Abstract
Objective:
This systematic review and meta-analysis assess the effectiveness of acupuncture as an adjunct to standard therapy in the management of nonspecific chronic low back pain (NScLBP), compared with standard therapy alone.
Methods:
A systematic literature search of full-text articles of randomized controlled trials in the date range of 2000–2020, utilizing PubMed and EBSCO databases, was performed to evaluate the efficacy of acupuncture treatment for nonspecific chronic lower back pain. The outcomes of interest were pain intensity and disability. The methodological quality of each study was evaluated using Cochrane risk-of-bias criteria. The studies were combined using meta-analysis when statistical pooling of data was possible.
Results:
This systematic review included 5 studies of which 4 were included in the meta-analysis. Acupuncture as an adjunct to standard therapy had clinically meaningful reduction in self-reported pain at post-treatment (mean difference = −1.04 [95% confidence interval (CI), −1.59 to −0.49], P < 0.001, I2 = 46.1%) and at intermediate term (mean difference = −0.82 [95% CI, −1.13 to −0.50], P < 0.001, I2 = 0%), compared with standard care. Levels of disability showed similar clinically meaningful reduction at post-treatment and intermediate term.
Conclusion:
Both the systematic review and meta-analysis demonstrate that acupuncture as an adjunct to standard therapy is a safe and effective method in reducing pain and disability among adults with NScLBP.
Keywords: acupuncture, electroacupuncture, nonspecific low back pain, chronic low back pain
INTRODUCTION
Low back pain (LBP) is one of the leading causes of disability among adults in the United States and has become a costly condition.1 Approximately 70%–80% of the population will experience at least 1 episode of LBP at some point in their lives, making it a common reason for lost workdays, reduced productivity in the workforce, and is associated with escalating medical expenses.2–6 Recent data show that musculoskeletal disorders had the highest health care costs in the United States with an estimated $380.9 billion of which $134.5 billion went toward the treatment of low back and neck pain.7 The total cost for LBP, including direct health care and indirect socioeconomic costs, is estimated to be $100 to $200 billion annually.8
LBP is defined as pain, muscle tension, or stiffness localized below the costal margin and above the inferior gluteal folds, with or without sciatica.9 It is usually classified into specific or nonspecific LBP (NSLBP). Approximately 10% of individuals with LBP are diagnosed with specific underlying pathology with the remaining 90% being classified as having NSLBP.5,10–12 NSLBP is of unknown cause and is not attributed to a recognizable pathology (e.g., infection, tumor, osteoporosis, fracture, structural deformity, inflammatory disorder, radicular syndrome, or cauda equina syndrome).13 Essentially, it is a diagnosis based on the exclusion of specific pathologies.11
The diagnostic process is mainly focused on triage and distinguishing those patients with nonspinal or serious spinal disorders from those with musculoskeletal pain disorder while ruling out potential red flags through medical history and physical examination.11–14 A systematic review was conducted by Dagenais et al. in 2010 evaluating clinical practice guidelines (CPG) for the assessment and management of LBP.15
When assessing a patient with LBP, Dagenais et al. found that all of the CPG had 1 main goal in common: to sequentially rule out potential serious spinal pathology, specific causes of LBP, and substantial neurologic involvement (loss of sensation, motor weakness, or loss of reflexes).15 Once serious disease and radicular syndrome has been ruled out, all other cases are classified as NSLBP.12–14
In clinical practice and published works, NSLBP is typically classified by the duration of the symptom.3,13 It is defined as being acute when symptoms persist for less than 6 weeks, subacute between 6 and 12 weeks (3 months), and chronic when symptoms persist for more than 3 months.11,13,16
The prognosis of NSLBP is dependent on the duration of symptoms. In general, most patients with acute LBP have a favorable prognosis with 60%–70% of the patients recovering within 6 weeks and 80%–90% by 12 weeks.4,12 In some literature, it has been found that only 5%–15% of acute LBP cases develop into a chronic condition with persistent symptoms.11,13 However, this optimistic depiction may not be accurate as it fails to include those who experience incomplete recovery and recurrent pain due to inadequate duration of follow-up.
