of stroke patients since the start of the COVID-19 pandemic [[46], [47], [48], [49], [50], [51]]. Other factors contributing to increased onset-to-door time may be delays in emergency medical services (EMS). These transport and first responder services are a important part in management of time sensitive medical emergencies such as stroke and STEMI. During the pandemic increased EMS call volumes were reported compared to pre-pandemic periods placing additional strain on these services [[52], [53], [54],]. Also, delays in EMS response time including time form EMS call to scene arrival and scene arrival to door time have been reported [52]. However, the majority of studies found increased time form symptom onset to EMS call between pre-pandemic and pandemic periods [[55], [56], [57]]. While EMS may play a role in the increased onset-to-door time found in this study, the increased time to EMS call found in articles suggest that it may be due increased patient hesitancy to seek medical care due to fear of COVID-19 exposure.
The decrease in total number of stroke cases and increase in onset-to-door time for stroke both reflect a deleterious effect of the pandemic on the management of stroke. However, we found that there was no significant change in door-to-CT, door-to-needle, door-to-puncture times, or mortality among stroke cases. These metrics reflect the speed with which stroke patients are directed to appropriate therapy upon presentation to the ED. The fact that there was not a significant increase in these markers suggests that EDs were able to accommodate the COVID-19 cases and protocols while also maintaining appropriate care for stroke patients. Similarly, door-to-balloon time and mortality among STEMI patients, was not found to be significantly different between the pre-pandemic and pandemic periods. This further demonstrates that managing COVID-19 cases and changes in isolation protocols did not preclude EDs from continuing to provide timely care for patients with STEMI.
One significant limitation of this analysis was that the included studies had a higher volume of pre-pandemic data compared to the pandemic period. The limited case volume during the pandemic period was largely due to the novelty of the COVID-19 pandemic and limited amount of published data during the search period compared to the literature regarding stroke and STEMI before the pandemic. Contributing to this was the search performed in this narrative review was limited to the National Library of Medicine. Furthermore, the pandemic has not been a singular change in terms of stress placed on the healthcare system. There have been peaks and troughs in terms of case load as well as multiple virus variants that have affected EDs differently. Another limitation of this study was that it did not stratify results by different phases of the pandemic. ED utilization has been shown to vary in time throughout the pandemic due to a number of factors [58]. These variations were not accounted for in our analysis which instead investigated the pre-and pandemic periods as a whole. As a result variations in stroke and STEMI care in EDs that may differ through pandemic phases may be masked in our analysis.
5. Summary
In summary, our analysis indicates that there was not a significant change in time required for key interventions for stroke and STEMI, including imaging (door-to-CT), tPA administration (door-to-needle), angiographic reperfusion (door-to-puncture), and percutaneous coronary intervention (door-to-balloon). In order to expand on these findings and more fully elucidate the effects of the pandemic on emergency medicine, further studies are needed. Potential future areas of investigation include how ED stroke and STEMI care has adapted in response to different COVID-19 variants or stages of the pandemic, and identifying strategies used by EDs that were successful in providing effective emergency care in the face of the pandemic.
Credit authorship contribution statement
W.H. Banfield: Writing – review & editing, Writing – original draft, Validation, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. O. Elghawy: Writing- review & editing, Writing - original draft, Resources, Methodology, Investigation, Formal analysis, Conceptulization. A. Dewanjee: Writing – review & editing, Writing – original draft, Resources, Methodology, Investigation, Formal analysis, Conceptualization. W.J. Brady: Writing - review & editing, Writing - original draft, Resources, Methodology, Investigation, Formal analysis, Conceptulization.
Declaration of Competing Interest
To whom it may concern
On behalf of all authors, I am submitting the following manuscript (“Cardiopulmonary Resuscitation Training: A Narrative Review Comparing Traditional Educational Programs with Alternative, Reduced-resource Methods of CPR Instruction for Lay Providers”) for consideration of publication in The American Journal of Emergency Medicine. None of the authors have any conflicts to declare.
Acknowledgments
The authors thank John S. Wang for his help in preparing this manuscript for publication. No primary funders or grants were involved utilized in this research.
References
- 1.CDC COVID Data Tracker. Centers for Disease Control and Prevention. Published March 28. 2020. https://covid.cdc.gov/covid-data-tracker Accessed January 20, 2022.
- 2.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of Covid-19. New Engl J Med. 2020 doi: 10.1056/NEJMsb2005114. Published online March 23. [DOI] [PubMed] [Google Scholar]
- 3.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323(15):1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 4.Livingston E., Desai A., Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020;323(19):1912–1914. doi: 10.1001/jama.2020.5317. [DOI] [PubMed] [Google Scholar]
- 5.CDC COVID Data Tracker. Centers for Disease Control and Prevention. Published March 28. 2020. https://covid.cdc.gov/covid-data-tracker Accessed March 16, 2022.
