Abstract
Background
Understanding the pattern of co-occurring mental illness in patients with substance use disorders (SUDs) is essential in improving the prevention and treatment of substance use-related problems. This study examined the pattern of SUDs, the associated co-occurring psychiatric morbidities, and associated factors among patients with SUDs managed at a tertiary health center.
Methods
The records of patients who presented with SUDs between 2010 and 2019 were examined. Socio-demographics of interest were extracted from case files. Substance use diagnoses, as well as associated co-occurring mental illness, were extracted and entered into SPSS software. Bivariate analyses including the risk of developing co-occurring mental disorder were calculated.
Findings
For most patients, the initiation of substance use was before the age of 21 years, while the onset of SUDs was between 21-30 years. Cannabis use disorders (CUDs), alcohol use disorders (AUDs), and nicotine use disorders (NUDs) were the commonest SUDs. Compared with those with CUDs, non-users of cannabis were significantly less likely to develop co-occurring mental illness [odds ratio (OR) = 0.25, 95% confidence interval (CI) =0.13-0.42, P = 0.001]. Those with tramadol use disorders (OR = 2.13, 95% CI = 1.03-4.41, P = 0.040) and those without pentazocine use disorders (P = 0.003) were more likely to have a comorbid mental illness. Patients with AUDs (P = 0.001), CUDs (P = 0.001), NUDs (P = 0.001), and tramadol use disorders (P = 0.045) were significantly more likely to be multiple substance users.
Conclusion
Results suggest an association between SUDs and co-occurring mental illness, though differences in these associations were noticed across the categories of substances. This emphasizes a holistic approach to prevention and care of patients presenting with SUDs.
Keywords: Dual diagnosis, Mental disorders, Substance-related disorders, Substance dependence
Introduction
Alcohol and other substance use continue to impact negatively on the productivity, health, economy, and social aspects of our societies.1 There is a growing challenge of the burdens of substance use disorders (SUDs) and mental illnesses in general, posed for health systems in both developed and developing countries. It is a major contributor to disability-adjusted life years (DALYs), years of life lost (YLLs) due to premature mortality, as well as years lived with disability (YLDs).2 Apart from the direct burden of substance use, it exerts a negative effect on other health outcomes, and along with other mental illnesses constitutes the leading cause of YLDs worldwide.1 Across the countries of the world, SUDs account for about 20 million DALYs and 8.6 million YLLs,2,3 and remain a continuous health crisis.4
Globally, of all SUDs, alcohol use disorders (AUDs) present with the greatest burden with 100.4 million estimated cases in 2016 followed by opioid dependence with an estimated 26.8 million cases and cannabis dependence with an estimated 22.1 million cases.1 In Nigeria, on the other hand, similar high burden had been reported from national surveys and specific population-based studies.5-8 According to Adamson et al. (2015), alcohol had the highest prevalence, while cannabis was the commonest illicit drug used. Among persons with mental illness, on the other hand, alcohol was the commonest substance ever used followed by tobacco and cannabis in that order.9 However, harmful tobacco use was reported in about 45% and about a third with harmful alcohol and cannabis use in the preceding 3 months.9
There is continuous evidence suggesting that people with SUDs also experience other psychiatric disorders.10 This is often bi-directional, with many people with other psychiatric diagnoses presenting with SUDs.11 Studies have shown that about half of people with mental illness often experience substance-related disorders at some points in the course of the illness, and vice versa.11 Several reasons have been attributed to the co-occurrence of SUDs and other psychiatric conditions. Firstly, both disorders are associated with common risk factors, and secondly, substance use may alter brain structure, thus increasing the risk of developing mental illness.11
The prevalence of mental disorders among those with substance use is higher than the general population, and the burden of disease due to SUDs varies significantly across different psychiatric settings and often co-occurs with other psychiatric diagnoses.10 The co-occurrence impacts negatively the course and the outcome of both diseases. This calls for the need for a comprehensive approach in the evaluation and management of both conditions. In this study, we examined the pattern of SUDs, the associated psychiatric comorbidities, and factors associated with them among patients with SUDs managed at the Ekiti State University Teaching Hospital in Ado-Ekiti, Nigeria.