An inception cohort study in Australia found that only 72% of those with acute LBP cases completely recovered within 12 months and only 41% of those patients whose pain still persisted at 3 months recovered within 12 months.17,18 Overall, those who develop chronicity with persistent LBP represent the greatest challenge because they have a poor prognosis with full recovery being slow and unlikely.4
By definition, NSLBP does not have a pathologic cause. Owing to the nature of this condition, there is no specific treatment for NSLBP. Currently, the goal is to manage NSLBP by focusing on reducing pain and disability. Most CPG recommend the use of brief education, advice to stay active, nonsteroidal anti-inflammatory drugs (NSAIDs), weak opioid analgesics, exercise therapy, and spinal manipulation therapy for the management of nonspecific chronic low back pain (NScLBP).17 In 2017, the American College of Physicians (ACP) developed a CPG of noninvasive treatments for acute, subacute, and chronic LBP.
For these chronic cases, the ACP recommends that the first line of treatment be of a nonpharmacologic modality. Exercises with multidisciplinary rehabilitation alongside complementary medicine such as acupuncture should be utilized before the prescription of a pharmacologic treatment with NSAIDs.19,20 Therefore, evaluating data on acupuncture to complement a modality such as physical therapy (PT), which rehabilitates patients through education, exercise, and manual therapy to manage NScLBP, is of interest to the health care community.
It is essential to note that selecting the appropriate outcome measures for clinical and research purposes is critical, when evaluating pain intensity and disability of the low back. A systematic review conducted by Chapman et al. evaluated common chronic LBP outcome measures based on validity, reliability, and responsiveness to change.21 For pain intensity, the visual analog scale (VAS) and numerical rating scale (NRS) were recommended for their ease of administration and responsiveness.21 For functional disability, Oswestry Disability Index and Roland–Morris Disability Questionnaire (RMDQ) were recommended for their validity, reliability, and responsiveness.21
Several systematic reviews and/or meta-analyses have focused on evaluating the efficacy of acupuncture for the treatment of NSLBP.
Li et al. evaluated the efficacy of acupuncture for NSLBP for any duration, Xiang et al. evaluated the efficacy of manual acupuncture (MA) and electroacupuncture (EA) relative to sham or placebo acupuncture for subacute and chronic NSLBP, Nascimento et al. evaluated the efficacy of acupuncture for NSLBP in older adults (over 60 years), Yeganeh et al. evaluated the efficacy of acupuncture, acupressure, and chiropractic for NScLBP in Iran, Lam et al. evaluated the efficacy of MA and EA for NScLBP but defined chronic as being 6 weeks or longer, Hutchinson et al. evaluated the efficacy of MA for NScLBP, Rubinstein evaluated the efficacy of spinal manipulative therapy, acupuncture, and herbal medicine for NSLBP, and Yuan et al. evaluated the efficacy of MA and EA for NSLBP of any duration.22–29
This will be the first systematic review with meta-analysis to evaluate the efficacy of acupuncture (MA and EA) relative to standard therapy, including PT, exercise, and usual care for the management of NScLBP, as defined by a symptom duration of more than 12 weeks in an adult population. The primary aim of this review is to evaluate the current evidence, within the past 20 years, for the efficacy of acupuncture (MA and EA) as an adjunct to standard therapy (PT, exercise, and usual care) in the management of NScLBP, compared with standard therapy alone.
For persons receiving standard therapy, is the addition of acupuncture more effective in reducing pain intensity and disability than standard therapy alone? The hypothesis of this research is that it will provide evidence that the addition of acupuncture to standard therapy is more effective in reducing pain and disability in patients with NScLBP than standard therapy alone.
METHODS
Study Identification
A systematic literature review was performed to explore the efficacy of acupuncture on the treatment of NScLBP. A PubMed and EBSCO (limited to MedLine and Rehabilitation & Sports Medicine Source) database search was conducted from March 15, 2020 using the keywords: EA or acupuncture and low back, LBP, nonspecific LBP, nonspecific LBP, chronic LBP, or NScLBP. Only full-text publications of randomized controlled trials (RCTs) published in English between January 1, 2000 and December 31, 2020 were eligible. Systematic reviews and/or meta-analyses related to NScLBP were reviewed for possible additional studies.
Study Selection
RCTs that involved human subjects (18 and older) with NScLBP for more than 12 weeks (3 months) were considered. Animal studies, pilot studies, preliminary studies, observational studies, case studies, and protocols for a study were excluded. The treatments used were MA, which is the insertion of needles into acupuncture points with manual stimulation, or EA, which stimulates the needles in the acupuncture points using an electrical stimulation device. RCTs that tested the efficacy of acupuncture (MA and/or EA) as an adjunct to standard therapy (PT, exercise, or usual care) were included. The studies needed to include at least one of the following outcomes of measure: either VAS or NRS for pain intensity or RMDQ for disability.