- 6.Lim R., Aarsen K.V., Sara Gray S., Rang L., Fitzpatrick J., Fischer L. Emergency medicine physician burnout and wellness in Canada before COVID19: a national survey. CJEM. 2020;22:603–607. doi: 10.1017/cem.2020.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323(15):1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 8.Freund Y. The challenge of emergency medicine facing the COVID-19 outbreak. Eur J Emerg Med. 2020;27:155. doi: 10.1097/MEJ.0000000000000699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fitzpatrick K., Patterson R., Morley K., Stoltzfus J., Stankewicz H. Physician wellness during a pandemic. West J Emerg Med. 2020;21(6):83–87. doi: 10.5811/westjem.2020.7.48472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stehman C.R., Testo Z., Gershaw R.S., Kellogg A.R. Burnout, drop out, suicide: physician loss in emergency medicine, part I [published correction appears in West J Emerg Med. 2019 Aug 21;20(5):840-841] West J Emerg Med. 2019;20(3):485–494. doi: 10.5811/westjem.2019.4.40970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teoh S.E., Masuda Y., Tan D.J.H., et al. Impact of the COVID-19 pandemic on the epidemiology of out-of-hospital cardiac arrest: a systematic review and meta-analysis. Ann Intensive Care. 2021;11(1):169. doi: 10.1186/s13613-021-00957-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glober N.K., Supples M., Faris G., et al. Out-of-hospital cardiac arrest volumes and characteristics during the COVID-19 pandemic. Am J Emerg Med. 2021;48:191–197. doi: 10.1016/j.ajem.2021.04.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gale R., et al. Public perspectives on decisions about emergency care seeking for care unrelated to COVID-19 during the COVID-19 pandemic. JAMA Network Open. 2021;4,8:e2120940. doi: 10.1001/jamanetworkopen.2021.20940. 2 Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kiss P., Carcel C., Hockham C., Peters S.A.E. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2021;7(1):18–27. doi: 10.1093/ehjqcco/qcaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scquizzato T., et al. The other side of novel coronavirus outbreak: fear of performing cardiopulmonary resuscitation. Resuscitation. 2020;150:92–93. doi: 10.1016/j.resuscitation.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Menees D.S., Peterson E.D., Wang Y., et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369(10):901–909. doi: 10.1056/NEJMoa1208200. [DOI] [PubMed] [Google Scholar]
- 17.Park J., Choi K.H., Lee J.M., et al. Prognostic implications of door-to-balloon time and onset-to-door time on mortality in patients with ST-segment–elevation myocardial infarction treated with primary percutaneous coronary intervention. J Am Heart Assoc. 2019;8(9) doi: 10.1161/JAHA.119.012188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehta B.P., Leslie-Mazwi T.M., Chandra R.V., et al. Reducing door-to-puncture times for intra-arterial stroke therapy: a pilot quality improvement project. J Am Heart Assoc. 2014;3(6) doi: 10.1161/JAHA.114.000963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saver J.L., Smith E.E., Fonarow G.C., Reeves M.J., Zhao X., Olson D.M., et al. The “golden hour” and acute brain ischemia: presenting features and lytic therapy in >30,000 patients arriving within 60 minutes of stroke onset. Stroke. 2010;41:1431–1439. doi: 10.1161/STROKEAHA.110.583815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Velez F.G.S., Alvarado-Dyer R., Brutto V.J.D., Carrión-Penagos J., Bulwa Z., Prabhakaran S. Impact of Covid-19 on stroke code activations, process metrics, and diagnostic error. Neurohospitalist. 2021;11(3):197–203. doi: 10.1177/1941874420976517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Velilla-Alonso G., García-Pastor A., Rodríguez-López Á., et al. Acute stroke care during the COVID-19 pandemic: reduction in the number of admissions of elderly patients and increase in prehospital delays. Cerebrovasc Dis. 2021;50(3):310–316. doi: 10.1159/000514140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saban M., Reznik A., Shachar T., Wilf-Miron R., Sivan-Hoffmann R. The effect of the COVID-19 pandemic on ED referrals and care for stroke patients: a four-year comparative study. J Crit Care. 2021;62:230–234. doi: 10.1016/j.jcrc.2020.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uchino K., Kolikonda M.K., Brown D., et al. Decline in stroke presentations during COVID-19 surge. Stroke. 2020;51(8):2544–2547. doi: 10.1161/STROKEAHA.120.030331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rinkel L.A., Prick J.C.M., Slot R.E.R., et al. Impact of the COVID-19 outbreak on acute stroke care. J Neurol. 