Methods
Design and setting: In this retrospective study, we identified patients who primarily presented with or had SUDs as the major presentation to the Department of Psychiatry of the Ekiti State University Teaching Hospital. The Ekiti State University Teaching Hospital, established in 2008, served as a secondary health facility prior to 2008 when there was no psychiatrist in the mental health unit of the hospital. In addition to other specialties of medicine, the Ekiti State University Teaching Hospital has a department of psychiatry with psychiatrists, clinical psychologists, and psychiatric nurses. Aside serving people from within Ekiti State, the hospital also attends to people from neighboring states.
Participants: Participants in the study were patients seen between October 2010 and September 2019 who presented with SUDs with or without other psychiatric disorders. Patients were evaluated and reviewed by a consultant psychiatrist or a senior resident and the diagnosis was made using the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) criteria. Those with specific harmful substance use or dependence were further classified as having SUDs for that specific substance.
Data collection: Data on socio-demographic characteristics such as age, level of education, gender, duration of substance use before presentation, primary SUD, and associated psychiatric diagnoses were retrieved from the case files by one of the researchers. The retrieved data were entered into SPSS software (version 21, IBM Corporation, Armonk, NY, USA).
Data collected were coded and analyzed using the SPSS. Data were presented using descriptive statistics such as frequency tables, figures, mean, and standard deviation (SD), and inferential statistics were calculated using bivariate analyses, chi-square test, including odds ratio (OR). A P-value ≤ 0.05 was adjudged to be significant.
Ethical considerations: Permission to carry out the study was obtained from departmental head and confidentiality of all information obtained from the case files was ensured.
Results
Socio-demographic characteristics: Of the total number of 2643 cases reviewed, 215 presented with SUDs. Their ages ranged from 15 to 50 years, with a mean and SD of 28.70 ± 8.40 years, while the age of onset of substance use ranged between 10 and 50 years with a mean and SD of 28.70 ± 22.25 years. Majority of cases were men (n = 207, 96.3%), between the age of 22 and 30 years (55.8%) at the time of presentation, less or equal to 21 years (55.1%) at the age of onset, and single (80.5%) at the time of presentation.
Pattern of substance use: Cannabis use disorders (CUDs) were the commonest SUDs with 44 (20.5%) harmful users and 119 (55.3%) dependent users. This was followed by alcohol with 101 (47.0%) harmful users and 50 (23.3%) with alcohol dependence and nicotine with 72 (33.5%) harmful users and 23 (10.7%) dependent users. The majority of cases reviewed (n = 149, 69.3%) were poly-drug users. Patterns of other SUDs were highlighted in table 1.
Table 1.
Pattern of substance use
| Substances | n (%) |
|---|---|
| Alcohol | |
| Harmful use | 101 (47.0) |
| Dependence | 50 (23.3) |
| Cigarette | |
| Harmful use | 72 (33.5) |
| Dependence | 23 (10.7) |
| Tramadol | |
| Harmful use | 21 (9.8) |
| Dependence | 15 (7.0) |
| Cannabis | |
| Harmful use | 44 (20.5) |
| Dependence | 119 (55.3) |
| Codeine | |
| Harmful use | 13 (6.0) |
| Rohypnol (flunitrazepam) | |
| None | 209 (97.2) |
| Harmful use | 6 (2.8) |
| Pentazocine | |
| Dependence | 5 (2.3) |
| Cocaine | |
| Dependence | 2 (0.9) |
| Extent of substance use | |
| Mono-drug use | 66 (30.7) |
| Poly-drug use | 149 (69.3) |
Relation between socio-demographic characteristics and comorbid mental illness: Table 2 shows the relationship between socio-demographics and the presence of comorbid mental illness. Male cases (P = 0.001) and those who were single, divorced, or separated (P = 0.001) were significantly more likely to have a comorbid mental illness. Age at presentation or onset, level of education, religion, and family type were not associated with comorbid mental illness (P > 0.050).