Trials that involved subjects with LBP caused by specific pathologic entities such as infections, tumors, systemic disease, known or suspected spinal pathology, radicular syndrome, cauda equina syndrome, previous surgery on the spinal column, and pregnancy were excluded. Studies that were evaluated included individualized acupuncture protocols, sham acupuncture, auricular points, extra points, and Ah Shi “ouch” points; as long as the studies included a standardized acupuncture protocol that provided MA/EA on classical meridian points on the body.
RCTs that examined the following Traditional Chinese Medicine interventions such as warming technique, fire needles, bleeding, moxibustion, cupping, guasha, and herbal medicine were excluded. For the standard therapy group, PT, back exercises, and usual care were the main intervention of interest that was evaluated. Usual care could include the use of medication (limited to NSAIDs, non-narcotic pain medication), primary care visits, and massage. Prohibited interventions include other forms of medication such as narcotics and muscle relaxants, transcutaneous electrical nerve stimulation, epidural injections, and trigger point injections.
Methodological Quality Assessment
The methodological quality assessment of the selected articles was performed using the Cochrane risk-of-bias guidelines.30 A study was considered to have a low risk of bias if all the criteria were met, unclear risk of bias when one or more of the criteria were partially met, and high risk of bias when one or more of the criteria were not met.
Data Synthesis and Statistical Analysis
All quantitative synthesis and statistical analyses were conducted using OpenMetaAnalyst software, for Sierra (10.12).31 Analysis of acupuncture in addition to standard therapy versus standard therapy for pain intensity and disability was conducted according to follow-up time frames defined as post-treatment (≤1 week), short-term (1–12 weeks), intermediate term (12–52 weeks), and long term (≥1 year). If a trial conducted more than 1 follow-up within the same time frame, the median for the weeks that the other studies performed their outcome assessment during that time frame was calculated. Then it was compared with the follow-up times from the same study and whichever assessment was closer to the median was included in the meta-analysis.
It should be noted that sham acupuncture (SA), defined by shallow needling at nonacupuncture points with minimal or no stimulation, was considered a valid form of acupuncture in this study for the following reasons. First, acupuncture is a procedure that involves needling not only at acupuncture points with a known or precise location but as well as at anatomical landmarks and Ah Shi “ouch” points that can be located anywhere on the body.32 Following this concept, any needle that penetrates the body constitutes as acupuncture. Second, there is quantifiable evidence of a biomechanical response to needling, known as the “needle grasp” at both acupuncture and nonacupuncture points.33
Langevin et al. found that this needle-tissue coupling allows a “spreading of matrix deformation and cell activation along connective tissue planes thus may mediate acupuncture effects remote from the acupuncture needle site.”34 Third, several studies have demonstrated that penetrating SA elicits a psychophysiologic response from the body.35 For example, SA relieved pain in patients with fibromyalgia,36 reduced serum cortisol concentration and anxiety,37 reduced migraine headaches,38 and relieved chronic LBP.39 For these reasons, penetrating SA is not an effective placebo-control for acupuncture trials.
It is critical to utilize a form of SA for which a patient is unable to distinguish between it and genuine acupuncture. Several nonpenetrating SA devices such as the “Streitberger” needle and “Park sham device” have been validated to be indistinguishable from real acupuncture in acupuncture-naive patients as well as in a Chinese population with acupuncture experience.40,41 Although nonpenetrating SA devices were found to evoke a brain response through tactile stimulation,42 there was a clear distinction between acupuncture and tactile stimulation in functional magnetic resonance imaging studies.43
For the purpose of this review, SA performed without devices such as the “Streitberger” needle or “Park sham device” that insert acupuncture needles into the body at nonacupuncture points was considered as verum acupuncture for this systematic review. If RCTs included different needling techniques, acupuncture point protocols, or penetrating SA, the results of the studies were pooled together as verum acupuncture and evaluated against standard therapy in the meta-analysis.
All outcomes in this study were continuous data. Means and standard deviation were used to calculate a mean difference (MD) or standardized mean difference (SMD) with a 95% confidence interval (CI) in the meta-analysis. MD was used if the analysis included outcomes measured using the same scales, SMD for different scales. However, if the analysis included a combination of results reported with postintervention values and change (from baseline) scores, SMD could not be used and MD was chosen instead.30
SMD was used to indicate the statistical power of effect size to determine magnitude of improvement: small for less than 0.3, medium between 0.3 and 0.8, and large for greater than 0.8.44 A negative effect size indicated that the intervention group (acupuncture as an adjunct to standard therapy) was more beneficial than the comparison group (standard therapy) in the reduction of pain or disability.
