Abstract
The stringent restrictions from shelter-in-place (SIP) policies placed on hospital operations during the COVID-19 pandemic led to a sharp decrease in planned surgical procedures. This study quantifies the surgical rebound experienced across a neurosurgical service post SIP restrictions in order to guide future hospital programs with resource management. We conducted a retrospective review of all neurosurgical procedures at a public Level 1 trauma center between February 15th to August 30th for the years spanning 2018–2020. We categorized patient procedures into four comparative one-month periods: pre-SIP; SIP; post-SIP; and late recovery. Patient procedures were designated as either cranial; spinal; and other; as well as Elective or Add-on (Urgent/Emergent). Categorical variables were analyzed using χ2 tests and Fisher’s exact tests. A total of 347 cases were reviewed across the four comparative periods and three years studied; with 174 and 152 spinal and cranial procedures; respectively. There was a proportional increase; relative to historical controls; in total spinal procedures (p-value < 0.001) and elective spinal procedures (p-value < 0.001) in the 2020 SIP to Post-SIP. The doubling of elective spinal cases in the Post-SIP period returned to historical baseline levels in three months after SIP restrictions were lifted. Total cranial procedures were proportionally increased during the SIP period relative to historical controls (p-value = 0.005). We provide a census on the post-pandemic neurosurgical operative demands at a major public Level 1 trauma hospital, which can potentially be applied for resource allocations in other disaster scenarios.
Abbreviations: SIP, Shelter-in-Place
Keywords: Cranial, COVID-19, Elective, Neurosurgery, Shelter-in-place, Spine
1. Introduction
As a response to the spread of the COVID-19 virus in Spring 2020; the California government; in-line with many governments around the globe; enacted a shelter-in-place (SIP) protocol curtailing unnecessary individual movement to stop the spread of the virus. During this period spanning March 2020 to May 2020; many hospitals and their surgical departments; neurosurgery included; faced temporary cessations of elective procedures and decreased patient volume [1], [2], [3], [4], [5], [6]. In previous work; we noted that the SIP protocols resulted in an acute; significant decrease in the total volume of traumatic brain injury and spinal fractures seen in the Santa Clara Valley Level 1 trauma centers [6].
Few studies have since reported on how neurosurgical practice was impacted in the post-SIP period. The restrictive measures are suspected to have delayed or forfeited neurosurgical care. Identifying the shifts in neurosurgical case flow during and post-pandemic will enable us to optimize resource allocation during future pandemics and improve patient access to neurosurgical care.
In this study; we analyzed the complete census of neurosurgical procedures in the months following the reinstatement of elective surgeries at the senior author’s hospital situated in one of the emerging centers of the COVID-19 pandemic. We hypothesized that lifting the SIP restrictions on elective neurological surgeries will lead to a rebound effect on both neurosurgical case-volume and hospital billing.
2. Methods
We performed a retrospective chart review with IRB approval at Santa Clara Valley Medical Center (SCVMC) during the time period February 15th; 2018; to August 30th; 2020. The start of the SIP period was formally established on March 16th; 2020 and ended on May 4th; 2020. To look at the effects of SIP; comparative periods were identified in months before and after SIP. We categorized patient procedures into one-month groups: pre-SIP (February 15th – March 15th; 2020); SIP (March 15th - April 15th); post-SIP (June 1st – June 30th); and late-recovery (August 1st – August 30th). One-month blocks were selected to capture the most acute response to the SIP and to enable consistent comparison between periods. Additionally; to control for seasonal effects; corresponding periods were identified in years preceding SIP; 2018 and 2019 case counts were summed to provide a historic control for each period.
The patient procedure record included all neurosurgical procedures seen within each time period across all three years at SCVMC. Patient records included procedure date; procedure type (cranial; spinal; other) and scheduling status (Elective; Add-on). Add-on cases were defined as an aggregate of urgent and emergent procedures.
Cranial procedures included: craniectomy; craniotomy; cranioplasty; burr hole placement; pituitary resection; endarterectomies; Ommaya reservoirs; and ventriculoperitoneal shunts. Spinal surgeries included: discectomies; corpectomies; decompressions; fusions; baclofen pumps; and lumboperitoneal shunts. An Other category included all remaining other procedures (Supplementary Table 1).
Financial data included physician and hospital billing records which corresponded to each patient’s procedure record as derived from procedure codes and Current Procedural Terminology codes.