Table 2.
Socio-demographic characteristics and comorbid mental illness
| Variables | Presence of comorbidity [n (%)] | Absence of comorbidity [n (%)] | P |
|---|---|---|---|
| Age group at presentation (year) | 0.116 | ||
| 21 and below | 22 (59.5) | 15 (40.5) | |
| 22-30 | 88 (73.3) | 32 (26.7) | |
| 31 and above | 35 (60.3) | 23 (39.7) | |
| Age at onset (year) | 0.549 | ||
| ≤ 21 | 82 (69.5) | 36 (30.5) | |
| 22 and above | 63 (65.6) | 33 (34.5) | |
| Marital status at presentation | 0.011 | ||
| Single | 124 (71.7) | 49 (28.3) | |
| Married | 14 (43.8) | 18 (56.3) | |
| Separated/divorced | 7 (70.0) | 3 (30.0) | |
| Gender | 0.016 | ||
| Women | 2 (25.0) | 6 (75.0) | |
| Men | 143 (69.1) | 64 (30.9) | |
| Level of education | 0.091 | ||
| Secondary and below | 68 (75.6) | 22 (24.4) | |
| Tertiary | 73 (61.3) | 46 (38.7) | |
| Religion | 0.210 | ||
| Christianity | 129 (65.8) | 67 (34.2) | |
| Islam | 15 (88.3) | 3 (16.7) | |
| Family type | 0.432 | ||
| Monogamous | 100 (66.2) | 51 (33.8) | |
| Polygamous | 27 (73.0) | 10 (27.0) | |
| Parental status | 0.066 | ||
| Both parents alive | 89 (63.6) | 51 (36.4) | |
| Both parents late/one late | 49 (76.6) | 15 (23.4) |
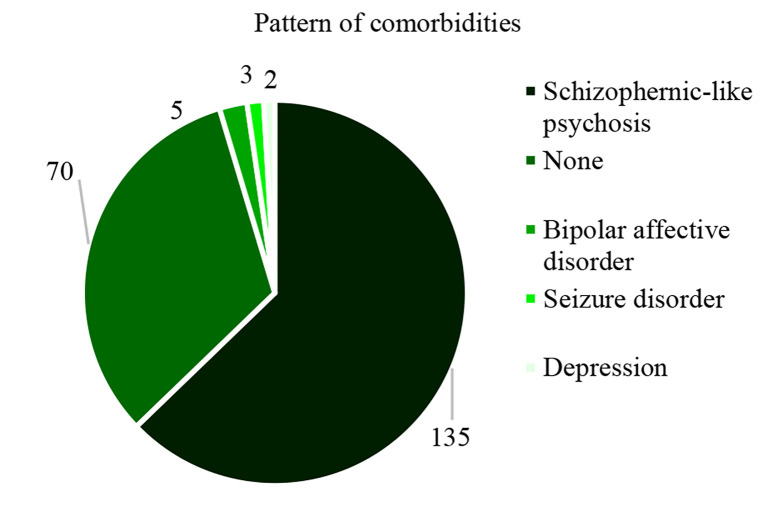
Pattern of comorbidities: Majority of the patients (n = 145, 67.4%) reviewed had other mental illnesses besides SUDs. Of which, the majority had schizophrenia/schizophrenic-like psychosis. This was followed by bipolar affective disorders. Others are as shown in figure 1.
Figure 1.
Pattern of psychiatric comorbidities
Relationship between substance use variables and the presence of co-occurring mental illness: The relationship between substance use variables and the presence of psychiatric comorbidity is as shown in table 3.
Table 3.