Heterogeneity was tested using the I2 statistic with values >50% indicating strong heterogeneity.23 If P > 0.1 and I2 < 50%, which means heterogeneity was not statistically significant, fixed-effect inverse variance model was used in the meta-analysis; if P < 0.1 and I2 > 50%, which means heterogeneity was statistically significant, per DerSimonian–Laird random-effects model was used.
RESULTS
Study Selection
The initial search using the keywords resulted in 5,098 publications. No additional RCTs were found after examining all systematic reviews or meta-analyses related to NScLBP. Four thousand two hundred sixty-three records were excluded after limiting publications within the set time frame between 2000 and 2020 (n = 534), full-text availability (n = 1,839), clinical trials (n = 1,858), and published in English (n = 32). Eight hundred thirty-five titles were screened and 815 records were excluded after title screening (n = 189) and duplicate removal (n = 626).
Twenty abstracts were reviewed and 11 records were excluded after the abstract screening: specific LBP (n = 2), inappropriate acupuncture (n = 3), and inappropriate comparison group (n = 6). Nine full-text articles were assessed for eligibility and 4 articles were excluded due to inappropriate outcome measures (n = 3) and inappropriate definition of chronic (n = 1). A total of 5 studies were included in the systematic literature review45–49 and 4 studies were included in the meta-analysis.45,47–49 Figure 1 provides the PRISMA diagram.
FIG. 1.
Flow diagram of study selection.
Study Characteristics
A total of 1,063 participants between the age of 18 and 80 years were enrolled in the 5 studies. The sample sizes ranged from 52 to 638, where two of the studies46,49 included between 50 and 100 subjects and three of the studies45,47,48 included more than 100 subjects. One study took place in research clinics,47 another study took place in hospitals,49 and 3 studies did not report clinical settings.45,46,48
Two studies involved MA using classical meridian points,47,48 1 study involved MA using classical meridian points and auricular points,45 and 2 studies involved EA on classical meridian points.46,49 The duration of intervention varied from 4 weeks46 to 12 weeks,45 and duration of treatment ranged from 20 minutes47–49 to 30 minutes.45,46 The total number of sessions ranged from 1047,49 to 20 sessions.45 All 5 studies compared acupuncture as an adjunct to standard therapy of which mostly included PT, exercise, and usual care.
Outcomes of measure included pain intensity and disability. Of the 5 studies that measured pain intensity, 1 study used the NRS46 and 3 studies used the VAS.45,48,49 One study was excluded in the evaluation of pain intensity because it used a bothersomeness scale for pain intensity.47 Of the 5 studies that measured disability, 3 studies used the RMDQ and were included in the evaluation.47–49 Two studies were excluded in the evaluation of disability because one used the pain disability index45 and another study used the Aberdeen LBP scale.46 All 5 studies were evaluated post-treatment,45–49 2 studies had short-term follow-ups,46,49 4 had intermediate-term follow-ups,45–48 and no long-term follow-ups were reported. Table 1 provides a descriptive summary of the studies included in this review.
Table 1.
Study Design and Outcome Measures
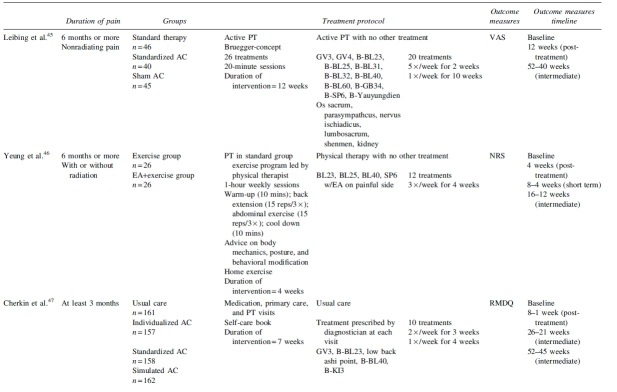
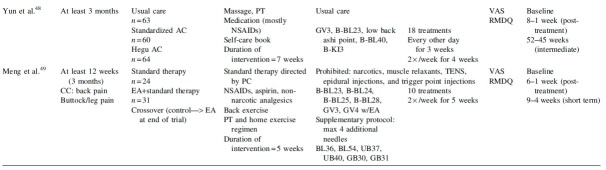
|
AC, acupuncture; B, bilateral; CC, chief complaint; EA, electroacupuncture; NRS, numerical rating scale; NSAIDs, nonsteroidal anti-inflammatory drugs; PC, primary care; PT, physical therapy; RMDQ, Roland–Morris Disability Questionnaire; TENS, transcutaneous electrical nerve stimulation; VAS, visual analog scale.