2021;268(2):403–408. doi: 10.1007/s00415-020-10069-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paliwal P.R., Tan B.Y.Q., Leow A.S.T., et al. Impact of the COVID-19 pandemic on hyperacute stroke treatment: experience from a comprehensive stroke Centre in Singapore. J Thromb Thrombolysis. 2020;50(3):596–603. doi: 10.1007/s11239-020-02225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Teo K.C., Leung W.C.Y., Wong Y.K., et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51(7):2228–2231. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pero G., Dória H.M., Giavarini M., et al. Impact of the SARS-COV-2 pandemic on the endovascular treatment of acute stroke - an Italian single-center experience. J Stroke Cerebrovasc Dis. 2021;30(10):106028. doi: 10.1016/j.jstrokecerebrovasdis.2021.106028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paolucci M., Biguzzi S., Cordici F., et al. Impact of COVID-19 pandemic on acute stroke care: facing an epidemiological paradox with a paradigm shift. Neurol Sci. 2021;42(2):399–406. doi: 10.1007/s10072-020-04914-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aboul Nour H., Affan M., Mohamed G., et al. Impact of the COVID-19 pandemic on acute stroke care, time metrics, outcomes, and racial disparities in a Southeast Michigan health system. J Stroke Cerebrovasc Dis. 2021;30(6):105746. doi: 10.1016/j.jstrokecerebrovasdis.2021.105746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walker L.E., Heaton H.A., Monroe R.J., et al. Impact of the SARS-CoV-2 pandemic on emergency department presentations in an integrated health system. Mayo Clin Proc. 2020;95(11):2395–2407. doi: 10.1016/j.mayocp.2020.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ben-Haim G., Zabatani A., Orion D., Leshem E., Irony A., Katorza E. The pandemic’s impacts on patients without Covid-19 on multidisciplinary aspects in emergency medicine care. Intern Emerg Med. 2021;16(8):2261–2268. doi: 10.1007/s11739-021-02680-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee K.D., Lee S.B., Lim J.K., et al. Providing essential clinical care for non-COVID-19 patients in a Seoul metropolitan acute care hospital amidst ongoing treatment of COVID-19 patients. J Hosp Infect. 2020;106(4):673–677. doi: 10.1016/j.jhin.2020.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mitra B., Mitchell R.D., Cloud G.C., et al. Presentations of stroke and acute myocardial infarction in the first 28 days following the introduction of state of emergency restrictions for COVID-19. Emerg Med Australas. 2020;32(6):1040–1045. doi: 10.1111/1742-6723.13621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Su Y.H., Wu K.H., Su C.M., et al. Influence of the coronavirus disease 2019 pandemic on patients with ST-segment elevation myocardial infarction in Taiwan. Emerg Med Int. 2021;2021 doi: 10.1155/2021/5576220. 5576220. Published 2021 Apr 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scholz K.H., Lengenfelder B., Thilo C., et al. Impact of COVID-19 outbreak on regional STEMI care in Germany. Clin Res Cardiol. 2020;109(12):1511–1521. doi: 10.1007/s00392-020-01703-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choudhary R., Gautam D., Mathur R., Choudhary D. Management of cardiovascular emergencies during the COVID-19 pandemic. Emerg Med J. 2020;37(12):778–780. doi: 10.1136/emermed-2020-210231. [DOI] [PubMed] [Google Scholar]
- 37.Rangé G., Hakim R., Beygui F., et al. Incidence, delays, and outcomes of STEMI during COVID-19 outbreak: analysis from the France PCI registry [published online ahead of print, 2020 Nov 23] J Am Coll Emerg Physicians Open. 2020;1(6):1168–1176. doi: 10.1002/emp2.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsubara Y., Izumikawa T., Washimi S., et al. Impact of the SARS-CoV-2 pandemic on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction. Int Heart J. 2021;62(6):1230–1234. doi: 10.1536/ihj.21-308. [DOI] [PubMed] [Google Scholar]
- 39.Grunau B., Helmer J., Lee S., et al. Decrease in emergency medical services utilization during early stages of the COVID-19 pandemic in British Columbia. CJEM. 2021;23(2):237–241. doi: 10.1007/s43678-020-00062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huynh K. Reduced hospital admissions for ACS - more collateral damage from COVID-19. Nat Rev Cardiol. 2020;17(8):453. doi: 10.1038/s41569-020-0409-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Luca G., Verdoia M., Cercek M., et al. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76(20):2321–2330. doi: 10.1016/j.jacc.2020.09.