Relationship between substance use variables, presence of co-occurring mental illness, and multiple substance use
| Variables | Presence of comorbidity | Absence of comorbidity | Statistics | Mono-drug use | Poly-drug use | Statistics |
|---|---|---|---|---|---|---|
| Cannabis | P = 0.001 | P = 0.001 | ||||
| None | 23 (43.4) | 30 (56.6) | OR (CI): 0.25 | 28 (52.8) | 25 (47.2) | OR (CI): 3.67 |
| Dependence/harmful use | 122 (75.3) | 40 (24.7) | (0.13-0.42) | 38 (23.5) | 124 (76.5) | (0.91-7.00) |
| Alcohol | P = 0.629 | P = 0.001 | ||||
| None | 44 (69.8) | 19 (30.2) | OR (CI): 1.17 | 44 (69.5) | 19 (30.2) | OR (CI): 13.68 |
| Dependence/harmful use | 101 (66.4) | 51 (33.6) | (0.62-2.21) | 22 (14.5) | 130 (85.5) | (6.75-27.63) |
| Cigarette | P = 0.390 | P = 0.001 | ||||
| None | 78 (65.5) | 42 (35.0) | OR (CI): 0.77 | 62 (51.7) | 58 (48.3) | OR (CI): 4.32 |
| Dependence/harmful use | 67 (70.5) | 28 (29.5) | (0.44-1.39) | 4 (4.2) | 91 (95.8) | (8.39-70.40) |
| Tramadol | P = 0.040 | P = 0.045 | ||||
| None | 126 (70.4) | 53 (29.6) | OR (CI): 2.13 | 60 (33.5) | 119 (66.5) | OR (CI): 2.01 |
| Dependence/harmful use | 19 (52.8) | 17 (47.2) | (1.03-4.41) | 6 (16.7) | 30 (83.3) | (0.94-4.30) |
| Codeine | P = 0.634 | |||||
| None | 137 (67.8) | 65 (32.2) | OR (CI): 1.32 | 66 (37.7) | 136 (67.3) | P = 0.011 |
| Dependence/harmful use | 8 (61.5) | 5 (38.5) | (0.42-4.18) | 0 (0) | 13 (100) | |
| Rohypnol | P = 0.394 | |||||
| None | 142 (67.9) | 67 (32.1) | OR (CI): 2.12 | 66 (31.6) | 143 (68.4) | P = 0.181 |
| Dependence/harmful use | 3 (50.0) | 3 (50.0) | (0.42-10.78) | 0 (0) | 6 (100) | |
| Pentazocine | P = 0.032 | |||||
| None | 145 (69.0) | 65 (31.0) | P = 0.003 | 62 (29.5) | 148 (70.5) | OR (CI): 0.11 |
| Dependence | 0 (0) | 5 (100) | 4 (80.0) | 1 (20.0) | (0.10-0.96) | |
| Benzodiazepine | ||||||
| None | 145 (67.8) | 69 (32.2) | P = 0.326 | 66 (30.8) | 148 (69.2) | P > 0.999 |
| Dependence | 0 (0) | 1 (100) | 0 (0) | 1 (100) | ||
| Cocaine | ||||||
| None | 145 (68.1) | 68 (31.9) | P = 0.105 | 66 (31.0) | 147 (69.0) | P > 0.999 |
| Dependence | 0 (0) | 2 (100) | 0 (0) | 2 (100) |
Data are presented n (%)
OR: Odds ratio; CI: Confidence interval
Patients who were non-users of cannabis were less likely to have co-occurring mental illness compared with those who had CUDs (harmful users or dependent on cannabis) [OR = 0.25, 95% confidence interval (CI) = 0.13-0.42, P = 0.001].
Likewise, harmful/dependent users of tramadol (OR = 2.13, 95% CI = 1.03-4.41, P = 0.040) and non-users of pentazocine (P = 0.003) were more likely to have co-occurring mental illness compared with their counterparts.