Methodological Quality Assessment
Methodological quality and risk of bias were evaluated for each included trial (Fig. 2). All studies specified the method of randomization and allocation concealment, and thus were assessed to have low risk of selection bias. However, blinding of participants and personnel was not always possible as they were directly involved in the treatment process. Therefore, in this review, a study was considered to have the lowest risk of performance and detection bias when the outcome assessors were blinded to group allocation.
FIG. 2.
Risk of bias summary.
All studies were assessed to have a low risk of performance bias but 1 study failed to mention blinding of outcome assessors and was assessed to have a high risk of detection bias.49 All studies fulfilled the heading of incomplete outcome data and other sources of bias. Two studies were assessed to have a high risk of reporting bias because 1 study failed to report all outcome measures with intention-to-treat analysis49 and another failed to report information on adverse effects.48 Overall, 3 studies were assessed to have a low risk of bias45–47 and 2 studies were assessed to have a high risk of bias.48,49
Meta-Analysis
Of the trials that measured pain intensity, 1 study used NRS46 and 3 studies used VAS.45,48,49 The outcome measures were reported as postintervention level for 2 studies45,47 and change score for 2 studies.45,49 Three studies that used the VAS were selected for meta-analysis; however, only the results of 2 studies45,48 could be pooled for the analysis because 1 study49 did not provide data using the intention-to-treat analysis. Those 2 studies were analyzed for post-treatment and intermediate term.45,48
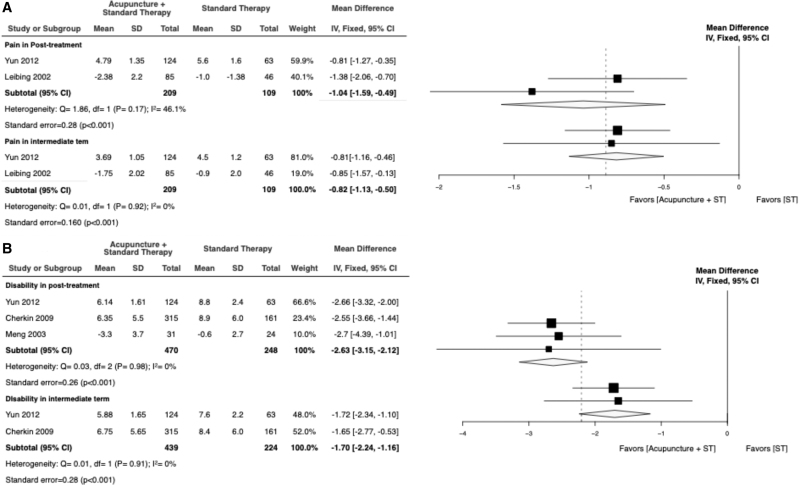
Evaluation of short-term data was not possible under the limitations set by the Cochrane guidelines and the 2 studies did not include long-term follow-ups. The analysis showed acupuncture as an adjunct to standard therapy was significantly more effective in reducing pain intensity, compared with standard therapy alone at the following time frames studied: MD of −1.04 (95% CI −1.59 to −0.49, P < 0.001; I2 = 46.1%) and MD of −0.82 (95% CI −1.13 to −0.50, P < 0.001; I2 = 0%) in post-treatment and intermediate term, respectively (Fig. 3A).
FIG. 3.
Forest plot for meta-analysis of acupuncture+ST versus ST for (A) pain and (B) disability. ST, standard therapy.
Of the trials that measured disability, 3 studies used RMDQ.47–49 The outcome measures were reported as postintervention level for 2 studies47,48 and change score for 1 study.49 Three studies could be pooled for disability analysis of which 3 were analyzed for post-treatment47–49 and only 2 for intermediate term47,48 Evaluation of short-term data was not possible under the limitations set by the Cochrane guidelines and the 2 studies did not include long-term follow-ups.