2.1. Statistics
Categorical variables were analyzed by chi-squared testing; or Fisher’s exact test when appropriate. Significance was set at 0.05.
3. Results
3.1. Total case counts
In total; 348 cases were identified across the four time periods and three years studied; of which 174 were spinal surgeries and 152 were cranial surgeries. During the corresponding SIP time periods; there were a total of 37; 31 and 21 cases in the years 2018; 2019; and 2020; respectively (Table 1 ; Fig. 1 ). In Post-SIP; there were a total of 26; 17 and 34 cases in 2018; 2019; and 2020.
Table 1.
Operative census and proportion of Elective and Add-on surgeries, either cranial or spinal, during the Pre-SIP, SIP, Post-SIP, and Late phases for years 2018–2020. SIP, shelter-in place. SIP; shelter in place.
|
Pre-SIP |
SIP |
Post-SIP |
Late |
|||||
|---|---|---|---|---|---|---|---|---|
| Cranial | N | N | N | N | ||||
| 2018 | 13 | 15 | 10 | 14 | ||||
| 2019 | 14 | 10 | 8 | 13 | ||||
| 2020 | 12 | 15 | 12 | 16 | ||||
| Spine | ||||||||
| 2018 | 11 | 20 | 12 | 15 | ||||
| 2019 | 15 | 19 | 8 | 18 | ||||
| 2020 | 16 | 5 | 22 | 13 | ||||
| Total Historical | 59 | 68 | 43 | 64 | ||||
| Total 2020 | 29 | 21 | 34 | 30 | ||||
| N | % | N | % | N | % | N | % | |
| Total Cranial 2020 | 12 | 41.4% | 15 | 71.4% | 12 | 35.3% | 16 | 53.3% |
| Total Spinal 2020 | 16 | 55.2% | 5 | 23.8% | 22 | 64.7% | 13 | 43.3% |
| Other | 1 | 3.4% | 1 | 3.4% | 0 | 0.0% | 1 | 3.4% |
| Total Cranial Historical | 27 | 45.8% | 25 | 36.8% | 18 | 41.9% | 27 | 42.2% |
| Total Spinal Historical | 26 | 44.1% | 39 | 57.4% | 20 | 46.5% | 33 | 51.6% |
| Total Other Historical | 6 | 10.2% | 4 | 5.9% | 5 | 11.6% | 4 | 6.3% |
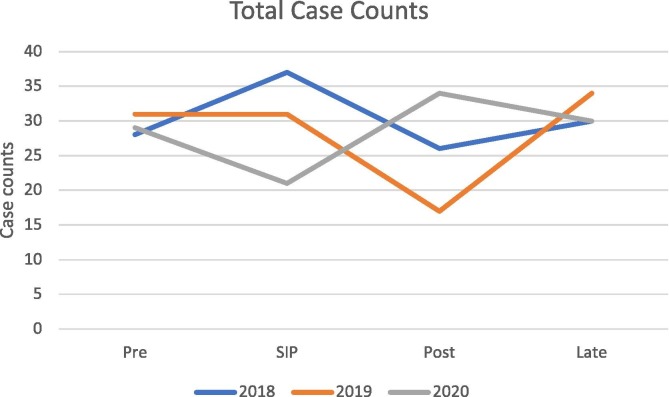
Fig. 1.
Line graph depicting the total case counts at Santa Clara Valley Medical Center during the Pre-SIP; SIP; Post-SIP; and Late phases for years 2018–2020. SIP; shelter-in place.
Between SIP and Post-SIP periods of 2020; there was a significant proportional increase in the total number of cases relative to historical controls. (2020: SIP 21 to Post-SIP 34; Historical control: SIP 68 to Post-SIP 43; χ2 = 7.88; p-value = 0.005; Table 1 ; Fig. 1). There were no significant differences in case counts between Pre-SIP and SIP or between SIP and Late phases (2020: Pre-SIP 29 to SIP 21 vs Historical control: Pre-SIP 59 to SIP 68; χ2 = 1.91; p-value = 0.167 and 2020: Pre-SIP 21 to Late 30 vs Historical control: Pre-SIP 68 to Late 64; χ2 = 1.57; p-value = 0.210; Table 1 ; Fig. 2 ).