Relationship between substance use variables and multiple substance use: Patients with AUDs (OR = 24.32, 95% CI = 8.39-70.40, P= 0.001), CUDs (OR = 3.67, 95% CI = 0.09-7.00, P = 0.001), nicotine use disorders (NUDs) (OR = 24.32, 95% CI = 8.39-70.40, P = 0.001), tramadol use disorders (OR = 2.01, 95% CI = 0.94-4.30, P = 0.045), and codeine use disorders (P = 0.011) were significantly more likely to be multiple substance users. Patients with pentazocine use disorder, on the other hand, were more likely to be a mono-drug user (OR = 0.11, 95% CI = 0.10-0.96, P = 0.032). Relationship between other substance use variables and history of multiple substance use is as shown in table 3.
Discussion
About 10 percent of patients managed in this psychiatric unit during the period under review presented primarily with SUDs. They were predominantly young adults at the time of presentation, with nearly three-quarters presenting before the age of 30. Besides, over half of this population had onset of substance use before the age of 21, suggesting the onset of use during a critical stage of development, when the brain has not assumed full maturation. Studies have identified substance use as a problem of young adults with the onset of use more often in adolescence.4,12-14 Individuals with early age of onset of substance use had been reported to have a higher risk of psychosocial issues, psychiatric disorders, peer relationship, work adjustment, and risky sexual behaviour.14-16 Early onset of substance use is associated with continued drug use, poly-drug use, and SUDs later in adulthood; this is in addition to other adverse psychosocial outcomes,14,16-18 including increased risk of incarceration for substance-related offenses.18,19
In contrast to what usually is obtained from epidemiological studies or the general population where alcohol was the commonest substance usually reported, cannabis use was the commonest SUD with over three-quarters of cases reviewed presenting with CUDs.
This might not be unconnected with the fact that early initiation and continuous use of cannabis in adolescents increase psychosocial impairment and problematic cannabis use, and also increase vulnerability to developing psychotic disorders.20-24
Early initiation of cannabis use has been reported as a risk factor for developing psychosis.24,25 This may explain the relatively high proportions of patients who had CUDs compared with AUDs or other SUDs presenting for care in the hospital. The psychosocial sequelae or the psychotic symptoms may have necessitated more people with CUDs to present in the hospital relative to other substance users. Besides, it also increases the use of other substances26 and this might explain the significant association between cannabis use and poly-drug use, thus increasing the likelihood of psychosocial consequences.
Unlike patients with pentazocine use disorder, patients with CUD, NUD, and AUD were more likely to use one or more additional substances. Oftentimes, pentazocine is usually initiated by healthcare practitioners, either in managing their patients or in managing themselves.27-29 Alcohol, on the other hand, is usually referred to as the gateway drug, with which most drugs of abuse are usually experimented;4,30,31 however, the probability of cannabis serving as the gateway to other licit and illicit drugs has been proposed.26 Most persons who abuse nicotine or cannabis are more likely to abuse alcohol too. This might explain the strong association between alcohol, cannabis, nicotine, and poly-drug use. History of poly-drug use, on the other hand, has been reported to be associated with increased substance use-associated deaths.32 Pentazocine, on the other hand, is a substance of circumstances, usually initiated or abused by health workers; hence, most patients abusing pentazocine are mono-drug users relative to other substance users. Although pentazocine was not significantly associated with other psychiatric disorders in this study, study has shown association between other opiate use disorders and psychiatric disorders.10
This study revealed that about two-thirds of those with SUDs had other psychiatric comorbidity. This corroborates earlier studies.23-25,33-35 There are several possible reasons for this observation. First, common predispositions such as genetic and environmental factors can contribute to the development of both SUDs and other mental ill-health.36,37 Moreover, other mental disorders can result from substance use and SUDs following alteration in brain structure and function by these agents;10,38,39 and people living with mental illness may use these substances as a form of self-medication.40-42
Conclusion
There is a high rate of co-occurrence of other psychiatric disorders among patients presenting SUDs in a clinical setting. Most of these patients, usually single young adult men, presented with poly-drug use that may compound the treatment of either the SUDs or the associated psychiatric morbidities. CUDs were the commonest SUD seen among this population. This might not be unconnected with a higher incidence of psychotic symptoms and psychosocial problems associated with cannabis use and CUDs, thus necessitating urgent care. Similar to patients with AUDs, those with CUDs were also more likely to be poly-drug users, thus complicating the management of cases. Evaluation and management of patients presenting with SUDs need to incorporate prevention, assessment, and treatment of other mental disorders.