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Erol M.K., Kayıkçıoğlu M., Kılıçkap M., et al. Treatment delays and in-hospital outcomes in acute myocardial infarction during the COVID-19 pandemic: a nationwide study. Anatol J Cardiol. 2020;24(5):334–342. doi: 10.14744/AnatolJCardiol.2020.98607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bersano A., Kraemer M., Touzé E., et al. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur J Neurol. 2020;27(9):1794–1800. doi: 10.1111/ene.14375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Janke A.T., Gettel C.J., Haimovich A., Kocher K.E., Krumholz H.M., Venkatesh A.K. Changes in emergency department arrival times for acute myocardial infarction during the COVID-19 pandemic suggest delays in care seeking [published online ahead of print, 2022 Feb 2] Circ Cardiovasc Qual Outcomes. 2022 doi: 10.1161/CIRCOUTCOMES.121.008402. CIRCOUTCOMES121008402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gutovitz S., Pangia J., Finer A., Rymer K., Johnson D. Emergency department utilization and patient outcomes during the COVID-19 pandemic in America. J Emerg Med. 2021;60(6):798–806. doi: 10.1016/j.jemermed.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rodriguez R.M., Medak A.J., Baumann B.M., et al. Academic emergency medicine physicians’ anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID-19 pandemic. Acad Emerg Med. 2020;27(8):700–707. doi: 10.1111/acem.14065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scquizzato T., et al. The other side of novel coronavirus outbreak: fear of performing cardiopulmonary resuscitation. Resuscitation. 2020;150:92–93. doi: 10.1016/j.resuscitation.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Czeisler M.É., Marynak K., Clarke K.E.N., et al. Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257. doi: 10.15585/mmwr.mm6936a4. 10.15585/mmwr.mm6936a4 Published 2020 Sep 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anderson K.E., McGinty E.E., Presskreischer R., Barry C.L. Reports of forgone medical care among US adults during the initial phase of the COVID-19 pandemic. JAMA Netw Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.34882. e2034882. Published 2021 Jan 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Taylor S., Landry C.A., Rachor G.S., Paluszek M.M., Asmundson G.J.G. Fear and avoidance of healthcare workers: an important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. 2020;75:102289. doi: 10.1016/j.janxdis.2020.102289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Laura E.W., J.E. Hawkins and S. Langness et al. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. Nejm Catalyst Innovations in Care Delivery 10.1056/CAT.20.0193. [DOI]
- 52.Handberry M., Bull-Otterson L., Dai M., et al. Changes in emergency medical services before and during the COVID-19 pandemic in the United States, January 2018-December 2020. Clin Infect Dis. 2021;73(Suppl. 1):S84–S91. doi: 10.1093/cid/ciab373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Al Amiry A., Maguire B.J. Emergency medical services (EMS) calls during COVID-19: Early lessons learned for systems planning (a narrative review) Open Access Emerg Med. 2021;13:407–414. doi: 10.2147/OAEM.S324568. Published 2021 Sep 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee S.H., Mun Y.H., Ryoo H.W., et al. Delays in the management of patients with acute ischemic stroke during the COVID-19 outbreak period: a multicenter study in Daegu, Korea. Emerg Med Int. 2021;2021:6687765. doi: 10.1155/2021/6687765. Published 2021 Mar 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Al Amiry A., Maguire B.J. Emergency medical services (EMS) calls during COVID-19: early lessons learned for systems planning (A narrative review) Open Access Emerg Med. 2021;13:407–414. doi: 10.2147/OAEM.S324568. Published 2021 Sep 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ramos-Pachón A., García-Tornel Á., Millán M., et al. Bottlenecks in the acute stroke care system during the COVID-19 pandemic in Catalonia. Cerebrovasc Dis. 2021;50(5):551–559. doi: 10.1159/000516309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baldi E., Auricchio A., Cresta R., et al. Patient voluntarily delays call to emergency medical system for ST-elevation myocardial infarction during COVID-19 pandemic. Int J Cardiol Heart Vasc. 2021;35:100824. doi: 10.1016/j.ijcha.2021.100824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barten D.G., Latten G.H.P., van Osch F.H.M. Reduced emergency department utilization during the early phase of the COVID-19 pandemic: viral fear or lockdown effect? [published online ahead of print, 2020 Aug 12] Disaster Med Public Health Prep. 2020:1–4. doi: 10.1017/dmp.2020.30. [DOI] [PMC free article] [PubMed] [Google Scholar]