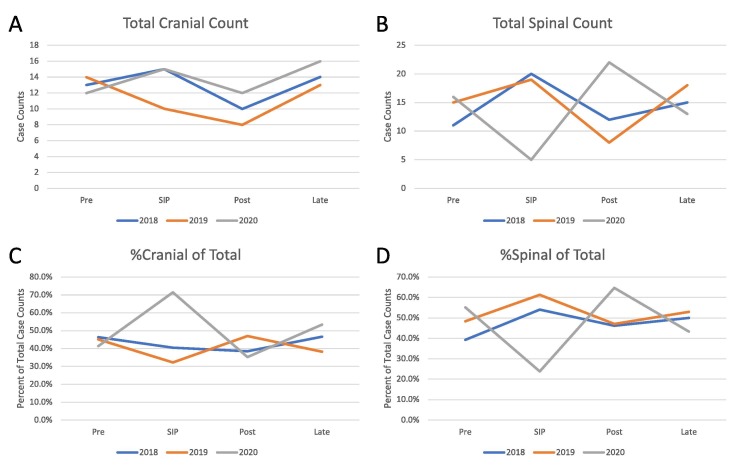
Fig. 2.
Line graphs depicting the census of cranial and spinal surgeries during the Pre-SIP; SIP; Post-SIP; and Late phases for years 2018–2020. A) Total volume of cranial surgeries. B) Total volume of spinal surgeries. C) Proportion of total cases which were cranial surgeries. D) Proportion of total cases which were spinal surgeries. SIP; shelter-in place.
3.2. Stratification by procedure type – Post-SIP
The proportion of SIP to Post-SIP 2020 spinal cases was significantly increased relative to historical controls (2020: SIP 5 to Post-SIP 22 vs Historical control: SIP 39 to Post-SIP 20; χ2 = 16.8; p-value < 0.001; Table 2 ; Fig. 2). The proportion of SIP to Post-SIP 2020 cranial cases remained similar relative to historical controls (2020: SIP 15 to Post-SIP 12 vs Historical control: SIP 25 to Post-SIP 18; χ2 = 0.045; p-value = 0.831; Table 2 ; Fig. 2).
Table 2.
Operative census and proportion of cranial and spinal surgeries during the Pre-SIP, SIP, Post-SIP, and Late phases for years 2018–2020. SIP, shelter-in place. SIP; shelter in place.
| Total | Cranial | Spinal | Other/Minor | |
|---|---|---|---|---|
| Add On | 131 | 82 | 46 | 3 |
| Elective | 217 | 70 | 128 | 19 |
| Cranial Elective | Pre | SIP | Post | Late |
| Historical | 12 | 14 | 10 | 15 |
| 2020 | 4 | 4 | 5 | 6 |
| Cranial Add-on | ||||
| Historical | 15 | 11 | 8 | 12 |
| 2020 | 8 | 11 | 7 | 10 |
| Spinal Elective | Pre | SIP | Post | Late |
| Historical | 20 | 31 | 17 | 22 |
| 2020 | 9 | 3 | 17 | 9 |
| Spinal Add-on | ||||
| Historical | 6 | 8 | 3 | 11 |
| 2020 | 7 | 2 | 5 | 4 |
During Post-SIP; there was no significant change in the proportion of cranial to spinal procedures in Post-SIP 2020; relative to historical control (Post-SIP 2020: 12 cranial to 22 spinal vs Post-SIP Historical control: 18 cranial to 20 spinal; χ2 = 1.08; p-values = 0.299).
3.3. Stratification by procedure type – During SIP
The proportion of total cranial cases during SIP 2020 was significantly higher than that of historical controls (SIP 2020: 15 cranial to 6 non-cranial vs Historical control: 25 cranial to 43 non-cranial; χ2 = 7.79; p-value = 0.005; Table 1 ; Fig. 2). Conversely; the proportion of total spinal cases in SIP 2020 was significantly lower relative to that of historical controls (SIP 2020: 5 spinal to 21 non-spinal vs Historical control: 39 spinal to 29 non-spinal; χ2 = 11.0; p-value = 0.001; Fisher’s exact; Table 1 ; Fig. 2).