This analysis determined that acupuncture as an adjunct treatment to standard therapy is statistically more effective in reducing patient disability when compared with standard therapy alone at post-treatment MD of −2.63 (95% CI −3.15 to −2.12, P < 0.001; I2 = 0%) and intermediate term with MD of −1.70 (95% CI −2.24 to −1.16, P < 0.001; I2 = 0%) (Fig. 3B).
DISCUSSION
This systematic review and meta-analysis evaluated the effectiveness of acupuncture as an adjunct to standard therapy versus standard therapy for the management of NScLBP, when measured by relief of pain intensity and disability. The included studies were grouped by follow-up time frames: post-treatment and intermediate term.
Overall, the analysis suggests that (1) patients who received acupuncture in addition to standard therapy reported statistically lower levels of pain at post-treatment and intermediate term follow-ups when compared with their counterparts who received standard therapy alone, with low heterogeneity and (2) patients who received acupuncture as an adjunct to standard therapy showed significant improvement in levels of function at post-treatment and intermediate-term follow-ups than those who received standard therapy alone, with low heterogeneity.
Overall, the findings of this systematic review and meta-analysis were in agreement with 2 meta-analyses conducted on this population.22,26 This will be the first study that assesses the efficacy of acupuncture as an adjunct to standard therapy for pain and disability at post-treatment and intermediate term for the management of NScLBP; defined by a symptom duration of more than 12 weeks. This specific comparison group included PT, exercise, and usual care.
The analysis of acupuncture points in this review showed that BL-23 shenshu was the most commonly used acupuncture point in all 5 studies,45–49 followed by BL-40 weizhong in 4 studies,45–48 GV-3 yaoyangguan in 4 studies,45,47–49 and BL-25 dachangshu in 3 studies.45,46,49
All 5 RCTs were approved either by the ethics committee or IRB and all participants gave informed consent. However, none of the RCTs mentioned neither Consolidated Standards of Reporting Trials (CONSORT) nor Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA) guidelines.
All 5 studies reported medication use at baseline and 4 RCTs reported medication use postintervention.46–49 Yeung et al. reported that there were no significant differences in medication use between the exercise group and EA with exercise group at baseline, postintervention, 1-month follow-up, and at the 3-month follow-up.46 Meng et al. also found no significant difference in medication use between the standard therapy group and EA with standard therapy group at baseline and postintervention.49
However, 2 studies found statistically significant decrease in medication use in the intervention group, compared with the control group.47,48 Cherkin et al. found that self-reported medication use decreased significantly more in all 3 acupuncture groups (individualized, standardized, and simulated), compared with the usual care group.47 Yun et al. reported similar medication use across all groups at baseline but found significant decrease in medication use in the Hegu acupuncture and standardized acupuncture groups, compared with the usual care group at postintervention and at the 48-week follow-up.48
Adverse events were reported in only 4 RCTs in this study.45–47,49 Adverse reactions were mostly minor and unserious. However, 1 study reported 1 severe experience of pain lasting 1 month.47 Overall, acupuncture was deemed to be safe.
This study had several limitations. First, this review only included studies that were published in English. Second, several RCTs in this study had a small sample size. Third, while most studies were evaluated to have low risk of bias, some of the studies failed to completely blind participants and personnel because they were directly involved with the treatment, which may contribute to performance bias. Fourth, there was clinical heterogeneity in study characteristics such as types of acupuncture administered, duration of treatment, number of treatments, difference in needling manipulation, and fixed or flexible sets of acupuncture points.
CONCLUSION
According to the results of this systematic review and meta-analysis, it can be concluded that acupuncture is an effective and safe method for reducing pain and disability in patients with NScLBP. Statistically significant improvements were seen with respect to pain intensity and disability at post-treatment and intermediate term. The medical community at large can apply the findings of this study to include acupuncture as a supplement to standard therapy and create a multimodal program for patients in the management of NScLBP.
When considering future research, there should be a focus on improving methodological and reporting quality of trials, systematic reviews, and meta-analyses by following STRICTA guideline, CONSORT statement, and Cochrane guidelines for systematic reviews. In addition, publishing study protocols to create an appropriate study design that addresses and eliminates risk of bias would strengthen the quality of trials that examine the efficacy of acupuncture. Finally, future research should focus on examining the lasting effect of acupuncture by including long-term follow-ups that are 1 year or more.
AUTHOR DISCLOSURE STATEMENT
No competing financial interests exist.
FUNDING INFORMATION
No funding was received for this article.