Limitations: Like other retrospective studies, the study possesses some limitations. The information available for analysis was limited to those available in the case files, thus limiting the ability to explore other confounding factors that may be associated with co-occurrence of other mental disorders. Some data of interest were not readily available in the case files, thus limiting the data available for analyses. It is also difficult to establish a cause-effect relationship using retrospective study; however, this study provided insightful data in guiding the development of future prospective or case-control studies.
Acknowledgments
The authors will want to thank the leadership of Department of Psychiatry, Ekiti State University Teaching Hospital for the opportunity to assess patients’ records.
Conflicts of Interest
The Authors have no conflict of interest.
Authors’ Contribution
Involved in conceptualization/design of the work, data analyses and interpretation, writing original draft, and supervision of the work: AO; involved in data curation, critical revision, and editing of the original draft: LOO; involved in data extraction and entry, data analyses, and visualization: BFK; involved in reviewing and editing of the manuscript: MUD.
REFERENCES
- 1.GBD 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012. doi: 10.1016/S2215-0366(18)30337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–86. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 3.Tran BX, Moir M, Latkin CA, Hall BJ, Nguyen CT, Ha GH, et al. Global research mapping of substance use disorder and treatment 1971-2017: Implications for priority setting. Subst Abuse Treat Prev Policy. 2019;14(1):21. doi: 10.1186/s13011-019-0204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Obadeji A, Kumolalo BF, Oluwole LO, Ajiboye AS, Dada MU, Ebeyi RC. Substance use among adolescent high school students in nigeria and its relationship with psychosocial factors. J Res Health Sci. 2020;20(2):e00480. doi: 10.34172/jrhs.2020.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adamson TA, Ogunlesi AO, Morakinyo O, Akinhanmi AO, Onifade PO, Erinosho O, et al. Descriptive National Survey of Substance Use in Nigeria. J Addict Res Ther. 2015;6:234. [Google Scholar]
- 6.Majekodunmi OE, Obadeji A, Oluwole LO, Oluwaranti AO. Patterns and predictors of alcohol and substance use disorders among prison's inmates in Nigeria. Ann Psychiatry Ment Health. 2018;6(2):1128. [Google Scholar]
- 7.Obadeji A, Kumolalo BF, Ajiboye AS, Oluwole LO, Oderinde KO, Ebeyi RC. Substance use among commercial motorcyclists and its relationship with life satisfaction and significant depressive symptoms. J Subst Use. 2021;26(2):177–83. [Google Scholar]
- 8.Okpataku CI, Kwanashie HO, Ejiofor JI, Olisah VO. Prevalence and socio-demographic risk factors associated with psychoactive substance use in psychiatric out-patients of a tertiary hospital in Nigeria. Niger Med J. 2014;55(6):460–4. doi: 10.4103/0300-1652.144695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abayomi o, Ojo T, Ibrahim N, Adelufosi A, Obasan A. Prevalence and correlates of substance use among persons with mental disorders in a Nigerian Psychiatric Hospital. Afr J Drug Alcohol Stud. 2012;11:29–35. [Google Scholar]
- 10.Parvaresh N, Masoudi A, Majidi-Tabrizi S, Mazhari S. The correlation between methadone dosage and comorbid psychiatric disorders in patients on methadone maintenance treatment. Addict Health. 2012;4(1-2):1–8. [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute on Drug Abuse. Comorbidity: Substance Use Disorders and Other Mental Illnesses DrugFacts [Online]. 2018. Available from: URL: https://www.drugabuse.gov/publications/drugfacts/comorbidity-substance-use-disorders-other-mental-illnesses.