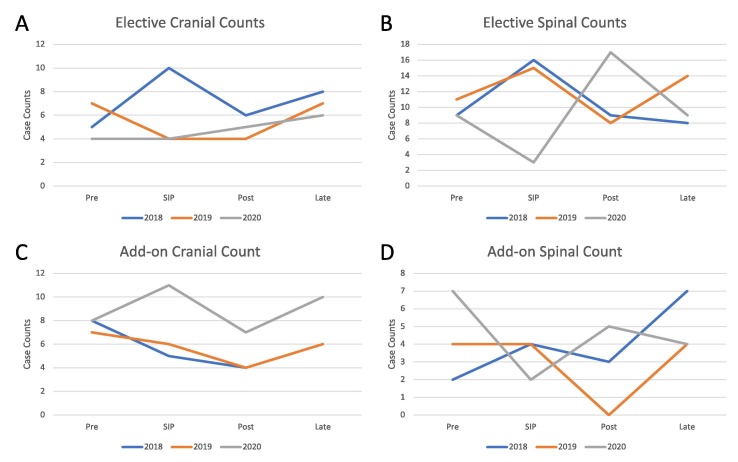
3.4. Stratification by scheduling status
The proportion of SIP to Post-SIP 2020 elective cranial procedures did not significantly change relative to that of historical controls (2020: SIP 4 to Post-SIP 5 and Historical control: SIP 14 to Post-SIP 10; Fisher’s exact; p-value = 0.697; Table 2 ; Fig. 3 ). The proportion of SIP to Post-SIP 2020 Add-on cranial procedures did not significantly change either (2020: SIP 11 to Post-SIP 7 vs Historical: SIP 11 to Post-SIP 8; χ2 = 0.040; p-value = 0.842; Table 2 ; Fig. 3).
Fig. 3.
Line graphs depicting the census of Elective and Add-on surgeries; either cranial or spinal during the Pre-SIP; SIP; Post-SIP; and Late phases for years 2018–2020. A) Total volume of Elective cranial surgeries. B) Total volume of Elective spinal surgeries. C) Total volume of Add-on cranial surgeries. D) Total volume of Add-on spinal surgeries. SIP; shelter-in place.
The proportion of SIP to Post-SIP 2020 elective spinal procedures was significantly increased relative to that of historical control (2020: SIP 3 to Post-SIP 17 vs Historical control: SIP 31 to Post-SIP 17 cases; χ2 = 13.9; p-value < 0.001; Table 2 ; Fig. 3). There was no significant change in the proportion of SIP to Post-SIP 2020 Add-on spinal cases (2020: SIP 2 to Post-SIP 5 vs Historical control: SIP 8 to Post-SIP 3; Fisher’s exact; p-value = 0.145; Table 2 ; Fig. 3).
3.5. Hospital billing
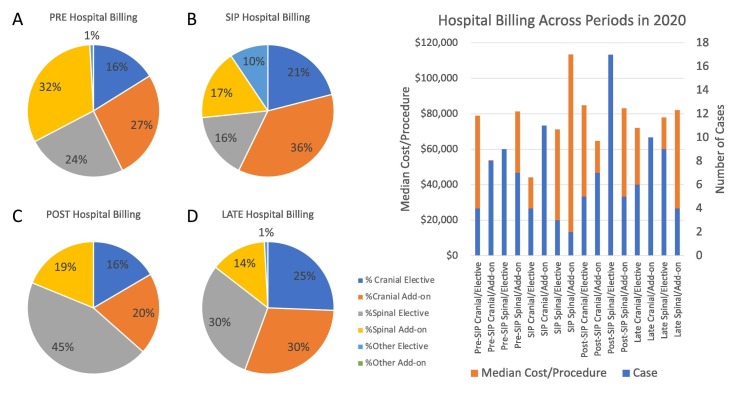
A similar stratification of procedures by procedure type and scheduling status was applied to hospital procedural billing (Fig. 4 ).
Fig. 4.
Pie charts depicting the proportion of total hospital billing; categorized by indication (Cranial; Spinal; or Other) and Scheduling Status (Elective; Add-on). A) Hospital billing during the Pre-SIP time period. B) Hospital billing during the SIP time period. C) Hospital billing during the Post-SIP time period. D) Hospital billing during the Late time period. SIP; shelter-in place.
4. Discussion
The impact of an acute pause in elective procedures has had delayed consequences across surgical subspecialties; including operative neurosurgery. This study describes the resulting redistribution of cases at a public; Level 1 trauma center at one of the first epicenters of the COVID-19 pandemic. An adjustment in operative activity appears to have occurred in the immediate period following relaxation of restrictive procedural policies; primarily due to a rebound influx of elective spinal procedures. Although other healthcare communities will have experienced a different response to local pandemic-related conditions and policies; the general trends we observed can serve as a template for future hospital responses to shelter-in-place policies.