REFERENCES
- 1. Centers for Disease Control and Prevention (CDC). Prevalence and most common causes of disability among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58(16):421–426. [PubMed] [Google Scholar]
- 2. Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin. 2007;2(25):353–371. [DOI] [PubMed] [Google Scholar]
- 3. Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318(5):291–300. [DOI] [PubMed] [Google Scholar]
- 4. Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581–585. [DOI] [PubMed] [Google Scholar]
- 5. Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290(18):2443–2454. [DOI] [PubMed] [Google Scholar]
- 6. Manchikanti L, Singh V, Falco FJE, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. 2014;17(Suppl. 2):3–10. [DOI] [PubMed] [Google Scholar]
- 7. Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996-2016. JAMA. 2020;323(9):863–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Katz JN. Lumbar disc disorders and low-back pain. J Bone Joint Surg Am. 2006;88(Suppl. 2):21–24. [DOI] [PubMed] [Google Scholar]
- 9. Chou R. Low back pain (chronic). Am Fam Physician. 2011;4(84):437–438. [Google Scholar]
- 10. Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992;268(6):760–765. [PubMed] [Google Scholar]
- 11. Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332(7555):1430–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–747. [DOI] [PubMed] [Google Scholar]
- 13. Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379(9814):482–491. [DOI] [PubMed] [Google Scholar]
- 14. Chenot JF, Greitemann B, Kladny B, Petzke F, Pfingsten M, Schorr SG. Clinical practice guideline: Non-specific low back pain. Dtsch Arztebl Int. 2017;114(51–52):883–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J. 2010;10(6):514–529. [DOI] [PubMed] [Google Scholar]
- 16. Markman JD, Czerniecka-Foxx K, Khalsa PS, et al. AAPT diagnostic criteria for chronic low back pain. J Pain. 2020;21(11–12):1138–1148. [DOI] [PubMed] [Google Scholar]
- 17. Costa LC, Maher CG, McAuley JH, et al. Prognosis for patients with chronic low back pain: Inception cohort study. BMJ. 2009;339:b3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Henschke N, Maher CG, Refshauge KM, et al. Prognosis in patients with recent onset low back pain in Australian primary care: Inception cohort study. BMJ. 2008;337(7662):a171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. [DOI] [PubMed] [Google Scholar]
- 20. Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2383. [DOI] [PubMed] [Google Scholar]
- 21. Chapman JR, Norvell DC, Hermsmeyer JT, et al. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine. 2011;36(21 Suppl.):S54–S68. [DOI] [PubMed] [Google Scholar]
- 22. Li Y, Yuan S, Jiang J, Li H, Wang Y. Systematic review and meta-analysis of effects of acupuncture on pain and function in non-specific low back pain. Acupunct Med. 2020;38(4):235–243. [DOI] [PubMed] [Google Scholar]
- 23. Xiang Y, He J, Tian H, Cao B, Li R. Evidence of efficacy of acupuncture in the management of low back pain: A systematic review and meta-analysis of randomised placebo- or sham-controlled trials. Acupunct Med. 2020;38(1):15–24. [DOI] [PubMed] [Google Scholar]
- 24. Nascimento PRC, Costa LOP, Araujo AC, Poitras S, Bilodeau M. Effectiveness of interventions for non-specific low back pain in older adults. A systematic review and meta-analysis. Physiotherapy. 2019;2(105):147–162. [DOI] [PubMed] [Google Scholar]
- 25. Yeganeh M, Baradaran HR, Qorbani M, Moradi Y, Dastgiri S. The effectiveness of acupuncture, acupressure and chiropractic interventions on treatment of chronic nonspecific low back pain in Iran: A systematic review and meta-analysis. Complement Ther Clin Pract. 2017;(27):11–18. [DOI] [PubMed] [Google Scholar]
- 26. Lam M, Galvin R, Curry P. Effectiveness of acupuncture for nonspecific chronic low back pain: A systematic review and meta-analysis. Spine (Phila Pa 1976). 2013;38(24):2124–2138. [DOI] [PubMed] [Google Scholar]
- 27. Hutchinson AJP, Ball S, Andrews JCH, Jones GG. The effectiveness of acupuncture in treating chronic non-specific low back pain: A systematic review of the literature. J Orthop Surg Res. 2012;7:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rubinstein SM, van Middelkoop M, Kuijpers T, et al. A systematic review on the effectiveness of complementary and alternative medicine for chronic non-specific low-back pain. Eur Spine J. 2010;19(8):1213–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yuan J, Purepong N, Kerr DP, Park J, Bradbury I, McDonough S. Effectiveness of acupuncture for low back pain: A systematic review. Spine (Phila Pa 1976). 2008;33(23):E887–E900. [DOI] [PubMed] [Google Scholar]
- 30. Higgins JPT, Thomas J, Chandler J, et al. , eds. Cochrane Handbook for Systematic Reviews of Interventions. 6.2 version (updated February 2021). Cochrane, 2021, Cochrane Training. Online document at: www.training.cochrane.org/handbook/current Accessed February 18, 2021.