- 12.Gil AG, Wagner EF, Tubman JG. Associations between early-adolescent substance use and subsequent young-adult substance use disorders and psychiatric disorders among a multiethnic male sample in South Florida. Am J Public Health. 2004;94(9):1603–9. doi: 10.2105/ajph.94.9.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kushwaha R, Rauniar GP, Koirala B, Mandal NK. Prevalence of substance use among undergraduate students in a medical college of Nepal. JNMA J Nepal Med Assoc. 2019;57(219):315–9. doi: 10.31729/jnma.4605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poudel A, Gautam S. Age of onset of substance use and psychosocial problems among individuals with substance use disorders. BMC Psychiatry. 2017;17(1):10. doi: 10.1186/s12888-016-1191-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Subodh BN, Sahoo S, Basu D, Mattoo SK. Age of onset of substance use in patients with dual diagnosis and its association with clinical characteristics, risk behaviors, course, and outcome: A retrospective study. Indian J Psychiatry. 2019;61(4):359–68. doi: 10.4103/psychiatry.IndianJPsychiatry_454_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly A, Weier M, Hall W. The age of onset of substance use disorders. In: McGorry PD, Sartorius N, de Girolamo G, editors. Age of onset of mental disorders: etiopathogenetic and treatment implications. New York, NY: Springer; 2019. pp. 149–67. [Google Scholar]
- 17.Behrendt S, Wittchen HU, Hofler M, Lieb R, Beesdo K. Transitions from first substance use to substance use disorders in adolescence: Is early onset associated with a rapid escalation? Drug Alcohol Depend. 2009;99(1-3):68–78. doi: 10.1016/j.drugalcdep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Slade EP, Stuart EA, Salkever DS, Karakus M, Green KM, Ialongo N. Impacts of age of onset of substance use disorders on risk of adult incarceration among disadvantaged urban youth: a propensity score matching approach. Drug Alcohol Depend. 2008;95(1-2):1–13. doi: 10.1016/j.drugalcdep.2007.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fergusson DM, Swain-Campbell NR, Horwood LJ. Arrests and convictions for cannabis related offences in a New Zealand birth cohort. Drug Alcohol Depend. 2003;70(1):53–63. doi: 10.1016/s0376-8716(02)00336-8. [DOI] [PubMed] [Google Scholar]
- 20.Akpa OM, Okekunle AP. Substance use and psychosocial functioning of adolescents in Benue State, Nigeria: Assessing the role of age. Afr J Psychol Study Soc Issues. 2019;22(2):36–50. [PMC free article] [PubMed] [Google Scholar]
- 21.Copeland J, Rooke S, Swift W. Changes in cannabis use among young people: Impact on mental health. Curr Opin Psychiatry. 2013;26(4):325–9. doi: 10.1097/YCO.0b013e328361eae5. [DOI] [PubMed] [Google Scholar]
- 22.Hall W, Leung J, Lynskey M. The effects of cannabis use on the development of adolescents and young adults. Annu Rev Dev Psychol. 2020;2(1):461–83. [Google Scholar]
- 23.Lev-Ran S, Le Foll, McKenzie K, George TP, Rehm J. Cannabis use and cannabis use disorders among individuals with mental illness. Compr Psychiatry. 2013;54(6):589–98. doi: 10.1016/j.comppsych.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 24.Lowe DJE, Sasiadek JD, Coles AS, George TP. Cannabis and mental illness: A review. Eur Arch Psychiatry Clin Neurosci. 2019;269(1):107–20. doi: 10.1007/s00406-018-0970-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paruk S, Burns JK. Cannabis and mental illness in adolescents: A review. S Afr Fam Pract. 2016;58(Suppl 1):S18–S21. [Google Scholar]