4.1. Changes in procedural Indications
Importantly we identified that this post-pandemic policy surge primarily occurred with Elective spinal bookings. This more than doubled in the immediate period following an SIP practice; before resolving back to normal levels. The number of elective spine procedures matched the sum of the two years prior. A similar decline in elective spinal procedures was cited in a multi-institution survey by the Lumbar Spine Research Society with most providers [7]. Within the first two months of the pandemic; there was a 90% decrease in operations; primarily limited to addressing cauda equina syndrome; symptomatic lumbar trauma; and spinal cord tumors which were symptomatic [7].
Meanwhile; cranial cases dominated the attention of the SIP period. This is perhaps driven by an increase in the number of Add-on cranial cases. For example; Add-on cranial cases in SIP 2020 matched the sum from the years before (11 in 2020; 11 in 2018–2019). Moreover; during SIP there was an increased proportion of Add-on cranial procedures (52.4%) to the point that they became the most represented subcategory among all cranial and spinal procedures. This is converse to historical periods when Add-on spinal procedures were the more dominant subgroup (45.6%).
Our observations suggest a rebalancing of cranial surgical needs during SIP and post-SIP periods. A trend towards increased Add-on cranial procedures can possibly be attributed to the more emergently scheduled status of late presenting or emergent indications that were prioritized during the pandemic. The decrease in Elective cranial cases may be partially related to how low grade and asymptomatic tumors were deferred care [8], [9], [10]. Pessina et al. documented their experiences at a cancer referral center and described about one-third fewer cases [11]. Moreover; we propose that some of these procedures included an increased representation of temporizing measures such as ventriculoperitoneal shunt revisions; some of which may have presented electively. Such patients may have been less willing to seek proactive work up from the outpatient route.
Using the billing information as an approximation of resource utilization; we can see that there were likely decreases in revenue per cranial procedure during SIP 2020. This may stem from less invasive or less complex cases taking place. Many of the emergent-related trauma or CSF diverting operations likely fall within this category [12]. Among all the cranial and spinal procedural subtypes; cranial procedures from SIP 2020 were with the lowest median hospital costs per procedure. The more resource intensive spinal cases can perhaps aid with revenue smoothing; as evidenced by the more expensive Elective spinal cases in the Post-SIP 2020 period. This is consistent with Arnold et al.’s survey data showing that among spinal procedures; lumbar fusion was the least frequently performed [7].
4.2. Finite backlogs to operative restriction
Importantly; we illustrate how the deferred cases from SIP can be addressed within a narrow time frame. This has major implications for hospital management; where concerns were raised over having enough supplies for an emergency surge and how delays or rescheduling would be feasibly accommodated. Similarly; Ceraudo et al. documented a two-months delay at an Italian pediatric referral center; however; there was limited discussion on the role of shunt management [13]. The impact of delayed care for stroke management has consistently described more severe presentation; delayed time to presentation; and increased rates of vasospasm [14], [15].
Logistically; there is a recurring theme across the literature that a major reason for the decreased intake of patients was in part related to logistical challenges of transporting patients [7], [11], [15]. This has been in part attributed to decreased patient comfort interfacing with the medical system; as well as comfort with institutional transfer. Adaptations are needed as our healthcare system moves from a pandemic to an endemic approach phase in management.
At the very least; our data seems to confirm a need to accommodate more elective spinal procedures post-SIP. This will require increased administrative; case management; and social work outreach. Survey data has shown that patients demanding lower-tier procedures for indications such spinal cord stimulators are willing to participate in the necessary quarantine steps to seek care [16]. Prior work on the pandemic phase care of high-risk glioma patients confirmed the safety of neurosurgical admissions [11]. Assuming hospitals are well staffed and stocked during future emergency restrictions; there is the potential for safely redistributing the elective spine cases into analogous SIP and Post-SIP periods.
The described experience reaffirms general principles for future resource allocation during operative restrictions and their recovery. An important element remains the triage of essential and non-essential surgery [17]. This releases personnel, facilities, and materials that can be redeployed for the emergent population. This information combined with the neurosurgical operative census can guide how department leaders redeploy personnel to critical units [18]. As a caveat, the neurosurgery community must remain flexible and understand that the patterns and trends seen here may not match at another institution of different size, case-mix, and restriction-severity. Fortunately, as a result of the COVID-19 experience, we have new literature surrounding the neurosurgical census in the periods following acute operative restrictions which can be used to guide future rationing [1], [3], [5], [6], [19].