- 31. Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. 2012;49(5):1–15. [Google Scholar]
- 32. Langevin HM, Wayne PM. What is the point? The problem with acupuncture research that no one wants to talk about. J Altern Complement Med. 2018;24(3):200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Langevin HM, Churchill DL, Fox JR, Badger GJ, Garra BS, Krag MH. Biomechanical response to acupuncture needling in humans. J Appl Physiol (1985). 2001;91(6):2471–2478. [DOI] [PubMed] [Google Scholar]
- 34. Langevin HM, Churchill DL, Cipolla MJ. Mechanical signaling through connective tissue: A mechanism for the therapeutic effect of acupuncture. FASEB J. 2001;15(12):2275–2282. [DOI] [PubMed] [Google Scholar]
- 35. Lundeberg T, Lund I, Sing A, Näslund J. Is placebo acupuncture what it is intended to be? Evid Based Complement Alternat Med. 2011;2011:932407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Poznanski A, Hsu M, Gracely R, Harris R. (298) Differences in central neural pain processing following acupuncture and sham acupuncture therapy in fibromyalgia. J Pain. 2008;9(4):50. [Google Scholar]
- 37. So EW, Ng EH, Wong YY, Lau EY, Yeung WS, Ho PC. A randomized double blind comparison of real and placebo acupuncture in IVF treatment. Hum Reprod. 2009;24(2):341–348. [DOI] [PubMed] [Google Scholar]
- 38. Linde K, Streng A, Hoppe A, et al. Treatment in a randomized multicenter trial of acupuncture for migraine (ART Migraine). Forsch Komplementmed. 2006;13(2):101–108. [DOI] [PubMed] [Google Scholar]
- 39. Haake M, Müller HH, Schade-Brittinger C, et al. German Acupuncture Trials (GERAC) for chronic low back pain: Randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167(17):1892–1898. [DOI] [PubMed] [Google Scholar]
- 40. Xie C, Wen X, Jiang L, Xie M, Fu WB. Validity of the ‘streitberger’ needle in a Chinese population with acupuncture: A randomized, single-blinded, and crossover pilot study. Evid Based Complement Alternat Med.2013;2013:251603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Park J, White A, Stevinson C, Ernst E, James M. Validating a new non-penetrating sham acupuncture device: Two randomised controlled trials. Acupunct Med. 2002;20(4):168–174. [DOI] [PubMed] [Google Scholar]
- 42. Dhond RP, Witzel T, Hämäläinen M, Kettner N, Napadow V. Spatiotemporal mapping the neural correlates of acupuncture with MEG. J Altern Complement Med. 2008;14(6):679–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hui KK, Liu J, Makris N, et al. Acupuncture modulates the limbic system and subcortical gray structures of the human brain: Evidence from fMRI studies in normal subjects. Hum Brain Mapp. 2000;9(1):13–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: L Erlbaum Associates; 1988. [Google Scholar]
- 45. Leibing E, Leondardt U, Koster G, et al. Acupuncture treatment of chronic low-back pain a randomized, blinded, placebo-controlled trial with 9-month follow-up. Pain. 2002;96(1–2):189–196. [DOI] [PubMed] [Google Scholar]
- 46. Yeung CKN, Leung MCP, Chow DHK. The use of electro-acupuncture in conjunction with exercise for the treatment of chronic low-back pain. J Altern Complement Med. 2003;9(4):479–490. [DOI] [PubMed] [Google Scholar]
- 47. Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169(9):858–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yun M, Shao Y, Zhang Y, et al. Hegu acupuncture for chronic low-back pain: A randomized controlled trial. J Altern Complement Med. 2012;18(2):130–136. [DOI] [PubMed] [Google Scholar]
- 49. Meng CF, Wang D, Ngeow J, Lao L, Peterson M, Paget S. Acupuncture for chronic low back pain in older patients: A randomized, controlled trial. Rheumatology (Oxford). 2003;42(12):1508–1517. [DOI] [PubMed] [Google Scholar]