- 26.Secades-Villa R, Garcia-Rodriguez O, Jin CJ, Wang S, Blanco C. Probability and predictors of the cannabis gateway effect: A national study. Int J Drug Policy. 2015;26(2):135–42. doi: 10.1016/j.drugpo.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adewoyin A, Adeyemi O, Davies N, Ojo M. Clinical and socio-demographic determinants of pentazocine misuse among patients with sickle cell disease, Benin City, Nigeria: A case-control study. Pan Afr Med J. 2019;34:88. doi: 10.11604/pamj.2019.34.88.17257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ibrahim A, Abubakar M, Yunus A, Dahiru I, Amaefulae K, Asuku M. Limb ulcerations in patients who abuse pentazocine: A demographic and clinical study of an under-recognized etiology of hard-to-heal ulcers in Zaria, Northwest Nigeria. Arch Int Surg. 2018;8(4):153. [Google Scholar]
- 29.Nwagha T, Babatunde O. Analgesia self-medication practice and pentazocine dependency in adult sickle cell patients in Southeast Nigeria. Niger J Med. 2020;29(2):197–202. [Google Scholar]
- 30.Kirby T, Barry AE. Alcohol as a gateway drug: A study of US 12th graders. J Sch Health. 2012;82(8):371–9. doi: 10.1111/j.1746-1561.2012.00712.x. [DOI] [PubMed] [Google Scholar]
- 31.Welte JW, Barnes GM. Alcohol: The gateway to other drug use among secondary-school students. J Youth Adolesc. 1985;14(6):487–98. doi: 10.1007/BF02139522. [DOI] [PubMed] [Google Scholar]
- 32.Akhgari M, Sardari-Iravani F, Ghadipasha M. Trends in poly drug use-associated deaths based on confirmed analytical toxicology results in Tehran, Iran, in 2011-2016. Addict Health. 2021;13(1):18–28. doi: 10.22122/ahj.v13i1.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(2):247–57. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- 34.Pettinati HM, O'Brien CP, Dundon WD. Current status of co-occurring mood and substance use disorders: a new therapeutic target. Am J Psychiatry. 2013;170(1):23–30. doi: 10.1176/appi.ajp.2012.12010112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gordon A, Holmwood C. Comorbidity of mental disorders and substance use: A brief guide for the primary care clinician. Canberra, Australia: Department of Health and Ageing; 2009. [Google Scholar]
- 36.Brook JS, Richter L, Rubenstone E. Consequences of adolescent drug use on psychiatric disorders in early adulthood. Ann Med. 2000;32(6):401–7. doi: 10.3109/07853890008995947. [DOI] [PubMed] [Google Scholar]
- 37.Kendler KS, Karkowski LM, Neale MC, Prescott CA. Illicit psychoactive substance use, heavy use, abuse, and dependence in a US population-based sample of male twins. Arch Gen Psychiatry. 2000;57(3):261–9. doi: 10.1001/archpsyc.57.3.261. [DOI] [PubMed] [Google Scholar]
- 38.Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR, et al. Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105(6):1117–28. doi: 10.1111/j.1360-0443.2010.02902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rappeneau V, Berod A. Reconsidering depression as a risk factor for substance use disorder: Insights from rodent models. Neurosci Biobehav Rev. 2017;77:303–16. doi: 10.1016/j.neubiorev.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 40.Goswami S, Mattoo SK, Basu D, Singh G. Substance-abusing schizophrenics: Do they self-medicate? Am J Addict. 2004;13(2):139–50. doi: 10.1080/10550490490435795. [DOI] [PubMed] [Google Scholar]
- 41.Harris KM, Edlund MJ. Self-medication of mental health problems: New evidence from a national survey. Health Serv Res. 2005;40(1):117–34. doi: 10.1111/j.1475-6773.2005.00345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Robinson J, Sareen J, Cox BJ, Bolton JM. Role of self-medication in the development of comorbid anxiety and substance use disorders: A longitudinal investigation. Arch Gen Psychiatry. 2011;68(8):800–7. doi: 10.1001/archgenpsychiatry.2011.75. [DOI] [PubMed] [Google Scholar]