Meanwhile, the normalization of practices should anticipate at least two to three months. We believe that our hospital experienced a rather mild to moderate exposure to the pandemic, suggesting the described recovery period is perhaps shorter than would be necessary at more affected institutions. Similar recovery timelines have been described with other institutions [13], [19]. Using staffing again as an example, this can be important information for staff shift or holiday scheduling. Documented anticipation of the recovery is essential, and the use of central dashboards or interval census reports can help providers forecast the relief on resources that can be returned to the full complement of procedures. Meanwhile, the use of telemedicine, which has been widely received should help with patient education and contingency scheduling [20], [21].
4.3. Limitations
This study is subject to the limitations common to retrospective studies. Not all clinical variables are available given the information provided. Given the database available; further specification of diagnoses was not permissible. The small sample size also restricts statistical power; potentially obscuring otherwise significant relationships. One advantage of our study is the inclusivity of a broad set of indications in neurosurgery; including the care for CSF diverting procedures and implants which still contribute to the practice of nearly all general neurosurgical practices.
Additionally; external validity is contingent on how our healthcare setting compares to other hospital systems; surrounding providers; implemented policies; local enforcement; and patient preferences. For example; although cranial cases remained steady within our community; the indications treated may not match elsewhere; such as at cancer and stroke centers. Changes in Elective or Add-on cranial cases may differ for a larger neurosurgical service or one with a different case mix.
5. Conclusion
The impact of the public health policy restrictions on operative neurosurgical practice extended beyond the initial months of pandemic onset. These findings have important parallels for other surgical practices as well as future crises management. These findings demonstrate how neurosurgical triage of elective spinal procedures compose a significant group of patients that are potentially deferred care and critical for resource budgeting across periods. Additional work is needed to investigate how these trends extend to additional hospital settings and networks.
6. Disclosure of Funding
MZ is funded by the National Institutes of Health (5T32CA009695-27). This research did not receive any specific grant from funding agencies in the public; commercial; or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jocn.2022.04.033.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Figueroa J.M., Boddu J., Kader M., Berry K., Kumar V., Ayala V., et al. The Effects of Lockdown During the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Pandemic on Neurotrauma-Related Hospital Admissions. World Neurosurg. 2021;146:e1–e5. doi: 10.1016/j.wneu.2020.08.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir. 2020;162(6):1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koester S.W., Catapano J.S., Ma K.L., Kimata A.R., Abbatematteo J.M., Walker C.T., et al. COVID-19 and Neurosurgery Consultation Call Volume at a Single Large Tertiary Center With a Propensity-Adjusted Analysis. World Neurosurg. 2021;146:e768–e772. doi: 10.1016/j.wneu.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raneri F., Rustemi O., Zambon G., Del Moro G., Magrini S., Ceccaroni Y., et al. Neurosurgery in times of a pandemic: a survey of neurosurgical services during the COVID-19 outbreak in the Veneto region in Italy. Neurosurg Focus FOC. 2020;49(6):E9. doi: 10.3171/2020.9.FOCUS20691. [DOI] [PubMed] [Google Scholar]
- 5.Saad H., Alawieh A., Oyesiku N., Barrow D.L., Olson J. Sheltered Neurosurgery During COVID-19: The Emory Experience. World Neurosurg. 2020;144:e204–e209. doi: 10.1016/j.wneu.2020.08.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang M., Zhou J., Dirlikov B., Cage T., Lee M., Singh H. Impact on neurosurgical management in Level 1 trauma centers during COVID-19 shelter-in-place restrictions: The Santa Clara County experience. J Clin Neurosci. 2021;88:128–134. doi: 10.1016/j.jocn.2021.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arnold P.M., Owens L., Heary R.F., Webb A.G., Whiting M.D., Vaccaro A.R., et al. Lumbar Spine Surgery and What We Lost in the Era of the Coronavirus Pandemic: A Survey of the Lumbar Spine Research Society. Clin Spine Surg. 2021;34(10):E575–E579. doi: 10.1097/BSD.0000000000001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azab M.A., Azzam A.Y. Impact of COVID-19 pandemic on the management of glioma patients around the world. An evidence-based review. Brain Disord. 2021;2:100012. doi: 10.1016/j.dscb.2021.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernhardt D., Wick W., Weiss S.E., Sahgal A., Lo S.S., Suh J.H., et al. Neuro-oncology Management During the COVID-19 Pandemic With a Focus on WHO Grade III and IV Gliomas. Neuro Oncol. 2020;22:928–935. doi: 10.1093/neuonc/noaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tzeng C.-W., Teshome M., Katz M.H.G., Weinberg J.S., Lai S.Y., Antonoff M.B., et al. Cancer Surgery Scheduling During and After the COVID-19 First Wave: The MD Anderson Cancer Center Experience. Ann Surg. 2020;272(2):e106–e111. doi: 10.1097/SLA.0000000000004092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pessina F., Navarria P., Bellu L., Clerici E., Politi L.S., Tropeano M.P., et al. Treatment of patients with glioma during the COVID-19 pandemic: what we learned and what we take home for the future. Neurosurg Focus. 2020;49(6):E10. doi: 10.3171/2020.9.FOCUS20704. [DOI] [PubMed] [Google Scholar]
- 12.Ahluwalia R., Rocque B.G., Shannon C.N., Blount J.P. The impact of imposed delay in elective pediatric neurosurgery: an informed hierarchy of need in the time of mass casualty crisis. Childs Nerv Syst. 2020;36(7):1347–1355. doi: 10.1007/s00381-020-04671-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ceraudo M., Balestrino A., Cama A., Macrina G., Piatelli G., Consales A. Pediatric Neurosurgery After the COVID-19 Pandemic: Management Strategies from a Single Pediatric Hospital in Italy. World Neurosurg. 2021;146:e1079–e1082. doi: 10.1016/j.wneu.2020.11.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aboukaïs R., Devalckeneer A., Boussemart P., Vromant A., Bricout N., Verdin M.-F., et al. Impact of COVID-19 pandemic on patients with intracranial aneurysm rupture. Clin Neurol Neurosurg. 2021;201:106425. doi: 10.1016/j.clineuro.2020.106425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.White T.G., Martinez G., Wang J., Gribko M., Boltyenkov A., Arora R., et al. Impact of the COVID-19 Pandemic on Acute Ischemic Stroke Presentation, Treatment, and Outcomes. Stroke Res Treat. 2021;2021:1–8. doi: 10.1155/2021/8653396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baranidharan G., Bretherton B., Eldabe S., Mehta V., Thomson S., Sharma M.L., et al. The impact of the COVID-19 pandemic on patients awaiting spinal cord stimulation surgery in the United Kingdom: a multi-centre patient survey. Br J Pain. 2021;15(3):282–290. doi: 10.1177/2049463720948092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mummaneni P.V., Burke J.F., Chan A.K., Sosa J.A., Lobo E.P., Mummaneni V.P., et al. Consensus-based perioperative protocols during the COVID-19 pandemic. J Neurosurg Spine. 2021;34(1):13–21. doi: 10.3171/2020.6.SPINE20777. [DOI] [PubMed] [Google Scholar]
- 18.Raith E.P., Luoma A.M.V., Earl M., Dalal M., Fairley S., Fox F., et al. Repurposing a Neurocritical Care Unit for the Management of Severely Ill Patients With COVID-19: A Retrospective Evaluation. J Neurosurg Anesthesiol. 2021;33(1):77–81. doi: 10.1097/ANA.0000000000000727. [DOI] [PubMed] [Google Scholar]
- 19.Wali A.R., Ryba B.E., Kang K., Santiago-Dieppa D.R., Steinberg J., Diaz-Aguilar L.D., et al. Impact of COVID-19 on a Neurosurgical Service: Lessons from the University of California San Diego. World Neurosurg. 2021;148:e172–e181. doi: 10.1016/j.wneu.2020.12.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blue R., Yang A.I., Zhou C., De Ravin E., Teng C.W., Arguelles G.R., et al. Telemedicine in the Era of Coronavirus Disease 2019 (COVID-19): A Neurosurgical Perspective. World Neurosurg. 2020;139:549–557. doi: 10.1016/j.wneu.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El Naamani K., Abbas R., Mukhtar S., El Fadel O., Sathe A., Kazan A.S., et al. Telemedicine during and post-COVID 19: The insights of neurosurgery patients and physicians. J Clin Neurosci. 2022;99:204–211. doi: 10.1016/j.jocn.2022.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.